Abstract
Total shoulder arthroplasty (TSA) remains a popular and reliable treatment alternative for severe arthritis of the shoulder. Proper glenoid component placement is critical to the long-term success of TSA. Improvements in preoperative surgical planning, intraoperative instrumentation, surgical technique, and implant designs have all helped to improve the ability to properly and securely implant a glenoid component in the optimal position. Modern imaging has helped to gain a better appreciation of variations in patient anatomy including glenoid shape, height, width, inclination, version, subluxation, subchondral bone density, and anticipation of how to reconstruct more normal joint relationships. Collectively, the ability to anticipate variations in glenoid anatomy, define a surgical plan, and accurately implement this plan when performing TSA will likely improve long-term success.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Since the first introduction in 1974, total shoulder arthroplasty (TSA) has become a reliable and reproducible treatment for end-stage arthritis that has failed to respond to nonoperative measures [18, 19, 25, 43, 57]. The utilization of TSA continues to expand at exponential rates with a 319 % increase in TSA procedures between 1993 and 2007 [17]. Analysis of outcomes following shoulder arthroplasty suggests that the addition of a glenoid component improves pain relief and outcomes [24, 47], suggesting significant advantages of TSA over hemiarthroplasty. This observation as resulted in a moderate strength recommendation to perform a total shoulder arthroplasty over a hemiarthroplasty for patients with glenohumeral joint osteoarthritis (AAOS). Nonetheless, glenoid component loosening has been shown to be the most common middle-term and long-term complication of TSA and is one of the most common causes of revision surgery [6, 10, 27, 50, 51, 74, 75]. Glenoid implant loosening has been associated with worse functional outcomes, worse pain, and inferior strength [59, 76]. Improvements in preoperative surgical planning, intraoperative instrumentation, surgical technique, and implant designs have all helped to improve the ability to properly and securely implant a glenoid component which will likely contribute to improved long-term results of total shoulder arthroplasty.
Glenoid Anatomy
A basic understanding of the variations in glenoid anatomy is critical for optimal utilization of glenoid components. Glenoid height, width, inclination, version, and vault size all play influential roles in surgical planning. Recent literature has shed greater light into the complexities of glenohumeral anatomy in the setting of arthritis.
Glenoid Height
Glenoid height can be measured from the distance from the most superior and inferior points on the glenoid (Fig. 7.1). Checroun et al. [9] reported a mean height of 37.9 mm using an analysis of 412 cadavers, Iannottii et al. [30] reported a mean height of 39 mm using an analysis of 140 shoulders, and Churchill observed an average height of 37.5 mm for men and 32.6 mm for women [11]. Analysis of the glenoid height helps to define glenoid component size during glenoid component preparation and implantation and is typically performed on coronal reconstruction of CT images.
Glenoid Width
Glenoid width can be measured from the most anterior and posterior points on the glenoid and is often influenced by osteophyte and wear patterns (Fig. 7.2). Variations in glenoid shape (Fig. 7.3) can influence the glenoid width, as pear-shaped and oval-shaped glenoids may have different variations in width. As an illustrative point, Ianottii [30] reported an average upper width of 23 mm and an average lower width of 29 mm. Others have reported averages of glenoid width without taking into consideration differences in shape. Kwon et al. [35] reported an average width of 26.8 mm, and Churchill et al. [11] reported an average width of 27.8 mm. Appreciation of the glenoid width also helps to define glenoid component size, as efforts should be made to prevent excessive overhang of the implant. Accurate measurement is often made difficult, as osteophytes and bone erosion often obscure the identification of the native glenoid limits.
Glenoid shape – variations in glenoid shape can be appreciated best by 3D CT reconstruction images. Osteophytes and wear patterns influence this shape. (a) Oval-shaped glenoid; (b) Pear-shaped glenoid with anterior-inferior osteophyte; (c–e). Pear-shaped glenoid with inferior osteophytes; (f) Posterior-superior glenoid wear alters the glenoid shape
Glenoid Inclination
Glenoid inclination is defined as the slope of the glenoid articular surface measured in the superior to inferior axis and can be measured both on AP radiographs and coronal reconstruction CT images (Fig. 7.4). Maur et al. found the angle between the glenoid fossa line (line from the superior to inferior tip of the glenoid), and the floor of the supraspinatus fossa was most reliable at measuring glenoid inclination [42]. Average inclination can range from 2.2° of inferior tilt to 4.2° of superior tilt with reported ranges from 12° of inferior tilt to 15° degrees of superior tilt [46]. Churchill et al. [11] found male patients to have an average of 4° of inferior tilt, whereas females had an average superior tilt of 4.5°. The observed range of inclination varied between 7° of inferior tilt to 15.8° of superior tilt. Appreciation of the glenoid inclination becomes important during glenoid implantation, as placement of the component with superior tilt has been associated with a greater incidence of rotator cuff disease postoperatively [78].
Glenoid inclination – glenoid inclination can be measured by the angle between the glenoid fossa line (vertical line) and a horizontal scapular reference. This can be measured on radiographs as well as CT reconstructed images. Maur et al. found the angle between the glenoid fossa line (line from the superior to inferior tip of the glenoid) and the floor of the supraspinatus fossa was most reliable at measuring glenoid inclination [42]
Glenoid Version
Glenoid version has gained a great deal of attention, as much of the pathologic changes in glenohumeral arthritis result in alterations in glenoid version. Glenoid version is most commonly calculated on axial CT images using the Friedman method [22], which is measured based on the glenoid axis (anterior to posterior rim of the glenoid) and the scapular axis (line connecting the medial boarder of the scapula and the center of the glenoid line) (Fig. 7.5). Alternatively, the vault method [41] is referenced based on the glenoid axis and the glenoid vault axis (line connecting the tip of the scapular vault to the glenoid axis) (Fig. 7.6). Matsumura et al. reported that both methods demonstrated high intra- and inter-rater reliability with normal glenoids having 1.1° ± 3.2° retroversion with the conventional method and 8.9° ± 2.7° retroversion with the vault method. In contrast, arthritic glenoids had average glenoid retroversion of 10.8° ± 9.3° measured with the conventional method and 18.2° ± 9.1° with the vault method. Variation in glenoid version in normal shoulders has been reported to average from 2° of anteversion to 9° of retroversion [11, 22, 39, 45], with greater degrees of average retroversion seen in arthritic shoulders [22] with wear patterns showing preferential wear in the posterior-inferior glenoid [12]. There has been criticism of the accuracy of 2D CT scans in calculating glenoid version due to alterations in pathologic anatomy, orientation of the scapula for axial cuts, and wear patterns of the glenoid. Recently, Scalise et al. utilized 3D CT reconstructions to assess glenoid version and observed an average retroversion of 15.6° in the arthritic shoulder and 7° in the normal shoulder [51]. Using 3D CT reconstructions, the plane of the scapula is defined by three points: inferior tip of the scapula, scapula trigonum, and the center of the glenoid. Once the plane of the scapula is defined, 2D images are made in the axial, coronal, and sagittal planes to help calculate glenoid version and inclination [51]. While 3D CT reconstructions may provide a more accurate assessment of glenoid version, utilization of 3D reconstructions to define the scapular plane and then create a new 2D axial image along this plane resulted in no significant differences in glenoid version measurements between 3D and 2D images [8]. Appreciation of glenoid version is important as reports have suggested inferior outcomes when glenoid components are implanted in excessive retroversion [29, 53, 77].
Glenoid version – glenoid version can be measured using the Friedman method which defines glenoid version based on the relationship between the glenoid axis (dotted line; anterior to posterior rim of the glenoid) and the scapular axis (solid line; line connecting the medial boarder of the scapula and the center of the glenoid line)
Glenoid Vault
The glenoid vault has gained recent attention based on the work of Iannotti and Williams [15, 23, 48–51, 68]. The concept, first described by Ianotti and Williams [68], relates to opportunities for glenoid component fixation when glenoid wear and bone loss becomes significant. While this scenario is more common in the revision setting, pathologic patterns of arthritic wear and joint destruction may allow for preferential glenoid component fixation within the vault and rim rather than the typical subchondral bone surface. Codsi et al. utilized a custom software program to measure variations in glenoid vault anatomy in 61 cadaveric specimens. A group of 5 sized glenoid vault implants were created, representing the consistent triangular anatomy observed in the glenoid vault. Appreciation of the glenoid vault helps to anticipate the ability of the glenoid component to fit within the glenoid vault rather than violating the medial cortex of the glenoid. Moreover, by understanding the glenoid vault anatomy, it is possible to recognize the alterations in glenoid anatomy and facilitate reconstruction efforts aimed at restoring normal version without medialization of the joint.
Subchondral Bone Density
Nearly all glenoid components rely on the subchondral support of the glenoid. Violation of this subchondral surface during glenoid preparation has been shown to result in subsidence of the glenoid implant [66, 67]. It has thus been advocated that the subchondral plate be preserved during glenoid reaming. Simon et al. recently reported an analysis of 3D CT osteoabsorptiometry on 21 patients with concentric glenoid wear and 21 patients with eccentric glenoid wear [52]. They observed differences in subchondral bone patterns for concentric and eccentric wear patterns, with greater density in the posterior zone for eccentric glenoids, whereas concentrically worn glenoids had a homogeneous pattern of bone density. In evaluating CT scans, attention should be directed to the thickness of the subchondral bone. This can assist in preoperative planning when eccentric reaming is necessary.
Subluxation Index
Subluxation of the glenohumeral joint in the setting of arthritis is rather common. Walsh et al. [62] described a method for calculating the subluxation index by measuring the percent subluxation of the humeral head on axial CT images. Using the midpoint of the glenoid axis (line between the anterior and posterior limits of the glenoid), the distance between this center point and the posterior limit of the humeral head is divided by the distance between the anterior and posterior limits of the humeral head (Fig. 7.7). A centered head has a subluxation index of 35–65 %. Posterior subluxation is defined as a subluxation index of greater than 65 % and anterior subluxation as less than 35 %. Appreciation of the amount of subluxation seen on both axillary radiographs and CT scans helps to understand wear patterns and formulate strategies for glenoid preparation.
Subluxation – subluxation of the humeral head can be appreciated best on axial CT images. Using the midpoint of the glenoid axis (line between the anterior and posterior limits of the glenoid), the distance between this center point and the posterior limit of the humeral head (line b) is divided by the distance between the anterior and posterior limits of the humeral head (line a). The glenohumeral relationship can then be classified as centered (35–65 %), posteriorly subluxated (>65 %), or anteriorly subluxated (<35 %)
Glenoid Morphology
Recognition of patterns of wear and the glenoid morphology is one of the most important aspects of surgical planning for glenoid component placement.
The most widely referenced classification of glenoid morphology was described by Walch et al. [61, 62] (Fig. 7.8). Five patterns of glenoid wear were described in a series of patients with osteoarthritis. Type A glenoids have a central pattern of wear with minor erosion (A1) and major erosion (A2). Type B glenoids have posterior subluxation without erosion (B1) and with posterior rim erosion (B2). B2 glenoids are commonly described as having a biconcave glenoid deformity. Type C glenoids have glenoid retroversion of more than 25° and are typically considered dysplastic glenoids. While this classification is typically observed on axial radiographs, axial CT images and 3D CT images help clarify the glenoid morphology.
Glenoid wear morphology in osteoarthritis – the most commonly referenced classification of glenoid morphology of glenohumeral osteoarthritis as described by Walch et al. [62]. The figure represents the Walch classification, (a1) centered humeral head with mild glenoid erosion. (a2) centered humeral head with major erosion, (b1) posterior subluxation with no erosion, (b2) posterior erosion with biconcave glenoid. (c) severe retroversion
Recently, Walch introduced the concept of the B3 glenoid, based on the recognition that as glenoid erosion advances in the setting of posterior subluxation, a biconcave wear pattern becomes difficult to recognize. This glenoid morphology typically has posterior subluxation of more than 70 %, retroversion of more than 10°, and no clear margin between the neoglenoid and paleoglenoid (CSSES Meeting, Tampa 2015).
Glenoid morphology patterns are different in the setting of rheumatoid arthritis. Levigne and Francheschi described a glenoid morphology classification based on a series of 50 shoulders treated with shoulder arthroplasty [36] (Fig. 7.9). Stage 1 represented an intact or minimally deformed subchondral bone plate. Stage 2 showed erosion reaching the base of the coracoid. Stage 3 patients demonstrated erosion beyond the coracoid base.
Surgical Plan
Common logic suggests that placement of the glenoid component in an ideal location should provide the best chance for long-term survivability of the implant. Ideally, the glenoid face should be prepared to perfectly match the backside of the glenoid component without overhang of the glenoid component or reaming past the subchondral bone. The fixation pegs or keels should be contained within the glenoid vault. The component should be placed in neutral to slight inferior inclination, specifically avoiding superior tilt. While there is no defined ideal version correction that has been shown to improve long-term fixation or wear, Iannotti et al. suggested that glenoid version should be corrected to within 5° of a plane perpendicular to the plane of the scapula [30]. Unfortunately, with increasing glenoid deformities, the ability to accurately place the glenoid component can be challenging [30], both in terms of planning and execution of the surgical plan.
Advances in imaging capabilities, integration of surgical planning software, improvements in implant innovation, and a greater understanding of glenoid anatomy and wear patterns have all contributed to the advancements in surgical planning of glenoid component implantation. The introduction of patient-specific instrumentation together with 3D modeling software developments has facilitated precise surgical planning with opportunities to carry out that plan with a high level of accuracy.
Radiographs continue to be the gold standard for the evaluation of glenohumeral arthritis. Properly oriented anteroposterior (AP) and axillary lateral views of the glenoid are critical [28, 69]. While properly performed axillary radiographs can be sufficient in evaluating glenoid wear patterns, the value of CT scan imaging with two- and three-dimensional reconstructions has become invaluable in surgical planning for glenoid component implantation.
2D reconstructed CT scan images allow the analysis of several key components of shoulder anatomy that are critical in preoperative planning of glenoid component implantation. Axial images are used to calculate the glenoid version, humeral head subluxation, eccentric wear patterns, glenoid width, subchondral bone density and location, location of osteophytes, depth of the glenoid vault, analysis of the quality of the subscapularis muscle and tendon, and identification of bone defects which may be present. Coronal reconstructions help to appreciate the glenoid height, inclination angle, superior humeral head subluxation, and quality of the supraspinatus and infraspinatus muscle and tendons. Sagittal reconstructions help to appreciate muscle atrophy of the rotator cuff musculature. Using two-dimensional images, glenoid planning can be performed [31]. The central axis point can be estimated which will serve for the axis of glenoid reaming. The amount of glenoid reaming necessary to restore appropriate version can be estimated as well.
The introduction of 3D reconstructions with humerus subtraction has helped to better understand the limitations of 2D CT imaging as well as gain a better appreciation of the location of wear patterns in pathologic glenoids. Not only can calculations of version, inclination, and subluxation be performed more accurately [60], but the actual location of glenoid wear patterns can be appreciated. In recent years, 3D printing technology has become more widely available. Printing scapular models of patient anatomy brings the understanding of glenoid anatomy to the next level and is now a part of most patient-specific instrumentation platforms currently available. The recent interest in patient-specific instrumentation has taken surgical planning to a high level of precision [31, 37, 38, 58, 64, 65]. The combination of virtual surgical planning, 3D printing of the scapula, and instrumentation developed specifically for reproducing the virtual surgical plan has improved the accuracy of carrying out the surgical plan for glenoid component placement to within a few degrees of error. With accurate planning, it is now possible to place the glenoid component accurately in the properly planned location, correct deformities of version and inclination, define the appropriate component rotation on the face of the glenoid, and properly size the glenoid components to avoid medial vault penetration.
Implant Selection
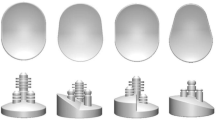
There are numerous variations in glenoid implant designs. Differences are seen in component shape, radial mismatch, backside curvature, keel and peg size and orientation, and method of fixation. It is important to understand the rationale behind each of these implant features.
Glenoid Shape
Most of the original glenoid component designs were oval shaped despite the pear shape of the native glenoid. The surgeon was often left with a decision of how to best size the prosthetic glenoid component, as proper sizing of the inferior glenoid often resulted in implant overhang superiorly. With the advent of the Aequalis (Tornier, Edina, MN) and the Solar (Stryker, Kalamazoo, MI), attention was focused on more closely matching the glenoid anatomy using a pear-shaped design [9]. Several glenoid implants have since been introduced with a more anatomic glenoid shape. The theoretical risk of the anatomically matched glenoid component is increased instability [1, 16]; however, to date there are no reports of greater instability seen with anatomically shaped glenoid components. It is generally accepted that the optimal glenoid component size is one that most closely matches the prepared glenoid surface without allowing for the component to hang off the glenoid bone.
Radius of Curvature Mismatch
Nearly all glenoid components have a mismatch between the radius of curvature of the humeral head and the glenoid. This is based on the rationale that normal glenohumeral mechanics result in translations between the humeral head and glenoid. In a cadaveric analysis, Karduna et al. observed that active translations seen in normal joints were best reproduced with glenoid components that were less conforming and determined that a radial mismatch of 4 mm best represents this relationship [32]. In a multicenter analysis of flat-back cemented polyethylene glenoids, Walch et al. observed that glenohumeral mismatch significantly influenced the incidence of radiolucent lines and described an ideal mismatch between 6 and 10 mm [63]. However, no study has defined the ideal radial mismatch for a glenoid component based on effects on outcomes, and variations in the radial mismatch remain common among different implant designs.
Glenoid Fixation
Critical to the long-term success of the glenoid component is implant fixation. There are several methods of component fixation that have been utilized in glenoid implant designs. Pegged and keeled designs are certainly the most common and have historically been cemented into the glenoid. Metal-backed glenoid components with polyethylene inserts allow for enhanced fixation using screws, pegs, and ingrowth metals. Recently, hybrid combinations of cemented and uncemented pegs have been utilized as methods of enhancing component fixation into the bone.
Fully cemented pegged and keel designs have been utilized since the first total shoulder arthroplasties performed by Charles Neer in the early 1970s. While keel designs remain the most popular worldwide, Edwards et al. reported significantly higher rates of radiolucent lines surrounding keeled implants than pegged implants both on initial postoperative radiographs and 2-year follow-up [20]. All cemented peg and keel designs vary with differences observed in the shape of the keel and the orientation and number of pegs.
The effect of cement technique on glenoid component fixation has been studied. Terrier et al. used an FEA to assess the stress interaction between the cement and glenoid bone and concluded that a 1.0 mm cement mantle thickness is ideal [55]. Nyffler performed axial pullout testing of variable glenoid component designs and observed that threaded pegs demonstrated higher pullout force than notched pegs, which were both higher than smooth pegs [45]. Additionally, they noted that increasing the cement mantle thickness from 0.1 to 0.6 mm increased the pullout force [45]. Roughened backside surface finish of glenoid components has also been shown to improve component stability in all-cemented glenoids [2, 45]. Finally, cement pressurization during glenoid component implantation has been associated with a low incidence of early radiolucent lines [4, 34].
Recently, enhanced fixation glenoids which support bone growth into or around pegs have gained interest based on improved biologic fixation. Early results are quite promising with high rates of bone growth observed between the flutes on the pegs [72, 73] in studies with up to 5-year follow-up [13]. With greater initial fixation of the component [14] and opportunity for biologic fixation of the pegs, enhanced fixation polyethylene glenoids may ultimately help to lower rates of radiolucent lines suggestive of glenoid loosening.
Metal-backed uncemented glenoid implants have lost popularity based upon a historical experience of high complications. The original designs utilized a metal casing secured with screw fixation and an exchangeable polyethylene insert. High rates of screw breakage, excessive polyethylene wear, dissociation, and high revision rates have been reported [40, 54]. Recently, new uncemented metal-backed designs utilizing modern fixation technologies have been introduced. These include implants with ingrowth metals and improved screw fixation methods that may help avoid the historical failures. However, to date there are no reports to suggest that the history of loosening and catastrophic failure has been avoided using these newer designs.
Glenoid Materials
As glenoid component fixation improves, initial failure modes may shift from component loosening due to loss of fixation to polyethylene wear and osteolysis. Cross-linked, ultrahigh molecular weight polyethylene is typically used for most glenoid components [71]. While polyethylene wear has been clearly linked with osteolysis in total hip arthroplasty, there are few reports of similar reactions following total shoulder arthroplasty [33, 79]. Osteolysis after TSA has been reported to be as high as 23 % [79] and has been shown to be more common with metal-backed glenoids [5, 33]. Wirth et al. evaluated the polyethylene debris particle size in retrievals of three failed total shoulder arthroplasties that were revised for aseptic loosening with osteolysis and compared them to failed total hip components revised for similar reasons. The wear debris was found to be larger and more fibrillary than the particles from failed total hip arthroplasty [70], suggesting a different mechanism of wear in shoulders than in hips. Differentiating between mechanical loosening from loss of fixation and osteolysis may ultimately be difficult as osteolytic regions can contribute to mechanical loosening.
Recently, the addition of vitamin E into highly cross-linked polyethylene has been introduced into total shoulder arthroplasty. This has been based on the success seen in total hip arthroplasty, which has demonstrated oxidative stability, low wear rates, and improved strength with the addition of vitamin E [7]. With enhanced fixation of glenoid components, efforts at utilizing this and other polyethylene materials with improved wear and strength properties will continue. Given the recent introduction of this technology, there is no clinical data supporting the use of these alternative polyethylene materials in total shoulder arthroplasty.
Surgical Execution
Proper glenoid exposure remains the critical step for placement of a glenoid component. This necessitates appropriate soft tissue releases, placement of retractors, and sufficient bone resections to allow clear visualization of the glenoid. Once the glenoid is exposed, all total shoulder arthroplasty systems now have instrumentation designed to prepare the glenoid surface to match the backside of the glenoid and precisely drill peg holes or a keel vault to match the selected glenoid component.
Glenoid Preparation
All glenoid components are defined based on a central axis. This axis, defined during surgical planning, defines all corrections in version, inclination, and translation. Once this axis is defined, glenoid reaming can be performed using glenoid reamers. These reamers are either cannulated based on a wire that has been placed down the central axis or non-cannulated utilizing a tip that fits within a hole in the central axis point on the glenoid face. The goal of glenoid preparation is to prepare a matching surface to the backside of the glenoid component. Early flat-back glenoid designs often required significant glenoid reaming, whereas concave glenoid designs typically require less glenoid reaming during preparation. A critical principle of glenoid preparation is to avoid reaming past the subchondral bone plate into more cancellous bone as this has been associated with early component subsidence [66, 67].
Once the glenoid is reamed to match the back surface of the glenoid component, the peripheral pegs or keels are created. For glenoids designed to utilize cement, the peg or keel preparation anticipates creating a cement mantle which is typically 1.0 mm [55]. Glenoid designs, which utilize pegs without the need for cement, create peg holes designed for a press fit.
The rotation of the glenoid component is defined during this step. Most TSA systems provide precision jigs which help to create the peripheral pegs or keel vault; however, the surgeon must define the rotation of the component. By referencing the biceps insertion on the supraglenoid tubercle, the proper rotation of the glenoid component can be selected. Patient-matched instrumentation systems have the capacity to integrate this step into a guide that is used during surgery, defining both the central axis for reaming and a peripheral peg hole to maintain the accuracy of glenoid component rotation in addition to version, inclination, and translation position [56].
Glenoid Implantation
Most all-polyethylene glenoid components utilize cement for component fixation. Modern cement techniques have evolved with most emphasizing drying the glenoid [21], cement mantle thickness of 1.0 mm [55], and cement pressurization either by injection into the peg hole or keel vault using a syringe [4, 34] or weep-hole vacuum assistance [26]. Use of additional cement on the back of the glenoid component is more controversial based on concerns regarding fracture and fragmentation of thin areas of cement and associated risk of third-body wear from dislodged cement particles. Once the glenoid component is placed, all extruded cement must be removed from the periphery of the glenoid component.
Conclusion
Modernization of total shoulder arthroplasty has greatly improved the understanding and appreciation of variations in glenoid anatomy in severely arthritic shoulders. Appreciation of both normal and abnormal glenoid anatomy has helped the surgeon understand patient pathology and has enhanced glenoid component design and surgical technique. Collectively, the surgeon now has a greater understanding of how to appreciate anatomical variations, properly plan glenoid placement, and accurately execute standard glenoid component placement during total shoulder arthroplasty.
References
Anglin C, Wyss UP, Nyffeler RW, Gerber C. Loosening performance of cemented glenoid prosthesis design pairs. Clin Biomech. 2001;16:144–50.
Anglin C, Wyss UP, Pichora DR. Mechanical testing of shoulder prostheses and recommendations for glenoid design. J Should Elb Surg. 2000;9:323–31.
Barwood S, Setter KJ, Blaine TA, Bigliani LU. The incidence of early radiolucencies about a pegged glenoid component using cement pressurization. J Should Elb Surg. 2008;17:703–8.
Boileau P, Moineau G, Morin-Salvo N, Avidor C, Godenèche A, Lévigne C, Baba M, Walch G. Metal-backed glenoid implant with polyethylene insert is not a viable long-term therapeutic option. J Shoulder Elbow Surg. 2015. pii: S1058-2746(15)00085–3. doi:10.1016/j.jse.2015.02.012.
Boileau P, Sinnerton RJ, Chuinard C, Walch G. Arthroplasty of the shoulder. J Bone Joint Surg (Br). 2006;88:562–75. doi:10.1302/0301-620X.88B5.16466.
Bracco P, Oral E. Vitamin E-stabilized UHMWPE for total joint implants: a review. Clin Orthop Relat Res. 2011;469(8):2286–93. doi:10.1007/s11999-010-1717-6.
Budge MD, Lewis GS, Schaefer E, Coquia S, Flemming DJ, Armstrong AD. Comparison of standard two-dimensional and three-dimensional corrected glenoid version measurements. J Should Elb Surg. 2011;20(4):577–83. doi:10.1016/j.jse.2010.11.003.
Checroun AJ, Hawkins C, Kummer FJ, Zuckerman JD. Fit of current glenoid designs: an anatomic cadaver study. J Should Elb Surg. 2002;11:614–7. doi:10.1067/mse.2002.126099.
Chin PYk SJ, Boyd AD, Thomas WH, Sledge CB, Thornhill TS. Failed shoulder arthroplasty. Orthop Trans. 1990;14:255–61.
Churchill RS, Brems JJ, Kotschi H. Glenoid size, inclination, and version: an anatomic study. J Should Elb Surg. 2001;10:327–32.
Churchill RS, Spencer Jr EE, Fehringer EV. Quantification of B2 glenoid morphology in total shoulder arthroplasty. J Should Elb Surg. 2015;24(8):1212–7. doi:10.1016/j.jse.2015.01.007. Epub 2015 Mar 4.
Churchill RS, Zellmer C, Zimmers HJ, Ruggero R. Clinical and radiographic analysis of a partially cemented glenoid implant: 5-year minimum follow-up. J Should Elb Surg. 2010;19:1091–7. doi:10.1016/j.jse.2009.12.022.
Churchill RS. Trends in glenoid component design in unconstrained shoulder arthroplasty. J Should Elb Surg. 2011;20:S41–6.
Codsi MJ, Bennetts C, Gordiev K, Boeck DM, Kwon Y, Brems J, Powell K, Iannotti JP. Normal glenoid vault anatomy and validation of a novel glenoid implant shape. J Should Elb Surg. 2008;17(3):471–8. doi:10.1016/j.jse.2007.08.010.
Collins D, Tencer A, Sidles J, Matsen III FA. Edge displacement and deformation of glenoid components in response to eccentric loading. The effect of preparation of the glenoid bone. J Bone Joint Surg Am. 1992;74:501–7.
Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Should Elb Surg. 2010;19(8):1115–20.
Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Should Elb Surg. 2005;14(5):471–9.
Edwards TB, Kadakia NR, Boulahia A, Kempf JF, Boileau P, Némoz C, Walch G. A comparison of hemiarthroplasty and total shoulder arthroplasty in the treatment of primary glenohumeral osteoarthritis: results of a multicenter study. J Should Elb Surg. 2003;12(3):207–13.
Edwards TB, Labriola JE, Stanley RJ, O’Connor DP, Elkousy HA, Gartsman GM. Radiographic comparison of pegged and keeled glenoid components using modern cementing techniques: a prospective randomized study. J Should Elb Surg. 2010;19(2):251–7.
Edwards TB, Sabonghy EP, Elkousy H, Warnock KM, Hammerman SM, O’Connor DP, Gartsman GM. Glenoid component insertion in total shoulder arthroplasty: comparison of three techniques for drying the glenoid before cementation. J Should Elb Surg. 2007;16(3 Suppl):S107–10.
Friedman RJ, Hawthorne KB, Genez BM. The use of computerized tomography in the measurement of glenoid version. J Bone Joint Surg Am. 1992;74:1032–7.
Ganapathi A, McCarron JA, Chen X, Iannotti JP. Predicting normal glenoid version from the pathologic scapula: a comparison of 4 methods in 2- and 3-dimensional models. J Should Elb Surg. 2011;20(2):234–44. doi:10.1016/j.jse.2010.05.024.
Gartsman GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg Am. 2000;82(1):26–34.
Goldberg BA, Smith K, Jackins S, Campbell B, Matsen 3rd FA. The magnitude and durability of functional improvement after total shoulder arthroplasty for degenerative joint disease. J Should Elb Surg. 2001;10(5):464–9.
Gross RM1, High R, Apker K, Haggstrom J, Fehringer JA, Stephan J. Vacuum assist glenoid fixation: does this technique lead to a more durable glenoid component? J Should Elb Surg. 2011;20(7):1050–60. doi:10.1016/j.jse.2011.04.007.
Hawkins RJ, Greis PE, Bonutti PM. Treatment of symptomatic glenoid loosening following unconstrained shoulder arthroplasty. Orthopedics. 1999;22:229–34.
Hertel R, Ballmer FT. Observations on retrieved glenoid components. J Arthroplasty. 2003;18:361–6. doi:10.1054/arth.2003.50048.
Ho J, Sabesan VJ, Iannotti JP. Glenoid component retroversion is associated with osteolysis. J Bone Joint Surg Am. 2013;95(12):e82.
Iannotti JP, Gabriel JP, Schneck SL, Evans BG, Misra S. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am. 1992;74:491–500.
Iannotti JP, Greeson C, Downing D, Sabesan V, Bryan JA. Effect of glenoid deformity on glenoid component placement in primary shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21(1):48–55. doi:10.1016/j.jse.2011.02.011.
Iannotti JP, Weiner S, Rodriguez E, Subhas N, Patterson TE, Jun BJ, Ricchetti ET. Three-dimensional imaging and templating improve glenoid implant positioning. J Bone Joint Surg Am. 2015;97(8):651–8. doi:10.2106/JBJS.N.00493.
Karduna AR, Williams GR, Williams JL, Iannotti JP. Glenohumeral joint translations before and after total shoulder arthroplasty. A study in cadavera. J Bone Joint Surg Am. 1997;79(8):1166–74.
Kepler CK, Nho SJ, Bansal M, Ala OL, Craig EV, Wright TM, Warren RF. Radiographic and histopathologic analysis of osteolysis after total shoulder arthroplasty. J Should Elb Surg. 2010;19(4):588–95. doi:10.1016/j.jse.2009.09.012. Epub 2009 Dec 29.
Klepps S, Chiang AS, Miller S, Jiang CY, Hazrati Y, Flatow EL. Incidence of early radiolucent glenoid lines in patients having total shoulder replacements. Clin Orthop Relat Res. 2005:118–25.
Kwon YW, Powell KA, Yum JK, Brems JJ, Iannotti JP. Use of three dimensional computed tomography for the analysis of the glenoid anatomy. J Should Elb Surg. 2005;14:85–90.
Levigne, Francheschi. Rheumatoid arthritis of the shoulder: radiological presentation and results of arthroplasty. In: Walch et al., editors. Shoulder arthroplasty. Berlin: Springer; 1999. p. 221–30.
Levy JC, Everding NG, Frankle MA, Keppler LJ. Accuracy of patient-specific guided glenoid baseplate positioning for reverse shoulder arthroplasty. J Should Elb Surg. 2014;23(10):1563–7. doi:10.1016/j.jse.2014.01.051.
Lewis GS, Stevens NM, Armstrong AD. J Shoulder Elbow Surg. 2015. pii: S1058-2746(15)00342–0. doi:10.1016/j.jse.2015.06.022.
Mallon WJ, Brown HR, Vogler JB 3rd, Martinez S. Radiographic and geometric anatomy of the scapula. Clin Orthop Relat Res. 1992; 142–54.
Martin SD, Zurakowski D, Thornhill TS. Uncemented glenoid component in total shoulder arthroplasty. J Bone Joint Surg. 2005;87A:1284–92. doi:10.2106/JBJS.C.00947.
Matsumura N, Ogawa K, Ikegami H, Collin P, Walch G, Toyama Y. Computed tomography measurement of glenoid vault version as an alternative measuring method for glenoid version. J Orthop Surg Res. 2014;9(1):17. doi:10.1186/1749-799X-9-17.
Maurer A, Fucentese SF, Pfirrmann CW, Wirth SH, Djahangiri A, Jost B, Gerber C. Assessment of glenoid inclination on routine clinical radiographs and computed tomography examinations of the shoulder. J Should Elb Surg. 2012;21(8):1096–103. doi:10.1016/j.jse.2011.07.010.
Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. J Should Elb Surg. 2002;11(2):130–5.
Nyffeler RW, Anglin C, Sheikh R, Gerber C. Influence of peg design and cement mantle thickness on pull-out strength of glenoid component pegs. J Bone Joint Surg (Br). 2003;85:748–52.
Nyffeler RW, Jost B, Pfirrmann CW, Gerber C. Measurement of glenoid version: conventional radiographs versus computed tomography scans. J Should Elb Surg. 2003;12:493–6.
Pinkas D, Wiater B, Wiater JM. The glenoid component in anatomic shoulder arthroplasty. J Am Acad Orthop Surg. 2015;23(5):317–26.
Radnay CS, Setter KJ, Chambers L, Levine WN, Bigliani LU, Ahmad CS. Total shoulder replacement compared with humeral head replacement for the treatment of primary glenohumeral osteoarthritis: a systematic review. J Should Elb Surg. 2007;16:396–402.
Ricchetti ET, Hendel MD, Collins DN, Iannotti JP. Is premorbid glenoid anatomy altered in patients with glenohumeral osteoarthritis? Clin Orthop Relat Res. 2013;471(9):2932–9. doi:10.1007/s11999-013-3069-5.
Sabesan V, Callanan M, Sharma V, Iannotti JP. Correction of acquired glenoid bone loss in osteoarthritis with a standard versus an augmented glenoid component. J Should Elb Surg. 2014;23(7):964–73. doi:10.1016/j.jse.2013.09.019.
Scalise JJ, Codsi MJ, Bryan J, Brems JJ, Iannotti JP. The influence of three-dimensional computed tomography images of the shoulder in preoperative planning for total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90(11):2438–45. doi:10.2106/JBJS.G.01341.
Scalise JJ, Codsi MJ, Bryan J, Iannotti JP. The three-dimensional glenoid vault model can estimate normal glenoid version in osteoarthritis. J Should Elb Surg. 2008;17:487–91. doi:10.1016/j.jse.2007.09.006.
Simon P, Gupta AK, Pappau I, Hussey MM, Santoni BG, Inoue N, Frankle MA. The relationship between the subchondral bone density distribution and glenoid depth: an -in-vivo pilot study of male total shoulder arthroplasty subjects. J Should Elb Surg. 2015;24(3):416–24. doi:10.1016/j.jse.2014.06.054.
Stephens SP, Paisley KC, Jeng J, Dutta AK, Wirth MA. Shoulder arthroplasty in the presence of posterior glenoid bone loss. J Bone Joint Surg Am. 2015;97(3):251–9. doi:10.2106/JBJS.N.00566. Review.
Taunton MJ, McIntosh AL, Sperling JW, Cofield RH. Total shoulder arthroplasty with a metal-backed, bone-ingrowth glenoid component: medium to long-term results. J Bone Joint Surg Am. 2008;90(10):2180–8.
Terrier A, Buchler P, Farron A. Bone-cement interface of the glenoid component: stress analysis for varying cement thickness. Clin Biomech (Bristol, Avon). 2005;20:710–7.
Testing of a novel pin array guide for accurate three-dimensional glenoid component positioning.
The treatment of glenohumeral joint osteoarthritis: guideline and evidence report. AAOS (http://www.aaos.org/Research/guidelines/glosummary.pdf).
Throckmorton TW, Gulotta LV, Bonnarens FO, Wright SA, Hartzell JL, Rozzi WB, Hurst JM, Frostick SP, Sperling JW. Patient-specific targeting guides compared with traditional instrumentation for glenoid component placement in shoulder arthroplasty: a multi-surgeon study in 70 arthritic cadaver specimens. J Should Elb Surg. 2015;24(6):965–71. doi:10.1016/j.jse.2014.10.013.
Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Should Elb Surg. 1997;6(6):495–505.
van de Bunt F, Pearl ML, Lee EK, Peng L, Didomenico P. Glenoid version by CT scan: an analysis of clinical measurement error and introduction of a protocol to reduce variability. Skelet Radiol. 2015;44:1627–35.
Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999;14:756–60.
Walch G, Boulahia A, Boileau J, Kempf JF. Primary glenohumeral osteoarthritis: clinical and radiographic classification. Acta Orthop Belg. 1998;64(Suppl II):48.
Walch G, Edwards TB, Boulahia A, Boileau P, Mole D, Adeleine P. The influence of glenohumeral prosthetic mismatch on glenoid radiolucent lines: results of a multicenter study. J Bone Joint Surg Am. 2002;84:2186–91.
Walch G. Management of posterior bone loss in TSA. Presented at Current Solutions in Shoulder and Elbow Surgery. Tampa, Jan 2015.
Walch G, Vezeridis PS, Boileau P, Deransart P, Chaoui J. Three-dimensional planning and use of patient-specific guides improve glenoid component position: an in vitro study. J Should Elb Surg. 2015;24(2):302–9. doi:10.1016/j.jse.2014.05.029.
Walch G, Young A, Melis B, Gazielly D, Loew M, Boileau P. Results of the convex back cemented keeled glenoid component in primary osteoarthritis. Multicentric Study with a follow-up >5 years. Shoulder concepts 2010 the glenoid, Sauramps Medical, 2010. Montpellier/Paris; 2010. p. 117–30.
Walch G, Young AA, Boileau P, Loew M, Gazielly D, Mole D. Patterns of loosening of polyethylene keeled glenoid components after shoulder arthroplasty for primary osteoarthritis: results of a multicenter study with more than 5 years follow-up. J Bone Joint Surg Am. 2012;94(2):145–50.
Williams Jr GR, Iannotti JP. Options for glenoid bone loss: composites of prosthetics and biologics. J Should Elb Surg. 2007;16:S267–72. doi:10.1016/j.jse.2007.05.003.
Wirth CJ, Peters G, Milachowski KA, Weismeier KG, Kohn D. Longterm results of meniscal allograft transplantation. Am J Sports Med. 2002;30:174–81.
Wirth MA, Agrawal CM, Mabrey JD, Dean DD, Blanchard CR, Miller MA, et al. Isolation and characterization of polyethylene wear debris associated with osteolysis following total shoulder arthroplasty. J Bone Joint Surg Am. 1999;81:29–37.
Wirth MA, Klotz C, Deffenbaugh DL, McNultry D, Richards L, Tipper JL. Cross-linked glenoid prosthesis: a wear comparison to conventional glenoid prosthesis with wear particulate analysis. J Should Elb Surg. 2009;18(1):130–7. doi:10.1016/j.jse.2008.06.015.
Wirth MA, Korvick DL, Basamania CJ, Toto F, Aufdemorte TB, Rockwood Jr CA. Radiologic, mechanical, and histologic evaluation of 2 glenoid prosthesis designs in a canine model. J Should Elb Surg. 2001;10:140–8.
Wirth MA, Loredo R, Garcia G, Rockwood Jr CA, Southworth C, Iannotti JP. Total shoulder arthroplasty with an all-polyethylene pegged bone-ingrowth glenoid component: a clinical and radiographic outcome study. J Bone Joint Surg Am. 2012;94(3):260–7. doi:10.2106/JBJS.J.01400.
Wirth MA, Rockwood CA Jr. Complications of shoulder arthroplasty. Clin Orthop Relat Res. 1994;47–69.
Wirth MA, Rockwood Jr CA. Complications of total shoulder replacement arthroplasty. J Bone Joint Surg Am. 1996;78:603–16.
Yian EH, Werner CM, Nyffeler RW, Pfirrmann CW, Ramappa A, Sukthankar A, et al. Radiographic and computed tomography analysis of cemented pegged polyethylene glenoid components in total shoulder replacement. J Bone Joint Surg Am. 2005;87:1928–36.
Yongpravat C, Kim HM, Gardner TR, Bigliani LU, Levine WN, Ahmad CS. Glenoid implant orientation and cement failure in total shoulder arthroplasty: a finite element analysis. J Should Elb Surg. 2013;22(7):940–7. doi:10.1016/j.jse.2012.09.007.
Young AA, Walch G, Pape G, Gohlke F, Favard L. Secondary rotator cuff dysfunction following total shoulder arthroplasty for primary glenohumeral osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg Am. 2012;94(8):685–93. doi:10.2106/JBJS.J.00727.
Zilber S, Radier C, Postel JM, Van Driessche S, Allain J, Goutallier D. Total shoulder arthroplasty using the superior approach: influence on glenoid loosening and superior migration in the long-term follow-up after Neer II prosthesis installation. J Should Elb Surg. 2008;17:554–63.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Levy, J. (2016). Standard Glenoid Replacement. In: Armstrong, A., Murthi, A. (eds) Anatomic Shoulder Arthroplasty. Springer, Cham. https://doi.org/10.1007/978-3-319-29164-2_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-29164-2_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29162-8
Online ISBN: 978-3-319-29164-2
eBook Packages: MedicineMedicine (R0)