Abstract
Context: Arrhythmia is a major cause of morbidity and mortality in Europe and in the United States. The aim of this review article was to assess the results of the prospective studies that evaluated the risk of arrhythmia in patients with overt and subclinical thyroid disease and discuss the management of this arrhythmia.
Evidence Acquisition: Reports published with the following search terms were searched: thyroid, hypothyroidism, hyperthyroidism, subclinical hyperthyroidism, subclinical hypothyroidism, levothyroxine, triiodothyronine, antithyroid drugs, radioiodine, deiodinases, atrial flutter, supraventricular arrhythmia, ventricular arrhythmia, ventricular tachycardia, ventricular fibrillation, torsade de pointe, amiodarone and atrial fibrillation. The investigation was restricted to reports published in English.
Evidence Synthesis: The outcome of this analysis suggests that patients with untreated overt thyroid dysfunction are at increased risk of arrhythmia.
Conclusions: The timely recognition and effective treatment of thyroid dysfunction in patients with arrhythmia is mandatory because the long-term and prognosis of arrythmias may be improved with the appropriate treatment of thyroid dysfunction.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The most common clinical manifestations of thyrotoxic heart disease are heart rate disorders, in particular, sinus tachycardia and atrial fibrillation, which presents in 28 % of patients [1]. Typical arrhythmias found in hyperthyroidism are atrial premature contractions or atrial fibrillation, the latter occurring in 9–22 % of patients [2]. Conversely, ventricular premature contractions are rare in this setting, and if present, their frequency is not decreased after treatment [3]. Malignant ventricular arrhythmias such as ventricular tachycardia or fibrillation, which are potentially fatal, are exceptional [4] and usually occur only in patients with marked heart failure or associated cardiac disease [5]. Surprisingly, there have been few population-based studies examining the long-term influence of thyroid disease and its treatment on morbidity and mortality [6].
Genomic Action of Thyroid Hormone on Heart
Thyroid hormone exerts a broad range of effects on development, growth, and metabolism. The clinical manifestations of thyroid hormone excess and deficiency are dramatic examples of the myriad actions of the hormone. Thyroxine (T4), the primary secretory product of the thyroid, is relatively inactive and is converted to the active hormone, triiodothyronine (T3), by the enzyme thyroxine 5′-deiodinase. The actions of thyroid hormone are primarily the result of the interaction of T3 with nuclear receptors for T3 that bind to regulatory regions of genes (thyroid hormone-response elements) and modify their expression [7]. These receptors have been cloned, and there has been considerable progress in unraveling the various mechanisms by which thyroid hormone regulates gene expression [8].
The clinical findings in hypothyroidism and hyperthyroidism are the net result of the actions of products of a variety of genes whose expression is directly or indirectly regulated by T3. There are markers of thyroid hormone action that can be monitored clinically and that provide information about the ability of T3 to regulate a gene product. Thyroid hormone excess reduces systemic vascular resistance, enhances cardiac contractility, and has a positive chronotropic effect [9]. Thyroid hormone deficiency has the opposite effects: it increases systemic vascular resistance, decreases contractility, and slows the heart rate. These changes in cardiac function are the result of both regulation of cardiac-specific genes by T3 [10] and changes in hemodynamic function induced by T3 [11]. The contractile properties of the heart are dependent on the relative amounts of the products of the various myosin genes [8, 12]. Thyroid hormone exerts marked effects on cardiac contractility through changes in the expression of thyroid hormone-responsive genes as well as through alterations in function of important regulatory proteins [1, 2]. It has been demonstrated that a variety of proteins in the cardiac myocyte, including the α- and β-myosin heavy chains, β-adrenergic receptors, sarcoplasmic reticulum (SR) calcium-activated adenosine triphosphatase (SERCA2), and phospholamban (PLB), calcium transporter proteins are regulated by thyroid hormone [12, 13]. The classically described cellular actions of thyroid hormone are mediated by nuclear triiodothyronine (T3) receptors that function to regulate the expression of specific cardiac genes [8, 10] such as plasma membrane sodium potassium ATPase [14] and voltage-activated K1 channel genes including Kv4.2, Kv4.3, and Kv1.5 [15].
In the ventricle, the transcription of the beta myosine heavy chain (β-MHC) antisense (AS) gene appears to be associated with and linked to the transcription of the α-MHC gene; both are induced in the presence of T3. However, in atria this expression appears to be uncoupled. As observed in the ventricles, the expression of the β-MHC AS gene in the atria is inversely correlated, while the expression of the α-MHC gene is not thyroid hormone responsive and highly expressed in all thyroid states. This observation demonstrates for the first time that the previously identified shared promoter region that lies in the intergenic region between the b-MHC and a-MHC genes is differentially regulated in a tissue-specific manner [10]. Exploration of the differences in cofactors and potential epigenetic influences in this shared intergenic promoter region in atria and ventricles may provide additional information regarding the potential mechanism by which T3 influences the MHC genes in the human heart [12].
Non Genomic Action of Thyroid Hormone on Heart
In addition to the well-characterized nuclear effects of thyroid hormone, some cardiac responses to thyroid hormone appear to be mediated through non genomic mechanisms [16], as suggested by relatively rapid onset of action-faster than can be accounted for by changes in gene expression and protein synthesis and failure to be affected by inhibitors of gene transcription. The significance of these diverse actions remains to be established, but may explain the ability of acute T3 to alter cardiovascular hemodynamics. They may alter the functional proprieties of membrane ion channels and pumps, including the sodium channel and inward rectifying potassium current (IK) [17].
Electrophysiology and Mechanism of Action of T3 on the Atria
Thyroid hormones have profound effects on the cardiovascular system. The mechanism of pacemaker activity in adult cardiac tissue is increasingly well documented. Although there is some controversy regarding the relative contributions of various ionic currents, it is becoming clear that a variety of ionic currents are responsible for pacemaker activity in various regions of the heart. Sun et al. [18] demonstrated through electrophysiological recordings that thyroid hormone increases the pacemaker rate of these myocytes by increasing the slope of spontaneous depolarization. Under voltage clamp conditions, Sun et al. focused on several ionic currents that may be involved in pacemaker activity in atrial cells, including ICa, If and INa/Ca. of the ionic currents studied, the electrogenic Na+−Ca2+ exchange current was the only candidate to be changed by T3 and which may have altered the slope of spontaneous depolarization. They suggest that, of the ionic currents studied, T3 might accelerate diastolic depolarization and pacemaker activity (at least in part) by an up-regulation of the Na+−Ca2+ exchanger.
Several ionic currents may contribute to pacemaker activity in this tissue, including If, the delayed rectifier potassium current (IK) [19–21], both the L-type (ICa,L) and T-type (ICa,T) calcium currents [20] and a background Na+ current (Ib) [19]. The electrogenic Na+−Ca2+ exchanger, triggered as a result of SR Ca2+ release, may also contribute to the initial phases of diastolic depolarization in the sinoatrial (SA) node [22]. Thus, the positive chronotropic action of thyroid hormones is potentially caused by modulation of any of these electrogenic ion conductances and/or by alterations in intracellular calcium homeostasis.
Early experimental studies of thyroid hormone effects on transmembrane potentials of sinoatrial node cells and atrial muscle cells showed an increased rate of diastolic depolarization and decreased duration of action potential in thyrotoxic animals, suggesting that conductance of K1 ions may be altered [23, 24].
Electrophysiology and Mechanism of Action of T3 on the Ventricles
Recent evidence has shown that thyroid hormones exert effects on the cardiovascular system that are not mediated by alterations in gene expression. Sakaguchi and co-workers [25] showed that T3 caused a shortening of the action potential duration in guinea pig ventricular myocytes by increasing whole cell inward rectifier potassium current (IK1).
In the rat ventricular myocyte, two primary depolarization-activated outward currents are important in regulating action potential duration: the Ca21-independent transient outward K1 current (Ito) and a slowly inactivating K1 current (IK) [26].
Although thyroid hormone has been shown to regulate the expression of numerous cardiac-specific genes, Sun et al. [27] show that T3 shortens the action potential duration (APD) in hypothyroid rats due at least in part to the increase of the delayed rectifier current IK. The Ito appears to be regulated by thyroid hormone at the transcriptional level, whereas the IK is regulated by a nongenomic mechanism of action.
Relation Between Thyroid Hormone and Adrenergic System
Many of the cardiovascular manifestations of thyroid hormone excess resemble those produced by sympathoadrenal stimulation. Since plasma catecholamine levels and turnover rates are not increased in hyperthyroidism [28], it has been argued that the effects of thyroid hormone result partly from increased responsiveness to catecholamines. This hypothesis is supported by studies that indicate that β-aderenergic receptor (βAR) number and sensitivity are increased in isolated hearts and cultured cells from experimental animals (most often the rat) treated with thyroid hormone [29, 30]. The influence of thyroid hormone on adrenergic responsiveness is particularly controversial in large animals and humans but Brian et al. [31] suggest that the cardiac mechanical effects of hyperthyroidism cannot be explained by enhanced sensitivity to catecholamines. Despite significant increases in basal heart rate and rates of left ventricular (LV) contraction and relaxation, the response to β-adrenergic agonists was not increased in hyperthyroid baboons. Increased basal indices of LV contraction and relaxation in this model are more clearly related to changes in myosin heavy chain isoform expression and the relative abundance of the sarcoplasmic reticulum (SR) calcium pumps (SR Ca2+-ATPase) and its phosphoprotein inhibitor, phospholamban, although other thyroid hormone–mediated effects, such as those reported for L-type calcium channels and Na+/K+-ATPase pumps cannot be excluded.
Thyroid hormone potentiates the effect of adrenergic system on heart. Catecholamine levels are either normal or decreased in thyrotoxicosis. Facilitation of action of catecholamines is by increasing tissue sensitivity by increased transcription of beta adrenergic receptors and structural similarity to catecholamines. Hyperthyroidism is associated with reduced vagal activity and reduced heart rate variability which can persist despite restoration of euthyroidism [32]. Ojamaa et al. [33] indicate that an analysis confined to the changes in 13-adrenergic receptor expression is insufficient to ascertain the role of catecholamines as mediators of thyroid hormone--dependent effects on cardiac autonomic responsiveness. It is important to consider all three components, the β3-adrenergic receptor, G-coupled protein, and catalytic subunit expression, in assessing adrenergic responsiveness of target tissues.
Mechanism Underlying the Effect of Thyroid Hormone (TH) on the Arrhythmogenesis
Thyroid hormone has been shown to have several cardiovascular effects, and hyperthyroidism has been known to be an important factor in the etiology of atria and ventricles arrhythmias [5]. In fact, there are always three main ingredients required for the production of a clinical arrhythmia: (1). the arrhythmogenic substrate; (2). the trigger factor; (3). the modulation factors of which the most common is the autonomic nervous system [34]. The cardiovascular manifestations of thyroid dysfunction is due to three potential mechanisms by which thyroid hormones might exert their cardiovascular actions by direct effects at the cellular level, by interacting with the sympathetic nervous system, through alterations of the peripheral circulation and energy metabolism [5]. Thyroid hormones have been shown to alter cardiac excitability, which may lead to arrhythmias [8].
Effects of Thyroid Hormones Excess on the Atrias
Hyperthyroidism has been known to be an important factor in the etiology of paroxysmal atrial fibrillation (AF) [5]. The pathogenesis of AF in these patients is postulated to result from shortening of the action potential (AP) duration in the atrial myocardium from excess thyroid hormone facilitating formation of multiple reentry circuits [35, 36]. Graves’ disease is one of the most common causes of hyperthyroidism. The prevalence of AF in patients with Graves’ disease, as in all other forms of hyperthyroidism, increases with age [36]. Shortening of the AP duration also decreases the refractoriness of cardiomyocytes, which may facilitate the maintenance of multiple reentrant circuits in heart. Using voltage clamp methods, several ionic currents have been investigated in cardiomyocytes. Calcium currents and delayed rectified potassium currents of ventricular cardiomyocytes were increased in hyperthyroidism [37]. Moreover, transient outward potassium currents and inward rectified currents have also been demonstrated to be increased in hyperthyroid ventricular cardiomyocytes [36].
Pulmonary veins (PVs) have been demonstrated to be important sources of ectopic beats with the initiation of paroxysmal AF or the foci of ectopic atrial tachycardia and focal AF [38]. Previous studies have demonstrated that PVs have pacemaker cells in several species [39]. Thyroid hormone changes the electrophysiological activity of the Pulmonary vein cardiomyocytes. Increased automaticity and enhanced triggered activity may increase the arrhythmogenic activity of PVs in hyperthyroidism [36]. Chen et al. suggest in their study that the electrophysiological features of paroxysmal AF associated with hyperthyroidism are essentially different from those of lone paroxysmal AF. In patients with paroxysmal AF and hyperthyroidism, a shortening of the refractory period in association with a facilitation of the atrial conduction delay could be expected to increase the propensity for AF, and a pre-existent arrhythmogenic substrate might not be essential to the genesis of AF. These findings suggest that the agents that prolong the atrial effective refractory period are effective against AF in patients with hyperthyroidism [40].
Effects of Thyroid Hormones Excess on the Ventricles
The onset of tachycardia or ventricular fibrillation (VF) has been reported within a thyrotoxic storm [41]. The presentation of these arrhythmias in the initial phase of the disease is much less common, and only a few isolated cases are described in the scientific literature. The majority [42, 43] occur in the context of thyrotoxic periodic paralysis with severe hypokalemia [44]. There has been an occasional patient in whom the ventricular arrhythmia were related to coronary spasm [45].
Nevertheless, the shortening of the Q–T interval and the effect of TH on the autonomic nervous system may affect ventricular arrhythmogenesis [46]. TH interacts with the sympathetic nervous system by altering responsiveness to sympathetic stimulation presumably by modulating adrenergic receptor function and/or density [5]. The density of myocardial adrenergic binding sites has been shown to be enhanced by chronic as well as acute treatment with thyroid hormone in hypothyroidism [47]. Thyroid hormone, in addition, induces a rate-dependent lengthening of the Purkinje fiber action potential while ventricular action potential shortens [48]. Consequently, these differences can enhance dispersion of myocardial repolarization and facilitate re-entrant arrhythmias including ventricular fibrillation (VF) [49]. It should also be noted that hyperthyroidism may affect myocardial electrical stability [50] due to increased excitability linked to triggered activity [51] resulting in ventricular premature beats (VPB) [52] that often initiate malignant arrhythmias [53].
On the other hand, it has been suggested that hypothyroidism might confer a protection against arrhythmias because they are rarely encountered in hypothyroid patients. Only atrioventricular blocks, sinus bradycardia, and rare episodes of “torsade de pointes” have been reported to be associated with clinical hypothyroidism [3]. In an animal model of ventricular fibrillation, hypothyroidism has been shown to increase the fibrillatory threshold of the ventricles [5].
In humans, the prolongation of the QTc interval encountered in hypothyroid patients is similar to that seen in euthyroid patients on class III antiarrhythmic agents [54]. In this regard, it has been suggested that the antiarrhythmic effect of amiodarone parallels its blocking effect on the peripheral thyroid hormone metabolism, suggesting that tissue hypothyroidism may have some antiarrhythmic properties [55]. However, this concept has been challenged by several observations. Tri-iodothyronine T3 administration to euthyroid patients treated with amiodarone for benign atrial or ventricular arrhythmias does not increase the frequency of arrhythmias [52]. In patients with hypothyroidism, thyroid replacement therapy did not increase significantly the frequency of benign atrial or ventricular premature beats [56].
Many patients with overt hypothyroidism have Q–T interval lengthening, which reflects the prolonged ventricular action potential due to electrical remodeling [57]. It renders the heart prone to ventricular arrhythmias, such as potentially lethal polymorphic tachycardia “Torsade de Pointes” [58]. The incidence of arrhythmia precedes the occurrence of early after depolarization (EAD) usually triggered in the setting of hypokalemia. EAD-induced triggered responses are traditionally thought to be involved in the generation of ventricular arrhythmias under long Q–T conditions. Dispersion of ventricular refractoriness resulting from heterogeneous myocardial structural remodeling [59] predisposes to Q–T dispersion and consequently to ventricular arrhythmias particularly in patients with subclinical hypothyroidism that are treated with L-thyroxine [60]. Furthermore, in hypothyroidism an atrioventricular block of different degrees may occur [61]. Nevertheless, the VF incidence is reduced in hypothyroidism [62] depression of TH levels seems to be beneficial in patients with angina and acute myocardial infarction [53, 63].
Finally, thyroid hormones may trigger arrhythmias mostly at the level of the atria, and there is some evidence that tissue hypothyroidism may increase the fibrillation threshold of the ventricles. However, there are no clear data in humans indicating that hypothyroidism confers a protection against ventricular or atrial arrhythmias [5].
Supraventricular Arrhythmia
Atrial Arrhythmia
The atrial arrhythmia includes AF, atrial flutter and atrial tachycardia. Atrial fibrillation is the most frequent atrial arrhythmia. Hyperthyroidism has been associated with atrial tachyarrhythmias [64] and with sustained AF occurring in 20–30 % of patients even after return to the euthyroid state [64]. The risk of atrial fibrillation or flutter in hyperthyroidism was higher in men than in women, and the risk of atrial fibrillation in hyperthyroidism increased by increasing age during the age range of 20–89 years. The presence of ischemic heart disease, congestive heart failure, and heart valve disease was also associated with an increased risk of atrial fibrillation [65].
We could not differentiate atrial fibrillation from atrial flutter because in the literature and a lot of articles didn’t differentiate the two arrhythmias. In fact, they had the same ICD-10 code [66]. In other hand, there is a low proportion of patients with pure atrial flutter these represent approximately 5 % of the recorded cases [37–39, 67].
Hyperthyroidism
Thyrotoxicosis is a common disorder with a prevalence of 3 % in females and 0.3 % in males in iodine-replete areas such as the United Kingdom and the United States [68]. It is known to induce many cardiovascular effects such as sinus tachycardia, systolic hypertension, changes in ventricular systolic and diastolic function, and predisposition to dysrhythmias, especially AF [6]. The prevalence of AF in patients with hyperthyroidism ranges between 2 and 20 %, and the risk is approximately sixfold greater than normal population [69].
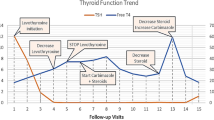
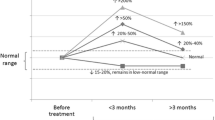
The first step in the management of atrial fibrillation, despite the cause, is to control the ventricular response. β-blockers are one of the mainstays of treatment of AF in the setting of hyperthyroidism [69]. Selective or non-selective β-blockers can provide rapid symptom relief by reducing the ventricular rate, but these agents are unlikely to convert AF to sinus rhythm as they have little effect on hyperthyroidism, the primary cause of cardiac stimulation and AF. Therefore, restoration of euthyroidism by radioiodine or anti-thyroid drugs is the ultimate treatment of choice for long-term AF management in this setting. Successful treatment of hyperthyroidism with either radioiodine or thioureas is associated with a reversion to sinus rhythm in a majority of patients within 2–3 months [70]. Zhen-Hu Zhou et al. demonstrated in their study that after euthyroidism or hypothyroidism states were achieved, very frequent paroxysmal AF were observed and no recurrence was noted at the end of the follow-up. Persistent AF, however, spontaneously converted to sinus rhythm in only 40 % of the patients, but persistent AF continued in the remaining patients. Further analysis showed that older age (>55 years) and a long duration of hyperthyroidism of more than 5 years, and a long duration of pre-treatment AF are independent predictors for continued AF following the successful treatment of hyperthyroidism [71]. In other hand, Xiao et al. suggested that Blockade of angiotensin II could improve abnormal atrial electrophysiological properties and further reduce AF vulnerability by extenuating ion channel, gap junction and structural remodeling in experimental thyrotoxic rabbits [72].
The management strategies for persistent AF following hyperthyroidism treatment are not entirely clear. The current recommendations are that after the patient has been rendered chemically euthyroid, electrical or pharmacological cardioversion should be attempted [69].
Elective cardioversion for persistent AF is highly effective and sinus rhythm maintenance rates are greater than 50 % over 10 years. The addition of anti-arrhythmic drugs may also help to maintain sinus rhythm in these patients [73]. Bepridil is as beneficial treatment to convert AF for the patients with hyperthyroidism-induced persistent AF as it is for the patients with AF due to other causes [74]. Yo Kunii et al. showed that bepridil converted hyperthyroidism-induced persistent AF to sinus rhythm as much as it does after a long duration of AF due to other causes, and the sinus rhythm maintenance rate was very high. Bepridil is very beneficial medicine for the patient of hyperthyroidism-induced AF, however, it should be used with caution, and frequent or continuous ECG monitoring is necessary, to avoid serious side effects [74].
Subclinical Hyperthyroidism and Atrial Fibrillation
Sub clinical hyperthyroidism is defined as low serum thyrotropin concentration in an asymptomatic patient with normal serum T3 and T4 concentration. It has a prevalence of 0.5–3.9 % in adults [75]. The prevalence of atrial fibrillation in patients with low serum thyrotropin concentration was 13.3 % compared to 2.3 % in persons with normal values. The relative risk of atrial fibrillation in subjects with low serum thyrotropin and normal free T3, T4 values compared to those with normal serum thyrotropin was 5.2 [32]. Osturk et al. [76] showed that left atrial mechanical and electromechanical function in subclinical thyroid disorders was impaired. TSH was an independent determinant of interatrial delay. Prolonged atrial electromechanical coupling time and impaired mechanical atrial functions may be related to the increased incidence of arrhythmias.
Hypothyroidism and Subclinical Hypothyroidism
Hypothyroidism is associated with cardiovascular risk factors, subclinical cardiovascular disease, and overt cardiovascular disease, all of which predispose to AF. Subclinical hypothyroidism was common. In fact, the prevalence was 4–8 % in people older than 60 years of age. Subclinical hypothyroidism has some clinical consequences like an increase in the prevalence of atria fibrillation [77]. However, Klemperer et al. [78] found that perioperative T3 administration in Cardiopulmonary bypass in euthyroid patients decreased the incidence and need for treatment of postoperative atrial fibrillation. This finding still unexplained. Kim et al. [79] did not identify a significant association between hypothyroidism and 10-year risk of incident AF in a community-based study from the Framingham heart study.
Euthyroid Range in Older Adults
Cappola et al. [80] examined the relationship between thyroid function testing within the euthyroid range and outcomes encompassing the cardiovascular system in cohort of community-dwelling individuals aged 65 years and older. They found increased risk of atrial Fibrillation at higher concentrations of FT4 and they suggested that there is no optimal set of thyroid function tests within current reference ranges to reflect the euthyroid ideal in the age group. Cappola et al. [80] proposed that the optimal TSH may need to be higher in older people than the currently defined references ranges.
Should We Anticoagulate and Attempt Cardioversion in Those with AF?
Anticoagulation of patients with hyperthyroidism and AF is controversial [81] as the risk for systemic thromboembolic events in the setting of thyrotoxicosis is not well defined [82], and anticoagulation drugs such as warfarin, are associated with a significant risk of bleeding complications and other side effects [82]. There are beliefs that in patients with hyperthyroidism it is advancing age rather than the presence of AF that is the main risk factor [81] for a thromboembolic event, and in younger patients without organic heart disease, hypertension, or other independent risk factors for embolization, the benefits of anticoagulation may actually be outweighed by the risks [69]. In our knowledge, no interaction between thyroid function and unfractionated heparin (UFH) has been documented, however Badawi [83] reported an interaction between thyroid function and UFH. Nakazawa et al. [84] suggested that spontaneous reversion of atrial fibrillation to sinus rhythm is highly unlikely if the duration of atrial fibrillation before the euthyroid state is achieved exceeds 13 months, or if it is still present after the patient has been in a euthyroid state for 4 months, Cardioversion should be performed at about the 16th week after the euthyroid state is achieved.
Arrhythmia and Amiodarone-Induced Hyperthyroidism
Amiodarone is the most commonly used antiarrhythmic drug worldwide [85]. It is effective in the treatment of both supraventricular and ventricular tachyarrhythmias and has the added advantage of being well tolerated in patients with both normal and impaired left ventricular systolic function [85]. The majority of patients (>70 %) on amiodarone will remain euthyroid. However, treatment may lead to either amiodarone-induced hypothyroidism (AIH) or amiodarone-induced thyrotoxicosis (AIT), with AIH more common in iodine-sufficient populations and AIT in iodine-deficient populations [86].
Amiodarone-induced thyroid dysfunction occurs in 15–20 % of amiodarone-treated patients [87]. Amiodarone-induced hypothyroidism (AIH) does not pose relevant problems, is easily controlled by L-thyroxine replacement, and does not require amiodarone withdrawal. Most frequently, AIH develops in patients with chronic autoimmune thyroiditis. Amiodarone-induced thyrotoxicosis (AIT) is most frequently due to destructive thyroiditis (type 2 AIT) causing release of thyroid hormones from the damaged, but otherwise substantially normal gland. Less frequently AIT is a form of hyperthyroidism (type 1 AIT) caused by the iodine load in a diseased gland (nodular goiter, Graves’ disease). A clear-cut differentiation between the two main forms is not always possible, despite recent diagnostic advances. As a matter of fact, mixed or indefinite forms do exist, contributed to by both thyroid damage and increased thyroid hormone synthesis. Treatment of type 1 (and mixed forms) AIT is based on the use of thionamides, a short course of potassium perchlorate and, if treatment is not rapidly effective, oral glucocorticoids. Glucocorticoids are the first-line treatment for type 2 AIT. Amiodarone should be discontinued, if feasible from a cardiac standpoint. Continuation of amiodarone has recently been associated with a delayed restoration of euthyroidism and a higher chance of recurrence after glucocorticoid withdrawal. Whether amiodarone treatment can be safely reinstituted after restoration of euthyroidism is still unknown. In rare cases of AIT resistance to standard treatments, or when a rapid restoration of euthyroidism is advisable, total thyroidectomy represents a valid alternative. Radioiodine treatment is usually not feasible due to the low thyroidal iodine uptake [4]. Dronedarone was approved in 2009 for the treatment of patients with atrial fibrillation. Like amiodarone, dronedarone is a benzofuran derivative with similar electrophysiologic properties. In contrast to amiodarone, however, dronedarone is structurally devoid of iodine and has a notably shorter half-life. Dronedarone proved to be associated with significantly fewer adverse effects than amiodarone, making it a more attractive choice for patients with atrial fibrillation or flutter, who are at risk of developing amiodarone-induced thyroid dysfunction [88].
Other Supraventricular Arrhythmia
Biondi et al. [46] reported the possibility that thyroid hormones may also induce other kinds of supraventricular arrhythmias not frequently described in hyperthyroid patients, such as reentrant atrioventricular (A-V) nodal tachycardia. This report also showed that reentrant A-V nodal tachycardia may be triggered by thyroid hormone in predisposed subjects. The reentrant A-V nodal tachycardia is a relatively common cause of regular, narrow QRS complex tachycardia, and it is more prevalent in women than in men with a ratio of 7:1 respectively [89]. Epidemiologically, it must be emphasized that both thyroid disease and reentrant A-V nodal tachycardia are highly prevalent in females.
In patients with reentrant A-V nodal tachycardia, at least two functionally distinct A-V nodal conduction patterns are demonstrable [90, 91]. One pathway, referred to as the fast pathway, is characterized by rapid conduction velocity and relatively long refractoriness. The second or slow pathway typically shows slow conduction velocity and short refractoriness. During sinus rhythm, the electric impulse is expected to reach the His bundle and the ventricle preferentially over the faster-conducting pathway with the frequent evidence of a short P-R interval. A-V nodal reentry of the common type (slow-fast) is typically initiated by an atrial premature beat that conducts down only through the slow pathway because of functional block of the fast pathway, and reenters back through the fast pathway because of recovery of its excitability. Conceivably, thyroid hormones might increase the occurrence of reentrant A-V nodal tachycardia in predisposed subjects because of the enhancement of atrial excitability, with consequent increase of the number of atrial premature beats and the shortening of the refractory period of the conducting tissues. Thus, reentrant A-V nodal tachycardia might be triggered in patients in whom L-T4 is exogenously administered to lower TSH [46].
Abbasoglu et al. [92] reported a case of Neonatal thyrotoxicosis with concurrent supraventricular tachycardia caused by the transplacental passage of thyroid stimulating immunoglobulins from mothers with Graves’ disease. The heart rate was between 260 and 300 beats/min. Matthew et al. [93] described a case of 43 year old woman who presented in supraventricular tachycardia and acute pulmonary edema and died without any evident cause of mortality. At autopsy the significant positive macroscopic findings were confined to the lungs (acute pulmonary edema) and thyroid (diffusely enlarged). Histology revealed features typical of Graves’ disease while post mortem thyroid function tests supported a diagnosis of thyrotoxic crisis in the setting of undiagnosed Graves’ disease.
Ventricular Arrhythmia
In contrast to high incidence of atrial arrhythmias in the hyperthyroid status, the ventricular arrhythmias are uncommon and found with a frequency similar to that in the normal population [3, 6, 89, 90]. It is likely because VF is exceptional in those with elevated TH without cardiomyopathy [41, 94, 95]. Thus, the occurrence of ventricular arrhythmias in thyrotoxic subjects during and after antithyroid therapy is rare [3, 6]. However, VF may occur in those with associated heart disease or heart failure of various etiology [5, 26].
Hyperthyroidism
Ventricular tachycardia (VT) is one of the major causes of death in patients with structural heart disease. Electrical storm (ES) is defined as hemodynamically significant VT occurring at least three times over a 24-h period and requiring delivery of direct current shocks [96]. Determining the etiology of extrastimulus ES is quite challenging and requires detailed evaluation of the patient. The etiology of ES varies and includes enhanced sympathetic tone, myocardial ischemia, electrolyte imbalance, endocrine disorders (pheochromocytoma, thyrotoxycosis, etc.), genetic abnormalities (Brugada syndrome, long-QT syndrome, arrhythmogenic right ventricular dysplasia, etc.). Tachycardia during ES might be monomorphic or polymorphic. Polymorphic ES without QT prolongation is frequently associated with myocardial ischemia [97].
Subclinical Hyperthyroidism
Subclinical hyperthyroidism exerts many significant effects on the cardiovascular system; it is usually associated with a higher heart rate and a higher risk of supraventricular arrhythmias, and with an increased left ventricular mass, often accompanied by an impaired diastolic function and sometimes by a reduced systolic performance on effort and decreased exercise tolerance. It is well known that these abnormalities usually precede the onset of a more severe cardiovascular disease, thus potentially contributing to the increased cardiovascular morbidity and mortality observed in these patients [98]. To our knowledge, the literature has not reported ventricular arrhythmias caused by subclinical hyperthyroidism.
Hypothyroidism
It is well known that an excess or deficit of thyroid hormones affects the cardiovascular system. A typical ECG in hypothyroidism shows bradycardia, a low voltage of the QRS complexes, elongation of the QT and flattening or inverting of the T waves. However, less well known is the fact that hypothyroidism may be the cause of atrioventricular blocks and of acquired long QT syndrome (LQTS). Only few publications reported life-threatening by possibility of torsade de pointes (TdP) type tachycardia and ventricular fibrillation occurring in patients with prolonged QT syndrome in the course of hypothyroidism [99].
Profound hypothyroidism and decreased expression of tri-iodothyronine in the heart cells may cause a worsening of cardiac contractility, a decreasing heart rate and a slowing down of the conduction of electrical stimuli in the heart muscle. This may be the reason for bradycardia and elongation of the QT interval and, in consequence, life-threatening arrhythmias may occur, for example TdP-type tachycardia. Decreased tri-iodothyronine expression and electrolyte disorders such as moderate hypokalaemia and hypocalcaemia probably prompted LQTS and shock in this case [99]. It is important to note that amiodarone was not sufficiently effective to prevent recurrent ventricular arrhythmias. Few publications reported that lidocaine or bretylium tosylate may interrupt this kind of paroxysmal tachycardia and endocavitary electrode stimulation [62].
Hypothyroidism may be the cause of life-threatening arrhythmias secondary to acquired long QT syndrome. Ventricular electrostimulation was a life-saving procedure in this case of prolonged QT syndrome. The use of temporary ventricular electrostimulation protected the patient against dangerous ventricular arrhythmias, while balancing the deficiency of thyroid hormones and electrolytes [31].
Subclinical Hypothyroidism
Subclinical hypothyroidism is a common disorder characterized by elevated serum thyroid-stimulating hormone, normal free thyroxine and free triiodothyronine levels. Its prevalence reportedly ranges between 1.3 and 17.5 %, depending on age, gender and the amount of iodine exposure [100]. Bakiner et al. detected prolonged QT intervals and increased QTc among their subclinical hypothyroid cases. The prolongation remained significant for the whole group, as well as within the subgroups. There was a positive correlation between TSH levels and QTc. Return of serum TSH levels from 110 mIU/l to values within the reference range resulted in normalization of QTc. Such an outcome for patients with TSH between 5 and 10 mIU/l remains to be investigated [101]. TSH concentration has a role in ventricular inhomogeneity and, therefore, subclinical hypothyroidism may predispose to ventricular arrhythmias [60].
Conclusion
Thyroid hormones may trigger arrhythmias mostly at the level of the atria. The incidence of cardiac arrhythmias is in relation to the altered thyroid status. It appears that hypothyroidism is mostly associated with reduced probability of cardiac arrhythmias unlike hyperthyroidism that increases a risk notably for atrial and to a lesser extent ventricular arrhythmias that occur particularly in a cardiomyopathic heart. The long-term arrhythmia depends of the precocity of thyroid disease treatment and cardiomyopathic heart.
Abbreviations
- AF:
-
Atrial fibrillation
- AIT:
-
Amiodarone-induced thyrotoxicosis
- AP:
-
Action potential
- EAD:
-
Early afterdepolarization
- ECG:
-
Electrocardiogram
- FT4:
-
Free thyroxine
- IK:
-
Delayed rectifier potassium current
- LQTS:
-
Long QT syndrome
- PLB:
-
Phospholamban
- PVs:
-
Pulmonary veins
- SERCA2:
-
Calcium-activated adenosine triphosphatase
- SR:
-
Sarcoplasmic reticulum
- SR Ca2+-ATPase:
-
Sarcoplasmic reticulum calcium pumps
- T3:
-
Triiodothyronine
- TdP:
-
Torsade de pointes
- TH:
-
Thyroid hormone
- TSH:
-
Thyroid stimuling hormone
- UFH:
-
Unfractionated heparin
- VF:
-
Ventricular fibrillation
- VPB:
-
Ventricular premature beats
- VT:
-
Ventricular tachycardia
References
Sawin CT, Geller A, Wolf PA, Belanger AJ, Baker E, Bacharach P, et al. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med. 1994;331(19):1249–52.
Golf S, Løvstad R, Hansson V. Beta-adrenoceptor density and relative number of beta-adrenoceptor subtypes in biopsies from human right atrial, left ventricular, and right ventricular myocard. Cardiovasc Res. 1985;19(10):636–41.
Von Olshausen K, Bischoff S, Kahaly G, Mohr-Kahaly S, Erbel R, Beyer J, et al. Cardiac arrhythmias and heart rate in hyperthyroidism. Am J Cardiol. 1989;63(13):930–3.
Roffi M, Cattaneo F, Brandle M. Thyrotoxicosis and the cardiovascular system. Minerva Endocrinol. 2005;30(2):47–58.
Polikar R, Burger AG, Scherrer U, Nicod P. The thyroid and the heart. Circulation. 1993;87(5):1435–41.
Osman F, Gammage MD, Sheppard MC, Franklyn JA. Clinical review 142: cardiac dysrhythmias and thyroid dysfunction: the hidden menace? J Clin Endocrinol Metab. 2002;87(3):963–7.
Glass CK, Holloway JM. Regulation of gene expression by the thyroid hormone receptor. Biochim Biophys Acta. 1990;1032(2–3):157–76.
Brent GA. The molecular basis of thyroid hormone action. N Engl J Med. 1994;331(13):847–53.
Woeber KA. Thyrotoxicosis and the heart. N Engl J Med. 1992;327(2):94–8.
Dillmann WH. Biochemical basis of thyroid hormone action in the heart. Am J Med. 1990;88(6):626–30.
Klein I, Ojamaa K, Samarel AM, Welikson R, Hong C. Hemodynamic regulation of myosin heavy chain gene expression. Studies in the transplanted rat heart. J Clin Invest. 1992;89(1):68–73.
Danzi S, Klein S, Klein I. Differential regulation of the myosin heavy chain genes alpha and beta in rat atria and ventricles: role of antisense RNA. Thyroid Off J Am Thyroid Assoc. 2008;18(7):761–8.
Ojamaa K, Kenessey A, Klein I. Thyroid hormone regulation of phospholamban phosphorylation in the rat heart. Endocrinology. 2000;141(6):2139–44.
Liu B, Huang F, Gick G. Regulation of Na, K-ATPase beta 1 mRNA content by thyroid hormone in neonatal rat cardiac myocytes. Cell Mol Biol Res. 1993;39(3):221–9.
Ojamaa K, Sabet A, Kenessey A, Shenoy R, Klein I. Regulation of rat cardiac Kv1.5 gene expression by thyroid hormone is rapid and chamber specific. Endocrinology. 1999;140(7):3170–6.
Davis PJ, Davis FB, Lin H-Y, Mousa SA, Zhou M, Luidens MK. Translational implications of nongenomic actions of thyroid hormone initiated at its integrin receptor. Am J Physiol Endocrinol Metab. 2009;297(6):E1238–46.
Bonow RO, Mann DL, Zipes DP, Libby P. Braunwald’s heart disease: a textbook of cardiovascular medicine. Philadelphia: Elsevier Health Sciences; 2011. 11033 p.
Sun ZQ, Ojamaa K, Nakamura TY, Artman M, Klein I, Coetzee WA. Thyroid hormone increases pacemaker activity in rat neonatal atrial myocytes. J Mol Cell Cardiol. 2001;33(4):811–24.
Hagiwara N, Irisawa H, Kasanuki H, Hosoda S. Background current in sino-atrial node cells of the rabbit heart. J Physiol. 1992;448:53–72.
Hagiwara N, Irisawa H, Kameyama M. Contribution of two types of calcium currents to the pacemaker potentials of rabbit sino-atrial node cells. J Physiol. 1988;395:233–53.
Kodama I, Boyett MR, Nikmaram MR, Yamamoto M, Honjo H, Niwa R. Regional differences in effects of E-4031 within the sinoatrial node. Am J Physiol. 1999;276(3 Pt 2):H793–802.
Hüser J, Blatter LA, Lipsius SL. Intracellular Ca2+ release contributes to automaticity in cat atrial pacemaker cells. J Physiol. 2000;524(Pt 2):415–22.
Kiehn J, Karle C, Thomas D, Yao X, Brachmann J, Kübler W. HERG potassium channel activation is shifted by phorbol esters via protein kinase A-dependent pathways. J Biol Chem. 1998;273(39):25285–91.
Johnson PN, Freedberg AS, Marshall JM. Action of thyroid hormone on the transmembrane potentials from sinoatrial node cells and atrial muscle cells in isolated atria of rabbits. Cardiology. 1973;58(5):273–89.
Sakaguchi Y, Cui G, Sen L. Acute effects of thyroid hormone on inward rectifier potassium channel currents in guinea pig ventricular myocytes. Endocrinology. 1996;137(11):4744–51.
Apkon M, Nerbonne JM. Characterization of two distinct depolarization-activated K+ currents in isolated adult rat ventricular myocytes. J Gen Physiol. 1991;97(5):973–1011.
Sun ZQ, Ojamaa K, Coetzee WA, Artman M, Klein I. Effects of thyroid hormone on action potential and repolarizing currents in rat ventricular myocytes. Am J Physiol Endocrinol Metab. 2000;278(2):E302–7.
Levey GS, Klein I. Catecholamine-thyroid hormone interactions and the cardiovascular manifestations of hyperthyroidism. Am J Med. 1990;88(6):642–6.
Williams LT, Lefkowitz RJ, Watanabe AM, Hathaway DR, Besch Jr HR. Thyroid hormone regulation of beta-adrenergic receptor number. J Biol Chem. 1977;252(8):2787–9.
Morkin E, Flink IL, Goldman S. Biochemical and physiologic effects of thyroid hormone on cardiac performance. Prog Cardiovasc Dis. 1983;25(5):435–64.
Hoit BD, Khoury SF, Shao Y, Gabel M, Liggett SB, Walsh RA. Effects of thyroid hormone on cardiac beta-adrenergic responsiveness in conscious baboons. Circulation. 1997;96(2):592–8.
Jayaprasad N, Francis J. Atrial fibrillation and hyperthyroidism. Indian Pacing Electr J. 2005;5(4):305–11.
Ojamaa K, Klein I, Sabet A, Steinberg SF. Changes in adenylyl cyclase isoforms as a mechanism for thyroid hormone modulation of cardiac beta-adrenergic receptor responsiveness. Metabolism. 2000;49(2):275–9.
Farre J. Philippe Coumel: a founding father of modern arrhythmology. Europace. 2004;6(5):464–5.
Freedberg AS, Papp JG, Williams EM. The effect of altered thyroid state on atrial intracellular potentials. J Physiol. 1970;207(2):357–69.
Chen Y-C, Chen S-A, Chen Y-J, Chang M-S, Chan P, Lin C-I. Effects of thyroid hormone on the arrhythmogenic activity of pulmonary vein cardiomyocytes. J Am Coll Cardiol. 2002;39(2):366–72.
Rubinstein I, Binah O. Thyroid hormone modulates membrane currents in guinea-pig ventricular myocytes. Naunyn Schmiedebergs Arch Pharmacol. 1989;340(6):705–11.
Haïssaguerre M, Jaïs P, Shah DC, Takahashi A, Hocini M, Quiniou G, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339(10):659–66.
Chen YJ, Chen SA, Chen YC, Yeh HI, Chan P, Chang MS, et al. Effects of rapid atrial pacing on the arrhythmogenic activity of single cardiomyocytes from pulmonary veins: implication in initiation of atrial fibrillation. Circulation. 2001;104(23):2849–54.
Komiya N, Isomoto S, Nakao K, Hayano M, Yano K. Electrophysiological abnormalities of the atrial muscle in patients with paroxysmal atrial fibrillation associated with hyperthyroidism. Clin Endocrinol (Oxf). 2002;56(1):39–44.
Jao YTFN, Chen Y, Lee W-H, Tai F-T. Thyroid storm and ventricular tachycardia. South Med J. 2004;97(6):604–7.
Boccalandro C, López-Penabad L, Boccalandro F, Lavis V. Ventricular fibrillation in a young Asian man. Lancet. 2003;361(9367):1432.
Fisher J. Thyrotoxic periodic paralysis with ventricular fibrillation. Arch Intern Med. 1982;142(7):1362–4.
Muñoz-Camacho JF, Sagristá-Sauleda J. Malignant ventricular arrhythmias as the initial manifestation of hyperthyroidism. Rev Esp Cardiol Engl Ed. 2007;60(4):449–50.
Wei JY, Genecin A, Greene HL, Achuff SC. Coronary spasm with ventricular fibrillation during thyrotoxicosis: response to attaining euthyroid state. Am J Cardiol. 1979;43(2):335–9.
Biondi B, Fazio S, Coltorti F, Palmieri EA, Carella C, Lombardi G, et al. Clinical case seminar: reentrant atrioventricular nodal tachycardia induced by levothyroxine. J Clin Endocrinol Metab. 1998;83(8):2643–5.
Gross G, Lues I. Thyroid-dependent alterations of myocardial adrenoceptors and adrenoceptor-mediated responses in the rat. Naunyn Schmiedebergs Arch Pharmacol. 1985;329(4):427–39.
Jaeger JM, Houser SR, Freeman AR, Spann Jr JF. Effect of thyroid hormone on canine cardiac Purkinje fiber transmembrane potential. Am J Physiol. 1981;240(6):H934–40.
Qu Z, Weiss JN. Dynamics and cardiac arrhythmias. J Cardiovasc Electrophysiol. 2006;17(9):1042–9.
Meo SD, de Martino RP, Piro MC, De Leo T. Electrophysiological properties of the hyperthyroid rat heart. Arch Int Physiol Biochim Biophys. 1994;102(2):153–9.
Buscemi S, Verga S, Cottone S, Andronico G, D’Orio L, Mannino V, et al. Favorable clinical heart and bone effects of anti-thyroid drug therapy in endogenous subclinical hyperthyroidism. J Endocrinol Invest. 2007;30(3):230–5.
Polikar R, Goy JJ, Schlapfer J, Lemarchand-Beraud T, Biollaz J, Magnenat P, et al. Effect of oral triiodothyronine during amiodarone treatment for ventricular premature complexes. Am J Cardiol. 1986;58(10):987–91.
Tribulova N, Knezl V, Shainberg A, Seki S, Soukup T. Thyroid hormones and cardiac arrhythmias. Vascul Pharmacol. 2010;52(3–4):102–12.
Surawicz B, Mangiardi ML. Electrocardiogram in endocrine and metabolic disorders. Cardiovasc Clin. 1977;8(3):243–66.
Nademanee K, Singh BN, Hendrickson JA, Reed AW, Melmed S, Hershman J. Pharmacokinetic significance of serum reverse T3 levels during amiodarone treatment: a potential method for monitoring chronic drug therapy. Circulation. 1982;66(1):202–11.
Polikar R, Feld GK, Dittrich HC, Smith J, Nicod P. Effect of thyroid replacement therapy on the frequency of benign atrial and ventricular arrhythmias. J Am Coll Cardiol. 1989;14(4):999–1002.
Di Meo S, Venditti P, De Leo T. Effect of iodothyronines on electrophysiological properties of rat papillary muscle fibres. Horm Metab Res. 1997;29(5):225–30.
Schenck JB, Rizvi AA, Lin T. Severe primary hypothyroidism manifesting with torsades de pointes. Am J Med Sci. 2006;331(3):154–6.
Fredlund BO, Olsson SB. Long QT interval and ventricular tachycardia of « torsade de pointe » type in hypothyroidism. Acta Med Scand. 1983;213(3):231–5.
Unal O, Erturk E, Ozkan H, Kiyici S, Guclu M, Ersoy C, et al. Effect of levothyroxine treatment on QT dispersion in patients with subclinical hypothyroidism. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2007;13(7):711–5.
LEE JK, LEWIS JA. Myxoedema with complete A-V block and Adams-Stokes disease abolished with thyroid medication. Br Heart J. 1962;24:253–6.
Chess-Williams R, Coker SJ. Ventricular fibrillation is reduced in hypothyroid rats with enhanced myocardial alpha-adrenoceptor responsiveness. Br J Pharmacol. 1989;98(1):95–100.
Friberg L, Werner S, Eggertsen G, Ahnve S. Rapid down-regulation of thyroid hormones in acute myocardial infarction: is it cardioprotective in patients with angina? Arch Intern Med. 2002;162(12):1388–94.
Epstein FH, Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system. N Engl J Med. 2001;344(7):501–9.
Frost L, Vestergaard P, Mosekilde L. Hyperthyroidism and risk of atrial fibrillation or flutter: a population-based study. Arch Intern Med. 2004;164(15):1675–8.
Frost L, Vestergaard P. Alcohol and risk of atrial fibrillation or flutter: a cohort study. Arch Intern Med. 2004;164(18):1993–8.
Frost L, Vestergaard P, Mosekilde L, Mortensen LS. Trends in incidence and mortality in the hospital diagnosis of atrial fibrillation or flutter in Denmark, 1980–1999. Int J Cardiol. 2005;103(1):78–84.
Tunbridge WM, Evered DC, Hall R, Appleton D, Brewis M, Clark F, et al. The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol (Oxf). 1977;7(6):481–93.
Klein I, Danzi S. Thyroid disease and the heart. Circulation. 2007;116(15):1725–35.
Nakazawa H, Lythall DA, Noh J, Ishikawa N, Sugino K, Ito K, et al. Is there a place for the late cardioversion of atrial fibrillation? A long-term follow-up study of patients with post-thyrotoxic atrial fibrillation. Eur Heart J. 2000;21(4):327–33.
Zhou Z-H, Ma L-L, Wang L-X. Risk factors for persistent atrial fibrillation following successful hyperthyroidism treatment with radioiodine therapy. Intern Med Tokyo Jpn. 2011;50(24):2947–51.
Xiao P, Gao C, Fan J, Du H, Long Y, Yin Y. Blockade of angiotensin II improves hyperthyroid induced abnormal atrial electrophysiological properties. Regul Pept. 2011;169(1–3):31–8.
Shimizu T, Koide S, Noh JY, Sugino K, Ito K, Nakazawa H. Hyperthyroidism and the management of atrial fibrillation. Thyroid Off J Am Thyroid Assoc. 2002;12(6):489–93.
Kunii Y, Uruno T, Matsumoto M, Mukasa K, Noh J, Ito K, et al. Pharmacological conversion of atrial fibrillation in the patients of Graves’ disease. Tokai J Exp Clin Med. 2012;37(4):107–12.
Bagchi N, Brown TR, Parish RF. Thyroid dysfunction in adults over age 55 years. A study in an urban US community. Arch Intern Med. 1990;150(4):785–7.
Ozturk S, Dikbas O, Baltacı D, Ozyasar M, Erdem A, Ayhan SS, et al. Evaulation of atrial conduction abnormalities and left atrial mechanical functions in patients with subclinical thyroid disorders. Endokrynol Pol. 2012;63(4):286–93.
Sawin CT. Subclinical hypothyroidism in older persons. Clin Geriatr Med. 1995;11(2):231–8.
Klemperer JD, Klein IL, Ojamaa K, Helm RE, Gomez M, Isom OW, et al. Triiodothyronine therapy lowers the incidence of atrial fibrillation after cardiac operations. Ann Thorac Surg. 1996;61(5):1323–7.
Kim E-J, Lyass A, Wang N, Massaro JM, Fox CS, Benjamin EJ, et al. Relation of hypothyroidism and incident atrial fibrillation (from the Framingham Heart Study). Am Heart J. 2014;167(1):123–6.
Cappola AR, Arnold AM, Wulczyn K, Carlson M, Robbins J, Psaty BM. Thyroid function in the euthyroid range and adverse outcomes in older adults. J Clin Endocrinol Metab. 2015;100(3):1088–96.
Petersen P, Hansen JM. Stroke in thyrotoxicosis with atrial fibrillation. Stroke J Cereb Circ. 1988;19(1):15–8.
Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2011;57(11):e101–98.
Badawi O. Possible effect of thyroid function on anticoagulant response to unfractionated heparin. Pharmacotherapy. 2006;26(2):285–8.
Nakazawa HK, Sakurai K, Hamada N, Momotani N, Ito K. Management of atrial fibrillation in the post-thyrotoxic state. Am J Med. 1982;72(6):903–6.
Singh BN. Amiodarone as paradigm for developing new drugs for atrial fibrillation. J Cardiovasc Pharmacol. 2008;52(4):300–5.
Narayana SK, Woods DR, Boos CJ. Management of amiodarone-related thyroid problems. Ther Adv Endocrinol Metab. 2011;2(3):115–26.
Bogazzi F, Tomisti L, Bartalena L, Aghini-Lombardi F, Martino E. Amiodarone and the thyroid: a 2012 update. J Endocrinol Invest. 2012;35(3):340–8.
Cohen-Lehman J, Dahl P, Danzi S, Klein I. Effects of amiodarone therapy on thyroid function. Nat Rev Endocrinol. 2010;6(1):34–41.
Ganz LI, Friedman PL. Supraventricular tachycardia. N Engl J Med. 1995;332(3):162–73.
Denes P, Wu D, Dhingra RC, Chuquimia R, Rosen KM. Demonstration of dual A-V nodal pathways in patients with paroxysmal supraventricular tachycardia. Circulation. 1973;48(3):549–55.
Rosen KM, Mehta A, Miller RA. Demonstration of dual atrioventricular nodal pathways in man. Am J Cardiol. 1974;33(2):291–4.
Abbasoğlu A, Ecevit A, Tuğcu AU, Erdoğan L, Kınık ST, Tarcan A. Neonatal thyrotoxicosis with severe supraventricular tachycardia: case report and review of the literature. J Pediatr Endocrinol Metab. 2015;28(3–4):463–6.
Lynch MJ, Woodford NWF. Sudden unexpected death in the setting of undiagnosed Graves’ disease. Forensic Sci Med Pathol. 2014;10(3):452–6.
Colzani RM, Emdin M, Conforti F, Passino C, Scarlattini M, Iervasi G. Hyperthyroidism is associated with lengthening of ventricular repolarization. Clin Endocrinol (Oxf). 2001;55(1):27–32.
Davison ET, Davison MJ. Triiodothyronine (T3) toxicosis with hypokalemic periodic paralysis and ventricular tachycardia. J Electrocardiol. 1995;28(2):161–4.
Dorian P, Cass D. An overview of the management of electrical storm. Can J Cardiol. 1997;13(Suppl A):13A–7.
Erdogan HI, Gul EE, Gok H, Nikus KC. Therapy-resistant ventricular tachycardia caused by amiodarone-induced thyrotoxicosis: a case report of electrical storm. Am J Emerg Med. 2012;30(9):2092.e5–e7.
Biondi B, Palmieri EA, Klain M, Schlumberger M, Filetti S, Lombardi G. Subclinical hyperthyroidism: clinical features and treatment options. Eur J Endocrinol. 2005;152(1):1–9.
Chojnowski K, Bielec A, Czarkowski M, Dmowska-Chalaba J, Kochanowski J, Wasowska A. Repeated ventricular. Cardiol J. 2007;14(2):198–201.
Samuels MH. Subclinical thyroid disease in the elderly. Thyroid Off J Am Thyroid Assoc. 1998;8(9):803–13.
Bakiner O, Ertorer ME, Haydardedeoglu FE, Bozkirli E, Tutuncu NB, Demirag NG. Subclinical hypothyroidism is characterized by increased QT interval dispersion among women. Med Princ Pract. 2008;17(5):390–4.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Meziou, S.M., Kanoun, F., Marrakchi, D.I., Kammoun, I., Kachboura, S. (2016). Thyroid Dysfunction and Arrhythmias. In: Imam, S., Ahmad, S. (eds) Thyroid Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-25871-3_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-25871-3_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-25869-0
Online ISBN: 978-3-319-25871-3
eBook Packages: MedicineMedicine (R0)