Abstract
Solitary fibrous tumors form a complex spectrum of neoplasms, at least part of which were previously related to perivascular cells and thus termed hemangiopericytomas. The classical solitary fibrous tumor, occurring in the form of several variants, typically develops in the pleuropulmonary compartment, but also exists in certain visceral organs, including the liver. Rare variants are those which contain components with hemangiopericytoma-like features. In addition to these lesions, there still exist so-called true hemangiopericytomas, neoplasms that typically occur in the meninges and the sinonasal space. In the liver, primary solitary fibrous presents as well-circumscribed and expanding lesions with fibroma-like features. Histologically, the neoplasms are cellular tumors composed of spindle cells looking different from fibroblasts and myofibroblasts. These cells are arranged in a storiform pattern or form dense sheaths surrounding slit-like vascular channels. The origin of the cells is not yet elucidated. Solitary fibrous tumors show recurrent breakpoints in 12q13, associated with frequent deletions affecting STAT6, caused by somatic fusions of two genes, NAB2 and STAT6.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Solitary Fibrous Tumor
- Vinyl Chloride Monomer
- Malignant Solitary Fibrous Tumor
- Recurrent Breakpoint
- Hepatic Ligament
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
ICD-O codes:
Solitary fibrous tumor | 8815/1 |
Hemangiopericytoma including lipomatous hemangiopericytoma | 9150/1 |
Introduction
This group of tumors was previously thought to be derived from specialized cells supporting blood vessels, i.e., pericytes and glomus cells, leading to the term hemangiopericytoma. The lesion was first described in 1942 as a vascular tumor featuring Zimmermann’s pericytes (Stout and Murray 1942). In 2002, the WHO tumor classification system reclassified soft tissue tumors known so far as hemangiopericytomas as a variant of solitary fibrous tumor. In particular, cellular solitary fibrous tumor is regarded as a synonym of hemangiopericytoma (Park and Araujo 2009). Solitary fibrous tumors represent a heterogeneous group of spindle cell neoplasms with a biological behavior varying between benign and low-grade malignant phenotypes. The term, solitary fibrous tumor (SFT), is now preferred to the former term, hemangiopericytoma, all the more so because the cell of origin is still disputed (Penel et al. 2012). In the WHO classification, solitary fibrous tumor is listed in the intermediate (rarely metastasizing) category, characterizing neoplasms that are often locally aggressive but may have the capability to give rise to distant metastases in some patients, the risk of such a metastatic phenotype being less than 2 % and not predictable from the histologic presentation. Solitary fibrous tumor has several subgroups, comprising fibrous, cellular, fat cell-containing, and giant cell variants. The cellular variant, showing a hypercellular component exceeding 90 % of the tumor, covers most of the “classical” hemangiopericytomas (Knösel et al. 2010). The fat cell-containing variant was previously termed lipomatous hemangiopericytoma, and the variant rich in giant cells is equivalent to giant cell angiofibroma.
Currently, a small spectrum of tumors with a hemangiopericytoma-like pattern may be considered (Table 1). However, recent molecular genetic findings suggest that the entire spectrum of lesions may be separated into two major groups, i.e., classic pleuropulmonary SFT showing the most common NAB2-STAT6 fusion variant, mainly occurring in older patients and having a more favorable course, and deep-seated hemangiopericytomas showing the second most common NAB2-STAT6 fusion variant, occurring in much younger patients, and having a more aggressive phenotype (Barthelmess et al. 2014).
Hemangiopericytoma was described in 1942 as a relatively uncommon distinctive vascular tumor thought to be derived from Zimmermann’s pericapillary pericytes (Stout and Murray 1942). Pericytes, identified in 1873 already (Rouget 1873) and analyzed in detail in 1923 (Zimmermann 1923), are dendritic or arborizing cells with multilineage features, arranged along capillaries and venules. In addition to their cases, Stout and Murray cite one or possibly two cases of hemangiopericytoma in a group of vascular tumors described in 1937 (Schmidt 1937) which this author, following the suggestion of Orsos (1934), termed gemmangiomata (gemmangiomas). The features of this neoplasm were characterized in more detail in the following years (Stout 1949; 1956; McMaster et al. 1975; Enzinger and Smith 1976; Mentzel et al. 1994; Nappi et al. 1995; Spitz et al. 1998), also in context with related tumors and the question as to the true entity of hemangiopericytoma (Gengler and Guillou 2006; Park and Araujo 2009). Pericytes can differentiate along fibroblastoid, myoid, osseous, and adipocyte lineages, what is of importance for the understanding of tumors derived thereof, because some pericytomas can develop a myoid component or produce neoplastic adipocytes (lipomatous hemangiopericytomas) (fat-forming solitary fibrous tumors; Lee and Fletcher 2011). Related tumors comprise myofibromatosis and the so-called infantile hemangiopericytoma, glomangiopericytoma, myopericytoma, and perivascular myoma. As most of the hepatic primary manifestations of this tumor category were described under the term hemangiopericytoma, this label will sometimes be used in addition to solitary fibrous tumor in the following paragraphs.
Epidemiology
Solitary fibrous tumor typically presents in adult individuals. Among 106 cases analyzed, the mean age at presentation was 45 years. The tumors were usually deep-seated lesions (Enzinger and Smith 1976). The tumors occupy clinically and biologically characteristic anatomical locations, including meningeal, cerebral, orbital, sinunasal, osseous, pulmonary, pleural, soft tissue, and visceral tumors. The tumors also occur in the pediatric age group (Fernandez-Pineda et al. 2011), including the entity of multicentric infantile hemangiopericytoma (Sulit et al. 2011). For hepatic SFT, the tumors develop more frequently in females, and the mean age at diagnosis was 55.8 years (Vennarecci et al. 2005). In an earlier study of nine patients, seven patients were female and two male, with an age range at presentation of 32–83 years (mean, 57.5 years; Moran et al. 1998). A recent review of 38 published cases listed 26 female and 12 male patients (Liu et al. 2013). In one investigation, hepatic hemangiopericytoma was associated with occupational exposure to vinyl chloride monomer (Hozo et al. 2000). Most reports concerning primary hepatic SFT described single cases or very small series of this neoplasm.
Selected References
Kim and Damjanov 1983; Kottke-Marchant et al. 1989; Kasano et al. 1991; Bost et al. 1995; Barnoud et al. 1996; Chan 1997; Khalifa et al. 1997; Levine and Rose 1997; Lecesne et al. 1998; Guglielmi et al. 1998; Moran et al. 1998; Fuksbrumer et al. 2000; Vaswani et al. 2000; Yilmaz et al. 2000; Lin et al. 2001; Saint-Marc et al. 2002; Chithriki et al. 2004; Neeff et al. 2004; Vennarecci et al. 2005; Moser et al. 2005; Changku et al. 2006; Ji et al. 2006; Jia et al. 2006; Lehmann et al. 2006; Nath et al. 2006; Terkivatan et al. 2006; Kwak et al. 2007; Obuz et al. 2007; Weitz et al. 2007; Chen et al. 2008; El-Khouli et al. 2008; Kandpal et al. 2008; Korkolis et al. 2008; Perini et al. 2008; Novais et al. 2010; Huanca et al. 2011; Güray Durak et al. 2013; Liu et al. 2013.
Hemangiopericytoma/Solitary Fibrous Tumor of the Liver
Clinical Features
Primary SFTs exhibit a clinical presentation that is non-characteristic in most patients, but particularly in the case of large tumors, abdominal distension, right upper quadrant or periumbilical pain, nausea, weight loss, and abnormal liver tests may occur. Hepatic SFT is a rare lesion, and metastatic disease may be difficult to exclude in a given patient owing to the peculiar biology of these neoplasms (Balouet and Destombes 1967; Bergnach 1967; Weitzner 1970; Klein et al. 1971; Wyrick and Wren 1975; Roesler et al. 1985; Thapa et al. 1986; Sano et al. 1991; Zornig et al. 1992; Maeda and Nakaba 1995; Noda et al. 1995; Flores-Stadler et al. 1997; Campion et al. 1999; Hozo et al. 2000; Kruskal and Kane 2002; Ghiur et al. 2003; Plikat et al. 2003; Caruso et al. 2009; Bokshan et al. 2012). In one series, tumor size ranged from 2 to 32 cm in diameter, and the largest weight of a published tumor was 4725 g (Vennarecci et al. 2005). The tumors can grow to such a large size that resection is not feasible, even in the absence of remote disease (Bergnach 1967). Primary hepatic SFT/hemangiopericytoma can present as a multicentric tumor with cystic cavernoma-like areas (Klein et al. 1971).
Part of the hepatic lesions have been reported to show an aggressive course (malignant hemangiopericytoma; Thapa et al. 1986; Sano et al. 1991; Yilmaz et al. 2000; Ghiur et al. 2003; Plikat et al. 2003; Chan et al. 2007; Seijas et al. 2009; Peng et al. 2011; Jakob et al. 2013). These lesions exhibit an invasive phenotype, can traverse the liver capsule, infiltrate the abdominal wall, and give rise to metastasis either in the liver or in extrahepatic sites. Frankly malignant variants may present with abdominal hemorrhage due to tumor rupture. In one patient SFT of the liver exhibited local recurrence 6 years after resection, and histologic examination of the recurrent tumor displayed features of an aggressive form of SFT (Brochard et al. 2010). In a given case, it is difficult to judge what the biologic course will probably be, although hypercellular parts with increased nuclear atypia and elevated proliferative activity have been observed, suggesting low-grade malignant transformation (Fuksbrumer et al. 2000).
Several observations document an association between SFT/hemangiopericytomas and sometimes severe hypoglycemia, a syndrome called non-islet cell tumor hypoglycemia (NICTH), tumor-associated hypoglycemia (TAH), and the Doege-Potter syndrome (Paullada et al. 1968; Wegmann et al. 1994; Adams et al. 1999), a phenomenon also known for primary SFT/hemangiopericytoma of the liver (Weitzner 1970; Guglielmi et al. 1998; Campion et al. 1999; Kruskal and Kane 2002; Plikat et al. 2003; Bokshan et al. 2012), related to the production of insulin-like growth factor II (ILGF-II) and caused by loss of imprinting of the respective gene (Sohda and Yun 1996; Grunenberger et al. 1999), or by ILGF-II- and ILGF-binding protein 6 (Hoekman et al. 1999), by these neoplasms. Tumor-associated hypoglycemia has also been detected in a patient with hepatic fibrosarcoma (Immerman et al. 1982).
Imaging Features
Hepatic solitary fibrous tumors/hemangiopericytomas are usually solitary lesions, but multicentricity has also been reported (Klein et al. 1971). Sonographically, a complex mass with hyper-isoechoic solid components and hypoechoic cystic areas was described (Caruso et al. 2009). Speckled calcifications may be found. Administration of contrast media in CT and MR imaging reflects the high vascularization of the lesions, showing early, intense, and prolonged enhancement (Caruso et al. 2009). Scintigraphically, large cold nodules in the liver have been reported in a patient with multifocal tumor (Klein et al. 1971). In MR pictures, solid tumor masses prevail, sometimes with a large central necrosis (Plikat et al. 2003).
Macroscopic Pathology
Similar to tumors in other locations, the neoplasms form well-circumscribed and expanding lesions and usually form solid masses of gray to reddish or tan color. The tissue is firm, similar to that of fibromas. The tumors often exhibit partial or apparently complete encapsulation, sometimes with a typically shiny capsule, or formation of a pseudocapsule with perifocal liver atrophy. The cut surface is lobulated. Part of the tumors exhibit whorled and fasciculated cut surface (Korkolis et al. 2008). Hemorrhages may occur, while gross necrosis is unusual, at least in primary tumors. However, very large tumors have shown extensive geographic and sometimes infarctoid central necrosis (Moran et al. 1998). Both gross necrosis and hemorrhage have been encountered (Guglielmi et al. 1998). Some primary hepatic tumors grow to large or huge size (Kottke-Marchant et al. 1989; Guglielmi et al. 1998; Fuksbrumer et al. 2000), and masses up to 22 cm in diameter have been seen (Weitzner 1970), with a weight exceeding 4 kg (Chan et al. 2007). Central cystic cavities have been reported (Barnoud et al. 1996), and the hepatic lesions rarely present as a cyst containing a hemorrhagic fluid and mural tumor nodules of varying size (Klein et al. 1971). SFT with a multiloculated cystic appearance has also been described (Güray Durak et al. 2013). An expanding growth mode prevails, with the adjacent liver showing marked compression atrophy and signs of vascular engorgement. Secondary vascular and/or bile duct compression is sometimes found, and local invasive growth can be encountered, including invasion of intrahepatic veins (Fuksbrumer et al. 2000). Rarely, a pedunculated growth pattern has been seen (Moran et al. 1998; Park et al. 2011). Hepatic SFT belongs to the category of liver neoplasm causing capsular retraction (Blachar et al. 2009).
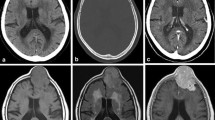
Histopathology
SFTs are often cellular tumors composed of spindle cells with a rather poorly developed and only slightly eosinophilic cytoplasm. These cells, which look different from both fibroblasts and myofibroblasts, either form a short storiform (so-called patternless) pattern or dense sheaths surrounding slit-like vascular channels (Figs. 1, 2, and 3). The latter pattern previously raised the suspicion that the cells might represent a pericyte or a pericyte-like cell. In most cells, the cytoplasm is not well delineated, and the nuclei are hyperchromatic and either spindled in shape or plump. Mitotic figures are usually rare, but one may find areas with 5–10 mitoses per ten high-power fields. The cellular lesions are traversed by a characteristic vascular ramifying tree showing a “staghorn” pattern. In silver stains, the tumor displays a very dense network of reticulin fibers, which encircle groups of spindle cells or even single cells, and is usually more dense in proximity of blood vessels (the pericapillary reticulin sheath; Stout 1949). In part of cases, an inflammatory response with lymphocytes and mast cells may be encountered. Focal myxoid change may occur (Korkolis et al. 2008), an alteration that can dominate SFT presentation in extrahepatic tumors (myxoid SFT; Lau et al. 2009).
Electron Microscopy
Electron microscopically, the tumor cells are closely apposed, but show poor development of cell-to-cell junctions. The organelle content of cells is highly variable and non-characteristic. Flocculent basement membrane material is deposited linearly along the surface of many tumor cells (Flores-Stadler et al. 1997).
Immunohistochemistry
Immunohistochemically, the majority of the tumor cells are markedly reactive for vimentin, and staining for BCL-2, CD99, and alpha-1 antitrypsin is at least focally present (Patra et al. 2012; Liu et al. 2013). Endothelia of the intervening vessels and part of the spindle cells are CD34 positive (Fig. 4; Hanau and Miettinen 1995; Barnoud et al. 1996; Kwak et al. 2007; Korkolis et al. 2008; Peng et al. 2011). CD34 reactivity is considered characteristic for SFT (Brunnemann et al. 1999). Part of hepatic SFT expressed VEGF in a pattern resembling that of proliferating hemangiomas, and some of the cells were reactive for factor XIIIa, similar to the interstitial cells of cellular hemangiomas of infancy (Flores-Stadler et al. 1997). A subpopulation of factor XIIIa-positive cells was identified, similar to the “interstitial cells” of cellular hemangiomas of infancy (Flores-Stadler et al. 1997). At least part of the tumors exhibit nuclear reactivity for STAT6 (Doyle et al. 2013; Schweizer et al. 2013; Barthelmess et al. 2014), linked to NAB2-STAT6 fusion (see below). Immunoreactivity for cytokeratins, epithelial membrane antigen (EMA), desmosomal proteins, S-100 protein, smooth muscle actin, and desmin is usually lacking, although keratin positivity has been reported in one instance (Kim and Damjanov 1983).
Solitary Fibrous Tumor/Hemangiopericytoma of Hepatic Ligaments
Hemangiopericytoma/SFT rarely develops in the ligamentum teres of the liver (Majnarich and Stout 1960) and in the falciform ligament (Gidwani et al. 2004).
Differential Diagnosis
SFTs/hemangiopericytomas primary to diverse locations can extensively metastasize to the liver (van Assendelft et al. 1984; Chakravarty et al. 1991; Nakamura et al. 2005; Alberti et al. 2006; Balaji et al. 2008; Cheng et al. 2008; Zalinski et al. 2009; Balibrea et al. 2013). Among these neoplasms, meningeal hemangiopericytoma is particularly prone to metastasize to the liver (Buccauw et al. 2011). The metastases can cause paraneoplastic non-islet cell hypoglycemia due to production of IGF-II (Bell and Buist 1981; Sohda and Yun 1996; Lawson et al. 2009). Intra-abdominal SFT/hemangiopericytoma located close to the liver and/or extensively spreading may mimic hepatic localizations of this tumor, e.g., peritoneal spread (Prakash et al. 2009; Reicks and Wilkinson 2011).
Molecular Genetic Alterations
In SFT, chromosome banding and FSH showed recurrent breakpoints in 12q13, associated with frequent deletions affecting STAT6. This feature is associated with somatic fusions of the two genes, NGFI-A-binding protein 2 (NAB2) and STAT6, and nuclear expression of the C-terminal part of STAT6 (Chmielecki et al. 2013; Mohajeri et al. 2013; Robinson et al. 2013; Schweizer et al. 2013; Barthelmess et al. 2014; Koelsche et al. 2014). In a series of 52 cases of SFT, 12 different NAB2-STAT6 fusion variants were detected in 92 % of cases. Immunohistochemically, all tumors showed strong and diffuse nuclear reactivity for STAT6 (Barthelmess et al. 2014). The NAB2-STAT6 fusion was also found in meningeal hemangiopericytomas (Schweizer et al. 2013). NAB2 is the transcriptional regulator NGFI-A-binding protein 2, a protein which functions in the nucleus to activate or repress transcription, in part through interaction with nucleosome remodeling and deacetylase complexes. NAB2 regulates and modulates the expression levels of the tumor necrosis factor (TNF) family member TNF-related apoptosis inducing ligand/TRAIL (Balzarolo et al. 2013). SFT also strongly expresses the GRIA2 gene (Vivero et al. 2014), encoding a protein of the ionotropic AMPA glutamate receptor.
Putative Cellular Origins
The cell of origin and the histogenesis of solitary fibrous tumors have not been elucidated so far, but putative mesothelial or primitive mesenchymal cells have been suggested. What is the evidence for the involvement of a mesenchymal progenitor cell? One argument is based on the finding of several lines of differentiation in solitary fibrous tumors: (1) fibrous variant, (2) cellular variant (more than 90 % cellularity), (3) adipocyte-forming variant (fat-forming SFT; lipomatous hemangiopericytoma), (4) giant cell-rich variant (giant cell angiofibroma with floret cells, including the vascular variant), (5) myxoid SFT, (6) synchronous pleuro-renal and renal solitary tumor, and (7) malignant solitary fibrous tumors. Based on electron microscopic investigations showing a mixture of mesenchymal cells and cells with features of mesothelia, a submesothelial origin of the tumor has been proposed (Kottke-Marchant et al. 1989; Barnoud et al. 1996). However, the convincing demonstration of SFTs at extrapleural sites strongly argues against its mesothelial or submesothelial origin. Parts of the cells are reactive for CD99 and CD34, and ultrastructurally the dominant cell population exhibits some degree of myofibroblastic differentiation, focal smooth muscle features, and undifferentiated cells in a perivascular location (Ide et al. 2005; Rodriguez-Gil et al. 2009). The involvement of a perivascular cell is also supported by the fact that solitary fibrous tumors may show transition to hemangiopericytomas (the hemangiopericytoma/solitary fibrous spectrum; Park and Araujo 2009). In fact, soft tissue with hemangiopericytoma-like growth patterns can now be divided into three categories, as summarized in the Table, and one of these categories is the solitary fibrous tumor group (Knösel et al. 2010). Therefore, a CD34-reactive fibroblastoid and vessel-associated progenitor cell may histogenetically be involved, but such a putative mesenchymal stem cell has not yet been identified in the normal liver. A common or characteristic cytogenetic anomaly has not been detected so far (Torabi et al. 2008; Torres-Olivera et al. 2009).
References
Adams J, Lodge JP, Parker D (1999) Liver transplantation for metastatic hemangiopericytoma associated with hypoglycemia. Transplantation 67:488–489
Alberti C, Benea G, Kopf B, De Giorgi U (2006) Hepatic metastases of hemangiopericytoma: contrast-enhanced MRI, contrast-enhanced ultrasonography and angiography findings. Cancer Imaging 6:56–59
Balaji R, Khoo JB, Sittampalam K, Chee SK (2008) CT imaging of malignant metastatic hemangiopericytoma of the parotid gland with histopathologic correlation. Cancer Imaging 8:186–190
Balibrea JM, Rovira-Argelaques M, Otero-Pineiro AM, Julian JF, Carrato C, Navinés J et al (2013) Multifocal hepatic cystic mass as first manifestation of metastatic spinal hemangiopericytoma. Int J Surg Case Rep 4:15–18
Balouet G, Destombes P (1967) Apropos of several apparently primary hepatic mesenchymatous tumours. Trial classification and diagnosis of spindle cell tumours of the liver (in French). Ann Anat Pathol (Paris) 12:273–286
Balzarolo M, Watzl C, Medema JP, Wolkers MC (2013) NAB2 and EGR-1 exert opposite roles in regulating TRAIL expression in human natural killer cells. Immunol Lett 151:61–67
Barnoud R, Arvieux C, Pasquier D, Pasquier B, Letoublon C (1996) Solitary fibrous tumour of the liver with CD34 expression. Histopathology 28:551–554
Barthelmess S, Geddert H, Boltze C, Moskalev EA, Bieg M, Suîrbu H, Brors B, Wiemann S et al (2014) Solitary fibrous tumors (SFTs)/hemangiopericytomas (HPCs) with different variants of the NAB2-STAT6 gene fusion are characterized by specific histomorphology and distinct clinicopathological features. Am J Pathol 184:1209–1218
Bell GM, Buist TA (1981) Arterial embolization in the management of liver tumour with recurrent hypoglycaemia. Postgrad Med J 57:534–536
Bergnach A (1967) On a case of perithelioma of the liver (in Italian). Friuli Med 22:1037–1048
Blachar A, Federle MP, Sosna J (2009) Liver lesions with hepatic capsular retraction. Semin Ultrasound CT MR 30:426–435
Bokshan SL, Doyle M, Becker N, Nalbantoglu I, Chapman WC (2012) Hepatic hemangioendothelioma/solitary fibrous tumor: a review of our current understanding and case study. J Gastrointest Surg 16:2170–2176
Bost F, Barnoud R, Peoc’h M, Le Marc’hadour F, Pasquier D, Pasquier B (1995) CD34 positivity in solitary fibrous tumor of the liver. Am J Surg Pathol 19:1334–1335
Brochard C, Michalak S, Aubé C, Singeorzan C, Fournier HD, Laccourreye L, Calès P et al (2010) A not so solitary fibrous tumor of the liver. Gastroenterol Clin Biol 34:716–720
Brunnemann RB, Ro JY, Ordonez NG, Mooney J, El-Naggar AK, Ayala AG (1999) Extrapleural solitary fibrous tumor: a clinicopathologic study of 24 cases. Mod Pathol 12:1034–1042
Buccauw K, Sciot R, Wolter P, Aerts R, Claus F (2011) Delayed liver metastasis of a meningeal solitary fibrous tumor. Acta Gastroenterol Belg 74:567–569
Campion JP, Gerard O, Dien F, Ramee MP, Turlin B (1999) Primary liver hemangiopericytoma associated with hypoglycemia: report of a second case. Hepatogastroenterology 46:1944–1948
Caruso S, Gruttadauria S, Mivervini MI, Miraglia R, Milazzo M, Luca A, Gridelli B (2009) Primary hemangiopericytoma of the liver: sonographic findings. J Clin Ultrasound 37:305–307
Chakravarty BJ, Munn S, Lane MR (1991) Hepatic metastasis from a meningeal haemangiopericytoma. Aust N Z J Med 21:884–885
Chan JKC (1997) Solitary fibrous tumor of the liver: everywhere, and a diagnosis in vogue. Histopathology 31:568–576
Chan G, Horton PJ, Thyssen S, Lamarche M, Nahal A, Hill DJ, Marliss EB, Metrakos P (2007) Malignant transformation of a solitary fibrous tumor of the liver and intractable hypoglycemia. J Hepatobiliary Pancreat Surg 14:595–599
Changku J, Shaohua S, Zhicheng Z, Shusen Z (2006) Solitary fibrous tumor of the liver: retrospective study of reported cases. Cancer Invest 24:132–135
Chen JJ, Ong SL, Richards C, Garcea G, Pollard C, Berry D, Dennison A (2008) Inaccuracy of fine-needle biopsy in the diagnosis of solitary fibrous tumour of the liver. Asian J Surg 31:195–198
Cheng NY, Chen RC, Chen TY, Tu HY (2008) Contrast-enhanced ultrasonography of hepatic metastasis of hemangiopericytoma. J Ultrasound Med 27:667–671
Chithriki M, Jaibaji M, Vandermolen R (2004) Solitary fibrous tumor of the liver with presenting symptoms of hypoglycemic coma. Am Surg 70:291–293
Chmielecki J, Crago AM, Rosenberg M, O’Connor R, Walker SR, Ambrogio L, Auclair D et al (2013) Whole-exome sequencing identifies a recurrent NAB2-STAT6 fusion in solitary fibrous tumors. Nat Genet 45:131–132
Doyle LA, Vivero M, Fletcher CD, Mertens F, Hornick JL (2013) Nuclear expression of STAT6 distinguishes solitary fibrous tumor from histologic mimics. Mod Pathol. doi:10.1038/modpathol.2013.164
El-Khouli RH, Geschwind JF, Bluemke DA, Kamel IR (2008) Solitary fibrous tumor of the liver: magnetic resonance imaging evaluation and treatment with transarterial chemoembolization. J Comput Assist Tomogr 32:769–771
Enzinger FM, Smith BH (1976) Hemangiopericytoma. An analysis of 106 cases. Hum Pathol 7:61–82
Fernandez-Pineda I, Parida L, Jenkins JJ, Davidoff AM, Rao BN, Rodriguez-Galindo C (2011) Childhood hemangiopericytoma: review of St Jude Children’s Research Hospital. J Pediatr Hematol Oncol 33:356–359
Flores-Stadler EM, Chou P, Walterhouse D, Bourtsos E, Gonzalez-Crussi F (1997) Hemangiopericytoma of the liver: immunohistochemical observations, expression of angiogenic factors, and review of the literature. J Pediatr Hematol Oncol 19:449–454
Fuksbrumer MS, Klimstra D, Panicek DM (2000) Solitary fibrous tumor of the liver: imaging findings. AJR Am J Roentgenol 175:1683–1687
Gengler and Guillou 2006. http://www.ncbi.nlm.nih.gov/pubmed/16359538
Ghiur M, Serbanoiu D, Nicolescu D, Ghiur L, Zbuchea A (2003) Malignant liver hemangiopericytoma ruptured after an abdominal traumatism (in Romanian). Chirurgia (Bucur) 98:249–251
Gidwani AL, Mullan FJ, Kenny B (2004) Solitary fibrous tumour of the falciform ligament containing multiple foci of malignant transformation. J Clin Pathol 57:546–547
Grunenberger F, Bachellier P, Chenard MP, Massard G, Caraman PL, Perrin E, Zapf J et al (1999) Hepatic and pulmonary metastases from a meningeal hemangiopericytoma and severe hypoglycemia due to abnormal secretion of insulin-like growth factor: a case report. Cancer 85:2245–2248
Guglielmi A, Frameglia M, Iuzzolino P, Martignoni G, De Manzoni G, Laterza E, Veraldi GF et al (1998) Solitary fibrous tumor of the liver with CD34 positivity and hypoglycemia. J Hepatobiliary Pancreat Surg 5:212–216
Güray Durak M, Sagol Ö, Tuna B, Ertener Ö, Ünek T, Karademir S, Dicle O (2013) Cystic solitary fibrous tumor of the liver: a case report. Turk Patoloji Derg 29:217–220
Hanau CA, Miettinen M (1995) Solitary fibrous tumor: histological and immunohistochemical spectrum of benign and malignant variants presenting at different sites. Hum Pathol 26:440–449
Hoekman K, van Doorn J, Gloudemans T, Maassen JA, Schuller AG, Pinedo HM (1999) Hypoglycaemia associated with the production of insulin-like growth factor II and insulin-like growth factor binding protein 6 by a haemangiopericytoma. Clin Endocrinol (Oxf) 51:247–253
Hozo I, Miric D, Bojic L, Giunio L, Lusic I, Culic V, Simunic M (2000) Liver angiosarcoma and hemangiopericytoma after occupational exposure to vinyl chloride monomer. Environ Health Perspect 108:793–795
Huanca L, Webb P, Ruiz E (2011) Hepatic solitary fibrous tumor (in Spanish). Rev Gastroenterol Peru 31:376–380
Ide F, Obara K, Mishima K, Saito I, Kusama K (2005) Ultrastructural spectrum of solitary fibrous tumor: a unique perivascular tumor with alternative lines of differentiation. Virchows Arch 446:646–652
Immerman SC, Sener SF, Khandekar JD (1982) Causes and evaluation of tumor-induced hypoglycemia. Arch Surg 117:905–908
Jakob M, Schneider M, Hoeller I, Laffer U, Kaderli R (2013) Malignant solitary fibrous tumor involving the liver. World J Gastroenterol 19:3354–3357
Ji Y, Fan J, Xu Y, Zhou J, Zeng HY, Tan YS (2006) Solitary fibrous tumor of the liver. Hepatobiliary Pancreat Dis Int 5:151–153
Jia C, Shi S, Zhao Z, Zhen S (2006) Solitary fibrous tumor of the liver: retrospective study of reported cases. Cancer Invest 24:132–135
Kandpal H, Sharma R, Gupta SD, Kumar A (2008) Solitary fibrous tumour of the liver: a rare imaging diagnosis using MRI and diffusion-weighted imaging. Br J Radiol 81:e282–e286
Kasano Y, Tanimura H, Tabuse Y, Nagai Y, Mori K, Minami K (1991) Giant fibrous mesothelioma of the liver. Am J Gastroenterol 86:379–380
Khalifa MA, Montgomery EA, Azumi N, Gomes MN, Zeman RK, Min KW, Lack EE (1997) Solitary fibrous tumors: a series of lesions, some in unusual sites. South Med J 90:793–799
Kim H, Damjanov I (1983) Localized fibrous mesothelioma of the liver. Report of a giant tumor studied by light and electron microscopy. Cancer 52:1662–1665
Klein W, Marx E, Hurter J, Huth F (1971) Multicentric hemangiopericytoma of the liver with cystic cavernoma-like areas (in German). Zentralbl Chir 96:387–391
Knösel T, Schulz B, Katenkamp K, Katenkamp D, Petersen I (2010) Solitary fibrous tumor and hemangiopericytoma: what is new ? (in German). Pathologe 31:123–128
Koelsche C, Schweizer L, Renner M, Warth A, Jones DTW, Sahm F, Euss DE, Capper D, Knösel T et al (2014) Nuclear relocation of STAT6 reliably predicts NAB2-STAT6 fusion for the diagnosis of solitary fibrous tumour. Histopathology 65:613–622
Korkolis DP, Apostolaki K, Aggeli C, Plataniotis G, Gontikakis E, Volanaki D, Sebastiadou M et al (2008) Solitary fibrous tumor of the liver expressing CD34 and vimentin: a case report. World J Gastroenterol 14:6261–6264
Kottke-Marchant K, Hart WR, Broughan T (1989) Localized fibrous tumor (localized fibrous mesothelioma) of the liver. Cancer 64:1096
Kruskal JB, Kane RA (2002) Paraneoplastic hypoglycemia associated with a hepatic hemangiopericytoma. J Ultrasound Med 21:927–932
Kwak SY, Gwak GY, Yun WK, Kim HJ, Do IG, Joh JW, Park CK (2007) A case of solitary fibrous tumor of the liver (in Korean). Korean J Hepatol 13:560–564
Lau SK, Weiss LM, Chu PG (2009) Myxoid solitary fibrous tumor: a clinicopathologic study of three cases. Virchows Arch 454:189–194
Lawson EA, Zhang X, Crocker JT, Wang WL, Klibanski A (2009) Hypoglycemia from IGF2 overexpression associated with activation of fetal promoters and loss of imprinting in a metastatic hemangiopericytoma. J Clin Endocrinol Metab 94:2226–2231
Lecesne R, Drouillard J, Le Bail B, Saric J, Balabaud C, Laurent F (1998) Localized fibrous tumor of the liver: imaging findings. Eur Radiol 8:36–38
Lee JC, Fletcher CD (2011) Malignant fat-forming solitary fibrous tumor (so-called “lipomatous hemangiopericytoma”): clinicopathologic analysis of 14 cases. Am J Surg Pathol 35:1177–1185
Lehmann C, Mourra N, Tubiana JM, Arrivé L (2006) Solitary fibrous tumor of the liver (in French). J Radiol 87:139–142
Levine TS, Rose DS (1997) Solitary fibrous tumor of the liver. Histopathology 30:396–397
Lin YT, Lo GH, Lai KH, Tsai CC, Pan HB, Tseng HH, Lo YS (2001) Solitary fibrous tumor of the liver. Zhonghua Yi Xue Za Zhi (Taipei) 64:305–309
Liu Q, Liu J, Chen W, Mao S, Guo Y (2013) Primary solitary fibrous tumors of liver: a case report and literature review. Diagn Pathol 8:195
Maeda S, Nakaba H (1995) Hemangiopericytoma of the liver (in Japanese). Ryoikibetsu Shokogun Shirizu 7:339–341
Majnarich G, Stout AP (1960) Hemangiopericytoma of the ligamentum teres of the liver; report of a case. Am J Surg 100:740–743
McMaster MJ, Soule EH, Ivins JC (1975) Hemangiopericytoma. A clinicopathologic study and long-term followup of 60 patients. Cancer 36:2232–2244
Mentzel T, Calonie E, Nascimento AG, Fletcher CD (1994) Infantile hemangiopericytoma versus infantile myofibromatosis. Study of a series suggesting a continuous spectrum of infantile myofibroblastic lesions. Am J Surg Pathol 18:922–930
Mohajeri A, Tayebwa J, Collin A, Nilsson J, Magnussen L, von Steyern FV, Brosjö O et al (2013) Comprehensive genetic analysis identifies a pathognomonic NAB2/STAT6 fusion gene, non-random secondary genomic imbalances, and a characteristic gene expression profile in solitary fibrous tumor. Genes Chromosomes Cancer 52:873–886
Moran CA, Ishak KG, Goodman ZD (1998) Solitary fibrous tumor of the liver: a clinicopathologic and immunohistochemical study of nine cases. Ann Diagn Pathol 2:19–24
Moser T, Nogueira TS, Neuville A, Riehm S, Averous G, Weber JC, Veillon F (2005) Delayed enhancement pattern in a localized fibrous tumor of the liver. AJR Am J Roentgenol 184:1578–1580
Nakamura S, Fukui M, Takeshita H, Tsuji Y, Murata H, Kubo T (2005) Malignant solitary fibrous tumor of the thigh accompanied by hypoglycemic coma. A case report. Anticancer Res 25:2461–2464
Nappi O, Ritter JH, Pettinato G, Wick MR (1995) Hemangiopericytoma: histopathological pattern or clinicopathologic entity? Semin Diagn Pathol 12:221–232
Nath DS, Rutzik AD, Sielaf TD (2006) Solitary fibrous tumor of the liver. AJR Am J Roentgenol 187:W187–W190
Neeff H, Obermaier R, Technau-Ihling K, Werner M, Kurtz C, Imdahl A, Hopt UT (2004) Solitary fibrous tumour of the liver: case report and review of the literature. Langenbecks Arch Surg 389:293–298
Noda N, Hasegawa H, Kanai M, Shimizu Y, Yoshida H, Matsumoto T, Akita M (1995) Recurrent hemangiopericytoma of the liver: report of a case. Surg Today 25:72–75
Novais P, Robles-Medranda C, Pannain VL, Barbossa D, Biccas B, Fogaça H (2010) Solitary fibrous tumor: is surgical approach the best option ? J Gastrointest Liver Dis 19:81–84
Obuz F, Secil M, Sagol O, Karademir S, Topalak O (2007) Ultrasonography and magnetic resonance imaging of solitary fibrous tumor of the liver. Tumori 93:100–102
Orsos F (1934) Gefässsprossgeschwulst (Gemmangioma). Beitr Path Anat 93:121
Park MS, Araujo DM (2009) New insights into the hemangiopericytoma/solitary fibrous tumor spectrum of tumors. Curr Opin Oncol 21:327–331
Park HS, Kim YK, Cho BH, Moon WS (2011) Pedunculated hepatic mass. Liver Int 31:541
Patra S, Vij M, Venugopal K, Rela M (2012) Hepatic solitary fibrous tumor: report of a rare case. Indian J Pathol Microbiol 55:236–238
Paullada JJ, Lisci-Garmilla A, Gonzales-Angulo A, Jurado-Mendoza J, Quijano-Narezo M, Gomez-Peralta L, Doria-Medina M (1968) Hemangiopericytoma associated with hypoglycemia. Metabolic and electron microscopic studies of a case. Am J Med 44:990–999
Penel N, Amela EY, Decanter G, Robin YM, Marec-Berard P (2012) Solitary fibrous tumors and so-called hemangiopericytoma. Sarcoma 2012:690251
Peng L, Liu Y, Ai Y, Liu Z, He Y, Liu Q (2011) Skull base metastases from a malignant solitary fibrous tumor of the liver. A case report and literature review. Diagn Pathol 6:127
Perini MV, Herman P, D’Albuquerque LA, Saad WA (2008) Solitary fibrous tumor of the liver: report of a rare case and review of the literature. Int J Surg 6:396–399
Plikat K, Reichle A, Elmlinger MW, Schölmerich J (2003) Hypoglycemia associated with the production of insulin-like growth factor (IGF)-II by a hemangiopericytoma (in German). Dtsch Med Wochenschr 128:257–260
Prakash M, Mumtaz HA, Sodhi KS, Kapoor R, Khandelwal N (2009) Hemangiopericytoma: an unusual cause of peritoneal carcinomatosis. Cancer Imaging 9:32–34
Reicks M, Wilkinson N (2011) Recurrent peritoneal hemangiopericytoma. Am Surg 77:E65–E66
Robinson DR, Wu YM, Kalyana-Sundaram S, Cao X, Lonigro RJ, Sung YS, Chen CL et al (2013) Identification of recurrent NAB2-STAT6 gene fusions in solitary fibrous tumor by integrative sequencing. Nat Genet 45:180–185
Rodriguez-Gil Y, Gonzalez MA, Carcavilla CB, Santamaria JS (2009) Lines of cell differentiation in solitary fibrous tumor: an ultrastructural and immunohistochemical study of 10 cases. Ultrastruct Pathol 33:274–285
Roesler A, Schreyer T, Keller E, Storkel S (1985) Hemangiopericytoma of the liver (in German). Roentgenblätter 38:58–59
Rouget C (1873) Mémoire sur le développement, la structure et propriétés physiologiques des capillaires sanguins et lymphatiques. Arch Physiol Norm Pathol 5:603
Saint-Marc O, Pozzo A, Causse X, Heitzmann A, Debillon G (2002) Solitary fibrous liver tumor: clinical, radiological and pathological characteristics (in French). Gastroenterol Clin Biol 26:171–173
Sano T, Terada T, Hayashi F, Kiribuchi Y, Setoyama R, Kawano N, Hatakeyama S (1991) Malignant hemangiopericytoma of the liver: report of a case. Jpn J Surg 21:462–465
Schmidt H (1937) Zur Kenntnis des Gemmangioms und seiner Beziehungen zum Angiosarkom. Frankfurt Ztschr Path 51:43
Schweizer L, Koelsche C, Sahm F, Piro RM, Capper D, Reuss DE, Pusch S, Habel A et al (2013) Meningeal hemangiopericytoma and solitary fibrous tumors carry the NAB2-STAT6 fusion and can be diagnosed by nuclear expression of STAT6 protein. Acta Neuropathol 125:651–658
Seijas R, Ares O, Sierra J, Pérez-Dominguez M (2009) Oncogenic osteomalacia: two case reports with surprisingly different outcomes. Arch Orthop Trauma Surg 129:533–539
Sohda T, Yun K (1996) Insulin-like growth factor II expression in primary meningeal hemangiopericytoma and its metastasis to the liver accompanied by hypoglycemia. Hum Pathol 27:858–861
Spitz FR, Bouvet M, Pisters PW, Pollock RE, Feig BW (1998) Hemangiopericytoma: a 20-year single-institution experience. Ann Surg Oncol 5:350–355
Stout AP (1949) Hemangiopericytoma: a study of 26 cases. Cancer 2:1027–1054
Stout AP (1956) Tumors featuring pericytes: glomus tumor and hemangiopericytoma. Lab Invest 5:217–223
Stout AP, Murray MR (1942) Hemangiopericytoma: a vascular tumor featuring Zimmermann’s pericytes. Ann Surg 116:26–33
Sulit DJ, Tom WL, Willert JR, Nespeca MP, Friedlander SF (2011) Multicentric infantile hemangiopericytoma: case report and review of the literature. J Pediatr Hematol Oncol 33:e166–e170
Terkivatan T, Kliffen M, de Witt JH, van Geel AN, Eggermont AM, Verhoef C (2006) Giant solitary fibrous tumour of the liver. World J Surg Oncol 4:81
Thapa BR, Narasimharao KL, Marwaha RK, Walia BN, Bannerjee CK, Mitra SK, Pathak IC (1986) Malignant hemangiopericytoma of liver. Indian Pediatr 23:551–553
Torabi A, Leie SM, DiMaio D, Pinnt JC, Hess MM, Nelson M, Bridge JA (2008) Lack of a common or characteristic cytogenetic anomaly in solitary fibrous tumor. Cancer Genet Cytogenet 181:60–64
Torres-Olivera FJ, Vargas MT, Torres-Gomez FJ, Trigo I, Diaz M, Gonzalez-Campora R (2009) Cytogenetic, fluorescence in situ hybridization, and immunohistochemistry studies in a malignant pleural solitary fibrous tumor. Cancer Genet Cytogenet 189:122–126
van Assendelft AH, Strengell-Usanov L, Kastarinen S (1984) Pulmonary haemangiopericytoma with multiple metastases. Eur J Respir Dis 65:380–383
Vaswani K, Guttikonda S, Vitellas KM (2000) Localized fibrous tumor of the liver. AJR Am J Roentgenol 175:875–876
Vennarecci G, Ettorre GM, Giovanelli L, Del Nonno F, Perracchio L, Visca P, Corazza V et al (2005) Solitary fibrous tumor of the liver. J Hepatobiliary Pancreat Surg 12:341–344
Vivero M, Doyle LA, Fletcher CDM, Mertens F, Hornick JL (2014) GRIA2 is a novel diagnostic marker for solitary fibrous tumour identified through gene expression profiling. Histopathology 65:71–80
Wegmann W, Vonesch HJ, Kamber J, Kiss D (1994) Recurrent and metastasizing hemangiopericytoma of the meninges with paraneoplastic hypoglycemia (in German). Schweiz Med Wochenschr 124:146–151
Weitz J, Klimstra DS, Cymes K, Jarnagin WR, D’Angelica M, La Quaglia MP, Fong Y et al (2007) Management of primary liver sarcomas. Cancer 109:1391–1396
Weitzner S (1970) Primary hemangiopericytoma of liver associated with hypoglycemia. Report of a case. Am J Dig Dis 15:673–678
Wyrick WJ, Wren HB (1975) Primary hepatic intra-abdominal hemangiopericytoma. J Ark Med Soc 71:247–248
Yilmaz S, Kirimlioglu V, Ertas E, Hilmioglu F, Yildirim B, Katz D, Mizrak B (2000) Giant solitary fibrous tumor of the liver with metastasis to the skeletal system successfully treated with trisegmentectomy. Dig Dis Sci 45:168–174
Zalinski S, Goumard C, Scatton O, Terris B, Plantier F, Dupin N, Soubrane O (2009) Liver recurrence of a subcutaneous temporal hemangiopericytoma: the index case. J Gastrointest Surg 13:1155–1159
Zimmermann KW (1923) Der feinere Bau der Blutkapillaren. Z Anat Entwicklungsgesch 68:29
Zornig C, Kremer B, Henne-Bruns D, Weh HJ, Schröder S, Brölsch CE (1992) Primary sarcoma of the liver in the adult. Report of five surgically treated patients. Hepatogastroenterology 39:319–321
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this entry
Cite this entry
Zimmermann, A. (2017). Solitary Fibrous Tumor/Hemangiopericytoma of the Liver. In: Tumors and Tumor-Like Lesions of the Hepatobiliary Tract. Springer, Cham. https://doi.org/10.1007/978-3-319-26956-6_61
Download citation
DOI: https://doi.org/10.1007/978-3-319-26956-6_61
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26954-2
Online ISBN: 978-3-319-26956-6
eBook Packages: MedicineReference Module Medicine