Abstract
The vast majority of recreational dives are performed by divers using single cylinders of compressed air and open-circuit breathing systems, typically to a maximum depth of 40 m of seawater (msw). More extreme dives (in terms of depth and duration) are performed by a small subgroup of recreational divers who refer to their activity as ‘technical diving’. Technical divers substitute helium for nitrogen in gas mixes for deep diving to reduce the narcotic effect of nitrogen respired at high partial pressures and to reduce the density of the gas. These mixes also contain less oxygen than air in order to manage the risk of cerebral oxygen toxicity. Adequate gas supplies for long dives are carried in multiple cylinders, or divers may utilise ‘rebreather’ devices that recycle expired gas through a carbon dioxide (CO2) absorbent and which include a system for maintaining a safe inspired pressure of oxygen (PO2) as oxygen is consumed. These devices are complex and error-prone, and there is some evidence for relatively high accident rates in their use. Using these techniques, compressed gas dives between 40 and 100 msw are now relatively ‘routine’, and more extreme dives to depths in excess of 300 msw have been completed. A challenge of deep technical diving is the effect on respiratory physiology. There are multiple factors (including increased density of the respired gas) that increase the work of breathing during deep dives. This, in turn, may cause significant perturbation of normal respiratory control. In particular, there is a tendency for divers to hypoventilate and retain CO2 which can produce a number of dangerous secondary effects. Another significant challenge is uncertainty over the optimal protocol for decompression from deep dives. Technical divers utilise progressively more oxygen-rich breathing mixes during ascent in order to accelerate inert gas elimination, but there is uncertainty over how to plan the duration and depths of the ‘decompression stops’ that are completed during the ascent to allow time for this elimination to occur.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Technical diving
- Pneumothorax
- Mediastinal emphysema
- Embolic injury
- Cerebral oxygen toxicity
- Decompression sickness
- Hypercapnia
- Decompression algorithms
1 Introduction
Diving using self-contained underwater breathing apparatus (scuba) is a popular recreational activity. Participants are drawn from most age groups (children to elderly) and both genders. There are well-established agencies which provide training courses for diving at entry and more advanced levels, and there is a substantial industry involving equipment manufacturers and travel providers. The vast majority of recreational divers perform short, relatively shallow dives using a single cylinder of compressed air in order to participate in what could be referred to as ‘underwater sightseeing’. Many recreational divers include activities such as seafood harvesting or photography in their dive plans.
There is a much smaller subgroup of ‘extreme’ recreational divers who use a suite of advanced diving techniques (often referred to as ‘technical diving’) to visit deeper depths or remain underwater longer (or both) [1, 2]. The relevant techniques have some similarities to those used for occupational (commercial and military) diving to deep depths and some important differences. Commercial diving to depths frequented by technical divers is typically conducted by divers who live for weeks at a time inside a dry, shipboard chamber at a pressure close to the pressure at the depth of the worksite. Divers commute to the worksite in a pressurised diving bell and make excursions into the sea to perform underwater work but remain connected to the diving bell by an umbilical that provides breathing gas, heating, power and communications. Divers are only exposed to the physiological stresses of decompressing back to sea level pressure once at the end of the job. This type of diving is prohibitively expensive for a recreational activity, and technical divers undertake what are commonly referred to as ‘bounce dives’ – that is, the descent and a relatively short period at depth are followed immediately by decompression back to the surface – and technical divers always use scuba. In this respect, technical diving has some similarities to military underwater mine countermeasure diving. However, this latter task motivates spending as short a time as possible in the water exposed to the minefield, whereas technical divers seek to maximise the time they can spend at depth.
This chapter is primarily intended to describe the methods and challenges relevant to technical divers, but it begins (for perspective and contrast) with a brief description of the features of the underwater environment relevant to all divers and a very brief account of conventional recreational diving.
2 The Underwater Environment and Its Challenges
Any form of swimming involves immersion in a dense non-respirable medium with high thermal conductivity that is frequently cold and which is subject to surges and currents. These characteristics of the aquatic environment are relevant to diving also, but most of the unique challenges and problems associated with underwater swimming arise from the changes in pressure that occur during descent and ascent through the water column. For every 10.13-m increase in depth of seawater, the ambient pressure (P amb) increases by 1 atmosphere (atm) (101.3 kPa). Thus, a diver at a depth of 10 m of seawater (msw) is exposed to a P amb of approximately 2 atmospheres absolute (atm abs), 1 atm exerted by atmospheric air above the water and 1 atm exerted by the weight of water above the diver. Similarly, a diver at 20 msw is exposed to a P amb of 3 atm abs, a diver at 30 msw is exposed to a P amb of 4 atm abs and so on. The term ‘absolute’ is used to distinguish from ‘gauge’ pressures which ignore the pressure exerted by atmospheric air – gauge pressures are commonly used in diving, for instance, when P amb is given in equivalent depth of seawater. The important effects of this exposure to increased P amb can be subdivided broadly into effects on compressible air spaces and effects on gas physiology.
2.1 Pressure Effects on Compressible Air Spaces
A diver has several anatomical air spaces which are subjected to the pressure changes associated with descent and ascent. Most important are the middle ear spaces which must be equalised with airway gas via the Eustachian tubes during changes in depth. This usually requires an active manoeuvre like a ‘Valsalva’ during descent but occurs passively during ascent. Failure to equalise pressure in the middle ear can lead to barotrauma in which there is an effusion or bleeding behind the tympanic membrane or even perforation of the membrane. The sinus spaces may be affected in much the same way though equalisation through widely patent sinus ostia usually occurs without any active intervention by the diver [3].
The lungs are also susceptible to barotrauma. During descent on a compressed gas dive, the pressure in the lungs is automatically compensated because the breathing apparatus supplies respired gas at P amb. However, if gas becomes trapped in the lungs (or a segment of the lung) during ascent, then expansion of that gas as P amb decreases may result in over-distension of the lung tissue. This, in turn, can lead to pneumothorax, mediastinal emphysema or the introduction of gas into the pulmonary veins (Fig. 25.1). The resulting bubbles in the systemic circulation can cause embolic injury to vulnerable organs such as the brain [4].
2.2 Pressure Effects on Gas Consumption and Gas Physiology
Scuba equipment supplies the diver with gas at P amb, and gas density therefore increases in direct proportion to P amb as the diver ventures deeper. This has two implications. First, the work of breathing is increased, and this will be further discussed later in this chapter. Second, since more molecules of gas occupy the same volume at higher pressures, gas is consumed at a rate that also increases proportionally to P amb. For example, at 30 msw (4 atm abs) a diver could expect to consume their gas supply twice as fast as at 10 msw (2 atm abs) or four times as fast as at the surface (1 atm abs).
Breathing air (nitrogen 78 %, oxygen 21 %) at elevated P amb results in respiration of oxygen and nitrogen at higher partial pressures than normal. In both cases this can have important consequences.
Oxygen breathed at elevated pressures can result in cerebral irritability and seizures with little or no warning; a phenomenon commonly referred to as ‘cerebral oxygen toxicity’. This is particularly dangerous because loss of consciousness underwater will often lead to drowning. The mechanism of oxygen toxicity is poorly understood, though risk increases with inspired PO2 (PiO2) and the duration of the exposure [5]. There is no clear threshold PiO2 known to be invariably safe, though there is broad consensus that a PiO2 of 1.3 atm abs is relatively safe, even for long duration exposures. This is discussed further below, but in the context of the present narrative, avoidance of a PiO2 of greater than 1.3 atm abs effectively limits the use of air as a breathing gas to depths less than 52 msw (where the P amb = 6.2 atm abs, and the PiO2 when breathing air is therefore 6.2 × 0.21 = 1.3 atm).
Nitrogen breathed at elevated pressures produces a narcotic effect, often referred to as ‘nitrogen narcosis’ that increases progressively with the PiN2. This effect becomes noticeable at depths greater than 30 msw (P amb = 4 atm abs), but it is probably present at shallower depths. There is no universal consensus on a threshold depth beyond which nitrogen narcosis becomes intolerable, but diving with air beyond 40–50 msw is often considered inappropriate for this reason. It should be obvious that cognitive impairment due to nitrogen narcosis could predispose towards incidents [6].
The respiration of gases at elevated pressures results in greater absorption into blood and tissues as predicted by Henry’s law. During ascent, bubbles can form from this accumulated gas. These bubbles may be intravascular (appearing first in the venous system because it is the venous blood ‘draining’ from tissues that is supersaturated), or they may form within the tissues themselves. Depending on the site and profusion of these bubbles, they may cause symptoms of decompression sickness (DCS) (often referred to as ‘the bends’). Venous gas bubbles are routinely detected by ultrasonic methods (venous gas emboli: VGE) after dives that do not result in DCS. However, there is substantial evidence that divers with large right to left shunt pathways (such as a patent foramen ovale) are more vulnerable to developing serious neurological symptoms, implying that VGE can become harmful if they reach the arterial circulation. There are probably many mechanisms by which intravascular and extravascular bubbles can cause pathological effects, including direct mechanical effects, micro-vessel obstruction and activation of coagulation and other complex inflammatory processes. The pathophysiology of this condition is complex and beyond the scope of this chapter. It is described in more detail elsewhere [7, 8]. Symptoms can range from non-serious (such as fatigue, rash, pain) to serious (such as paralysis, cardiopulmonary collapse) [9].
3 Recreational Scuba Air Diving
The most common scuba configuration for recreational diving is a single cylinder of compressed air worn on the back with a ‘regulator’ which reduces the cylinder air pressure to P amb and supplies air during inhalation. The diver exhales into the surrounding water. Divers also require a mask (for vision) and fins (for underwater propulsion), and diving in temperate water usually requires the use of thermal protection in the form of a wet suit or dry suit. Most divers wear some form of buoyancy control device, effectively an inflatable water wing to which compressed air can be added (or removed) thus making the diver more (or less) buoyant. A diver wearing an equipment configuration typical of recreational air diving is shown in Fig. 25.2.
Recreational scuba air divers are taught to perform ‘no-decompression’ dives. That is, they are instructed to perform dives where nitrogen absorption into tissues is limited so that a direct ascent to the surface (at a rate not exceeding 9 m/min) is possible at all times during the dive. If the time/depth profile of a dive exceeds so-called no-decompression limits, then decompression stops to allow more time for tissue gas elimination must be made during the ascent. Most divers carry a dive computer that incorporates a timer, a pressure sensor, a microprocessor and an output screen and which continually updates a decompression algorithm and informs the diver how much time they have remaining at the current depth before an ascent with decompression stops becomes necessary. If the no-decompression time is exceeded, then the computer will prescribe the appropriate decompression stops during the ascent. With avoidance of the need for decompression stops and some of the other issues discussed above in mind, recreational diver training organisations usually recommend 40 msw as the maximum depth for scuba air diving.
Despite the seemingly daunting challenges above, recreational scuba air diving is a relatively safe sport. A training database maintained by the Professional Association of Diving Instructors indicates a fatality rate on scuba air training dives of 0.5 deaths per 100,000 dives [10]. Estimates of mortality and nonfatal decompression sickness in non-training scuba air dives are two per 100,000 and ten per 100,000 dives, respectively [11].
4 Technical Diving
There is a relatively small group of ‘technical divers’ who perform ‘extreme’ scuba dives beyond the depths and/or durations of typical recreational dives, typically for the purposes of reaching a deep shipwreck or exploring a long-flooded cave. Dives to depths of about 90 msw have become relatively common in this context, and some dives have exceeded 300 msw. Dives in caves lasting well over 12 h have been undertaken.
The challenges involved in the conduct of deep and/or long dives can be predicted from the preceding discussion and include:
-
1.
Reducing the narcotic effect of nitrogen in the respired gas
-
2.
Reducing the toxic effect of oxygen in the respired gas
-
3.
Managing the density of the respired gas
-
4.
Decompressing as quickly as possible while keeping the risk of decompression sickness low
-
5.
Carrying enough gas for very long duration dives
-
6.
Complex logistics including gas supplies and surface support and achieving adequate thermal protection
4.1 Mixed Gas Diving: The Pivotal Role of Helium
The first three of these challenges can be met by use of breathing gas mixes containing helium. Helium is a light inert gas that does not produce narcosis at elevated partial pressures. Thus, substituting helium for at least some of the nitrogen in the breathing gas ameliorates both the narcosis and density problems. This typically results in the diver breathing ‘trimix’: a combination of oxygen, helium and nitrogen. Technical divers define the particular mix by stating the fraction of oxygen and helium present. For example, ‘trimix 8:60’ would consist of 8 % oxygen and 60 % helium, and the unstated balance (32 %) is nitrogen.
Nitrogen is rarely substituted completely with helium for several reasons. One is the high cost of helium. This is less of an issue when using a rebreather which recycles exhaled gas (see later), but in open-circuit diving (where all exhaled gas is lost to the water), pure oxygen–helium mixtures (heliox) would be very expensive to use. In addition, some decompression models tend to penalise the use of high helium fractions by mandating longer decompressions. Although this may be unnecessary (see later), it remains a consideration for many divers in planning their gas mixes. Finally, in very deep dives beyond 150 msw, the inclusion of nitrogen in the breathing mix helps to ameliorate the high-pressure neurological syndrome (HPNS) which can cause troublesome tremors and cognitive impairment. HPNS is thought to be due to a pressure effect on excitable membranes, and the dissolution of highly soluble nitrogen into those membranes has an ameliorating effect which is not fully understood [6].
The ‘recipe’ for the optimal trimix for use during the deepest portion of the dive is based on the planned depth, the duration of the dive, the diver’s perception of the maximum safe inspired PO2 and the maximum tolerable narcotic effect. For example, in considering a dive to 90 msw (10 atm abs), the first decision is how much oxygen the mix should contain. Divers will usually aim to breathe as much oxygen as is considered safe, since breathing more oxygen means less inert gas uptake and therefore less decompression. Assuming that a maximum safe PiO2 of 1.3 atm (see earlier) is chosen:
The mix would therefore contain 13 % oxygen for breathing at 90 msw.
The second decision is the amount of nitrogen in the mix. A common basis for this decision is the degree of narcosis that the diver is prepared to tolerate which in turn is notionally ‘calibrated’ on a comparison with air diving. Thus, assuming a diver is comfortable with the level of narcosis experienced during air diving at 40 msw, they might aim to breathe an equivalent PN2 during the deepest phase of a trimix dive. This is easily calculated by multiplying the fraction of nitrogen in air (0.78) by the ambient pressure at 40 msw (5 atm abs) which gives a PN2 of 3.95 atm. Therefore:
The trimix should therefore contain 40 % nitrogen. This calculation assumes oxygen is not narcotic, but a more conservative approach assuming equal narcotic potency of oxygen and nitrogen yields only a small difference. Having calculated the ideal fractions of oxygen (FO2) and nitrogen (FN2) for the trimix, the helium content (FHe) simply makes up the balance, thus:
This planning process has determined that an appropriate trimix for a dive to 90 msw is 13 % oxygen, 47 % helium and 40 % nitrogen, designated trimix 13: 47. Another parameter often forgotten in such planning is the density of the resulting gas at the target depth. There is an increasing risk of CO2 retention as the inspired gas density increases, and this result can have life-threatening consequences (see later). It follows that there are sound reasons for ameliorating risk factors for hypercapnia, of which density is one; but there is no clear consensus on the upper density limit. Testing of equipment with gas at a density of 8 g L−1 has seen this figure sometimes cited, but recent (and as yet unpublished) data suggest a risk inflection for CO2 retention around a density of 6.2 g L−1. Calculation of gas density at a target depth is easily achieved based on proportions and adjustment for P amb if given the following densities (g L−1) at 1.0 atm abs: oxygen 1.43, nitrogen 1.25 and helium 0.18. In the above example, trimix 13: 47 at 90 msw (10 atm abs) would have a density of 7.7 g L−1. To comply with a 6.2 g L−1 recommendation, the mix could be adjusted to trimix 13: 60. The respiratory physiology of extreme deep diving is the first of two focus areas treated in more detail later in this chapter.
4.2 Decompressing as Quickly as Possible While Keeping the Risk of Decompression Sickness Low
Deep dives rapidly accumulate a decompression obligation (the need for decompression stops during the ascent), and it is one of the recognised travails of deep technical diving that more time (often substantially more) may need to be spent decompressing than actually on the bottom. Decompression can be a physically and mentally taxing experience, particularly when conducted in cold water and where there are environmental challenges such as wave action, currents and the onset of darkness. There is a strong motivation to minimise time spent decompressing while at the same time maintaining an acceptably low risk of DCS.
One universally employed strategy to accelerate decompression from deep dives is to increase the fraction of inspired oxygen while maintaining a safe PiO2 as the depth (and ambient pressure) decreases. Breathing a higher FO2 increases the gradient for diffusion of inert gas from tissue to alveoli and thus accelerates inert gas elimination. In many cases, divers choose a breathing mix with less or no helium in the shallower depths during decompression because helium’s low density and non-narcotic properties are no longer necessary. This also saves on the cost of this expensive gas, especially in open-circuit diving. In addition, merely switching from helium to nitrogen is also perceived to accelerate decompression (see later). Thus, divers frequently breathe so-called ‘nitrox’ mixes during decompression. Nitrox is a mix of oxygen and nitrogen with a fraction of oxygen higher than that in air. The mixes are named for the fraction of oxygen (nitrox 32 is 32 % oxygen and 68 % nitrogen). Thus, for example, during ascent a diver might switch to breathing nitrox 32 at 30 msw where the PiO2 would be 1.3 atm. There might be further changes to progressively ‘richer’ oxygen mixes, culminating in a final decompression stop at 3 msw conducted breathing pure (100 %) oxygen (where the PiO2 would also be 1.3 atm).
4.3 Carrying Large Gas Supplies or Extending Gas Supply
In order to undertake deep decompression dives, extreme divers must carry much greater supplies of gas or a means of extending a limited supply of gas. For open-circuit divers this inevitably means carrying multiple cylinders of gas during the dive (Fig. 25.3) and, in some cases, staging more cylinders of gas at strategic points on preliminary dives so that they are there for use on the ‘main dive’. The accurate planning of the required gas volumes for deep and/or long dives is one of the most critical skills for a technical diver but will not be described in more detail here.
Technical diver conducting a decompression stop. The two regulators from the diver’s twin, back-mounted cylinders are stowed, and diver is breathing from one of two ‘stage’ cylinders of decompression gas mixtures carried clipped to his harness. The reel of line is connected to a surface marker buoy that the diver deployed so that the surface vessel can track the dive team during a free-floating decompression. Note the diver propulsion vehicle which is not in use and is stowed. (Photo courtesy of A. Hagberg.)
The increasing use of rebreathers for the purpose of reducing gas consumption is arguably the most important development in technical diving over the last decade. A rebreather is a circle circuit containing one-way check valves, one or more counter-lungs, a CO2 absorbent canister and systems for maintaining both the volume of the circuit and an appropriate inspired PO2. Rebreathers are categorised by the nature of the system for maintaining the inspired PO2, and it is beyond the scope of this chapter to detail the operation of all of them. The most prevalent is the so-called electronic closed-circuit rebreather (eCCR). The typical (and simplified) functional layout of one of these devices is shown in Fig. 25.4, and divers wearing rebreathers are shown in Fig. 25.5.
During use, the diver exhales into the counter-lung through a CO2 absorbent and then inhales from the counter-lung. The one-way check valves in the mouthpiece ensure that flow around the circuit is unidirectional. Three galvanic fuel cells are exposed to the gas in the circuit. These are essentially oxygen-powered batteries that produce an electric current directly proportional to the PO2 to which they are exposed. After calibration against a known PO2, the averaged output of the three cells indicates the circuit PO2, and this is constantly monitored by a microprocessor. A target PiO2 (PO2 ‘set point’) is selected by the diver, and as oxygen consumption reduces the circuit PO2 below this target, the microprocessor opens an electronic solenoid valve to allow oxygen into the circuit to restore and maintain a relatively constant PO2 near the set point. This set point is typically 0.7 atm at the surface and is increased to a higher target (such as 1.3 atm) once the dive is underway.
The volume of the circuit is maintained as Pamb increases during descent by the addition of a diluent gas. When the counter-lung is compressed, the diver will begin to generate a negative pressure in the circuit during inhalation. This opens a mechanical diluent addition valve (Fig. 25.4) allowing diluent gas into the circuit and restoring its volume. For safety reasons, the diluent gas typically contains a fraction of oxygen high enough that the gas is breathable but low enough that the circuit PO2 can still be lowered to the desired set point at the deepest point in the dive. For a dive to less than 50 msw with a PO2 set point of 1.3 atm, air could be used as the diluent gas. Its oxygen fraction of 0.21 still allows a circuit PO2 of ~1.3 atm at 50 msw (ambient pressure of 6 atm abs × 0.21 = 1.26 atm), and at shallower depths the rebreather will add oxygen to maintain the PiO2 at 1.3 atm. Thus, the diver will be breathing a nitrox mix whose oxygen and nitrogen content varies with depth but whose PiO2 remains constant. For a deep dive the diluent gas (usually trimix) is chosen using virtually the same principles as described earlier for mixed-gas diving.
It should be obvious that the crucial advantage of a rebreather is the recycling of exhaled gas thus preserving expensive components like helium. Indeed, the use of diluent gas effectively ends on arrival at the deepest depth provided there is no up-and-down depth variation from that point on. In contrast to open-circuit diving, gas consumption changes little with depth, and the absolute amounts of gas used are vastly smaller.
Another major advantage of rebreathers is the breathing of the optimal safe inspired fraction of oxygen for minimising inert gas uptake and for accelerating decompression throughout the dive. In open-circuit diving, for each gas carried the inspired fraction of oxygen can only be optimal at one depth. Thus, in the example cited earlier, if a PiO2 of 1.3 atm is considered safe, then nitrox 32 breathed during decompression is only an optimal decompression gas at 40 m. On ascent to shallower depth, the PiO2 falls, and the fraction of inspired oxygen is no longer as high as it can safely be (and therefore no longer optimal). In contrast, an eCCR will raise the inspired fraction of oxygen to maintain the 1.3 atm PO2 set point throughout the ascent.
Other rebreather advantages include the breathing of warm, humidified gas and production of few or even no bubbles. The major disadvantages are that the devices are complex, costly and maintenance intensive, provide numerous opportunities for user error and have many potential failure points. Arguably the most significant of these is the oxygen cells which are ‘consuming’ and therefore have a limited and somewhat unpredictable life. Inaccurate data from oxygen cells has been the root cause of many accidents. This potential for failure mandates the requirement for access to open-circuit gas supplies (commonly referred to as ‘bailout’) appropriate for all depths visited and adequate to allow decompression from any point of the dive plan. Planning the carriage of bailout gases is very similar to the planning of an open-circuit deep dive described above. Notwithstanding this precaution, it is perhaps not surprising that crude estimates suggest that rebreather diving is associated with higher mortality (perhaps an order of magnitude higher) than open-circuit diving [12].
4.4 Logistics of Technical Diving
Technical diving frequently involves complex logistics to support these ambitious dives. Deep wrecks usually lie in open ocean, and diving them requires large boats for safe and reliable surface support in weather conditions that are rarely optimal. Accurate GPS and sounding equipment are vital, and teams develop considerable skill in accurately dropping a shot line down on to a wreck in deep waters. Divers usually descend and ascend on these shot lines, and purpose-built decompression stages with bars at the depths of the long stops help divers accurately maintain stop depths and allow multiple divers to comfortably occupy the station at the same depth (Fig. 25.5). However, strong currents can complicate such plans and necessitate the use of live boating, where the divers descend from an unanchored surface vessel up-current of the target and complete decompression drifting underneath a surface marker buoy so that the divers do not have to hold onto a shot line against the force of the current. To enhance safety, teams often arrange themselves into bottom diver and support diver roles. Bottom divers actually visit the wreck, and support divers help with surface logistics and visit the bottom divers during decompression. This allows any developing needs to be met and messages to be relayed to the surface.
The exploration of long and frequently deep caves has a different set of logistical challenges. Sequential dives, often very dependent on the use of battery-powered diver propulsion vehicles, are used to penetrate progressively further into the cave and to lay lines into new sections. As there is progress to greater distances, it may become necessary to stage gas supplies at strategic points on the way in before ‘pushing’ the cave further. In this setting, divers may arrange themselves into large teams with specific roles for each individual. Lead divers perform the long pushes. Setup divers may be required to stage gas prior to the dive, and support divers visit the lead divers during their decompression which, as in deep wreck diving, allows any developing needs to be met and messages to be relayed to the surface. In some major cave penetrations, support divers may even install dry underwater habitats (such as an upside-down rainwater tank filled with air) in which the lead divers can actually leave the water while still under pressure in order to rest, eat, drink and warm up.
In both wreck and cave settings, there are numerous logistical considerations which are vitally important but too numerous to discuss here. These include thermal protection and temperature management, hydration and nutrition, gas logistics, medical support and evacuation plans. It should be obvious from this discussion that merely training in the technical diving methods described above is only the start of the process of becoming an exploration-level technical diver.
4.5 Current Scope of Technical Diving
The boundary between technical diving and mainstream recreational diving is fluid because technical diving methods and equipment are adopted by and become part of recreational diving [13]. It is difficult to imagine now, but the use of nitrox, presently considered ‘mainstream’ in recreational diving, was viewed as highly technical and fiercely opposed by the recreational diving industry in the early 1990s. In what may prove to be a similar development, there are current plans to develop and promote simplified closed-circuit rebreathers for mainstream recreational diving.
Open-circuit and rebreather trimix dives to a maximum of about 90 msw for bottom times of 30–60 min represent the current state of typical technical diving. Several training agencies specialise in training for this type of diving and several of the large recreational training agencies have also entered this market. Depth record-setting dives (now in excess of 300 msw on open-circuit equipment) typically involve immediate ascent from the maximum depth. However, technical divers are conducting purposeful cave exploration dives in excess of 200-m fresh water (mfw) with substantial bottom times. A notable recent example is the exploration of the Pearse Resurgence cave system in New Zealand to 221 mfw. In addition, some dives of remarkable duration are now being undertaken to explore caves over long distances. The most conspicuous are those conducted by the Woodville Karst Plains Project in northern Florida. This team has conducted exploration out to 7.9 km in Wakulla Springs, a dive requiring 11 h of bottom time at an average depth of 80 mfw, followed by 16 h of decompression.
As technical divers have extended these boundaries deeper and longer, a number of physiological challenges have been pushed into the spotlight, often because of related accidents. This chapter concludes with a more detailed discussion of two such challenges: the respiratory implications of deep diving and issues pertaining to decompression from deep dives.
4.6 Respiratory Challenges of Deep Diving
Breathing in the underwater environment invariably requires greater work to achieve lung ventilation than during breathing at the surface. There are multiple potential contributors to this increased work [14].
First, the use of underwater breathing apparatus imposes an external breathing resistance that is not present during normal ventilation. The degree of impediment depends on the type and design of the device. In general, a well-tuned high-quality open-circuit regulator provides less external resistance than a rebreather device because during inhalation, once the demand valve is tripped, the supplied gas flows relatively freely. In addition, exhalation is via a simple mushroom valve to the external environment. In contrast, in a rebreather the diver must generate all the work necessary to move gas through the hoses, valves and CO2 absorbent. Based on evaluation of the influence of work of breathing on dyspnea and CO2 retention (see later), Warkander et al. (1992) proposed that the external work of breathing for UBA should not exceed 1.5–2.0 J/L in the ventilation range of 30–75 L/min [15].
Second, the increase in gas density that occurs as gas is respired at higher ambient pressure increases the resistance to flow through both the diver’s airways and the orifices, hoses and valves of the UBA. Not only does this further increase work of breathing, it also predisposes to the onset of dynamic airway compression during exhalation at much lower flow rates than normal [16]. Since the pressure drop along the airway occurs more quickly when exhaling a dense gas, the equal pressure point will be reached more proximally and at lower flow rates during a forced exhalation. Not surprisingly, the maximum voluntary ventilation is markedly reduced as depth increases [14]. For example, during air breathing, maximum voluntary ventilation is halved at 4 atm abs (30 msw equivalent) compared to 1 atm abs, even when measured with low-resistance respiratory laboratory equipment. In what is probably a subconscious attempt to reduce dynamic airway collapse, divers breathing dense gas tend to increase their expiratory reserve volume. This increases the calibre of small airways by stretching them, but it also shifts tidal breathing to a less favourable part of the lung compliance curve, further increasing the work of breathing [17].
Third, during immersion there is the potential for development of so-called static lung loads (SLLs). These exist if the gas pressure inside the airway is either higher (positive SLL) or lower (negative SLL) than the external water pressure at the level of the notional lung centroid [18]. For example, in the upright diver using an open-circuit UBA, there will be a negative SLL because the gas is supplied by the regulator at ambient pressure at the depth of the mouth, whereas the lung centroid will be approximately 25 cm H2O deeper. This is similar to head-out immersion. Similarly, a negative SLL exists for a rebreather diver swimming horizontally if the counter-lung is on the back (shallower than the lung centroid). A negative static lung load probably makes premature dynamic airway closure more likely during exhalation [19], and it also promotes engorgement of the distensible pulmonary circulation by blood thus reducing lung compliance and increasing work of breathing [18].
The most important physiological consequence of these changes in work of breathing is disturbance of CO2 homeostasis. In particular, there is a tendency to the development of hypercapnia during diving [14, 20]. The most important contributing factor is probably the increase in work of breathing described above, and this interacts with other physiologic, circumstantial and equipment factors as follows:
First, there appears to be substantial interindividual differences in the behaviour of the respiratory controller when there is an increased requirement for respiratory work to maintain normocapnia. Thus, some subjects maintain normocapnia as the work of breathing increases during a dive, whereas others don’t; it is as though the respiratory controller ‘prefers’ to allow hypercapnia over the alternative of driving the extra work required to keep the PaCO2 normal [21]. This phenomenon is often referred to as ‘CO2 retention’, and vulnerable individuals are deemed to be ‘CO2 retainers’. The tendency is maximally unmasked at precisely the point in the dive when it is most dangerous (at deep depth, breathing dense gas and exercising), and it may be exacerbated by breathing oxygen at an elevated inspired PO2 (which, as previously described, is the norm in technical diving).
Second, in rebreather diving it is possible for the CO2 absorbent to fail to remove all expired CO2 so that CO2 is subsequently re-inhaled. Under normal (non-diving) circumstances, normocapnia can be maintained by an increase in minute volume despite the presence of small amounts of inspired CO2 [22]. However, it is much less likely that such compensation will take place in the diving context where the work of breathing is concomitantly increased. Several rebreather manufacturers have recently incorporated CO2 detectors in the inhale limb of their circuits, but this is far from universal.
Third, there is an increase in physiological dead space during diving and ventilation with hyperoxic gases [23]. The cause is probably multifactorial, though a derangement in V/Q matching is probably the most important contributor. This reduces the efficiency of any increase in ventilation effort during diving and would exacerbate any tendency to hypoventilate in the face of rising CO2.
Finally, a rare potential contributor to disastrous hypercapnia may be encountered by divers visiting the most extreme depths. It relates to the premature onset of dynamic airway compression at very low flow rates when breathing very dense gas, particularly in the presence of a negative static lung load. These conditions can markedly reduce expiratory flow [16], potentially to the point where maximum voluntary ventilation falls below the minute volume required to maintain normocapnia. Under these circumstances the rising PaCO2 will drive more respiratory effort which will serve only to produce more CO2, and the diver can enter a spiral into terminal hypercapnia. This mechanism is thought to have contributed to one widely publicised rebreather diving fatality at 264-mfw depth in which the diver videoed the circumstances of his own death [24]. Other extreme deep divers using rebreathers have reported the onset of characteristic ‘coughing exhalations’ when attempting to exercise at extreme depth [25] and have self-rescued by ceasing exercise and reducing depth.
Hypercapnia is dangerous for several reasons. First it may cause unpleasant symptoms such as dyspnea, headache and confusion which may progress to panic or incapacitation. Notably, it has been repeatedly demonstrated that some divers are poor at recognising the early symptoms and that incapacitation may supervene with little or no warning [26, 27]. Carbon dioxide is a narcotic gas, and its effects will be additive to those of nitrogen narcosis. Finally, hypercapnia increases the risk of cerebral oxygen toxicity, probably by causing cerebral vasodilation and thereby increasing the dose of oxygen to which the brain is exposed [28]. For these reasons, divers undertaking extreme deep dives are advised to minimise exercise during the deep phase of the dive, pay attention to projected gas densities during the planning phases of dives, ensure their equipment is optimally configured to reduce work of breathing and (in rebreather diving) to be sure to replace the CO2 absorbent in a timely manner to ensure maximum efficiency. Rebreathers frequently incorporate a mouthpiece with a ‘bailout valve’ that allows switching to an open-circuit gas supply without removing the mouthpiece, a manoeuvre that has proved impossible for some dyspneic hypercapnic divers to perform [29].
4.7 Decompression from Technical Dives
The putative cause of DCS is excessive formation and growth of bubbles in body tissues as a result of reduction in ambient pressure (decompression). In diving, these bubbles arise from excess gas taken up while breathing compressed gas. For an animal breathing air that has not made an excursion in ambient pressure, the nitrogen in air is dissolved in the body tissues at a concentration proportional to the alveolar nitrogen partial pressure as described by Henry’s law. In this state, the chemical activity of the dissolved nitrogen is described by the partial pressure (P N2) of the gas in the alveoli with which it is in equilibrium. P j is used to describe the chemical activity of any dissolved gas (j), whether or not it is in equilibrium with a gas phase. Thus P j is equivalent to the gas partial pressure that is, or would be required, in a gas phase at equilibrium with the dissolved gas.
During a dive, alveolar inert gas partial pressures will change as a result of the changes in ambient pressure and therefore inspired gas mixture pressure and if the fractions of nitrogen, helium and oxygen in the inspired gas mixture are changed. A change in the alveolar inert gas pressures will result in the transport of that inert gas between lungs and tissues, eventually establishing a new equilibrium where alveolar and tissue partial pressures are again equal. During a typical technical dive, the result will be an increase in the sum of the dissolved gas partial pressures compared to that at the surface. Ascent from a dive can result in ambient pressure falling below the sum of the partial pressures of all gases dissolved in tissue (gas supersaturation):
where the subscript tis refers to gas dissolved in tissue and P H20 is the water vapour pressure at tissue temperature. If gas supersaturation occurs in tissue, bubbles may form.
The sum of all gas partial pressures inside a spherical bubble (P bub) of radius r is given by:
The second term on the right-hand side is the pressure increase across the gas-liquid interface due to surface tension (σ). The last term on the right-hand side is pressure exerted by displaced tissue. Assuming no pressure due to tissue displacement, assuming equilibrium between gas partial pressures inside and outside the bubble and rearranging Eq. 25.2 as an inequality give:
Equation 25.3 indicates that only bubbles above some critical radius can persist for any combination of tissue surface tension and gas supersaturation. A consequence of this is that large supersaturation is required to form bubbles de novo from dissolved gas. Gas supersaturation pressures of 190–300 atm are required to form bubbles from nitrogen or helium dissolved in pure water (which has surface tension of 0.073 N m−1) [30]. These pressures are much higher than ever achieved in human diving. However, in humans, detectable venous gas bubbles follow decompression to sea level from air saturation dives to 3.6 m [31], indicating bubbles can form with supersaturation less than 0.36 atm. Bubbles could only form de novo from dissolved gas at such low supersaturation if tissue surface tensions were lower than have been measured [32]. It is therefore widely accepted that bubble forms at the supersaturation pressures encountered in human diving from pre-existing gas nuclei (theoretical proto-bubbles) [33–35].
Once formed, the bubble will shrink or grow as gas diffuses to or from surrounding tissue according to partial pressure gradients at the bubble surface. This transfer of gas across the bubble surface is given by Fick’s first law:
where V bub is the volume and total gas mixture pressure inside the bubble, D j and α tisj are the bulk diffusivity and solubility of gas j in the tissue, A is the bubble surface area and dP tisj /dr is the gas partial pressure gradient evaluated at the bubble surface.
4.8 Tissue Gas Kinetics
It is clear from the description above that the physiological exchange of gases is relevant to managing the risk of DCS. This gas exchange is covered in detail elsewhere [14] and will only be summarised here. Oxygen can only be safely breathed over a relatively narrow range of inspired partial pressures, and tissue oxygen partial pressure, along with carbon dioxide partial pressure, typically varies over a narrow range determined by tissue metabolic needs. As a result, it is common to consider tissue oxygen and carbon dioxide partial pressures, along with water vapour pressure, as fixed. On the other hand, inert gases vary considerably.
Equilibration of arterial blood to changes in inspired helium or nitrogen partial pressures is sufficiently rapid that, over a time course relevant to decompression physiology, arterial blood can be considered in equilibrium with inspired gas. Blood-tissue exchange is typically described using a single-compartment kinetic model in which P tisj is each represented by a single, time-varying partial pressure, and arterial-tissue inert gas partial pressure difference (P a − P tis) declines mono-exponentially. Underlying this assumption of compartmental models is that, owing to rapid diffusion, equilibration of inert gas partial pressure gradients across the tissue region represented by the compartment is much faster than transport in and out of the compartment. The rate of change of compartmental partial pressure is given by:
where the second term on the right-hand side accommodates transfer of gas between tissue and bubble and vanishes if there is no bubble.
Tissue perfusion is the principal factor determining equilibration of tissues with inspired inert gases, and therefore the time constant τ is usually defined y:
where V tis is tissue volume, Q tis is tissue blood flow and α tis/α blood is the tissue–blood gas partition coefficient. Diffusion-limited gas uptake may occur in poorly vascularised or avascular areas of the body that are relevant to DCS, such as articular cartilage and synovium [36] or the perilymph and endolymph spaces of the inner ear [37]. In decompression physiology it is common to characterise gas exchange using the half-time which is equal to ln(2)τ.
4.9 Decompression Algorithms
To minimise the risk of DCS, decompressions are conducted according to pressure/time/breathing gas decompression schedules that control the rate of decompression. In diving practice, the rate of decompression is typically controlled by interrupting ascent with ‘decompression stops’, by convention, at 10-fsw (3 msw) increments. Decompression proceeds by ascending to establish a gradient between alveolar and tissue inert gas partial pressures, and decompression stops are taken to allow washout of tissue inert gas limit tissue gas under conditions of limited supersaturation and consequent bubble formation. Successively shallower decompression stops may include switches to progressively higher oxygen fraction breathing gases (in accord with a maximum safe inspired oxygen partial pressure) to increase the alveolar–tissue inert gas partial pressure gradient. These decompression schedules are derived from decompression algorithms that exercise models of bubble formation and/or tissue gas uptake and washout.
Whereas early recreational divers were able to adopt readily available, military air decompression tables which were validated against databases of dives with known outcomes, no such trimix tables were available to early technical divers. Instead, technical divers implemented decompression algorithms which had, or in some cases were adapted to have, a structure that can accommodate the use of trimix breathing gases. The following is a brief account of the principal features of decompression algorithms available to technical divers. Decompression models and algorithms are more completely reviewed elsewhere [38].
4.9.1 Gas-Content Decompression Algorithms
Gas-content algorithms track the uptake and elimination of inert gas in notional tissue compartments with different gas kinetic properties and schedule decompression stops to limit the degree and duration of supersaturation. For instance, the most prevalent decompression algorithms are simply Eq. 25.5 (with no bubble) and specified maximum permissible supersaturations in the corresponding compartment. Since the tissue sites relevant to DCS are unknown, it is common to model collection of such compartments, each with a different half-time chosen to span some range thought to encompass all relevant tissues. This parallel compartment approach dates to Haldane and colleagues who produced the first decompression model and decompression schedules in the early twentieth century [39].
The earliest technical divers used custom trimix decompression tables prepared for them by R.W. Hamilton using a proprietary software (DCAP) implementation of the Tonawanda II decompression algorithm and the 11-F6 M-value matrix [40]. M-values specify the maximum permissible gas partial pressures at given decompression stop depths in the model compartments [41] and are a common method for specifying the maximum permissible supersaturation. Almost immediately thereafter, technical divers began implementing the Buhlmann ZH-L16 decompression algorithm, descriptions of which were readily available in the open scientific literature [42–44]. To accommodate trimix diving, both of these algorithms track helium and nitrogen independently in each compartment. In Tonawanda II, some compartments have a different half-time for helium than for nitrogen, and in ZH-L16 all compartments have nitrogen half-times that are 2.65-fold longer than helium half-times.
4.9.2 Bubble Decompression Algorithms
There are two general classes of bubble decompression algorithms, although they have overlapping aspects. One class calculates bubble size using equations of bubble growth and resolution due to gas diffusion between bubbles and the surrounding tissue [45, 46]. The second class of algorithms is much simpler, focusing on predictions of the number of bubbles that form during decompression [47]. These latter bubble-counting algorithms will be outlined here because they are widely available to technical divers [48, 49].
The varying permeability model (VPM) assumes a population of spherical gas nuclei, stabilised by a coating of surface-active agents, and a theoretical distribution of their radii that, along with Eq. 25.3, is used to calculate the number of gas nuclei activated into growing bubbles by the maximum supersaturation encountered during decompression [47]. In the simplest form of the VPM algorithm, decompression can be controlled by a predicted maximum allowed number of bubbles and, therefore, a maximum allowed supersaturation. Alternatively, the number of bubbles is converted to a simple index representing the number of bubbles and their growth by multiplying the number of bubbles by the time integral of supersaturation. The allowed supersaturation is that which, if sustained throughout the ascent, results in the target value of this bubble index. The parameters of the VPM algorithm were originally adjusted to give decompression times similar to existing military decompression tables [47].
4.9.3 Implementation and Availability of Decompression Algorithms for Technical Diving
Decompression algorithms may be used to produce a printed schedule (or ‘table’ of many schedules) that must be adhered to during the dive. There are several commercially available software implementations of the decompression algorithms that run on microcomputers (desktop decompression software) and which technical divers use to generate printed decompression schedules. Such software allows the user to tailor the decompression schedule to the depth/time/breathing gas plan intended to be used. Alternatively, decompression algorithms used by technical divers are also programmed into diver-carried dive computers.
Both Tonawanda II-11F6 and ZH-L16 are available in desktop decompression software, and ZH-L16 is also implemented in several dive computers used by technical divers. The ZH-L16 algorithm is probably the more widely used of the two gas-content algorithms, but the original parameterisation is rarely used by technical divers. Instead, ZH-L16 is modified by the end user, often using ‘gradient factors’. In this usage, gradient refers, unconventionally (because it is not a gradient), to the difference between ambient pressure and an algorithm M-value [49, 50]. Supersaturation is limited to a fraction of the difference between ambient pressure and the original M-value. These fractions have come to be known as gradient factors [50]. Thus, if a diver elects to limit supersaturation to 80 % of the usual difference between ambient pressure and the M-value, this is referred as ‘gradient factor 80’ (GF 80). Typical proprietary implementations of the gradient factor method require the diver to select two gradient factors: the ‘low’ gradient factor modifies permitted supersaturation at the deepest decompression stop, and the ‘high’ controls supersaturation at the point of surfacing. The algorithm then interpolates a series of modified M-values in between these two user-specified points. If the first gradient factor is set less than 100 %, this forces deeper stops to limit supersaturation in the fast tissues early in the ascent, and setting the second gradient factor to less than 100 % will produce longer shallower stops to reduce supersaturation in the slower tissues in the latter phase of the ascent. A gradient factor higher than 100 % can be used to allow greater supersaturation and therefore shorter decompression stops than the original algorithm.
Several derivatives of VPM are available as desktop decompression software or programmed into dive computers. VPM-B is probably the most widely used variant [51]. Implementations of the VPM model for technical diving have a compartment structure similar to the ZH-L16 in which helium and nitrogen half-times differ in each compartment [51]. Most implementations have user-adjustable parameters that result in longer or shorter decompression times.
4.10 Technical Diving Decompression Schedules Are Not Validated
The decompression procedures promulgated by well-resourced organisations (e.g. the US Navy) are developed and validated in conjunction with human dive trials in which the conditions that influence the risk of decompression sickness (DCS) are well documented, the depth/time/breathing gas profiles are accurately recorded and the schedule prescribed by the algorithm and dive outcomes (typically DCS or not) are known. In the development phase, decompression algorithm parameters are found by prospective trial-and-error testing of dives that accurately follow the prescription of the decompression algorithm or by formal statistical fit of decompression models to existing databases of well-documented dives. The final decompression algorithm is validated by comparison to other man dives. The development and validation man dives are conducted under conditions similar to the intended use of the procedures. The final decompression schedules, either in the form of tables or as an algorithm programmed in a dive computer, are associated with rules that confine the routine use of the decompression algorithm to a domain in which it has been tested.
This approach is necessary because the bubble-tissue interactions that result in DCS have not been observed, and the tissues in which bubble injury manifests as DCS are sometimes uncertain. Consequently, the relevant gas uptake and washout, bubble formation and growth have not been measured, and these processes are represented with latent variables in decompression models. Furthermore, many factors known to influence the risk of DCS (such as diver work rate and thermal status) are not accommodated in the decompression algorithms. The decompression algorithms that result from manned development and validation are embodiments of the development data and are not intended for, and indeed do not extrapolate well to, all types of diving.
In contrast to the approach outline above, the decompression schedules used by technical divers have not been formally validated. First, the underlying decompression algorithms have not been developed and validated with the types of dives conducted by technical divers. Both Tonawanda II-11F6 and ZH-L16 were developed in association with laboratory testing, but few of these dives were relevant to technical diving. For instance, development of ZH-L16 included many man dives, although most were substantially shallower or deeper than the 60–90-m sea water (msw) typical of technical diving, and there were few trimix dives [44]. To our knowledge there is no formal validation of VPM-based technical diving decompression schedules. Second, technical divers rarely use schedules generated using the original parameterisations of these decompression algorithms but instead employ various end-user adjustments.
Early use of the original parameterisation of ZH-L16 was perceived to have an unacceptably high incidence of DCS. Indeed the only study documenting DCS incidence in technical diving, although very small, supports this notion [52]. Such perceptions lead to modifications such as gradient factors (see above). The original version of VPM has also largely been superseded by the more conservative derivative VPM-B, which itself is not a single algorithm but has user-adjustable parameter settings that make it more or less conservative. Other changes to decompression procedures have been driven by the belief that they will minimise time spent decompressing while at the same time maintaining an acceptably low risk of DCS (though none have been tested to prove this).
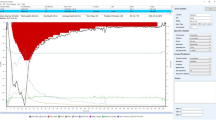
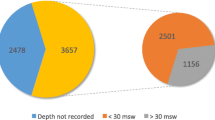
Some have suggested that the evolution of technical diving decompression procedures represent selection of improved practice through natural experiment. However, there clearly has been no community-wide experiment, most importantly because no data comparing different technical diving decompression procedures has been collected. The required data to evaluate decompression procedures are high-fidelity recordings of depth/time/breathing gas history and a measure of outcome (typically DCS or not). While there are some databases of depth/time recordings uploaded from dive computers which provide useful snapshots of relatively recent practice, these recordings are not accompanied by any outcome measure. Individuals or small groups have modified decompression practice based on their personal observations, and some of these changes have influenced changing fashions in the technical diving community. In this context it is worth exploring some areas where emerging evidence contradicts some assumptions of technical diving decompression practice.
4.10.1 Deep Stops
A characteristic of bubble algorithms is they typically prescribe deeper decompression stops than gas-content algorithms [47, 53]. In simple terms, bubble decompression algorithms favour deeper stops to limit supersaturation and thereby bubble formation early in the decompression, whereas traditional gas-content decompression algorithms favour a more rapid ascent to maximise the alveolar–tissue gradient of inert gas partial pressures to maximise tissue inert gas washout. Deep stops came to the attention of early technical divers in the form of empirical ‘Pyle stops’, a practice serendipitously developed by ichthyologist and technical diving pioneer Richard Pyle, arising from a requirement to vent the swim bladders of fish specimens collected at great depth before arriving at his first decompression stop. Pyle stops are one or more decompression stops performed deeper than the deepest stop prescribed by a gas-content algorithm and are followed by completing the longer decompression prescribed by the algorithm incorporating this extra time at depth [54]. There followed a strong trend towards the adoption of bubble algorithms and also for the use of manipulation of gradient factors to force gas-content algorithms to impose deep stops. Based largely on supportive anecdote, a widespread belief emerged among technical divers that deep-stop decompression schedules are more efficient than shallow-stop schedules. Efficiency, in this context, means that a schedule of the same or even shorter duration has a lower risk of DCS than some alternative schedule.
The few studies available at the time of adoption of deep stops by technical divers [53, 55] have been interpreted to support this notion. The earliest of these papers, an observational study of the practices of pearl divers in the Torres Strait of Australia [53], often cited as unqualified support for deep stops, is difficult to obtain and worth summarising here. These pearl divers performed air dives to depths up to 80 msw followed by empirically derived decompression schedules that had deeper stops and were somewhat shorter than accepted navy decompression schedules. Thirteen depth/time recordings were made of such dives, and these dives resulted in six cases of DCS (46 % incidence). The remaining data was a count of dives performed from four fishing vessels over a 2-month period, and these 468 man dives resulted in 31 reported cases of DCS (7 % incidence). It takes a certain cognitive dissonance to interpret these high incidences of DCS as supporting a deep-stop approach. The later of these papers used the then new method of ultrasonic VGE detection, and measurements were made during decompression from dry chamber dives (where chamber occupants are exposed to hyperbaric gas pressures). Fewer VGE were detected in five subjects whose decompression includes an additional decompression stop 10-fsw deeper than the schedules followed by other subjects [55]. The relevance of this observation to DCS is uncertain, because it is unknown if the difference in VGE grades persisted after surfacing, and it is the peak VGE grade, usually occurring 1–2 h after surfacing, that is (weakly) associated with the incidence of DCS [56]. Recently, however, evidence has been accumulating from comparative trials that shows deep stops are not more efficient, and possibly less efficient, than shallow stops. Several studies have shown no difference in VGE after deep-stop or shallow-stop decompression from air or trimix decompression dives [57–59], although it should be noted that these studies were underpowered. One large study has shown a higher incidence of DCS following deep stops than following shallow-stop decompression from air dives [60].
4.10.2 Multiple Inert Gases
In the Buhlmann ZH-L16 gas-content decompression model [43], each of the 16 compartments has a half-time for helium that is 2.65-fold shorter than the corresponding nitrogen half-time. These, or similar, compartment half-times are used in most decompression models available to technical divers. As a result of these compartment half-times, such decompression models will prescribe less decompression for a bounce dive conducted breathing nitrox or trimix than for a dive conducted breathing heliox because of a slower uptake of nitrogen than helium [44]. Faster uptake results in a deeper first stop and therefore longer decompression. Similarly, such decompression models will prescribe shorter decompressions if switching to nitrox breathing during decompression from a heliox or trimix dive [44].
It is not clear that the apparent differences in bounce diving decompression resulting from different inert gases are real. Direct measurement of helium and nitrogen exchange rates in faster exchanging tissues relevant to bounce diving indicates very similar rates of exchange for nitrogen and helium [14]. These latter data suggest heliox, nitrox and trimix decompression from bounce dives of the same depth and duration should be similar, and this is supported by comparison of nitrox and heliox no-stop dives [61]. Experiments comparing dives with heliox-to-air gas switching to dives with all heliox decompression are confounded by different decompression schedules and small numbers of dives, particularly on the schedules that provoked DCS [44]. On the other hand, a US Navy man trial indicates that a heliox-to-nitrox switch does not accelerate decompression [62].
4.11 Decompression Sickness in Technical Divers
The pathophysiology and manifestations of DCS in technical divers are the same as for any other diving communities. However, one manifestation of DCS that appears to be associated with very deep decompression dives is injury to the vestibulocochlear apparatus (inner-ear DCS), characterised by nausea, vertigo and hearing loss, often with no other manifestations. This is of particular concern to technical divers because symptoms characteristically onset during decompression and are life threatening for a SCUBA diver who must choose between the risk of drowning or omitting a substantial decompression obligation [37].
Inner-ear DCS during decompression from deep heliox dives characteristically follows switching to nitrox breathing gas (e.g. air) [63–65]. Symptoms of injury to the vestibulocochlear apparatus have occurred after breathing nitrogen-rich gas mixtures during deep heliox chamber dives, without any change in depth [66]. This latter finding is explained by a physiological model of the inner ear which indicates that following a switch from a helium-rich to a nitrogen-rich breathing mixture, transient supersaturation can develop in the vascularised membranous labyrinth without any change in depth, principally due to diffusion of helium from the endolymph and perilymph exceeding the counter-diffusion of nitrogen in the opposite direction [37]. This effect is opposite to the predictions of all decompression algorithms available to technical divers, in which a helium-to-nitrogen switch will result in a transient undersaturation, as noted in the preceding section.
The actual contribution of gas switches to inner-ear DCS during decompression from technical dives is uncertain. The inner-ear model [37] predicts substantial pre-existing supersaturation in the inner ear during decompression from such dives and that the counter-diffusion of gases following a helium-to-nitrogen mix gas switch makes only a small contribution to the total supersaturation at the depths where such switches are usually made.
Inner-ear DCS, without other symptoms, also occurs following relatively shallow air or nitrox dives, and among such cases there is a high prevalence of major right to left shunting of venous bubble contrast, demonstrated using transcranial Doppler sonography [67, 68]. This association suggests that inner-ear DCS might be caused by passage of arterialised venous bubbles into the labyrinthine artery. These divers frequently do not develop cerebral manifestations despite the fact that if bubbles reach the labyrinthine artery they must also distribute widely in the brain because the labyrinthine artery is usually a tiny branch of the much larger basilar artery. The selective vulnerability of the inner ear in this setting may relate to slower inert gas washout, and therefore more prolonged supersaturation, in the inner ear than the brain. Under these circumstances, small arterial bubbles reaching the inner ear are more likely to grow and cause symptoms than bubbles reaching the brain [69].
This mechanism may also be relevant to the onset of inner-ear DCS at depth during decompression, when inner-ear symptoms characteristically occur in technical diving. Thus, it is possible that arterialised VGE could reach the inner-ear microcirculation at a time during decompression when substantial supersaturation is predicted [37]. It may be coincidental that gas switches are often made at a time when the inner ear is supersaturated, or it may be that these bubbles can grow more quickly following a nitrogen-to-helium switch because of the greater flux of helium into the vascular tissue than removal of nitrogen, as previously described.
References
Mitchell SJ, Doolette DJ. Recreational technical diving part 1. An introduction to technical diving. Diving Hyperb Med. 2013;43:86–93.
Doolette DJ, Mitchell SJ. Recreational technical diving part 2. Decompression from deep technical dives. Diving Hyperb Med. 2013;43:96–104.
Molvaer O. Otorhinolaryngological aspects of diving. In: Brubakk AO, Neuman TS, editors. The physiology and medicine of diving. Edinburgh: Saunders; 2003. p. 227–64.
Neuman TS. Arterial gas embolism and pulmonary barotrauma. In: Brubakk AO, Neuman TS, editors. The physiology and medicine of diving. Edinburgh: Saunders; 2003. p. 557–77.
Vann RD, Hamilton RW. Central nervous system oxyen toxicity In: Vann RD, Mitchell SJ, Denoble PJ, Anthony TG, editors. Technical diving conference proceedings. Durham: Divers Alert Network; 2009. p. 38–66.
Bennett PB, Mitchell SJ. Nitrogen narcosis, oxygen narcosis, and the high pressure nervous syndrome. In: Vann RD, Mitchell SJ, Denoble PJ, Anthony TG, editors. Technical diving conference proceedings. Durham: Divers Alert Network; 2009. p. 67–98.
Francis TJR, Mitchell SJ. Pathophysiology of decompression sickness. In: Brubakk AO, Neuman TS, editors. The physiology and medicine of diving. Edinburgh: Saunders; 2003. p. 530–56.
Vann RD, Butler FK, Mitchell SJ, Moon RE. Decompression illness. Lancet. 2011;377:153–64.
Francis TJR, Mitchell SJ. Manifestations of decompression disorders. In: Brubakk AO, Neuman TS, editors. The physiology and medicine of diving. Edinburgh: Saunders; 2003. p. 578–99.
Richardson D. Training scuba divers: a fatality and risk analysis. In: Vann RD, Lang MA, editors. Recreational diving fatalities. Proceedings of the Divers Alert Network 2010 April 8–10 workshop. Durham: Divers Alert Network; 2011. p. 119–64.
Ladd G, Stepan V, Stevens L. The abacus project: establishing the risk of recreational scuba death and decompression illness. SPUMS J. 2002;32:124–8.
Fock AW. Analysis of closed-circuit rebreather deaths 1998–2010. Diving Hyperb Med. 2013;43:78–85.
Richardson D. Taking ‘tec’ to ‘rec’: the future of technical diving. SPUMS J. 2003;33:202–5.
Doolette DJ, Mitchell SJ. Hyperbaric conditions. Compr Physiol. 2011;1:163–201.
Warkander DE, Norfleet WT, Nagasawa GK, Lundgren CEG. Physiologically and subjectively acceptable breathing resistance in divers’ breathing gear. Undersea Biomed Res. 1992;19:427–45.
Wood LDH, Bryan AC. Effect of increased ambient pressure on flow volume curve of the lung. J Appl Physiol. 1969;27:4–8.
Hesser CM, Linnarsson D, Fagraeus L. Pulmonary mechanics and work of breathing at maximal ventilation and raised air pressure. J Appl Physiol. 1981;50:747–53.
Lundgren CEG. Immersion effects. In: Lundgren CEG, Miller JN, editors. The lung at depth. New York: Marcel Decker; 1999. p. 91–128.
Koulouris NG, Valta P, Lavoie A, Corbeil C, Chasse M, Braidy J, Milic-Emili J. A simple method to detect expiratory flow limitation during spontaneous breathing. Eur Respir J. 1995;8:306–13.
Moon RE, Cherry AD, Stolp BW, Camporesi EM. Pulmonary gas exchange in diving. J Appl Physiol. 2009;106:668–77.
Poon CS. Ventilatory control in hypercapnia and exercise: optimization hypothesis. J Appl Physiol. 1987;62:2447–59.
Camporesi EM, Bosco G. Ventilation, gas exchange, and exercise under pressure. In: Brubakk AO, Neuman TS, editors. Bennett and Elliott’s physiology and medicine of diving. 5th ed. Edinburgh: Saunders; 2003. p. 77–114.
Mummery HJ, Stolp BW, deL Dear G, Doar PO, Natoli MJ, Boso AE, Archibold JD, Hobbs GW, El-Moalem HE, Moon RE. Effects of age and exercise on physiological dead space during simulated dives at 2.8 atm abs. J Appl Physiol. 2003;94:507–17.
Mitchell SJ, Cronje F, Meintjes WAJ, Britz HC. Fatal respiratory failure during a technical rebreather dive at extreme pressure. Aviat Space Environ Med. 2007;78:81–6.
Harris R. Rebreathers: overcoming obstacles in exploration. In: Vann RD, Denoble PJ, Pollock NW, editors. Rebreather forum 3 proceedings. Durham: AAUS/DAN/PADI; 2014. p. 56–61.
Warkander DE, Norfleet WT, Nagasawa GK, Lundgren CE. CO2 retention with minimal symptoms but severe dysfunction during wet simulated dives to 6.8 atm abs. Undersea Biomed Res. 1990;17:515–23.
Shykoff BE, Warkander DE. Exercise carbon dioxide (CO2) retention with inhaled CO2 and breathing resistance. Undersea Hyperb Med. 2012;39:815–28.
Lambertsen CJ, Ewing JH, Kough RH, Gould R, Stroud MW. Oxygen toxicity. Arterial and internal jugular blood gas composition in man during inhalation of air, 100% O2 and 2% CO2 in O2 at 3.5 atmospheres ambient pressure. J Appl Physiol. 1955;8:255–63.
Trytko B, Mitchell SJ. Extreme survival: a deep technical diving accident. SPUMS J. 2005;35:23–7.
Hemmingsen EA. Cavitation in gas-supersatured solutions. J Appl Phys. 1975;46:213–8.
Eckenhoff RG, Olstad CS, Carrod G. Human dose-response relationship for decompression and endogenous bubble formation. J Appl Physiol. 1990;69:914–8.
Weathersby PK, Homer LD, Flynn ET. Homogenous nucleation of gas bubbles in vivo. J Appl Physiol. 1982;53:940–6.
Evans A, Walder DN. Significance of gas micronuclei in the aetiology of decompression sickness. Nature. 1969;222:251–2.
McDonough PM, Hemmingsen EA. Bubble formation in crustaceans following decompression from hyperbaric gas exposure. J Appl Physiol. 1984;56:513–9.
Vann RD, Grimstad J, Nielsen CH. Evidence for gas nuclei in decompressed rats. Undersea Biomed Res. 1980;7:107–12.
Weathersby PK, Meyer P, Flynn ET, Homer LD, Survanshi S. Nitrogen gas exchange in the human knee. J Appl Physiol. 1986;61:1534–45.
Doolette DJ, Mitchell SJ. A biophysical basis for inner ear decompression sickness. J Appl Physiol. 2003;94:2145–50.
Tikuisis P, Gerth WA. Decompression theory. In: Brubakk AO, Neuman TS, editors. Bennett and Elliott’s physiology and medicine and diving. 5th ed. Edinburgh: Saunders; 2003. p. 419–54.
Boycott AE, Damant GCC, Haldane JS. The prevention of compressed-air illness. J Hygiene (Lond). 1908;8:342–443.
Hamilton RW, Turner P. Decompression techniques based on special gas mixes for deep cave exploration [Abstract]. Undersea Biomed Res. 1988;15(Suppl):70.
Workman RD. Calculation of decompression schedules for nitrogen-oxygen and helium oxygen dives. Research Report. Washington, DC: Navy Experimental Diving Unit; 1965. Report No: 6–65.
Bühlmann AA. Experimentalle Grundlagen der risikoarmen Dekompression nach Überdruckexpositionen. Schweiz Med Wochenschr. 1982;112:48–59.
Bühlmann AA. Die Berechnung der risikoarmen Dekompression. Schweiz Med Wochenschr. 1988;118:185–97.
Buhlmann AA. Decompression – decompression sickness. In: Michel GPt, editor. Berlin: Springer; 1984.(English translation of Dekompression – dekompressionkrankheit, first published 1983).
Gernhardt ML. Development and evaluation of a decompression stress index based on tissue bubble dynamics [Thesis]. Philadelphia: University of Pennsylvania; 1991.
Gerth WA, Vann RD. Probabilistic gas and bubble dynamics models of decompression sickness occurrence in air and N2-O2 diving. Undersea Hyperb Med. 1997;24:275–92.
Yount DE, Hoffman DC. On the use of a bubble formation model to calculate diving tables. Aviat Space Environ Med. 1986;57:149–56.
Yount DE, Maiken EB, Baker EC. Implications of the varying permeability model for reverse dive profiles. In: Lang MA, Lehner CE, editors. Proceedings of the reverse dive profiles workshop; 1999 Oct 29–30; Washington DC. Washington, DC: Smithsonian Institution; 2000. p. 29–60.
Wienke BR. Reduced gradient bubble model. Int J Biomed Comput. 1990;26:237–56.
Baker EC. Clearing up the confusion about “deep stops”. Immersed. 1998;3:23–31.
Baker EC. Varying permeability model (VPM) decompression program in FORTRAN with Boyle’s law compensation algorithm (VPM-B) [Internet]. cited 20 Jan 2004. 2003. Available from URL: ftp://decompression.org/Baker.
Doolette DJ. Decompression practice and health outcome during a technical diving project. SPUMS J. 2004;34:189–95.
LeMessurier DH, Hills BA. Decompression sickness: a thermodynamic approach arising from a study of Torres Strait diving techniques. Hvalradet Skrifter. 1965;48:84.
Pyle RL. The importance of deep safety stops: rethinking ascent patterns from decompression dives. SPUMS J. 1997;27:112–5.
Neuman TS, Hall DA, Linaweaver PG. Gas phase separation during decompression in man: ultrasound monitoring. Undersea Biomed Res. 1976;3:121–30.
Nishi RY, Brubakk AO, Eftedal OS. Bubble detection. In: Brubakk AO, Neuman TS, editors. Bennett and Elliott’s physiology and medicine of diving. 5th ed. Edinburgh: Saunders; 2003. p. 501–29.
Blatteau JE, Hugon M, Gardette B, Sainty JM, Galland FM. Bubble incidence after staged decompression from 50 or 60 msw: effect of adding deep stops. Aviat Space Environ Med. 2005;76:490–2.
Blatteau JE, Hugon M, Gardette B. Deeps stops during decompression from 50 to 100 msw didn’t reduce bubble formation in man. In: Bennett PB, Wienke BR, Mitchell SJ, editors. Decompression and the deep stop. Proceedings of the Undersea and Hyperbaric Medical Society Workshop; 2008 Jun 24–25; Salt Lake City (UT). Durham: Undersea and Hyperbaric Medical Society; 2009. p. 195–206.
Gutvik CR, Dunford RG, Dujic Z, Brubakk AO. Parameter estimation of the Copernicus decompression model with venous gas emboli in human divers. Med Biol Eng Comput. 2010;48:625–36.
Doolette DJ, Gerth WA, Gault KA. Redistribution of decompression stop time from shallow to deep stops increases incidence of decompression sickness in air decompression dives. Technical Report. Panama City: Navy Experimental Diving Unit; 2011 Report No: NEDU TR 11-06.
Hamilton RW, Thalmann ED, Flynn ET, Temple DJ. No-stop 60 fsw wet and dry dives using air, heliox, and oxygen-nitrogen mixtures. Data report on projects 88-06 and 88-06A. Technical Report. Silver Spring: Naval Medical Research Center; 2002. Report No: 2002-002.
Survanshi SS, Parker EC, Gummin DD, Flynn ET, Toner CB, Temple DJ, et al. Human decompression trial with 1.3 ATA oxygen in helium. Technical Report. Bethesda: Naval Medical Research Institute; 1998. Report No: 98-09. 80 p.
Farmer JC, Thomas WG, Youngblood DG, Bennett PB. Inner ear decompression sickness. Laryngoscope. 1976;86:1315–27.
Bennett PB, Vann RD, Roby J, Youngblood D. Theory and development of subsaturation decompression procedures for depths in excess of 400 feet. In: Shilling CW, Beckett MW, editors. Underwater Physiology VI. Proceedings of the Proceedings of the 6th Symposium on Underwater Physiology. Bethesda: Federation of American Societies for Experimental Biology; 1978. p. 367–81.
Bühlmann AA, Gehring H. Inner ear disorders resulting from inadequate decompression “vertigo bends”. In: Lambertsen CJ, editor. Underwater Physiology V. Proceedings of the Proceedings of the 5th Symposium on Underwater Physiology. Bethesda: FASEB; 1976. p. 341–7.
Lambertsen CJ, Idicula J. A new gas lesion syndrome in man, induced by “isobaric gas counterdiffusion”. J Appl Physiol. 1975;39:434–43.
Cantais E, Louge P, Suppini A, Foster PP, Palmier B. Right-to-left shunt and risk of decompression illness with cochleovestibular and cerebral symptoms in divers: case control study in 101 consecutive dive accidents. Crit Care Med. 2003;31:84–8.
Klingmann C. Inner ear decompression sickness in compressed-air diving. Undersea Hyperb Med. 2012;39:589–94.
Mitchell SJ, Doolette DJ. Selective vulnerability of the inner ear to decompression sickness in divers with right to left shunt: the role of tissue gas supersaturation. J Appl Physiol. 2009;106:298–301.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Mitchell, S.J., Doolette, D.J. (2017). Extreme Scuba Diving Medicine. In: Feletti, F. (eds) Extreme Sports Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-28265-7_25
Download citation
DOI: https://doi.org/10.1007/978-3-319-28265-7_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28263-3
Online ISBN: 978-3-319-28265-7
eBook Packages: MedicineMedicine (R0)