Abstract
Sleep and epilepsy are common bedfellows. Sleep influences seizures and epilepsy in terms of frequency and occurrence of interictal spikes and occurrence, timing, and threshold of seizure. On the other hand, epilepsy can worsen sleep architecture and severity of sleep disorders. Thus a vicious cycle is set. Additionally, antiepileptic drugs also influence sleep. So sleep complaints/disorder also should be considered when selecting appropriate antiepileptic drugs. Moreover, sudden unexpected death in epilepsy (SUDEP) occurs in sleep and is most likely associated with cardiorespiratory changes in sleep, occurring ictally or postictally. Furthermore, poor sleep is associated with worsened quality of life, neurocognitive and behavioral functioning, and memory deficits on top of preexisting worsening due to epilepsy itself. Improving sleep and treatment of sleep disorders improve seizure frequency and overall well-being in patients with epilepsy. Hence, sleep evaluation and management are important in patient with epilepsy. In this chapter, we have discussed these interactions.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Sleep architecture
- Obstructive sleep apnea
- SUDEP
- BECTS
- Sleep disorders
- ESES
- NFLE
- JME
- Serotonin
- Cyclic alternating pattern
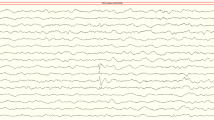
Epilepsy affects 1 % of the population in the USA and causes significant impact on society [1]. In layman’s terms, recurrent unprovoked seizures define epilepsy. A few years ago, the International League Against Epilepsy (ILAE) redefined epilepsy to be more inclusive and to advocate early treatment. Based on the new definition, (1) two or more unprovoked seizures, occurring more than 24 h apart, or (2) a single unprovoked seizure (reflex seizure) with at least 60 % chances of recurrence or (3) diagnosis of an epileptic syndrome is diagnosed as epilepsy [2]. The diagnosis is based on clinical history and specific diagnostic tests that identify patterns for seizure occurrence. One such testing modality is electroencephalogram (EEG), which as the name suggests measures the electrical potentials of the pyramidal neurons. The abnormal activity which is linked to epilepsy is spike-wave discharges or interictal epileptiform discharges (IEDs), the presence of which may be helpful in diagnosing an event as a seizure. Based on the cerebral location, frequency of occurrence, morphology, and amplitude of abnormalities on EEG, certain epilepsy syndromes are identified. One example is benign epilepsy with centrotemporal spikes [BECTS or benign Rolandic epilepsy (BRE)], which is discussed later in the chapter. Additionally, rhythmic, evolving EEG patterns that disrupt the normal electrical background activity constitute most seizures electrographically. In the last two decades, there has been significant advancement in treatment of epilepsy as several new drugs and a few new devices have become available. Despite these, epilepsy largely remains incurable and in about a third of the patients, uncontrollable. Moreover, significant comorbidities have also been reported, one of which is coexisting sleep disorders and sleep problems.
Sleep and epilepsy are interrelated. This is well known since the ancient times. Aristotle wrote that sleep is similar to epilepsy and in the same way that sleep is to epilepsy. In 1885, Gower described that 21 % of children had nocturnal seizures. He also reported that nocturnal seizures occurred at specific times in sleep. Ferre described that seizures affected sleep [3–5]. The effects of sleep and epileptiform discharges were first described by Gibbs and Gibbs in 1947 [3–5]. In this chapter, we discuss these interactions.
Effect of Sleep on EEG, Seizures, and Epilepsy
Sleep activates interictal epileptiform discharges (IEDs). Studies in adults with focal epilepsy show that the spike frequency increases with increasing depth of NREM sleep besides the field of discharge, which also increases [6, 7]. On the other end, spike frequency and the field are reduced in REM sleep [8]. Due to both of these phenomena, REM-related IEDs can help to identify the seizure focus [9, 10]. Studies in children have shown that some children may have spikes only during sleep [11]. In children, the IEDs in focal epilepsies are more common during N1 and N2 stages of sleep [12].
Seizures are also known to occur during specific sleep stages. It is well documented that seizures are rare in REM sleep. A recent study reevaluated and confirmed that REM sleep was protective for seizure occurrence by reviewing 42 studies. The study showed that seizures in N1, N2, and N3 were 87, 68, and 51 times more common than in REM sleep, respectively. Even compared to wakefulness, both generalized and focal seizures were less common in REM sleep. Moreover, EEG of certain epilepsy syndromes such as BECTS and electrical status epilepticus during sleep (ESES) had marked improvement in REM sleep [13]. Additionally, sleep also influences epilepsy based on the location of seizure origin. In a study, 78 % of frontal lobe seizures were sleep related, while only 20 % of temporal lobe seizures were sleep related [14]. The temporal lobe seizures were more likely to generalize in sleep [15]. Furthermore, sleep can provide a differential diagnosis for psychogenic non-epileptic seizures (PNES) from epileptic seizures as PNES do not occur in sleep, so occurrence of events during sleep helps to diagnose seizures [16].
Just like sleep and other bodily functions, seizures also follow circadian rhythms. Studies show that tonic and tonic-clonic seizures occurred more frequently in sleep, while clonic, absence, atonic seizures and myoclonic seizures occurred in wakefulness. Epileptic spasms had two peaks at 6–9 am and 3–6 pm in wakefulness [17]. Seizures of temporal lobe origin occurred mainly between 1100 and 1700, while frontal seizures were seen mostly between 2300 and 0500 [18]. In another study, occipital seizures peaked at 1600–1900, parietal and frontal peaked at 0400–0700, and temporal seizures peaked bimodally at 0700 and 1600–1900 [19]. The proof that this is not just time based but actually based on circadian rhythm was provided by a study correlating dim light melatonin onset (DLMO) with seizure occurrence. In the study, temporal seizures occurred most frequently during the times 6 h before DLMO and frontal seizures mainly in 6–12 h after the DLMO [20]. Since these studies were performed in a hospital epilepsy monitoring unit setting, which may not represent a true sleep-wake cycle for subjects, a study evaluated circadian pattern of seizure occurrence on ambulatory EEG where patients are in the home environment. In this cohort, frontal lobe seizures occurred more frequently between 12 am and 12 pm, and temporal lobe seizures occurred more frequently between 12 pm and 12 am. Moreover, frontal lobe seizures clustered between 5:15 and 7:30 am, while temporal lobe seizures clustered between 6:45 and 11:56 pm [21]. Furthermore, sunlight may also affect seizure occurrence as complex partial seizures were less likely to occur on bright sunny days, than dull days in a study [22].
This information on circadian pattern of seizure occurrence is very helpful for treatment strategies. There is possibility of light therapy and changing the circadian pattern for treatment of epilepsy. Additionally, a study suggested that differential dosing with two-third dose in the evening for predominantly nocturnal seizures led to seizure freedom in 64.7 % of patients, while 88.2 % experienced more than 50 % reductions in seizures [23]. There was mild increase in nocturnal peak levels as compared to daytime levels with the differential dosing. This approach may also be helpful in reducing side effects of antiepileptic drugs (AEDs).
Sleep deprivation is one of the most commonly reported seizure precipitating factors in children with intractable epilepsy [24]. Additionally, patients with JME are very sensitive to seizure occurrence due to sleep deprivation. However, there is still some controversy whether sleep deprivation increases IEDs. In general, activation is seen even if no sleep is recorded on the EEG, and hence, most EEG laboratories have established protocols for sleep-deprived EEGs. Sleep deprivation is also known to induce seizures in certain epilepsies and in patients with no history of seizures [12, 25, 26].
There are several mechanisms hypothesized to explain the activated IEDs and seizures in sleep. During NREM sleep neuronal networks are hypersynchronized. This helps to propagate the IEDs which are also believed to be generated by the same thalamocortical circuit similar to the sleep-specific architecture such as spindle and slow waves. During REM sleep, this synchronization is absent which reduces the spread of IEDs.
The second theory relates to a cyclic alternating pattern (CAP), described in sleep EEG which is a marker of unstable sleep. This pattern is present in NREM sleep and at the transition from NREM to REM sleep. The pattern is defined by two phases, first is phase A, of transient events, and second is phase B, the background rhythm in between. Additionally, CAP phase A is further divided into (1) phase of synchrony (A1 subtype), which comprises of delta bursts, K-complex sequences, vertex sharp transients, and polyphasic bursts with <20 % of EEG desynchrony; (2) phase of a mixture of slow and fast rhythms (A2 subtype), which includes polyphasic bursts with 20–50 % of EEG desynchrony; and (3) phase of rapid low-voltage rhythms (A3 subtype), which includes K-alpha, EEG arousals, and polyphasic bursts with >50 % of EEG desynchrony. Each CAP cycle begins with phase A and ends with phase B and lasts 2–60 s in duration. At least two such cycles form CAP sequence. CAP sequences are intermixed with non-CAP, which is the absence of CAP for more than 60 s, and represent stable sleep. CAP sequences, particularly, phases A2 and A3, have 87 % of the arousals seen in NREM sleep. CAP rate is calculated as the percentage ratio of total CAP time to non-REM sleep time, which is a measure of arousal instability and has been used as a measure for restorative sleep in sleep disorders [27].
CAP cycles have also been evaluated in patients with epilepsy. In genetic generalized epilepsy, higher CAP rate is reported along with spikes occurring during phase A1. In lesional temporal lobe epilepsy, higher IEDs are seen during CAP cycle, specifically, during phase A1 as compared to non-CAP. Ninety-one percent of secondarily generalized focal lesional bursts are identified in CAP, while 96 % of all the generalized IEDs are found in CAP phase A [28]. Additionally, seizures also occurred during CAP cycle and in phase A than in phase B [29]. Moreover, in children with BECTS, CAP analysis showed reduced instability due to the presence of spikes which replaced the phase A1 and suggested that the centrotemporal spikes may disrupt the physiological synchronization mechanism [30]. In children with drug-resistant epilepsy, an increase of CAP rate in N2 was noted as compared to children with BECTS. Additionally, an increase in A1 index in N1 and N2 and significant reduction of A3 index in N1 were noted [31].
Based on these data, it is hypothesized that both CAP and IEDs are derived from similar if not the same anatomical pathways (thalamocortical). It is believed that CAP sequence triggers paroxysmal bursts like IEDs and IEDs promote the generation of phase A and, hence, increase instability. On the other hand, non-CAP part of sleep is unfavorable to IED generation due to reduced arousals [28].
Adenosine is also implicated in the complex relationships of sleep and epilepsy. Extracellular adenosine is antiepileptic, exerting its effects through pre- and postsynaptic adenosine receptors. The adenosine level depends upon the adenosine kinase (ADK) activity. Increased activity of ADK reduces adenosine and increases neuronal excitability. This endogenous adenosine mechanism is disrupted in chronic epilepsy. In studies, ADK activity was found to be overexpressed in mesial temporal sclerosis and temporal lobe epilepsy. Additionally, there was decreased expression of level of A1 receptors [32]. Moreover, adenosine is essential in regulation of sleep homeostasis. In the event of disrupted system, poor sleep is noted [33]. So dysregulated adenosine system may also be a factor causing poor sleep in patients with chronic epilepsy.
Sleep-Related Epilepsy Syndromes
Certain epilepsy syndromes are related to sleep-wake cycle or occur depending on sleep state or arousal from sleep. These are termed sleep-related epilepsies and include the following.
West Syndrome [34]
It is characterized by epileptic spasm, hypsarrhythmia, and developmental delay. The onset occurs at 3–12 months of age. The spasms are flexor or extensor movements of the head, trunk, and limbs, which are brief and typically occur in clusters. The classic EEG pattern of hypsarrhythmia is characterized by very high amplitude multifocal spikes occurring over a chaotic background. This pattern is often seen in NREM sleep at the onset of the disorder and sometimes exclusively. Additionally, the associated epileptic spasms occur in clusters soon after awakening, which is pseudo-normalization of the EEG during that time. Treatment is recommended as early as possible after the diagnosis. Adrenocorticotrophic hormone and vigabatrin are approved treatment options.
Panayiotopoulos Syndrome [34]
It is an age-related benign focal epilepsy syndrome with usual onset between 3 and 6 years of age. Seizures are characterized by nausea, visual changes, and prominent autonomic symptoms with preserved consciousness. Majority of seizures occur in sleep (70 %) or up on awakening (13 %). These seizures can last from 30 min to several hours (autonomic status). EEG most commonly shows occipital discharges; however, temporal and parietal discharges are also seen. The ictal EEG shows theta waves intermixed with spikes or fast activity in anterior or posterior head region. The prognosis is good with resolution within 1–2 years of onset.
Benign Epilepsy with Centrotemporal Spikes (BECTS) [34]
BECTS or benign Rolandic epilepsy is the most common epilepsy in childhood. The onset occurs between 3 and 13 years of age and remission occurs by 16 years of age. The typical seizures are hemifacial sensory or motor and associated with speech slurring and drooling. Consciousness is typically preserved. They may progress to unilateral arm and leg and occasionally to generalization. About 70 % of seizures occur in sleep. EEG shows characteristic spikes and wave discharges in fronto-central and temporal head region occurring independently or synchronously with a horizontal dipole. The IEDs are amplified in NREM sleep. The seizure frequency and severity is disproportionate to the amount of IEDs. Cognitive behavioral and sleep problems have been associated with the syndrome. Treatment with focal antiepileptic drugs is effective and long-term prognosis is good.
Electrical Status Epilepticus During Sleep (ESES) and Related Disorders [34]
ESES is characterized by spike and wave discharges occurring almost continuously during slow-wave sleep. This pattern is associated with seizures and cognitive dysfunction. The term continuous spike-wave discharges during sleep (CSWS) was coined to dissociate clinical connotation from “status epileptics” in the ESES terminology. These terms are used interchangeable in literature many times. The syndromes are age-dependent epileptic encephalopathies with peak onset at 2–4 years of age. The seizure onset is prior to typical EEG pattern. Generalized tonic-clonic seizures as well as daytime atypical absences are seen. Tonic seizures are not seen. Cognitive deficits and behavioral problems are associated with the syndrome and may occur as an acute regression or insidious development after months of seizure onset. Daytime EEG may show focal or generalized spikes and sleep EEG shows spike-wave index of 85–100 % during NREM sleep. Additionally, recognition of normal sleep architecture is difficult. Treatment of spikes may improve cognitive function and should be started immediately and aggressively after the diagnosis. Treatment options are high-dose benzodiazepines, steroids, valproic acid, levetiracetam, immunoglobulins, etc. The prognosis is dependent upon etiology, duration, and treatment response.
Landau-Kleffner Syndrome
It is a disorder characterized by acquired receptive aphasia due to auditory agnosia and epilepsy. The EEG shows almost continuous spike and wave discharges in unilateral or bilateral temporal region during NREM sleep. In addition to language, cognitive and behavioral problems can also be associated. Onset is between 2 and 8 years with regression. Treatment of EEG spikes improves language function. Treatments are similar to ESES treatments.
Atypical Benign Partial Epilepsy/Pseudo-Lennox Syndrome
The syndrome is characterized by similar presentation as benign focal epilepsies but associated ESES EEG pattern and mental deficits. The prognosis and treatments are similar to ESES.
The presence of GRIN2A mutations in ESES, Landau-Kleffner syndrome, and BECTS suggests that these syndromes possibly occur as a continuum.
Juvenile Myoclonic Epilepsy [34]
JME affects 1–2 % of general population worldwide. It is closely linked to sleep as most seizures occur upon awakening and sleep deprivation is a strong trigger for seizure occurrence. The age of onset is from 12 to 18 in 79 % of patients. The characteristic seizures are myoclonic jerks that occur upon or soon after awakenings and may progress to generalized tonic-clonic seizures. The myoclonic seizures may be missed at the onset as they are thought to be clumsiness (dropping things) or tics/twitches. The diagnosis is typically made after a generalized tonic-clonic seizure (GTC), and upon obtaining further history, the myoclonic seizures become evident. About 20 % of patients have absence seizure which may suggest a poor prognosis for seizure freedom if these occur at the onset of the epilepsy. The characteristic EEG pattern is polyspikes and waves and/or spike and wave discharges occurring at 2.5–3.5 Hz. Treatment with valproic acid and other broad-spectrum AEDs is recommended. Prognosis for seizure control on AEDs is good, with majority of the patients requiring lifelong treatment.
Nocturnal Frontal Lobe Epilepsy [34]
Nocturnal frontal lobe epilepsy represents an epilepsy syndrome which is misdiagnosed as parasomnia often. The onset is in adolescence or young adulthood. Three clinical seizure patterns were described which are (1) paroxysmal arousals, (2) nocturnal paroxysmal dystonia, and (3) episodic nocturnal wandering. The autosomal dominant type, called as autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE), is associated with mutations in nicotinic acetylcholine receptor (CHRNA4) and in other genes (KCNT1 and DEPDC5). The clinical manifestations can vary between individuals in the family, but for the same individual, the seizures are stereotypic. Complex behaviors and sleep-related violent behaviors may also be present in addition to above-described pattern. The corresponding EEG findings include ictal epileptiform abnormalities predominantly over frontal areas in 31.6 % of patients or rhythmic ictal slow-wave activity over larger anterior cortical areas in another 47.4 %. A third of patients also have associated non-REM parasomnias [35].
Effect of Seizures and Epilepsy on Sleep
A seizure occurring in sleep causes significant reduction of REM sleep and sleep efficiency and increases N1. If the seizure occurs before the first REM cycle, the REM sleep and sleep efficiency are further reduced. Decrease in total sleep time due to reduced REM sleep and increased wake times have also been reported [36].
Epilepsy also affects sleep. In adults with epilepsy, increased N1 and decreased N3 and REM were seen [37]. Additionally, increase in sleep instability in terms of stage shifts and sleep fragmentation caused by increased arousals and wake times was seen [36]. Fragmented sleep was more common in temporal lobe epilepsy as compared to frontal lobe or generalized epilepsy [36, 38]. In children with refractory focal epilepsy, decreased time in bed, total sleep time, and increased N3 were seen [39]. In children with generalized epilepsy, increased N1% and REM sleep latency were seen [40]. In children with epileptic encephalopathies, fragmented sleep, increased REM latency, and reduced total sleep times were seen [41]. In children with refractory epilepsy with a brain lesion, reduction in total sleep time and sleep latency and an increase in REM latency and wake times have been described [31]. In children with tuberous sclerosis, increased arousals, wake time, increased N1, and reduced REM sleep were seen [42]. As discussed above, poor quality of sleep essentially creates a sleep-deprived state which then can precipitate seizures. Additionally, reduction in REM sleep and increased N1 sleep also perpetuates seizures, which further reduces REM sleep.
Effect of Antiepileptic Drugs (AEDs) on Sleep
Various studies in healthy adults and patients with epilepsy show that AEDs also affect sleep architecture. In healthy adults, clobazam reduced sleep latency. Clobazam also reduced arousals and wake time, similar to levetiracetam, phenobarbital, tiagabine, and pregabalin. Carbamazepine reduced sleep latency, arousal, and wake times. Gabapentin increased REM sleep, while carbamazepine, levetiracetam, and phenobarbital reduced it. Levetiracetam, carbamazepine, tiagabine, and pregabalin enhanced slow-wave sleep. Lacosamide did not affect sleep architecture in healthy adults [43]. The effects of antiepileptic drugs in patients with epilepsy are shown in Table 15.1. Even though there are reports of AEDs increasing sleepiness, in objective studies this was not identified for zonisamide, lamotrigine, topiramate, and vigabatrin. Valproic acid, phenobarbital, and high-dose levetiracetam objectively caused sleepiness in studies [44].
Non-medication treatments of epilepsy have also been shown to influence sleep. VNS improved daytime sleepiness and slow-wave sleep. Epilepsy surgery improved total sleep time (TST) and reduced arousals if the seizure frequency was also improved. Ketogenic diet also improved nocturnal sleep. As discussed above, improved seizure frequency may affect the sleep architecture by itself. Hence, when evaluating effects of AEDs on sleep architecture, it is important to note that many of these studies did not analyze effects on sleep independent of improved seizure frequency [44].
Several AEDs have been implicated in either precipitating or worsening of sleep disorders. Vagus nerve stimulator use has been associated with sleep-related breathing disorders such as obstructive sleep apnea and central apneic patterns [45, 46]. AEDs such as benzodiazepine and phenobarbital have been suggested to worsen obstructive sleep apnea [47]. Depakote is also suggested to worsen OSA; however, this was not found in a study [48]. Felbamate and lamotrigine have been thought to worsen insomnia [47]. A recent study suggested that zonisamide by affecting carbonic anhydrase activity and causing weight loss may improve obstructive sleep apnea in obese adults with epilepsy [49].
Antiepileptic drugs significantly affect sleep architecture; hence the selection of AED for an individual patient should be customized, i.e., in a patient with insomnia, gabapentin may be useful. In a patient with higher risk of sleep apnea, proper sleep evaluation and treatment should be undertaken and continued before VNS is implanted and stimulation is increased to rapid cycling. Felbamate and possibly lamotrigine should be avoided or administered early in the evening in patients with insomnia. Valproic acid and phenobarbital should be avoided in children with excessive sleepiness in addition to sleep evaluation.
Sleep Disorders in Epilepsy and Impact of Treatment of Sleep Disorders on Epilepsy
Sleep disorders are common in epilepsy and many of the disorders have a higher prevalence than the general population.
Questionnaire-Based Studies for Sleep Problems
Studies using questionnaires have shown that children with epilepsy have higher sleep problems than siblings or healthy controls. Difficulty initiating and maintaining sleep and co-sleeping were more common in children with epilepsy as compared to siblings [50–54]. Even in children with new onset seizures, sleep problems were present in 45 % and were associated with worse neuropsychological functioning [51]. Among epilepsy-related factors, nocturnal seizures and seizure frequency contributed toward higher sleep problems [50]. In younger children, sleep-related anxieties were more common, while in older children, poor sleep was associated with poor daytime behavior [55]. Additionally in a study, higher sleep problems were associated with worse quality of life [53].
Sleep Apnea
In adults with refractory epilepsy, obstructive sleep apnea was noted in a third of the patients [56]. Several other studies have suggested higher prevalence of OSA in epilepsy as compared to general population [22, 48]. In children with epilepsy, screened with clinical history and questionnaires for OSA, 80 % had obstructive apnea [57]. In retrospective studies in patients referred to sleep lab, sleep-disordered breathing is reported in 40 % of children [58]. In another study, uncontrolled epilepsy was a risk factor for obstructive sleep apnea as compared with primary snoring [48]. Obstructive index increased with increasing number of antiepileptic drugs [48]. Additionally, children with epilepsy had higher number of arousals, prolonged sleep latency, and higher O2 desaturations as compared to controls with higher severity of OSA [58].
Central Sleep Apnea (CSA)
A retrospective study suggested that children with abnormal MRI of the brain are at higher risk of central sleep apnea [59]. No other data exist in children. In adults with epilepsy, OSA and mixed apnea were more prevalent than CSA. CSA was more common in males and in focal epilepsy [60]. Central apneas are also associated with seizures [31].
Restless Leg Syndrome (RLS)/Periodic Limb Movement Disorder (PLMD)
In retrospective studies in cohort of children referred to sleep lab, PLMs/PLMD was found in 5–10 % [58, 61]. In studies in adults with epilepsy, 15 % had PLMD and 17 % had PLMs in sleep [62, 63]. In adult patients with epilepsy, RLS was identified in 18–35 % [62, 64]. No data exist on RLS in children with epilepsy. This may be due to difficulties in diagnosing children with RLS due to difficulty obtaining history from younger children, confusing the diagnosis with growing pains and studies focusing on referrals to sleep lab. As RLS and PLMD coexist in children, it is possible that some of the studies may have included the children with combination of the disorders.
Insomnia
Insomnia is under-recognized in children with epilepsy. In a study, 82 % of surveyed providers used melatonin or a hypnotic for sleep problems, prior to referral to a sleep specialist [61]. In children with epilepsy referred for sleep evaluation, insomnia was identified in 11 % [61]. In adult with epilepsy, 40–55 % subjects had insomnia [51, 65]. Sleep maintenance insomnia is more common (52 %) than sleep onset insomnia (34 %) [64]. Insomnia correlates with number of AEDs and higher scores on depression scales. Insomnia and poor sleep quality predict poorer quality of life [66].
Parasomnia
Parasomnias are common in children, especially in younger children. Hence, just by mere association, these are common in children with epilepsy also. This presents challenges for diagnosis in nocturnal epilepsy. Additionally, in patients with nocturnal frontal lobe epilepsy (NFLE), 30 % also have arousal parasomnia [67]. Hence, evaluation with careful history and video EEG monitoring may be needed for accurate diagnosis in these children. Some of the differentiating features include onset parasomnia seen in children younger than 10 years of age, whereas seizures of NFLE start at a later age, and parasomnia events are longer, have different behavior patterns, and occur during earlier part of the night, out of N3. On the other end, NFLE seizures are brief and highly stereotypic, may occur multiple times in the night, and are usually out of N1/N2 [68].
Sleepiness
Sleepiness is very common in children with epilepsy, present in 28–48 % of patients. However, referrals for sleep evaluations are limited for this complaint. The reason may be that most neurologists attribute sleepiness to antiepileptic drugs [61]. However, prospective studies in adults with epilepsy suggest that sleepiness is correlated with sleep apnea and RLS symptoms, habitual snoring, observed apneas, recurrence of seizures, neck circumference, and anxiety also [62, 69, 70]. Similarly, in children with epilepsy, 46.2 % of children with epilepsy had sleepiness which was associated with sleep disorders and not with the epilepsy syndrome, AEDs, and the presence or absence of seizure freedom [71].
Impact of Treatment of Sleep Disorders
OSA
There are several studies showing that treatment of OSA improves seizure frequency. A retrospective review in adult patients with OSA and epilepsy, treated with CPAP at least for 6 months, showed decreased seizure frequency. More than half of the CPAP-compliant subjects became seizure-free. In the non-compliant group, no significant differences were seen [72]. CPAP also improved IEDs in wakefulness and sleep except for REM sleep [73]. In a randomized study, 50 % responder rate was 28 % on CPAP as compared to 15 % of controls [74]. A recent study showed that the odds of more than 50 % reduction or seizure freedom in PAP-treated subjects were 9.9 and 3.91 times compared to untreated OSA and no OSA, respectively. PAP-treated subjects had 32.3 times the odds of having 50 % or more seizure reduction compared with the untreated OSA and 6.13 times compared with no OSA [75]. Additionally, treatment of underlying OSA with adenotonsillectomy resulted in improvement in seizure frequency [76].
Melatonin
A few randomized studies evaluated the effect of treatment of insomnia with melatonin in epilepsy. In a study, significant improvement was seen in sleep questionnaire total sleep score on melatonin [77]. In a study in children and young adults, no improvement was seen on actigraphy or sleep diary [78]. However, seizure frequency was significantly reduced. In another study, sleep latency was reduced on melatonin on sleep logs [79]. In a class I study, sleep latency and WASO were improved significantly. Additionally, there was some improvement in sleep efficiency (3.8 %) on polysomnography, total sleep time on actigraphy, and sleep duration and later wake times based on sleep diary on melatonin. Moreover, N3% was increased on melatonin. There was a trend toward improvement in epileptiform discharges [80].
Sudden Unexpected Death in Epilepsy (SUDEP), Sleep, and Cardiorespiratory Abnormalities
SUDEP is defined as a “sudden, unexpected, witnessed or unwitnessed, non-traumatic and non-drowning death in patients with epilepsy with or without evidence for a seizure and excluding documented status epilepticus in which postmortem examination does not reveal a toxicologic or anatomic cause for death” [81]. The incidence depends on the age, the seizure frequency, and the type of epilepsy and could be as high as 6.0–9.3 per 1000 patient-years among patients with refractory surgery evaluated for or treated with epilepsy surgery or vagus nerve stimulation for epilepsy [82]. The incidence in children is estimated to be 1–2/10,000 patient-years, with a slight male preponderance [83]. Up to 70 % of these deaths occur in sleep, and hence, it is a concern for sleep providers as they may be evaluating patients at risk for it. A variety of risk factors and mechanisms have been suggested and there is no one accepted theory for causation. In children, the risk factors are believed to be major neurological impairment, refractory seizures, and generalized tonic-clonic seizures. In a study, half of the children with SUDEP had symptomatic epilepsy [83]. In children with epilepsy but without neurological handicap, risk of death was similar to general population [84]. Since most deaths occur after seizures, it is believed that it is related to events occurring during or after seizures. One of the mechanisms thought to be responsible for SUDEP is respiratory and cardiac changes during seizures. The respiratory abnormalities include central and obstructive apneas, hypoventilation, hypercapnia, and desaturation with acidosis, bradypnea, and tachypnea [85]. Respiratory abnormalities such as central apnea or hypopneas were noted in 53 % of the seizures, and oxygen desaturation below 90 % occurred in a third of the seizures. Additionally, there was substantial increase in CO2 levels [86]. In studies in pediatric epilepsy, risk factors for ictal central apnea were younger age, temporal lobe seizures, left hemispheric seizures, symptomatic generalized seizures, longer seizures, desaturation, ictal bradycardia, and more antiepileptic drugs. Similarly, desaturation was more prevalent in longer-duration seizures, ictal apnea, ictal bradycardia, and more AEDs [87]. The cardiac abnormalities include postictal changes in heart rate variability caused by sympathetic activation, ictal bradycardia, asystole, repolarization, anomalies (prolonged or shortened QTc interval), and atrial fibrillation [85]. In pediatric epilepsy, ictal bradycardia was more prevalent in male patients, longer-duration seizures, desaturation, and more AEDs [87]. Additionally, children with Dravet syndrome have also been shown to be at higher risk due to decrease in heart rate variability presumably caused by sodium channel mutations [88, 89]. Moreover, postictal EEG suppression may be another mechanism which is more common in adults [85, 90]. Dysfunction in the serotonin system has been linked to epilepsy. Additionally, respiratory changes such as apnea or hypoventilation are common with generalized seizures. Serotonergic system also plays an important role in breathing control. Additionally, in animal model of epilepsy, SSRIs have been shown to reduce post-seizure respiratory arrest [86]. Hence, SSRIs may have a role in SUDEP prevention.
Behavior, Quality of Life, and Memory, Sleep, and Epilepsy
Poor memory, behavior, and quality of life along with psychiatric problems are common in patients with epilepsy. Sleep problems can worsen these [25]. Even in children with new onset seizures, sleep disturbances are associated with higher behavioral problems as well as poorer neuropsychological function [51]. Other studies have shown more behavioral problems and poorer psychological functioning in children with sleep problems than without sleep problems [25, 55]. Additionally, psychiatric problems and depression are also associated with epilepsy. In a recent study, suicidal ideation was also linked to poor sleep quality in patients with epilepsy [91]. Moreover, patients with epilepsy and sleep problems have poorer quality of life as compared to patients without sleep problems [92–94]. These have been seen in the domains of physical cognitive and social function [53]. Furthermore, sleep enhances memory consolidation. Slow-wave sleep enhances declarative memories, while REM sleep improves procedural and emotional memory. Hence, poor sleep can affect memory in children with epilepsy. In a recent study, children with idiopathic focal epilepsies had poorer sleep-related memory consolidation. This also correlated with IEDs in NREM sleep [95]. Hence, sleep problems worsen the other comorbidities of epilepsy, and adequate treatments should be performed for sleep problems and sleep disorders.
Conclusion
Sleep and epilepsy are interrelated and worsening of one worsens the other and sets up a vicious cycle. Epilepsy comorbidities of poor behavior, quality of life, and memory are further worsened by poor sleep. Moreover, sleep disorders are very common and treatment of them may improve seizure control. Hence, education on improving sleep quality and screening, evaluation, and treatment for sleep problems should be a part of routine care in patients with epilepsy.
References
Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342(5):314–9.
Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55(4):475–82. doi:10.1111/epi.12550.
Bazil CW, Malow BA, Sammaritano MR. Sleep and epilepsy: the clinical spectrum. 1st ed. Amsterdam: Elsevier; 2002.
Lüders H, Dinner DS. Epilepsy and sleep: physiological and clinical relationships. San Diego: Academic; 2001.
Kotagal P. The relationship between sleep and epilepsy. Semin Pediatr Neurol. 2001;8(4):241–50.
Malow BA, Lin X, Kushwaha R, Aldrich MS. Interictal spiking increases with sleep depth in temporal lobe epilepsy. Epilepsia. 1998;39(12):1309–16.
Sammaritano M, Gigli GL, Gotman J. Interictal spiking during wakefulness and sleep and the localization of foci in temporal lobe epilepsy. Neurology. 1991;41(2 (Pt 1)):290–7.
Foldvary-Schaefer N, Grigg-Damberger M. Sleep and epilepsy. Semin Neurol. 2009;29(4):419–28. doi:10.1055/s-0029-1237115.
Malow BA, Aldrich MS. Localizing value of rapid eye movement sleep in temporal lobe epilepsy. Sleep Med. 2000;1(1):57–60.
Rocamora R, Andrzejak RG, Jimenez-Conde J, Elger CE. Sleep modulation of epileptic activity in mesial and neocortical temporal lobe epilepsy: a study with depth and subdural electrodes. Epilepsy Behav. 2013;28(2):185–90. doi:10.1016/j.yebeh.2013.04.010.
Shinnar S, Kang H, Berg AT, Goldensohn ES, Hauser WA, Moshe SL. EEG abnormalities in children with a first unprovoked seizure. Epilepsia. 1994;35(3):471–6.
Kothare SV, Kaleyias J. Sleep and epilepsy in children and adolescents. Sleep Med. 2010;11(7):674–85. doi:10.1016/j.sleep.2010.01.012. S1389-9457(10)00214-5 [pii].
Ng M, Pavlova M. Why are seizures rare in rapid eye movement sleep? Review of the frequency of seizures in different sleep stages. Epilepsy Res Treat. 2013;2013:932790. doi:10.1155/2013/932790.
Crespel A, Coubes P, Baldy-Moulinier M. Sleep influence on seizures and epilepsy effects on sleep in partial frontal and temporal lobe epilepsies. Clin Neurophysiol. 2000;111 Suppl 2:S54–9. doi:S1388245700004028 [pii].
Herman ST, Walczak TS, Bazil CW. Distribution of partial seizures during the sleep – wake cycle: differences by seizure onset site. Neurology. 2001;56(11):1453–9.
Bazil CW, Walczak TS. Effects of sleep and sleep stage on epileptic and nonepileptic seizures. Epilepsia. 1997;38(1):56–62.
Zarowski M, Loddenkemper T, Vendrame M, Alexopoulos AV, Wyllie E, Kothare SV. Circadian distribution and sleep/wake patterns of generalized seizures in children. Epilepsia. 2011;52(6):1076–83. doi:10.1111/j.1528-1167.2011.03023.x.
Hofstra WA, Spetgens WP, Leijten FS, van Rijen PC, Gosselaar P, van der Palen J, et al. Diurnal rhythms in seizures detected by intracranial electrocorticographic monitoring: an observational study. Epilepsy Behav. 2009;14(4):617–21. doi:10.1016/j.yebeh.2009.01.020.
Durazzo TS, Spencer SS, Duckrow RB, Novotny EJ, Spencer DD, Zaveri HP. Temporal distributions of seizure occurrence from various epileptogenic regions. Neurology. 2008;70(15):1265–71. doi:10.1212/01.wnl.0000308938.84918.3f.
Hofstra WA, Gordijn MC, van der Palen J, van Regteren R, Grootemarsink BE, de Weerd AW. Timing of temporal and frontal seizures in relation to the circadian phase: a prospective pilot study. Epilepsy Res. 2011;94(3):158–62. doi:10.1016/j.eplepsyres.2011.01.015.
Pavlova MK, Woo Lee J, Yilmaz F, Dworetzky BA. Diurnal pattern of seizures outside the hospital: is there a time of circadian vulnerability? Neurology. 2012;78(19):1488–92. doi:10.1212/WNL.0b013e3182553c23.
Baxendale S. Seeing the light? Seizures and sunlight. Epilepsy Res. 2009;84(1):72–6. doi:10.1016/j.eplepsyres.2008.11.015.
Guilhoto LM, Loddenkemper T, Vendrame M, Bergin A, Bourgeois BF, Kothare SV. Higher evening antiepileptic drug dose for nocturnal and early-morning seizures. Epilepsy Behav. 2011;20(2):334–7. doi:10.1016/j.yebeh.2010.11.017.
Fang PC, Chen YJ, Lee IC. Seizure precipitants in children with intractable epilepsy. Brain Dev. 2008;30(8):527–32.
van Golde EG, Gutter T, de Weerd AW. Sleep disturbances in people with epilepsy; prevalence, impact and treatment. Sleep Med Rev. 2011. doi:10.1016/j.smrv.2011.01.002. doi:S1087-0792(11)00004-9 [pii].
Malow BA. Sleep deprivation and epilepsy. Epilepsy Curr. 2004;4(5):193–5. doi:10.1111/j.1535-7597.2004.04509.x.
Parrino L, Ferri R, Bruni O, Terzano MG. Cyclic alternating pattern (CAP): the marker of sleep instability. Sleep Med Rev. 2012;16(1):27–45. doi:10.1016/j.smrv.2011.02.003.
Parrino L, Smerieri A, Spaggiari MC, Terzano MG. Cyclic alternating pattern (CAP) and epilepsy during sleep: how a physiological rhythm modulates a pathological event. Clin Neurophysiol. 2000;111 Suppl 2:S39–46.
Manni R, Zambrelli E, Bellazzi R, Terzaghi M. The relationship between focal seizures and sleep: an analysis of the cyclic alternating pattern. Epilepsy Res. 2005;67(1-2):73–80. doi:10.1016/j.eplepsyres.2005.08.008.
Bruni O, Novelli L, Luchetti A, Zarowski M, Meloni M, Cecili M, et al. Reduced NREM sleep instability in benign childhood epilepsy with centro-temporal spikes. Clin Neurophysiol. 2010;121(5):665–71. doi:10.1016/j.clinph.2009.12.027.
Pereira AM, Bruni O, Ferri R, Palmini A, Nunes ML. The impact of epilepsy on sleep architecture during childhood. Epilepsia. 2012;53(9):1519–25. doi:10.1111/j.1528-1167.2012.03558.x.
Boison D. Adenosine dysfunction in epilepsy. Glia. 2012;60(8):1234–43. doi:10.1002/glia.22285.
Boison D, Aronica E. Comorbidities in neurology: is adenosine the common link? Neuropharmacology. 2015;97:18–34. doi:10.1016/j.neuropharm.2015.04.031.
Schmitt B. Sleep and epilepsy syndromes. Neuropediatrics. 2015;46(3):171–80. doi:10.1055/s-0035-1551574.
Jain SV, Kothare SV. Sleep and epilepsy. Semin Pediatr Neurol. 2015;22(2):86–92. doi:10.1016/j.spen.2015.03.005.
Touchon J, Baldy-Moulinier M, Billiard M, Besset A, Cadilhac J. Sleep organization and epilepsy. Epilepsy Res Suppl. 1991;2:73–81.
Marzec ML, Selwa LM, Malow BA. Analysis of the first night effect and sleep parameters in medically refractory epilepsy patients. Sleep Med. 2005;6(3):277–80. doi:10.1016/j.sleep.2005.01.002. doi:S1389-9457(05)00023-7 [pii].
Crespel A, Baldy-Moulinier M, Coubes P. The relationship between sleep and epilepsy in frontal and temporal lobe epilepsies: practical and physiopathologic considerations. Epilepsia. 1998;39(2):150–7.
Nunes ML, Ferri R, Arzimanoglou A, Curzi L, Appel CC, Costa da Costa J. Sleep organization in children with partial refractory epilepsy. J Child Neurol. 2003;18(11):763–6.
Maganti R, Sheth RD, Hermann BP, Weber S, Gidal BE, Fine J. Sleep architecture in children with idiopathic generalized epilepsy. Epilepsia. 2005;46(1):104–9. doi:10.1111/j.0013-9580.2005.06804.x. doi:EPI06804 [pii].
Carotenuto M, Parisi P, Esposito M, Cortese S, Elia M. Sleep alterations in children with refractory epileptic encephalopathies: a polysomnographic study. Epilepsy Behav. 2014;35:50–3. doi:10.1016/j.yebeh.2014.03.009.
Bruni O, Cortesi F, Giannotti F, Curatolo P. Sleep disorders in tuberous sclerosis: a polysomnographic study. Brain Dev. 1995;17(1):52–6.
Hudson JD, Guptill JT, Byrnes W, Yates SL, Williams P, D’Cruz O. Assessment of the effects of lacosamide on sleep parameters in healthy subjects. Seizure. 2015;25:155–9. doi:10.1016/j.seizure.2014.10.012.
Jain SV, Glauser TA. Effects of epilepsy treatments on sleep architecture and daytime sleepiness: an evidence-based review of objective sleep metrics. Epilepsia. 2014;55(1):26–37. doi:10.1111/epi.12478.
Parhizgar F, Nugent K, Raj R. Obstructive sleep apnea and respiratory complications associated with vagus nerve stimulators. J Clin Sleep Med. 2011;7(4):401–7. doi:10.5664/JCSM.1204.
Khurana DS, Reumann M, Hobdell EF, Neff S, Valencia I, Legido A, et al. Vagus nerve stimulation in children with refractory epilepsy: unusual complications and relationship to sleep-disordered breathing. Child’s Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg. 2007;23(11):1309–12. doi:10.1007/s00381-007-0404-8.
Bazil CW. Effects of antiepileptic drugs on sleep structure: are all drugs equal? CNS Drugs. 2003;17(10):719–28. doi:17103 [pii].
Jain SV, Horn PS, Simakajornboon N, Glauser TA. Obstructive sleep apnea and primary snoring in children with epilepsy. J Child Neurol. 2012. doi:10.1177/0883073812440326. doi:0883073812440326 [pii].
Eskandari D, Zou D, Karimi M, Stenlof K, Grote L, Hedner J. Zonisamide reduces obstructive sleep apnoea: a randomised placebo-controlled study. Eur Respir J. 2014;44(1):140–9. doi:10.1183/09031936.00158413.
Batista BH, Nunes ML. Evaluation of sleep habits in children with epilepsy. Epilepsy Behav. 2007;11(1):60–4. doi:10.1016/j.yebeh.2007.03.016. doi:S1525-5050(07)00100-X [pii].
Byars AW, Byars KC, Johnson CS, DeGrauw TJ, Fastenau PS, Perkins S, et al. The relationship between sleep problems and neuropsychological functioning in children with first recognized seizures. Epilepsy Behav. 2008;13(4):607–13.
Cortesi F, Giannotti F, Ottaviano S. Sleep problems and daytime behavior in childhood idiopathic epilepsy. Epilepsia. 1999;40(11):1557–65.
Wirrell E, Blackman M, Barlow K, Mah J, Hamiwka L. Sleep disturbances in children with epilepsy compared with their nearest-aged siblings. Dev Med Child Neurol. 2005;47(11):754–9. doi:10.1017/S0012162205001581.
Ong LC, Yang WW, Wong SW, alSiddiq F, Khu YS. . Sleep habits and disturbances in Malaysian children with epilepsy. J Paediatr Child Health. 2010;46(3):80–4. doi:10.1111/j.1440-1754.2009.01642.x.
Stores G, Wiggs L, Campling G. Sleep disorders and their relationship to psychological disturbance in children with epilepsy. Child Care Health Dev. 1998;24(1):5–19.
Malow BA, Levy K, Maturen K, Bowes R. Obstructive sleep apnea is common in medically refractory epilepsy patients. Neurology. 2000;55(7):1002–7.
Becker DA, Fennell EB, Carney PR. Daytime behavior and sleep disturbance in childhood epilepsy. Epilepsy Behav. 2004;5(5):708–15.
Kaleyias J, Cruz M, Goraya JS, Valencia I, Khurana DS, Legido A, et al. Spectrum of polysomnographic abnormalities in children with epilepsy. Pediatr Neurol. 2008;39(3):170–6. doi:10.1016/j.pediatrneurol.2008.06.002. doi:S0887-8994(08)00265-8 [pii].
Kritzinger FE, Al-Saleh S, Narang I. Descriptive analysis of central sleep apnea in childhood at a single center. Pediatr Pulmonol. 2011;46(10):1023–30. doi:10.1002/ppul.21469.
Vendrame M, Jackson S, Syed S, Kothare SV, Auerbach SH. Central sleep apnea and complex sleep apnea in patients with epilepsy. Sleep Breathing Schlaf Atmung. 2014;18(1):119–24. doi:10.1007/s11325-013-0858-8.
Jain SV, Simakajornboon N, Glauser TA. Provider practices impact adequate diagnosis of sleep disorders in children with epilepsy. J Child Neurol. 2012. doi:10.1177/0883073812449692. doi:0883073812449692 [pii].
Malow BA, Bowes RJ, Lin X. Predictors of sleepiness in epilepsy patients. Sleep. 1997;20(12):1105–10.
Malow BA, Fromes GA, Aldrich MS. Usefulness of polysomnography in epilepsy patients. Neurology. 1997;48(5):1389–94.
Khatami R, Zutter D, Siegel A, Mathis J, Donati F, Bassetti CL. Sleep-wake habits and disorders in a series of 100 adult epilepsy patients – a prospective study. Seizure. 2006;15(5):299–306. doi:10.1016/j.seizure.2006.02.018. doi:S1059-1311(06)00044-6 [pii].
Lopez MR, Cheng JY, Kanner AM, Carvalho DZ, Diamond JA, Wallace DM. Insomnia symptoms in South Florida military veterans with epilepsy. Epilepsy Behav. 2013;27(1):159–64. doi:10.1016/j.yebeh.2013.01.008.
Vendrame M, Yang B, Jackson S, Auerbach SH. Insomnia and epilepsy: a questionnaire-based study. J Clin Sleep Med. 2013;9(2):141–6. doi:10.5664/jcsm.2410.
Bisulli F, Vignatelli L, Naldi I, Licchetta L, Provini F, Plazzi G, et al. Increased frequency of arousal parasomnias in families with nocturnal frontal lobe epilepsy: a common mechanism? Epilepsia. 2010;51(9):1852–60. doi:10.1111/j.1528-1167.2010.02581.x.
Derry CP, Duncan JS, Berkovic SF. Paroxysmal motor disorders of sleep: the clinical spectrum and differentiation from epilepsy. Epilepsia. 2006;47(11):1775–91. doi:10.1111/j.1528-1167.2006.00631.x. doi:EPI631 [pii].
Manni R, Politini L, Sartori I, Ratti MT, Galimberti CA, Tartara A. Daytime sleepiness in epilepsy patients: evaluation by means of the Epworth sleepiness scale. J Neurol. 2000;247(9):716–7.
Giorelli AS, Neves GS, Venturi M, Pontes IM, Valois A, Gomes Mda M. Excessive daytime sleepiness in patients with epilepsy: a subjective evaluation. Epilepsy Behav. 2011;21(4):449–52. doi:10.1016/j.yebeh.2011.05.002.
Maganti R, Hausman N, Koehn M, Sandok E, Glurich I, Mukesh BN. Excessive daytime sleepiness and sleep complaints among children with epilepsy. Epilepsy Behav. 2006;8(1):272–7. doi:10.1016/j.yebeh.2005.11.002. doi:S1525-5050(05)00464-6 [pii].
Vendrame M, Auerbach S, Loddenkemper T, Kothare S, Montouris G. Effect of continuous positive airway pressure treatment on seizure control in patients with obstructive sleep apnea and epilepsy. Epilepsia. 2011;52(11):e168–71. doi:10.1111/j.1528-1167.2011.03214.x.
Pornsriniyom D, Shinlapawittayatorn K, Fong J, Andrews ND, Foldvary-Schaefer N. Continuous positive airway pressure therapy for obstructive sleep apnea reduces interictal epileptiform discharges in adults with epilepsy. Epilepsy Behav. 2014;37:171–4. doi:10.1016/j.yebeh.2014.06.025.
Malow BA, Foldvary-Schaefer N, Vaughn BV, Selwa LM, Chervin RD, Weatherwax KJ, et al. Treating obstructive sleep apnea in adults with epilepsy: a randomized pilot trial. Neurology. 2008;71(8):572–7.
Pornsriniyom D, Kim H, Bena J, Andrews ND, Moul D, Foldvary-Schaefer N. Effect of positive airway pressure therapy on seizure control in patients with epilepsy and obstructive sleep apnea. Epilepsy Behav. 2014;37:270–5. doi:10.1016/j.yebeh.2014.07.005.
Segal E, Vendrame M, Gregas M, Loddenkemper T, Kothare SV. Effect of treatment of obstructive sleep apnea on seizure outcomes in children with epilepsy. Pediatr Neurol. 2012;46(6):359–62. doi:10.1016/j.pediatrneurol.2012.03.005.
Gupta M, Aneja S, Kohli K. Add-on melatonin improves sleep behavior in children with epilepsy: randomized, double-blind, placebo-controlled trial. J Child Neurol. 2005;20(2):112–5.
Goldberg-Stern H, Oren H, Peled N, Garty BZ. Effect of melatonin on seizure frequency in intractable epilepsy: a pilot study. J Child Neurol. 2012;27(12):1524–8. doi:10.1177/0883073811435916.
Coppola G, Iervolino G, Mastrosimone M, La Torre G, Ruiu F, Pascotto A. Melatonin in wake-sleep disorders in children, adolescents and young adults with mental retardation with or without epilepsy: a double-blind, cross-over, placebo-controlled trial. Brain Dev. 2004;26(6):373–6.
Jain SV, Horn PS, Simakajornboon N, Beebe DW, Holland K, Byars AW, et al. Melatonin improves sleep in children with epilepsy: a randomized, double-blind, crossover study. Sleep Med. 2015;16(5):637–44. doi:10.1016/j.sleep.2015.01.005.
Nashef L. Sudden unexpected death in epilepsy: terminology and definitions. Epilepsia. 1997;38(11 Suppl):S6–8. doi:10.1111/j.1528-1157.1997.tb06130.x.
Devinsky O. Sudden, unexpected death in epilepsy. N Engl J Med. 2011;365(19):1801–11. doi:10.1056/NEJMra1010481.
Camfield P, Camfield C. Sudden unexpected death in people with epilepsy: a pediatric perspective. Semin Pediatr Neurol. 2005;12(1):10–4.
Berg AT, Nickels K, Wirrell EC, Geerts AT, Callenbach PM, Arts WF, et al. Mortality risks in new-onset childhood epilepsy. Pediatrics. 2013;132(1):124–31. doi:10.1542/peds.2012-3998.
Kothare SV, Singh K. Cardiorespiratory abnormalities during epileptic seizures. Sleep Med. 2014;15(12):1433–9. doi:10.1016/j.sleep.2014.08.005.
Richerson GB, Buchanan GF. The serotonin axis: shared mechanisms in seizures, depression, and SUDEP. Epilepsia. 2011;52 Suppl 1:28–38. doi:10.1111/j.1528-1167.2010.02908.x.
Singh K, Katz ES, Zarowski M, Loddenkemper T, Llewellyn N, Manganaro S, et al. Cardiopulmonary complications during pediatric seizures: a prelude to understanding SUDEP. Epilepsia. 2013;54(6):1083–91. doi:10.1111/epi.12153.
Skluzacek JV, Watts KP, Parsy O, Wical B, Camfield P. Dravet syndrome and parent associations: the IDEA League experience with comorbid conditions, mortality, management, adaptation, and grief. Epilepsia. 2011;52 Suppl 2:95–101. doi:10.1111/j.1528-1167.2011.03012.x.
Delogu AB, Spinelli A, Battaglia D, Dravet C, De Nisco A, Saracino A, et al. Electrical and autonomic cardiac function in patients with Dravet syndrome. Epilepsia. 2011;52 Suppl 2:55–8. doi:10.1111/j.1528-1167.2011.03003.x.
Pavlova M, Singh K, Abdennadher M, Katz ES, Dworetzky BA, White DP, et al. Comparison of cardiorespiratory and EEG abnormalities with seizures in adults and children. Epilepsy Behav. 2013;29(3):537–41. doi:10.1016/j.yebeh.2013.09.026.
Wigg CM, Filgueiras A, Gomes Mda M. The relationship between sleep quality, depression, and anxiety in patients with epilepsy and suicidal ideation. Arq Neuropsiquiatr. 2014;72(5):344–8.
de Weerd A, de Haas S, Otte A, Trenite DK, van Erp G, Cohen A, et al. Subjective sleep disturbance in patients with partial epilepsy: a questionnaire-based study on prevalence and impact on quality of life. Epilepsia. 2004;45(11):1397–404.
Xu X, Brandenburg NA, McDermott AM, Bazil CW. Sleep disturbances reported by refractory partial-onset epilepsy patients receiving polytherapy. Epilepsia. 2006;47(7):1176–83.
Piperidou C, Karlovasitou A, Triantafyllou N, Terzoudi A, Constantinidis T, Vadikolias K, et al. Influence of sleep disturbance on quality of life of patients with epilepsy. Seizure. 2008;17(7):588–94. doi:10.1016/j.seizure.2008.02.005. doi:S1059-1311(08)00057-5 [pii].
Galer S, Urbain C, De Tiege X, Emeriau M, Leproult R, Deliens G, et al. Impaired sleep-related consolidation of declarative memories in idiopathic focal epilepsies of childhood. Epilepsy Behav. 2014;43C:16–23. doi:10.1016/j.yebeh.2014.11.032.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Jain, S.V., Kothare, S.V. (2017). Sleep and Epilepsy. In: Nevšímalová, S., Bruni, O. (eds) Sleep Disorders in Children. Springer, Cham. https://doi.org/10.1007/978-3-319-28640-2_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-28640-2_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28638-9
Online ISBN: 978-3-319-28640-2
eBook Packages: MedicineMedicine (R0)