Abstract
There exists an extensive body of literature examining the value of intraoperative recurrent laryngeal nerve monitoring (IONM) during thyroid and parathyroid surgery. These studies have advanced the understanding of electrophysiologic nerve monitoring and culminated in the publication of an international standards guideline statement. This chapter reviews the value of intraoperative nerve monitoring with a specific interest in its application regarding parathyroid surgery. The rationale for monitoring is addressed in the context of the unique circumstances of parathyroid surgery. Furthermore, the expected value of nerve monitoring for the intraoperative decision process, techniques, and equipment, as well as contemporary trends and future directions of IONM are covered.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
There exists an extensive body of literature examining the value of intraoperative recurrent laryngeal nerve monitoring (IONM) during thyroid and parathyroid surgery. These studies have advanced the understanding of electrophysiologic nerve monitoring and culminated in the publication of an international standards guideline statement. Most studies, though, have been an admixture of both thyroid and parathyroid surgical cases with varying indications in which parathyroid surgical cases represent the minority of cases. This chapter reviews the value of intraoperative nerve monitoring with a specific interest in its application regarding parathyroid surgery.
Electrophysiologic Recurrent Laryngeal Nerve Monitoring
Rationale for Monitoring
The location of the recurrent laryngeal nerves (RLN) adjacent to the thyroid gland and in close anatomic proximity to the parathyroid glands leads to the risk of RLN injury either from a rare parathyroid carcinoma disease process (Fig. 36.1) or during parathyroid surgery, most commonly performed for nonmalignant hyperparathyroidism. Injury rates to the RLN can vary significantly among surgeons, but the rate of permanent RLN injury after initial surgery for primary hyperparathyroidism (HPT) has been consistently lower than 1 % in large retrospective studies that have originated from experienced centers [1, 2]. Concern has been raised that the rate is most likely higher when performed by less experienced surgeons [3]. Complications in the reoperative setting are more common secondary to extensive scarring, obfuscation of dissection planes and anatomic relationships, and proximity of the disease that necessitates reoperation to the RLN [4].
Temporary hoarseness can occur after any surgery that involves general anesthesia, but the potential for RLN injury in parathyroid surgery mandates greater concern when hoarseness occurs after this type of procedure [5]. The other nerves of major interest, which are frequently less directly addressed during parathyroid surgery, are the bilateral superior laryngeal nerves (SLN) , injury to which can impair the ability to change pitch and reduce voice projection [6]. The obvious result of vocal fold paralysis (VFP) is loss of voice. In addition, debilitation can result from dysphagia and aspiration; an important role of the larynx is to achieve tight vocal fold closure necessary for normal swallowing. Shortness of breath and exercise intolerance can also result from this lack of closure necessary to Valsava [7]. Finally, the most dreaded of concerns is the life-threatening loss of airway patency and respiratory distress if a bilateral injury were to occur that would potentially necessitate a tracheostomy.
There has been a recent report looking at the impact of unilateral or bilateral (VCF) following thyroid surgery. The cost analysis could be similarly applicable to patients sustaining injury after parathyroid surgery. Seventy six patients who sustained either unilateral or bilateral (VCF) were compared to 238 patients who did not have injury during thyroid surgery. The two groups are matched to age, sex, race, and type of procedure. The authors found that, “patients who suffer a unilateral or bilateral VFP after undergoing thyroidectomy experience significantly more morbidity than similar patients who do not have VFP after thyroidectomy. The VFP patients incurred significantly more charges for health care in the first 90 days after surgery ([8]; Benninger et al. 2015).”
The avoidance of nerve injury in parathyroid surgery is centered on injury prevention measures that begin not during surgery but rather at the time of the initial evaluation of the patient. This evaluation is coupled with intraoperative and postoperative management decisions that optimize patient outcome. A detailed history, review of pathology, outside surgical records if applicable, and review of surgical indications with the patient and family are necessary to assess risk for any patient being considered for parathyroid surgery.
Experienced surgeons with low nerve complication rates are guided by principles to which they adhere with great discipline. Meticulous hemostasis throughout the surgical procedure cannot be overemphasized. It affords the surgeon with a clear view, often aided with loupe magnification, of the operative field to identify critical anatomic landmarks that lead to the identification of the RLN [7]. Recurrent laryngeal nerve visualization is currently considered the gold standard for nerve preservation [9]. It is associated with a lower risk of RLN palsy [10, 11].
The precise handling of tissue around the nerve to prevent stretch or traction injury on the nerve is of utmost importance. There is limited data in the literature to suggest that approximately 10 % of nerves that are traumatized are visually identified and appreciated as injured by the surgeon [3]. This places further emphasis on the importance of tissue handling and management of hemostasis. Nerve transection, which would generally be appreciated by surgeons who routinely identify the nerve, the standard for nerve protection, may not be as common of a contemporary reason for nerve injury.
Unique Circumstances in Parathyroid Surgery
Parathyroid surgery, in general, is an elective procedure without the acute threat of morbidity or mortality associated with malignancy. While guidelines exist for surgical candidacy, many patients present in an asymptomatic or low symptom profile state secondary to incidental blood testing that led to the diagnosis of hyperparathyroidism. This often healthier population carries an expectation for a lower treatment complication rate than that associated with other conditions. Although nerve identification is a routine practice for most surgeons during thyroid surgery, the same assumption cannot be extrapolated to parathyroid surgery. Many experienced and high-volume parathyroid surgeons do not routinely find the RLN nor certainly the SLN in each case. A particularly vulnerable and common area for nerve injury during thyroid surgery is at the ligament of Berry, where an extralaryngeal RLN bifurcation is susceptible to nerve injury [12]. This particular area does not have the same significance in parathyroid surgery, where the parathyroid gland does not have to be removed off the trachea at the ligament of Berry and thus does not place the nerve at the same level of risk for heat, traction, or transection risk. Recommendation has been made for surgeons though to have a low threshold for identifying the RLN during parathyroid surgery [13, 14]. There is no substitute for identifying the nerve to reduce inadvertent nerve injury rates [15].
Nevertheless, as discussed elsewhere in this book, changing practice patterns with evidence-based support for directed parathyroid surgery utilizing very small incisions, minimally invasive endoscopic approaches, or even remote access approaches does raise the concern for potential RLN or SLN nerve injury due to limited exposure for dissection. This risk is compounded by the aforementioned minority of nerve injuries that are even appreciated by surgeons intraoperatively. Recurrent laryngeal nerve monitoring may be valuable in identifying and confirming the location of the RLN [16, 17]. Because the frequency of RLN injury is low among experienced surgeons, who are a primary source of evidence-based surgical studies examining IONM, it is difficult to adequately power studies to provide evidence of its value in preventing nerve injuries [10, 18]. Furthermore, many experienced surgeons may commonly perform routine parathyroid procedures under local anesthesia because they believe the risk of nerve injury is quite low and the clinical scenario would not warrant IONM.
An interesting recent publication has examined the anatomic proximity of parathyroid tumors to the RLN in patients with primary hyperparathyroidism undergoing parathyroidectomy [16]. This is unique from much of the literature that primarily combines both thyroid and parathyroid patients. In this prospective study consisting of 136 patients with primary hyperparathyroidism, IONM was used to confirm RLN identification and to record the distance from the anatomically confirmed RLN to the parathyroid tumor. The findings confirmed that the RLN often lies in close proximity to the parathyroid adenoma at an average of just 0.52 cm, with tumors of the right upper position most commonly abutting the nerve compared to other positions. The tumors in the right upper position were on average only 0.25 cm from the nerve with 47 % of the tumors in the right upper position abutting the nerve [16]. This may clearly have implications for a personalized approach with consideration for IONM for tumors in this area if a directed approach is taken.
Other circumstances that may also demand consideration for IONM during parathyroid surgery may include difficult parathyroidectomy procedures such as reoperations. The superior parathyroid gland develops in an embryological position posterior to the RLN when viewed in a sagittal plane (Fig. 36.2). Therefore, large superior parathyroid glands and inferiorly descended, ectopic superior thyroid glands behind the RLN in the retroesophageal region may place the RLN at a greater risk. Further consideration should be given for missing parathyroid glands, nonlocalizing preoperative imaging studies, prior neck surgery for spine surgery, trauma or any other reason, morbid obesity, or other patient anatomic factors creating exposure difficulty. These factors can certainly increase technical difficulty and have been shown to increase the rate of RLN injury [12]. IONM can be complimentary and beneficial to direct anatomic visualization of the RLN and perhaps even the SLN if an ectopic gland exploration would demand dissection that could potentially place it at risk (Fig. 36.3).
Expected Value of Nerve Monitoring for the Intraoperative Decision Process
The International Neural Monitoring Study Group, a multidisciplinary international group of surgeons and researchers dedicated to thyroid and parathyroid surgery, and neural monitoring, had proposed three modes listed below for IONM application that are relevant for parathyroid surgery [18].
Identification of the RLN
The application of intraoperative neural monitoring can assist in neural mapping using the neural monitor probe to electrically map the course of the nerve in the paratracheal region. Success for nerve identification rates between 98 and 100 % has been reported in multiple studies [19]. The use of the RLN nerve monitor does not prevent nerve injuries but is an excellent adjunct that may be helpful.
Several large studies have compared a monitored group of patients and a nonmonitored group to determine if there was a difference in RLN injuries. These studies contained both thyroid and parathyroid surgeries with the majority of patients undergoing thyroid surgery. The documentation of proof that the use of nerve monitoring prevents nerve injury has been elusive for the previously stated reasons, especially for experienced surgeons with low complication rates. This may not be applicable to surgeons in general who perform these procedures. One of the largest of the series was a multi-institutional prospective nonrandomized study of over 16,000 patients who underwent thyroidectomy. The authors concluded that there was no statistical significant difference between visual identification alone and combined visualization with RLN monitoring [10]. Because of the unique circumstances of parathyroid surgery, it is even more unclear and difficult to power a similar study to examine a difference in nerve injury rates for monitored versus unmonitored patients in just parathyroid surgery. It is clear, however, that nerve monitoring will not turn an unsafe surgeon into a safe surgeon [20] and thus the aforementioned points of meticulous technique must always be respected.
Aid in Dissection
After identifying the nerve, stimulation applied in intermittent fashion could provide feedback to assist the dissection. This could be particularly valuable in a reoperative setting to trace the nerve’s course through scar that obscures the field and allow for its dissection off the parathyroid tumor. In a study examining intraoperative electromyographic monitoring of the RLN in reoperative thyroid and parathyroid surgery, 52 cervical re-exploration procedures were performed with electromyography. Thirty one percent of the procedures were for parathyroid conditions (1 parathyroid carcinoma) and this group was compared to a nonmonitored group with similar characteristics. The monitoring did not decrease RLN complications in the study, but the authors did state that locating the RLN was generally not the source of injury, but rather resection of close disease placed the nerve most at risk [4]. The potential to dissect through these obscured planes with close disease utilizing neural monitoring as an adjunct could be valuable.
Neural Function Prognostication
The functional information provided by IONM could be invaluable to the physician who has seen a visually intact nerve but wants further support of its functional status before proceeding to the contralateral side for a four gland exploration. Dissection on the contralateral side could place the other nerve at risk, potentially resulting in a compromised airway at the end of an elective procedure. In other words, a nerve that is compromised on one side may give the surgeon pause to continue on and lead him or her to stage the procedure once an expected return of function on the compromised side has occurred. It would also allow for investigation of the nerve for potentially treatable injuries that would include a crush injury from a suture tie or clip or lead to a primary repair of a discovered transected nerve that had not been appreciated during the initial dissection.
Prevention of bilateral paralysis is perhaps the most important application of IONM. Prior to neural testing there had been no other mechanism to accurately identify the location of nerve injury. Excellent evidence exists that final evoked potential amplitudes on intraoperative electromyography of the RLN correlates with immediate postoperative vocal fold function after thyroid surgery [21, 22]. In this study, the immediate postoperative vocal cord paralysis experience was reviewed when an EMG amplitude of less than 200 μv was set as a cutoff. The sensitivity, specificity, positive and negative predictive values, and accuracy at this level for vocal cord paralysis were found to be 95.5 %, 99.2 %, 72.4 %, 99 %, and 99.1 % respectively. This could certainly be applicable in parathyroid surgery. It would be of great value to the surgeon to alert him or her to the complication before it was clinically evident and therefore allow for preparations to be made, especially if it involved securing a compromised airway.
Although the routine use of neural monitoring in parathyroid surgery is controversial, there are clinicians who are proponents of its routine use to benefit patients. Expert opinion has advocated that neural monitoring be performed routinely because difficult cases cannot always be predicted preoperatively. The routine use of monitoring will allow for an advancement in the learning curve for surgeons so that they have greater experience in signal interpretation and troubleshooting [18, 23].
Technique and Equipment
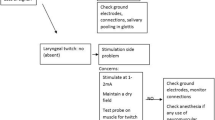
The technique and standards of equipment for electrophysiologic monitoring of the RLN has been comprehensively outlined in the International Standards Guideline Statement from the International Neural Monitoring Study Group [18]. This document further provides an algorithm for evaluating the loss of signal during monitoring and for troubleshooting (Fig. 36.4). Importantly, normative intraoperative electrophysiologic waveform analysis has also been published for both the superior laryngeal nerve external branch and recurrent laryngeal nerve in patients undergoing thyroid surgery [24]. It is incumbent upon the surgeon to be familiar with the techniques available, equipment, and normative values of IONM to gain the desired level of predictive information regarding postoperative RLN function.
Preconditions
Optimization of IONM is contingent upon several elements that have been outlined by the International Neural Monitoring Study Group [18]. These elements include preoperative laryngoscopy in all cases. One of the main values of IONM is to provide information regarding the functional status of the vocal cords; therefore, the baseline status should be known before surgery. Attention should be paid to the vocal exam with a recommendation to strongly consider viewing the vocal folds by indirect laryngoscopy or flexible laryngoscopy for every patient in which surgery is contemplated. Recently multidisciplinary guidelines, “Clinical practice guideline: Improving voice outcomes after thyroid surgery,” have been developed to address voice outcomes in relationship to thyroid surgery [25] and could also be readily applicable to any contemplated parathyroid surgery. This guideline focused on how to address the patient with disordered voice before and after thyroid surgery. The voice could be remarkably normal to perception even in the face of a nerve compromise resulting in vocal fold immobility. This may result in alterations in surgical planning and preparation. Understandably, is also important to perform a postoperative laryngoscopy, a recommendation of the International Neural Monitoring Study Group. Neural stimulation at the end of surgery and postoperative function are highly correlated but not perfect.
Presurgical dissection and postsurgical dissection suprathreshold vagal nerve stimulation have been recommended to respectively verify the IONM system function to have confidence in its accuracy and for testing of the neural circuit after the dissection. The vagal stimulation after the dissection would prevent potential false-negative findings of stimulating a compromised RLN distal to the injury site. It may be uncertain in a focused parathyroid dissection if this would require a larger incision to gain access to the carotid sheath to perform this maneuver. The comfort level of the surgeon to gain this access through limited exposure may be quite variable from surgeon to surgeon when performing parathyroid surgery. This would be an interesting area for future study.
Anesthesia
Standards in anesthesia have been provided by the International Neural Monitoring Study Group [18]. Muscle relaxation should be avoided because the monitoring would be sensitive to neuromuscular blockade. This blockade is avoided during the induction of general endotracheal anesthesia, or if it is necessary during induction, a short-acting agent is needed [20, 26]. Careful and open dialogue with the anesthesia team is necessary for this coordinated team effort.
Equipment
Various methods have been developed to monitor RLN and SLN activity. The vast majority of experiences have examined intermittent RLN monitoring using a probe to stimulate anatomic structures of concern. Continuous stimulation has been described and is discussed later in the chapter under future direction. The most commonly used strategy employs an electromyographic (EMG) system utilizing a specialized endotracheal tube with surface electrodes to monitor activated laryngeal musculature secondary to stimuli including pressure, heat, traction, or intentional stimulation with a probe [20]. Commercial availability and ease of use have made endotracheal tubes with surface electrodes as sensors for RLN monitoring very popular. As previously stated, this would be of no value for those parathyroid surgical cases performed under local anesthesia. Another technique that has been used but requires greater skill, experience, and general anesthesia is the placement of hook electrodes, intramuscular vocal cord electrodes [4, 27]. Finally, postcricoid surface electrodes have been found effective but not used in widespread fashion [28]. General equipment setup including the algorithm for monitoring tube placement intubation, recording and stimulation ground electrodes, patient positioning and tube fixation, and monitor setting (Fig. 36.5) have been well described by International Neural Monitoring Study Group [18], and the International Guidelines Statement serves as an excellent reference.
Contemporary Trends and Future Direction
Although a preponderance of data fails to show that neuromonitoring significantly reduces the rate of nerve injury in thyroid and parathyroid surgery, surgeons seem to be increasingly using the technology [20]. The potential benefits of nerve identification, dissection, prediction of nerve injuries, and reduction in the risk of bilateral RLN injury have been outlined. Surveys have delved into the thought process of surgeons as to why they use IONM. One of the most recent studies was a multi-institutional survey of 103 otolaryngology and affiliated 103 general surgery programs in the United States evaluating trends in intraoperative neural monitoring for thyroid and parathyroid surgery. A majority of otolaryngologists, 80.6 %, and 48 % of general surgeons reported using IONM. Use in all cases was 44.3 % for otolaryngologists and 30.8 % for general surgeons. High-volume surgeons tended to use IONM more. The study results indicated that general surgeons tended to use IONM for RLN identification, and otolaryngologists tended to use it more for dissection, resection, and medicolegal consideration purposes. There appeared to be a discordance in motivation for its use [29].
Finally, preliminary studies are exploring the dynamic assessment of the nerve through continuous vagal monitoring. This could be advantageous to alert the physician regarding EMG changes that may herald an impending nerve injury and allow for modification of surgical maneuvers to reverse the situation [30, 31]. Future studies will be needed to provide data regarding the impact of this strategy on surgical outcomes, particularly as it applies to parathyroid surgery.
Summary
Intraoperative nerve monitoring has been extensively studied in thyroid and parathyroid surgery, but much of the literature has focused primarily on its role in thyroid surgery. Contemporary parathyroid surgery with often a more directed and minimal approach may not necessarily warrant the routine use of IONM for those surgeons who perform this procedure under a general anesthetic. However, there are circumstances in parathyroid surgery where the use of IONM may be very valuable and the knowledge gained from its routine use by a surgeon in endocrine surgery can be of utmost value in those cases. Reoperative parathyroid surgeries, glands adherent to the nerve, ectopic or missing glands, nonlocalizing glands, and patient anatomic constraints will continue to create challenges in the future for surgeons and the use of IONM as a surgical adjunct can prove very helpful despite a lack of literature evidence that it prevents nerve injuries.
Society Guidelines
International Neural Monitoring Study Group and the International Guidelines Statement [18].
Best Practices:
N/A
Expert Opinion
Understanding the value and limitations of intraoperative nerve monitoring as an adjunct in parathyroid surgery is essential for optimization of surgical outcomes specific to the unique circumstances of parathyroid gland surgery. Continued study and development of IONM will refine well-established guidelines that serve as a current template for its use.
References
Allendorf J, DiGorgi M, Spanknebel K, Inabnet W, Chabot J, Logerfo P. 1112 consecutive bilateral neck explorations for primary hyperparathyroidism. World J Surg. 2007;31(11):2075–80. Population/Observational Study: Level 3; Grade A.
Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg. 2002;235(5):665–70. Population/Observational Study: Level 3; Grade A.
Bergenfelz A, Jansson S, Martensson H, Reiner E, Wallin G, Kristoffersson A, Lausen I. Scandinavian Quality Register for Thyroid and Parathyroid Surgery: audit of surgery for primary hyperparathyroidism. Langenbecks Arch Surg. 2007;392(4):445–51. Population/Observational Study: Level 3; Grade A.
Yarbrough DE, Thompson GB, Kasperbauer J, Harper M, Grant C. Intraoperative electromyographic monitoring of the recurrent laryngeal nerve in reoperative thyroid and parathyroid surgery. Surgery. 2004;136(6):1107–15. Population/Observational Study: Level 3; Grade B.
Mendels EJ, Brunings JW, Hamaekers AE, et al. Adverse laryngeal effects following short-term general anesthesia: a systematic review. Arch Otolarygol Head Neck Surg. 2012;117:399–404. Clinical Review: Level 3; Grade B.
Roy N, Smith ME, Dromey C, et al. Exploring the phonatory effects of external superior laryngeal nerve paralysis: an in vivo model. Laryngoscope. 2009;119:816–26. Population/Observational Study: Level 3; Grade A.
Benninger M, Scharpf J. Vocal fold paralysis and thyroid surgery. In: Hanks JB, Inabnet W, editors. Controversies in thyroid surgery. New York: Springer; 2015. Clinical Review: Level N/A; Grade N/A.
Gardner GM, Smith MM, Yaremchuk KL, et al. The cost of vocal fold paralysis after thyroidectomy. Laryngoscope. 2013;123:1455–63. Population/Observational Study: Level 4.
Randolph GW, Kamani D. Intraoperative neural monitoring in thyroid cancer surgery. Langenbecks Arch Surg. 2014;399:199–207. Clinical Review: Level N/A; Grade N/A.
Dralle H, Sekulla C, Haerting J, Timmerman W, Neumann HJ, Kruse E, Grond S, Muhlig HP, Richter C, Voss J, Tomusch O, Lippert H, Gastinger I, Brauckhoff M, Gimm O. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004;136(6):1310–22. Population/Observational Study: Level 3; Grade A.
Hermann M, Alk G, Roka R, Glaser K, Freissmuth M. Laryngeal recurrent nerve injury in surgery for benign thyroid diseases: effect of nerve dissection and impact of individual surgeon in more than 27,000 nerves at risk. Ann Surg. 2002;235(2):261–8. Population/Observational Study: Level 3; Grade A.
Snyder SK, Lairmore TC, Hendricks JC, Roberts JW. Elucidating mechanisms of recurrent laryngeal nerve injury during thyroidectomy and parathyroidectomy. J Am Coll Surg. 2008;1(206):123–30. Population/Observational Study: Level 3; Grade B.
Randolph G, Urken M. Surgical management of primary hyperparathyroidism. In: Randolph G, editor. Surgery of the thyroid and parathyroid glands. Philadelphia: Saunders; 2003. p. 507–28. Clinical Review: Level N/A; Grade N/A.
Harrison B, Triponez F. Intraoperative adjuncts in surgery for primary hyperparathyroidism. Langenbecks Arch Surg. 2009;394:799–809. Clinical Review: Level N/A; Grade N/A.
Miller MC, Spiegel JR. Identification and monitoring of the recurrent laryngeal nerve during thyroidectomy. Surg Oncol Clin N Am. 2008;17:121–44. Clinical Review: Level N/A; Grade N/A.
Untch BR, Adam M, Danko M, Barfield M, Dixit D, Scheri R, Olson J. Tumor proximity to the recurrent laryngeal nerve in patients with primary hyperparathyroidism undergoing parathyroidectomy. Ann Surg Oncol. 2012;19:3823–6. Population/Observational Study: Level 3; Grade A.
Dackiw AP, Rotstein LE, Clark OH. Computer-assisted evoked electromyography with stimulating surgical instruments for recurrent/external laryngeal nerve identification and preservation in thyroid and parathyroid operation. Surgery. 2002;132(6):1100–8. Population/Observational Study: Level 3; Grade B.
Randolph GW, Dralle H, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: International Standards Guideline Statement. Laryngoscope. 2011;121:S1–16. Clinical Review: Level N/A; Grade N/A.
Timmermann W, Hammelmann W, Thomusch O, et al. Effectiveness and results of intraoperative neuromonitoring in thyroid surgery. Statement of the Interdisciplinary Study Group on Intraoperative Neuromonitoring of Thyroid Surgery. Chirurg. 2004;75(9):916–22. Clinical Review: Level N/A; Grade N/A.
Angelos P. Recurrent laryngeal nerve monitoring: state of the art, ethical and legal issues. Surg Clin N Am. 2009;89:1157–69. Clinical Review: Level N/A; Grade N/A.
Genther DJ, Kandil EH, Noureldine SI, Tufano RP. Correlation of final evoked potential amplitudes on intraoperative electromyography of the recurrent laryngeal nerve with immediate postoperative vocal fold function after thyroid and parathyroid surgery. JAMA Otolaryngol Head Neck Surg. 2014;140(2):124–8. Population/Observational Study: Level 3; Grade B.
Genther DJ, Kandil EH, Noureldine SI, et al. Correlation of final evoked potential amplitudes on intraoperative electromyography of the recurrent laryngeal nerve with immediate postoperative vocal cord function after thyroid surgery. Otolaryngol Head Neck Surg. 2014;140:124–8. Population/Observational Study: Level 3; Grade B.
Dionigi G, Bacuzzi A, Boni L, Rovera F, Dionigi R. What is the learning curve for intraoperative neuromonitoring in thyroid surgery? Int J Surg. 2008;6 Suppl 1:S7–12. Population/Observational Study: Level 3; Grade A.
Potenza AS, Phelan EA, Cernea CR, Slough CM, Kamani D, Darr A, Zurakowski D, Randolph G. Normative intra-operative electrophysiologic waveform analysis of super laryngeal nerve external branch and recurrent laryngeal nerve in patients undergoing thyroid surgery. World J Surg. 2013;37:2336–42. Population/Observational Study: Level 3; Grade A.
Chandrasekhar SS, Randolph GW, Seidman MD, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg. 2013;148:S1–37. Clinical Review: Level N/A; Grade N/A.
Hemmerling TM, Schmidt J, Bosert C, et al. Intraoperative monitoring of the recurrent laryngeal nerve in 151 consecutive patients undergoing thyroid surgery. Anesth Analg. 2001;93(2):396–9. Population/Observational Study: Level 3; Grade A.
Tschopp KP, Gottardo C. Comparison of various methods of electrophysiologic monitoring of the recurrent laryngeal nerve in thyroid surgery. Ann Otol Rhinol Laryngol. 2002;111(9):811–6. Population/Observational Study: Level 3; Grade B.
Marcus B, Edwards B, Yoo S, et al. Recurrent laryngeal nerve monitoring in thyroid and parathyroid surgery: the University of Michigan experience. Laryngoscope. 2003;113(2):356–61. Population/Observational Study: Level 3; Grade B.
Ho Y, Carr M, Goldenberg D. Trends in intraoperative neural monitoring for thyroid and parathyroid surgery amongst otolaryngologists and general surgeons. Eur Arch Otorhinolaryngol. 2013;270:2525–30. Population/Observational Study: Level 5.
Schneider R, Randolph GW, Seimer A, et al. Continuous intraoperative vagus nerve stimulation for identification of imminent recurrent nerve injury. Head Neck. 2013;35:1591–8. Population/Observational Study: Level 3; Grade A.
Lamade W, Ulmer C, Seimer A, et al. A new system for continuous recurrent laryngeal nerve monitoring. Minim Invasive Ther Allied Technol. 2007;16:149–54. Population/Observational Study: Level 3; Grade A.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Scharpf, J., Randolph, G. (2017). Intraoperative Nerve Monitoring for Parathyroid Surgery. In: Stack, Jr., B., Bodenner, D. (eds) Medical and Surgical Treatment of Parathyroid Diseases. Springer, Cham. https://doi.org/10.1007/978-3-319-26794-4_36
Download citation
DOI: https://doi.org/10.1007/978-3-319-26794-4_36
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26792-0
Online ISBN: 978-3-319-26794-4
eBook Packages: MedicineMedicine (R0)