Abstract
Radial head fracture is the most common elbow fracture in adults.
The most common traumatic mechanism is a fall onto the outstretched hand with the elbow partially flexed and the forearm in pronation.
Many factors should be considered in the decision-making process to ensure optimal outcomes. The characteristics of the radial head fracture, including the number and displacement of the fragments, articular surface involvement, and bone quality, all influence the treatment.
A variety of treatment options are used, including early motion with nonsurgical treatment or with a surgery by the fragment excision, radial head excision, repair, and replacement. The principal goals of all the treatments are to restore the elbow motion, and in case of the surgical treatment, the primary aims are to restore the anatomy and the articular congruity.
The rehabilitation program of radial head fractures depends primarily on the presence of associated osseous and ligamentous injuries (simple or complex fractures, respectively) and if the patient has undergone surgery or not.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Radial Head
- Comminuted Radial Head Fractures
- Lateral Collateral Ligament
- Mason Type
- Average Mayo Elbow Performance Score
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Radial head fracture is the most common elbow fracture in adults. Its incidence ranges from 1.7% to 5.4% of all adult fractures (Harrington and Tountas 1981; Mason 1954; Herbertsson et al. 2004a; Tejwani and Mehta 2007; Duckworth et al. 2012a; Kaas et al. 2010), and approximately 85% of these fractures occur in active individuals (from 20 to 60 years old).
The most common traumatic mechanism is a fall onto the outstretched hand with the elbow partially flexed and the forearm in pronation. This position results in axial force transmission from the hand, through the wrist and forearm, and it is related to an impaction of the radial head against the capitellum. It may also occur from direct or penetrating trauma or as consequences of a high-energy trauma.
The fracture pattern ranges from non-displaced to comminuted radial head fractures may be an isolated fracture, but more frequently it is a part of a complex injury (complex elbow dislocation) in association with other elbow fractures (the olecranon fracture with or without the coronoid fracture), ligament injuries (the lateral collateral ligament, the medial collateral ligament), or an elbow dislocation.
Many treatment options exist, including nonoperative management, internal fixation, arthroplasty, and resection.
2 The Anatomy and Biomechanical Roles of the Radial Head
The radial head aspect is a disc-shaped structure approximately 3.5 mm thick. It is not round and shows significant difference between orthogonal diameters as ovoid rather than circular (2.5 cm longer in the anteroposterior plane and 2.2 cm in the coronal plane).
It has a shallow proximal depression covered by hyaline cartilage articulating with the capitellum as well as the 250 degrees arc of circumference that articulates with the lesser sigmoid notch; the remaining part of the circumference is not involved in the forearm rotation, and it is not entirely covered by the hyaline cartilage. This area is called “safe zone,” and it is the place where the internal fixation devices are best applied (Smith and Hotchkiss 1996).
The lateral collateral complex and the annular ligament are important stabilizers of the proximal radius. In particular the annular ligament allows the rotation but prevents proximal migration of the radius contrasting the biceps forces that are present during the elbow flexion.
Biomechanical studies have reported as the radial head has an important role in the elbow and forearm stabilizer. Morrey et al. (1991) demonstrated that the radial head serves as a secondary constraint of the elbow to valgus stress, in association with the anterior bundle of the medial collateral ligament (Fig. 13.1).
Radio-capitellar joint congruency also helps to stabilize the joint; it resists external valgus forces and serves as a mechanical block to proximal migration of the radius (longitudinal stability of the forearm).
Load transmission from the wrist to the elbow occurs through the radius, the ulna, the interosseous membrane, and the triangular fibrocartilage complex (Morrey et al. 1988; Rabinowitz et al. 1994) (Fig. 13.2). The radius transfers more than 60% of the forearm loads (Morrey et al. 1988; Hotchkiss 1997; Rozental et al. 2003).The most force is transmitted to the radial head with the elbow extended and forearm pronated (Morrey et al. 1988).
If the interosseous membrane and the ligaments of the distal radioulnar joint are damaged from injury, the radius will migrate proximally, and the longitudinal and distal radioulnar dissociation occurs (Sowa et al. 1995; Hotchkiss 1994). Shepard et al. (2001) observed as for each millimeter of radial shortening, the distal ulnar load increases by approximately of the 10%.
In case of radial head excision, the transfer load changed, and the forces are transferred to the ulna from the distal radius through the interosseous membrane so the tension in the medial collateral ligament increases when a valgus stress is applied (Hotchkiss and Weiland 1987; O’Driscoll et al. 1991; Beingessner et al. 2004).
3 The Clinical Assessments
A spectrum of injury patterns often occurs in association with radial head fractures. A systematic clinical assessment is required to identify associated fractures and ligament injuries. Although tenderness over the radial head is ordinary, tenderness at other sites can be related to the presence of an associated injury.
Pain over the lateral epicondyle might indicate lateral collateral ligament injury, and over the sublime tubercle or the medial epicondyle might indicate a medial collateral ligament injury.
Pain and tenderness at the distal radioulnar joint or in the forearm should be related to an axial instability as in an Essex-Lopresti lesion (Essex-Lopresti 1951).
The range of motion in both planes will be reduced due to the presence of an intra-articular hematoma; limitation of forearm rotation can be due to a mechanical block from a displaced radial head fracture with the fragments that caused an impingement with lesser sigmoid notch or with the capitellum articular surfaces.
In acute lesions, the stability tests are often not possible without anesthesia.
4 The Imaging Assessments
The X-rays performed in the orthogonal planes with the addition of oblique views are important to define the radial head fracture and other bone injuries.
The X-rays have been used also to analyze the aspects of the capitellum, trochlea, and coronoid. Incongruence of the radio-capitellar or ulno-humeral joints suggests concomitant ligamentous injuries. In particular comminuted radial head fractures can be associated with coronoid fractures and ligamentous injuries as in the case of terrible triad lesion.
Computed tomography is particularly useful to better characterize fracture types. It is helpful to quantify the displacement, and it allows a better assessment of the reparability of the fracture fragments (Guitton et al. 2010) (Fig. 13.3).
Magnetic resonance imaging can provide more information regarding associated soft tissue injuries of the collateral ligaments and the interosseous membrane of the forearm. Other injuries that can be identified are the chondral lesions and loose bodies.
5 The Classifications
The most common classification for radial head fractures was described by Mason (1954) in 1954. Johnston (1962) modified this in 1962 to include a Mason–Johnston type IV lesion.
Mason’s original classification (Mason 1954) was modified by Broberg and Morrey (1987) to quantify the extent of head involvement and to include radial neck fractures.
-
Type I: fracture of the radial head or neck with 2 mm displacement
-
Type II: fracture of the radial head or neck displaced 2 mm and involving 30% of the articular surface
-
Type III: comminuted fracture of the radial head or neck
-
Type IV: elbow dislocation with fracture of the radial head
Hotchkiss (1997) described a modified classification that aims to direct treatment.
-
Type I: minimally displaced fracture with no mechanical block to motion and intra-articular displacement of 2 mm or a marginal lip fracture
-
Type II: displaced 2 mm fracture of the head or neck without severe comminution and with or without a mechanical block to motion
-
Type III: severely comminuted fracture of the radial head or neck with or without a mechanical block to motion
An important aspect in determining appropriate treatment includes recognizing associated injuries and considering their implications (Van Riet and Morrey 2008).
Ring (2008) summarized the most common injuries that occur in association with radial head fractures:
-
Elbow dislocation and subluxation
-
Medial collateral ligament rupture or capitellar fracture
-
Terrible triad injuries (radial head fracture, coronoid fracture, and elbow dislocation)
-
Posterior trans-olecranon fracture–dislocation (posterior Monteggia)
-
Interosseous membrane rupture (Essex-Lopresti)
6 The Treatment Options
Many factors should be considered in the decision-making process to ensure optimal outcomes. The characteristics of the radial head fracture, including fragment number, displacement, articular surface involvement, and bone quality, all influence the treatment. It is also imperative to establish the presence of associated ligamentous injury or associated elbow fractures or dislocation.
A variety of treatment options are used, including early motion with nonsurgical treatment or with a surgery by the fragment excision, radial head excision, repair, and replacement. The principal goals of all the treatments are to restore the elbow motion, and in case of the surgical treatment, the primary aims are to restore the anatomy and the articular congruity.
Non-displaced or minimally displaced fractures are common and represent approximately 40–50% of all radial head fractures, and they are considered stable (Akesson et al. 2006; Herbertsson et al. 2004b).
Minimally displaced fractures with no mechanical block to motion without instability should be treated nonoperatively with an early mobilization.
After trauma, aspiration of the elbow joint decompresses the joint, and an intra-articular injection of local anesthetic can dramatically decrease the pain. This permits a better evaluation of the range of movements and of the stability. However, Holdsworth et al. (1987) neglected to find a significant improvement in outcome after this procedure.
Although early mobilization should be encouraged, a study by Radin and Riseborough (1966) advised to proceed cautiously with fractures involving more than one third of the articular surface, as further displacement can occur. Regular follow-ups with radiographs are essential to ensure that delayed displacements of the fracture are not missed (Weseley et al. 1983).
Different studies have reported 85%–95% good results when isolated displaced partial (two-part) radial head fractures are managed nonoperatively with early active motion (Akesson et al. 2006; Herbertsson et al. 2004b). After excluding a mechanical block, the primary concern in the management of these lesions is the prevention of the elbow stiffness.
The exact displacement of a radial head fracture that predicts good outcome with nonoperative treatment has not been established.
Fractures, involving less than one third of the articular surface with less than 2 mm of displacement or in low demand populations (elderly patients), are at low risk of further displacement (Beingessner et al. 2004; Radin and Riseborough 1966).
Following the risk of secondary displacement of the fragments in particular in young active patients, some authors advocate operative fixation of all partial displaced articular fractures (Johnston 1962; Miller et al. 1981; King et al. 1991; Ikeda et al. 2003; Esser et al. 1995).
7 Surgical Treatments
Excision of radial head fragments involving more than 25% of the surface area of the radial head should be avoided (Beingessner et al. 2004). Capitellar fragments usually arise from the posterior aspect as a consequence of a posterolateral rotatory subluxation of the elbow and can be excised if they are less than approximately one-quarter of the capitellar surface (Caputo et al. 2006).
Radial head fragments involving more than one third of the articular surface should be fixed or replaced (Caputo et al. 2006).
Radial head resection can be considered in cases of isolated, displaced, and comminuted radial head fractures without instability (Van Riet and Morrey 2008). Following radial head excision, intraoperative fluoroscopic assessments (varus and valgus and axial stress examinations) of the elbow should be performed to exclude the presence of joint instability.
Some controversy is around the radial head excision. Follow-up studies demonstrate a high prevalence of radiographic arthritis that is sometimes associated with symptoms. (Boulas and Morrey 1998; Goldberg et al. 1986; Ikeda and Oka 2000; Janssen and Vegter 1998; Morrey et al. 1979). The modifications of the elbow joint biomechanics following radial head resection can lead to premature cartilage wear (Beingessner et al. 2004).
Biomechanical analysis of elbows following radial head resection has shown altered kinematics and stability (Jensen et al. 1999) of the elbow joint. In particular Jensen et al. (1999) have defined the key roles of the ligaments in the setting of radial head resection, and they advise intraoperative varus, valgus, and axial stressing of the elbow and wrist to exclude an elbow instability or an Essex-Lopresti lesion.
Long-term outcomes are conflicting (Herbertsson et al. 2004a; Goldberg et al. 1986; Ikeda and Oka 2000). Herbertsson et al. (2004a) reported fair to good results after excision for Mason types II and III, with no significant difference in outcome between primary and delayed resection. Ikeda and Oka (2000) reported disappointing results after early excision for Mason type II and III.
8 Reduction and Internal Fixations
8.1 Arthroscopic Technique
The arthroscopy of the elbow has become a standard treatment option for many indications. It gives an excellent intra-articular view with soft tissues and articulate bone damage visualizations.
It was originally considered to be an unsafe procedure because of the small size of the elbow joint capsule and its close proximity to several neurovascular structures. Over the past decade, however, this procedure has become safer and more effective. These improvements can be attributed to a better understanding of elbow anatomy and of the pathologies.
The most common indications for elbow therapeutic arthroscopy procedures include removal of loose bodies, synovectomy, debridement, and excision of osteophytes and capsular release, but it can assist in effectively the diagnosis and management of acute intra-articular fractures.
It has been used in the treatment of minimally displaced radial head, coronoid and capitellum fractures in adults, and displaced radial neck and lateral humeral condyle fractures in children with good results (Van Tongel et al. 2012; Graveleau et al. 2006).
The arthroscope is also useful in the identification of varus, valgus, and posterolateral rotatory instability, particularly when these instabilities are not clear as to the acute clinical examination or if they are associated to radial head and coronoid fractures (Holt et al. 2004).
Most of the complications associated with elbow arthroscopy can be avoided by the proper surgical technique. Successful elbow arthroscopy requires a thorough understanding of the arthroscopic anatomy. The joint should be kept distended during the setup of the portals to move the neurovascular structures away from the arthroscopic devices.
The patient is placed in lateral or prone positions. Most of the procedures can be accomplished with the 4.0 mm 30° scope; 70° scope provides a better visualization of the radial head and capitellum.
In case of radial head fracture, the joint visualization is performed through the medial (proximal anteromedial and anteromedial) and lateral (proximal anterolateral and anterolateral) portals. The soft spot portal can be useful to reduce the fragment and to place the internal fixations.
A 3.5 mm shaver is useful for removing the hematoma and debris. Retractors can be used to pull out the annular ligament distally to allow direct access to the fracture fragments. Provisional reduction of the fragments can be obtained using “K-wires” in conjunction with probes and graspers (Baker and Brooks 1996). Definite fixation can be performed using absorbable pins or cannulated screws.
8.2 Open Technique
Articular displaced radial head fractures can be managed with open reduction and internal fixation, with good results (King et al. 1991; Ikeda et al. 2003). A block to rotation and the presence of associated fractures and ligament injuries can also influence the decision to proceed with an open reduction and internal fixation.
For radial head fracture fragments involving more than one third of the articular surface and causing a mechanical block, particularly in young and active patients, open reduction and stable internal fixation are recommended (Hotchkiss 1997; Beingessner et al. 2004).
9 Surgical Technique and Related Aspects
The patient is in supine position with the arm on the chest or on the arm holder.
Most commonly a lateral skin incision is used. The deep approach is typical through the Kocher approach (between the anconeus and the extensor carpi ulnaris muscles) or the Kaplan approach (extensor-splitting muscle approach). Both approaches offer adequate visualization and exposure for internal fixation of the radial head. When the medial and lateral sides of the elbow need to be addressed, the global approach using a posterior midline incision is preferred.
During the procedure, the interosseous nerve should be protected, i.e., with the forearm pronation that increases the distance between the radial head and the nerve.
A cadaver study on the radial head plating performed by Tornetta et al. (1997) reported that in only 1 (2%) of 50 arms. The posterior interosseous nerve lies directly on the radius, and the average distance from the radial head to the origin of the posterior interosseous nerve was at 1.2–1.9 mm, with average being proximal to the radial head in 31 cases. The muscular branch to the extensor carpi radialis longus was located from 7.1 to 1.8 mm from the radial head (Graveleau et al. 2006).
The radial head is exposed through the annular ligament and preserving the posterior bundle of the lateral collateral ligament. It is important to remain anterior to the equator of the radial head (anterior to the line drawn along the axis of the radius).
The debridement of the fracture is performed, and the reduction should be performed preserving as much as possible of the periosteum and the soft tissue around the radial head for keeping the integrity of the vascular supplies (Yamaguchi et al. 1997; Patel and Elliott 1999).
A fine “K-wire” can be used to manipulate fragments into position. If reducing the fragments results in a cancellous defect, bone graft can be harvested from the olecranon or the lateral epicondyle.
The concept of an anatomic “safe zone” must be reminded when a reduction and internal fixation is performed. Intraoperatively, the safe zone is defined by a 110° arc centered over the equator of the radial head with the forearm in neutral rotation (O’Driscoll et al. 2003): it is the portion of the radial head that is presented laterally under the wound with the forearm in neutral position (Smith and Hotchkiss 1996; Soyer et al. 1998) (Fig. 13.4).
Alternatively, the safe zone may be identified with the wrist in neutral; the zone lies between two longitudinal lines drawn from Lister’s tubercle and the radial styloid proximally.
The cartilage of the safe zone is thinner and has a gray hue when compared to the remaining part of the radial head. Hardware may be placed into this zone without causing impingement with the lesser sigmoid notch.
A variety of devices can be used to achieve the goals of surgery, which consist of obtaining stable fixation, restoring the articular surface, and recovery the head-neck relationship.
Although current implants and techniques for internal fixation of small articular fractures have made it possible to repair most fractures of the radial head, data by Ring et al. (2008) suggest that open reduction and internal fixation are best reserved for minimally comminuted fractures with three or fewer articular fragments.
For fractures that do not involve the radial neck, the fixation is typically obtained by using small screws such as mini-fragment screws (sizes 2.0 or 2.7 mm). Screws should be countersunk beneath the articular surface, but not protrude through the opposite cortex. Fractures involving the radial neck are often impacted and require bone grafting to elevate the radial head. These fractures may be amenable to screw and plate fixations.
If plate is chosen for radial head and neck fixation, low-profile plates are indicated to reduce the impingement between the less sigmoid notch and the annular ligament.
In case of small fragments or in the presence of a piece of cartilage, the fibrin glue and bio-absorbable implants (K-wire and screw) can be used in particular if the fragment is not in the articular portion of the radial head (Givissis et al. 2008).
Early complications from internal fixation are usually a consequence of inadequate fixation, hardware malposition, or injury to the posterior interosseous nerve.
The most common late complications include hardware prominence (particularly in thinner individuals) and elbow stiffness with or without heterotopic ossification or the proximal radioulnar synostosis.
Regaining motion is an important goal after surgery that can be achieved with early active motion throughout the range of motion.
10 Outcomes and Related Considerations
Ring et al. (2002) presented a large series of patients (56 patients) with Mason types II and III fractures managed with internal fixation. The mean arc of motion after surgery ranges from 129° to 18° in flexion-extension, with a mean pronation of 67° and 59° in supination. Six patients had painful nonunion treated with radial head excision. They concluded that open reduction and internal fixation should be reserved for fractures with less than three articular fragments. All the patients with Mason type III fractures with more than three fragments had an unsatisfactory result, in contrast to all the patients with Mason type II fractures with satisfactory outcomes.
Ikeda et al. (2003) showed excellent results in ten patients, three of whom had a Mason type III fracture and seven with a type IV; all of them were treated with pre-contoured low-profile implants. The mean arc of motion in flexion-extension ranges from 135° to 7°, with a mean pronation of 76° and 85° in supination. However, 90% of the patients subsequently required hardware removal.
Esser et al. (1995) described nine Mason type III and six Mason type IV fractures treated with Herbert screws and AO mini-plates. In the first group, the mean arc of motion obtained ranged from 3° in extension to 138° in flexion, and the mean rotation was pronation at 86° and supination at 85°. In the second group, the arc of motion ranged from 13° in extension to 131° in flexion; the mean supination was 87° with 70° for pronation. No major complications were reported in both series.
Rolla et al. (2006) described an original technique for the arthroscopic diagnosis and treatment of the radial head fractures. This procedure was performed in six patients. Short-term preliminary results show a satisfactory functional outcome. The advantages of the technique are the minimal invasive approach and the direct visualization of the fracture.
Yeoh et al. (2012) reviewed the literature on the outcomes of elbow arthroscopy to obtain an evidence-based recommendation for this technique in the treatment of various conditions. They found some fair quality evidence for elbow arthroscopy in the treatment of rheumatoid arthritis and lateral epicondylitis. Poor quality evidence was also found for the arthroscopic treatment of radial head, capitellum, and coronoid fractures. They concluded that the available evidence supports the use of elbow arthroscopy in the management of these conditions, but the quality of the evidence is generally low.
11 Summary
-
X-rays and CT scan are useful to define the preoperative plan and to assess the more adequate fixation.
-
Intraoperative fluoroscopy evaluation is useful to assess the radial head reduction, the residual stability of the elbow and to check the impingement of the device with the lesser sigmoid notch and the capitellum during the motions.
-
Internal fixation of the radial head is indicated in fractures with less than three fragments.
-
The common surgical approaches are the Kocher and Kaplan exposures. The Kocher’s approach allows the complete exposure of the lateral collateral ligament complex.
-
The lateral collateral ligament should be preserved during the surgical exposure and in case of concomitant detachments from the bone insertions which have to be repaired.
-
The annular ligament is incised to approach the radial head, and it should be repaired at the end of the procedure.
-
The posterior interosseous nerve should be protected, keeping the forearm in pronation and avoiding compression forces using a Hohmann retractor or other devices around the radial head and neck soft tissues.
-
The hardware should be placed in the non-articular safe zone to avoid any impingement with the lesser sigmoid notch. Check for any extraarticular placement of subchondral screws.
-
Ligament repairs are an important step to be performed at the end of the procedure using heavy nonabsorbable sutures.
-
Postoperative motions started as soon as possible also if the drainages are still in place. If there is a residual risk for a posterolateral instability or if the lateral ligament was repaired, the postoperative rehabilitation is performed with the forearm in pronation (the articular brace can be used to protect the motion).
-
Indomethacin therapy can be used to reduce the risk of heterotopic ossification.
12 Radial Head Replacement
Radial head replacement is considered when the fracture is comminuted, and a stable internal fixation is not possible. It is also considered when the fracture involves more than one third of the radial head. It is particularly indicated for fractures with associated ligamentous injury and coronoid or olecranon fractures which are displaced or unstable.
For displaced radial head fractures with greater than three fracture fragments, open reduction and internal fixation has been reported to be less reliable, and radial head replacement may be the preferred technique. With these complex fracture patterns, it is difficult to maintain length and alignment during the fixation. Open reduction and internal fixation in the setting of comminuted fractures can result in nonunion, loss of fixation, and unpredictable forearm rotation (Ikeda et al. 2003; Ikeda et al. 2005; Bain et al. 2005).
In summary, the radial head replacement is indicated in the following acute situations:
-
Acute comminuted fracture in which anatomic reduction and stable fixation cannot be obtained (Ring 2011)
-
Complex elbow injuries that involve more than 30% of the articular rim of the radial head, which cannot be reconstructed
-
Fractures with three or more fragments or significant comminution (Ikeda et al. 2003; Ring 2011)
-
Intraoperative instability of the elbow after radial head resection (Hotchkiss 1997; Monica and Mudgal 2010)
-
Essex-Lopresti lesion (Ring 2011)
-
Associated terrible triad injuries (Smith and Hotchkiss 1996)
-
Non-reconstructable radial head fractures with concomitant medial collateral ligament injury, interosseous membrane injury, or elbow dislocation (Monica and Mudgal 2010; Gao et al. 2013; Grewal et al. 2006; Pfaeffle et al. 2005).
Contraindications to radial head replacement in acute situations are:
-
Active infection around the elbow joint
-
Neurologic injuries (Ring 2011; Monica and Mudgal 2010; Gao et al. 2013; Grewal et al. 2006)
The modern radial head prosthesis is pyrocarbon or metallic implants. Silicone rubber prostheses are no longer used, as they are not rigid enough and are predisposed to the fragmentation (Vanderwilde et al. 1994).
The silicone flexibility limited its ability to transfer loads across the elbow (Carn et al. 1986). Another problem related to this device is the subsequent reactive synovitis and pain, as well as implant loosening (Gordon and Bullough 1982; Worsing et al. 1982; Morrey et al. 1981; Martinelli 2008).
The silicone implants are associated with bad clinical scores, increased elbow arthritis, and increased radial shortening.
Different implants are available for radial head replacement, and some of these try to replicate as much as possible the native radial head. Current prostheses are manufactured from cobalt–chrome alloys or titanium. Designs vary in respect to head shape and stem fixation techniques, including smooth, press fit, ingrowth, and cemented stems. Monoblock and modular prostheses are available, including bipolar implants. The recent radial head prosthesis can be classified according to the design concepts, such as bipolar versus monopolar, cemented versus uncemented, and anatomic versus an asymmetric head shape (Fig. 13.5).
Anthropometric studies of the proximal radius demonstrate that the head is elliptical in shape, it has a variable offset from the axis of the neck, and its diameter correlates poorly with the diameter of medullary canal of the neck (King et al. 2001). These findings may support that the use of modular implants allows improved sizing options that are more similar to the anatomy of the radial head and proximal radius.
13 Surgical Technique and Related Aspects
The radial head replacement as in case of the open reduction and internal fixation technique may be performed through a lateral or posterior approach. When concomitant fractures or complex injuries that involve the ligaments are present and require treatment, an extensile posterior approach is preferred. A skin incision is made between the lateral condylar ridge and the lateral aspect of the ulna through the mid-axial line of the radial neck.
The two cutaneous flaps are elevated and the subcutaneous sensitive nerves are protected. The dissection runs through:
-
1.
The Kocher interval between the anconeus and extensor carpi ulnaris muscles
-
2.
The Kaplan interval between the extensor carpi radialis longus and extensor digitorum communis muscles
-
3.
The splitting of the extensor digitorum communis, as described by Hotchkiss (1997)
Using the Kocher approach, the lateral collateral ligament complex (LCLC) is exposed, and the annular ligament is prepared.
The lateral collateral ligament (LCL) is incised anterior to a line bisecting the articular surface of the capitellum from a lateral side (Hotchkiss 1997).
Inspection of the LCL complex should be performed. The elbow capsule and annular ligament should be incised in line with the posterior margin of the extensor carpi ulnaris. The capsule can also be incised in a ligamentous-sparing Z capsulotomy, as described by Bain et al. (2005). The capsule is elevated from the anterior distal humerus, and more of the radio-capitellar joint may be exposed by elevating the origin of the brachioradialis muscle.
The posterior interosseous nerve has to be protected avoiding traction and compression of the soft tissues around the radial head (Morrey 2009).
The pronation of the forearm without traction on the anterior soft tissues is useful to reduce the possibility of iatrogenic injury to the posterior interosseous nerve. Exposure provided by retractors, such as the Hohmann retractor placed anteriorly around the radial head or neck, is excellent; however, it is recommended to prevent any strong traction on the anterior soft tissue. If a wide exposure of the radius is necessary, we advise to release the supinator muscle from the ulna and to reflect medially both the heads of the muscle. In this way the radial neck and the proximal radial bone can be safely exposed by protecting the nerve. If the radial head needs to be moved out of the wound for better exposure, placing a small Hohmann retractor gently on the dorsal surface of the head will be helpful to elevate it out of wound preserving the posterior bundle of the LCL (Hotchkiss 1997).
Once the radial head is exposed, the degree of comminution and displacement is assessed.
The native head should be resected at the metaphyseal level proximally to the bicipital tuberosity, preserving the annular ligament and as much as possible of the radial neck. Once resected, it can be used to decide the adequate sizes of the cup of the implant (Ring 2004; Van Glabbeek et al. 2005; Van Glabbeek et al. 2004).
The aim of replacement is to replicate the native radial head anatomy as closely as possible paying special attention to the radial head size and height (King 2004). Different biomechanical studies have demonstrated the importance of accurate radial head sizing (Pomianowski et al. 2001; Van Riet et al. 2007).
The fractured head should be reassembled as closely as possible to the native one, and an appropriate head size is selected. Care should be taken to avoid overstuffing in the radio-capitellar joint because it has been associated with radio-capitellar wear and erosion (King 2004; Pomianowski et al. 2001; Van Riet et al. 2007).
It is important to check the radial neck for un-displaced fractures prior to insertion of the implant. Any un-displaced fractures should be prophylactically wired before prosthesis insertion because displacement or collapse may occur when the prosthesis is inserted.
An important mark is the proximal margin of the articular surface of the lesser sigmoid notch; in particular Doornberg et al. (2006) demonstrated using CT scans of 17 elbows that the native radial head lies an average of 0.9 mm distal to the proximal margin of the sigmoid notch, and this observation can be used during the radial head replacement to replicate the anatomical relationship (Fig. 13.6).
Van Riet et al. (2007) have shown that with the forearm in neutral rotation, the proximal edge of the lesser sigmoid notch can be used as a marker for the proximal end of the radial head. They showed that radial neck lengthening around 2.5 mm altered the radio-capitellar biomechanics, with a significant decrease in varus-valgus laxity and created an ulna mal-tracking. Radial neck shortening had the opposite effect (Fig. 13.7). Different authors recommended a smaller size implant than the native head, both with regards to diameter and thickness (King 2004; Pomianowski et al. 2001; Van Riet et al. 2007; Doornberg et al. 2006).
In general, it is preferable to be slightly undersized regarding the diameter and the thickness of the prosthesis (Ring and King 2008). A prosthesis, with a diameter that is too large, gives a load on the margins of the sigmoid notch, whereas a prosthesis that is too small gives a load on the sigmoid notch (King et al. 1999). A radial head with an incorrect diameter also has a cam effect, which produces abnormal loading on the capitellum. Insertion of a radial head that is too short contributes to radio-capitellar instability (King et al. 1999).
The medullary canal of the proximal radius is then prepared with serial-sized broaches until an adequate fit is obtained in the canal at the appropriate depth. The appropriate-sized trial stem is inserted ensuring that the collar of the prosthesis is flush with the resected neck. In modular designs, the trial head is secured to the trial stem, and the elbow and forearm are placed through a full arc of motion. Tracking as well as the relationship between the prosthesis and the capitellum is carefully assessed. Once acceptable alignment and tracking are determined, the trial components are removed, and the final prosthesis is inserted. The stem may be press fit or cemented in place depending on the design and stability of the stem in the medullary canal.
Inserting the stem may be difficult if the LCL is intact. An effective way to facilitate prosthesis insertion is to place a retractor under the radial neck and lever the proximal part of the radius anteriorly and laterally away from the capitellum (Ring and King 2008).
After the implant has been inserted, the elbow should be moved through a wide range of motion while the surgeon observes the radio-capitellar contact for congruency and tracking with the height and diameter of the implant. Elbow alignment and implant sizing can also be assessed by examining the parallelism of the medial ulno-trochlear joint space with fluoroscopy. The implant should articulate with the lateral trochlea at the level of the proximal radioulnar joint, approximately 2 mm distal to the tip of the coronoid (Van Riet et al. 2007; Doornberg et al. 2006). Distal radioulnar alignment and ulnar variance should also be examined. It is important to check for an over lengthening of the radius also using a fluoroscopy evaluation (van Riet et al. 2004).
The lateral collateral ligament complex is repaired to the lateral epicondyle with heavy nonabsorbable sutures using transosseous tunnels or suture anchors. The medial collateral ligament repair is not usually necessary, but if the elbow remains unstable after the radial head replacement and lateral ligament repair, it will be necessary.
Formal assessment of elbow stability as described by Bain et al. (2005) includes stress testing with the elbow in 30° flexion, and the forearm pronated is important. In this position, narrowing of the radio-capitellar joint by 2 mm with valgus stress testing is indicative of integrity loss of the anterior band of the ulnar collateral ligament. Transosseous sutures should be used for stabilization of the lateral collateral ligament with the elbow in 30° flexion and the forearm in full pronation (King et al. 1999).
Beingessner et al. (2004) reported in a biomechanical study that varus-valgus laxity was controlled after radial head replacement and lateral collateral ligament repair but not after the only radial head replacement without ligament repair. They noted only a small amount of valgus instability in elbows with disrupted medial collateral ligaments after radial head replacement.
14 Outcomes and Related Considerations
Good clinical results have been reported for metallic radial head implants for comminuted radial head fractures in a number of recent reports (Moro et al. 2001; Popovic et al. 2000; Smets et al. 2000; Zwingmann et al. 2013). However, the long-term effect on the capitellar articular cartilage and problems such as implant loosening and failure have been described.
Authors (Moro et al. 2001; Popovic et al. 2000; Smets et al. 2000; Zwingmann et al. 2013) observed as the correct diameter and height of the prosthesis is the key for a successful outcome. Using a larger diameter head will result in loading on the margins of the sigmoid notch, while an excessively small prosthesis will result in point loading. An incorrect head diameter can produce a cam effect, inducing abnormal load on the capitellum. The correct diameter of the radial head can be selected by comparing the excised and reassembled radial head fragments with the range of trial prostheses. The prosthesis should be congruent and have a smooth motion with the capitellum throughout the full range of motion (Bain et al. 2005; Pomianowski et al. 2001). The prosthesis should be seated on a stable rim of radial neck. Increasing the height results in overstuffing the joint, which may result in stiffness and lateral elbow pain, which has become a relatively commonly reported problem. A prosthesis that is inserted too short will result in instability (Markolf et al. 2004). To ensure a normal articulation with the proximal radioulnar joint, the height of the prosthesis must be the same as that of the trochlear notch.
Harrington and Tountas (1981) published one of the first series using titanium radial head prosthesis in 1981. The investigators reported good or excellent results in 14 (93%) of 15 patients at average follow-up of 6.9 years.
Bain et al. (2005) reported on 16 patients with Mason type III fractures treated with titanium prosthesis and found good to excellent results in 80% of them at 2.8-year follow-up.
Grewal et al. (2006) reported their experience using a metal modal implant on 24 patients with Mason type III fractures at an average of 25 months; they observed 12 excellent, 4 good, 6 fair, and 2 poor results.
Harrington et al. (2001) reported they experience using a metallic implant. The series included in 14 Mason type IV (comminuted fracture dislocations), 3 Monteggia fracture dislocations, 2 medial ligament tears associated with radial head fractures, and 1 Mason type II radial neck and coronoid. Sixteen patients out of 20 patients (80%) obtained a good or excellent outcome, based on the Mayo Elbow scores, at mean follow-up of 12.1 years (range 6–29 years). Only 6 (30%) of 20 were completely pain-free at final follow-up, but an additional ten had pain only with continuous activity. The investigators note degenerative changes of the capitellum in nine patients (45%).
Doornberg et al. (2007) reported as the majority of patients with loose fitting stems have radiographic lucency around the stem at follow-up. They followed up 27 patients (11 with Mason type II and 16 with Mason type III fractures) for an average of 40 months and reported average range of motion of 20° of extension, 131° of flexion, 73° of pronation, and 57° of supination. Twenty of 27 patients had excellent results on Mayo Elbow Performance score.
Knight et al. (1993) reported a reliable restoration of stability and prevention of proximal radial head migration after metal prosthesis in 31 patients at an average of 4.5 years’ follow-up; 68% of the radial head fractures were associated with elbow dislocations. They noted a low complication rate and only two implants were removed for aseptic loosening.
Shore et al. (2008) studied 32 patients, with mean follow-up of 8 years (range 2–14 years), treated with delayed radial head replacement at an average of 2.4 years after the injury. The radial head fractures were associated with an elbow dislocation in 17 patients and terrible triad in 7 patients. The average Mayo Elbow Performance score was 83, with 21 (66%) obtaining good or excellent results. Post-traumatic arthritis was observed in 74%; they did not remove any implants.
Moro et al. (2001) retrospectively reviewed 25 patients with 10 Mason III and 15 Mason IV radial head fractures, treated with acute radial head replacement using a non-cemented titanium prosthesis. At mean follow-up of 39 months (range 26–58 months), the investigators noted 16 (64%) good or excellent results with 5 (20%) patients demonstrating radiographic evidence of posttraumatic arthritis. Heterotopic ossification was found in 8 (32%) patients.
Ashwood et al. (2004) studied outcomes in 16 patients treated with a titanium radial head prosthesis. The average Mayo Elbow Performance score at final follow-up (average 2.8 years) was 87 (range 65–100) with 13 (81%) obtaining good or excellent results, and 7 of 9 employed patients were able to return to work.
Rotini et al. (2012) described 31 radial head prostheses used in 30 patients. In ten patients, the mean time from trauma to surgical treatment was 2.4 days, while the remaining 20 patients were treated after an average of 19 days from trauma. The implant design was monopolar in 12 cases and bipolar in 19. At a mean follow-up of 2 years (range 13–36 months), the mean Mayo Elbow Performance score was 90 points. Heterotopic ossifications were found in 14 cases. Bone reabsorption was observed in nine cases; in their experience they found no significance evidence of a superiority of bipolar or monopolar designs.
Judet et al. (1996) reported their preliminary experience using the bipolar prosthesis on five patients with an average follow-up of 43 months, evaluated using the Broberg and Morrey score obtaining two excellent results. Afterward Judet et al. (2001) reported the results of a larger series of 22 cases treated using the bipolar prosthesis and evaluated using the Broober-Morrey score at an average follow-up of 12 months. Twenty-one satisfactory results and one unsatisfactory result were obtained.
Popovic et al. (2000) reported the use of bipolar prostheses in acute pathology on 11 patients with Mason type III fractures of the radial head associated with elbow dislocation; the date was analyzed using Booberg-Morrey, obtaining satisfactory results in eight patients; the remaining three patients presented an unsatisfactory result due to the presence of a limited range of motion and pain during everyday activities.
Smets et al. (2000) reported their experience using the bipolar prosthesis on 13 cases with a follow-up of 25.2 months evaluated using the Mayo Elbow Performance score: 7 proved to be excellent, 2 good, 1 sufficient, and the remaining 2 unsatisfactory, and one wherein the prosthesis had to be removed. The cause of the unsatisfactory result in three cases was pain with a limited range of motion.
Holmenschlager et al. (2002) published their experience in acute cases using the bipolar prosthesis on 16 patients, evaluated at an average follow-up of 18 months using the Booberg-Morrey score; 14 patients obtained a satisfactory result and two unsatisfactory one; these were patients with associated radius or coronoid process fractures.
Frosch et al. (2003) reported their experience with the bipolar implant on 10 patients with 11 implants. At an average follow-up of 5 years, nine patients (ten implants as one died due to causes not connected to the elbow injury) were assessed using the Broberg–Morrey score. Satisfactory results were obtained in seven patients (eight implants), and the remaining two were unsatisfactory.
Celli et al. (2010) reported their experience with a bipolar Judet radial head prosthesis for the treatment of the acute radial head fractures. Sixteen patients were assessed following radial head replacement with a mean follow-up of 41.7 months; the outcome was satisfactory in 87.5% of cases. The mean postoperative ranges of motion were greater than the functional arcs both in flexion-extension and in pronation-supination, and the results did not appear to be influenced in a significant way by the type of original lesion. All elbows were stable. The main complication was the development of heterotopic ossifications. They concluded that the bipolar radial head design represents a suitable option for acute treatment of irreparable acute radial head fractures. Afterward, the authors (Celli and Celli 2012) reported a larger group of patients treated using the same bipolar design (95 implants), and 70 patients were assessed; 39 patients (39 implants) underwent a radial head replacement for acute fractures, at a mean follow-up of 39.1 months; according to the Mayo Elbow Performance score, 32 were excellent, 2 good, 1 fair, and 4 poor.
The complications related to the implant design in this group are the disassemblage of the cup, the capitellar erosion, the overstuffing, and the posterolateral subluxation of the cup, but the majority of the complications observed are related to the joint as joint stiffness and heterotopic ossifications.
Ricon et al. (Ricon et al. 2012) performed a retrospective analysis of 28 patients with Mason III radial head fractures treated with a pyrocarbon radial head prosthesis. The radial head fracture was associated with an elbow dislocation in 23 patients. At an average follow-up of 23 months, patients had an average Mayo Elbow Performance score of 92 (range 70–100). The mean flexion-extension arc was 105 (range 65–130). Although these outcomes are comparable to those achieved with cobalt–chromium and titanium prostheses, enthusiasm should be tempered until longer-term follow-up data are not available.
15 Summary
-
X-rays and CT scans are useful to assess the preoperative plan and to define the concomitant fractures.
-
Intraoperative fluoroscopy evaluation is useful to assess the correct position and size of the radial head implant and also to assess the ulno-humeral articular space.
-
Radial head replacement is considered when the fracture is comminuted and stable internal fixation is not possible.
-
Current implants are manufactured from cobalt–chrome alloys or titanium. They can be classified according to the design concepts, such as bipolar versus monopolar, cemented versus uncemented, and anatomic versus asymmetric head shape.
-
Lateral or posterior approaches can be used to perform the radial head replacement similar to the open reduction and internal fixation technique. The deep exposure runs through the Kocher or the Kaplan interval.
-
The lateral collateral ligament complex is incised anteriorly to a line bisecting the articular surface of the capitellum from a lateral side preserving the posterior bundle. The annular ligaments are incised too.
-
The posterior interosseous nerve has to be protected; avoid traction and compression of the soft tissues around the radial head and neck.
-
The resection of the native head should be at the metaphyseal level proximal to the bicipital tuberosity.
-
The radial head replacement has to replicate the native radial head anatomy as closely as possible (paying special attention to the radial head size and height). It is preferable for the diameter and the thickness of the prosthesis to be slightly undersized.
-
The proximal edge of the lesser sigmoid notch can be used as a marker for the proximal end of the radial head to avoid an over-lengthening.
-
Un-displaced radial neck fractures have to be checked prior the insertion of the implant.
-
After the implant has been inserted, the elbow should be put through a range of motion checking for the radio-capitellar contact and tracking with the height and diameter of the implant.
-
The lateral collateral ligament complex is repaired to the lateral epicondyle using heavy nonabsorbable sutures through the transosseous tunnels or suture anchors.
-
The medial collateral ligament is typically not necessary to repaired, but if the elbow remains unstable after the radial head replacement and lateral ligament repair, it will be necessary.
-
Postoperative motions start as soon as possible even if the drainages are still in place. If there is a residual risk for a posterolateral instability or if the lateral ligament was repaired, the postoperative rehabilitation is performed, avoiding the complete forearm supination (the articular brace can be used to protect the motion).
-
Indomethacin can be used to reduce the risk of heterotopic ossification.
16 Rehabilitation Aspects
The rehabilitation program of radial head fractures depends primarily on the presence of associated osseous and ligamentous injuries (simple or complex fractures, respectively) and if the patient has undergone surgery or not. In case of simple fracture surgery, the strength and stability of the repaired structures have to be clearly communicated by the surgeon to the physiatrist and therapist.
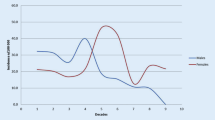
Non-displaced or minimally displaced fractures (Mason type II or II without mechanical block) are actually treated in a nonoperative way, and usually the extent of the trauma is not so heavy to create associated lesions. So the elbow rests in a collar and cuff sling flexed at 90° for about 1 week and after an active range of motion should be started (Liow et al. 2002). To do this it is necessary that pain and edema have subsided, and to achieve this purpose, we can implement all the possibilities described in the previous chapter (see articular distal humeral fractures rehabilitation). When fracture healing appears on X-ray, we can dedicate to a more vigorous range of movement (ROM) recovery with passive ROM and stretching exercises if there is the need (usually near full ROM is achieved 4–5 weeks after trauma). When pain is under control and ROM restored enough, we even begin muscle strengthening recovery. In our clinical practice according to the literature, outcomes after conservative treatment are satisfactory (Shore et al. 2008; Coonrad et al. 2005; Dunning et al. 2001; Armstrong et al. 2000; Szekeres et al. 2008; Herbertsson et al. 2005; Broberg and Morrey 1986; Duckworth et al. 2012b).
If a simple radial head fracture has been synthesized, postoperatively we use a protective brace with elbow flexed to 90° to limit forearm rotation and elbow extension for about 3 weeks, but early ROM is instituted, usually within the first week post-surgery. Flexion is theoretically unlimited although its recovery is gradual because while the elbow flexes, gradually the radio contact humerus increases leading to stress on the synthesis. For this reason we have to be very careful when bending the elbow to avoid causing pain.
So active-assisted or gravity-assisted and active ROM of the elbow and adjacent joints start, as pain and edema decrease. Elbow flexion and extension recovery is performed with forearm neutral rotation. Pronation and supination are performed with the elbow flexed at 90° because between flexion angles of 0° and 45°, the anterolateral portion of the radial head bears a great axial stress. We must be careful not to place stress on the synthesis during the pronation of the radial head for its posterior translation.
We usually have to wait for about 1 month before starting passive ROM, when the fracture has become stable and is at least at an early healing stage, as evident on X-ray (Fig. 13.8a, b). The same applies to stretching and manual therapy useful to decrease residual pain or muscle spasm and increase collagen or muscular tissue elasticity and therefore range of motion. Quite often it is necessary to recover full extension and supination which are lacking. Modalities (such as heat) or manual therapy can be useful to prepare the joint for stretching or mobilization (Mulligan or Maitland). In case of elbow instability with or without radial head excision, avoid any elbow joint mobilizations.
Muscle strengthening of the wrist, shoulder, and scapular muscles (Fig. 13.9a–f) can start immediately after surgery but only after 3–4 weeks for the forearm and in a progressive way and above all, for the flexor-pronator muscles (Fig. 13.10). Their reinforcement is useful because they act as dynamic valgus elbow stabilizers, but muscular recruitment generates forces through the radial head that have not to be too strong. For strengthening against resistance, we have to wait about 6 weeks and start using “safe positions” as described for active ROM. At the same time we can even gradually increase the reinforcement of all upper limb, scapula\thoracic, and core muscles. The progression of rehabilitation is the same as that already described for the distal humeral fractures.
In case of radial head complex fractures, the ligament- or bone-associated injuries and their treatment influence the planning and progression of rehabilitation, so this information is of fundamental importance to be reported. Usually patients wear a hinged brace that allows the movement in a safe arc established by the surgeon and avoid valgus and varus stress on the joint. The brace is used continuously for 3–4 weeks, and it is discharged only when performing the exercises assigned. In the brace the elbow is flexed at 90°, but forearm rotation depends on ligament health and instability pattern.
In case of posterolateral instability due to fracture or if the lateral collateral ligament (LCL) is injured or sutured, the forearm will be in pronation and vice versa for an anteromedial instability or medial collateral ligament injury for 4–6 weeks. If both ligaments are injured or repaired, the forearm will be in neutral position. The same position will be kept during the active exercises. Extension will be gained slowly, and the full range is allowed from the 4th week. Prono-supination is performed with elbow flexed to 90°. To protect the LCL patient has to avoid shoulder abduction and external rotation because the varus stress on the elbow can interfere with LCL healing in addition to being a source of pain for the patient.
If a coronoid fracture is associated, elbow splint is blocked over 60 ° of extension and then 10° per week are added. The last 30° of extension are not allowed for 4 weeks. If an olecranon fracture is associated, both full active and passive flexion beyond 90° are avoided, likewise active extension to protect fixation preventing triceps tendon muscle traction for about 4 weeks. This is our behavior unless it is the surgeon that allows to modify the program due to a stable surgical synthesis (e.g., plate, screw, and wire or cerclage). In case of radial head replacement, elbow joints were rested in a 60° flexion position for 3 weeks followed by rehabilitation (Gao et al. 2013).
After radial head excision the elbow has a high potential for instability in valgus and axial directions. For this reason the muscle strengthening program is very important to compensate instability.
So, even in case of complex fractures, active-assisted ROM is begun early, at about 10–14 days after surgery, but in the safe arc defined by the surgeon and with the necessary precautions as stated before. Elbow muscle isometric reinforcement in stable position begins 4 weeks post-surgery, but if a stable position cannot be ensured, it is delayed even to 6–8 weeks. Reinforcement against resistance is allowed after 8–12 weeks according to the stability that has been obtained (Figs. 13.11a, b and 13.12). For wrist, shoulder, and scapular-thoracic muscles, isometric work can start immediately post-surgery according to patient tolerance. Usually the patients can gradually resume their activities after 3–4 months after surgery (Bano and Kahlon 2006).
(a, b) Examples of biceps muscle reinforcement against resistance. Since in this second case (b), resistance is placed progressively toward the patient’s hand, so that the radial lever is extended, this exercise (and similar ones) will be reserved for a gradually more advanced stage of the biceps muscle reinforcement program
Indomethacin can be used for 3 weeks following surgery, 25 mg twice daily, as prophylaxis against heterotopic ossification, although evidence of efficacy is weak.
Radiation at 700 cGy can be used within 72 h of surgery following the excision of heterotopic ossifications rather than for primary prevention.
Radiographic evaluation will help to determine when bone union is sufficient to allow passive ROM recovery, joint mobilization or stretching, typically at 6 weeks (Szekeres et al. 2008). Joint mobilization is contraindicated in case of unstable elbow, radial head excision, or arthroplasty (see Rehabilitation Highlights at the end).
17 The Decision-Making Process
Many factors should be considered in the decision-making process: the characteristics of the radial head fracture (including fragment number, displacement, articular surface involvement, and bone quality) influence the treatment. It is also important to establish the presence of associated ligamentous injuries (medial and lateral) or associated coronoid fracture.
The following algorithm is useful for the surgical process decision between radial head reduction and replacement and ligaments repair (Table 13.1).


References
Akesson T, Herbertsson P, Josefsson PO et al (2006) Primary nonoperative treatment of moderately displaced two-part fractures of the radial head. J Bone Joint Surg Am 88:1909–1914
Armstrong AD, Dunning CE, Faber KJ et al (2000) Rehabilitation of the medial collateral ligament-deficient elbow: an in vitro biomechanical study. J Hand Surg 25A:1051–1057
Ashwood N, Bain GI, Unni R (2004) Management of Mason type-III radial head fractures with a titanium prosthesis, ligament repair, and early mobilization. J Bone Joint Surg Am 86(2):274–280
Bain GI, Ashwood N, Baird R et al (2005) Management of Mason type-III radial head fractures with a titanium prosthesis, ligament repair, and early mobilization. Surgical technique. J Bone Joint Surg Am 87(suppl 1):136–147
Baker CL, Brooks AA (1996) Arthroscopy of the elbow. Clin Sports Med 15(2):261–281
Bano KY, Kahlon RS (2006) Radial head fractures: advanced techniques in surgical management and rehabilitation. J Hand Ther 19:114–136
Beingessner DM, Dunning CE, Gordon KD et al (2004) The effect of radial head excision and arthroplasty on elbow kinematics and stability. J Bone Joint Surg Am 86-A:1730–1739
Boulas HJ, Morrey BF (1998) Biomechanical evaluation of the elbow following radial head fracture. Comparison of open reduction and internal fixation vs. excision, silastic replacement, and non-operative management. Chir Main 17:314–320
Broberg MA, Morrey BF (1986) Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am 68(5):669–674
Broberg MA, Morrey BF (1987) Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res:109–119
Caputo AE, Burton KJ, Cohen MS et al (2006) Articular cartilage injuries of the capitellum interposed in radial head fractures: a report of ten cases. J Shoulder Elbow Surg 15:716–720
Carn RM, Medige J, Curtain D et al (1986) Silicone rubber replacement of the severely fractured radial head. Clin Orthop Relat Res 209:259–269
Celli A, Celli L. (2012) The radial head replacement using the bipolar design, clinical results and complications observed in large group of patients oral presentation at the 24th Congress of the European Society for surgery Shoulder and the Elbow Dubrovnik Croatia Abstract book 161–162.
Celli A, Modena F, Celli L (2010) The acute bipolar radial head replacement for isolated unreconstructable fractures of the radial head. Musculoskelet Surg 94(Suppl 1):S3–S9
Coonrad RW, Roush TF, Major NM et al (2005) The drop sign, a radiographic warning sign of elbow instability. J Shoulder Elbow Surg 14:312–317
Doornberg JN, Linzel DS, Zurakowski D et al (2006) Reference points for radial head prosthesis size. J Hand Surg Am 31:53–57
Doornberg JN, Parisien R, van Duijn J et al (2007) Radial head arthroplasty with a modular metal spacer to treat traumatic elbow instability. J Bone Joint Surg Am 89:1075–1080
Duckworth AD, Clement ND, Jenkins PJ et al (2012a) The epidemiology of radial head and neck fractures. J Hand Surg 37A:112–119
Duckworth AD, Ciement ND, Jenkins PJ et al (2012b) Socioeconomic deprivation predicts outcome following radial head and neck fractures. Injury 43(7):1102–1106
Dunning CE, Zarzour ZD, Patterson SD et al (2001) Muscle forces and pronation stabilize the lateral ligament deficient of the elbow. Clin Orthop Relat Res 388:118–124
Esser RD, Davis S, Taavao T (1995) Fractures of the radial head treated by internal fixation: late results in 26 cases. J Orthop Trauma 9:318–323
Essex-Lopresti P (1951) Fractures of the radial head with distal radio-ulnar dislocation; report of two cases. J Bone Joint Surg 33B:244–247
Frosh KH, Knopp W, Dresing K et al (2003) A Bipolar Radial Head Prosthesis after Comminuted Radial Head Fractures: Indications, Treatment and Outcome after 5 Years. Unfallchirurg 106(5):367–373
Gao Y, Zhang W, Duan X et al (2013) Surgical interventions for treating radial head fractures in adults. Cochrane Database Syst Rev 31:5
Givissis PK, Symeonidis PD, Ditsios KT et al (2008) Late results of absorbable pin fixation in the treatment of radial head fractures. Clin Orthop Relat Res 466:1217–1224
Goldberg I, Peylan J, Yosipovitch Z (1986) Late results of excision of the radial head for an isolated closed fracture. J Bone Joint Surg 68A:675–679
Gordon M, Bullough PG (1982) Synovial and osseous inflammation in failed silicone-rubber prostheses. J Bone Joint Surg Am 64:574–580
Graveleau N, Bauer T, Hardy P (2006) Arthroscopic treatment of acute elbow fractures. Chir Main 25(Suppl 1):S114–S120
Grewal R, MacDermid JC, Faber KJ et al (2006) Comminuted radial head fractures treated with a modular metallic radial head arthroplasty. Study of outcomes. J Bone Joint Surg Am 88(10):2192–2200
Guitton TG, van der Werf HJ, Ring D (2010) Quantative three-dimensional computer tomography measurement of radial head fractures. J Shoulder Elbow Surg 19(7):973–977
Harrington IJ, Tountas AA (1981) Replacement of the radial head in the treatment of unstable elbow fractures. Injury 12:405–412
Harrington IJ, Sekyi-Otu A, Barrington TW et al (2001) The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: a long-term review. J Trauma 50:46–52
Herbertsson P, Josefsson PO, Hasserius R et al (2004a) Fractures of the radial head and neck treated with radial head excision. J Bone Joint Surg Am 86:1925–1930
Herbertsson P, Josefsson PO, Hasserius R et al (2004b) Uncomplicated Mason type-II and III fractures of the radial head and neck in adults. A longterm follow-up study. J Bone Joint Surg Am 86-A:569–574
Herbertsson P, Josefsson PO, Hasserius R et al (2005) Displaced Mason type I fractures of the radial head and neck in adults: a fifteen- to thirty-three-year follow-up study. J Shoulder Elbow Surg 14(l):73–77
Holdsworth BJ, Clement DA, Rothwell PN (1987) Fractures of the radial head. The benefit of aspiration: a prospective controlled trial. Injury 18:44–47
Holmenschlager F, Halm JP, Winckler S (2002) Fresh fractures of the radial head: results with the Judet Prosthesis. Revue de Chirurgie Orthopédique 88(4):387–397
Holt MS, Savoie FH, Field LD et al (2004) Arthroscopic management of elbow trauma. Hand Clin 20(4):485–495
Hotchkiss RN (1994) Injuries to the interosseous ligament of the forearm. Hand Clin 10:391–398
Hotchkiss RN (1997) Displaced fractures of the radial head: Internal fixation or excision? J Am Acad Orthop Surg 5:1–10
Hotchkiss RN, Weiland AJ (1987) Valgus stability of the elbow. J Orthop Res 5:372–377
Ikeda M, Oka Y (2000) Function after early radial head resection for fracture: a retrospective evaluation of 15 patients followed for 3–18 years. Acta Orthop Scand 71:191–194
Ikeda M, Yamashina Y, Kamimoto M et al (2003) Open reduction and internal fixation of comminuted fractures of the radial head using low-profile mini-plates. J Bone Joint Surg Br 85:1040–1044
Ikeda M, Sugiyama K, Kang C et al (2005) Comminuted fractures of the radial head. Comparison of resection and internal fixation. J Bone Joint Surg 87A:76–84
Janssen RP, Vegter J (1998) Resection of the radial head after Mason type-III fractures of the elbow: follow-up at 16 to 30 years. J Bone Joint Surg 80B:231–233
Jensen SL, Olsen BS, Søjbjerg JO (1999) Elbow joint kinematics after excision of the radial head. J Shoulder Elbow Surg 8:238–241
Johnston GW (1962) A follow-up of one hundred cases of fracture of the head of the radius with a review of the literature. Ulster Med J 31:51–56
Judet T, Garreau de Loubresse C, Piriou P et al (1996) A floating prosthesis for radial-head fractures. J Bone Joint Surg 78-B:244–249
Judet T, Piriou P, Garreau de Loubrese C. (2001) Prothese de tete radiale a cupule flottante; Cahiers d’enseignement de la SOFCOT, Protheses du coude, Allieu Y, Masmejean E, Elsevier ed Pag 257–263
Kaas L, van Riet RP, JPAM V et al (2010) The epidemiology of radial head fractures. J Shoulder Elbow Surg 19:520–523
King G, Zarzour Z, Patterson S et al (2001) An anthropometric study of the radial head: implications in the design of a prosthesis. J Arthroplasty 16(1):112–116
King GJ, Evans DC, Kellam JF (1991) Open reduction and internal fixation of radial head fractures. J Orthop Trauma 5:21–28
King GJ, Zarzour ZD, Rath DA et al (1999) Metallic radial head arthroplasty improves valgus stability of the elbow. Clin Orthop 368:114–125
King GJW (2004) Management of comminuted radial head fractures with replacement arthroplasty. Hand Clin 20:429–441
Knight DJ, Rymaszewski LA, Amis AA et al (1993) Primary replacement of the fractured radial head with a metal prosthesis. J Bone Joint Surg Br 75:572–576
Liow RY, Cregan A, Nanda R et al (2002) Early mobilization for minimally displaced radial head fractures is desirable. A prospective randomized study of two protocols. Injury 33:801–806
Markolf KL, Tejwani SG, O’Neil G et al (2004) Load-sharing at the wrist following radial head replacement with a metal implant. A cadaveric study. J Bone Joint Surg Am 86:1023–1030
Martinelli B (2008) The Swanson radial head prosthesis. In: Celli A, Celli L, Morrey BF (eds) Treatment of elbow lesions. Springer, Milan/New York, pp 145–148
Mason ML (1954) Some observations on fracture of the head of the radius with a review of one hundred cases. Br J Surg 42:123–132
Miller GK, Drennan DB, Maylahn DJ (1981) Treatment of displaced segmental radial-head fractures. Long-term follow-up. J Bone Joint Surg Am 63:712–717
Monica JT, Mudgal CS (2010) Radial head arthroplasty. Hand Clin 26(3):403–410
Moro JK, Werier J, MacDermid JC et al (2001) Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg 83A:1201–1211
Morrey BF (2009) Surgical exposures of the elbow. In: Morrey BF, Sanchez-Sotelo J (eds) The elbow and its disorders, 4th edn. Sanders-Elsevier, Philadelphia, pp 115–142
Morrey BF, Chao EY, Hui FC (1979) Biomechanical study of the elbow following excision of the radial head. J Bone Joint Surg 61A:63–68
Morrey BF, Askew L, Chao EY (1981) Silastic prosthetic replacement for the radial head. J Bone Joint Surg Am 63:454–458
Morrey BF, An KN, Stormont TJ et al (1988) Force transmission through the radial head. J Bone Joint Surg Am 70:250–256
Morrey BF, Tanaka S, An KN (1991) Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop Relat Res 265:187–195
O’Driscoll S, Jupiter J, Cohen M et al (2003) Difficult elbow fractures: pearls and pitfalls. Instr Course Lect 52:113–134
O’Driscoll SW, Bell DF, Morrey BF (1991) Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am 73:440–446
Patel VR, Elliott DS (1999) Salvage of the head of the radius after fracturedislocation of the elbow. A case report. J Bone Joint Surg Br 81:306–308
Pfaeffle HJ, Stabile KJ, Li ZM et al (2005) Reconstruction of the interosseous ligament restores normal forearm compressive load transfer in cadavers. J Hand Surg 30(2):319–325
Pomianowski S, Morrey BF, Neale PG et al (2001) Contribution of monoblock and bipolar radial head prostheses to valgus stability of the elbow. J Bone Joint Surg Am 83:1829–1834
Popovic N, Gillet P, Rodriguez A et al (2000) Fracture of the radial head with associated elbow dislocation: results of treatment using a floating radial head prosthesis. J Orthop Trauma 14:171–177
Rabinowitz RS, Light TR, Havey RM et al (1994) The role of the interosseous membrane and triangular fibrocartilage complex in forearm stability. J Hand Surg Am 19:385–393
Radin EL, Riseborough EJ (1966) Fractures of the radial head. A review of eighty-eight cases and analysis of the indications for excision of the radial head and non-operative treatment. J Bone Joint Surg Am 48:1055–1064
Ricon FJ, Sanchez P, Lajara F et al (2012) Result of a pyrocarbon prosthesis after comminuted and unreconstructable radial head fractures. J Shoulder Elbow Surg 21(1):82–91
Ring D (2004) Load-sharing at the wrist following radial head replacement with a metal implant. A cadaveric study. J Bone Joint Surg Am 86-A:2569–2570
Ring D (2008) Displaced, unstable fractures of the radial head: fixation vs. replacement: what is the evidence? Injury 39:1329–1337
Ring D (2011) Radial head fracture: open reduction internal fixation or prosthetic replacement. J Shoulder Elbow Surg 20(Suppl 2):S107–S112
Ring D, King G (2008) Radial head arthroplasty with a modular metal spacer to treat acute traumatic elbow instability: surgical technique. J Bone Joint Surg Am 90:63–73
Ring D, Quintero J, Jupiter JB (2002) Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am 84-A:1811–1815
Rolla PR, Surace MF, Bini A et al (2006) Arthroscopic treatment of fractures of the radial head. Arthroscopy 22:233–236
Rotini R, Marinelli A, Guerra E et al (2012) Radial head replacement with unipolar and bipolar SBi system: a clinical and radiographic analysis after a 2-year mean follow-up. Musculoskelet Surg 96(Suppl 1):S69–S79
Rozental TD, Beredjiklian PK, Bozentka DJ (2003) Longitudinal radioulnar dissociation. J Am Acad Orthop Surg 11:68–73
Shepard MF, Markolf KL, Dunbar AM (2001) Effects of radial head excision and distal radial shortening on load-sharing in cadaver forearms. J Bone Joint Surg Am 83-A:92–100
Shore BJ, Mozzon JB, MacDermid JC et al (2008) Chronic posttraumatic elbow disorders treated with metallic radial head arthroplasty. J Bone Joint Surg Am 90(2):271–280
Smets S, Govaers K, Jansen N et al (2000) The floating radial head prosthesis for comminuted radial head fractures: a multicentric study. Acta Orthop Belg 66:353–358
Smith GR, Hotchkiss RN (1996) Radial head and neck fractures: anatomic guidelines for proper placement of internal fixation. J Shoulder Elbow Surg 5:113–117
Sowa DT, Hotchkiss RN, Weiland AJ (1995) Symptomatic proximal translation of the radius following radial head resection. Clin Orthop Relat Res 317:106–113
Soyer AD, Nowotarski PJ, Kelso TB et al (1998) Optimal position for plate fixation of complex fractures of the proximal radius: a cadaver study. J Orthop Trauma 12:291–293
Szekeres M, Chinchalkar SJ, King GJ (2008) Optimizing elbow rehabilitation after instability. Hand Clin 24:27–38
Tejwani NC, Mehta H (2007) Fractures of the radial head and neck: current concepts in management. J Am Acad Orthop Surg 15:380–387
Tornetta P, Hochwald N, Bono C et al (1997) Anatomy of the posterior interosseous nerve in relation to fixation of the radial head. Clin Orthop Relat Res 345:215–218
Van Glabbeek F, Van Riet RP, Baumfeld JA et al (2004) Detrimental effects of overstuffing or understuffing with a radial head replacement in the medial collateral-ligament deficient elbow. J Bone Joint Surg Am 86:2629–2635
Van Glabbeek F, van Riet RP, Baumfeld JA et al (2005) The kinematic importance of radial neck length in radial head replacement. Med Eng Phys 27:336–342
Van Riet RP, Morrey BF (2008) Documentation of associated injuries occurring with radial head fracture. Clin Orthop Relat Res 466:130–134
van Riet RP, Van Glabbeek F, Verborgt O et al (2004) Capitellar erosion caused by a metal radial head prosthesis. A case report. J Bone Joint Surg 86A:1061–1064
Van Riet RP, Van Glabbeek F, de Weerdt W et al (2007) Validation of the lesser sigmoid notch of the ulna as a reference point for accurate placement of a prosthesis for the head of the radius: a cadaver study. J Bone J Surg Br 89:413–416
Van Tongel A, Macdonald P, Van Riet R et al (2012) Elbow arthroscopy in acute injuries. Knee Surg Sports Traumatol Arthrosc 20(12):2542–2548
Vanderwilde RS, Morrey BF, Melberg MW et al (1994) Inflammatory arthritis after failure of silicone rubber replacement of the radial head. J Bone Joint Surg Br 76:78–81
Weseley MS, Barenfeld PA, Eisenstein AL (1983) Closed treatment of isolated radial head fractures. J Trauma 23:36–39
Worsing RA Jr, Engber WD, Lange TA (1982) Reactive synovitis from particulate Silastic. J Bone Joint Surg Am 64:581–585
Yamaguchi K, Sweet FA, Bindra R et al (1997) The extraosseous and intraosseous arterial anatomy of the adult elbow. J Bone Joint Surg Am 79:1653–1662
Yeoh KM, King GJ, Faber KJ et al (2012) Evidence-based indications for elbow arthroscopy. Arthroscopy 28(2):272–282
Zwingmann J, Welzel M, Dovi-Akue D et al (2013) Clinical results after different operative treatment methods of radial head and neck fractures A systematic review and meta-analysis of clinical outcome Injury, Int. J. Care Injured 44:1540–1550
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Celli, A., Kantar, S.S. (2018). Radial Head Fracture: Synthesis or Prosthetic Replacement. In: Porcellini, G., Rotini, R., Stignani Kantar, S., Di Giacomo, S. (eds) The Elbow. Springer, Cham. https://doi.org/10.1007/978-3-319-27805-6_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-27805-6_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-27803-2
Online ISBN: 978-3-319-27805-6
eBook Packages: MedicineMedicine (R0)