Abstract
Age-related decline in bone mass is a universal phenomenon among laboratory mammals. Research on aging has been conducted using various models from yeast and nematode to mouse and non-human primates, and has rapidly progressed due to the recent development of forward and reverse genetics, as well as functional genomics. Some mouse models bearing artificially or naturally modified genes develop bone phenotypes with various pathologies. Among those mice, some are considered to be potent models for understanding the pathophysiology of age-related bone loss and osteoporosis in humans. Here, available models for the study of age-related bone loss and osteoporosis are introduced and discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Age-related decline in bone mass is a universal phenomenon among laboratory mammals. Research on aging has been conducted using various models from yeast and nematode to mouse and non-human primates, and has rapidly progressed due to the recent development of forward and reverse genetics, as well as functional genomics. Some mouse models bearing artificially or naturally modified genes develop bone phenotypes with various pathologies. Among those mice, some are considered to be potent models for understanding the pathophysiology of age-related bone loss and osteoporosis in humans. Here, available models for the study of age-related bone loss and osteoporosis are introduced and discussed.
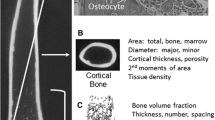
Normally Aged Animal Models
Besides mice and rats, studies of osteoporosis in guinea pigs, rabbits, cats, dogs, and pigs have been reported. And while, compared to mice and rats, some of those evaluated are considered to be better models relatively to humans in terms of similarity in estrus cycles or Haversian remodeling, the number of studies is quite limited. Studies in non-human primates, such as monkeys, have been considered to be the best and most relevant in terms of human skeletal structure and metabolism [1–6]. While breeding cost and ethical considerations are the highest among the animal models, therapeutic trials in non-human primate models are considered the most informative relative to humans. An age-dependent bone loss in these animals has also been well described. On the other hand, primary screening of candidate anti-osteoporotic compounds has been tested more often in rat than mouse models, probably because they have relatively more bone mass and an overall better response to ovariectomy (OVX). As observed in humans, decreased bone marrow cellularity and increased adiposity, as well as an age-related decline in bone mass, are apparent in rodent models of aging (Fig. 6.1). Laboratory mice usually live for 2–3 years and show a peak bone mass at 4–8 months of age followed by declining bone mass as they age.
A comparison of bone marrow between young and old rats. The figure shows remarkably higher levels of bone marrow fat (white areas) in a 24-month-old rat (b) as compared with a 4- month-old rat (a). In addition, the trabecular thickness is reduced in the old rat, as is the amount of hematopoietic tissue (Adapted from Duque [119])
A popular laboratory mouse strain, C57BL/6, develops a senile osteoporosis-like bone phenotype with decreased bone mass and quality [7–14]. Both trabecular and cortical bones suffer dynamic changes upon aging in these mice. Two studies [7, 8] have assessed the age-related changes in the bone of C57BL/6 J male mice. Mice were aged between 4 and 104 weeks. In young mice, rapid growth was marked by substantial increases in bone size, mineral mass, and mechanical properties. Maturity occurred between 12 and 42 weeks of age with the maintenance of bone mass and mechanical properties. From peak levels, mice aged for 104 weeks experienced decreased whole femur mass (12.1 and 18.6 % for dry and ash mass, respectively), percentage mineralization (7.4 %), diminished whole bone stiffness (29.2 %), energy to fracture (51.8 %), and decreased cortical thickness (20.1 %). Indices of surface-based formation decreased rapidly while the periosteal perimeter and, consequently, the cross-sectional moments of inertia continued to increase through 104 weeks, thus maintaining structural properties. This compensated for cortical thinning and increased brittleness due to decreased mineralization and stiffness. The shape of the mid-diaphysis became increasingly less elliptical in aged mice, and endocortical resorption and evidence of subsequent formation were present in 20–50 % of femurs aged ≥ 78 weeks. This, combined with the appearance of excessive endocortical resorption after 52 weeks, indicated a shift in normal mechanisms regulating bone shape and location, and was suggestive of remodeling. The authors concluded that the pattern of bone loss at the femoral mid-diaphysis was markedly similar to that seen in cortical bone in the human femoral neck in age-related osteoporosis.
Interestingly, expression of RANKL, also known as osteoclast differentiation factor, is increased upon aging and correlates with cancellous bone volume [9, 10]. On the other hand, bone marrow hematopoiesis is often affected by aging [11–14]. C57BL/6 is known to develop clonal B cell expansion and lymphoma frequently in this aging mouse strain [13, 14], suggesting that age-related, strain-specific hematopoietic disorganization, such as lymphoma, largely affects bone metabolism and bone resorption in particular. Furthermore, in another common strain, BALB/c, osteogenic stem cells from 24-month-old mice exhibit a decrease in proliferative potential upon aging [11]. It is suggested that the age-related bone loss in this model is caused by decreased osteogenic potential due to both quantitative and qualitative declines, especially in stem cell function (Figs. 6.2, 6.3, and 6.4).
MicroCT analysis (a–f) to evaluate bone structure and sections of undecalcified bone stained with von Kossa (a–f, right panels) (magnification × 10) to evaluate mineralized tissue (black) and fat volume (white). The figure shows three-dimensional images of the trabecular bone and coss-sectional images of the cortical bone from rats aged 4, 20 and 30 months (a–f). The loss in bone volume, the reduction in both trabecular bone and cortical thickness and the increasing cortical porosity with age are visually apparent. Age-related changes in bone mineral density (BMD) (g) and bone volume/trabecular volume (BV/TV) (h) showed a significant decline in both groups matching similar levels of bone mass and bone quality at 30 months of age. ap < 0.01, bp < 0.001 compared with 4 months, one-way ANOVA and Dunnett’s test; cp < 0.01, dp < 0.001 males vs. females (From Duque et al. [19])
Predicted pathways connecting the gene products responsible for the premature aging mutant phenotype. Most of the mouse models for premature aging described by now are caused by mutations in the genes involved in genomic integrity and subsequent cell cycle regulation. Errors and damage to the genome or telomere shortening, which also affects DNA integrity could, in theory, be detected and corrected. Mutations in the genes responsible for genomic stability cause accumulation of phenotypic abnormalities. Genomic disorganization activates cell cycle-regulating pathways involving checkpoint kinases and p53. Oxidative stress is among the triggers that elicit genomic instability via DNA damage. Elevation and excess of ROS affect downstream signaling, including PKCδ which subsequently stimulates the anti-ROS pathway, including transcriptional activation of Prdx1 (From Watanabe and Hishiya, Ref. [118]. With permission from Elsevier)
Schematic presentation of osteogenesis and aging. Observations in naturally aged laboratory animals and mutant mice with aging phenotypes suggest that one of the keys to understanding aging and premature aging pathogenesis may be self-renewing stem cells. In these models, the pathway involving p53 (Fig. 6.3) upregulates the genes responsible for cell cycle arrest and/or apoptosis, lowering the regenerative potential necessary for homeostasis and tissue repair. While the mechanisms responsible for aging are largely unknown, the existing models suggest that there are common pathways, which may help in our understanding of the aging phenotype (From Watanabe and Hishiya, Ref. [118]. With permission from Elsevier)
In mature rats (from 8 to 36 months of age), the only change reported in bone structure is an increase in the cross-sectional moment of inertia (distribution of the bone around the central axis), due to the expansion of the outer diameter (periosteal deposition) of their bones, with a thinning of the cortical walls (endosteal resorption) [15]. Other study [16, 17], performed in trabecular bones in proximal tibias of 23-month-old and 5-month-old rats, found that mineral density, bone volume fraction, and trabecular number were significantly reduced in the aged rats compared with the younger rats. In addition, serum markers of bone formation were also reduced in the older rats [17, 18]. Interestingly, a model of “healthy-aging” rats known as LOU rats show the typical features of age-related osteoporosis – including high levels of bone marrow fat – despite their longer life span and low prevalence of diabetes and cancer [19].
Overall, the “normally aged” animal model of osteoporosis has the advantage of closely mimicking the age-related changes in bone. However, disadvantages include the high cost of maintaining a normally aging colony, the variability between different strains in terms of peak of bone mass and levels of bone turnover, and the fact that steroid hormones could play an important role in the levels of bone turnover during the post-menopausal months, which also vary from strain to strain.
Genetic Manipulation and Accelerated Aging
Development of genetic approaches to mimic osteoporosis is becoming a common practice worldwide. Genetic manipulation has been instrumental to our rapidly expanding knowledge of the molecular and cellular mechanisms underlying both normal and pathological bone biology. This methodology, which is more easily applied to mice, includes the targeted manipulation and ablation in vivo of one or several genes.
Some of the genetically modified mice recently developed by knockout or transgenic techniques show premature aging phenotypes. The clearest conclusion to be drawn from these models is that single gene mutations cause multiple aging phenotypes. This advantage is useful in defining the mechanisms regulating bone metabolism.
Amongst those mouse models, the senescence accelerated mice (SAM) have been established by Takeda et al., and accepted as suitable models for aging [20]. The SAM lines, derived from a mouse strain AKR/J, are divided into two classes; SAM-P lines exhibit an accelerated aging phenotype with shortened life-span, and SAM-R lines, which show a less accelerated phenotype than that of SAM-P. The aging phenotype of SAM-P lines becomes apparent at 6–8 months of age. Among the SAM lines, SAM-P6 has been demonstrated to be a correlative model for age-related osteoporosis in humans [21–24], and its bone phenotype has been well described. For example, Jilka et al. [21] demonstrated that the osteopenic phenotype in SAM-P6 is caused by reduced osteoblastogenesis and that their bone metabolism is resistant to gonadectomy. Furthermore, increased adipogenesis and myelopoiesis are observed in the bone marrow of these mice [23]. In addition, the long bones in SAM-P6 are longer but more fragile than controls [22]. This line is among the best studied as a model for age-related osteoporosis not only in terms of skeletal morphology and pathology, but also in terms of its application for therapeutic-targeting experiments, such as drug testing and bone marrow transplantation [25–27]. Other numerous in vivo and ex vivo reports of SAM-P6 have been published whose observations are thought to be consistent between these aged mice and humans, but also include some controversial observations or interpretations, probably due to their complicated genetic backgrounds. Because the SAM strains are polygenic, the specific genetic factors accounting for their bone phenotype remain to be elucidated.
The observed differences in bone metabolism resulting from the various genetic backgrounds of these different mouse strains have been quantified by QTL analyzes. For example, whereas C57BL/6 mice have a relatively low bone mineral density (BMD) and reduced bone mass, C3H/HeJ have high BMD and are resistant to bone loss in response to OVX [28, 29]. These studies indicate that usage of wild-type inbred strains of mice, as well as rats, need to be well-characterized and given strong consideration in studies of bone metabolism and pathophysiology.
Other mouse models mimicking the human progeroid syndromes have been reported [30–35]. These genetically modified mice develop multiple aging phenotypes and exhibit a shortened life span (Table 6.1). For example, Werner syndrome is caused by a loss-of-function mutation in WRN, encoding the RecQ family DNA helicase, which plays a role in genome stability including telomere maintenance [36]. Unexpectedly, knockout mice for the Wrn gene are essentially normal and exhibit no characteristics of premature aging [37]. Mice have long telomeres and relatively high telomerase activity, suggesting that the aging phenotype is latent in these mice and results from residual activity surrounding telomere maintenance. Evidently, double knockout mice for Wrn and Terc, which encodes the RNA component of telomerase activity, show a Werner-like phenotype with osteoporosis [38, 39]. RecQ like-4 (Recql4) is a gene mutated in a subset of Rothmund-Thomson syndrome, recognized as a premature aging syndrome [40, 41]. Although Reql4 null mice are embryonic lethal, targeted deletion of exon 13 results in a form of aging phenotype that includes osteopenia [42]. Yang et al. showed that osteoprogenitors are significantly decreased in heterozygous Recql4 (±) mice compared to wild-type controls [43]. In addition, mutated Recql4 has also been reported in Baller-Gerold syndrome, a rare autosomal recessive disorder with radial aplasia/hypoplasia and craniosynostosis [44].
Recently, a gene encoding lamin A has been identified to be responsible for human progeria, Hutchinson-Gilford syndrome [45, 46]. Mice carrying an autosomal recessive point mutation in the lamin A gene, corresponding to that identified in humans, also develop a progeria-like phenotype with osteoporotic symptoms [47]. Interestingly, expression of lamin A/C in osteoblasts and chondrocytes of C57BL/6 mice is decreased in an age-related manner [48]. In addition, recent studies have reported that lamin A-deficient mice are osteoporotic [49, 50], show a low anabolic response to exercise [51], and have high levels of fat infiltration in muscle and bone [52].
Furthermore, mice presenting with multiple aging phenotypes have also been reported. Null mutation of a gene, Ku86 (also known as Ku80), which plays roles in DNA repair and transcription exhibits a shortened life span and elicits a premature aging phenotype including osteopenia [53]. The aging phenotype has also been observed in mice lacking proliferation-associated SNF2-like gene (PASG), an SNF-like molecule that functions in DNA methylation [54]. Mutant mice show decreased BMD and a delay in the secondary ossification of the tibial epiphyses [54]. In addition to mutations in genes involved in genomic stability and nuclear organization, mice carrying mitochondrial DNA polymerase mutations that exclude a region responsible for its proofreading activity, also present the osteoporotic phenotype together with other premature aging symptoms [55]. A sir2/SIRT family of NAD-dependent histone deacetylases regulates life span. Knockout mice for Sirt6 exhibit genomic instability and an aging-like phenotype with osteopenia [56]; in particular decreased bone mass, now considered a hallmark of premature aging phenotypes. However, most observations of the skeletal phenotype were examined by X-ray analysis. The pathophysiology, including histology, of the bone phenotype in these models for premature aging, has not yet been fully described.
Errors in cell duplication, such as those miss programmed by the above-mentioned mutations can be detected and corrected by arresting the cell cycle. A system of cell cycle checkpoints has been shown to play a critical mechanistic role [57, 58]. Checkpoint kinase cascades are involved in DNA replication and other cell cycle events. ATM is a PI3K family kinase involved in DNA repair and oxidative response [59]. The gene encoding the protein kinase has been identified as a gene mutated in ataxia telangiectasia, recognized as one of the human premature aging syndromes [60]. Knockout mice for ATM exhibit a similar phenotype to the human disease, including hyper-radiosensitivity and ataxic defects [61–63]. It has been shown that the self- renewal capacity of hematopoietic stem cells in Atm knockout mice is significantly impaired with elevated reactive oxygen species (ROS), and that treatment with anti-oxidative agents rescues the bone marrow failure [64]. An osteopenic phenotype has also been observed in these knockout mice. Colony formation assays revealed that the phenotype was mainly caused by a proliferative defect in bone marrow mesenchymal stem cells or its progenitors [65].
Gain-of-function mutations in p53, a downstream effector of ATM kinase, also exhibit premature aging with an osteoporotic phenotype [66, 67]. Among them, p44 transgenic mice show a low progenitor turnover with significant decreases in osteoblast number and a slight reduction of osteoclasts [67]. Although further characterization of these models is required, these data suggest that the stem cell defect due to cell cycle arrest upon DNA damage or other cell cycle abnormalities, at least in part, may account for the decreased bone formation and subsequent osteopenia observed in these premature aging models.
In addition to stem cell defects in p53 and other checkpoint deficiencies, recent evidence indicates that p53 can directly regulate osteoblast differentiation [68]. Wang et al. [69] showed that mice lacking p53 exhibit increased bone mass due to accelerated osteoblast differentiation caused by elevated Osterix levels. Lengner et al. [68] examined osteoblast-specific ablation of Mdm2, a negative regulator of p53, and found reduced proliferation and decreased levels of Runx2 in the osteoblasts. Furthermore, they also described elevated Runx2 levels in p53-null osteoblasts, suggesting that p53 negatively regulates bone development and growth by inhibition of Runx2. Defects in osteoblast differentiation caused by dysregulation of Osterix was also recently reported in Atm knockout mice [70]. Thus, not only stem cell defects but also cell autonomous differentiation defects of osteoblasts are associated with the osteopenic phenotype in mouse models of premature aging.
Osteopenia Caused by Decrease in Bone Formation
Low turnover rates or uncoupling between bone resorption and formation in aged bones is often associated with a decline in osteoblast function [71]. Reduced bone formation is one of the features observed in models for age-related osteoporosis. Some genes that play critical roles in bone formation have been described using genetically modified mice [72–75]. Several typical models are listed in Table 6.2. Sca1/Ly6A is a GPI-anchored membrane protein expressed in hematopoietic stem cells and a subset of bone marrow stromal cells [76, 77]. Whereas Sca1 knockout mice have normal bone development, the aged animals (15 months of age) show a significant bone loss [78]. Progenitor and differentiation assays of bone marrow cells in these mice reveal that decreased bone mass is caused by impaired self-renewal of mesenchymal progenitors. Stem cell defects in hematopoietic lineages have also been reported in Sca1 knockout mice [79]. Although multiple aging phenotypes in Sca1 knockout mice have been reported, this is a good model for age-related osteoporosis in humans, supporting the stem cell hypothesis in the pathogenesis of age-related osteoporosis [80].
In addition, IRS1 is a major substrate of insulin receptor (IR) and IGF-1 receptor (IGF1R) that transduces signals by interacting with signaling molecules in a phosphorylation-dependent manner, which is expressed in osteoblasts but not in osteoclasts. IRS1 knockout mice exhibit low bone mass compared to wild-type controls, and cultured osteoblasts from the knockout mice are impaired in IGF-induced proliferation and differentiation, whereas BMP-induction is not altered [73]. Reduced osteoclast formation is then the result of defective osteoblasts, resulting in low turnover osteopenia [81].
Wnt signaling regulates bone mass through the osteoblastic lineage. It has been revealed that an autosomal recessive disorder, osteoporosis-pseudoglioma syndrome (OPPG), is caused by mutations in the gene encoding LRP5, a cell surface co-receptor for Wnt [82]. It has also been independently shown that Val171 mutation of LRP5 causes high bone density in humans [83]. These correlative findings indicate a role for the Wnt pathway in bone development and remodeling. Kato et al. generated mice deficient in Lrp5, and showed that Lrp5 knockout mice also develop osteopenia caused by reduced osteoblast proliferation and function [84]. A significant decrease in the number of bone marrow stromal progenitor cell (CFU-F) colonies was observed in the knockout mice. Inhibition of GSK3, a negative regulator of Wnt/β-catenin signaling stimulates osteoblastic differentiation of the progenitors [85, 86]. The ligands, such as Wnt10b, specifically activate the canonical pathway, and constitutively activate β-catenin-stimulated osteoblast differentiation [87]. These findings support the idea that the canonical pathway via β-catenin signaling of Wnt plays a role in the regulation of osteoblasts. It should be noted that the canonical pathway also inhibits adipogenic differentiation of progenitor cells [88], suggesting that the pathway is also important in lineage commitment between osteoblastic and adipogenic fates. This observation may be associated with age-related alterations of bone marrow, resulting in decreased bone formation and increased adipogenesis to what is described as “fatty marrow”.
On the other hand, some models presenting with osteopenia exhibit defects in osteoblast differentiation. Mice lacking a transcriptional cofactor, four and a half LIM domains 2 (Fhl2), also present with a significant decrease in bone mass [89]. Although numbers of osteoblasts and osteoclasts were comparable to littermate controls, bone formation rate was markedly reduced. Furthermore, transgenic mice overexpressing Fhl2 in osteoblasts exhibited enhanced bone formation and increased bone mass. Fhl2 interacts with Runx2 to increase its transcriptional activity and stimulates osteoblast maturation, suggesting that the Fhl2 knockout is a unique model for osteopenia caused by osteoblast activation deficiency [90].
Furthermore, c-Abl, a downstream protein kinase of ATM, functions in DNA repair and oxidative stress response [91]. Mice deficient for the Abl gene also develop osteopenia with reduced bone formation [92]. Ex vivo assays of osteoclastogenesis were not affected, and the number of osteoclasts in the Abl-deficient mice was similar to that of wild-type controls. Whereas the number of progenitors in bone marrow is significantly decreased, the differentiation of osteoblasts from Abl knockout mice is also impaired [92]. Using osteoblast culture, distinct roles in the oxidative stress response between c-Abl and ATM, have been proposed [93]. Although decreased expression of peroxiredoxin 1 (Prdx1) due to down-regulation of PKCδ was observed upon arsenate-induced oxidative stress in osteoblasts from Atm knockout mice, expression of the redox protein, through the upregulation of PKCδ, was increased in the cells derived from Abl knockouts. The opposite roles in the oxidative stress response may cause similar bone phenotypes in the knockout mice of Abl and Atm genes through distinct mechanisms. Life-span shortening and age-related defects have been reported in mice lacking Prdx1 or MsrA, which encodes methionine sulfoxide reductase [94, 95]. Both genes play important roles in the oxidative stress response through anti-ROS activity. Whereas the bone phenotype in these mutant mice has not yet been described, it will be interesting to see the potential pathogenic phenotype in bone from these mice. Oxidative stress, such as that caused by ROS, often causes damages in DNA, suggesting that the genomic stability and oxidative stress response may share some common pathways in the aging phenotype. As mentioned with Atm mice, an antioxidant also partially rescues the perinatal lethality observed in Ku86 knockout mice [96]. In addition to DNA damage, ROS is important in signal transduction and pathogenesis of diseases as well. For example, anti-oxidative agents reverse insulin resistance in diabetic models [97, 98]. Although it remains unclear whether ROS targets are part of the mechanistic pathways affected by aging, management of ROS may be significantly implicated in osteoblast function and aging.
The Aging Phenotype and Defects in Mineral Metabolism
Other models for accelerated aging phenotypes, where the responsible genes are apparently not directly involved in genomic integrity also exist. Mice carrying hypomorphic mutations of the gene Klotho show multiple aging phenotypes [99]. In Klotho mice (kl/kl), both bone formation and resorption are reduced, indicating a low turnover of bone metabolism resembling human osteoporosis [100]. Although neither osteoblasts nor osteoclasts express the kl gene, ex vivo cultures of osteoblastogenesis and osteoclastogenesis show reduced differentiation independently in both lineages. In contrast to the canonical progeroid models, this is a unique model for age-related osteoporosis in humans. Indeed, the molecular functions of KL protein have been reported. The protein, which is structurally similar to β-glucosidase, possesses β-glucuronidase activity [101]. KL protein acts as a co-receptor for IGF and is also required for FGF23 signaling through FGFR1 [102–107]. FGF23 has been identified as a gene responsible for autosomal dominant hypophosphatemic rickets and is suggested to play an important role in phosphate metabolism as a hormone, a candidate for phosphatonin [104]. FGF23 knockout mice also exhibit a premature aging-like phenotype [105]. Interestingly, the mice have elevated serum levels of vitamin D and hyperphosphatemia, and a part of the aging phenotype was rescued by lowering the vitamin D levels [105–107]. It is therefore suggested that control of the phosphate-regulating system by FGF23-KL is associated with the aging phenotype including osteoporosis. Notably, PHEX (phosphate-regulating gene with homology to endopeptidases on the X chromosome) is highly expressed in osteocytes [108–111], and declines with age as well as with post-OVX and mechanical unloading [112–114]. Conceivably, osteocytes may be implicated in phosphate metabolism and age-related osteoporosis. In fact, FGF signaling coordinately regulates mineralization-related genes in the osteoblast lineage, and that ERK signaling is essential for Dmp1 expression and osteocyte differentiation in vivo [115].
What Mouse Models Teach
It has been recently described that mice deficient for molecular clock genes, such as Per1/2, Cry1/2, and BMAL1, exhibit increased bone mass with elevated bone formation [116]. The clock components inhibit osteoblast proliferation triggered by CREB activation responding to signals from sympathetic neurons. In contrast, it has also been reported that BMAL1 knockout mice have impaired circadian rhythms and display a premature aging phenotype including decreased bone mass [117]. Although these apparently opposite observations might be due to age differences (increased bone mass at 2 months; decreased at 40 weeks of age, compared to wild-type controls), bone phenotype is largely affected by many factors including mobility. Thus, the same mouse can tell different stories. Whereas decreased bone mass is a major indication of the aging phenotype as mentioned, age-related structural and functional alterations are seen not only in bone but also in other tissues and organs as well. Age-related osteoporosis has been recognized as due to a combination of age-related changes in bone caused by bone cell dysfunction, age-related decline in mineral metabolism or hormonal regulation, and neuronal and/or gonadal dysregulation. Nevertheless, these models inform us of the molecular mechanisms involved in bone biology, especially the molecular and cellular basis of bone pathophysiology, and include the possibility that cell autonomous bone defects may be implicated, at least in part, in the pathogenesis of age-related osteoporosis. Furthermore, the described genetically defined models can be useful for elucidation of the underlying mechanisms in pharmacological and other therapeutic-targeting studies.
References
Aufdemorte TB, Fox WC, Miller D, Buffum K, Holt GR, Carey KD. A non-human primate model for the study of osteoporosis and oral bone loss. Bone. 1993;14(3):581–6.
Champ JE, Binkley N, Havighurst T, Colman RJ, Kemnitz JW, Roecker EB. The effect of advancing age on bone mineral content of female rhesus monkeys. Bone. 1996;19(5):485–92.
Colman RJ, Kemnitz JW, Lane MA, Abbott DH, Binkley N. Skeletal effects of aging and menopausal status in female rhesus macaques. J Clin Endocrinol Metab. 1999;84(11):4144–8.
Colman RJ, Lane MA, Binkley N, Wegner FH, Kemnitz JW. Skeletal effects of aging in male rhesus monkeys. Bone. 1999;24(1):17–23.
Jayo MJ, Rankin SE, Weaver DS, Carlson CS, Clarkson TB. Accuracy and precision of lumbar bone mineral content by dual-energy X-ray absorptiometry in live female monkeys. Calcif Tissue Int. 1991;49(6):438–40.
Jayo MJ, Weaver DS, Rankin SE, Kaplan JR. Accuracy and reproducibility of lumbar bone mineral status determined by dual photon absorptiometry in live male cynomolgus macaques (Macaca fascicularis). Lab Anim Sci. 1990;40(3):266–9.
Halloran BP, Ferguson VL, Simske SJ, Burghardt A, Venton LL, Majumdar S. Changes in bone structure and mass with advancing age in the male C57BL/6 J mouse. J Bone Miner Res. 2002;17(6):1044–50.
Ferguson VL, Ayers RA, Bateman TA, Simske SJ. Bone development and age-related bone loss in male C57BL/6 J mice. Bone. 2003;33(3):387–98.
Perkins SL, Gibbons R, Kling S, Kahn AJ. Age-related bone loss in mice is associated with an increased osteoclast progenitor pool. Bone. 1994;15(1):65–72.
Cao J, Venton L, Sakata T, Halloran BP. Expression of RANKL and OPG correlates with age-related bone loss in male C57BL/6 mice. J Bone Miner Res. 2003;18(2):270–7.
Bergman RJ, Gazit D, Kahn AJ, Gruber H, McDougall S, Hahn TJ. Age-related changes in osteogenic stem cells in mice. J Bone Miner Res. 1996;11(5):568–77.
Morrison SJ, Wandycz AM, Akashi K, Globerson A, Weissman IL. The aging of hematopoietic stem cells. Nat Med. 1996;2(9):1011–6.
Ghia P, Melchers F, Rolink AG. Age-dependent changes in B lymphocyte development in man and mouse. Exp Gerontol. 2000;35(2):159–65.
LeMaoult J, Manavalan JS, Dyall R, Szabo P, Nikolic-Zugic J, Weksler ME. Cellular basis of B cell clonal populations in old mice. J Immunol. 1999;162(11):6384–91.
LaMothe JM, Hepple RT, Zernicke RF. Selected ontribution: bone adaptation with aging and long-term caloric restriction in Fischer 344 x Brown-Norway F1-hybrid rats. J Appl Physiol. 2003;95:1739–45.
Westerbeek ZW, Hepple RT, Zernicke RF. Effects of aging and caloric restriction on bone structure and mechanical properties. J Gerontol A Biol Sci Med Sci. 2008;63(11):1131–6.
Pietschmann P, Skalicky M, Kneissel M, Rauner M, Hofbauer G, Stupphann D, Viidik A. Bone structure and metabolism in a rodent model of male senile osteoporosis. Exp Gerontol. 2007;42(11):1099–108.
Ikeda T, Utsuyama M, Hirokawa K. Expression profiles of receptor activator of nuclear factor kappaB ligand, receptor activator of nuclear factor kappaB, and osteoprotegerin messenger RNA in aged and ovariectomized rat bones. J Bone Miner Res. 2001;16(8):1416–25. 12-.
Duque G, Rivas D, Li W, Li A, Henderson JE, Ferland G, Gaudreau P. Age-related bone loss in the LOU/c rat model of healthy ageing. Exp Gerontol. 2009;44(3):183–9.
Takeda T, Matsushita T, Kurozumi M, Takemura K, Higuchi K, Hosokawa M. Pathobiology of the senescence-accelerated mouse (SAM). Exp Gerontol. 1997;32(1-2):117–27.
Jilka RL, Weinstein RS, Takahashi K, Parfitt AM, Manolagas SC. Linkage of decreased bone mass with impaired osteoblastogenesis in a murine model of accelerated senescence. J Clin Invest. 1996;97(7):1732–40.
Silva MJ, Brodt MD, Ettner SL. Long bones from the senescence accelerated mouse SAMP6 have increased size but reduced whole-bone strength and resistance to fracture. J Bone Miner Res. 2002;17(9):1597–603.
Kajkenova O, Lecka-Czernik B, Gubrij I, et al. Increased adipogenesis and myelopoiesis in the bone marrow of SAMP6, a murine model of defective osteoblastogenesis and low turnover osteopenia. J Bone Miner Res. 1997;12(11):1772–9.
Matsushita M, Tsuboyama T, Kasai R, et al. Age-related changes in bone mass in the senescence-accelerated mouse (SAM). SAM-R/3 and SAM-P/6 as new murine models for senile osteoporosis. Am J Pathol. 1986;125(2):276–83.
Takada K, Inaba M, Ichioka N, et al. Treatment of senile osteoporosis in SAMP6 mice by intra-bone marrow injection of allogeneic bone marrow cells. Stem Cells. 2006;24(2):399–405.
Duque G, Macoritto M, Dion N, Ste-Marie LG, Kremer R. 1,25(OH)2D3 acts as a bone-forming agent in the hormone-independent senescence-accelerated mouse (SAM-P/6). Am J Physiol Endocrinol Metab. 2005;288(4):E723–30.
Ichioka N, Inaba M, Kushida T, et al. Prevention of senile osteoporosis in SAMP6 mice by intrabone marrow injection of allogeneic bone marrow cells. Stem Cells. 2002;20(6):542–51.
Li CY, Schaffler MB, Wolde-Semait HT, Hernandez CJ, Jepsen KJ. Genetic background influences cortical bone response to ovariectomy. J Bone Miner Res. 2005;20(12):2150–8.
Beamer WG, Shultz KL, Donahue LR, et al. Quantitative trait loci for femoral and lumbar vertebral bone mineral density in C57BL/6 J and C3H/HeJ inbred strains of mice. J Bone Miner Res. 2001;16(7):1195–206.
Hishiya A, Watanabe K. Progeroid syndrome as a model for impaired bone formation in senile osteoporosis. J Bone Miner Metab. 2004;22(5):399–403.
Warner HR, Sierra F. Models of accelerated ageing can be informative about the molecular mechanisms of ageing and/or age-related pathology. Mech Ageing Dev. 2003;124(5):581–7.
Hasty P, Vijg J. Accelerating aging by mouse reverse genetics: a rational approach to understanding longevity. Aging Cell. 2004;3(2):55–65.
Hasty P, Campisi J, Hoeijmakers J, van Steeg H, Vijg J. Aging and genome maintenance: lessons from the mouse? Science. 2003;299(5611):1355–9.
Kuro-o M. Disease model: human aging. Trends Mol Med. 2001;7(4):179–81.
Kipling D, Davis T, Ostler EL, Faragher RG. What can progeroid syndromes tell us about human aging? Science. 2004;305(5689):1426–31.
Yu CE, Oshima J, Fu YH, et al. Positional cloning of the Werner's syndrome gene. Science. 1996;272(5259):258–62.
Lombard DB, Beard C, Johnson B, et al. Mutations in the WRN gene in mice accelerate mortality in a p53-null background. Mol Cell Biol. 2000;20(9):3286–91.
Du X, Shen J, Kugan N, et al. Telomere shortening exposes functions for the mouse werner and bloom syndrome genes. Mol Cell Biol. 2004;24(19):8437–46.
Chang S, Multani AS, Cabrera NG, et al. Essential role of limiting telomeres in the pathogenesis of Werner syndrome. Nat Genet. 2004;36(8):877–82.
Mohaghegh P, Hickson ID. DNA helicase deficiencies associated with cancer predisposition and premature ageing disorders. Hum Mol Genet. 2001;10(7):741–6.
Kitao S, Shimamoto A, Goto M, et al. Mutations in RECQL4 cause a subset of cases of Rothmund-Thomson syndrome. Nat Genet. 1999;22(1):82–4.
Hoki Y, Araki R, Fujimori A, et al. Growth retardation and skin abnormalities of the Recql4-deficient mouse. Hum Mol Genet. 2003;12(18):2293–9.
Yang J, Murthy S, Winata T, et al. Recql4 haploinsufficiency in mice leads to defects in osteoblast progenitors: Implications for low bone mass phenotype. Biochem Biophys Res Commun. 2006;344(1):346–52.
Van Maldergem L, Siitonen HA, Jalkh N, et al. Revisiting the craniosynostosis-radial ray hypoplasia association: Baller-Gerold syndrome caused by mutations in the RECQL4 gene. J Med Genet. 2006;43(2):148–52.
Eriksson M, Brown WT, Gordon LB, et al. Recurrent de novo point mutations in lamin A cause Hutchinson-Gilford progeria syndrome. Nature. 2003;423(6937):293–8.
De Sandre-Giovannoli A, Bernard R, Cau P, et al. Lamin a truncation in Hutchinson-Gilford progeria. Science. 2003;300(5628):2055.
Mounkes LC, Kozlov S, Hernandez L, Sullivan T, Stewart CL. A progeroid syndrome in mice is caused by defects in A-type lamins. Nature. 2003;423(6937):298–301.
Duque G, Rivas D. Age-related changes in lamin A/C expression in the osteoarticular system: laminopathies as a potential new aging mechanism. Mech Ageing Dev. 2006;127(4):378–83.
Rivas D, Li W, Akter R, Henderson JE, Duque G. Accelerated features of age-related bone loss in zmpste24 metalloproteinase-deficient mice. J Gerontol A Biol Sci Med Sci. 2009;64(10):1015–24.
Li W, Yeo LS, Vidal C, McCorquodale T, Herrmann M, Fatkin D, Duque G. Decreased bone formation and osteopenia in lamin a/c-deficient mice. PLoS One. 2011;6(4), e19313.
Duque G, Li W, Yeo LS, Vidal C, Fatkin D. Attenuated anabolic response to exercise in lamin A/C haploinsufficient mice. Bone. 2011;49(3):412–8.
Tong J, Li W, Vidal C, Yeo LS, Fatkin D, Duque G. Lamin A/C deficiency is associated with fat infiltration of muscle and bone. Mech Ageing Dev. 2011;132(11-12):552–9.
Vogel H, Lim DS, Karsenty G, Finegold M, Hasty P. Deletion of Ku86 causes early onset of senescence in mice. Proc Natl Acad Sci U S A. 1999;96(19):10770–5.
Sun LQ, Lee DW, Zhang Q, et al. Growth retardation and premature aging phenotypes in mice with disruption of the SNF2-like gene. PASG Genes Dev. 2004;18(9):1035–46.
Trifunovic A, Wredenberg A, Falkenberg M, et al. Premature ageing in mice expressing defective mitochondrial DNA polymerase. Nature. 2004;429(6990):417–23.
Mostoslavsky R, Chua KF, Lombard DB, et al. Genomic instability and aging-like phenotype in the absence of mammalian SIRT6. Cell. 2006;124(2):315–29.
Hartwell L. Defects in a cell cycle checkpoint may be responsible for the genomic instability of cancer cells. Cell. 1992;71(4):543–6.
Nurse P. Checkpoint pathways come of age. Cell. 1997;91(7):865–7.
Rotman G, Shiloh Y. ATM: from gene to function. Hum Mol Genet. 1998;7(10):1555–63.
Lavin MF, Shiloh Y. The genetic defect in ataxia-telangiectasia. Annu Rev Immunol. 1997;15:177–202.
Barlow C, Hirotsune S, Paylor R, et al. Atm-deficient mice: a paradigm of ataxia telangiectasia. Cell. 1996;86(1):159–71.
Xu Y, Ashley T, Brainerd EE, Bronson RT, Meyn MS, Baltimore D. Targeted disruption of ATM leads to growth retardation, chromosomal fragmentation during meiosis, immune defects, and thymic lymphoma. Genes Dev. 1996;10(19):2411–22.
Elson A, Wang Y, Daugherty CJ, et al. Pleiotropic defects in ataxia-telangiectasia protein-deficient mice. Proc Natl Acad Sci U S A. 1996;93(23):13084–9.
Ito K, Hirao A, Arai F, et al. Regulation of oxidative stress by ATM is required for self-renewal of haematopoietic stem cells. Nature. 2004;431(7011):997–1002.
Hishiya A, Ito M, Aburatani H, Motoyama N, Ikeda K, Watanabe K. Ataxia telangiectasia mutated (Atm) knockout mice as a model of osteopenia due to impaired bone formation. Bone. 2005;37(4):497–503.
Tyner SD, Venkatachalam S, Choi J, et al. p53 mutant mice that display early ageing-associated phenotypes. Nature. 2002;415(6867):45–53.
Maier B, Gluba W, Bernier B, et al. Modulation of mammalian life span by the short isoform of p53. Genes Dev. 2004;18(3):306–19.
Lengner CJ, Steinman HA, Gagnon J, et al. Osteoblast differentiation and skeletal development are regulated by Mdm2-p53 signaling. J Cell Biol. 2006;172(6):909–21.
Wang X, Kua HY, Hu Y, et al. p53 functions as a negative regulator of osteoblastogenesis, osteoblast-dependent osteoclastogenesis, and bone remodeling. J Cell Biol. 2006;172(1):115–25.
Rasheed N, Wang X, Niu QT, Yeh J, Li B. Atm-deficient mice: an osteoporosis model with defective osteoblast differentiation and increased osteoclastogenesis. Hum Mol Genet. 2006;15(12):1938–48.
Manolagas SC, Jilka RL. Bone marrow, cytokines, and bone remodeling. Emerging insights into the pathophysiology of osteoporosis. N Engl J Med. 1995;332(5):305–11.
Davey RA, MacLean HE, McManus JF, Findlay DM, Zajac JD. Genetically modified animal models as tools for studying bone and mineral metabolism. J Bone Miner Res. 2004;19(6):882–92.
Chien KR, Karsenty G. Longevity and lineages: toward the integrative biology of degenerative diseases in heart, muscle, and bone. Cell. 2005;120(4):533–44.
Karsenty G. The complexities of skeletal biology. Nature. 2003;423(6937):316–8.
Karsenty G. The genetic transformation of bone biology. Genes Dev. 1999;13(23):3037–51.
Yeh ET, Reiser H, Benacerraf B, Rock KL. The expression, function, and ontogeny of a novel T cell-activating protein, TAP, in the thymus. J Immunol. 1986;137(4):1232–8.
Stanford WL, Haque S, Alexander R, et al. Altered proliferative response by T lymphocytes of Ly-6A (Sca-1) null mice. J Exp Med. 1997;186(5):705–17.
Bonyadi M, Waldman SD, Liu D, Aubin JE, Grynpas MD, Stanford WL. Mesenchymal progenitor self-renewal deficiency leads to age-dependent osteoporosis in Sca-1/Ly-6A null mice. Proc Natl Acad Sci U S A. 2003;100(10):5840–5.
Ito CY, Li CY, Bernstein A, Dick JE, Stanford WL. Hematopoietic stem cell and progenitor defects in Sca-1/Ly-6A-null mice. Blood. 2003;101(2):517–23.
Duque G, Troen BR. Understanding the mechanisms of senile osteoporosis: new facts for a major geriatric syndrome. J Am Geriatr Soc. 2008;56(5):935–41.
Ogata N, Chikazu D, Kubota N, et al. Insulin receptor substrate-1 in osteoblast is indispensable for maintaining bone turnover. J Clin Invest. 2000;105(7):935–43.
Gong Y, Slee RB, Fukai N, et al. LDL receptor-related protein 5 (LRP5) affects bone accrual and eye development. Cell. 2001;107(4):513–23.
Boyden LM, Mao J, Belsky J, et al. High bone density due to a mutation in LDL-receptor-related protein 5. N Engl J Med. 2002;346(20):1513–21.
Kato M, Patel MS, Levasseur R, et al. Cbfa1-independent decrease in osteoblast proliferation, osteopenia, and persistent embryonic eye vascularization in mice deficient in Lrp5, a Wnt coreceptor. J Cell Biol. 2002;157(2):303–14.
Kulkarni NH, Onyia JE, Zeng Q, et al. Orally bioavailable GSK-3alpha/beta dual inhibitor increases markers of cellular differentiation in vitro and bone mass in vivo. J Bone Miner Res. 2006;21(6):910–20.
Clement-Lacroix P, Ai M, Morvan F, et al. Lrp5-independent activation of Wnt signaling by lithium chloride increases bone formation and bone mass in mice. Proc Natl Acad Sci U S A. 2005;102(48):17406–11.
Bennett CN, Longo KA, Wright WS, et al. Regulation of osteoblastogenesis and bone mass by Wnt10b. Proc Natl Acad Sci U S A. 2005;102(9):3324–9.
Ross SE, Hemati N, Longo KA, et al. Inhibition of adipogenesis by Wnt signaling. Science. 2000;289(5481):950–3.
Gunther T, Poli C, Muller JM, et al. Fhl2 deficiency results in osteopenia due to decreased activity of osteoblasts. Embo J. 2005;24(17):3049–56.
Kharbanda S, Yuan ZM, Weichselbaum R, Kufe D. Functional role for the c-Abl protein tyrosine kinase in the cellular response to genotoxic stress. Biochim Biophys Acta. 1997;1333(2):O1–7.
Hantschel O, Superti-Furga G. Regulation of the c-Abl and Bcr-Abl tyrosine kinases. Nat Rev Mol Cell Biol. 2004;5(1):33–44.
Li B, Boast S. de los Santos K, et al. Mice deficient in Abl are osteoporotic and have defects in osteoblast maturation. Nat Genet. 2000;24(3):304–8.
Li B, Wang X, Rasheed N, et al. Distinct roles of c-Abl and Atm in oxidative stress response are mediated by protein kinase C delta. Genes Dev. 2004;18(15):1824–37.
Moskovitz J, Bar-Noy S, Williams WM, Requena J, Berlett BS, Stadtman ER. Methionine sulfoxide reductase (MsrA) is a regulator of antioxidant defense and lifespan in mammals. Proc Natl Acad Sci U S A. 2001;98(23):12920–5.
Neumann CA, Krause DS, Carman CV, et al. Essential role for the peroxiredoxin Prdx1 in erythrocyte antioxidant defence and tumour suppression. Nature. 2003;424(6948):561–5.
Reliene R, Goad ME, Schiestl RH. Developmental cell death in the liver and newborn lethality of Ku86 deficient mice suppressed by antioxidant N-acetyl-cysteine. DNA Repair (Amst). 2006.
Furukawa S, Fujita T, Shimabukuro M, et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004;114(12):1752–61.
Houstis N, Rosen ED, Lander ES. Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature. 2006;440(7086):944–8.
Kuro-o M, Matsumura Y, Aizawa H, et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature. 1997;390(6655):45–51.
Kawaguchi H, Manabe N, Miyaura C, Chikuda H, Nakamura K, Kuro-o M. Independent impairment of osteoblast and osteoclast differentiation in klotho mouse exhibiting low-turnover osteopenia. J Clin Invest. 1999;104(3):229–37.
Tohyama O, Imura A, Iwano A, et al. Klotho is a novel beta-glucuronidase capable of hydrolyzing steroid beta-glucuronides. J Biol Chem. 2004;279(11):9777–84.
Kurosu H, Ogawa Y, Miyoshi M, et al. Regulation of fibroblast growth factor-23 signaling by klotho. J Biol Chem. 2006;281(10):6120–3.
Kurosu H, Yamamoto M, Clark JD, et al. Suppression of aging in mice by the hormone Klotho. Science. 2005;309(5742):1829–33.
ADHR-Consortium. Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. Nat Genet. 2000;26(3):345–8.
Razzaque MS, Sitara D, Taguchi T, St-Arnaud R, Lanske B. Premature aging-like phenotype in fibroblast growth factor 23 null mice is a vitamin D-mediated process. Faseb J. 2006;20:720–2.
Tsujikawa H, Kurotaki Y, Fujimori T, Fukuda K, Nabeshima Y. Klotho, a gene related to a syndrome resembling human premature aging, functions in a negative regulatory circuit of vitamin D endocrine system. Mol Endocrinol. 2003;17(12):2393–403.
Yoshida T, Fujimori T, Nabeshima Y. Mediation of unusually high concentrations of 1,25-dihydroxyvitamin D in homozygous klotho mutant mice by increased expression of renal 1alpha-hydroxylase gene. Endocrinology. 2002;143(2):683–9.
Liu S, Zhou J, Tang W, Jiang X, Rowe DW, Quarles LD. Pathogenic role of Fgf23 in Hyp mice. Am J Physiol Endocrinol Metab. 2006;291(1):E38–49.
Thompson DL, Sabbagh Y, Tenenhouse HS, et al. Ontogeny of Phex/PHEX protein expression in mouse embryo and subcellular localization in osteoblasts. J Bone Miner Res. 2002;17(2):311–20.
Westbroek I, De Rooij KE, Nijweide PJ. Osteocyte-specific monoclonal antibody MAb OB7.3 is directed against Phex protein. J Bone Miner Res. 2002;17(5):845–53.
Miao D, Bai X, Panda D, McKee M, Karaplis A, Goltzman D. Osteomalacia in hyp mice is associated with abnormal phex expression and with altered bone matrix protein expression and deposition. Endocrinology. 2001;142(2):926–39.
Aguirre JI, Plotkin LI, Stewart SA, et al. Osteocyte apoptosis is induced by weightlessness in mice and precedes osteoclast recruitment and bone loss. J Bone Miner Res. 2006;21(4):605–15.
Jilka RL, Weinstein RS, Bellido T, Roberson P, Parfitt AM, Manolagas SC. Increased bone formation by prevention of osteoblast apoptosis with parathyroid hormone. J Clin Invest. 1999;104(4):439–46.
Tomkinson A, Gevers EF, Wit JM, Reeve J, Noble BS. The role of estrogen in the control of rat osteocyte apoptosis. J Bone Miner Res. 1998;13(8):1243–50.
Kyono A, Avishai N, Ouyang Z, Landreth GE, Murakami S. FGF and ERK signaling coordinately regulate mineralization-related genes and play essential roles in osteocyte differentiation. J Bone Miner Metab. 2012;30(1):19–30.
Fu L, Patel MS, Bradley A, Wagner EF, Karsenty G. The molecular clock mediates leptin-regulated bone formation. Cell. 2005;122(5):803–15.
Kondratov RV, Kondratova AA, Gorbacheva VY, Vykhovanets OV, Antoch MP. Early aging and age-related pathologies in mice deficient in BMAL1, the core component of the circadian clock. Genes Dev. 2006;20(14):1868–73.
Watanabe K, Hishiya A. Mouse models of senile osteoporosis. Mol Aspects Med. 2005;26(3):221–31.
Duque G. As a matter of fat: new perspectives on the understanding of age-related bone loss. BoneKEy-Osteovision. 2007;4(4):129–40.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Watanabe, K., Duque, G. (2016). Animal Models for Aging Bone. In: Duque, G., Kiel, D. (eds) Osteoporosis in Older Persons. Springer, Cham. https://doi.org/10.1007/978-3-319-25976-5_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-25976-5_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-25974-1
Online ISBN: 978-3-319-25976-5
eBook Packages: MedicineMedicine (R0)