Abstract
A non-linear perspective may be relevant to understanding mental disorders, particularly in primary care settings. There is growing evidence that variability in heart rate and mood over time, that non-linearity of a variety of parameters (from heart rate to mood), and that the degree of co-variability of anxiety and depression may be relevant to our understanding of what constitutes mental health and illness as well as their outcomes. In a small study (n = 15) of adult primary care patients with major depressive disorder, panic disorder, or neither disorder, patients recorded hourly levels of anxiety and depression while awake for 4 weeks. Analysis of data employed measures of non-linearity as well as state space grid analysis. Eleven subjects completing the mood diary had missing data rates of 0–2.4 %. Results showed that all three groups differed in their patterns of mood variability and anxiety–depression co-variability. These results suggest that healthy mood variability includes both linear and non-linear components, and that mental illness may represent a disturbance in either of these components or in the coupling between different moods. Such a proposed model is based upon the linear–non-linear relationships between symptoms of anxiety and depression, and how these dynamics change as illness severity increases. If true, then non-linear dynamics may have important clinical implications for classification of mental disorders (necessitating revision in diagnostic approaches and the classification of mental disorders), identification of novel treatments (small but well-timed, pulse interventions or multifaceted, whole patient approaches), and monitoring of dynamics (i.e., cardiac monitoring) and response. For this reason, a dynamical systems approach has been advocated for psychiatrists and psychologists alike, but such advice may be of particular importance to primary care physicians. However, these implications are based upon preliminary evidence that a non-linear, dynamical basis for classification and treatment of mental disorders is more parsimonious than the current linear, symptom level model. Further investigations are needed to assess whether a non-linear, dynamical framework may provide us with a new, yet rewarding, perspective for understanding the emergence and evolution of mental illness.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Traditional views of mental disorders depend upon a mechanistic model which assumes that you can study the parts and thereby understand the whole person. Such approaches assume a linear view, in which you apply a treatment and get a predictable response. Current concepts of classification and treatment of mental disorders are based upon a paradigm (derived from research in mental health settings) that symptoms can be clustered into discrete diagnostic groups and assumes predictability of response. Because patients seeking care from mental health professionals have more severe symptomatology, more impairment, more psychiatric co-morbidity, and a worse disease course but less medical co-morbidity than those in primary care settings [1, 2], we should expect that the dynamics of their symptoms may differ as well. If mental disorders are, contrary to current assumptions, non-linear phenomena (in which the input or magnitude of the intervention is not proportional to the output or response) in primary care patients, then a categorical system of diagnosis may be a “poor fit” for these patients and recognition by rigid criteria would suffer because such phenomena are unpredictable in their dynamics and course. Similarly, disorders with non-linear dynamics would not respond predictably to targeted, single-agent interventions and thus practice guidelines may not hold the same usefulness among primary care patients as they would among those in mental health settings displaying linear dynamics.
In this chapter, we will look at mental illness from a complexity science standpoint, noting that non-linear dynamics may be especially relevant to mentally ill patients seen in primary care settings. Focusing on affective disorders, we will examine the evidence for the importance of dynamics in mental disorders. Finally, we will re-conceptualize affective disorders from a non-linear perspective and identify the clinical implications of such a perspective if it is borne out.
1 Complexity Science in Mental Health
There is a growing realization that “health” is defined by its non-linearity [3]; conversely, illness is associated with loss of variability. Thomasson and Pezard [4] suggest that mental health and psychopathology need to be viewed on a continuum with mental disorders representing bifurcations in mood dynamics. The exact nature of the mood dynamics observed may depend upon the severity of illness, the presence of resources, and social interactions. The fact that mental illness can be controlled but not cured suggests a dynamical disease [5]. Furthermore, when a disorder varies without an obvious cause, it suggests non-linearity resulting from a complex interaction between endogenous and environmental factors [6]. Dynamics assessment has been applied to mood variability in specific disorders. For example, attempts to control problematic thoughts and emotions among patients with generalized anxiety disorder and personality disorders may produce non-linear dynamics [7]. In addition, non-linear dynamics has been suggested as a framework for understanding change in families [8] and family interactions [9]. Recently, Katerndahl et al. [10] found that intimate partner violence demonstrates non-linearity over time for most violent relationships. Both Ehlers [11] and Guastello [12] have extolled the value of non-linear modelling in mental illness.
Even simple systems can display non-linear patterns depending upon their constraints, resources, and interconnections [13]. Non-linear systems can change their behavior and dynamics, moving from randomness to chaos to periodicity based on the state of the system, decreasing the number of possible values of the system as non-linearity decreases. An emerging belief is that, when systems are using healthy, non-linear dynamics, they exhibit adaptability and are resistant to external stressors that might disrupt these healthy dynamics. However, when these systems transition into periodicity due to illness, they become predictable and amenable to intervention, permitting physicians to treat them effectively and hopefully restore the healthy, non-linear dynamics. These considerations then suggest that, even though extreme variability may be detrimental within an illness (such as diabetes) [14], overall non-linearity may be critical to health and well-being. This transition from healthy non-linear dynamics to unhealthy linear dynamics can be understood by realizing that non-linear systems can display a variety of dynamics, depending upon their resources and constraints, interconnectedness, and feedback. But, as the number of chronic medical problems increases, the patient’s resourcefulness, flexibility, and adaptability (and, hence, non-linearity) may decrease, leading to linear dynamics and poor overall health, and suggesting that non-linearity may be particularly important in settings that provide care for patients with chronic medical problems (e.g., primary care). As Fig. 11.1 shows, if we view phenomena as a continuum from linear to non-linear dynamics, the constraining nature of disease severity, co-morbidity, and chronic stress would be expected to suppress health trends towards non-linearity, thus leading to linear dynamics. Recovery from anxiety states, for example, occurs at different rates, and depends upon co-morbidity and disease severity [15]. On the other hand, social interaction and availability of resources with resultant adaptability should encourage the development of non-linear dynamics. Kendler et al. [16] found that familial environment determined symptom expression in major depression. Fone et al. [17] found that poor mental health was associated with low community cohesion and income deprivation. Thus, the dynamics we observe in anxiety and depression may depend upon the severity of their mental illness, chronic stress levels, and co-morbidity as well as social connectedness and support.
1.1 Dynamics and Mental Illness
Understanding the dynamics of a system begins with the study of its variability over time. Recently, mental health research has studied the dynamics and variability (usually, standard deviation across time) of autonomic-related measures such as heart rate, blood pressure and respiration, neurological measures such as brain waves, and, ultimately, mood in a variety of patient groups. Although some of these measures may appear to have little to do with mental illness, many in fact correlate with mood or outcomes. Thus, several affective disorders in general demonstrate decreased variability in heart rate and mood compared with healthy individuals, and such loss of variability may be associated with poorer clinical outcomes. Taken a step further, the degree of non-linearity in dynamics has been evaluated in several mental disorders as well.
Recently, investigators have applied measures of non-linearity and non-linear pattern recognition to the study of mental illness. Non-linearity has been measured using approximate entropy (APEN) and Lyapunov exponent (LE). In addition, the identification of attractors within time series has been sought. Finally, the recognition of particular dynamic patterns (i.e., chaos) has been attempted in time series of mood levels.
APEN is an information-based measure and estimates the lack of regularity in time series [18]. Patients with panic disorder have increased respiratory rate APEN compared with controls [19, 20] and, in fact, paroxetine lowers this APEN [21]. Brain wave activity among depressed patients shows a reduced pre-treatment APEN for their first episode of depression when compared with those having recurrent depression and healthy controls [22]. Although the respiratory APEN among panic disorder patients does not correlate with anxiety severity [20], APEN of EEG measures does correlate with mood and response to treatment [23], and mood APEN correlates with happiness ratings among healthy controls [24]. Thus, APEN measures can distinguish mentally healthy from those who are ill and may correspond to clinical outcomes.
LE, a measure of sensitivity to minor differences in starting points, has also been used in mental health research. For example, LLE of QT intervals is lower in controls than patients with panic disorder or major depression [25] and LE is lower for heart rate but higher for blood pressure in those with panic disorder [26, 27]. Children with anxiety disorders [28] or panic disorder have a lower LE for heart rate than controls [29]. Similarly, LE of respiratory measures is increased in panic disorder [19] and paroxetine lowers these LEs [21]. Based on EEG activity, Bob et al. [30] found increased LEs in most adults with panic disorder and controls when asked to recall a stressful memory. In addition, SSRIs have been found to increase LE, improving OCD and normalizing hyperactivity in the striatum [31]. Healthy individuals uniformly display positive LEs in mood variability [32]. Increased LE in EEG activity correlates with anxiety levels [30], while LE of mood correlates positively with hypomania and negatively with anhedonia scores in healthy individuals [32]. As with APEN, LE measures can distinguish healthy from mentally ill individuals and some LEs may have clinical significance.
Although few studies have attempted to study attractors, depression patterns in bipolar patients suggest that attractors may be important. Few patients (15 %) had an attractor in the healthy symptom range; the majority either had two attractors (35 %) or an unstable pattern (28 %) [33]. Correlation dimension (a measure of the strength of attractors) correlated with pleasant affect (and inversely with anhedonia) among healthy controls [32]. Overall, EEG complexity appears to be reduced in patients with depression [22, 34]; white matter connectivity is increased among patients with panic disorder and connectivity correlates with panic severity [35]. Thus, unstable attractors or strong attractors may be associated with mental disorders.
Whether looking at heart rate variability, brain wave activity, or mood change, healthy individuals differ from those with mental disorders in the degree of non-linearity observed. Overall, studies of HRV demonstrate similar patterns despite the time-scale, suggesting a high degree of interdependence in heart rate [36]. As a result, healthy individuals exhibit more chaotic patterns in heart rate but less chaotic patterns in QT variability than those with mental illness [25], and low-dimensional chaos in mood variability as well [32, 37]. Woyshville et al. [38] found more mood interdependence in patients with affective instability, and Hall et al. [39] found circadian and ultradian patterns of mood variability in both depressed and normal patients. In fact, depressed individuals displayed patterns of combined periodicity and chaos in mood variability [37, 40], while controls displayed these patterns for both heart rate and mood variability [36, 41].
1.2 Examining Mood Dynamics Among Primary Care Patients with Affective Disorders
To explore the relationship between the dynamics of symptoms of anxiety and depression in patients with newly diagnosed major depressive episode or panic disorder, we enrolled five primary care patients each with either panic disorder, major depressive episode or neither disorder. They were asked to record their hourly levels of anxiety and depression using visual analog scales for 1 month. The resultant time series were analyzed using time series analysis, state space grid analysis, and differential structural equation modelling.
1.2.1 Dynamic Patterns of Anxiety/Depression
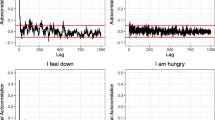
Healthy patients with neither major depression nor panic disorder demonstrated chaotic patterns in hourly mood variability overlaying a linear (circadian) pattern, possibly related to diurnal cortisol levels (see Fig. 11.2a). For example, the healthy 51-year-old female clerk reported a circadian pattern of mood (depression) variation underlying chaotic hourly variation. However, mentally ill patients may lose one or both of these dynamical components. For example, Fig. 11.2b shows the variability in anxiety levels of a 46-year-old male patient with panic disorder who retained his linear diurnal but lost the embedded hourly chaotic pattern, instead displaying more linear-on-linear dynamics. His low level of education (less than high school diploma), lack of employment, and low income further reduced his resources and adaptability, encouraging linear dynamics. On the other hand, Fig. 11.2c shows the variability in hourly levels of depression in a 48-year-old female patient with major depressive episode and bronchitis; while the hourly chaotic pattern was still seen, the linear circadian pattern was lost. Although unemployed, her college education may have allowed her to maintain her adaptive chaotic pattern even though she has lost her circadian cortisol levels. Hence, patients with major depression may lose their circadian baseline while patients with panic disorder may lose their overlying chaos [41].
Hourly variability in level of anxiety/depression among subjects. (a) Depression levels in a healthy 51-year-old female; (b) Linear diurnal changes coupled with linear hourly changes in anxiety levels in a 46-year-old male with panic disorder; (c) Hourly non-linear changes in level of depression without an underlying circadian pattern in a 48-year-old female with major depressive episode
In general, non-linearity in mood correlates with mental health and positive clinical outcomes. This non-linearity may result from the combination of the predictability of periodic circadian dynamics with the responsive minute-to-minute chaotic dynamics. Mental illness may represent an uncoupling of this combined periodicity–chaos with selective alteration of one or both components, leading to an overall reduction in non-linearity of mood.
1.2.2 Dynamic Co-variability of Anxiety and Depression
In addition to patterns of variation for a particular mood (e.g., anxiety), emotional state may reflect the constellation of patterns of various moods combined. In addition, symptom levels of anxiety and depression typically are highly correlated in cross-sectional studies. Yet, lagged correlations in time series are often non-significant [15]. In our study, anxiety and depression were highly correlated in healthy individuals [42], suggesting that healthy individuals may perceive these moods as nonspecific distress [43]. However, anxiety and depression were less-correlated in patients with either major depression or panic disorder, suggesting that such patients perceive these moods as distinct. In addition, while healthy controls reported few, highly stable anxiety–depression configurations (attractors), such attractors were highly unstable in patients with major depression [42]. For example, Fig. 11.3 shows the instability over a 4-week period of the preferred anxiety–depression mood configurations for a 52-year-old female patient with major depressive episode, asthma, hypertension, and reflux esophagitis taking six medications. Not only did these preferred configurations change week-to-week, but at times they split into more than one configuration, further emphasizing mood instability. Furthermore, while anxiety and depression levels are interdependent over time in patients with major depression, panic disorder and controls, the accelerations in these moods were the most interdependent [44].
Thus, the degree of coupling between symptoms of anxiety and depression may be an important measure of co-variability. If tightly linked, then we may observe few, but stable recurrent emotional states. If loosely coupled, we may observe many, transiently stable emotional states.
2 Imperative for Change
Emotional state is a reflection of a person’s inherent mood coupled with their response to their current environment. Toro et al. [45] suggest that cognitions, emotions, perceptions, and behaviors depend upon CNS interconnectedness, and that these interconnections are due to the union of an inherently non-linear system with environmental effects. EEG coherence is lower in those with panic disorder, reflecting decreased inter-hemispheric connectivity [46]. Similarly, although healthy individuals demonstrate a baseline circadian cortisol pattern, levels of cortisol vary with stress. In fact, salivary cortisol levels show different patterns, affected by more than just stress (i.e., work, exhaustion) [47]. Mental illness alters such patterns of mood and cortisol variability. In depression, for example, circadian rhythms are disrupted, possibly due to loss of variability and capacity for variation. In fact, it may be this dysrhythmia in cortisol and/or mood that may produce the depressed state due to either an underlying vulnerability or to mis-attribution [48]. Once depression is established, non-linearity may be enhanced due to increased cortisol reactivity [49] or differing physiological and behavioral time-scales [22]. This biological–psychological interplay is what we would expect under a biotic model in which the simple underlying biological processes change first (biological priority) but ultimately organize into a psychological state which dominates and feeds back upon its biological origins (psychological supremacy) [50].
If we accept that healthy mood variability includes both linear and non-linear components (as in Fig. 11.2a), then mental illness may represent a disturbance in either of these components or in the coupling between different moods. Such a model is proposed based upon the linear-non-linear relationships between symptoms of anxiety and depression, and how these dynamics change as severity increases. As shown in Fig. 11.4, healthy individuals have anxiety and depressive symptoms that strongly covary. So closely coupled are anxiety and depressive symptoms that they may be indistinguishable. Patterns of variation of individual moods (i.e., anxiety levels) have both linear and non-linear components. As the severity of mental illness increases, sub-threshold disorders manifest themselves with loosely coupled anxiety and depression levels; patients can begin to distinguish anxiety and depression from general distress. As distinct disorders emerge, the healthy linear–non-linear individual patterns change; people with depressive disorders lose the linear component to their depressive symptoms as their diurnal cortisol cycle is disrupted (see Fig. 11.2b), while those with anxiety disorders lose their non-linear component (with its minute-to-minute adaptability) to their anxiety symptoms (see Fig. 11.4). At this point, anxiety symptoms clearly differ from depressive symptoms, vary in different patterns, and are independent of each other (see Fig. 11.2c).
Such a dynamical paradigm would carry important clinical implications. First, if diagnostic differences are shown to be more dependent upon differences in dynamics and co-variability rather than disease severity, a non-linear approach could lead to a revision in diagnostic approaches and the classification of mental disorders. Just as linear and non-linear measures in HRV may discriminate between different diagnostic populations [51], such measures applied to mood variability may also have important diagnostic applications [6]. Classification of patients into diagnostic categories may reflect bifurcation points in brain activity [34] or establishment of dysfunctional CNS interconnections [45]. Better understanding of mood dynamics, and the relationship between anxiety and depression may help explain the problems of lack of recognition and treatment adequacy observed in primary care settings.
Second, as mentioned above, measures of non-linearity correlate with clinical outcomes. In healthy populations, non-linear measures correlate with levels of happiness, anhedonia, and hypomania. This suggests that assessment of mood variability via patient-completed mood diaries may have diagnostic and prognostic utility. Recent studies suggest that, as catastrophic events approach, dynamics signs (increased variability and lagged autocorrelations) are sent [52]. Glenn et al. [53] found that APEN of daily mood measurements was higher among bipolar patients who experienced an episode of either mania or depression than those who remained euthymic. In addition, the fact that mood variability patterns are self-similar no matter what the time-scale may be, demonstrating the scale-free power law of interdependence, suggests that non-linearity measures of mood variability could be obtained via in-office computer assessment over a few minutes [32] to be used for diagnostic and prognostic purposes. In fact, because HRV may correlate with clinical outcomes, cardiac monitoring among patients with mental illness may also have clinical applications for following treatment response.
Finally, assessment of non-linear dynamics may have treatment implications, especially at the individual patient level [54]. Although antidepressants, resources, and social interaction may work via their effect on dynamics [48], non-linearity may explain poor treatment response to traditional approaches, limiting the benefits of “cookbook” practice guidelines; management plans will need to be tailored to patients. Hence, initial assessment of dynamics and co-variability may imply that, in those patients displaying non-linear dynamics, standard single-agent approaches will probably not help. Such non-linearity in treatment response is supported by the importance of chronotherapy (timed dosing based on biological rhythms); drug efficacy often varies with the time-of-day [55, 56]. Finally, demonstrating non-linearity and co-variability would attest to the presence of a complex system at work, and suggest novel interventions. Interventions targeting dynamics may have applications here; treatments (such as anti-control interventions) would focus on changing the dynamic pattern (i.e., from periodicity to chaos) rather than on symptom levels [6, 57]. Small but well-timed pulse interventions may be successful in altering dynamics without affecting mood extremes, but yielding improved outcomes [6]. In addition, if non-linear dynamics are found, then multifaceted, whole patient approaches may be more successful than single-agent interventions.
But these implications are based upon the construct that a non-linear, dynamical basis for classification and treatment of mental disorders is more parsimonious than the current linear, symptom level model. However, such a paradigm shift is far from proven. Instead, we are left with many questions. What are the determinants of linear and non-linear dynamics in mood variability? What is the optimal time-frame over which to measure such dynamics? What constitutes an attractor in mood variability? How should co-variability in moods be measured? Before we can begin to address these issues, we need basic, large-scale investigations of patients with affective disorders of varying severity from various clinical settings. Measuring mood levels hourly over an extended period of time, such investigation would need to compare the validity of classification based upon DSM criteria versus classification based on dynamical group in terms of its prognosis, co-morbidity, health-related disability, and treatment response. In addition, data from such patients could be used to determine their co-variability using linear and non-linear measures (such as cross-correlation and cross-APEN) to determine their relative impact compared with DSM classification on clinical outcomes. Such investigations could begin to assess whether a non-linear, dynamical framework may provide us with a new, yet rewarding, perspective for understanding the emergence and evolution of mental illness. Only if these non-linear, dynamical approaches can better predict observations and outcomes will this complex systems perspective supplant the entrenched linear, reductionist paradigm.
3 Conclusion
A non-linear perspective of mental disorders may be particularly relevant to understanding mental disorders, especially in primary care settings. There is growing evidence that non-linearity of a variety of parameters (from heart rate to mood) may be relevant to our understanding of what constitutes mental health and illness. Monitoring of daily anxiety/depression levels among psychiatric patients demonstrates non-linearity, attractors, and covariation. If true, then non-linear dynamics may have important clinical implications for classification of mental disorders, identification of novel treatments, and monitoring of response. For this reason, a dynamical systems approach has been advocated for psychiatrists and psychologists alike [54], but such advice may be of particular importance to primary care physicians.
References
Klinkman M, Schwenk T, Coyne J. Depression in primary care-more like asthma than appendicitis. Can J Psychiatry. 1997;42:966–73.
Wells KB, Burnam A, Camp P. Severity of depression in prepaid and fee-for-service general medical and mental health specialty practices. Med Care. 1995;33:350–64.
Albrecht G, Freeman S, Higginbotham N. Complexity and human health. Cult Med Psychiatry. 1998;22(1):55–92.
Thomasson N, Pezard L. Dynamical systems and depression. Acta Biotheor. 1999;47:209–18.
Belair J, Glass L, van der Heiden U, Milton J, editors. Dynamical disease: mathematical analysis of human illness. Woodbury, NY: American Institute of Physics; 1995.
Heath RA. Complexity and mental health. In: Holt TA, editor. Complexity for clinicians. Abingdon: Radcliffe; 2004.
Warren K, Sprott JC, Hawkins RC. Spirit is willing. Nonlinear Dynamics Psychol Life Sci. 2002;6:55–70.
Koopmans M. Chaos theory and the problem of change in family systems. Nonlinear Dynamics Psychol Life Sci. 1998;2:133–48.
Pincus D. A framework and methodology for the study of nonlinear, self-organizing family dynamics. Nonlinear Dynamics Psychol Life Sci. 2001;5:139–73.
Katerndahl DA, Burge SK, Ferrer RL, Becho J, Wood R. Dynamics of violence. J Eval Clin Pract. 2014;20:695–702.
Ehlers CL. Chaos and complexity. Arch Gen Psychiatry. 1995;52:960–4.
Guastello SJ. Nonlinear dynamics in psychology. Discret Dyn Nat Soc. 2001;6:11–29.
Morrison F. Art of modeling dynamic systems. New York: Wiley; 1991.
Hirsch IB, Brownlee M. Should minimal blood glucose variability become the gold standard of glycemic control? J Diabetes Complicat. 2005;19:178–81.
De Vries MW, Dijkman-Caes CIM, Delespaul PAEG. Sampling of experience. In: Maser JD, Cloninger CR, editors. Comorbidity of mood and anxiety disorders. Washington, DC: American Psychiatric Association; 1990.
Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Familial influences on the clinical characteristics of major depression. Acta Psychiatr Scand. 2007;86:371–8.
Fone D, Dunstan F, Lloyd K, Williams G, Watkins J, Palmer S. Does social cohesion modify the association between area income deprivation and mental health? Int J Epidemiol. 2007;36:1–8. doi:10.1093/ije/dym004.
Pincus SM. Approximate entropy as a measure of irregularity for psychiatric serial metrics. Bipolar Disord. 2006;8:430–40.
Yeragani VK, Radhakrishna RKO, Tancer M, Uhde T. Nonlinear measures of respiration. Neuropsychobiology. 2002;46:111–20.
Caldirola D, Bellodi L, Caumo A, Migliarese G, Perna G. Approximate entropy of respiratory patterns in panic disorder. Am J Psychiatry. 2004;161:79–87.
Yeragani VK, Rao R, Tancer M, Uhde T. Paroxetine decreases irregularity of linear and nonlinear measures of respiration in patients with panic disorder. Neuropsychobiology. 2004;49:53–7.
Pezard L, Nandrino JL, Renault B, El Massioui F, Allilaire JF, Muller J, et al. Depression as a dynamical disease. Biol Psychiatry. 1996;39:991–9.
Thomasson N, Pezard L, Allilaire JF, Renault B, Martinerie J. Nonlinear EEG changes associated with clinical improvement in depressed patients. Nonlinear Dynamics Psychol Life Sci. 2000;4:203–18.
Yeragani VK, Pohl R, Mallavarapu M, Balon R. Approximate entropy of symptoms of mood. Bipolar Disord. 2003;5:279–86.
Yeragani VK, Rao KAR. Nonlinear measures of QT interval series. Psychiatry Res. 2003;117:177–90.
Rao RKA, Yeragani VK. Decreased chaos and increased nonlinearity of heart rate time series in patients with panic disorder. Auton Neurosc. 2001;88:99–108.
Yeragani VK, Mallavarapu M, Radhakrishna RKA, Tech M, Tancer M, Uhde T. Linear and nonlinear measures of blood pressure variability. Depress Anx. 2004;19:85–95.
Yeragani VK, Rao KAR, Pohl R, Jampala VC, Balon R. Heart rate and QT variability in children with anxiety disorders. Depress Anx. 2001;13:72–7.
Srinivasan K, Ashok MV, Vaz M, Yeragani VK. Decreased chaos of heart rate time series in children of patients with panic disorder. Depress Anx. 2002;15:159–67.
Bob P, Kukleta M, Riecansky I, Susta M, Kukumberg P, Jagla F. Chaotic EEG patterns during recall of stressful memory related to panic attack. Physiol Res. 2006;55(1):S113-9.
Kubota S, Sakai K. Relationship between obsessive-compulsive disorder and chaos. Med Hypotheses. 2002;59:16–23.
Schuldberg D, Gottlieb J. Dynamics and correlates of microscopic changes in affect. Nonlinear Dynamics Psychol Life Sci. 2002;6:231–57.
Johnson SL, Nowak A. Dynamical patterns in bipolar depression. Personal Soc Psychol Rev. 2002;6:380–7.
Sarbadhikari SN, Chakrabarty K. Chaos in the brain. Med Eng Phys. 2001;23:445–55.
Han DH, Renshaw PF, Dager SR, Chung A, Hwang J, Daniels MA, et al. Altered cingulated white matter connectivity in panic disorder patients. J Psychiatr Res. 2008;42:399–407.
Cecen AA, Erkal C. Long march: from monofractals to endogenous multifractality in heart rate variability analysis. Nonlinear Dynamics Psychol Life Sci. 2009;13:181–206.
Combs A, Winkle M, Daley C. Chaotic systems analysis of rhythms in feeling states. Psychol Record. 1994;44:359–68.
Woyshville MJ, Lackamp JM, Eisengart JA, Gilliland JAM. On the meaning and measurement of affective instability. Biol Psychiatry. 1999;45:261–9.
Hall DP Jr., Sing HC, Romanoski AJ. Identification and characterization of greater mood variance in depression. Am J Psychiatry. 1991;148:1341–5.
Heiby EM, Pagano IS, Blaine DD, Nelson K. Modeling unipolar depression as a chaotic process. Psychol Assess. 2003;15(3):426–34.
Katerndahl D, Ferrer R, Best R, Wang CP. Dynamic patterns in mood among newly-diagnosed patients with major depressive episode, panic disorder, and normal controls. Prim Care Comp J Clin Psychiatry. 2007;9(3):183–7.
Katerndahl D, Wang CP. Dynamic co-variation of symptoms of anxiety and depression among newly-diagnosed patients with major depressive episode, panic disorder and controls. Nonlinear Dynamics Psychol Life Sci. 2007;11(3):349–65.
Barlow DH, Campbell LA. Mixed anxiety-depression and its implications for models of mood and anxiety disorders. Compr Psychiatry. 2000;41(suppl. 1):55–60.
Katerndahl DA. Power laws in covariability of anxiety and depression among newly-diagnosed primary care patients with major depressive disorder, panic disorder and controls. J Eval Clin Pract. 2009;15:565–70.
Toro MG, Ruiz JS, Talavera JA, Blanco C. Chaos theories and therapeutic commonalities among depression, Parkinson’s disease, and cardiac arrhythmias. Compr Psychiatry. 1999;40:238–44.
Hanaoka A, Kikuchi M, Komuro R, Oka H, Kidani T, Ichikawa S. EEG coherence analysis in never-medicated patients with panic disorder. Clin EEG Neurosc. 2005;36:42–8.
Dahlgren A, Akerstedt T, Kecklund G. Individual differences in the diurnal cortisol response to stress. Chronobiol Int. 2004;21:913–22.
Healy D, Williams JMG. Dysrhythmia, dysphoria, and depression. Psychol Bull. 1988;103:163–78.
Sussman EJ, Dorn LD, Inoff-Germain G, Nottelmann ED, Chrousos GP. Cortisol reactivity, distress behavior, and behavioral and psychological problems in young adolescents. J Res Adoles. 1997;7:81–105.
Sabelli HC. Bios: a study of creation. New Jersey: World Scientific; 2005.
Yeragani VK, Nadella R, Hinze B, Yeragani S, Jampala VC. Nonlinear measures of heart period variability. Depress Anx. 2000;12:67–77.
Scheffer M, Bascompte J, Brock WA, Brovkin V, Carpenter SR, Dakos V, et al. Early-warning signals for critical transitions. Nature. 2009;461:53–9.
Glenn T, Whybrow PC, Rasgon N, Grof P, Alda M, Baethge C, Bauer M. Approximate entropy of self-reported mood prior to episodes in bipolar disorder. Bipolar Disord. 2006;8:424–9.
Tschacher W. Dynamics of psychosocial crises. J Nerv Ment Dis. 1996;184:172–9.
Nagayama H. Influences of biological rhythms on the effects of psychotropic drugs. Psychosom Med. 1999;6:618–29.
Kraft M, Martin RJ. Chronobiology and chronotherapy in medicine. Disease-A-Month 1995;41:503–75.
Christini D, Collins J, Linsay P. Experimental control of high dimensional chaos. Phys Rev E. 1996;54:4824–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Katerndahl, D.A. (2016). Viewing Mental Health Through the Lens of Complexity Science. In: Sturmberg, J. (eds) The Value of Systems and Complexity Sciences for Healthcare. Springer, Cham. https://doi.org/10.1007/978-3-319-26221-5_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-26221-5_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26219-2
Online ISBN: 978-3-319-26221-5
eBook Packages: MedicineMedicine (R0)