Abstract
The technique of multiphase postmortem computed tomography angiography (MPMCTA) is today’s most often used and published method of postmortem angiography (PMA). It consists of a standardized protocol of perfusion parameters, injection material, and data acquisition. Specific material has been developed to ease the use of the technique and document the perfusion of the body. Thanks to this technique, it is possible to visualize the vascular system of the head, thorax, abdomen, and partially the limbs of a body even after a long postmortem delay. Therefore, diagnosis of various vascular, organic, and soft-tissue lesions can be achieved radiologically. In general, this minimally invasive method is performed via the cannulation of the femoral vessels of one side of the body. However, as an alternative, the cannulation site can be switched to the axillary vessels. No matter which approach is chosen, the same injection parameters are applied, leading to no change in the technical protocol. This chapter explains in detail how an MPMCTA is performed using either the femoral or the axillary approach.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
The technique of multiphase postmortem computed tomography angiography (MPMCTA) is today’s most often used and published method of postmortem angiography (PMA). It consists of a standardized protocol of perfusion parameters, injection material, and data acquisition. Specific material has been developed to ease the use of the technique and document the perfusion of the body. Thanks to this technique, it is possible to visualize the vascular system of the head, thorax, abdomen, and partially the limbs of a body even after a long postmortem delay. Therefore, diagnosis of various vascular, organic, and soft-tissue lesions can be achieved radiologically. In general, this minimally invasive method is performed via the cannulation of the femoral vessels of one side of the body. However, as an alternative, the cannulation site can be switched to the axillary vessels. No matter which approach is chosen, the same injection parameters are applied, leading to no change in the technical protocol. This chapter explains in detail how an MPMCTA is performed using either the femoral or the axillary approach.
1 Introduction
The method of multiphase postmortem computed tomography angiography (MPMCTA) [1] is today the most regularly used and best investigated technique of postmortem angiography (PMA). Multiple studies have evaluated the performance of the technique in different study populations, such as cases of cardiac death [2–5], postsurgical interventions [6, 7], fatal hemorrhage [6–9], or trauma [10]. Chevallier et al. [11] investigated the diagnostic value of MPMCTA compared to conventional autopsy and native postmortem computed tomography (PMCT) on a “normal” medico-legal population without any selection according to the indication of the medico-legal autopsy requested by the prosecutor. In comparing findings based on the different methods for 50 cases, these authors identified those that could be detected by one method exclusively. Findings were divided according to their anatomic compartment (soft tissue, bone, organs, vascular) and their importance for solving the medico-legal cases. The results essentially showed that MPMCTA and conventional autopsy would have led to similar conclusions regarding causes of death with almost 60 % of all findings that were visualized with both techniques. However, the two radiologic methods (PMCT and MPMCTA) were clearly superior to autopsy for detecting bone and vascular findings, while autopsy remained superior for investigating organs. Overall, adding MPMCTA to native PMCT could increase the sensitivity for detecting findings from approximately 65–81 %. Autopsy led to results similar to those of MPMCTA with about 83 % of detected findings. Surprisingly, concerning essential results, MPMCTA was superior to autopsy with approximately 93 % reported findings (autopsy detected about 77 % of them). Today, a similar study that is in preparation for publication followed an almost identical study design but was carried out using a multicenter approach at nine European centers of legal medicine with 500 cases. Preliminary results are promising, and MPMCTA performed even better than in the study of Chevallier et al. [11].
As described in Chap. 6, the visualization of the vascular system is not the only criterion for judging a method of PMA. The readability of the images obtained and the availability of keys for correct radiologic reading are also determinants for the applicability of the technique. Because MPMCTA is such a widespread technique, experience has already been gained [3, 12] that allows for a correct interpretation of the data obtained with it. Comprehensive guidance and suggestions can be found in this atlas because most chapters and images deal with this method. In addition, the influence of the contrast agent mixture on other medico-legal examinations is important to be explored and understood. Concerning the influence of MPMCTA on autopsy, histology, immunohistology, toxicology, genetic, biochemical, and microbiological analysis, studies have already been carried out [5, 13–16] to ensure a correct and complete medico-legal investigation with no complications arising from the influence of contrast media. These results are summarized and discussed in Chaps. 29 and 30.
Based on the present knowledge, MPMCTA is a standardized and validated method that can be applied without skepticism in medico-legal cases.
2 Development of MPMCTA
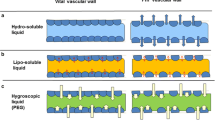
The development of MPMCTA is essentially based on research initiated by the Virtopsy® team at the University of Bern, Switzerland, where Grabherr and colleagues started research on the injection of oily liquids as contrast agents [17]. This idea was born from the knowledge acquired in an in-depth literature study of classic methods of PMA [18]. In fact, as already described by Barmayer [19], oily liquids can remain intravascular without penetration through the vascular wall into the surrounding tissue. For this reason, Barmayer could use them to perfuse the coronary arteries and study the flow capacity of those vessels [19]. The same ability is known and used for chemoembolization.
In fact, oily contrast agents such as lipiodol are injected into tumor vessels to embolize them [20, 21]. Depending on the viscosity of the oily liquid, the perfusion will stop at a certain level of vascular diameter, and the oil will remain intravascular, creating an intraluminal thrombus and therefore obstructing perfusion of the vessel. This obstruction should lead to an infarction of the depending tumoral area and subsequent necrosis of the tumor. The effect of this “microembolization” of vessels was studied in a microscopic study by Grabherr and coworkers, who tested the occlusion of vessels by diesel oil using a chorioallantoic membrane (CAM) model and a fluorescence microscope [22]. That study showed that injection of diesel oil leads to occlusion of the vessels at a precapillary level but that perfusion of the vascular system is still possible thanks to the presence of arteriolo-venous shunts. Therefore, the authors concluded that oily liquids are ideal for performing a postmortem perfusion because the liquid remains intravascular and blocks the capillary system, which is especially vulnerable to postmortem changes [22]. It can, however, switch from the arterial to the venous system via small shunt vessels.
The perfusion of the vascular system with oily liquids was then studied by establishing a “postmortem circulation” with diesel oil on animal cadavers [17, 22]. The tests showed that such a perfusion was possible. Once that was established, an oily contrast agent was injected, allowing excellent visualization of the vascular system [22]. Although this method of PMA proved to be feasible, it also involved clear limitations such as the discharge of perfusion volume into the stomach and the intestine, mostly because of the high enzymatic activity and bacterial decomposition of these organs and, of course, the odor of the diesel oil.
To overcome the problem of perfusate loss in those “locus minoris resistentiae,” Grabherr tested different oily liquids with different viscosities and developed a specific contrast agent for PMA called Angiofil® (FUMEDICA, Muri, Switzerland) [23]. Mixed with a solvent that decreases its viscosity, it can be applied to perform microangiography, for example, on mice [23]. Mixed with paraffin oil of specific viscosity (paraffinum liquidum with a viscosity of minimum 100 and maximum 23 mPa), it proved to be adequate for the perfusion of a human body [1].
Another problem to solve in transferring the angiography technique using oily liquids from an animal model to a human body was the choice of an adequate injection device. Although a simple roller pump is sufficient to perfuse the body of a cat or a dog [18, 22] and a simple manual injection is successful for perfusing a mouse [23], the perfusion of a human body is much more complex (see Chap. 6). For this reason, Grabherr introduced a modified heart–lung machine to allow the constant and regular injection necessary with a postmortem perfusion [24]. The developed technique using an oily perfusion, the injection of an oily contrast agent, and perfusion via a modified heart–lung machine was called a “two-step postmortem angiography” [24]. In fact, this technique consisted of the establishment of a postmortem circulation mimicking in vivo conditions as a first step and the injection of an oily contrast agent (lipiodol ultra-fluide, Guerbet Laboratories, Villepinte, France) as a second step. Using this technique made it possible to visualize the vascularization of the limbs of human bodies in detail and the pathologic changes such as injection marks and vascular occlusions [24].
With the aims of easing the performance of PMA and developing a standardized approach for whole-body PMA, the University Center of Legal Medicine in Lausanne-Geneva initiated a research project on PMA. An interdisciplinary team consisting of forensic pathologists, radiologists, radiographers, engineers, and cardio-technicians started to test different perfusion protocols and technical equipment to increase the quality of the vascular perfusion and visualization with the aim of improving the diagnostic accuracy of the obtained images. This project, which resulted in the development of MPMCTA, also revealed two important features that are necessary to perform high-quality PMA. The first is a complete vascular opacification, which can be obtained only by using high perfusion volumes; the second is the need for multiple different angiographic phases on native PMCT scan prior to the contrast agent injection [1]. In fact, only if the vessels are completely perfused and their lumina entirely contrasted can a diagnosis be obtained. To achieve this contrast in the vessels, the method of MPMCTA involves injection of high volumes of a contrast agent mixture consisting of paraffin oil (paraffinum liquidum with a viscosity of minimum 100 and maximum 23 mPa) and the recently developed Angiofil® (FUMEDICA, Muri, Switzerland) in a mixture of 6 %. Because the remaining blood and postmortem blood clots can still lead to filling defects of the lumina, Grabherr [1] found that such artefacts can be recognized thanks to the performance of different phases of angiography (see Chap. 29). For this reason, different multidetector computed tomography (MDCT) acquisitions are performed, and the images have to be compared to each other. The MPMCTA protocol thus includes one arterial (after the filling of the arterial system), one venous (after the filling of the venous system), and one dynamic phase. The last is performed during an ongoing perfusion with the aims of mimicking in vivo conditions and visualizing the vascular system under a perfusion pressure, similar to clinical angiography. This last phase is essentially performed to confirm a diagnosis obtained in the first two phases. Only if a finding is still visible can it be interpreted as a real finding and not as artefact (e.g., the remaining blood mimicking a vascular occlusion in the arterial phase moves further on in the dynamic phase and can therefore be recognized).
Parallel to the development of MPMCTA and the scientific approach to learning how to interpret the obtained images, an industrial partner of the research team, the Swiss enterprise FUMEDICA, Muri, Switzerland, started to develop specific equipment for performing PMA according to the expectations and wishes of the team. This step made development of a specific perfusion device for MPMCTA possible. In contrast to the modified heart–lung machine that was used until then, the so-called Virtangio® device (Fig. 10.1) is much easier to use, has a simplified tubing system allowing for rapid handling, is semi-automatic, can be manipulated from a laptop in the CT control room, and has a control system that regularly measures the injection pressure in the tubing system just before the contrast agent mixture enters the vessels of the body. This last point seems especially important because it allows creation of a pressure curve that can be followed during the injection on the screen (Fig. 10.2). For each investigated case, the registered pressure curves can be exported and stored on a USB key after the examination (Fig. 10.3) to establish the regular performance of the method and rule out any periods of over-pressure that could have damaged the body’s vascular system. In fact, in such a case, the system automatically stops and alerts the user to a problem (e.g., malposition of the cannula in the surrounding tissue leading to a pressure increase). Such documentation could have a crucial role in a trial to rule out any wrong manipulation or complication of the perfusion and demonstrate the regular performance of the standardized method.
View of the screen of the Virtangio® device indicating the actual pressure measured inside the cannula just before entering the vascular system of the body (site of highest pressure). Note that the intracannular pressure does not correspond to the intraluminar pressure inside of the body but is much higher
3 The Technical Approach of MPMCTA
As mentioned earlier, the technique of MPMCTA is standardized, using a defined injection protocol, cannulation process, and CT data acquisitions at predefined moments. A native PMCT is recommended before any manipulation of the body as part of the MPMCTA technique. Also, the performance of sampling using CT-guided biopsy or tissue puncture should be included if MPMCTA is performed. Advice concerning ideal sampling for further analysis can be found in Chaps. 29 and 30. Of course, the sampling protocol may vary among centers according to internal standards and the medico-legal case. An example for sampling procedures was published in 2012 by Schneider [25]. The description of how to perform the MPMCTA itself is presented in the following two sections.
4 The Femoral Approach
In most cases, MPMCTA is performed by using the femoral vessels to access the vascular system. In fact, this approach is generally preferred because the inguinal region is simple to access, and the vessels are situated close to the body surface. A detailed description indicating the different steps for performing MPMCTA by cannulating the femoral vessels follows.
4.1 Choice of Cannulation Site
In a first step, the native CT scan can be used to visualize the deeper structures of the femoral region and give a first look at the state of the vessels (e.g., the presence of atherosclerosis, stent, hematoma). Depending on the outcomes, the side for performing the cannulation of the femoral vessels can be chosen. Cannulation in a region where medical interventions have been performed (such as insertion of vascular catheters or stents) should be avoided. In cases of trauma, the side with fewer pathologic changes, such as intramuscular hematomas, should be chosen. It should also be considered that a regularly performed MPMCTA allows visualization of the arterial system of the contralateral leg but not of the vessels of the leg on the cannulated side. Thus, the choice of cannulation should be considered case by case according to the medico-legal question and the condition of the body.
4.1.1 Dissection Technique
The second step consists of preparing the dissection instruments and the angiography set (Fig. 10.4). Generally, eight instruments are used: one scalpel, one to two retractors, two clamps, one clip, one scissors, and one Halstead mosquito forceps. The intervention is performed in the triangle of Scarpa (Fig. 10.5). The best location for the incision can be detected by putting the thumb on the anterosuperior iliac spine, then the medium finger on the pubic symphysis. In this position, the forefinger automatically indicates where to make an incision of 5–10 cm.
The dissection consists of retracting the soft tissues in order to find the femoral vessels without cutting them. Therefore, curved scissors are used, which are inserted into the tissue in a closed position. By simply opening them, the fatty tissues can be dissected in a blunt way, avoiding the risk of creating vascular lesions. Retractors are used to keep the cannulation site open during the manipulation (Fig. 10.6). Once the femoral artery and vein are located, the strings can be passed around them by using the Halstead mosquito forceps (Fig. 10.7). Afterward, the plastic tube is put on the string using the hook. It is then inserted into the plastic tube, the two ends of the string are grabbed with the hook (Fig. 10.8), and the tube is pushed over the string. This procedure is done for the artery and vein, fixing them both with a string covered by a plastic tube that is needed later to fix the cannula (Fig. 10.9).
4.1.2 Insertion of Cannulas
Next, a small incision is performed in the vessels to insert the cannulas into the lumina. The cannula with the blue mark is inserted into the femoral vein and the one with the red mark into the femoral artery. To avoid any dissection of the vessel, the vascular wall should be held with the clip, and the lumen can be predilated by inserting the mosquito forceps in a closed position and opening it inside of the lumen; in this way it can be viewed and the integrity of the wall controlled (Fig. 10.10). The cannulas are inserted ideally about 5 cm into the vessels lumina by effecting slight rotational movements while pushing them forward. Then they are fixed with the plastic tube, which is pushed over the string until it touches the cannula. The tube is compressed and the clamp closed behind it. To ensure a tight fix, the thumb can be used to push the clamp into the correct position before closing it. After having controlled the fixation of the cannula in the vessels, the tape can be used to fix the distal end of the cannulas on the body’s skin (Fig. 10.11).
4.1.3 Connection to the Perfusion Device
Once the cannulas are inserted, they can be connected to the tubing system. Therefore, care must be taken that the tubes are completely filled with the contrast agent mixture. As the tubes approach the cannulas, the cannulas also should be filled with the liquid by pressing the foot pedal of the Virtangio® device (Fig. 10.12). This procedure of eye-controlled filling of the whole system just before connecting the tube and cannula (Fig. 10.13) avoids introducing air into the cannulation system and air bubble–related artefacts on the images. The final connection should be done only when the whole system is filled with the liquid (Fig. 10.14).
4.1.4 Control of the Cannula Position
In most cases, the insertion of the cannulas is easy, without any resistance. However, in cases with advanced arteriosclerosis, the cannula insertion can be difficult. If any doubt exists about the correction position of the cannulas, it can be verified by injecting a small amount of contrast agent and performing a local CT acquisition around the inguinal region.
4.1.5 CT Data Acquisition
Once the cannulas are correctly connected to the perfusion device, the angiography procedure can be started. Care is required to ensure that the CT data acquisition is well coordinated with the injection of the contrast agent mixture. As mentioned previously, a native CT scan should be done prior to the cannulation and sampling if possible. If this scan cannot be done at this point (e.g., cannulation of the body in a medico-legal department and imaging in a radiology department), it must be done prior to injection of the control agent.
Otherwise, the angiographic procedure starts with injection of the contrast agent according to the standardized perfusion protocol of MPMCTA (Table 10.1). Once the arterial injection is complete (automatically by using the Virtangio® device), the CT data acquisition of the arterial phase can be done. A proposition of CT acquisition parameters for 8 and 64 row scanners can be found as an example in Tables 10.2 and 10.3. After the CT acquisition has ended, the venous injection follows. Again, CT acquisition is started immediately after the perfusion process is finished.
For the third, so-called dynamic phase, it is important to calculate the exact time for starting the CT acquisition. Because the injection is done with a perfusion of 200 mL/min and 500 mL of the perfusion mixture is to be injected, the dynamic phase will take 150 s. The CT data acquisition must be started with the goal of completing it at the same time or 1 or 2 s before the end of the perfusion to ensure an ongoing perfusion of liquid throughout the scan time. Thus, the estimated time of CT scanning must be considered to calculate the best moment to start the scanning procedure. The coordination between the perfusion device and CT acquisition is schematized in Fig. 10.15. The rest of the uninjected mixture of contrast agent can be kept and used for another case.
5 Axillary Approach
MPMCTA has primarily been performed by gaining access to the femoral artery and veins of the lower limb via the femoral triangle [1, 24, 26]. An alternative approach in gaining access through the upper limb has proved beneficial in certain forensic cases. As recently reported, a novel approach in MPMCTA via the axillary artery and vein is advantageous because it allows complete visualization of the lower limb vascular system.
The femoral approach is not without flaws: MPMCTA via the femoral approach is not ideal in cases of thromboembolism of the superficial and deep femoral vessels of the lower limb, traumatic injuries of the lower limb, and postoperative limb injuries because the cannulation may be complicated and the vessels of the lower limbs are not visualized completely [27–30]. On the other hand, when MPMCTA is performed via the axillary access, it can aid visualization of the head and neck, mediastinum, and entire lower vascular tree (e.g., iliac tract, abdominal aorta, portal system) in most pathophysiologic obstructions to blood flow (Fig. 10.16, Table 10.4).
The novel approach requires access through the axillary vessels unilaterally. The first incision need not be more than 5 cm long and should extend from the upper third of the anterior axillary line corresponding to the anterior axillary fold to the lower border of the pectoralis major muscle with the underlying pectoralis minor muscle. In addition, the arm should be abducted to about 45°. A second incision of no more than 5 cm long should continue from the origin of the first incision to the border of the coracobrachialis muscle. The axillary skin flaps must be reflected superiorly and inferiorly along the course of the groove of the axillary vessels, ensuring visibility of the subcutaneous fat and fasciae covering the axillary sheath and its contents (axillary bundle). The axillary sheath must be incised with a scalpel followed by blunt dissection until the tracts of the brachial plexus passing through the axilla are observed (roots of the median nerve, ulnar nerve with cutaneous nerve). The relation of the brachial artery and brachial vein to the median nerve (superiorly) and the ulnar nerve (inferiorly) should be noted. Following isolation of the aforementioned vessels, cannularization can be performed in the third part of the axillary artery (for the arterial system) and into the underlying axillary vein through the axillary sheath (Figs. 10.17 and 10.18).
Cannulas are regularly connected to the tube system of the perfusion device (Fig. 10.19), as described for the femoral approach. The whole procedure of CT data acquisition is the same as that described for the femoral approach.
A further advantage of such an approach is its hidden location. Upon completion, the incision through the anterior axillary fold is virtually nonexistent when the arm is completely adducted (Fig. 10.20).
In conclusion, the traditional femoral approach to visualize the lower extremity vascular system can be replaced by the axillary approach to magnify the diagnostic power of MPMCTA in cases of suspicion of venous thromboembolism of the lower legs, traumatic injuries relating to the lower limb, and postoperative injuries of the lower limb [31].
Dissection of the axillary region: The anterior surface of the axillary sheath should be incised with a scalpel, followed by blunt dissection of the brachial artery, brachial vein, and median and lateral roots of the medial and lateral cords of the median and ulnar nerves. (A), Lateral root of the lateral cord; (B), median root of the medial cord; (C), axillary artery; (D), axillary vein; (E), ulnar nerve; (1, median nerve; 2, axillary artery; 3, brachial vein; 4, ulnar nerve). Following the course of the brachial artery and vein, the cannula must be inserted into the “third part of the axillary artery” (for the arterial system) and into the corresponding axillary vein through to the axillary sheath
References
Grabherr S, Doenz F, Steger B, Dirnhofer R, Dominguez A, Sollberger B, et al. Multi-phase post-mortem CT-angiography. Development of a standardized protocol. Int J Legal Med. 2011;125:791–802.
Michaud K, Grabherr S, Jackowski C, Bollmann MD, Doenz F, Mangin P. Postmortem imaging of sudden cardiac death. Int J Legal Med. 2013;127:819–23.
Michaud K, Grabherr S, Faouzi M, Grimm J, Doenz F, Mangin P. Pathomorphological and CT-angiographical characteristics of coronary atherosclerotic plaques in cases of sudden cardiac death. Int J Legal Med. 2015;129(5):1067–77.
Michaud K, Grabherr S, Doenz F, Mangin P. Evaluation of postmortem MDCT and MDCT-angiography for the investigation of sudden cardiac death related to atherosclerotic coronary artery disease. Int J Cardiovasc Imag. 2012;28:807–22.
Palmiere C, Lobrinus JA, Mangin P, Grabherr S. Detection of coronary thrombosis after multi-phase postmortem CT-angiography. Leg Med. 2013;15:12–8.
Villaverde RV, Vanhaebost J, Grabherr S, Palmiere C. Pulmonary artery rupture during Swan-Ganz catheterisation: a case report. J Forensic Leg Med. 2014;21:48–52.
Zerlauth JB, Doenz F, Dominguez A, Palmiere C, Uské A, Meuli R, Grabherr S. Surgical interventions with fatal outcome: utility of multi-phase postmortem CT angiography. Forensic Sci Int. 2013;225:32–41.
Palmiere C, Binaghi S, Doenz F, Bize P, Chevallier C, Mangin P, Grabherr S. Detection of hemorrhage source: the diagnostic value of post-mortem CT-angiography. Forensic Sci Int. 2012;222:33–9.
Michaud K, Grabherr S, Lesta MD, Augsburger M, Doenz F, Mangin P. Ruptured pseudo-aneurysm of a femoral artery in a drug abuser revealed by post-mortem CT angiography. Int J Legal Med. 2013;127:819–23.
Grabherr S, Grimm J. Multiphase post-mortem Ct-angiography (MPMCTA): a new method for investigation of violent death. In: Püschel K H, Radiology, Society X-Rays: Tool and Document editors. Forensics. Hamburg, Germany: Dr. Kovač Verlag; 2014. p. 156–63.
Chevallier C, Doenz F, Vaucher P, Palmiere C, Dominguez A, Binaghi S, et al. Postmortem computed tomography angiography vs. conventional autopsy: advantages and inconveniences of each method. Int J Legal Med. 2013;127:981–9.
Bruguier C, Mosimann PJ, Vaucher P, Uské A, Doenz F, Jackowski C, et al. Multi-phase post-mortem CT angiography: recognizing technique-related artefacts and pitfalls. Int J Legal Med. 2013;127:639–52.
Grabherr S, Widmer C, Iglesias K, Sporkert F, Augsburger M, Mangin P, Palmiere C. Postmortem biochemistry performed on vitreous humor after postmortem CT-angiography. Leg Med (Tokyo). 2012;6:297–303.
Palmiere C, Egger C, Grabherr S, Jaton-Ogay K, Greub G. Postmortem angiography using femoral cannulation and postmortem microbiology. Int J Legal Med. 2015;4:861–7.
Palmiere C, Grabherr S, Augsburger M. Postmortem computed tomography angiography, contrast medium administration and toxicological analyses in urine. Leg Med (Tokyo). 2015;3:157–62.
Rutty GN, Barber J, Amoroso J, Morgan B, Graham EA. The effect on cadaver DNA identification by the use of targeted and whole body post-mortem computed tomography angiography. Forensic Sci Med Pathol. 2013;9:489–95.
Grabherr S. Postmortaler Kreislauf mit angiographischer Darstellung der arteriellen, kapillären und venösen Strombahn (thesis) [Post-mortem circulation with angiographic demonstration of the arterial, capillary and venous system]. Innsbruck: Medical University of Innsbruck; 2004.
Grabherr S, Djonov V, Yen K, Thali MJ, Dirnhofer R. Postmortem angiography: review of former and current methods. Am J Roentgenol. 2007;188:832–8.
Barmeyer J. Post mortem coronary angiography and perfusion of normal and diseased hearts: perfusibility of intercoronary anastomoses [In German]. Beitr Pathol Anat. 1968;137:373–90.
Nakakuma K, Tashiro S, Hiraoka T, Uemura K, Konno T, Miyauchi Y, et al. Studies on anticancer treatment with an oily anticancer drug injected into the ligated feeding hepatic artery for liver cancer. Cancer. 1983;52:2193–200.
Kan Z. Dynamic study of iodized oil in the liver and blood supply to hepatic tumors: an experimental investigation in several animal species. Acta Radiol Suppl. 1996;408:1–25.
Grabherr S, Djonov V, Friess A, Thali MJ, Ranner G, Vock P, Dirnhofer R. Postmortem angiography after vascular perfusion with diesel oil and a lipophilic contrast agent. Am J Roentgenol. 2006;187:W515–23.
Grabherr S, Hess A, Karolczak M, Thali MJ, Friess S, Kalender W. Angiofil®-mediated visualization of the vascular system by microcomputed tomography: a feasibility study. Microsc Res Tech. 2008;71:551–6.
Grabherr S, Gygax E, Sollberger B, Ross S, Oesterhelweg L, Bolliger S, et al. Two-step postmortem angiography with a modified heart-lung machine: preliminary results. Am J Roentgenol. 2008;190:345–51.
Schneider B, Chevallier C, Dominguez A, Bruguier C, Elandoy C, Mangin P, Grabherr S. The forensic radiographer: a new member in the medico-legal team. Am J Forensic Med Pathol. 2012;33:30–6.
Saukko P, Knight B. Knight’s forensic pathology. 3rd ed. London: Hodder Arnold; 2004. p. 342.
Torbicki A, van Beek EJR, Charbonnier B, Meyer G, Morpurgo M, Palla A, Perrier A. Guidelines on diagnosis and management of acute pulmonary embolism. Task Force on Pulmonary Embolism, European Society of Cardiology. Eur Heart. 2000;21:301–36.
Ro A, Kageyama N, Tanifuji T, Fukunaga T. Pulmonary thromboembolism: overview and update from medicolegal aspects. Leg Med (Tokyo). 2008;10:57–71.
Elhammady G, Schubeck AT, El-Najjar V, Robinson MJ. Postmortem demonstration of the source of pulmonary thromboembolism: the importance of the autopsy. Case Rep Vasc Med. 2011;2011:108215.
Fineschi V, Turillazzi E, Neri M, Pomara C, Riezzo I. Histological age determination of venous thrombosis: a neglected forensic task in fatal pulmonary thrombo-embolism. Forensic Sci Int. 2009;186:22–8.
Bello S, Neri M, Grilli G, Pascale N, Pomara C, Riezzo I. Multi-phase post-mortem CT-angiography (MPMCTA) is a very significant tool to explain cardiovascular pathologies. A sudden cardiac death case. Exp Clin Cardiol. 2014;20(1):1419–30.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Grabherr, S., Rinaldi, A., Dominguez, A., Pomara, C. (2016). Multiphase Postmortem Computed Tomography Angiography (MPMCTA). In: Grabherr, S., Grimm, J., Heinemann, A. (eds) Atlas of Postmortem Angiography. Springer, Cham. https://doi.org/10.1007/978-3-319-28537-5_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-28537-5_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28535-1
Online ISBN: 978-3-319-28537-5
eBook Packages: MedicineMedicine (R0)