Abstract
Hypercalcemia associated with hydrochlorothiazide is a well-known clinical entity, likely due to an increased renal tubular reabsorption of calcium. However, it is estimated that approximately two-thirds of patients with thiazide-associated hypercalcemia have underlying primary hyperparathyroidism (PHPT). Persistence of hypercalcemia after more than 2 years of thiazide use and higher serum calcium and parathyroid hormone (PTH) levels at diagnosis suggest PHPT. Many commonly used medications can also influence calcium and PTH measurement in patients with PHPT, including estrogen, raloxifene, calcium, and vitamin D. A number of other commonly used medications can influence PTH and calcium measurements in patients without PHPT including numerous antihypertensive agents, aromatase inhibitors, estrogen, tenofovir, and several osteoporosis therapies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Primary hyperparathyroidism
- Hypercalcemia
- Hydrochlorothiazide
- Lithium
- Bisphosphonates
- Teriparatide
- Estrogen
- Raloxifene
- Aromatase inhibitors
- Tenofovir
Case Presentation
An 82-year-old female is referred for evaluation of hypercalcemia, with a serum calcium of 11.7 mg/dL (nl, 8.9–10.1) that was identified on lab work 1 month prior after she complained of increasing fatigue over the last 2 months. Subsequent laboratory testing identified the following: serum calcium – 10.8 mg/dL and phosphorus – 3.7 mg/dL (nl, 2.5–4.5) with at concomitant PTH of 48 pg/mL (nl, 15–50). Previous calcium measurements were noted to be normal, but more recently when checked, were high normal. Further laboratory studies that were done and normal included TSH, complete blood count, serum protein electrophoresis, serum creatinine, and 25-hydroxyvitamin D. Her medications of note included one calcium carbonate daily (600 mg elemental calcium per tablet), one multivitamin per day, and hydrochlorothiazide 25 mg one daily for hypertension. Her estimated daily dietary calcium intake was 600 mg per day. She denied a history of external beam radiation treatments to her head or neck, and there was no family history of primary hyperparathyroidism (PHPT) or hypercalcemia, familial endocrine syndromes, or hip fractures.
She denied a history of nephrolithiasis or fragility fractures. Her dual-energy X-ray absorptiometry (DXA) bone mineral density (BMD) revealed a non-dominant left one-third radius T-score of – 0.5, worst femur neck T-score of – 2.0, and lumbar spine T-score of – 1.0. The hip and spine had declined 6.2 % and 4.7 %, respectively, both greater than the least significant change, from the previous measure done approximately 6.5 years previously. Her physical examination revealed a height of 157.6 cm, weight of 85.1 kg, and blood pressure of 136/64 but was otherwise unremarkable.
Assessment and Diagnosis
The patient’s lab work is consistent with primary hyperparathyroidism (PHPT). However, thiazide diuretics can also be associated with hypercalcemia [1]. Increased renal tubular reabsorption of calcium resulting in reduced urine calcium excretion is the most likely explanation for hypercalcemia associated with thiazide diuretics [2–4]. A mean increase of 0.8 mg/dL in albumin-adjusted serum calcium level is seen with thiazide use. Serum calcium concentrations are increased independently of PTH [5]. However, the increase in renal tubular calcium resorption and serum calcium is no longer observed after 2 years of therapy [6]. Upon review of the patient’s medical record, she had been on hydrochlorothiazide for more than 10 years, making it unlikely that thiazide use was the primary cause of her hypercalcemia. It is estimated that approximately two-thirds of patients with thiazide-associated hypercalcemia have underlying PHPT, based on the persistence of hypercalcemia after discontinuation of the thiazide [1]. Additional factors favoring PHPT in thiazide-associated hypercalcemia include higher serum calcium and PTH levels at diagnosis [1].
Several other medications have effects on PTH and serum calcium that should be considered when evaluating patients with PHPT. In women with PHPT, estrogen and raloxifene lower serum total calcium, but PTH levels do not change significantly [7, 8]. PTH secretion can also be modified by calcium [9] and vitamin D supplements [10] in PHPT subjects. Lithium has been associated with hypercalcemia as well as parathyroid hyperplasia and adenomas [11].
There are a number of other commonly used medications that can influence PTH and calcium measurements in patients without PHPT. Aromatase inhibitors such as letrozole have been associated with a reduction in PTH in postmenopausal women likely related to efflux of calcium from the skeleton with lower estrogen levels [12]. On the other hand, there is a trend toward an increase in PTH with estrogen treatment in postmenopausal women without PHPT likely related to a reduction in skeletal calcium release [13, 14]. Similarly, antiresorptive osteoporosis therapies such as denosumab [15] and potent bisphosphonates [16–18] can also be associated with an increase in PTH and reductions in serum calcium levels. Teriparatide, rhPTH (1–34), can lead to mild elevations of serum calcium in osteoporotic subjects, but are generally not clinically meaningful [19]. In addition, the timing of the serum calcium measurement after the teriparatide is critical, such that measures done >16 h post-dose are unlikely to be elevated [19, 20]. Several antihypertensive agents have effects on PTH secretion without significant effects on serum calcium including loop diuretics and calcium channel blockers which have been associated with an increased PTH [21, 22], whereas renin-angiotensin-aldosterone system inhibitors have been associated with a lower PTH [22]. Finally, antiretroviral therapy for HIV-1 infection which includes tenofovir disoproxil fumarate (TDF) is also associated with increased PTH and excess bone loss [23].
Management
The patient followed-up 3 months after discontinuation of hydrochlorothiazide and her serum calcium and phosphorus were 11 mg/dL and 3.6 mg/dL, respectively, with a PTH of 70 pg/mL, consistent with PHPT. Long-term discontinuation of hydrochlorothiazide may not be necessary in patients with thiazide-associated hypercalcemia since serious sequelae related to hypercalcemia in these patients despite continued use are rare [1]. However, she remained off of hydrochlorothiazide and opted to observe after a discussion about the risks and benefits of parathyroid surgery. She did have a 10-year probability of major osteoporotic and hip fracture risk, as calculated by WHO Fracture Risk Assessment Tool (FRAX®), of 15 % and 4 %, respectively. Hence, after a discussion of risks and benefits of alendronate therapy, she decided to initiate treatment. She was advised to continue her current calcium intake and avoid falls.
Outcome
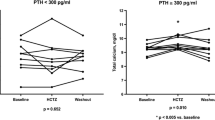
The patient remained clinically stable over years of follow-up. Her maximum serum calcium level, 5 years after her initial elevation, was 11.2 mg/dL. However, she had intermittently high normal calcium measurements as well. Her last measured serum calcium was 10.1 mg/dL at 7 years after her diagnosis of PHPT. Her PTH was periodically measured and was generally 1.5-fold elevated. Her primary provider discontinued alendronate after 6.5 years of treatment. The patient fell, suffered an acetabular fracture, and died shortly thereafter at 90 years of age, 8 years after her diagnosis of PHPT.
Clinical Pearls/Pitfalls
-
Approximately two-third patients with thiazide-associated hypercalcemia have underlying PHPT.
-
After 2 years of thiazide use, the increase in renal tubular calcium resorption and serum calcium is no longer observed.
-
Many commonly used medications can influence the calcium and PTH measurement in patients with PHPT, including estrogen, raloxifene, calcium, and vitamin D.
-
A number of other commonly used medications can influence PTH and calcium measurements in patients without PHPT including numerous antihypertensive agents, aromatase inhibitors, estrogen, tenofovir, and several osteoporosis therapies.
-
In patients with PHPT and increased fracture risk, who opt for observation rather than parathyroidectomy, consider treatment with bisphosphonates.
References
Wermers RA, Kearns AE, Jenkins GD, Melton 3rd LJ. Incidence and clinical spectrum of thiazide-associated hypercalcemia. Am J Med. 2007;120:911 e919–915.
Brickman AS, Massry SG, Coburn JW. Changes in serum and urinary calcium during treatment with hydrochlorothiazide: studies on mechanisms. J Clin Invest. 1972;51:945–54.
Grieff M, Bushinsky DA. Diuretics and disorders of calcium homeostasis. Semin Nephrol. 2011;31:535–41.
Middler S, Pak CY, Murad F, Bartter FC. Thiazide diuretics and calcium metabolism. Metabolism. 1973;22:139–46.
Rejnmark L, Vestergaard P, Heickendorff L, Andreasen F, Mosekilde L. Loop diuretics alter the diurnal rhythm of endogenous parathyroid hormone secretion. A randomized-controlled study on the effects of loop- and thiazide-diuretics on the diurnal rhythms of calcitropic hormones and biochemical bone markers in postmenopausal women. Eur J Clin Invest. 2001;31:764–72.
Bolland MJ, Ames RW, Horne AM, Orr-Walker BJ, Gamble GD, Reid IR. The effect of treatment with a thiazide diuretic for 4 years on bone density in normal postmenopausal women. Osteoporos Int. 2007;18:479–86.
Marcus R, Madvig P, Crim M, Pont A, Kosek J. Conjugated estrogens in the treatment of postmenopausal women with hyperparathyroidism. Ann Intern Med. 1984;100:633–40.
Rubin MR, Lee KH, McMahon DJ, Silverberg SJ. Raloxifene lowers serum calcium and markers of bone turnover in postmenopausal women with primary hyperparathyroidism. J Clin Endocrinol Metab. 2003;88:1174–8.
Tohme JF, Bilezikian JP, Clemens TL, Silverberg SJ, Shane E, Lindsay R. Suppression of parathyroid hormone secretion with oral calcium in normal subjects and patients with primary hyperparathyroidism. J Clin Endocrinol Metab. 1990;70:951–6.
Grey A, Lucas J, Horne A, Gamble G, Davidson JS, Reid IR. Vitamin D repletion in patients with primary hyperparathyroidism and coexistent vitamin D insufficiency. J Clin Endocrinol Metab. 2005;90:2122–6.
Mallette LE, Eichhorn E. Effects of lithium carbonate on human calcium metabolism. Arch Intern Med. 1986;146:770–6.
Heshmati HM, Khosla S, Robins SP, O’Fallon WM, Melton 3rd LJ, Riggs BL. Role of low levels of endogenous estrogen in regulation of bone resorption in late postmenopausal women. J Bone Miner Res. 2002;17:172–8.
Khosla S, Melton 3rd LJ, Riggs BL. The unitary model for estrogen deficiency and the pathogenesis of osteoporosis: is a revision needed? J Bone Miner Res. 2011;26:441–51.
Lufkin EG, Wahner HW, O’Fallon WM, et al. Treatment of postmenopausal osteoporosis with transdermal estrogen. Ann Intern Med. 1992;117:1–9.
Bekker PJ, Holloway DL, Rasmussen AS, et al. A single-dose placebo-controlled study of AMG 162, a fully human monoclonal antibody to RANKL, in postmenopausal women. J Bone Miner Res. 2004;19:1059–66.
Adami S, Mian M, Bertoldo F, et al. Regulation of calcium-parathyroid hormone feedback in primary hyperparathyroidism: effects of bisphosphonate treatment. Clin Endocrinol. 1990;33:391–7.
Generali D, Dovio A, Tampellini M, et al. Changes of bone turnover markers and serum PTH after night or morning administration of zoledronic acid in breast cancer patients with bone metastases. Br J Cancer. 2008;98:1753–8.
Greenspan SL, Holland S, Maitland-Ramsey L, et al. Alendronate stimulation of nocturnal parathyroid hormone secretion: a mechanism to explain the continued improvement in bone mineral density accompanying alendronate therapy. Proc Assoc Am Physicians. 1996;108:230–8.
Wermers RA, Recknor CP, Cosman F, Xie L, Glass EV, Krege JH. Effects of teriparatide on serum calcium in postmenopausal women with osteoporosis previously treated with raloxifene or alendronate. Osteoporosis Int. 2008;19:1055–65.
Krege JH, Donley DW, Marcus R. Teriparatide, osteoporosis, calcium, and vitamin D. N Engl J Med. 2005;353:634–5; author reply 634–5.
Rejnmark L, Vestergaard P, Pedersen AR, Heickendorff L, Andreasen F, Mosekilde L. Dose-effect relations of loop- and thiazide-diuretics on calcium homeostasis: a randomized, double-blinded Latin-square multiple cross-over study in postmenopausal osteopenic women. Eur J Clin Invest. 2003;33:41–50.
Brown J, de Boer IH, Robinson-Cohen C, et al. Aldosterone, parathyroid hormone, and the use of renin-angiotensin-aldosterone system inhibitors: the multi-ethnic study of atherosclerosis. J Clin Endocrinol Metab. 2015;100:490–9.
Overton ET, Chan ES, Brown TT, Tebas P, McComsey GA, Melbourne KM, Napoli A, Hardin WR, Ribaudo HJ, Yin MT. Vitamin D and calcium attenuate bone loss with antiretroviral therapy initiation. Ann Intern Med. 2015;162:815–24.
Conflict of Interest
All authors state that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Mayo Foundation for Medical Education and Research
About this chapter
Cite this chapter
Wermers, R.A., Griebeler, M.L. (2016). Medication Considerations in Hypercalcemia and Hyperparathyroidism. In: Kearns, A., Wermers, R. (eds) Hyperparathyroidism. Springer, Cham. https://doi.org/10.1007/978-3-319-25880-5_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-25880-5_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-25878-2
Online ISBN: 978-3-319-25880-5
eBook Packages: MedicineMedicine (R0)