Abstract
Radioguided surgery involves utilizing a radiation detection device within the operating room in a real-time fashion to identify a radioisotope that has been administered to a patient prior to the time of attempted detection and for the sole purpose of guiding the successful performance of the surgical procedure. Since its first description in the late 1940s, radioguided surgery has expanded tremendously and has become a well-established discipline within the practice of surgery. It has been investigated and applied to the surgical management of numerous solid malignancies and has most significantly impacted upon the surgical management of breast cancer, melanoma, and parathyroid disease. Radioguided surgery provides the surgeon with critical and real-time information regarding the exact location of the disease and the overall extent of disease burden, as well as allows the surgeon to minimize the degree of surgical invasiveness associated with many commonplace diagnostic and therapeutic surgical procedures, while still maintaining maximum treatment-directed benefits to the patient. As we move forward through the twenty-first century, we envision further growth of the current technological platforms of radioguided surgery, with a continued emphasis upon promoting integration of handheld radiation detection devices and advanced nuclear medicine molecular imaging for guiding and optimizing the intraoperative detection and resection of conditions affecting both cancer and noncancer patients.
Portions of the contents of this chapter are adapted from the prior Open Access review article, Povoski et al.: A comprehensive overview of radioguided surgery using gamma detection probe technology. World Journal of Surgical Oncology. 2009;7:11.; doi:10.1186/1477-7819-7-11; (http://www.wjso.com/content/pdf/1477-7819-7-11.pdf); © 2009 Povoski et al.; licensee BioMed Central Ltd.; This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Radioguided surgery
- Surgical guidance
- Radioisotopes
- Intraoperative
- Radiation detection devices
- Surgeons
- Tumors
- Neoplasms
- Cancer
1 Overview: Conceptualization and Realization of Radioguided Surgery
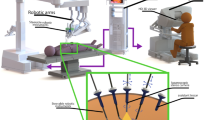
Radioguided surgery is simply the general concept of utilizing a radiation detection device within the operating room in a real-time fashion to identify a radioisotope that has been administered to a patient prior to the time of attempted detection and for the sole purpose of guiding the successful performance of the surgical procedure. Since its first description in the late 1940s, the use of radioguided surgery has expanded tremendously and has evolved into a well-established discipline within the practice of surgery [1]. Its use has been investigated and applied to the surgical management of numerous solid malignancies and has most significantly revolutionized the surgical management of breast cancer, melanoma, and parathyroid disease. Radioguided surgery has proven impactful on many levels in the surgical management of various disease entities and has most significantly contributed to providing the surgeon with critical and real-time information regarding the exact location of the disease and the overall extent of disease burden. Furthermore, radioguided surgery allows the surgeon to minimize the degree of surgical invasiveness associated with many commonplace diagnostic and therapeutic surgical procedures, while still maintaining maximum treatment-directed benefits to the patient.
2 The Early Years: Historical Milestones in Radioguided Surgery
The first reported description in the literature of utilizing a radiation detection device within the operating room to identify a radioisotope administered to a patient dates back to 1949 and comprises the work performed by Bertram Selverstone and his colleagues from Massachusetts General Hospital and Harvard Medical School (Boston, Massachusetts, USA) [1–3]. The radiation detection device utilized in this first reported description of radioguided surgery [2, 3] was a Geiger-Müller counter, a device that non-discriminately detects ionizing radiation, including alpha, beta, and gamma radiation, and for which the development of this practical electron counting tube (i.e., Geiger-Müller tube) was first realized in 1928 by Hans Geiger and Walther Müller at the University of Kiel (Kiel, Germany) [4].
In their initial published reports, Selverstone et al. [1–3] from Massachusetts General Hospital and Harvard Medical School (Boston, Massachusetts, USA) utilized a portable handheld gas-filled Geiger-Müller counter device to intraoperatively detect ionizing radiation during brain tumor surgery emitted from phosphorus-32 (32P), a pure beta-emitting radionuclide with a physical half-life of 14.3 days. The characteristic constraining feature of beta emissions, such as those from 32P, is their ability to only travel a few millimeters within biologic tissues. In their cumulative reported experience, Selverstone et al. [3] described a series of 33 patients with suspected brain tumors (as determined preoperatively by neurologic examination, electroencephalography, and ventriculography) that were intravenously injected with 0.95–4.2 millicuries (35.2–155.4 megabecquerels) of 32P in a buffered sodium phosphate solution at a time interval of 1.8–186.8 h prior to the surgical procedure. They utilized a prototype sterilizable handheld argon-ethyl acetate gas-filled Geiger-Müller counter device (possessing a 2 or 3 mm diameter cannula-like shaft containing the radiation-sensitive portion of the device for more easily penetrating the brain tissue) which was connected to either a preamplifier and a standard binary scaling unit or an analog-display counter ratemeter located outside of the sterile surgical field. At surgery, after the appropriate area of the cerebral cortex was exposed by way of a craniotomy, the cannula-like shaft of the handheld Geiger-Müller counter device was then placed on the surface of the brain in the area of the suspected brain tumor and advanced at successive 1 cm increments beneath the surface, to a maximum depth of up to approximately 6 cm, with count data (corrected counts per minute) taken at the location. A similar process for count data collection was performed on an area of presumed normal brain tissue away from the location of the suspected brain tumor. In selected cases, following successful location of the brain tumor, attempts were made to demarcate its tumor boundaries using the Geiger-Müller counter. Of 33 evaluated patients, 28 brain tumors (including 14 glioblastomas, 4 astrocytomas, 3 unclassified gliomas, 2 metastatic carcinomas, 1 medulloblastoma, 1 astroblastoma, 1 oligodendroglioma, 1 ependymoma, and 1 angiosarcoma) were localized using the handheld Geiger-Müller counter device, of which 23 brain tumors were located beneath the surface of the brain. In 12 patients, the handheld Geiger-Müller counter device was used to attempt to demarcate the tumor boundaries in order to facilitate total extirpation of tumor. In four patients, tumor was not localized by means of the handheld Geiger-Müller counter device, including two false-negative results that were attributed to the inability to correctly place the handheld Geiger-Müller counter device in close proximity to the tumor, one patient with diffuse infiltration of the entire cerebral hemisphere with tumor that precluded distinguishing it from normal adjacent tissue, and one patient in which no tumor was correctly identified.
Shortly thereafter in 1950–1951, Selverstone and his colleagues from Massachusetts General Hospital and Harvard Medical School (Boston, Massachusetts, USA) [5–7] also applied this technique of radioguided brain mapping during brain tumor surgery not only to 32P in 114 presumed brain tumor patients but also to potassium-42 (42K) in 36 presumed brain tumor patients. The radionuclide 42K has a physical half-life of 12.4 h, and its emission profile was described by Selverstone et al. [6] as including “more energetic beta particles” that could “theoretically be detected at distances of up to 1.8 cm through the brain,” as well as gamma emissions that were relatively inefficient in being counted by their handheld Geiger-Müller counter device. Sweet [7], who noted that 42K not only had a propensity to accumulate in brain tumors but also avidly accumulated in the muscle surrounding the calvarium, emphasized that the gamma emission capabilities of 42K “permits external localization through the intact skull in many cases.”
It was then not until 1956, when C. Craig Harris and his colleagues at the Oak Ridge National Laboratory and Oak Ridge Institute of Nuclear Studies Medical Hospital (Oak Ridge, Tennessee, USA) reported the first description in the literature of radioguided surgery utilizing a gamma scintillation detection device, and, most specifically, a portable handheld gamma detection probe system, with the specific application of the identification of thyroid tissue [1, 8]. This system described by Harris et al. [8] consisted of a handheld gamma detection probe, utilizing a thallium-activated cesium iodide (CsI(TI)) scintillation crystal. There were two separate nickel probe head configurations which were designed with platinum collimation, including one probe head measuring 1/4 in. in diameter and 3 5/8 in. in length and containing a CsI(TI) scintillation crystal of 0.22 in. in diameter and 3/8 in. in length and another probe head measuring 1/8 in. in diameter and 3 1/2 in. in length and containing a CsI(TI) scintillation crystal of 0.10 in. in diameter and 1/4 in. in length. These two probe head designs were mounted to a handheld photomultiplier-preamplifier and connected by a coaxial cable to a metal box unit containing the power supply, an analog-display counter ratemeter, and speaker/volume control to elicit an audible signal (i.e., “howler”). In their published report, Harris et al. [8] described the evaluation of a patient with a history of thyroid cancer who had previously undergone a total thyroidectomy some 3 years earlier and who had persistent iodine uptake in the neck region. The patient was intravenously injected with 0.25 millicuries (9.25 megabecquerels) of iodine-131 (131I), a radionuclide gamma emitter with a physical half-life of 8.04 days, which has a minority of gamma emissions (representing approximately 10 % of its energy, with 81 % of gamma emissions being at 364 keV) and which has a majority of beta emissions (representing approximately 90 % of its energy, which travel only up to 2 mm in biologic tissue, and are responsible for its tissue damage effect as a form of radiotherapy). At surgery, using this handheld gamma detection probe, they were able to localize a discrete solitary area of significant radioactivity situated along the left side of the trachea, and this allowed for the successful identification and successful excision of a 5 × 5 × 2 mm nodule near the entrance of the left recurrent laryngeal nerve that was subsequently histologically proven to represent an area of residual thyroid tissue.
Then, in the late 1950s, the principles of radioguided surgery using gamma detection devices were first applied in the development of techniques for continuous monitoring of systemic leakage during performance of regional isolated perfusion for locally advanced and unresectable malignancies [1, 9–12]. Early on in the development of regional isolated perfusion technologies, John Stehlin and his colleagues at the University of Texas M.D. Anderson Hospital and Tumor Institute (Houston, Texas, USA) recognized two important considerations in achieving the highest possible dose of chemotherapeutic agent for attaining maximum clinical efficacy from regional isolated perfusion [9–12]. These considerations were (1) “local tissue tolerance” (i.e., the maximum amount of chemotherapy agent which normal tissues can tolerate without being permanently damaged) and (2) the “leakage factor” (i.e., the extent of “cross-circulation” between the isolated circuit of the perfused region and the systemic circulation). John Stehlin and his colleagues believed that the “leakage factor” represented the most serious limitation to achieving a successful regional isolated perfusion procedure, and were the first to recognize the potential beneficial utility of radioguided technologies for monitoring of systemic leakage during regional isolated perfusion, and investigated radioguided monitoring techniques during regional isolated perfusion for locally advanced and unresectable malignancies, such as malignant melanoma, sarcoma, squamous cell carcinoma, basal cell carcinoma, and adenocarcinoma, which were confined to the extremities, as well as a small number of cases which were confined to the pelvic region and head region. Stehlin et al. [10, 11] injected 2–10 microcuries (0.074–0.370 megabecquerels) of 131I-labeled human serum albumin intravenously into the patient for determination of a calibration count baseline and injected approximately tenfold more 131I-labeled human serum albumin, consisting of 20–100 microcuries (0.74–3.70 megabecquerels) of 131I-labeled human serum albumin into the arterial line leading from the perfusion pump to the isolated perfusate circuit for eventual calculation of the percentage systemic leakage factor. For monitoring of the systemic leakage during the regional isolated perfusion procedure, they utilized a single, small field-of-view scintillation crystal detector probe unit with a built-in photomultiplier tube and preamplifier and with 1.25 in. thickness of lead side shielding for detection of gamma emissions. The single, small field-of-view scintillation detector unit was mounted overhead on a wheel-based pole tower apparatus for easy mobility and positioning during the regional isolated perfusion procedure and was positioned over the heart for lower extremity cases or positioned over the groin for upper extremity cases. The single, small field-of-view scintillation detector unit was connected by way of a 30 ft coaxial cable to an analog-display counter ratemeter and a rectilinear pen recorder for quantifying and recording the results of the systemic leakage of 131I-labeled human serum albumin from the isolated perfusate circuit.
Although some 30 years later, the same principles of radioguided monitoring of systemic leakage during regional isolated perfusion, which were first established by John Stehlin [10–12] using an overhead-mounted small field-of-view scintillation detector unit, were later adapted to the use of a handheld semiconductor gamma detection system [1, 13]. This system, described in 1989 by Sardi et al. [13] at the Ohio State University (Columbus, Ohio, USA), consisted of two commercially available handheld gamma probes, each consisting of a Neoprobe® 1000 gamma detection probe (formerly Neoprobe Corporation, Dublin, Ohio, USA), which each employed a cadmium zinc telluride (CdZnTe) semiconductor crystal of 11 mm in diameter and 15 mm in length. One of the handheld gamma probes was positioned over the precordial area, and the other handheld gamma probe was positioned over the distal aspect of the thigh. Patients received 0.8 millicuries (29.6 megabecquerels) of technetium-99 m (99mTc) pentetate through the isolated perfusate circulation. 99mTc is a radionuclide gamma emitter with a physical half-life of 6.04 h, which has a predominant gamma emission at 140 keV. The percentage of 99mTc pentetate leakage was calculated by a simultaneous reading of the two gamma detection probes at 1 min intervals, as well as determined by the standard method of intermittent simultaneous blood sampling from the isolated perfusate and systemic circulations at 15 min intervals using a gamma well counter. An essentially identical percentage of systemic leakage was detected by the minute-by-minute monitoring of the two handheld gamma probe system as compared to that determined by the intermittent (every 15 min) blood sampling method from the isolated perfusate and systemic circulations. Nevertheless, the minute-by-minute monitoring of the two handheld gamma probe system provided the surgeon with a more instantaneous and real-time indication of any fluctuations in the percentage of systemic leakage than did the intermittent (every 15 min) blood sampling method from the isolated perfusate and systemic circulations, thus allowing the surgeon to make more immediate intraoperative decision-making during regional isolated perfusion procedure.
3 Innovative Clinical Applications of Radioguided Surgery in the 1980s
During most of the 1960s and 1970s, the application of radiation detection devices for guiding surgical procedures within the operating room fell into some level of dormancy. However, starting in the early 1980s, successful clinical application of innovative radioguided surgery techniques began to develop at a more accelerated rate. This included the development of clinical applications of radioguided surgery directed toward the biopsy and resection of suspicious bone lesions, the identification of parathyroid tissue, and the development of antigen-directed intraoperative radioimmunodetection for the radioguided localization and resection of tumors (i.e., radioimmunoguided surgery) [1].
It was in 1981 that the application of radioguided surgery was first applied to the biopsy and resection of suspicious bone lesions [1, 14, 15]. At that time, Harvey et al. [14] at the Presbyterian Hospital of Dallas (Dallas, Texas, USA) first reported the application of a sterilizable prototype handheld scintillation gamma detection probe for intraoperative radioguided biopsy of benign and metastatic bone lesions in four patients using an intravenous injection of 2–20 millicuries (74–740 megabecquerels) of 99mTc-methylene diphosphonate in three cases and 5 millicuries (185 megabecquerels) of gallium-67 (67Ga) citrate in one case. 67Ga is a radionuclide gamma emitter with a physical half-life of 78.3 h, which has predominant gamma emissions at 93 keV (37.8 % abundance), 184 keV (20.1 % abundance), and 300 keV (16.8 % abundance). This system consisted of a prototype handheld gamma detection probe containing a 0.64 × 2.54 cm thallium-activated sodium iodide (NaI(TI)) scintillation crystal housed in a stainless steel housing (16.5 cm in length × 1.5 cm diameter) with 2 mm of lead side shielding for collimation (formerly Harshaw Chemical Company, Solon, Ohio) and which was coupled to a 38 mm bialkali (antimony reacted with potassium and cesium) photomultiplier tube (Hamamatsu Photonic K.K., Hamamatsu City, Shizuoka Prefecture, Japan), via a flexible fiber-optic cable which was attached to an audible count-rate indicator. Additionally, in 1981, Ghelman et al. [15] at the Hospital for Special Surgery (New York, New York, USA) also reported the application of another prototype handheld scintillation gamma detection probe for intraoperative radioguided resection of a single patient with a benign bone tumor (i.e., osteoid osteoma) using an intravenous injection of 15 millicuries (555 megabecquerels) of 99mTc-methylene diphosphonate. This system consisted of a prototype handheld gamma detection probe containing a nonspecified thallium-activated sodium iodide (NaI(TI)) scintillation crystal housed in a stainless steel housing (18.2 cm in length × 1.6 cm diameter) and enveloped in a cylindrical lead shield for collimation measuring 20.5 cm in length and with an 8 mm distal end aperture (formerly Harshaw Chemical Company, Solon, Ohio, USA) and which was attached to a digital-/analog-display scaler/counter ratemeter (Lundlum Measurements, Inc., Sweetwater, Texas, USA) for count recording.
It was in 1984 that the application of radioguided surgery was first applied to the identification of parathyroid tissue [1, 16]. At that time, Ubhi et al. [16] at Queen’s Medical Centre/University Hospital (Nottingham, England, UK) reported the application of a sterilizable handheld gamma semiconductor gamma detection probe for identification and radioguided resection of an ectopic mediastinal parathyroid adenoma within a patient undergoing neck exploration with the finding of two normal left neck parathyroid glands and only one normal right neck parathyroid gland after a 1.6 millicuries (60 megabecquerels) intravenous injection using of thallium-201 (201Tl) thallous chloride. This system consisted of a handheld gamma detection probe containing a cadmium telluride (CdTe) semiconductor crystal connected to a digital-display counter ratemeter for count recording. 201Tl has a physical half-life of 73.0 h, and decays predominantly by electron capture, emitting Hg X-rays (in the 70–80 keV range), and has gamma photon emission at 167 keV of 10 % abundance and at 135 keV of 3 % abundance.
However, it was not for another decade until further refinements in radioguided surgical techniques for the identification of parathyroid tissue were reported in the literature and thus subsequently leading to the adoption of this technology for the surgical management of primary hyperparathyroidism [1, 17, 18]. Specifically, in 1995, Martinez et al. at [17] the Ohio State University (Columbus, Ohio, USA) first reported the use of 99mTc-methoxyisobutylisonitrile (MIBI) for the radioguided surgical detection of parathyroid gland pathology in three patients. The patients were intravenously injected with 0.4–2.0 millicuries (14.8–74 megabecquerels) of 99mTc-MIBI. Then, approximately 2–6 h after 99mTc-MIBI administration, patients underwent intraoperative radioguided localization of abnormal parathyroid glands using the commercially available handheld Neoprobe® 1000 gamma detection probe (formerly Neoprobe Corporation, Dublin, Ohio). Then, in 1997, Norman and Chheda [18] at the University of South Florida (Tampa, Florida, USA) reported on their first series of 15 patients undergoing minimally invasive radioguided surgery using 99mTc-MIBI for the surgical management of primary hyperparathyroidism. This report by Norman and Chheda [18] was followed by many other publications by the Norman group, and led to the popularization and widespread application of minimally invasive radioguided parathyroidectomy using 99mTc-MIBI for the surgical management of primary hyperparathyroidism, and which today remains an important mainstay in parathyroid surgery.
The year 1984 also marked the inauguration of the radioguided surgical concept of radioimmunoguided surgery [1]. The idea of utilizing antibodies directed against cancer-specific antigens for intraoperative radioimmunodetection, localization, and resection of tumors was pioneered at the Ohio State University (Columbus, Ohio, USA) by a surgical oncologist, Dr. Edward W. Martin, Jr., and a professor emeritus of electrical engineering, Dr. Marlin O. Thurston [1]. Their initial experimental animal model testing and human application of intraoperative radioimmunodetection were first reported in 1984 by Aitken et al. [1, 19, 20]. In their initial experimental animal model testing, they grow subcutaneous tumor implants of CEA-producing human colonic adenocarcinoma cells (CX-1) on the flank in Swiss nude mice and demonstrated the feasibility of handheld gamma probe detection of 131I-labeled baboon anti-CEA polyclonal antibody within these subcutaneous tumor implants, with greater sensitivity of the handheld gamma detection probe as compared to gamma camera imaging for small tumor implants [1, 19, 20]. In their first clinical application of intraoperative radioimmunodetection, they intravenously injected a single patient with rectal carcinoma with 1.9 millicuries (70.3 megabecquerels) of 131I-labeled baboon anti-CEA polyclonal antibody at a time of 3 days prior to the planned surgical procedure and intraoperatively utilized a prototype handheld gamma detection probe system (consisting of a single CdTe semiconductor crystal housed within a 16 mm diameter lead collimator with a 4 mm aperture, and connected to a preamplifier, and an amplifier with a digital-display counter) for radioactive count recording [1, 20]. The prototype handheld gamma detection probe intraoperatively detected an increased level of the 131I-labeled baboon anti-CEA polyclonal antibody in the rectal tumor as compared to normal sigmoid colon, ileum, abdominal wall, and anal verge. Shortly thereafter in 1985, Martin et al. [1, 21] reported the results of the first radioimmunoguided surgery clinical series involving 28 patients with primary (n = 12) and recurrent (n = 16) colorectal cancer and using the same prototype handheld gamma detection probe system. Each patient was intravenously injected with 2.2 millicuries (81.4 megabecquerels) of 131I baboon anti-CEA polyclonal antibody at approximately 48–72 h prior to the planned surgical procedure. Preoperative whole-body scintillation imaging correctly localized tumor in only 33 % of the patients with primary colorectal cancer and only 64 % of patients with recurrent colorectal cancer. In contrast, intraoperative radioimmunodetection with the prototype handheld gamma detection probe was successful in all 28 patients, with a mean tumor-to-background ratio of 3.97:1 in primary lesions and 4.18:1 in recurrent lesions. Thereafter, nearly all subsequent radioimmunoguided surgery clinical trials conducted at the Ohio State University (Columbus, Ohio, USA) used various monoclonal antibodies targeted against tumor-associated glycoprotein-72 (TAG-72), a mucin-like, extracellular antigen overexpressed by many adenocarcinomas, which were radiolabeled with iodine-125 (125I) [1].
4 Innovative Clinical Applications of Radioguided Surgery in the 1990s
Beginning in the early 1990s, there was a further acceleration in the development of successful clinical applications for radioguided surgery. This included the development of radioguided sentinel lymph node biopsy for melanoma and breast cancer, as well as radioguided lesion localization for the surgical excision of non-palpable breast lesions seen on breast imaging [1].
The generalized concept of a so-called “sentinel node” in our modern medical literature was first coined by Ernest A. Gould and his colleagues from the Washington Hospital Center (Washington, DC, USA) in 1960 in their description of a lymph node that was routinely “noted at the junction of the anterior and posterior facial vein” at the time of surgery for parotid gland cancer [1, 22]. In their landmark report, Gould et al. [22] stated “The lymph node that is now used routinely for frozen section assay is easily found. After the skin incision has been made and the flaps reflected, the inferior posterior surface of the parotid is separated from the anterior margin of the sternomastoid muscle. The anterior facial vein curves downward and posteriorly at the lower edge of the gland to meet the posterior facial vein to form the common facial truck. It is in the area of the angle formed by the junction of these 2 veins that this “sentinel node” is always found. It may be removed easily, and the parotid dissection may progress during the pathologist’s study of the node”. They concluded by remarking that “routine excision of this angular node be done for frozen section study.” However, it was not until almost two decades later in 1977 that the “sentinel node” concept reappeared in the modern medical literature and was more notably attributed to the work of Ramón M. Cabañas at the National University of Asunción (Asunción, Paraguay) in the area of penile squamous cell carcinoma [1, 23]. This reappearance of the “sentinel node” concept was based upon the careful work and meticulous description of lymphadenography of the dorsal lymphatics of the penis which was previously published by Manuel Riveros, Ramiro Garcia, and Ramón M. Cabañas at the same university in 1967 [1, 24]. In his landmark report, Cabañas [23] stated “A 5-cm incision is made parallel to the inguinal ligament, two finger-breadths (4.5 cm) lateral and two finger-breadths (4.5 cm) distal to the pubic tubercle….. This lies over the greater sapheno-femoral junction. By inserting the finger under the upper flap towards the pubic tubercle, the SLN is encountered….. The SLN corresponds to the lymph nodes associated with the superficial epigastric vein….. The position of the SLN in relationship to the superficial epigastric vein may vary but never by a distance greater than 1 cm.” Cabañas concluded by remarking that “Anatomically, clinically, and pathologically it was found that the SLN is the first site of metastasis and may be the only lymph node involved….. If SLN biopsies are negative for metastases, no further surgical therapy is immediately indicated.” In their landmark reports, the strict definition of the “sentinel node” by both Gould in 1960 [1, 22] and Cabañas in 1977 [1, 23] was based solely upon its proximity to a static, predefined anatomical landmark (i.e., the angle of the confluence of the anterior and posterior facial veins, as described by Gould, and the superficial epigastric vein, as described by Cabañas), and this definition of the “sentinel node” was not based upon actual variations in the pattern of lymphatic drainage observed within patients undergoing any sort of individualized, real-time, intraoperative lymphatic mapping procedure at the time of surgery.
The actual concept of intraoperative lymphatic mapping for selective identification and removal of sentinel lymph nodes at the time of surgery was first introduced into the modern medical literature in 1992 for melanoma by Donald L. Morton and his colleagues at the John Wayne Institute for Cancer Treatment and Research (Santa Monica, California, USA) using intradermally injected vital blue dyes alone in a total of 223 melanoma patients [25]. Sentinel lymph nodes were successfully identified in 194 of the 237 lymph node basins evaluated. However, it was not until 1 year later in 1993 that David N. Krag, James C. Alex, and colleagues at the University of Vermont (Burlington, Vermont, USA) published the first reports of intraoperative radioguided identification of sentinel lymph nodes in both melanoma and breast cancer patients using 99mTc-sulfur colloid and a handheld gamma detection probe [26, 27]. Alex et al. [26] reported on ten melanoma patients who were intradermally injected with 0.4 millicuries (14.8 megabecquerels) 99mTc-sulfur colloid in 0.5 milliliters of normal saline, underwent preoperative lymphoscintigraphy between 10 min and 150 min after injection, and subsequently underwent a sentinel lymph node biopsy procedure approximately 2.5–5.0 h after injection utilizing a handheld gamma detection probe. The handheld gamma detection probe contained a NaI scintillation crystal coupled to a photomultiplier tube, and both contained within a tungsten-alloyed housing and connected to a preamplifier and a signal processor with a digital and analog readout for radioactive count recording (C-Trak, Care Wise Medical Products, Morgan Hill, California, USA). Sentinel lymph nodes were successfully identified in all ten patients. Krag et al. [27] reported on 22 breast cancer patients who were injected with 0.4 millicuries (14.8 megabecquerels) 99mTc-sulfur colloid in 0.5 milliliters of normal saline into the normal breast tissue adjacent to the lesion or the biopsy site and subsequently underwent a sentinel lymph node biopsy procedure approximately 1–9 h after injection utilizing the same previously described handheld gamma detection probe system. Sentinel lymph nodes were successfully identified in 18 of the 22 patients injected. It is realistic to assert that the introduction of radioguided sentinel lymph node biopsy to the surgical management of melanoma and breast cancer by Krag and Alex [26, 27] represents the single most impactful advancement that radioguided surgery has had on reshaping the surgical management of any given disease entity.
The concept of radioguided localization of non-palpable breast lesions was first introduced into the literature in 1996 by Charles E. Cox and colleagues from the H. Lee Moffitt Cancer Center and Research Institute (Tampa, Florida, USA) [28]. In their initial case report, Cox et al. [28] described a breast cancer patient intravenously injected 1 h prior to surgery with 18 millicuries (692 megabecquerels) of 99mTc-MIBI and subsequently performed radioguided excision of the breast cancer using a handheld gamma detection probe. This initial report laid the groundwork for the subsequent development of two variations in the technique of radioguided localization and excision of non-palpable breast lesions utilizing mammographic or ultrasound-guided placement of a radionuclides into the region of the non-palpable breast lesion. Starting in 1998, Alberto Luini and Umberto Veronesi from the European Institute of Oncology (Milan, Italy) reported the first series of papers on the radioguided occult lesion localization (ROLL) technique, which involved an intratumoral injection (using prior-day mammographic or ultrasound guidance) of 0.1 millicuries (3.7 megabecquerels) of 99mTc-colloidal human serum albumin in 0.2–0.3 milliliters of normal saline, followed by next day radioguided excisional breast biopsy using various handheld gamma detection probes [29–31]. Their reported cumulative success rate was 99.5 % among 647 patients [31]. Similarly, starting in 1999, Emilia L. Dauway, Charles E. Cox, and Richard J. Gray from the H. Lee Moffitt Cancer Center and Research Institute (Tampa, Florida, USA) reported the first series of papers on the radioguided seed localization (RSL) technique, which involved placement of a 0.29 millicuries (10.7 megabecquerels) 125I-labeled titanium seed (4.5 mm × 0.8 mm in dimension) up to 5 days prior to surgery, followed by radioguided excisional breast biopsy using a handheld gamma detection probe [32–34]. Their reported cumulative success rate was 100 % among 51 patients [34].
5 Concluding Remarks
It is very evident that radioguided surgery has a long and rich history dating back to the late 1940s, with significant groundbreaking contributions from many individuals and with far too many contributions of significance to even begin to be discussed within this introductory chapter alone. Therefore, the collective expectations of this current textbook are to show exactly how the many current applications and future innovative directions of radioguided surgery can impact upon all discipline within the clinical practice of surgery. As we move forward through the twenty-first century, we envision further growth of the current technological platforms of radioguided surgery, with a continued emphasis upon promoting integration of handheld radiation detection devices and advanced nuclear medicine molecular imaging for guiding and optimizing the intraoperative detection and resection of conditions affecting both cancer and noncancer patients.
References
Povoski SP, Neff RL, Mojzisik CM, O’Malley DM, Hinkle GH, Hall NC, Murrey Jr DA, Knopp MV, Martin Jr EW. A comprehensive overview of radioguided surgery using gamma detection probe technology. World J Surg Oncol. 2009;7:11.
Selverstone B, Solomon AK, Sweet WH. Location of brain tumors by means of radioactive phosphorus. J Am Med Assoc. 1949;140:277–8.
Selverstone B, Sweet WH, Robinson CV. The clinical use of radioactive phosphorus in the surgery of brain tumors. Ann Surg. 1949;130:643–51.
Geiger H, Müller W. Elektronenzählrohr zur messung schwächster aktivitäten. Naturwissenschaften. 1928;16:617–8.
Selverstone B, Sweet WH, Ireton RJ. Radioactive potassium, a new isotope for brain tumor localization. Surg Forum. 1950;1:371–5.
Selverstone B, White JC. Evaluation of the radioactive mapping technic in the surgery of brain tumors. Ann Surg. 1951;134:387–96.
Sweet WH. The uses of nuclear disintegration in the diagnosis and treatment of brain tumor. N Engl J Med. 1951;245:875–8.
Harris CC, Bigelow RR, Francis JE, Kelly GG, Bell PR. A CsI(TI)-crystal surgical scintillation probe. Nucleonics. 1956;14:102–8.
Reemtsma K, Ryan RF, Krementz ET, Creech Jr O. Treatment of selected adenocarcinomas by perfusion technique. AMA Arch Surg. 1959;78:724–7; discussion 727–8.
Stehlin Jr JS, Clark Jr RL, White EC, Smith Jr JL, Griffin AC, Jesse Jr RH, Healey Jr JE. Regional chemotherapy for cancer: experiences with 116 perfusions. Ann Surg. 1960;151:605–69.
Stehlin Jr JS, Clark Jr RL, White EC, Healey Jr JE, Dewey WC, Beerstecher S. The leakage factor in regional perfusion with chemotherapeutic agents. Arch Surg. 1960;80:934–45.
Stehlin Jr JS, Clark Jr RL, Dewey WC. Continuous monitoring of leakage during regional perfusion. Arch Surg. 1961;83:943–9.
Sardi A, Minton JP, Mojzisik C, Nieroda CA, Ferrara PJ, Hinkle GH, Thurston MO, Martin Jr EW. The use of a hand-held gamma detector improves the safety of isolated limb perfusion. J Surg Oncol. 1989;41:172–6.
Harvey WC, Lancaster JL. Technical and clinical characteristics of a surgical biopsy probe. J Nucl Med. 1981;22:184–6.
Ghelman B, Thompson FM, Arnold WD. Intraoperative radioactive localization of an osteoid-osteoma. Case report. J Bone Joint Surg Am. 1981;63:826–7.
Ubhi CS, Hardy JG, Pegg CA. Mediastinal parathyroid adenoma: a new method of localization. Br J Surg. 1984;71:859–60.
Martinez DA, King DR, Romshe C, Lozano RA, Morris JD, O’Dorisio MS, Martin Jr E. Intraoperative identification of parathyroid gland pathology: a new approach. J Pediatr Surg. 1995;30:1306–9.
Norman J, Chheda H. Minimally invasive parathyroidectomy facilitated by intraoperative nuclear mapping. Surgery. 1997;122:998–1003; discussion 1003–4.
Aitken DR, Thurston MO, Hinkle Jr GH, Martin DT, Haagensen Jr DE, Houchens D, Tuttle SE, Martin Jr EW. Portable gamma probe for radioimmune localization of experimental colon tumor xenografts. J Surg Res. 1984;36:480–9.
Aitken DR, Hinkle GH, Thurston MO, Tuttle SE, Martin DT, Olsen J, Haagensen Jr DE, Houchens D, Martin Jr EW. A gamma-detecting probe for radioimmune detection of CEA-producing tumors, Successful experimental use and clinical case report. Dis Colon Rectum. 1984;27:279–82.
Martin DT, Hinkle GH, Tuttle S, Olsen J, Nabi H, Houchens D, Thurston M, Martin Jr EW. Intraoperative radioimmunodetection of colorectal tumors with a hand-held radiation detector. Am J Surg. 1985;150:672–5.
Gould EA, Winship T, Philbin PH, Kerr HH. Observations on a “sentinel node” in cancer of the parotid. Cancer. 1960;13:77–8.
Cabanas RM. An approach for the treatment of penile carcinoma. Cancer. 1977;39:456–66.
Riveros M, Garcia R, Cabañas R. Lymphadenography of the dorsal lymphatics of the penis. Technique and results. Cancer. 1967;20:2026–31.
Morton DL, Wen DR, Wong JH, Economou JS, Cagle LA, Storm FK, Foshag LJ, Cochran AJ. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg. 1992;127:392–9.
Alex JC, Weaver DL, Fairbank JT, Rankin BS, Krag DN. Gamma-probe-guided lymph node localization in malignant melanoma. Surg Oncol. 1993;2:303–8.
Krag DN, Weaver DL, Alex JC, Fairbank JT. Surgical resection and radiolocalization of the sentinel lymph node in breast cancer using a gamma probe. Surg Oncol. 1993;2:335–9; discussion 340.
Cox CE, Hyacinthe M, Berman C, Dupont EL, Wagner A. Localization of an occult primary breast cancer with technetium-99m sestamibi scan and an intraoperative gamma probe. Cancer Control. 1996;3:448–50.
Luini A, Zurrida S, Galimberti V, Paganelli G. Radioguided surgery of occult breast lesions. Eur J Cancer. 1998;34:204–5.
Luini A, Zurrida S, Paganelli G, Galimberti V, Sacchini V, Monti S, Veronesi P, Viale G, Veronesi U. Comparison of radioguided excision with wire localization of occult breast lesions. Br J Surg. 1999;86:522–5.
Gennari R, Galimberti V, De Cicco C, Zurrida S, Zerwes F, Pigatto F, Luini A, Paganelli G, Veronesi U. Use of technetium-99m-labeled colloid albumin for preoperative and intraoperative localization of nonpalpable breast lesions. J Am Coll Surg. 2000;190:692–8; discussion 698–9.
Dauway EL, Sanders R, Friedland J, Berman C, Ku NN, Reintgen DS, Yeatman T, Falcone R, Crawford S, Cox CE. Innovative diagnostics for breast cancer: new frontiers for the new millennium using radioactive seed localization. Surg Forum. 1999;50:348–9.
Gray RJ, Giuliano R, Dauway EL, Cox CE, Reintgen DS. Radioguidance for nonpalpable primary lesions and sentinel lymph node(s). Am J Surg. 2001;182:404–6.
Gray RJ, Salud C, Nguyen K, Dauway E, Friedland J, Berman C, Peltz E, Whitehead G, Cox CE. Randomized prospective evaluation of a novel technique for biopsy or lumpectomy of nonpalpable breast lesions: radioactive seed versus wire localization. Ann Surg Oncol. 2001;8:711–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Povoski, S.P. (2016). The History of Radioguided Surgery: Early Historical Milestones and the Development of Later Innovative Clinical Applications. In: Herrmann, K., Nieweg, O., Povoski, S. (eds) Radioguided Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-26051-8_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-26051-8_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26049-5
Online ISBN: 978-3-319-26051-8
eBook Packages: MedicineMedicine (R0)