Abstract
This chapter will discuss how simulation-based technology and techniques can be used to make patients safer. The chapter starts with a primer on patient safety terminology, followed by a discussion of the use of simulation to improve patient safety at the individual and team levels, and an exploration of the application of simulation to improve patient safety at system levels. Many of the existing simulation-based medical education interventions in the pediatric community can be adapted to maximize their impact on patient safety. Additionally, novel applications of simulation with a specific focus on patient safety have great potential to increase the value proposition of healthcare simulation. This value includes both soft dollars in savings related to traditional simulation-based training and hard dollars related to increased efficiency and reductions in serious safety events and potential litigation.
Healthcare providers with an expertise in simulation can use this chapter as a guide to integrating simulation activities into your institutions’ existing risk, safety, and/or quality activities. A discussion on how to foster sustainable ongoing collaborations will be presented, including the development of new collaborations with experts in systems engineering, human factors, and the behavioral sciences. The chapter will finish by exploring the barriers and future application of simulation to patient safety. This integration will maximize the impact of this patient safety work on pediatric patient outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Patient Safety
- Quality
- Structure
- Process
- Outcomes
- High-reliability organizations
- Resilience
- Risk reduction
- Teamwork
- Communication
- Simulation
- In situ simulation
- Individual
- Provider
- Systems
- Quality improvement
- Donabedian
- Competency
- Summative assessment
- TeamSTEPPS
- Shared mental model
- Root cause analysis
- Human factors
- Systems engineering
- Latent safety threats
- Systems integration
- Resilience engineering
- Return on investment
- Patient outcomes
- Handoffs
-
1.
The role of pediatric simulation in improving patient safety is evolving and has tremendous potential.
-
2.
Simulation is increasingly being used to evaluate systems and processes in both a retrospective and prospective fashion.
-
3.
Simulation is a powerful bridge between existing safety initiatives and frontline providers.
-
4.
The integration of simulation into ongoing patient safety, risk reduction, and quality initiatives has great potential to demonstrate the return on investment of simulation and to improve patient outcomes.
Background
Pediatric simulation practitioners often conduct their work to improve proximal outcomes such as provider skills and teamwork. In addition, simulation can be used within the broader context of the practice and improvement of patient safety as it allows for an individual-provider and/or team-based and/or systems-based approach to patient safety . Simulation activities can be focused on a single individual (knowledge, skills, and attitudes), individuals interacting with other individuals (teamwork, communication) , and individuals interacting with systems (in situ simulation) . Collaborations between simulation practitioners and safety scientists from other disciplines such as systems/industrial engineering, human factors , health-outcomes research, and the behavioral sciences are critical to future innovations in our field. The application of theory and processes from these domains has great potential to maximize the impact of simulation on improving the safety behaviors of healthcare providers/teams, technologies/devices, and the performance of the system itself.
Pediatric-specific reviews on the role of simulation in patient safety have been published and largely discuss microsystem applications of simulation including routine training for emergencies, training for teamwork, testing new procedures for safety, evaluating competence, testing device usability, investigating human performance, and providing skills training outside of the production environment [1, 2]. A number of recent publications point to the value of simulation in improving the safety of pediatric patients through translational outcomes [3–7] . Many pediatric institutions are at the cutting edge of innovation in the development of a systems-based approach to patient safety with simulation-based activities integrated into their quality, risk, and safety initiatives (see Table 5.1 for examples).
This chapter will begin with patient safety terminology; discuss the role of simulation to enhance patient safety at the provider, team, and systems level; outline the importance of systems and simulation integration in a robust patient safety program; and conclude with future directions for simulation and patient safety.
Definitions
The elements of patient safety and how it is practiced are the subject of multiple perspectives and domains, and it is important that common language be applied to the various characteristics and activities of patient safety. It is only by assuring that there are similar concepts relative to the language and terms used in describing patient safety that programs can move forward with some confidence in work that utilizes simulation as a means to develop and enhance patient safety. Therefore, the first requirements are to define and develop common understanding of basic terms and concepts in patient safety.
Patient safety refers to “freedom from accidental or preventable injuries produced by medical care” [8]. Thus, practices or interventions that improve patient safety are those that reduce the occurrence of preventable adverse events. Patient safety is often described as a characteristic or something that an organization possesses or achieves. Moreover, the usual definitions of patient safety describe it in terms of what patient safety is not (i.e., the events that constitute an absence of patient safety) [9]. More realistically, patient safety is dynamic; it is something that an organization and most importantly the people in the organization think about and practice [10]. When an organization believes it has achieved safety, the organization may have lost it.
A number of frameworks exist to describe patient safety domains. Donabedian provided one of the earliest frameworks to describe quality of care that included three domains: (1) structure of care, (2) process of care, and (3) outcomes of care [11]. In this model, structure includes those things external to the patient: the environment, organizational and human resources , and the regulations and policies affecting patient care. The process includes what actually occurred in the care of the patient and includes the patients’ and providers’ activities. One might think of it as the actual work performed in caring for the patient. Finally, the outcome describes the effect of the care on the individual patient as well as the population as a whole [11].
More recent safety frameworks provide more detail, specifically describing the patient, healthcare providers, and system factors that affect patient safety. For example, the Systems Engineering Initiative for Patient Safety (SEIPS) model describes patient safety in terms of the interactions, relationships, and influences of various system components, including the individuals that are part of the system [12] (see Fig. 5.1). This more sophisticated and multifactorial model allows for a more nuanced view of the various elements that affect patient care.
The terms quality and safety in health care are sometimes confused or used interchangeably. In order to clarify this confusion, the Institute of Medicine describes six elements of high-quality patient care. High-quality care is safe, effective, efficient, patient-centered, timely, and equitable [13]. In this model, safety is described as only one element of quality health care. An alternative way to think about the relationship between safety and quality is to envision safety as the floor or threshold of care and quality as the ceiling or goal [14]. Health care may be safe but not meet the other six targets for quality of care established by the Institute of Medicine. However, safe care is a requisite element of high-quality health care.
High-reliability organizations (HROs) manage to conduct operations in high-risk environments in a remarkably safe fashion . HROs are defined as organizations that operate in high-risk environments or are engaged in high-risk activities but suffer fewer than expected adverse events. Some examples of industries with HROs include commercial aviation, military (aircraft carriers), and nuclear power. HROs have five specific characteristics that have been described: (1) reluctance to simplify, (2) sensitivity to operations , (3) deference to expertise, (4) preoccupation with failure, and (5) commitment to resilience [15]. In recent years, a number of healthcare organizations have attempted to develop an HRO culture and practice HRO behaviors. Of interest, many of the types of organizations that are exemplars of an HRO utilize simulation and/or regular training as a tool to develop and maintain an HRO culture and HRO behaviors [16]. For example, licensed civilian nuclear power plants in the USA require their operators to participate in ongoing simulation-based training approximately 25 % of the time that they are working. The Nuclear Regulatory Commission sets standards for the fidelity of the nuclear simulators , the types of training, and scenarios that should occur as well as standards for simulation instructors [17].
Simulation-Based Patient Safety Activities at the Provider Level
At the core of patient safety are healthcare providers equipped with the knowledge and skills necessary to safely diagnose and treat patients and their varied, often complex, medical concerns. This applies to both trainees and frontline providers in all healthcare fields—medicine, nursing , pharmacy, respiratory therapy, etc. Herein lies one of the fundamental tensions in healthcare provider education—providing trainees the opportunities to learn while at the same time providing safe care to patients. Since its introduction into health care, simulation has been used successfully to improve providers’ knowledge, skills, behaviors, and attitudes. A large systematic review reported that simulation-based training was associated with large effects for outcomes of confidence, knowledge, skills, attitudes, and behaviors [18]. A review conducted specifically in pediatrics noted large effects on knowledge, skills, and behaviors in 57 studies [19]. Further discussion of this evidence can be found in this book, Chaps. 7 (“Assessment”), 13 (“Simulation along the healthcare education continuum”), and 15 (“Interprofessional Education”) . Through simulation, the apprenticeship paradigm of “do one, see one, teach one” is giving way to a thoughtful competency-based approach with graded levels of supervision and independence or entrustment assigned to the trainee based (in part) on performance in a simulated setting. These efforts will continue to ensure that providers at all levels and in all disciplines work in an environment in which they can develop and maintain their skills while keeping patients safe.
With the increasing focus on competency and the rapid pace at which new equipment, technologies, procedures, and processes are incorporated into health care, simulation can provide a means by which providers can continually train, practice, and be assessed in an ongoing manner. In some institutions, healthcare providers are being required to demonstrate competency with new equipment, technology, and processes in order to receive and/or maintain clinical privileges. At a national level, anesthesia leads the medical field and has included simulation as part of the maintenance of professional certification of physicians through the American Board of Anesthesiology since 2010. All physicians seeking recertification are required to participate in 6 h of simulations and structured debriefs and to identify areas of improvement in their own practices [20, 21]. Since 2009, residents completing surgical residencies in the USA have been required to successfully complete a Fundamentals of Laparoscopic Surgery course. While other specialty boards (e.g., family medicine) utilize computer-based simulations, no other medical boards require full-body or haptic-type simulations for initial certification or recertification [21]. Currently, simulation is not part of the pediatric board examination process; however, many institutions have started to implement simulation as a requirement at the local level (examples in Table 5.1). The application of simulation for summative assessment has been limited by the availability of robust assessment tools that are sufficiently valid to inform these high-stakes decisions (see also Chap. 7 “Assessment”).
Recent studies have taken the important step of translating improvements in knowledge and skill into improved patient outcomes . A systematic review noted 50 studies reporting patient outcomes and that simulation was associated with small to moderate benefits on patient outcomes [22]. In fields outside of pediatrics, significant effects have been noted for central-line placement [23] , obstetrical-neonatal outcomes [4], and laproscopic surgery [24]. Unfortunately, of the 50 studies included in this review, only 4 were in pediatrics [22]. One such pediatric study showed improved cardiopulmonary arrest survival rates for pediatric patients following the implementation of simulation-based mock code resident resuscitation training [3]. Additional pediatric studies have demonstrated a positive effect of simulation on acquisition of procedural skills (see also Chap. 11).
Simulation also has a role in advancing providers’ adherence to established patient safety tools, such as the use of care bundles. For example, evidence-based practice to decrease central-line infections have been well studied with the result being an effective bundle of practices that, when performed together, have a significant impact on the rate of central-line-associated bloodstream infections. What was unclear was the best way to ensure that staff were trained and followed the recommended procedures. A simulation-based intervention reduced central-line infections by 74 % compared with a unit in which residents were not required to undergo training [25]. Additionally, this intervention was noted to be highly cost-effective with a net annual savings of US$700,000 per US$100,000 allocated [26]. Unfortunately, cost-benefit analyses are infrequent and incomplete in most simulation studies [27].
Simulation-Based Patient Safety Activities at the Team Level
The role of teamwork and communication in improving patient safety is well established, with studies demonstrating deficiencies in these domains contributing to an estimated 70 % of medical errors [28] . Interprofessional simulation provides a training ground for teams to practice and improve their teamwork and communication skills . Numerous studies have incorporated simulation-based teamwork training modules and identified improvement in teamwork behaviors. [29–34]. An example of a well-developed and widely disseminated team-training program is the Agency for Healthcare Research and Quality (AHRQ) TeamSTEPPS program [35]. Compared to a didactic-only TeamSTEPPS program, a simulation-based TeamSTEPPS program was associated with 37 % decrease in adverse outcomes. [29]. Likewise, a systematic review noted that in nine studies, simulation-based crisis resource management training translated to improved patient outcomes and decreased mortality [36].
Simulation affords the opportunity to embed key behaviors in high-risk clinical endeavors. For example, the concept of a shared mental model was introduced and practiced in simulation-based training in a pediatric emergency department. This term is common to safety science and refers to the team members being “on the same page” [37]. In practice, sharing a mental model involves four elements: “this is what I think is going on,” “this is what we have done,” “this is what we need to do,” and “does anyone have any other ideas” or “what am I missing.” We encourage team leaders to share a mental model in the first 3–5 min of any crisis situation and to update it frequently. Alternatively, any team member can ask for the mental model or that the mental model be updated when the situation is not progressing as expected or the situation is confusing. The introduction of this concept was viewed as so helpful by emergency nurses in one study that they incorporated it as a required item in a resuscitation flow sheet. If the team leader had not shared a mental model in the first 3–5 min of caring for a patient, the nursing team leader would request it [6].
Handoffs between providers are another example of key safety behaviors ripe for simulation-based process improvement and research [38] . One institution incorporated simulation-based handoff training into teamwork and communication training following a serious event investigation that identified lack of handoff standardization as a root cause of the serious event. Observations after the training demonstrated an increase in the communication of crucial information between nurses during handoffs [39]. Another group used simulated patient cases to study patient handoffs as a first step in creating an effective, standardized handoff process [40].
Simulation-Based Patient Safety Activities at the System Level
The preceding paragraphs focus on the potential to improve providers’ and team performance in order to reduce patient harm. Newer approaches to patient safety involve a systems-based approach with the view that errors or safety threats reflect the risks and hazards that providers and patients face in the context of a poorly designed system [41, 42]. Instead of focusing on individual failings, this approach identifies the components of the system that contribute to harm and involves the implementation of systemic changes that minimize the likelihood of these events. A robust simulation-based patient safety program involves identification of system threats using both retrospective reviews of adverse events and near misses as well as prospective efforts to identify and mitigate risk before an actual patient incident occurs (examples are provided in Table 5.1).
Retrospective Approach to Safety at the System Level
Simulation can be used to retrospectively examine why an error occurred (e.g., simulation-informed root cause analysis (RCA)). Simulation of adverse outcomes (SAO) has been used in the surgical arena as a method of conducting investigations of the causality of adverse surgical outcomes [43, 44]. This process involved conducting each simulation up to seven times (with debriefings) to identify sources of errors in order to augment traditional RCA processes. The addition of simulation and re-creation of adverse events identified an increased number of systems issues compared to a traditional RCA. The debriefings allowed for a greater understanding of why and how decisions leading to the adverse event were made. By re-creating the adverse event, it became possible to understand what the individual team members were seeing and hearing that made the actions seem logical at the time of the event. These types of simulations can also identify periods of heavy workload, possible task fixation, and loss of situation awareness.
Prospective Approach to Safety at the System Level
Prospective risk reduction applies methods developed in the engineering community (e.g., human factors or ergonomics, systems engineering, probabilistic risk assessment, cognitive task analysis) and used in other HROs combined with simulation techniques to optimize the safety of the system. A good example was the use of simulation during implementation of a new electronic medical record. When Yale-New Haven Children’s Hospital implemented a new electronic medical record, simulation was used for provider training. The program collaborated with human factors engineers and informatics experts to provide feedback on the usability of the system in the clinical environment from providers during in situ simulations prior to formal implementation in the clinical environment. One specific example from this work was a group of simulations that provided information on the implications of nurses working with a new electronic medical record while concurrently caring for a severely injured trauma patient in the actual clinical environment. This work identified that it was difficult for the documenting nurse to see the vital signs on the monitor while working on the electronic record. The documenting nurse also reported multiple challenges with the usability of the graphic user interface. This work resulted in a requirement for an additional nurse in trauma resuscitations due to the increased workload during the first months of implementation (Marc Auerbach, written communication, October 2014) .
Another familiar use of simulation to prospectively improve safety is through the use of in situ simulation to identify potential latent safety threats (LSTs) . LSTs have been defined as systems-based threats to patient safety that can materialize at any time and are previously unrecognized by healthcare providers [45]. In situ simulation in a pediatric emergency department (ED) proved a practical method for the detection of LSTs as well as reinforcing team training [46–49]. In its most effective form, in situ simulation can become a routine expectation of staff that positively influences operations and the safety climate in high risk-clinical settings [6]. In situ simulation can also be used to monitor the impact of other risk reduction strategies (new processes and procedures) through on-demand measurement and is discussed in more detail in Chap. 12 (examples are provided in Table 12.1). The authors encourage simulation practitioners to collaborate with content experts as they embark on these types of systems-level simulation-based initiatives.
Simulation for Improving the Safety of New Processes
Incorporating simulation into process development offers an opportunity to road test the process and revise it before clinical implementation . In one institution, a new process for response to critical airways was developed and tested using simulation [50]. Six simulations were conducted at baseline, and six simulations were conducted to test the new critical airway response. While two of the six simulated patients “died” in the original airway response system, no simulated patients “died” in the new airway response system. In addition, there was a significant decrease in the otolaryngologist’s response time to the emergency department . In another experience, five iterative simulations were used in the development of a massive bleeding emergency protocol. The final protocol was more pragmatic and reliable for staff and resulted in marked reductions in laboratory turnaround times for crucial bleeding labs (Kimberly Stone, written communication, October 2014) .
Simulation to Improve the Safety of New Environments
Simulation has been used to test the staffing model and safety of a new pediatric ED [5], a new general ED [6], and a children’s hospital’s obstetrical unit [51]. In the case of the new pediatric ED, in situ simulation prior to clinical occupancy resulted in changes to team members’ roles and responsibilities as well as identifying latent threats in the new clinical space. Several hospitals have successfully utilized in situ simulation prior to opening new hospital units to identify and mitigate LSTs identified before caring for patients as documented in Table 5.1 [51].
Systems Integration: Simulation–Patient Safety–Quality
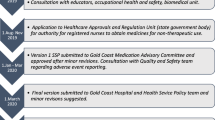
Simulation programs can maximize their impact on safety through systems integration . Systems integration is defined by the Society for Simulation in Healthcare (SSH) as “consistent, planned, collaborative , integrated and iterative application of simulation-based assessment and teaching activities with systems engineering and risk management principles to achieve excellent bedside clinical care, enhanced patient safety, and improved metrics across the health care system” [52]. An institution’s simulation activities should be integrated into ongoing safety programs. Examples of opportunities for integration are listed in Table 5.2. This integration should result in regular bi-directional flow of information between these groups. For example, the goals and objectives of simulation-based exercises are created based on perceived risk, adverse events, and near misses identified from realpatient databases. Subsequently, the simulations and debriefings inform the analysis of how to reduce risk. Optimally, simulations and debriefings identify and bring attention to risks that may not have been otherwise recognized and help organizations to anticipate and mitigate harm to patients. In Fig. 5.2, we provide an example of how simulation can be integrated into ongoing patient safety activities after a serious event (see also Chap. 6 “Systems Integration”).
In an integrated system, simulation-based activities are a part of everyday activities of an institution that is expected by staff as part of their daily work. Additionally, in some established programs, errors or threats identified in simulation are reported in the hospital event reporting system in the same manner that a real patient event is reported (e.g., Yale-New Haven Children’s Hospital, Seattle Children’s Hospital). This provides a clear reporting structure, allows for prioritization and tracking of actionable findings, and applies the accepted quality and safety nomenclature to simulation-based events (near miss, serious safety event, etc.). Formal reporting of simulation-identified threats also removes the responsibility of the mitigation of identified risks from the simulation team as, typically, the simulation team or program will not have the ability to influence the multiple factors often involved in systems issues . The risk is when providers participate in simulations, but do not believe that feedback from those sessions will be heard or lead to change, they come to believe that the organization is building safety only on the backs of the increased vigilance of providers rather than by addressing system issues[45]. An effective simulation culture exists when there is buy-in from the highest level of leadership (top-down) and from the frontline providers (bottom-up) across multiple disciplines.
Barriers/Challenges to Simulation in Patient Safety
In order to fully realize the potential of simulation to improve the practice of patient safety , it will be critical to develop tools that are able to link simulation practices to improvement in patient outcomes . It will also be necessary to leverage the expertise of those working in various fields of safety sciences in domains external to health care. Terry Fairbanks, human factors expert and emergency physician, has stated that when airlines wanted to become safer, they did not ask pilots and flight attendants how to become safer, they involved engineers, cognitive psychologists, and human factors experts (Terry Fairbanks, written communication, June 2013).
The cost of implementing simulation in terms of provider time, instructor time, and equipment/resources can be balanced through savings related to improved quality of care, avoidance of adverse events, reduction in malpractice and liability insurance, and decreased litigation costs. Additional study is needed to understand the cost avoidance associated with simulation-based safety activities.
Future Directions
Though simulation has historically been utilized to assess individual and team competencies , in recent years simulation is increasingly being used to assess system competencies and to evaluate new facilities, new teams, and new processes [5, 6, 50, 51]. Historically, healthcare providers have not embraced expertise that originated outside of health care ; however, increasingly, there is a recognition of relevant expertise in fields outside of health care and a willingness to incorporate this expertise in healthcare simulation and safety work. This includes recognition of the value of human factors , cognitive task analysis, and engineering (cognitive, industrial, and systems) in addressing some of the major issues facing health care today .
In recent years, resident work hours in the USA have been reduced. Though the hours and length of shifts for residents have substantially decreased from the typical number of hours worked by residents a decade ago, there has not been a corresponding increase in the length of postgraduate medical training [53, 54]. It is well described that expertise in any domain is related to the hours spent in deliberate practice and coaching [55]. A significant issue for those in medical education is how to assure competence with a decreased number of hours devoted to training and an ever-increasing knowledge base. The question of whether simulation can accelerate the development of expertise is beginning to be explored but is yet unanswered [56]. It is clear that simulation-based deliberate practice in laparoscopic surgery or central line placement results in improved performance in an actual clinical environment [22–26]. However, it is less clear that non-procedural expertise, for example, recognition of the patient with sepsis, is sensitive to simulation-based training. To understand the effect of simulation on the development of this type of medical expertise will require collaboration with experts in the development of expertise, naturalistic decision-making, and cognitive bias and de-biasing .
Another area of safety that is suitable for simulation is the exploration of the adaptive capacity of systems and teams relative to unexpected disturbances. This is related to the safety science of resilience engineering. While resilience engineering is employed in other industries, it has only recently surfaced in health care. Often, resilience engineering is concerned with retrospective evaluation of systems that have failed or succeeded spectacularly such as the space shuttle Columbia and Challenger disasters [57]. Though still theoretical, simulation offers a prospective way to evaluate systems’ adaptive responses, tolerance for disturbance, and ability to recover from disruptions to the system. In health care, this could mean evaluation of existing and proposed systems relative to normal function and the ability to adapt to and recover from unexpected events in health care. Simulation also offers a method to evaluate the effect of proposed changes in the system relative to adaptive capacity and the brittleness of a system in the face of changing resources, for example, staffing , team configuration, and institution of an electronic health record .
In the future, as a simulation community, we will need to demonstrate that integrated simulation-based patient safety programs lead to measurable improvements in the health care that is delivered, a financial return on investment , and improved health outcomes .
Conclusions
Simulation is a natural partner for ongoing patient safety activities at the individual , team, and systems levels of organizations. A growing number of simulation-based training programs are linking their program improvements in knowledge, skills, and teamwork to patient outcomes. Increasingly, simulation is being used at the systems level to identify and mitigate patient safety risks. Simulation can facilitate the discovery of error-producing conditions before those conditions affect patients and a deeper understanding of these conditions when they have affected patients. Safety science and simulation experts will need to integrate and coordinate their activities within existing and new programs in order to achieve maximum patient safety.
References
Griswold S, Ponnuru S, Nishisaki A, Szyld D, Davenport M, Deutsch ES, et al. The emerging role of simulation education to achieve patient safety: translating deliberate practice and debriefing to save lives. Pediatr Clin North Am. 2012;59(6):1329–40.
Nishisaki A, Keren R, Nadkarni V. Does simulation improve patient safety? Self-efficacy, competence, operational performance, and patient safety. Anesthesiol Clin. 2007;25(2):225–36.
Andreatta P, Saxton E, Thompson M, Annich G. Simulation-based mock codes significantly correlate with improved pediatric patient cardiopulmonary arrest survival rates. Pediatr Crit Care Med. 2011;12(1):33–8.
Draycott T, Sibanda T, Owen L, Akande V, Winter C, Reading S, et al. Does training in obstetric emergencies improve neonatal outcome? BJOG. 2006;113(2):177–82.
Geis GL, Pio B, Pendergrass TL, Moyer MR, Patterson MD. Simulation to assess the safety of new healthcare teams and new facilities. Simul Healthc. 2011;6(3):125–33.
Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual Saf. 2013;22(6):468–77.
Patterson MD, Geis GL, LeMaster T, Wears RL. Impact of multidisciplinary simulation-based training on patient safety in a paediatric emergency department. BMJ Qual Saf. 2013;22(5):383–93.
http://www.psnet.ahrq.gov/popup_glossary.aspx?name=patientsafety. Accessed 9 Jan 2014.
Lawton R, Taylor N, Clay-Williams R, Braithwaite J. Positive deviance: a different approach to achieving patient safety. BMJ Qual Saf. 2014;23:880–3.
Frankel AS, Leonard MW, Denham CR. Fair and just culture, team behavior, and leadership engagement: the tools to achieve high reliability. Health Serv Res. 2006;41(4 Pt 2):1690–709.
Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–8.
Carayon P, Schoofs Hundt A, Karsh BT, Gurses AP, Alvarado CJ, Smith M, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15(Suppl 1):50–8.
Institute of Medicine (U.S.). Committee on Quality of Health Care in America editor. Crossing the quality chasm: a new health system for the 21st century. Vol. xx. Washington, D.C.: National Academy Press; 2001. p. 337.
Stevens P, Matlow A, Laxer R. Building from the blueprint for patient safety at the hospital for sick children. Healthc Quart. 2005;8:132–9.
Weick KE, Sutcliffe KM. Managing the unexpected: assuring high performance in an age of complexity. 1st ed. Vol. xvi. San Francisco: Jossey-Bass; 2001. p. 200.
Chassin MR, Loeb JM. High-reliability health care: getting there from here. Milbank Q. 2013;91(3):459–90.
International Atomic Energy Agency. Use of control room simulators for training of nuclear power plant personnel Vienna. Austria: Nuclear Power Engineering Section, International Atomic Energy Agency; 2004. p. 101. http://www-pub.iaea.org/MTCD/publications/PDF/te_1411_web.pdf.
Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9):978–88.
Cheng A, Lang TR, Starr SR, Pusic M, Cook DA. Technology-enhanced simulation and pediatric education: a meta-analysis. Pediatrics. 2014;133:1313–23. (?rest of journal citation)
Levine AI, Flynn BC, Bryson EO, Demaria S Jr. Simulation-based maintenance of certification in anesthesiology (MOCA) course optimization: use of multi-modality educational activities. J Clin Anesth. 2012;24(1):68–74.
Levine AI, Schwartz AD, Bryson EO, Demaria S Jr. Role of simulation in U.S. physician licensure and certification. Mount Sinai J Med NY. 2012;79(1):140–53.
Zendejas B, Brydges R, Wang AT, Cook DA. Patient outcomes in simulation-based medical education: a systematic review. J Gen Intern Med. 2013;28(8):1078–89.
Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med. 2009;169(15):1420–3.
Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM. Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg. 2010;199(1):115–20.
Barsuk JH, Cohen ER, Potts S, Demo H, Gupta S, Feinglass J, et al. Dissemination of a simulation-based mastery learning intervention reduces central line-associated bloodstream infections. BMJ Qual Saf. 2014;23(9):749–56.
Cohen ER, Feinglass J, Barsuk JH, Barnard C, O’Donnell A, McGaghie WC, et al. Cost savings from reduced catheter-related bloodstream infection after simulation-based education for residents in a medical intensive care unit. Simul Healthc. 2010;5(2):98–102.
Zendejas B, Wang AT, Brydges R, Hamstra SJ, Cook DA. Cost: the missing outcome in simulation-based medical education research: a systematic review. Surgery. 2013;153(2):160–76.
Smith IJ. The Joint Commission guide to improving staff communication. 2nd ed. Oakbrook Terrace: Joint Commission Resources; 2009. p. x, 142.
Riley W, Davis S, Miller K, Hansen H, Sainfort F, Sweet R. Didactic and simulation nontechnical skills team training to improve perinatal patient outcomes in a community hospital. Jt Comm J Qual Patient Saf. 2011;37(8):357–64.
Salas E, DiazGranados D, Weaver SJ, King H. Does team training work? Principles for health care. Acad Emerg Med. 2008;15(11):1002–9.
Weaver SJ, Dy SM, Rosen MA. Team-training in healthcare: a narrative synthesis of the literature. BMJ Qual Saf. 2014;23(5):359–72.
Sigalet EL, Donnon TL, Grant V. Insight into team competence in medical, nursing and respiratory therapy students. J Interprof Care. 2014;22:1–6. [Epub ahead of print].
Sigalet E, Donnon T, Cheng A, Cooke S, Robinson T, Bissett W, Grant V. Development of a team performance scale to assess undergraduate health professionals. Acad Med. 2013;88(7):989–96.
Sigalet E, Donnon T, Grant V. Undergraduate students’ perceptions of and attitudes toward a simulation-based interprofessional curriculum; the KidSIM ATTITUDES questionnaire. Simul Healthc. 2012;7(6):353–8.
Kyriacou DN, Ricketts V, Dyne PL, McCollough MD, Talan DA. A 5-year time study analysis of emergency department patient care efficiency. Ann Emerg Med. 1999;34(3):326–35.
Boet S, Bould MD, Fung L, Qosa H, Perrier L, Tavares W, et al. Transfer of learning and patient outcome in simulated crisis resource management: a systematic review. Can J Anaesth. 2014;61(6):571–82.
Mathieu JE, Heffner TS, Goodwin GF, Salas E, Cannon-Bowers JA. The influence of shared mental models on team process and performance. J Appl Psychol. 2000;85(2):273–83.
Cooper JB. Using simulation to teach and study healthcare handoffs. Simul Healthc. 2010;5(4):191–2.
Berkenstadt H, Haviv Y, Tuval A, Shemesh Y, Megrill A, Perry A, et al. Improving handoff communications in critical care: utilizing simulation-based training toward process improvement in managing patient risk. Chest. 2008;134(1):158–62.
Kendall L, Klasnja P, Iwasaki J, Best JA, White AA, Khalaj S, et al. Use of simulated physician handoffs to study cross-cover chart biopsy in the electronic medical record. AMIA Annu Symp Proc. 2013;2013:766–75.
Russ AL, Fairbanks RJ, Karsh BT, Militello LG, Saleem JJ, Wears RL. The science of human factors: separating fact from fiction. BMJ Qual Saf. 2013;22(10):802–8.
Carayon P, Xie A, Kianfar S. Human factors and ergonomics as a patient safety practice. BMJ Qual Saf. 2014;23(3):196–205.
Simms ER, Slakey DP, Garstka ME, Tersigni SA, Korndorffer JR. Can simulation improve the traditional method of root cause analysis: a preliminary investigation. Surgery. 2012;152(3):489–97.
Slakey DP, Simms ER, Rennie KV, Garstka ME, Korndorffer JR Jr. Using simulation to improve root cause analysis of adverse surgical outcomes. Int J Qual Health Care. 2014;26(2):144–50.
Alfredsdottir H, Bjornsdottir K. Nursing and patient safety in the operating room. J Adv Nurs. 2008;61(1):29–37.
Patterson MD, Blike GT, Nadkarni VM. In situ simulation: challenges and results. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors Advances in patient safety: new directions and alternative approaches (Vol 3: performance and tools). Advances in Patient Safety, Rockville; 2008.
Wetzel EA, Lang TR, Pendergrass TL, Taylor RG, Geis GL. Identification of latent safety threats using high-fidelity simulation-based training with multidisciplinary neonatology teams. Jt Comm J Qual Patient Saf. 2013;39(6):268–73.
Burton KS, Pendergrass TL, Byczkowski TL, Taylor RG, Moyer MR, Falcone RA, et al. Impact of simulation-based extracorporeal membrane oxygenation training in the simulation laboratory and clinical environment. Simul Healthc. 2011;6(5):284–91.
Wheeler DS, Geis G, Mack EH, LeMaster T, Patterson MD. High-reliability emergency response teams in the hospital: improving quality and safety using in situ simulation training. BMJ Qual Saf. 2013;22(6):507–14.
Johnson KGG, Oehler J, Houlton J, Tabangin M, Myer C, Kerrey B. High fidelity simulation to design a novel system of care for pediatric critical airway obstruction.(The American Society of Pediatric Otolaryngology April 2012; San Diego, CA2012 (? should this be Johnson K, Geis G, Oehler J, Meinzen-Derr J, Bauer J, Myer C et al. Simulation to implement a novel system of care for pediatric critical airway obstruction). Arch Otolaryngol Head Neck Surg. 2012;138(10):907–11.
Ventre KM, Barry JS, Davis D, Baiamonte VL, Wentworth AC, Pietras M, et al. Using in situ simulation to evaluate operational readiness of a children’s hospital-based obstetrics unit. Simul Healthc. 2014;9(2):102–11.
http://www.ssih.org/Portals/48/Accreditation/Provisional_Docs/2013_ProvisionalAccreditationStandards.pdf. Accessed 12 Mar 2014.
Desai SV, Feldman L, Brown L, Dezube R, Yeh HC, Punjabi N, et al. Effect of the 2011 vs 2003 duty hour regulation-compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff: a randomized trial. JAMA Intern Med. 2013;173(8):649–55.
Ahmed N, Devitt KS, Keshet I, Spicer J, Imrie K, Feldman L, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg. 2014;259(6):1041–53.
Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(Suppl 10):70–81.
Phillips JK, Klein G, Sieck WR. Expertise in judgment and decision making: a case for training intuitive decision skills. In: Harvey DJKN, editor. Blackwell handbook of judgment and decision making. Malden: Blackwell Publishing Ltd; 2004.
Nemeth C, Wears R, Woods D, Hollnagel E, Cook R. Minding the gaps: creating resilience in health care. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors Advances in patient safety: new directions and alternative approaches (Vol 3: performance and tools). Rockville: Advances in Patient Safety; 2008.
Connelly LG, Bair AE. Discrete event simulation of emergency department activity: a platform for system-level operations research. Acad Emerg Med. 2004;11(11):1177–85.
Huang L, Norman D, Chen R. Addressing hospital-wide patient safety initiatives with high-fidelity simulation. Phys Executive J. 2010:36 (4):34–39.
INSPIRE Network. 2014. http://inspiresim.com/. Accessed 12 April 2014.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Auerbach, M., Stone, K., Patterson, M. (2016). The Role of Simulation in Improving Patient Safety. In: Grant, V., Cheng, A. (eds) Comprehensive Healthcare Simulation: Pediatrics. Comprehensive Healthcare Simulation. Springer, Cham. https://doi.org/10.1007/978-3-319-24187-6_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-24187-6_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-24185-2
Online ISBN: 978-3-319-24187-6
eBook Packages: MedicineMedicine (R0)