Abstract
Cough is the often presenting feature of several non-life-threatening and life-threatening conditions, including obstructive airway disease. It is a vital reflex of the respiratory tract to clear the upper airways. Suppression of this reflex may lead to retention of airway secretions and respiratory infections [1]. A thorough medical history is important to denote whether a cough is acute (<3 weeks), subacute (3–8 weeks), or chronic (>8 weeks). This chapter will focus only on chronic cough.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Chronic Obstructive Pulmonary Disease
- Force Vital Capacity
- Peak Expiratory Flow
- Chronic Cough
- Chronic Obstructive Pulmonary Disease Exacerbation
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Chronic Cough
Cough is often the presenting feature of several non-life-threatening and life-threatening conditions, including obstructive airway disease. It is a vital reflex of the respiratory tract to clear the upper airways. Suppression of this reflex may lead to retention of airway secretions and respiratory infections [1]. A thorough medical history is important to denote whether a cough is acute (<3 weeks), subacute (3–8 weeks), or chronic (>8 weeks). This chapter will focus only on chronic cough.
Chronic cough can present difficulty in diagnosis and result in complications such as vomiting, rib fractures, urinary incontinence, syncope, muscle pain, fatigue, and depression [1]. The most common causes of chronic cough with normal chest radiograph in descending order, include upper airway cough syndrome (UACS) or formerly known as postnasal drip syndrome , chronic obstructive pulmonary disease (COPD), asthma and gastro-esophageal reflux disease (GERD), cigarette smoking or second hand exposure, and ACE-inhibitor use [1, 2]. These causes may occur alone or in combination. The diagnostic goal is to exclude serious conditions that present with chronic cough.
Cough is the primary feature of chronic cough. It is important to note the time of day the cough is most prominent, associated sputum production, as well as signs of drainage in the posterior pharynx, throat clearing, nasal discharge, cobblestone appearance of the oropharyngeal mucosa, and mucus in the oropharynx are relatively sensitive findings but are nonspecific for UACS [3]. If associated with heartburn, water brash, and belching and/or globus sensation most likely GERD is the cause. It is important to understand that cough alone can still be the only presenting feature of UACS , GERD, or cough variant asthma. Certainly, if the patient is taking an ACE-inhibitor, it may need to be discontinued as it is a possible cause of chronic cough.
After completion of a thorough history and physical examination, it may be helpful to obtain a chest radiograph and pulmonary function testing, bronchial provocation challenge, and sputum eosinophilia. Further investigation may be warranted and can include 24 h esophageal pH monitoring, upper endoscopy or video fluroscopic swallow evaluation, barium esophagram, sinus imaging, high resonance CT scan, bronchoscopy, echocardiogram, and environmental assessment [4].
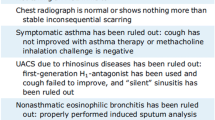
Chronic cough can be multifactorial. If a patient has limited response to monotherapy, it is important to consider a treatment plan that addresses multiple etiologies. See Fig. 1.
Recommended management of chronic cough ≥15 years of age [2]
Asthma
Asthma, one cause of ongoing cough, is a common respiratory disorder, characterized by periods of reversible airflow obstruction, inflammation, and hyperresponsiveness of the airways. Unfortunately, in the last 10 years, the number of persons with asthma in the USA has increased by 28 % [2]. Approximately 39.5 million people, including 10.5 million children, in the USA have been affected by asthma. In 2010, asthma accounted for 3,404 deaths, 439,400 hospitalizations, 1.8 million emergency department (ED) visits, and 14.2 million physician office visits [5, 6].
Asthma exacerbations are triggered by multiple factors including exercise, airway infections, airborne allergens (e.g., pollen, mold, animal dander, dust mites), occupational exposures, and air pollution (e.g., environmental tobacco smoke, particulate matter, and volatile organic compounds) [7, 8]. Although there is no cure, asthma can be controlled with appropriate medical therapies by avoidance of environmental exposures, particularly environmental exposures that may trigger an attack [7].
Common symptoms of asthma are wheezing, coughing, shortness of breath, and chest tightness or pain. Asthma attacks may be classified as mild, moderate, or severe enough to become life-threatening events [4]. The physical signs may be wheezing, rhonchi, or course breath sounds on auscultation. In addition, the patient may appear in respiratory distress with signs of accessory muscle usage, nasal flaring or grunting (in children), and altered mental status. Children may present will nocturnal cough only, while geriatric patients may present with chronic cough in absence of wheezing. In cases when wheezing occurs with exercise alone, the diagnosis of exercise-induced asthma (EIB) should be considered (Table 1).
Asthma is diagnosed on spirometry by observing a change in FEV1 following bronchodilator administration . An increase of more than 12 % in patients 5–18 years of age, or more than 12 % and more than 200 mL in adults confirms the diagnosis of asthma. Although no single parameter has been identified to assess exacerbation severity, lung function is a useful method of assessment, with a PEF of 40 % or less of predicted function indicating a severe attack in patients 5 years or older [4].
If both the FEV1/FVC ratio and the FVC are low, the patient has a mixed defect. Alternatively, a restrictive pattern is indicated by an FVC below the fifth percentile based on NHANES III data in adults, or less than 80 % in patients 5–18 years of age. If a restrictive pattern is detected, a consideration for pulmonary referral should be made for further evaluation and treatment.
Asthma exacerbation is defined as an increase in wheezing with or without hypoxia. If hypoxemia is present despite initial bronchodilator therapy, hospitalization should be considered. Management of asthma exacerbation is very similar to COPD exacerbation management with the exception of antibiotic therapy if no clear diagnosis of a bacterial infection is found. See Fig. 2.
In order to determine appropriate medical therapy, it is important to assess asthma severity. This can be done during an office visit by either assessing symptoms through asthma assessment tools (ACT, ACQ, or ATAQ) or performing a peak expiratory flow (PEF) rate . There are well-validated questionnaires such as the asthma control test (ACT), asthma control questionnaire (ACQ), or asthma therapy assessment questionnaire (ATAQ) tools that can assist in assessment of asthma severity [4]. A PEF of 80 % or more of predicted or personal best categorizes patients’ asthma as well controlled; however, less than 60 % of predicted or personal best indicates very poor control. Either technique has similar benefits in determining asthma control.
Asthma should be reassessed frequently if stepping up therapy or deescalating therapy.
The asthma severity determines the optimal initial therapy regimen (Tables 2 and 3). Close follow-up is warranted to reassess response to treatment and need for additional step up in therapy (Fig. 3). Treating more aggressively to obtain rapid control and then deescalating therapy to a maintenance regimen may be a more optimal approach. All patients regardless of severity should be provided a short-acting beta agonist. The use of a spacer with administration of metered-dose inhaler promotes drug distribution and effectiveness.
Maintaining asthma control [9]
Arterial blood gas (ABG) is helpful in the inpatient setting when a patient has an exacerbation of asthma and is associated with moderate to severe hypoxia due to hypoventilation. If severe hypoxemia or hypercapnia is detected on ABG, it indicates the need for assisted ventilator support.
Certainly if avoidance is not helpful, there may be a role for antihistamines and nasal sprays. Consideration of a referral to an allergist may be helpful if allergy desensitization may be helpful for patients with severe asthma.
COPD
Often, the diagnosis of COPD is evident based on patient’s history and physical examination alone. Any patient who has chronic dyspnea, cough, or sputum production along with a history of smoking exposure should be evaluated for COPD. However, pulmonary function test (PFT) is required to make a diagnosis of COPD [11]. Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality in the USA and worldwide. Though it is one of the most preventable diseases, it affects more than 5 % of the US adults, and it is the third leading cause of death [9]. It is characterized by persistent airflow obstruction that is usually progressive and is not fully reversible. Cigarette smoking is the leading cause of COPD. However, long-term exposure to other irritants such as air pollution, chemical fumes, and household smoke can also contribute to COPD. Also, according to the WHO, passive smoking carries serious risks, especially for children and those chronically exposed [10]. The other rare cause of COPD is a genetic factor that causes deficiency of alpha-1 antitrypsin deficiency. If patient presents with COPD symptoms before the age of 40, consideration should be made to screen for alpha-1 antitrypsin deficiency .
The most common presenting symptoms of COPD include chronic cough, dyspnea that worsens on exertion, and chronic sputum production. COPD can remain unrecognized for number of years given its slowly progressive nature.
On physical examination , patients may have wheezing, decreased breath sounds on auscultation, or have completely normal exam. Since smoking is the most common cause of COPD, it is not uncommon that patients may appear older than stated age. During severe exacerbations, the patient may have labored breathing, appear altered in regards to mental status, and be acutely hypoxic.
Pulmonary Function Testing and Spirometry
Most helpful informations of the PFT are the forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), the FEV1/FCV ratio, and the peak expiratory flow rate (PEFR). The postbronchodilator FEV1/FVC < 0.70 or below the fifth percentile, based on data from the Third National Health and Nutrition Examination Survey (NHANES III) in adults, and less than 85 % in patients 5–18 years of age establishes the diagnosis. Severity of disease is further based on FEV1 (Table 1 in Chap. 6, “Population Health: Who Are Our Patients?”).
Patients should be routinely assessed in the clinic about their symptoms of COPD through the use of the COPD assessment test (CAT) and modified British Medical Research Council questionnaire (mMRC) score [12]. This helps to classify patients into four groups: group A (less symptoms, low risk), group B (more symptoms, less risk), group C (less symptoms, high risk), and group D (more symptoms, high risk) [11].
Laboratory and Imaging
Even though no lab is needed for diagnosis of COPD, different lab tests are sometimes ordered depending on the degree of suspicion for alternative diagnosis. For instance, CBC can be done for assessment of anemia as it can also present with dyspnea. Other labs that can be done depending on suspicion of other diagnosis may include plasma BNP for heart failure and urea nitrogen/creatinine for underlying kidney disease. An elevated serum bicarbonate may indirectly suggest chronic hypercapnia [13]. Arterial blood gas (ABG) is helpful in the inpatient setting when a patient has an exacerbation of COPD and is associated with moderate to severe hypoxia due to hypoventilation. If severe hypoxemia or hypercapnia is detected on ABG, it indicates the need for assisted ventilator support.
Though chest radiography or any other imaging is not indicated in diagnosis of COPD, there are a few radiographic features that suggest COPD such as: a flat diaphragmatic contour due to hyperinflation and increased retrosternal airspace on a lateral radiograph.
Special Testing
If a patient presents with symptoms of COPD and has persistent airflow obstruction prior to age of 40, especially in nonsmoker patient, testing for alpha-1 antitrypsin (AAT) should be considered. A serum level of AAT below 57 mg/dL is diagnostic [11].
Management
The approaches to management of both asthma and COPD are very similar and include avoidance, immunotherapy , exercise, pharmacological therapies, and psychological support.
COPD exacerbation can be defined as baseline change in patient’s dyspnea, sputum quantity, and quality. Most of the exacerbations occur due to upper respiratory infection or air pollution, but one third can happen without any known cause [14]. Treatment for acute exacerbation includes consistent use of short-acting bronchodilators, antibiotics, and short course of oral prednisone [15, 16]. A recent study found that 5 days of oral prednisone use is noninferior to 14 days [17]. Oxygen supplementation may be needed depending on severity of symptoms and hypoxia. Interestingly, there is no evidence of superiority of nebulizer to MDI/spacer beta agonist delivery for home or emergency room setting [18].
COPD
For patients with intermittent symptoms, inhaled short-acting beta-2 agonists such as albuterol or/and anticholinergic inhaled medications such as ipratropium (Atrovent) can be used to relieve symptoms for acute episodes. When combined together, they provide additive response [19]. For patients with moderate to severe COPD, they should be on daily long-acting bronchodilators which can include beta-2 agonists like salmeterol (Severent) and/or long-acting anticholinergic such as tiotropium (Spiriva). One study has shown that when comparing tiotropium to salmeterol , it resulted in preventing exacerbations for longer period [19]. Often, when patient’s symptoms are not well controlled with one class, these agents can be used together. Also, inhaled corticosteroids are approved in several combinations with long-acting beta-2 agonists. However, these can be considered when patients experience several COPD exacerbations. These are not approved to be used as monotherapy. Pneumonia is an important complication of treatment with inhaled corticosteroid-LABA products [19]. TORCH study has shown that it reduces exacerbation by 25 %; however, it does not slow progression of disease nor does it help to decrease mortality [20]. For patients with very severe COPD, consider starting triple therapy with a long-acting anticholinergic and a combined long-acting beta-2 agonist and corticosteroid. This may be warranted if symptoms persist despite dual medication therapy as it seems to reduce exacerbations and overall mortality [19].
Roflumilast (Daliresp) is an oral phosphodiesterase inhibitor which is indicated for patients with severe COPD associated with chronic bronchitis and history of several exacerbations [19]. Common side effects include nausea and diarrhea. Importantly, long-term oxygen therapy should be considered for patients with persistent hypoxemia of <88 % or PaO2 of 55 mmHg. See Table 3 for list of commonly used inhalers and their dosages.
Prevention of Exacerbations of Asthma and COPD
Climate
The interplay of climate and outdoor and indoor pollution on patients with asthma and COPD is very important. Extreme weather such as dry air of winter or humid air of the summer can impact the severity of both lung diseases. Often, staying indoors during times of extreme weather with appropriate filtered air conditioning and heating system to maintain a constant climate indoors is vital.
Outdoor Air Pollution
Allergens that are more prominent during the four different seasons can easily cause exacerbations of lung disease. Attempts to avoid both manufactured and natural substances from tree, grass, plants, and molds can assist in control of pulmonary disease.
Indoor Air Pollution
Elimination of both personal and secondhand smoke exposure is very important in limiting factors for exacerbation. In addition, removing potential irritants from carpets, plants, air fresheners, and cleaning chemicals can reduce number of irritants in the indoor environment. Also, changing air filters of the heating and cooling unit monthly is just as important.
Immunization
An influenza vaccine is recommended yearly, October through March, for all asthma and COPD patients. Both twenty three valent and 13 valent pneumococcal vaccines should be offered according to the current recommendations of the Advisory Council on Immunization Practice [11].
Self-Management Education
Important topics which should be discussed include appropriate and proper use of their inhalers and spacer , early recognition of exacerbation symptoms, and perhaps discussion about advance directive [21, 22].
Exercise
Aerobic exercise is vital to improve exercise capacity, quality of life, and decrease health care utilization of patients with asthma and COPD [7]. Physical training lasting for at least 20–30 min, two to three times a week for at least 6 weeks, improves physical fitness in patients with asthma [7]. Pulmonary rehabilitation should be considered for patients who are more symptomatic (CAT ≥ 10 or mMRc ≥ 2) [7] .
Special Populations
Pregnancy and Breastfeeding
The management of asthma does not change in the setting of pregnancy or breastfeeding. It is important to gain control early to prevent the risk of fetal hypoxia. Medications typically used to treat asthma do not confer any contraindication during pregnancy or lactation. Also, vaccination against pneumococcal and influenza during pregnancy is important.
Family and Community Issues
COPD is marked by gradual decline in health and increase in exacerbations over time. Respiratory failure, cardiovascular disease, and malignancy are major causes of death in patients with COPD. Hence, palliative care and hospice care are important components for patients with advanced COPD. Moreover, stepwise decline of quality of life may lead to isolation, depression, and anxiety. It is important to address emotional, family, and community support when caring for patients with COPD and severe asthma.
Prevention
Smoking cessation is a crucial step for all patients with COPD and asthma. It can reduce rate of decline in FEV1 and, hence, can help to slow the rate of progression of disease. It can be done through behavior counseling if patient is ready to quit. Other pharmacological interventions can be used including nicotine replacement therapy (nicotine patches, gum, and inhalers), bupropion (Wellbutrin), and varnicline (Chantix). Studies have shown that the combination of medical therapy and counseling yields best results for smoking cessation [23].
References
Chung K, Pavord I. Prevalence, pathogenesis, and causes of chronic cough. Lancet. 2008;371:1364–74.
Blasio F, Virchow J, Polverino M, Zanasi A, Behrakis P, Kilinc G, Balsamo R, Danieli G, Lanata L. Cough management: a practical approach. Cough. 2011;7:7. doi:10.1186/1745-9974-7-7.
Pratter M. Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1):63S–71.
Expert Panel Report 3 (EPR3). Guidelines for the diagnosis and management of asthma. National Asthma Education and Prevention Program. 2007. http://www.nhlbi.nih.gov/guidelines/asthma/.
CDC. National Health Interview Survey (NHIS) data: 2011 lifetime and current asthma: US Department of Health and Human Services, CDC. 2012. http://www.cdc.gov/asthma/nhis/2011/data.htm.
Barnett S, Nurmagambetov T. Costs of asthma in the United States: 2002–2007. J Allergy Clin Immunol. 2011;127:145–52.
National Asthma Education and Prevention Program. Expert panel report 3: guidelines for the diagnosis and management of asthma. National Heart, Lung and Blood Institute, National Institutes of Health: U.S. Department of Health and Human Services; 2007. Report No.: NIH Publication No. 07-4051.
Institute of Medicine (U.S.). Committee on the Assessment of Asthma and Indoor Air. Clearing the air: asthma and indoor air exposures. Washington, DC: The National Academies Press; 2000. 1.
COPD homepage. The Centers for Disease control and Prevention [Internet]. 2014 [updated: 2013 Nov 13; cited 2015 Jan 1]. http://www.cdc.gov/copd/index.htm.
COPD international statistics [Internet] [updated: 2012 July; cited 2015 Jan]. http://www.copd-international.com/Library/statistics.htm.
Global Initiative for Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. 2011. http://www.goldcopd.com. Accessed 1 Jan 2015.
Tsiligianni G, Van der Molen T, Moraitaki D. Assessing health status in COPD. A head-to-head comparison between the COPD assessment test (CAT) and the clinical COPD questionnaire (CCQ). BMC Pulm Med. 2012;12:20.
Rakel R, Rakel, D. Textbook of family medicine. 8th ed. Philadephia: Elsevier saunders, 1600 john E kenneyd blvd ste 1800, 19103–2899.
Aaron S. Management and prevention of exacerbations of COPD. BMJ. 2014;349:5237.
Vogelmeier C. Tiotropium versus salmeterol for the prevention of exacerbations of COPD. NEJM. 2011;364:1093.
Wedzicha J. Choice of bronchodilator therapy for patients with COPD. NEJM. 2011;364:1167.
Leuppi J. Short-term vs conventional glucocorticoid therapy in acute exacerbations of chronic obstructive pulmonary disease. JAMA. 2013;309:2223.
Dhuper S, Chandra, A, Ahmed A, Bista S, Moghekar A, Verma R, Chong C, Shim C, Cohen H, Choksi S. Efficacy and cost comparison of bronchodilator administration between metered dose inhalers with disposable spacers and nebulizers for acute asthma treatment. J emergency med. 2011
Drugs for Asthma and COPD (2013) Treatment guidelines from Medical letter. 2013;11(132):83–6
Criner G, Bourbeau J, Diekemper R. Prevention of acute exacerbation of chronic obstructive pulmonary disease: American College of Chest Physicians and Canadian Thoracic Society guideline.
Casaburi R, Wallack R. Pulmonary rehabilitation for management of chronic obstructive pulmonary disease. N Engl J Med. 2009;360:1329.
Cameron-Tucker et al. Chronic disease self management and exercise in COPD as pulmonary rehabilitation: a randomized controlled trial. Int J COPD. 2014;513–523.
Strassmann R. Smoking cessation interventions in COPD: a networkmetaanalysis of randomized trials. EurRespir J. 2009;34:634–40.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this entry
Cite this entry
Aggarwal, A., Osineme, C. (2017). Obstructive Airway Disease. In: Paulman, P., Taylor, R., Paulman, A., Nasir, L. (eds) Family Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-04414-9_90
Download citation
DOI: https://doi.org/10.1007/978-3-319-04414-9_90
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-04413-2
Online ISBN: 978-3-319-04414-9
eBook Packages: MedicineReference Module Medicine