Abstract
Mitochondrial diseases are connected to a plethora of clinical phenotypes, with the majority of them connected to pathologies within the nervous system. Mutations in either mtDNA or nDNA genes coding for mitochondrial proteins are known to lead to catastrophic diseases in humans that are the most common cause of inborn errors of metabolism, with a frequency of about 1 in 5000. Therefore, an understanding of mitochondrial roles in normal physiology and pathological conditions is essential for the development of possible treatments for patients suffering from various forms of mitochondrial disease. Many attempts have been made to model mitochondrial dysfunction, but this has proven to be challenging due to unique features of mitochondrial genetics. Despite this, over the last 20 years, a number of very important transgenic mouse models have been developed that in a lesser or higher degree recapitulated changes detected in human patients. Here we discuss some of the most important mouse models generated to mimic mitochondrial encephalomyopathies and the lessons learned from them.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Mitochondrial encephalomyopathies
- Mitochondrial diseases
- mtDNA
- OXPHOS deficiency
- Cybrids
- Transgenic mice
- CaMKIIα-Cre
- mtDNA mutations
- Neuronal dysfunction
- Ataxia
- Leucoencephalopathy
1 Introduction
Mitochondria are unique organelles that allowed the development of multicellular life on our planet by providing eukaryotic cells with a highly efficient form of energy production, through the process of oxidative phosphorylation (OXPHOS). Besides this, mitochondria play an important role in versatile cell processes and signalling pathways, including calcium homeostasis, cell cycle regulation, apoptosis, reactive oxygen species (ROS) production, and thermogenesis [1]. As a relic of their alphaproteobacterial origin, they possess their own genome, mitochondrial DNA (mtDNA) that encodes 13 polypeptide subunits of OXPHOS complexes I, III, IV, and V and a full set of RNAs (22 tRNAs and 2 rRNAs) necessary for the effective protein synthesis inside mitochondria. All other polypeptides (≈1500), including other OXPHOS subunits, various metabolic enzymes, and a full complement of proteins required for mtDNA maintenance and expression, are encoded by the nuclear genome (nDNA), translated in the cytoplasm, and imported into mitochondria (see Chap. 1). The dual origin of mitochondrial proteins gives clear ideas about the importance of the constant and regulated communication between nDNA and mtDNA for the maintenance of cell metabolism and homeostasis. Moreover, mitochondrial dynamics and involvement in cellular adaptive responses and quality control through processes of autophagy and apoptosis add additional layers to the integral picture of mitochondria complexity.
The integration of mitochondria into different aspects of cell physiology is reflected by dramatic repercussions linked to mitochondrial dysfunction. Syndromes featuring impaired mitochondrial energy production are commonly referred to as “mitochondrial diseases”. Although mitochondrial diseases are usually multisystemic, the brain and muscle are the most commonly affected tissues. This notion became apparent almost four decades ago when paediatric neurologists coined the term “mitochondrial encephalomyopathies” to call attention to the frequent occurrence of brain disease in children with mitochondrial alterations in their muscle biopsies [2]. This term today is reserved for defects of the respiratory chain (OXPHOS). Even within these boundaries, the classification of the mitochondrial encephalomyopathies became quite complicated, including two types of primary mtDNA mutations (impairment of global mitochondrial protein synthesis and of the translation of specific respiratory chain subunits), and a much larger menu of Mendelian disorders (due to mutations in nuclear-encoded mitochondrial respiratory chain proteins). Also, genetic errors in other fundamental mitochondrial functions that do not directly affect the respiratory chain have major deleterious effects on the nervous system, including impaired import of mitochondrial proteins and defects of mitochondrial dynamics, such as motility, fission, fusion, and distribution.
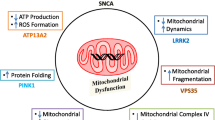
Central nervous system (CNS) involvement in mitochondrial disorders is clinically heterogeneous, manifesting as epilepsy, stroke-like episodes, migraine, ataxia, spasticity, extrapyramidal abnormalities, bulbar dysfunction, psychiatric abnormalities, neuropsychological deficits, or hypophyseal abnormalities [3]. Mutations in mtDNA, the generation and presence of ROS, and environmental factors may contribute to energy failure and lead to neurodegenerative diseases. Furthermore, mitochondrial dysfunction has been associated with the pathogenesis of neurodegeneration in age-associated diseases such as Parkinson’s, Huntington’s, and Alzheimer’s diseases [3, 4].
Taking into consideration the complexity of multifaceted mitochondria, in this chapter we will make an overview of the research being done in order to model mitochondrial dysfunction in neurodegeneration, specifically connected to mitochondrial diseases. Although many different attempts have been made to model mitochondrial diseases in various organisms, this chapter will focus on genetic manipulations in the mammalian model system – transgenic mice. We have classified different mouse models according to whether they targeted the mtDNA integrity and stability or the introduced mutation is in nucleus-encoded proteins affecting activity, levels, and stability of OXPHOS complexes (Table 13.1).
2 Modelling the Role of mtDNA Mutations and Loss of mtDNA Integrity in Neurodegeneration
Generation of animal models carrying specific mtDNA mutations has proven to be extremely challenging mainly because stable DNA transfection into mammalian mitochondria is still basically unfeasible. The introduced DNA must cross not one, but three membranes – the plasma membrane plus two mitochondrial membranes, the innermost of which is impermeable to large hydrophilic polyanions such as DNA or RNA. Even if the DNA molecule were able to access the matrix, it would need to be stably recombined into an endogenous copy of mtDNA or maintained independently. As the level of mtDNA recombination is believed to be very low in many species, including mammals, only entire mitochondrial genomes could be used as a potential vector for replication, meaning that an incoming genome needs to rapidly associate with the soluble and membrane-bound factors necessary to promote mtDNA transmission. Finally, as mtDNA is present in many copies in any one mammalian cell, it is unlikely that transfection would introduce many copies of foreign DNA inside mitochondria certifying that only a minute portion of mitochondria will carry the desired mutation. However, a minimum critical proportion of mutated mtDNA is necessary before biochemical defects and tissue dysfunction become apparent. Typically, this threshold value is in the range of 60–90 % mutant to wild-type mtDNA, resulting in a requisite of numerous transformation events to ensure introduced mtDNA reaches meaningful levels [31]. Several attempts have been made to transform mitochondria within cells using: (1) the “ProtoFection” technology that uses recombinant human mitochondrial transcription factor A (TFAM) engineered with an N-terminal protein transduction domain (PTD) followed by the mitochondrial localisation signal (MLS) to deliver mtDNA cargo to the mitochondria of living cells [7] or (2) nanocarriers, including DQAsomes [dequalinium-based liposome-like vesicles], cationic, self-assembling vesicles that target the mitochondrion [32], and MITO-Porter, which enters cells by macropinocytosis and mediates mitochondrial membrane fusion [31]. However, these approaches have been heavily criticised for the lack of a mechanism for how mtDNA crossed the three membranes or the size of mtDNA fragments that could be transported, and even more importantly, so far, no researchers outside the laboratories of the inventors have successfully reported the use of any of these systems for mitochondrial transformation inside living cells [9].
Additional attempts have been tried to introduce DNA into isolated mitochondria with a bit more success in the hands of multiple researchers. Successful import of DNA into isolated mitochondria has been reported using the protein import pathway [33, 34], electroporation [35], natural competence [36], or bacterial conjugation [37]. However, none of these methods are commonly used or generally accepted for mitochondrial transformation, not least as it raises a concern of how these mitochondria would be reintroduced into host cells [9].
These technical difficulties have given rise to different methods to manipulate the mtDNA integrity in experimental animals. To date, two different approaches have been successfully tried for introducing genetically distinct mtDNA into mouse models: (1) cybrid technology using fusion of cell cytoplasts bearing mutant mtDNA to undifferentiated mouse stem cells, followed by injection into mouse blastocysts [38], or directly to mouse single-cell embryos [6] and (2) manipulation of proteins essential for mtDNA maintenance, primarily leading to increases in spontaneous mtDNA mutations [11], rearrangements [13], and depletion of mitochondrial genome [39].
2.1 Cybrid Models of Mitochondrial Diseases: Transmitochondrial Mice
Cybrids, or “cytoplasmic hybrids”, are cultured cells manipulated to contain introduced mitochondrial DNA (mtDNA). They are produced by fusion of the whole cell with a cytoplast, which contains cytoplasm and organelles, including mitochondria, but lacks nucleus. The enucleation is achieved by simultaneous application of centrifugal force and treatment of the cell with an agent that disrupts the cytoskeleton. A number of laboratories have reported use of cybrid methodologies to create transmitochondrial mouse models [5, 6, 38, 40, 41]. Here we will mention the most important examples and specifically focus on results regarding neurological phenotypes.
2.1.1 CAPR Mice
At the turn of the last century, two groups in parallel produced the very first transmitochondrial mice carrying an m.2379A>T mutation in the highly conserved part of mitochondrial 16S rRNA gene, warranting chloramphenicol resistance (CAPR) to its host, hence the name CAPR mice [5, 40]. Although using slightly different approaches, both groups have managed to produce cybrid embryonic stem (ES) cells, mostly carrying mutant mtDNA (90–100 %) that was injected into blastocysts, and the obtained embryos are implanted into pseudopregnant females [5, 40]. Analysis of heteroplasmy in different tissues of obtained chimeric mice demonstrated that despite heavy manipulation and chloramphenicol selection, the ES cells with mtDNA m.2379A>T mutation were able to contribute to the development of different tissues, although at fairly low levels (on average, less than 10 %) [5, 40]. Remarkably, the germ-line transmission of the CAPR mutation even when present in moderate levels (44–52 %) resulted in severe growth retardation, myopathy, dilated cardiomyopathy, and perinatal or in utero lethality [38]. However, these mice did not present any neural phenotypes, besides prominent hamartomatous-like changes (a benign, focal malformation that resembles a neoplasm) of the optic nerve head [38].
2.1.2 ΔmtDNA Mice
A slightly different approach was used to create delta-mtDNA (ΔmtDNA) mice [6]. Mitochondria carrying somatic mtDNA mutation (Δmt4696) from aged mouse brain [synaptosomes] were fused to cells lacking mtDNA (ρ0 cells) to create cybrid clones expressing mtDNA with a 4696 bp deletion that included genes encoding for 6 tRNAs (K, G, R, H, S, L) and 7 polypeptides (ND3, ND4, ND4L, ND5, COXIII, ATP6, and ATP8) [6]. These cybrids were then enucleated, again fused to pronuclear-state embryos, and implanted into pseudopregnant females [6]. Although this procedure produced a low level of alive heteroplasmic animals, some founder females were identified, and with subsequent breeding, germ-line transmission of the mtDNA deletion was obtained through three generations [6]. This came as a surprise, as germ-line transmission of large mtDNA deletions rarely occurs in humans. Furthermore, although high tissue-specific differences in the amount of mutant mtDNAs are common in patients suffering from mitochondrial diseases, individual ΔmtDNA mice showed similar proportions of deleted mtDNA in all tissues that varied greatly among individuals (5–90 %) [6]. Furthermore, gene mapping of transmitted mtDNA revealed the presence of a partially duplicated mtDNA molecule consisting of one wild-type and one Δmt4696 mtDNA. The skeletal muscle, heart, and blood contained 0–17 % of the partially duplicated mtDNA, but it was not detected in other tissues [6].
There was a strong correlation between pathological phenotypes and the level of deleted mtDNA. Mice with about 30–50 % of Δmt4696 at birth were healthy, but developed mitochondrial respiratory deficiency and disease phenotypes when the load of mtDNA deletions reached 75–80 %, leading to shortening of the lifespan to about 1.5 years. On the other hand, ΔmtDNA mice carrying more than 70 % mtDNA with the deletion at birth died at around 6 months of age [40]. Most clinical phenotypes, including low body weight, lactic acidosis, systemic ischaemia, hearing loss, male infertility, and a very prominent renal failure, conveyed when the mtDNA with deletions reached the threshold of around 80 % [6, 40, 42, 43]. This came as a bit of a surprise because renal failure is not a common pathology associated with mitochondrial diseases. Nevertheless, phenotypes of ΔmtDNA mice mimic early-onset Pearson syndrome in humans that is caused by a single heteroplasmic mtDNA deletion and leads to anaemia, mitochondrial myopathy, and pancreatic and renal insufficiency [6].
Mice carrying more than 60 % of Δmt4696 already had mitochondrial respiration defects in the visual cortex and dentate gyrus, accompanied by impairment of memory at long retention delays, but not learning and temporal memory [7]. The authors associated this with reduced levels of Ca2+/calmodulin-dependent kinase II-α (CaMKIIα), a protein important for the establishment of spatial remote memory [7]. The mechanism by which moderate respiratory deficiency affects CaMKIIα is not completely clear, but it was proposed that either (1) increased lactic acidosis resulting from respiratory deficiency could deplete calcium and disturb signalling in nerve cells, which would lead to a general reduction of the CaMKIIα protein levels [44], or (2) reduction and depletion of the mitochondrial energy supply could affect the processes of translation and/or targeting of CaMKIIα mRNAs [7]. Although both of these models await experimental confirmation, it seems that the ΔmtDNA mouse could be a valuable model since it represents the only mammalian model with impairment of spatial remote memory caused by mitochondrial respiration deficiency [7]. On the other hand, ΔmtDNA mice do not faithfully recreate the most common phenotypes caused by a single large mtDNA deletion in humans, ranging from mild myopathy to devastating multisystemic syndromes such as Kearns-Sayre syndrome (KSS) [45, 46].
2.1.3 MT-COI Mice
The first transmitochondrial mouse carrying a point mutation in the mtDNA was created by introducing the missense m.6589T>C mutation in the COI gene [8]. These mice are created by fusing respiratory-deficient mouse B82 cell lines to ES cells depleted of mitochondria. As B82 cells lack thymidine kinase, unfused cells could not survive in the selection medium with hypoxanthine/aminopterin/thymidine (HAT) and therefore were effectively eliminated [8]. ES cell clones positive for the mutation were introduced in 8-cell stage embryos and subsequently transferred to a pseudopregnant female. The resulting mice were homoplasmic for the introduced mutation in all analysed tissues [8]. Further analysis was carried in the F6 mice backcrossed to a C57B6 background to show that the observed phenotype does not come from ΔmtDNA nuclear incompatibility. The analysed mice showed growth retardation and 50–70 % decrease in COX activity in the brain, heart, liver, and skeletal muscle (of the control levels) [8]. Although increased blood lactate levels were detected in these mice, there were no signs of epilepsy, as reported in patients with mt-COI missense mutation [47]. The authors did not proceed further in their analysis of these mice, and therefore we do not have reports of any additional phenotypes arising in them.
2.1.4 MT-ND6 Mice
Possibly the mouse model that most accurately copies the human pathology was created for Leber’s hereditary optic neuropathy (LHON) by introducing the human optic atrophy ND6 G14600A (P25L) mutation into the mouse [9]. LHON is the first inherited mtDNA disease reported [48] and probably the most prevalent one caused by mtDNA missense mutations, having an estimated frequency of 15 in 100,000 [49]. LHON is typically caused by mutations in one of the three mtDNA-encoded complex I (CI) genes (MT-ND1, MT-ND4, and MT-ND6) [49]. Patients with classic LHON experience loss of central vision, usually in both eyes, between 15 and 35 years of age due to preferential loss of papillomacular bundle nerve fibres [49].
Creation of MT-ND6 homoplasmic mutant mice started with mutagenesis of murine LMTK cell line, followed by enrichment of introduced mtDNA mutations by ethidium bromide depletion, reamplification, and cloning and subsequent selection of the respiratory-deficient clones using glucose- or galactose-containing media. This approach produced a clone carrying homoplasmic m.13997G>A mutation (MT-ND6 P25L substitution) with isolated CI deficiency (23 % residual activity), 65 % reduction in ATP synthesis, and increased ROS production [9]. The enucleated clones were fused with mouse ES cells, chimeric females were identified, and the maternal transmission of the homoplasmic MT-ND6 m.13997G>A mtDNA mutation was confirmed by mtDNA sequencing [9]. Remarkably, despite the systemic reduction of CI activity, like in LHON patients, the phenotype was restricted to the optic nerve. The mice mirrored some of the typical LHON patient phenotypes like: reduction in retinal function by electroretinogram (ERG), age-related decline in central smaller calibre optic nerve fibres with sparing of larger peripheral fibres, neuronal accumulation of abnormal mitochondria, axonal swelling, and demyelination decreased retinal response, preferential loss of small retinal fibres, and swollen axons of retinal ganglion cells, due to the accumulation of morphologically abnormal mitochondria [9]. Reduced CI activity and highly increased ROS levels were detected in mitochondria and synaptosomes isolated from the brain of these mice. Surprisingly, normal ATP levels were detected in synaptosomes of these mice, indicating that the primary cause of the retinal impairment was the chronic oxidative damage rather than the energetic failure [9]. As the aetiology of LHON still requires better understanding, this mouse model could be essential for better characterisation of the relationship between mtDNA and optic nerve dysfunction and could further be used to test antioxidant therapies in vivo.
Surprisingly, mice with the same m.13997G>A mutation that arose independently in C57BL Lewis lung tumour cells on a different mtDNA background had a distinctly different phenotype [50]. They showed moderate complex I defects and increased lactate levels at a young age, but no other phenotypes related to mitochondrial diseases [50]. Later in life, these MT-ND6 mice developed some age-associated phenotypes, such as development of B lymphoma and diabetes, but no neurological or ophthalmological symptoms were detected [51]. It is currently not clear where this strong discrepancy between the two models is coming from, although, at least in part, it could be ascribed to different genetic backgrounds. Further studies using both models in parallel are clearly needed to address this issue.
2.1.5 MT-TK Mice
A transmitochondrial mouse with an m.7731G>A mutation in MT-TK (mitochondrial tRNALys) gene was recently generated from a mouse lung carcinoma P29 cell line [10]. Mitochondrial transfer RNA (mt-tRNA) mutations are the most common mtDNA mutations to cause human disease, and this was the very first mouse model with a point mutation in mitochondrial tRNA gene that has a counterpart in human patients affected by mitochondrial disease. The mice were created by fusing ES cells depleted of mitochondria with the cybrid clone having 70 % heteroplasmy for MT-TK m.7731G>A [10]. The mutation was transmitted through subsequent generations, if present in ≤85 % heteroplasmy, while oocytes containing a higher mutational load seem to be lost during development [10]. Mice with predominant m.7731G>A heteroplasmy displayed some features of mitochondrial diseases, such as short body length and muscle weakness, but not ragged red fibres (RRFs). However, MT-TK m.7731G>A did not reproduce the severe phenotype of patients with matching human MT-TK mutation (m.8344G>A) associated with MERRF (myoclonic epilepsy with ragged red fibres) possibly because of the lower heteroplasmy level transmitted to the progeny. At this point, a possibility for a late onset of the disease in mice cannot be excluded. One striking difference between MT-TK m.7731G>A and human patients with matching mutation(s) is the loss of oocytes with high mutational load in mice [10]. This aspect underlines once more the difficulties in creating mouse models resembling human defects and, probably, species-specific differences in mtDNA selection during germ-line transmission and segregation in tissues. Nevertheless, we believe that this mouse model will be useful for studying specific aspects of human mitochondrial myopathies and possibly testing therapeutic compounds.
2.2 Manipulating Proteins Essential for mtDNA Maintenance
Besides the direct manipulation of mtDNA, manipulation of proteins involved in mitochondrial genome maintenance, primarily mtDNA replication, has been used in order to create animal models for mitochondrial diseases. Replication of the mitochondrial genome requires unique enzymatic machinery, composed of a set of factors encoded by nuclear DNA and recruited to mitochondria. In vitro studies showed that the basic replication fork of human mitochondria can be reconstituted using primed single-stranded DNA substrate and at least five mtDNA maintenance factors: catalytic and accessory subunit of DNA polymerase gamma (POLG and POLG2), mitochondrial RNA polymerase (POLRMT), replicative DNA helicase (TWINKLE), and the mitochondrial single-stranded DNA binding protein (MTSSB) [52]. Although this simple mitochondrial replisome is sufficient to duplicate a DNA substrate in vitro, proper maintenance and effective replication of the mitochondrial genome involve a much longer and still growing list of factors.
2.2.1 MtDNA Mutator Mouse
Development of mtDNA mutator mice allowed detailed analysis and understanding of the role of random somatic mtDNA mutations in the development of mitochondrial pathologies [11]. MtDNA mutator mice are created by introducing a single point mutation in the highly conserved exonuclease domain of POLG, resulting in almost complete inactivation of proofreading exonuclease activity in these mice [11]. As the proofreading was abolished, mtDNA mutator mice accumulated three to five times more random mtDNA mutations and developed a range of phenotypes reminiscent of naturally occurring ageing and had a very significantly shortened lifespan [11]. The high number of mtDNA point mutations in mtDNA mutator mice leads to the synthesis of respiratory chain (RC) subunits with many amino acid substitutions that likely cause instability of the RC complexes [53]. Although initial studies indicated that neuronal phenotypes are not predominant in mtDNA mutator mice [11], some studies have specifically addressed changes in the central nervous system (CNS) of these mice [54]. Initially it was reported that mitochondrial dysfunction in the mtDNA mutator mouse brain leads to a metabolic shift from aerobic respiration to glycolytic metabolism [54]. Using proton magnetic resonance spectroscopy, increased brain lactate levels have been detected in these mice, and this was assigned to mitochondrial dysfunction in neurons that, instead of metabolising pyruvate through the tricarboxylic acid (TCA) cycle, supposedly rely on glycolysis and anaerobic metabolism [54]. However, a later study on the CNS phenotypes failed to confirm general mitochondrial dysfunction in mtDNA mutator brains and instead described embryonic-onset dysfunction of somatic stem cells (SCs), including neural progenitors [55]. It has been demonstrated that development of neural and haematopoietic progenitor cells of the mtDNA mutator mice is already affected during foetal development and that neural stem cells showed decreased abundance in vivo as well as reduced self-renewal capacity in vitro [55]. Moreover, the observation that treatment with the antioxidant N-acetylcysteine restores the self-renewal ability of neural progenitor cells has led to the conclusion that an aberrant change in ROS signalling or redox status is sufficient to modify signalling in somatic stem cells and severely disrupt their homeostasis [55]. Recently, another study on mtDNA mutator mice has shown that a combination of inherited and somatic mtDNA mutations causes stochastic brain malformation, which suggests that starting life with healthy mitochondria might be crucial for maintaining brain health during the course of ageing [12]. This study further showed that the initial report on the more general mitochondrial dysfunction in the mtDNA mutator brain is likely a result of the increased, inherited mtDNA mutation load, rather than lifelong somatic mtDNA mutation accumulation. It seems that in mice, unlike humans, spontaneous somatic mtDNA mutations are less likely to cause pathological phenotypes in the brain than other tissues, like the heart, spleen, or skeletal muscle.
Although mtDNA mutator mice were extremely valuable to model and understand the general role of random somatic mtDNA mutations, they cannot be used to model numerous diseases caused by POLG mutations. Mutations in POLG have been associated with a number of mitochondrial disorders that affect the stability of mtDNA, primarily leading to mtDNA deletion and depletion syndromes [56, 57]. The most common disease caused by POLG mutations is the autosomal dominant (ad) or autosomal recessive (ar) form of familial progressive external ophthalmoplegia (PEO) [57–59]. Additional clinical presentations like autosomal recessive sensory ataxic neuropathy with dysarthria and ophthalmoplegia (SANDO) and Alpers’ hepatophatic poliodystrophy have also been associated with POLG mutations [60–62]. Furthermore, dominant POLGA mutations have shown to cause a severe multisystemic disorder including Parkinsonism and premature menopause, which are not typical of mitochondrial disease [63]. To accurately model these diseases, novel mice that carry specific POLG patient mutations should be developed.
2.2.2 Deletor Mouse
TWINKLE is a hexameric helicase that together with POLG and MTSSB forms the minimal mtDNA replisome in vitro [52]. Dominant mutations in TWINKLE are associated with PEO [64]. A decade ago, two transgenic mice models overexpressing either in-frame duplication [352–364] or amino acid substitution (A359T) found in human patients were developed [13]. The in-frame duplication is structurally the most severe mutation so far described in TWINKLE patients, and correspondingly Twinkledup mice showed more severe phenotypes than TwinkleA359T [13]. They are named “deletor mice” as their main feature is the age-dependent accumulation of multiple large mtDNA deletions, along with the respiratory chain dysfunction. A predominant phenotype in deletor mice is mitochondrial myopathy, and the muscles of the mice faithfully replicate all of the key histological, genetic, and biochemical features of PEO patients [13]. Brain respiratory deficiency followed the muscle phenotypes, and COX-deficient (COX-) neurons are primarily found to be Purkinje cells and large pyramidal neurons in the hippocampal CA2 region. A few COX- neurons were also identified from the olfactory bulbs, substantia nigra, and hypothalamus [13]. In contrast to mtDNA mutator mice, deletor mice did not show signs of premature ageing, although they showed progressive respiratory chain deficiency due to the accumulated mtDNA deletions. These mice represent a very good model for the late-onset progressive mitochondrial disease, without affecting the lifespan [13]. More recently, a mouse model expressing mutated TWINKLE (352–364 duplication) specifically in dopaminergic neurons of substantia nigra was created [14]. These mice feature late-onset mild respiratory dysfunction accompanied with increased mtDNA deletions and reduction in parkin levels with alterations in autophagy, which together causes dopaminergic neuron degeneration and movement defects [14]. Although interesting and with results in agreement with previous deletor mice, this specific model conceptually adds novelty in modelling mitochondrial involvement in certain brain regions.
2.2.3 MILON and MitoPark Mice
One of the very first mouse models mimicking mitochondrial dysfunction found in patients was the TFAM (mitochondrial transcription factor A)-deficient mouse [39]. Tfam encodes a protein with dual function that is on one side important for packaging of mtDNA and on the other is an important transcriptional activator necessary for mitochondrial replication and transcription. TFAM is an essential mitochondrial protein whose constitutive depletion leads to embryonic lethality between E8.5 and E10.5 [39]. Tissue-specific depletion of Tfam in forebrain neurons and hippocampus using Cre recombinase under CaMKIIα promoter (CaMKIIα-Cre) leads to creation of the so-called MILON (mitochondrial late-onset neurodegeneration) mouse that showed reduced mtDNA levels already at 2 months and severe respiratory chain deficiency in neurons from 4 months of age [15]. Strong respiratory deficiency led to progressive neurodegeneration and massive apoptosis followed by evident gliosis in the cortex and hippocampus, starting around 5 months of age [15]. MitoPark mouse was another conditional Tfam knockout mouse created using Cre recombinase under the dopamine transporter promoter (DAT-Cre) that depleted TFAM in dopaminergic neurons of substantia nigra [16]. MtDNA expression was dramatically reduced at 6 weeks of age, although phenotypic manifestations of Parkinsonism (Parkinson’s disease [PD]-like phenotypes) started to develop much later. MitoPark mice showed significantly decreased locomotion and rearing behaviour at 14 weeks of age, and from 20 weeks of age, the mice started to display apparent disease manifestations such as tremor, twitching, and abnormal gait [16]. This slowly progressive impairment of motor function was accompanied by formation of intraneuronal inclusions and dopamine nerve cell death, and like in PD patients, these mice responded to l-DOPA therapy with a differential success depending on disease stage [16]. Therefore, the MitoPark mouse model was the first to recapitulate many of the cardinal clinical features of PD, namely, progressive neurodegeneration and death of neurons, loss of motor function, and therapeutic response to l-DOPA, and is extensively being used in PD research [65–67].
2.2.4 Tk2-Deficient Mice
The correct maintenance of mtDNA depends not only on the normal activity of the enzymes involved in replication, but also on a balanced pool of dNTPs. The first step for the salvage pathway synthesis of dNTPs, on which postmitotic tissues primarily rely to maintain their dNTP pools, is provided by the constitutively expressed mitochondrial thymidine kinase (TK2) [68]. Mutations in the TK2 gene primarily cause mitochondrial DNA depletion syndrome (MDS) with a broad clinical spectrum ranging from severe fatal infantile myopathy with motor regression, spinal muscular atrophy, and rigid spine syndrome to mild mitochondrial myopathy [69, 70]. To model the MDS, two different TK2-deficient mice were developed in parallel: one was created by deleting exons 4 and 5 (Tk2–/–) [17] and the other by introducing the H126N mutation (Tk2 H126N) [18] corresponding to the human pathogenic H121N mutation that drastically reduces TK2 activity [69]. Despite the genetic difference and the presence of some residual TK2 activity in the Tk2 H126N animals, these two mouse models shared phenotypes of severe isolated encephalopathy with a growth defect, but no major skeletal muscle alterations [17, 18]. Progressive mtDNA depletion was associated with depletion of dNTP pools and a severe mitochondrial defect, characterised by loss of mtDNA-encoded OXPHOS subunits, CI and CIV deficiency, and ATP reduction [17, 18]. As the brain was the most affected tissue, these mice displayed primarily neurological phenotypes like ataxic gait, coarse tremors, impaired motor coordination, abnormal limb clasping, and generalised weakness [17, 18]. This also represents the main difference in comparison to patients that also have a strong myopathic phenotype that was lacking in mice or is possibly masked by a severity of neurological phenotype [17, 18, 69, 70]. However, these mice still represent a very valuable tool to study MDS, but once again show that even mutations homologous to that found in human patients do not necessarily lead to development of the same pathologies.
2.2.5 Tymp-Deficient Mice
Thymidine phosphorylase (TP), a protein encoded by the TYMP gene, is also an enzyme involved in the pyrimidine salvage pathway, required for the reversible reaction catalysing thymidine and phosphate to thymine and deoxyribose-1-phosphate [19]. Mutations in TYMP cause mitochondrial neurogastrointestinal encephalopathy (MNGIE), an autosomal recessive syndromic disease clinically defined by the occurrence of gastrointestinal dysmotility with intestinal pseudo-obstruction, peripheral neuropathy, ptosis, ophthalmoparesis, and hearing loss [19]. Loss of TP catalytic activity causes an accumulation of thymidine and nucleosides in the blood and tissues of affected patients leading to multiple deletions and depletion of mtDNA [71].
To model MNGIE in mice, both TYMP and UPP1 gene, encoding uridine phosphorylase (UP), had to be knocked down, as in mice, unlike humans, UP can compensate for the loss of TP [21]. Initial study described leucoencephalopathy with enlarged myelinated fibres in Tymp–/–/Upp1–/– mice, but no mtDNA abnormalities, leading them to conclude: “encephalopathy in MNGIE patients does not appear to be caused by mtDNA alterations” [21]. However, a consequent study questions these results and conclusion, as they showed that elevated thymidine and uridine levels lead to mtDNA depletion, respiratory chain defects, and histological alterations in the brain of Tymp–/–/Upp1–/– mice [20]. However, these mice only partially resembled MNGIE patients, since they presented mtDNA depletion and pathophysiological changes only in the brain, despite ubiquitous TP deficiency [20]. A few possible explanations have been put forward for this discrepancy including: (1) the shorter lifespan of mice may not be sufficient to allow significant accumulation of somatic mtDNA alterations and consequent respiratory dysfunction in most tissues, (2) mitochondrial dNTP pool imbalances in MNGIE patients are more dramatic than in Tymp–/–/Upp1–/– mice and therefore could cause mtDNA instability in more tissues, and (3) differential expression and activities of other enzymes involved in the pyrimidine metabolism are likely to influence in the balance of the mitochondrial dNTP pools and contribute to the tissue-specific effects in mice and humans [20]. Despite these differences, this knockout mouse represents an important model to further investigate the pathophysiology of leucoencephalopathy in mitochondrial diseases and is a useful tool to develop therapeutic strategies for MNGIE.
3 Manipulating nDNA-Encoded Proteins Involved in Mitochondrial Diseases and Neurodegeneration
The OXPHOS complexes are composed of subunits encoded by both nDNA and mtDNA with the exception of complex II, which is exclusively encoded by nDNA. For fully and correctly assembled OXPHOS complexes, exact coordination of the expression of nuclear and mitochondrial proteins is needed. Defects in OXPHOS result in varied pathologies and metabolic diseases, mostly affecting the organs with high-energy demands, such as the heart, skeletal muscle, and brain. Many attempts to create mouse models for OXPHOS deficiencies have failed because of the essential nature of targeted genes for mitochondrial function, leading to embryonic lethality in generated models [72]. However, in recent years, a number of viable mouse models related to the components of OXPHOS proteins encoded by the nuclear genome were constructed in order to study pathogenic mechanisms underlying these diseases.
3.1 Complex I-Deficient Models
Mammalian complex I (CI) or NADH-ubiquinone oxidoreductase is the largest enzyme of the OXPHOS and consists of at least 38 subunits encoded by nDNA and 6 subunits encoded by mtDNA [73]. Isolated complex I deficiency is the most frequently diagnosed mitochondrial defect accounting for almost 23 % of all cases of childhood respiratory chain deficiency [74]. The most common phenotypes associated with isolated complex I deficiency are the Leigh syndrome (LS) and Leigh-like disease which mainly cause psychomotor retardation, brainstem dysfunction, seizures, failure to thrive, muscular hypotonia, dystonia, abnormal eye movements, and lactic acidosis [75].
3.1.1 Ndufs4-Deficient Mice
NDUFS4 (NADH-ubiquinone oxidoreductase iron-sulphur protein 4) is an 18 kDa protein, inserted at a late stage of CI biogenesis, essential for CI assembly and stability. Ndufs4 gene is a mutational hot spot in humans leading to development of LS and Leigh-like encephalomyopathy phenotype [76]. The first NDUFS4-deficient mouse model was a whole-body knockout (Ndufs4–/–) that rapidly developed a Leigh-like phenotype characterised by ataxia, blindness, retarded growth rate, lethargy, and increased serum lactate, leading to premature death at about 7 weeks of age [22]. These mice developed isolated CI deficiency with a very specific tissue distribution, with liver and CNS being the most affected tissues, whereas CI activity in the skeletal muscle of Ndufs4–/– mice was reduced to about 50 % of control levels [22]. It is also quite interesting that these mice lived for about 5 weeks without signs of illness after which they rapidly developed a fatal phenotype. Although it was assumed that NDUFS4 subunit plays an essential role in assembly and stability of the CI, the results from Ndufs4–/– mice demonstrated that CI could be formed without it, most probably because of the compensatory activity of other subunits in a tissue-specific manner [22]. Remarkably, mice deficient in NDUFS4, exclusively in neurons and glia (using Nestin-Cre), copied the phenotype of full-body knockouts [23]. These mice (Ndufs4 L/L; Nestin-Cre) had clear signs of progressive glial activation that promotes neuronal death and ultimately results in mortality. Neurons in the olfactory bulbs (OBs), vestibular nuclei (VN), and posterior lobules of the cerebellar vermis appear to be the most vulnerable [23]. The basic neuropathology featuring mitochondrial disorders consists of nonspecific histological lesions, neuronal loss, necrosis, gliosis, demyelination, and spongiform degeneration [77] that were all apparent when studying the brains of these mice. Therefore, both of these mouse models (Ndufs4–/– and Ndufs4 L/L; Nestin-Cre) are going to be essential for understanding the progression of symptoms in LS and looking for potential therapeutic interventions [22, 23].
Interestingly, disruption of NDUFS4 in midbrain dopaminergic neurons (Ndufs4 L/L; DAT-Cre) did not lead to overt neurodegeneration, loss of striatal innervation, or symptoms of Parkinsonism [24]. However, dopamine (DA) homeostasis was abnormal with impaired DA release and increased levels of DA metabolites allowing the authors to conclude that complex I deficiency still can contribute to the pathophysiology of PD [24].
Another two Ndufs4-deficient mouse models were created that did not completely recapitulate observed phenotypes [78, 79]. Firstly, an Ndufs4 knockout model was created by spontaneous transposable element insertion within the gene that produced a premature stop codon and resulted in an unstable transcript [78]. These Ndufs4 knockout mice were smaller at birth, lost their fur at 2 weeks of age, displayed some neurological impairment at 5 weeks, and died prematurely at about 7 weeks. However, the authors did not observe significant neuropathological changes in the brain of these mice, in contrast to previous reports [22, 23]. This has been explained by an earlier time point used to analyse these mice, due to ethical permit restrains [78]. In the future, comparative analysis of all three models will be needed to shed more light on the observed phenotypic differences.
A second model was created as a knock-in model, by introducing a premature stop codon in the Ndufs4 gene [79]. Unexpectedly, homozygous knock-in mice were embryonic lethal, while heterozygous mice showed a mild phenotype, with a reduction of CI activity of about 30 % in the heart, brain, and skeletal muscle mitochondria, accompanied by elevated lactate levels in the brain and heart [79]. It seems that the introduced mutation could have a dominant-negative effect as it creates a stop codon that results in the expression of a truncated NDUFS4 protein of about 14.4 kDa lacking the last 10–15 amino acids. The truncated protein seems to be incorporated at low levels into the fully assembled CI resulting in significant complex deficiency and might explain the differences with other Ndufs4 knockout models [79].
3.1.2 Ndufa5-Deficient Mice
Initial attempts to create mice deficient for NADH-ubiquinone oxidoreductase 1 alpha subcomplex subunit 5 (NDUFA5) were done using a gene-trap technology, but without success, as it turned out that Ndufa5 was an essential mitochondrial protein necessary for embryonic survival [25]. This might be also the reason why there are no human patients with mutations in NDUFA5 gene. To study the role of NDUFA5 in adult mice, a conditionally targeted Ndufa5 gene was created and deleted specifically in forebrain neurons and hippocampus using CaMKIIα-Cre [25]. These mice were healthy until the age of 10–11 months when they became lethargic and showed significantly reduced motor coordination compared to the controls of the same age. Although levels of the fully assembled CI (75–80 %) and CI activity (40 %) were markedly reduced in the cortex, neither oxidative stress, neuronal loss, nor gliosis was observed in the knockout mice [25]. The mild phenotype of Ndufa5 knockout mouse could be the result of the compensatory mechanisms such as physiological adjustment to ketogenic environment, since the brain actively metabolises ketone bodies in periods of energy shortage [80]. This was suggested after noting the increased levels of ketogenic enzyme ACAT1 [mitochondrial acetyl-CoA acetyltransferase] in the knockout brains [25]. Another compensatory effect could be the increased electron flow via the electron transfer flavoprotein dehydrogenase to CoQ10, since there was an upregulation of electron-transferring-flavoprotein subunit A (ETFA) in knockout brains [25].
3.2 Coenzyme Q Deficiency
Coenzyme Q10 (CoQ10) is a mobile lipophilic electron carrier located in the inner mitochondrial membrane that transfers electrons from CI to CII and to complex III [81]. Besides its role in the OXPHOS system, CoQ10 is a potent antioxidant molecule and participates in the de novo pyrimidine biosynthesis pathway [81]. CoQ10 endogenous biosynthesis occurs ubiquitously in the mitochondria, and several pathogenic mutations in genes encoding proteins involved in this process have been identified [82, 83]. Mutations in CoQ biosynthetic genes produce primary CoQ10 deficiency, a mitochondrial syndrome associated with five major clinical phenotypes: encephalomyopathy, severe infantile multisystemic disease, nephropathy, cerebellar ataxia, and isolated myopathy [83].
3.2.1 Coq9-Deficient Mice
COQ9 gene encodes 1 of the 11 proteins required for the biosynthesis of CoQ10 within mitochondria and is the disease-causing gene reported in a patient with primary CoQ10 deficiency [84]. The patient with a COQ9 homozygous stop mutation developed neonatal lactic acidosis followed by multisystemic disease including intractable seizures, global developmental delay, hypertrophic cardiomyopathy, and renal tubular dysfunction [84]. To better understand the pathophysiological consequences of primary CoQ10 deficiency, a mouse model carrying a homozygous mutation in Coq9 gene (R239X, Coq9 R239X), which is homologous to the human R244X mutation, was created [84]. The homozygous Coq9 R239X mice were normal at birth, but between 3 and 6 months, they developed a rapid and progressive paralysis followed by death, suggesting an involvement of the central nervous system in the pathogenic mechanism of the disease [26]. Further analysis of Coq9 R239X mice showed intense vacuolisation, astrogliosis, and neuronal death in the brain and severe demyelination of peripheral tissues. The lack of CoQ10 caused a loss of CI and an increase in free CIII, leading to a decrease in mitochondrial respiration and ATP synthesis only in the brain of the Coq9 R239X mice [26]. However, before accepting Coq9 R239X mouse as an excellent model of mitochondrial encephalomyopathy associated with CoQ10 deficiency, it has to be determined if the observed phenotypes are independent from other metabolic pathways fundamental for proper brain development in foetuses and newborns, like cholesterol metabolism, which shares the biosynthetic pathway of CoQ10.
3.3 Complex III-Deficient Models
Complex III (CIII, ubiquinol-cytochrome c reductase, or cytochrome bc1 complex) consists of three catalytic and eight structural subunits, yet deficiencies in this complex are very rare, but with a broad range of clinical features and tissue specificity [85]. Although a few mouse models have been created that have deficiency in CIII subunits, only Uqcrfs1-deficient mice were analysed for CNS phenotypes.
3.3.1 Uqcrfs1-Deficient Mice
Rieske iron-sulphur protein (RISP) is one of the catalytic subunits of CIII encoded by nuclear DNA, more specifically, the UQCRFS1 gene. Similar to the previously described Ndufa5 gene, Uqcrfs1 is essential for mouse embryonic development, providing explanation as to why no human patients are described so far. To study the role of RISP in an adult mammalian brain, a conditional strategy was used to create forebrain neurons and hippocampus-specific Uqcrfs1 knockout mice (Uqcrfs1 L/L; CaMKIIα-Cre) [27]. These mice lived up to 3 months, with CIII deficiency becoming apparent in both cortex and hippocampus already at 1 month of age and progressing rapidly until the end of their lifespan [27]. CIII deficiency was accompanied with an increase in citrate synthase and CIV activities and higher mtDNA/nDNA ratios, all of which indicate increased mitochondrial biogenesis as a compensatory response to respiratory deficiency [27]. Uqcrfs1 knockout mice also showed extensive oxidative damage followed by neuronal death, mainly in the piriform cortex and hippocampus at 3 months of age and therefore could be a great model for testing antioxidants as therapeutic agents in mitochondrial diseases [27].
3.4 Complex IV-Deficient Models
Cytochrome c oxidase (COX) or complex IV (CIV) is the terminal enzyme of the electron transport chain in mitochondria that receives electrons from cytochrome c molecules and transfers them to molecular oxygen, thus converting it to two molecules of water. CIV is a very significant factor in the aetiology, progression, and prevalence of numerous human neurodegenerative diseases and represents an important target for developing diagnostic and therapeutic tools against those diseases [86]. COX deficiency may cause clinically heterogeneous disorders ranging from isolated myopathy to severe multisystemic disease [87]. Mutations in genes encoding both the CIV structural subunits (COI and COII) and assembly factors (SURF1, SCO2) have been implicated in human diseases.
3.4.1 SURF1-Deficient Mice
Remarkably, mutations in the COX assembly genes are a major cause of isolated COX deficiency and LS [87]. It has been estimated that about one-third of all LS cases are caused by SURF1 mutations [88]. Therefore, it came as a great surprise that mice lacking SURF1 (Surf1–/–) did not show any signs of neurodegeneration [28]. In fact, these mice showed protection from Ca2+-dependent neurotoxicity caused by kainic acid and had significantly increased median lifespan [28]. The biochemical and assembly COX defect was present in Surf1–/–mice, but much milder than in human patients, suggesting alternative CIV assembly factors are present in mouse mitochondria [28]. Therefore, despite the fact that SURF1 is evolutionarily conserved, its function in COX assembly in mice seems to be redundant and therefore could be partly taken over by other unknown factors. One possible explanation is that mild mitochondrial dysfunction in Surf1–/– mice could lead to activation of compensatory genetic and epigenetic mechanisms that in turn can lead to increased longevity through hormetic responses. Indeed, the results of a most recent study suggested that impaired mitochondrial function as observed in Surf1–/– mice can lead to induction of mitochondrial stress pathways like mitochondrial biogenesis and mitochondrial unfolded protein response, to confer protective effects on cellular homoeostasis [89]. It was also reported that loss of SURF1 leads to key metabolic changes resulting in reduced adiposity, improved insulin sensitivity, and induction of mitochondrial biogenesis in white adipose tissue [90]. These novel findings may also contribute to the prolonged lifespan of Surf1–/– mice and suggest that although these mice are not a good model for human LS pathologies, they might be invaluable to study other aspects of mitochondrial function, like mitohormesis and the role of mitochondrial dysfunction in mammalian ageing.
3.4.2 Cox10-Deficient Mice
COX10 is a farnesyltransferase, necessary for the assembly of CIV. In humans, mutations in COX10 have been associated with leucodystrophy, hypotonia, lactic acidaemia, deafness, etc. [91]. To gain better understanding of the role of COX10 in the mammalian CNS, two different conditional Cox10 knockout mice were generated: one with a primary deficiency in neurons [27] and the other in oligodendrocytes and Schwann cells [29]. The neuron-specific Cox10 knockout (Cox10 L/L; CaMKIIα-Cre) represents an encephalopathy mouse model with pronounced behavioural abnormalities [27]. Although COX-deficient neurons were detected at 2 months of age in the cortex and hippocampus, the neurodegenerative phenotype was slowly progressing until the age of 8 and 12 months when the mice die [27]. This was accompanied with a delayed onset of oxidative stress and gliosis [27]. The myelin-producing cell-specific ablation of COX10 (Cox10 L/L; Cnp1-Cre) showed a severe neuropathy phenotype with dysmyelination, muscle paralysis, and atrophy in the peripheral nervous system. On the contrary, in the adult CNS, no signs of demyelination nor axonal degradation were found, suggesting that postmyelination oligodendrocytes survive well in the absence of COX activity, relying on glycolytic metabolism [29]. Moreover, brain lactate was increased in Cox10 L/L /PLPErt2-Cre mice, which can be effectively used by myelinated axons when energy deprived. This model indicates that an increased rate of oligodendroglial glycolysis can supply aerobic glycolysis products to support axonal energy needs suggesting a model in which axon-glia metabolic coupling serves a physiological function [29].
3.4.3 Ethe1-Deficient Mice
ETHE1 gene encodes a b-lactamase-like, iron-coordinating metalloprotein that is mutated in ethylmalonic encephalopathy, a devastating infantile metabolic disorder affecting the brain, gastrointestinal tract, and peripheral vessels connected with COX deficiency [92]. In the mouse model deficient in ETHE1 (Ethe1–/–), sulphur dioxygenase activity was absent, disabling sulphide detoxification in mitochondria. Sulphide is a powerful inhibitor of COX and short-chain fatty acid oxidation, with vasoactive and vasotoxic effects that explain the microangiopathy in ethylmalonic encephalopathy patients [30]. This mouse model of ethylmalonic encephalopathy is the first example of an inherited mitochondrial disease resulting from toxic inhibition of aerobic energy metabolism [30]. The toxic mechanism underpinning ethylmalonic encephalopathy makes effective therapy a realistic goal. Even though this mouse model isn’t mimicking the direct deficiency in OXPHOS, it shows how deficiency in other genes can affect particular parts of OXPHOS, and that is why it represents a valuable model [30].
4 Conclusion
Despite the great advance being made in constructing mouse models with OXPHOS defects, we still have a gap in knowledge in explaining tissue specificity and the difference in severity of the phenotypes obtained from these models. Another problem that we are dealing with is the difference between human patients’ clinical phenotypes and what we observe in our mouse models, with the same deficiency. The latter complicates finding suitable therapeutic approaches.
The aim of this review was to summarise the mouse models displaying the neurodegenerative phenotype and compare it with the known human patients’ diseases. Mitochondrial diseases are extraordinarily diverse, not only in their phenotypic presentation but also in their genetic background. The multifaceted nature of mitochondria is shown in versatile causes of neurodegenerative disease. From disruptions in mtDNA expression, over energy production problems, to defected mitochondrial dynamics and quality control, we can clearly see how every aspect of mitochondrial well-being is important for health maintenance. On the other hand, the mechanisms of many diseases have yet to be elucidated in order to get closer to effective therapeutic approaches. More mouse models depicting human neurodegenerative diseases need to be constructed. Moreover, the inability to genetically transform mammalian mitochondria is a serious impediment to research on mitochondrial disorders and limits gene therapeutic approaches to mtDNA diseases.
References
Wallace DC. Diseases of the mitochondrial DNA. Annu Rev Biochem. 1992;61:1175–212.
Howard MA, Volkov IO, Noh MD, Granner MA, Mirsky R, Garell PC. Chronic microelectrode investigations of normal human brain physiology using a hybrid depth electrode. Stereotact Funct Neurosurg. 1997;68(1–4 Pt 1):236–42.
DiMauro S, Schon EA. Mitochondrial disorders in the nervous system. Annu Rev Neurosci. 2008;31:91–123.
Wallace DC. Mitochondrial genetics: a paradigm for aging and degenerative diseases? Science. 1992;256:628–32.
Marchington DR, Barlow D, Poulton J. Transmitochondrial mice carrying resistance to chloramphenicol on mitochondrial DNA: developing the first mouse model of mitochondrial DNA disease. Nat Med. 1999;5(8):957–60.
Inoue K, Nakada K, Ogura A, Isobe K, Goto Y, Nonaka I, et al. Generation of mice with mitochondrial dysfunction by introducing mouse mtDNA carrying a deletion into zygotes. Nat Genet. 2000;26(2):176–81.
Tanaka D, Nakada K, Takao K, Ogasawara E, Kasahara A, Sato A, et al. Normal mitochondrial respiratory function is essential for spatial remote memory in mice. Mol Brain. 2008;1:21.
Kasahara A, Ishikawa K, Yamaoka M, Ito M, Watanabe N, Akimoto M, et al. Generation of trans-mitochondrial mice carrying homoplasmic mtDNAs with a missense mutation in a structural gene using ES cells. Hum Mol Genet. 2006;15(6):871–81.
Lin CS, Sharpley MS, Fan W, Waymire KG, Sadun AA, Carelli V, et al. Mouse mtDNA mutant model of Leber hereditary optic neuropathy. Proc Natl Acad Sci U S A. 2012;109(49):20065–70.
Shimizu A, Mito T, Hayashi C, Ogasawara E, Koba R, Negishi I, et al. Transmitochondrial mice as models for primary prevention of diseases caused by mutation in the tRNA(Lys) gene. Proc Natl Acad Sci U S A. 2014;111(8):3104–9.
Trifunovic A, Wredenberg A, Falkenberg M, Spelbrink JN, Rovio AT, Bruder CE, et al. Premature ageing in mice expressing defective mitochondrial DNA polymerase. Nature. 2004;429:417–23.
Ross JM, Coppotelli G, Hoffer BJ, Olson L. Maternally transmitted mitochondrial DNA mutations can reduce lifespan. Sci Rep. 2014;4:6569.
Tyynismaa H, Mjosund KP, Wanrooij S, Lappalainen I, Ylikallio E, Jalanko A, et al. Mutant mitochondrial helicase Twinkle causes multiple mtDNA deletions and a late-onset mitochondrial disease in mice. Proc Natl Acad Sci U S A. 2005;102(49):17687–92.
Song L, Shan Y, Lloyd KC, Cortopassi GA. Mutant Twinkle increases dopaminergic neurodegeneration, mtDNA deletions and modulates Parkin expression. Hum Mol Genet. 2012;21(23):5147–58.
Sorensen L, Ekstrand M, Silva JP, Lindqvist E, Xu B, Rustin P, et al. Late-onset corticohippocampal neurodepletion attributable to catastrophic failure of oxidative phosphorylation in MILON mice. J Neurosci. 2001;21(20):8082–90.
Ekstrand MI, Terzioglu M, Galter D, Zhu S, Hofstetter C, Lindqvist E, et al. Progressive parkinsonism in mice with respiratory-chain-deficient dopamine neurons. Proc Natl Acad Sci U S A. 2007;104(4):1325–30.
Zhou X, Solaroli N, Bjerke M, Stewart JB, Rozell B, Johansson M, et al. Progressive loss of mitochondrial DNA in thymidine kinase 2-deficient mice. Hum Mol Genet. 2008;17(15):2329–35.
Akman HO, Dorado B, Lopez LC, Garcia-Cazorla A, Vila MR, Tanabe LM, et al. Thymidine kinase 2 (H126N) knockin mice show the essential role of balanced deoxynucleotide pools for mitochondrial DNA maintenance. Hum Mol Genet. 2008;17(16):2433–40.
Nishino I, Spinazzola A, Hirano M. Thymidine phosphorylase gene mutations in MNGIE, a human mitochondrial disorder. Science. 1999;283(5402):689–92.
Lopez LC, Akman HO, Garcia-Cazorla A, Dorado B, Marti R, Nishino I, et al. Unbalanced deoxynucleotide pools cause mitochondrial DNA instability in thymidine phosphorylase-deficient mice. Hum Mol Genet. 2009;18(4):714–22.
Haraguchi M, Tsujimoto H, Fukushima M, Higuchi I, Kuribayashi H, Utsumi H, et al. Targeted deletion of both thymidine phosphorylase and uridine phosphorylase and consequent disorders in mice. Mol Cell Biol. 2002;22(14):5212–21.
Kruse SE, Watt WC, Marcinek DJ, Kapur RP, Schenkman KA, Palmiter RD. Mice with mitochondrial complex I deficiency develop a fatal encephalomyopathy. Cell Metab. 2008;7(4):312–20.
Quintana A, Kruse SE, Kapur RP, Sanz E, Palmiter RD. Complex I deficiency due to loss of Ndufs4 in the brain results in progressive encephalopathy resembling Leigh syndrome. Proc Natl Acad Sci U S A. 2010;107(24):10996–1001.
Sterky FH, Hoffman AF, Milenkovic D, Bao B, Paganelli A, Edgar D, et al. Altered dopamine metabolism and increased vulnerability to MPTP in mice with partial deficiency of mitochondrial complex I in dopamine neurons. Hum Mol Genet. 2012;21(5):1078–89.
Peralta S, Torraco A, Wenz T, Garcia S, Diaz F, Moraes CT. Partial complex I deficiency due to the CNS conditional ablation of Ndufa5 results in a mild chronic encephalopathy but no increase in oxidative damage. Hum Mol Genet. 2014;23(6):1399–412.
Garcia-Corzo L, Luna-Sanchez M, Doerrier C, Garcia JA, Guaras A, Acin-Perez R, et al. Dysfunctional Coq9 protein causes predominant encephalomyopathy associated with CoQ deficiency. Hum Mol Genet. 2013;22(6):1233–48.
Diaz F, Garcia S, Padgett KR, Moraes CT. A defect in the mitochondrial complex III, but not complex IV, triggers early ROS-dependent damage in defined brain regions. Hum Mol Genet. 2012;21(23):5066–77.
Dell’agnello C, Leo S, Agostino A, Szabadkai G, Tiveron C, Zulian A, et al. Increased longevity and refractoriness to Ca(2+)-dependent neurodegeneration in Surf1 knockout mice. Hum Mol Genet. 2007;16(4):431–44.
Funfschilling U, Supplie LM, Mahad D, Boretius S, Saab AS, Edgar J, et al. Glycolytic oligodendrocytes maintain myelin and long-term axonal integrity. Nature. 2012;485(7399):517–21.
Tiranti V, Viscomi C, Hildebrandt T, Di Meo I, Mineri R, Tiveron C, et al. Loss of ETHE1, a mitochondrial dioxygenase, causes fatal sulfide toxicity in ethylmalonic encephalopathy. Nat Med. 2009;15(2):200–5.
Tuppen HA, Blakely EL, Turnbull DM, Taylor RW. Mitochondrial DNA mutations and human disease. Biochim Biophys Acta. 2010;1797(2):113–28.
Nakada K, Sato A, Hayashi J. Reverse genetic studies of mitochondrial DNA-based diseases using a mouse model. Proc Jpn Acad Ser B Phys Biol Sci. 2008;84(5):155–65.
Seibel P, Trappe J, Villani G, Klopstock T, Papa S, Reichmann H. Transfection of mitochondria: strategy towards a gene therapy of mitochondrial DNA diseases. Nucleic Acids Res. 1995;23(1):10–7.
Vestweber D, Schatz G. DNA-protein conjugates can enter mitochondria via the protein import pathway. Nature. 1989;338:170–2.
Moraes CT, Bacman SR, Williams SL. Manipulating mitochondrial genomes in the clinic: playing by different rules. Trends Cell Biol. 2014;24(4):209–11.
Moraes CT. A magic bullet to specifically eliminate mutated mitochondrial genomes from patients’ cells. EMBO Mol Med. 2014;6(4):434–5.
Pinto M, Moraes CT. Mitochondrial genome changes and neurodegenerative diseases. Biochim Biophys Acta. 2014;1842(8):1198–207.
Sligh JE, Levy SE, Waymire KG, Allard P, Dillehay DL, Nusinowitz S, et al. Maternal germ-line transmission of mutant mtDNAs from embryonic stem cell-derived chimeric mice. Proc Natl Acad Sci U S A. 2000;97(26):14461–6.
Larsson NG, Wang J, Wilhelmsson H, Oldfors A, Rustin P, Lewandoski M, et al. Mitochondrial transcription factor A is necessary for mtDNA maintenance and embryogenesis in mice. Nat Genet. 1998;18(3):231–6.
Nakada K, Sato A, Sone H, Kasahara A, Ikeda K, Kagawa Y, et al. Accumulation of pathogenic DeltamtDNA induced deafness but not diabetic phenotypes in mito-mice. Biochem Biophys Res Commun. 2004;323(1):175–84.
Irwin MH, Johnson LW, Pinkert CA. Isolation and microinjection of somatic cell-derived mitochondria and germline heteroplasmy in transmitochondrial mice. Transgenic Res. 1999;8(2):119–23.
Nakada K, Inoue K, Ono T, Isobe K, Ogura A, Goto YI, et al. Inter-mitochondrial complementation: mitochondria-specific system preventing mice from expression of disease phenotypes by mutant mtDNA. Nat Med. 2001;7(8):934–9.
Nakada K, Sato A, Yoshida K, Morita T, Tanaka H, Inoue S, et al. Mitochondria-related male infertility. Proc Natl Acad Sci U S A. 2006;103(41):15148–53.
Jackson DC. Surviving extreme lactic acidosis: the role of calcium lactate formation in the anoxic turtle. Respir Physiol Neurobiol. 2004;144(2–3):173–8.
Grady JP, Campbell G, Ratnaike T, Blakely EL, Falkous G, Nesbitt V, et al. Disease progression in patients with single, large-scale mitochondrial DNA deletions. Brain. 2014;137(Pt 2):323–34.
Berio A, Piazzi A. Multiple endocrinopathies (growth hormone deficiency, autoimmune hypothyroidism and diabetes mellitus) in Kearns-Sayre syndrome. Pediatr Med Chir. 2013;35(3):137–40.
Varlamov DA, Kudin AP, Vielhaber S, Schroder R, Sassen R, Becker A, et al. Metabolic consequences of a novel missense mutation of the mtDNA CO I gene. Hum Mol Genet. 2002;11(16):1797–805.
Wallace DC, Singh G, Lott MT, Hodge JA, Schurr TG, Lezza AMS, et al. Mitochondrial DNA mutation associated with Leber’s hereditary optic neuropathy. Science. 1988;242:1427–30.
Sadun AA, La Morgia C, Carelli V. Leber’s hereditary optic neuropathy. Curr Treat Options Neurol. 2011;13(1):109–17.
Yokota M, Shitara H, Hashizume O, Ishikawa K, Nakada K, Ishii R, et al. Generation of trans-mitochondrial mito-mice by the introduction of a pathogenic G13997A mtDNA from highly metastatic lung carcinoma cells. FEBS Lett. 2010;584(18):3943–8.
Hashizume O, Shimizu A, Yokota M, Sugiyama A, Nakada K, Miyoshi H, et al. Specific mitochondrial DNA mutation in mice regulates diabetes and lymphoma development. Proc Natl Acad Sci U S A. 2012;109(26):10528–33.
Korhonen JA, Pham XH, Pellegrini M, Falkenberg M. Reconstitution of a minimal mtDNA replisome in vitro. EMBO J. 2004;23(12):2423–9.
Edgar D, Trifunovic A. The mtDNA mutator mouse: dissecting mitochondrial involvement in aging. Aging (Albany NY). 2009;1(12):1028–32.
Ross JM, Oberg J, Brene S, Coppotelli G, Terzioglu M, Pernold K, et al. High brain lactate is a hallmark of aging and caused by a shift in the lactate dehydrogenase A/B ratio. Proc Natl Acad Sci U S A. 2010;107(46):20087–92.
Ahlqvist KJ, Hamalainen RH, Yatsuga S, Uutela M, Terzioglu M, Gotz A, et al. Somatic progenitor cell vulnerability to mitochondrial DNA mutagenesis underlies progeroid phenotypes in Polg mutator mice. Cell Metab. 2012;15(1):100–9.
Suomalainen A, Kaukonen J. Diseases caused by nuclear genes affecting mtDNA stability. Am J Med Genet. 2001;106(1):53–61.
Van Goethem G, Dermaut B, Lofgren A, Martin JJ, Van Broeckhoven C. Mutation of POLG is associated with progressive external ophthalmoplegia characterized by mtDNA deletions. Nat Genet. 2001;28(3):211–2.
Lamantea E, Tiranti V, Bordoni A, Toscano A, Bono F, Servidei S, et al. Mutations of mitochondrial DNA polymerase gammaA are a frequent cause of autosomal dominant or recessive progressive external ophthalmoplegia. Ann Neurol. 2002;52(2):211–9.
Agostino A, Valletta L, Chinnery PF, Ferrari G, Carrara F, Taylor RW, et al. Mutations of ANT1, Twinkle, and POLG1 in sporadic progressive external ophthalmoplegia (PEO). Neurology. 2003;60(8):1354–6.
Van Goethem G, Schwartz M, Lofgren A, Dermaut B, Van Broeckhoven C, Vissing J. Novel POLG mutations in progressive external ophthalmoplegia mimicking mitochondrial neurogastrointestinal encephalomyopathy. Eur J Hum Genet. 2003;11(7):547–9.
Naviaux RK, Nguyen KV. POLG mutations associated with Alpers’ syndrome and mitochondrial DNA depletion. Ann Neurol. 2004;55(5):706–12.
Ferrari G, Lamantea E, Donati A, Filosto M, Briem E, Carrara F, et al. Infantile hepatocerebral syndromes associated with mutations in the mitochondrial DNA polymerase-{gamma}A. Brain. 2005;128(Pt 4):723–31. Epub 2005 Feb 2.
Luoma P, Melberg A, Rinne JO, Kaukonen JA, Nupponen NN, Chalmers RM, et al. Parkinsonism, premature menopause, and mitochondrial DNA polymerase gamma mutations: clinical and molecular genetic study. Lancet. 2004;364(9437):875–82.
Suomalainen A. Mitochondrial DNA, and disease. Ann Med. 1997;29(3):235–46.
Gellhaar S, Marcellino D, Abrams MB, Galter D. Chronic L-DOPA induces hyperactivity, normalization of gait and dyskinetic behavior in MitoPark mice. Genes Brain Behav. 2015;14(3):260–70.
Grauer SM, Hodgson R, Hyde LA. MitoPark mice, an animal model of Parkinson’s disease, show enhanced prepulse inhibition of acoustic startle and no loss of gating in response to the adenosine A(2A) antagonist SCH 412348. Psychopharmacology (Berl). 2014;231(7):1325–37.
Li X, Redus L, Chen C, Martinez PA, Strong R, Li S, et al. Cognitive dysfunction precedes the onset of motor symptoms in the MitoPark mouse model of Parkinson’s disease. PLoS One. 2013;8(8):e71341.
Ferraro P, Pontarin G, Crocco L, Fabris S, Reichard P, Bianchi V. Mitochondrial deoxynucleotide pools in quiescent fibroblasts: a possible model for mitochondrial neurogastrointestinal encephalomyopathy (MNGIE). J Biol Chem. 2005;280(26):24472–80.
Saada A, Shaag A, Mandel H, Nevo Y, Eriksson S, Elpeleg O. Mutant mitochondrial thymidine kinase in mitochondrial DNA depletion myopathy. Nat Genet. 2001;29(3):342–4.
Oskoui M, Davidzon G, Pascual J, Erazo R, Gurgel-Giannetti J, Krishna S, et al. Clinical spectrum of mitochondrial DNA depletion due to mutations in the thymidine kinase 2 gene. Arch Neurol. 2006;63(8):1122–6.
Hirano M, Lagier-Tourenne C, Valentino ML, Marti R, Nishigaki Y. Thymidine phosphorylase mutations cause instability of mitochondrial DNA. Gene. 2005;354:152–6.
Joza N, Oudit GY, Brown D, Benit P, Kassiri Z, Vahsen N, et al. Muscle-specific loss of apoptosis-inducing factor leads to mitochondrial dysfunction, skeletal muscle atrophy, and dilated cardiomyopathy. Mol Cell Biol. 2005;25(23):10261–72.
Hirst J, Carroll J, Fearnley IM, Shannon RJ, Walker JE. The nuclear encoded subunits of complex I from bovine heart mitochondria. Biochim Biophys Acta. 2003;1604(3):135–50.
Loeffen JL, Smeitink JA, Trijbels JM, Janssen AJ, Triepels RH, Sengers RC, et al. Isolated complex I deficiency in children: clinical, biochemical and genetic aspects. Hum Mutat. 2000;15(2):123–34.
Morris AAM, Leonard IV, Brown GK, Bidouki SK, Bindoff LA, Woodward CE, et al. Deficiency of respiratory chain complex I is a common cause of Leigh disease. Ann Neurol. 1996;40(1):25–30.
Anderson SL, Chung WK, Frezzo J, Papp JC, Ekstein J, DiMauro S, et al. A novel mutation in NDUFS4 causes Leigh syndrome in an Ashkenazi Jewish family. J Inherit Metab Dis. 2008;31 Suppl 2:S461–7.
Betts J, Lightowlers RN, Turnbull DM. Neuropathological aspects of mitochondrial DNA disease. Neurochem Res. 2004;29(3):505–11.
Leong DW, Komen JC, Hewitt CA, Arnaud E, McKenzie M, Phipson B, et al. Proteomic and metabolomic analyses of mitochondrial complex I-deficient mouse model generated by spontaneous B2 short interspersed nuclear element (SINE) insertion into NADH dehydrogenase (ubiquinone) Fe-S protein 4 (Ndufs4) gene. J Biol Chem. 2012;287(24):20652–63.
Ingraham CA, Burwell LS, Skalska J, Brookes PS, Howell RL, Sheu SS, et al. NDUFS4: creation of a mouse model mimicking a Complex I disorder. Mitochondrion. 2009;9(3):204–10.
Guzman M, Blazquez C. Ketone body synthesis in the brain: possible neuroprotective effects. Prostaglandins Leukot Essent Fatty Acids. 2004;70(3):287–92.
Turunen M, Olsson J, Dallner G. Metabolism and function of coenzyme Q. Biochim Biophys Acta. 2004;1660(1–2):171–99.
Luna-Sanchez M, Diaz-Casado E, Barca E, Tejada MA, Montilla-Garcia A, Cobos EJ, et al. The clinical heterogeneity of coenzyme Q10 deficiency results from genotypic differences in the Coq9 gene. EMBO Mol Med. 2015;7(5):670–87.
Emmanuele V, Lopez LC, Berardo A, Naini A, Tadesse S, Wen B, et al. Heterogeneity of coenzyme Q10 deficiency: patient study and literature review. Arch Neurol. 2012;69(8):978–83.
Duncan AJ, Bitner-Glindzicz M, Meunier B, Costello H, Hargreaves IP, Lopez LC, et al. A nonsense mutation in COQ9 causes autosomal-recessive neonatal-onset primary coenzyme Q10 deficiency: a potentially treatable form of mitochondrial disease. Am J Hum Genet. 2009;84(5):558–66.
Benit P, Lebon S, Rustin P. Respiratory-chain diseases related to complex III deficiency. Biochim Biophys Acta. 2009;1793(1):181–5.
Arnold S. Cytochrome c oxidase and its role in neurodegeneration and neuroprotection. Adv Exp Med Biol. 2012;748:305–39.
Shoubridge EA. Cytochrome c oxidase deficiency. Am J Med Genet. 2001;106(1):46–52.
Sacconi S, Salviati L, Sue CM, Shanske S, Davidson MM, Bonilla E, et al. Mutation screening in patients with isolated cytochrome c oxidase deficiency. Pediatr Res. 2003;53(2):224–30.
Pulliam DA, Deepa SS, Liu Y, Hill S, Lin AL, Bhattacharya A, et al. Complex IV-deficient Surf1(–/–) mice initiate mitochondrial stress responses. Biochem J. 2014;462(2):359–71.
Deepa SS, Pulliam D, Hill S, Shi Y, Walsh ME, Salmon A, et al. Improved insulin sensitivity associated with reduced mitochondrial complex IV assembly and activity. FASEB J. 2013;27(4):1371–80.
Valnot I, von Kleist-Retzow JC, Barrientos A, Gorbatyuk M, Taanman JW, Mehaye B, et al. A mutation in the human heme a: farnesyltransferase gene (COX10) causes cytochrome c oxidase deficiency. Hum Mol Genet. 2000;9(8):1245–9 [In Process Citation].
Tiranti V, D’Adamo P, Briem E, Ferrari G, Mineri R, Lamantea E, et al. Ethylmalonic encephalopathy is caused by mutations in ETHE1, a gene encoding a mitochondrial matrix protein. Am J Hum Genet. 2004;74(2):239–52.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing
About this chapter
Cite this chapter
Aradjanski, M., Trifunovic, A. (2016). Can We Accurately Model Mitochondrial Dysfunction in Neurodegeneration?. In: Reeve, A., Simcox, E., Duchen, M., Turnbull, D. (eds) Mitochondrial Dysfunction in Neurodegenerative Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-28637-2_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-28637-2_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28635-8
Online ISBN: 978-3-319-28637-2
eBook Packages: MedicineMedicine (R0)