Abstract
Substance use disorders during pregnancy are common and are often associated with increased maternal and fetal risk. In the emergency department (ED), a physician must try to engage these patients in treatment while safely managing intoxication and withdrawal to mitigate risk. In this chapter, the emergency management of various substance use disorders (specifically alcohol, benzodiazepines, cannabis, opioids, stimulants, and nicotine) in the care of the pregnant patient is reviewed. This review includes assessment of risks to both mother and fetus, recommendations for acute management, and disposition considerations for treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pregnancy
- Lactation
- Prenatal
- Maternal
- Fetal
- Alcohol
- Benzodiazepines
- Cannabis
- Opioid
- Stimulant
- Cocaine
- Methamphetamine
- Nicotine
Introduction
Intoxication from alcohol and other illicit substances is a frequent reason for emergency department visits. Clinicians who encounter patients with substance use disorders in the ED have a privileged opportunity to intervene with evidence-based treatments and a chance to help patients move toward the highest level of health possible.
This is a particularly compelling clinical scenario when the patient is pregnant and using substances. While pregnancy was once thought to be a period of decreased risk for psychiatric illness, it is now understood that mental illness and substance use disorders continue, and sometimes worsen, during a woman’s pregnancy. It is critical that screening for substance use disorders occurs during every emergency department visit, particularly for pregnant women and women of reproductive potential.
In the field of addiction medicine, it is firmly established that a clinician’s nonjudgmental attitude powerfully and positively influences the efficacy of their intervention [1]. Despite this, many clinicians may struggle with maintaining a nonjudgmental attitude, especially in the clinical encounter with a pregnant woman using substances. This issue is worthy of emphasis because, in the authors’ experience, pregnant women using substances often feel particularly shameful and guilty about their substance use, and as a result of that shame may be inclined to avoid treatment, including prenatal care [2]. Clinicians should do their best to establish a clinician-patient relationship without discrimination or stigmatization. All important information about the risks of substance use and the benefits of treatment should be communicated in a nonjudgmental, respectful, non-stigmatizing, and empathic manner [3].
The use of alcohol, illicit substances and psychoactive drugs is common in pregnancy and can lead to multiple health and social problems for both the mother and her baby [4]. In this chapter, we will review the risks associated with the following substances: alcohol, benzodiazepines, cannabis, opioids, stimulants (including cocaine and amphetamine ), and nicotine. We will specifically review the risks to the mother and the developing fetus, as well as the potential risks and benefits of emergency department interventions used to treat these substance use disorders. Attention will be given to relevant legal and ethical issues and the goals of the emergency department encounter will be identified.
Alcohol
Chronic alcohol use during pregnancy (as defined by the ingestion of 2 or more drinks/day) can lead to both adverse obstetrical outcomes and negative effects on fetal development [5]. In terms of obstetric risk, alcohol use is associated with a threefold increase in preterm deliveries, as well as increased rates of other serious complications including spontaneous abortion, low-birth-weight infants, placental abruption, amnionitis, and overall perinatal mortality [3].
Maternal alcohol use during pregnancy is also associated with an increased risk of fetal alcohol syndrome (FAS) : a pattern of neurologic, behavioral, and cognitive deficits that can interfere with growth, learning, and socialization. FAS has three major components: a characteristic pattern of facial abnormalities (small eye openings, indistinct or flat philtrum, thin upper lip), growth deficiencies, and central nervous system abnormalities that include structural, neurological, and functional deficits [6].
Alcohol use on a regular basis can put a pregnant woman at risk for a withdrawal syndrome that can be severe and even life-threatening, which often requires emergency care. Given the potential risks associated with alcohol withdrawal, the lack of significant harm that has been demonstrated from short-term benzodiazepine use in pregnancy , and the evidence supporting the use of benzodiazepines in the management of alcohol withdrawal in the general population, the World Health Organization (WHO) recommends that hospitalization for medically monitored detoxification be considered in the withdrawal management of pregnant women with alcohol dependence [6]. The WHO also recommends that alcohol withdrawal management be facilitated by the use of an alcohol-withdrawal scale such as the CIWA-Ar , and include administration of folate, multivitamin, and thiamine. While not specifically stated by the WHO, it is generally considered good clinical practice to consult OB while the patient is admitted for medically monitored detoxification.
Benzodiazepines
Studies concerning the teratogenicity of benzodiazepines have produced conflicting results. Recent studies, however, have not provided substantive evidence that in-utero exposure to benzodiazepines causes an increase in any specific malformation or pattern of malformations [7]. Early studies that reported an association with adverse outcomes were criticized because of recall bias and possible exposure to multiple drugs [8]. Infants of mothers taking chronic doses of benzodiazepines near term are at risk for developing withdrawal symptoms postnatally [9]. For this reason, women should be counseled to discontinue use well before delivery. If abstinence is not possible, the lowest possible dose should be used, and one of the shorter-acting benzodiazepines should be considered, such as lorazepam [10].
Many women who are taking benzodiazepines may have psychiatric illnesses, epilepsy, or be dependent on other drugs or alcohol. Maternal illness or illicit drug use is likely to create an environment that is not conducive to optimal infant development, both prenatally and in the postpartum period. Each of these conditions is a risk factor during pregnancy and, therefore, it is difficult to discern negative clinical effects due specifically to benzodiazepines, especially in relation to subsequent neurobehavioral dysfunction.
If a pregnant woman presents to the ED intoxicated with benzodiazepines, abrupt cessation of use can lead to withdrawal, which can be severe and result in seizures or delirium. As such, long-acting benzodiazepines such as clonazepam should be used to manage benzodiazepine withdrawal. In addition, psychosocial interventions should be offered throughout the period of benzodiazepine withdrawal, and inpatient care should be strongly considered in the withdrawal management of pregnant women with benzodiazepine dependence.
An important additional component of emergency care for alcohol and benzodiazepine use disorders in pregnancy is referral to further treatment. This can begin in the ED setting with a consultation referral to social work services, who can then assist in establishing adequate psychiatric, substance use and general medical follow-up. Subsequent to assessment and stabilization in the ED, continued care would ideally include integrated obstetric, psychiatric, substance use treatment , and case management assistance. Patients may benefit from an intensive outpatient treatment program or a residential program, such as the Day Hospital at Women and Infant’s Hospital in Providence, RI (http://www.womenandinfants.org/services/behavioral-health/day-hospital.cfm).
Cannabis
Marijuana use – both medical and recreational – is on the rise in reproductive-aged women [11]. This is no surprise given that many states have legalized or are now moving forward with legalization of medical marijuana. It is estimated that roughly half of female marijuana users continue to use during pregnancy [12]. While marijuana is often considered to be a relatively benign substance and is viewed by some as being safer than traditional medications for the treatment of depression and anxiety, data show that the developing fetus may be particularly vulnerable to its effects.
The use of cannabis during pregnancy has been associated with a spectrum of risks to the developing fetus. These include increased risk of intrauterine growth restriction, low birth weight, increased risk of stillbirth , and cognitive delays and deficits, including poor executive functioning [13]. Infants prenatally exposed to cannabis had decreased birth weight and were more likely to need placement in the neonatal intensive care unit or intensive care unit compared to infants whose mothers did not use cannabis during pregnancy.
Women who use cannabis have been shown to have an increased risk of anemia during pregnancy. One study has demonstrated a risk for precipitous labor [14]. In terms of breastfeeding, there are insufficient data to evaluate the effects of marijuana use on infants during lactation and breastfeeding, and in the absence of such data, marijuana use is discouraged [13].
While there are well-documented risks stemming from maternal exposure to cannabis, nonetheless there appears to be a growing number of people who view marijuana as a more effective or safer option than traditional pharmacologic interventions for the treatment of a variety of conditions, including nausea and vomiting, depression, anxiety, and insomnia. At this point, there is no data to support the use of marijuana for the management of these symptoms. The American Academy of Obstetrics and Gynecology recommends that pregnant women or women contemplating pregnancy should be counseled to discontinue use of marijuana for medicinal purposes in favor of an alternative therapy for which there is better data regarding reproductive safety [13].
Opioids
Opioid use disorders are a rising nationwide trend, and pregnant women are included in the significant impact of this problem. The prevalence of opioid use disorders during pregnancy has increased by 127% from 1998 to 2011 [15]. Opioid use carries significant risk during pregnancy, including increased risk of obstetrical maternal mortality [16]. Opioid use during pregnancy has also been associated with significant increases in fetal risk. During maternal opioid intoxication, respiratory suppression can cause fetal hypoxemia, which can lead to intrauterine growth restriction , placental insufficiency, low birth weight, and other complications [16]. During maternal opiate withdrawal, increased autonomic arousal may cause uterine contraction, potentially resulting in miscarriage or premature labor [17]. A major adverse neonatal outcome is neonatal abstinence syndrome (NAS) , which is a neonatal drug withdrawal syndrome that often requires neonatal intensive care and is associated with significant medical complications [17]. For all these reasons, it is essential to facilitate treatment for pregnant women with opioid use disorders presenting in the emergency department with the goal of minimizing potential risks to both mother and fetus.
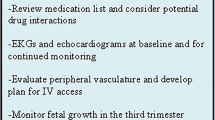
In the emergency department, if a woman presents with opioid intoxication, she should receive close monitoring and attentive supportive care. To avoid precipitating acute withdrawal, the use of naloxone should be reserved for cases of life-threatening maternal overdose [18]. A thorough psychiatric and addiction evaluation should take place as soon as she is able to participate, in order to identify any acute safety concerns, comorbid psychiatric illness, and other substance use disorders. In addition to urine toxicology screening, medical work-up should include liver function tests and electrocardiogram (to assist in determining best treatment, as given below). With informed consent, it is prudent to consider screening for hepatitis B and C, HIV , and other conditions for which the patient may be at risk due to her opioid use disorder; however if the patient’s expected emergency department stay is shorter than the time it would take for these tests to return, it may be appropriate to defer these tests to a treatment setting in which more reliable follow-up of test results can occur.
Given significant risk of maternal and fetal complications if left untreated, opioid withdrawal should be addressed diligently; the standard of care is initiation of maintenance therapy (and prevention of withdrawal) with substitution agents, either buprenorphine or methadone. If a patient is beginning to show signs of withdrawal during her ED stay, one of these medications should be initiated during that visit, with the ultimate plan for inpatient admission. Otherwise, initiation of substitution therapy could be deferred to the inpatient treatment setting, where acute withdrawal can be most safely managed. Maintenance therapy is preferred to medical detoxification off opioids completely because it may improve maternal and infant outcomes, and because it decreases risk of relapse [19]. Both methadone and buprenorphine have been demonstrated as effective treatment strategies in preventing prenatal opioid withdrawal and in maintenance of abstinence [20]. Specific studies are limited, but there are no major congenital malformations associated with either when used during pregnancy, although there is still a risk of NAS [21].
Both methadone and buprenorphine are compatible with breastfeeding as the amount of either drug transferred into the breast milk is low [22], and breastfeeding is generally recommended for stable mothers on methadone or buprenorphine maintenance therapy (who are not concurrently using illicit substances) because doing so may decrease the severity of NAS [23].
Methadone has been the drug of choice for treating opioid use disorders during pregnancy for decades. Methadone can prolong the QT interval, so it is appropriate to obtain an EKG before administration. In the acute setting, for a pregnant patient in opioid withdrawal, an initial single dose of methadone 10–20 mg could be started, with subsequent doses of methadone 5–10 mg given every 4–6 hours as needed until signs and symptoms of withdrawal are suppressed. If opioid withdrawal begins in the ED, then this process should be started while the patient is there, in order to avoid fetal distress or adverse pregnancy outcomes. Treatment can then be continued after she is admitted for ongoing medical care in the inpatient setting.
A growing collection of data supports buprenorphine as an equally good option for maintenance therapy during pregnancy, and this may be used to treat acute withdrawal if it is the chosen option for ongoing treatment. Again, treatment should be started in the ED setting if the patient is already in withdrawal at that time , with continued dose titration during an inpatient medical admission. Compared to methadone, it has been associated with less severe NAS and has fewer drug-drug interactions [21]. Baseline liver function tests should be obtained prior to initiation of buprenorphine due to concerns about potential buprenorphine-induced hepatotoxicity . A combined formulation of buprenorphine with naloxone (i.e., Suboxone) is not recommended during pregnancy because of the risks of precipitating withdrawal with naloxone if it is used improperly [19]. Buprenorphine , as a partial opioid receptor agonist, can precipitate withdrawal symptoms if administered too soon after a full opioid receptor agonist. Therefore, buprenorphine should not be administered unless a patient is showing signs of at least moderate withdrawal, and should be given no less than 24 hours after last use of a short-acting opioid (such as heroin).
The decision of which agent to use in the treatment of opioid withdrawal and for potential initiation of maintenance therapy should be made with the patient’s participation, factoring in what has worked for the patient previously, patient preference, access to care (availability of methadone clinic versus access to buprenorphine prescriber), and medical comorbidities.
An important additional component of emergency care is referral to further treatment. Most experts recommend inpatient admission for medical management of withdrawal and for initiation of substitution therapy acutely [24]. Subsequently, continued care would ideally include integrated obstetric, psychiatric, substance use treatment, and case management assistance. Patients may benefit from a subsequent intensive outpatient treatment program or a residential program. Referrals should be made to a clinic for ongoing treatment with methadone or buprenorphine. In many areas, there are programs specifically designed to care for pregnant women with opioid use disorders, and it is often possible to bypass usually long waitlists for care.
Stimulants (Cocaine and Methamphetamine)
Cocaine use during pregnancy is associated with adverse maternal and fetal outcomes, including increased risk for premature rupture of membranes, placental abruption, preterm birth, low birth weight, small for gestational age infants, decreased fetal head circumference, and adverse effects on childhood cognitive/social development [18]. Methamphetamine use during pregnancy is associated with adverse effects similar to those of cocaine, including low birth weight, preterm birth, intrauterine fetal death, gestational hypertension, preeclampsia , and abnormal childhood neurocognitive development [18, 25]. Given these significant risks, if a pregnant woman with a stimulant use disorder presents to the ED, in addition to medical and obstetrical assessments , effort should be made to engage her in motivational interviewing to promote sobriety and to connect her to addiction treatment. If a pregnant woman presents to the ED intoxicated on stimulants, treatment with benzodiazepines and/or antipsychotic medications (from either the typical or atypical antipsychotic class) for the management of acute agitation, anxiety, or psychosis may be appropriate and necessary interventions, and in this scenario, the benefit of acute treatment would likely outweigh risks of fetal exposure to these medications. In the case of acute agitation of a pregnant woman, all efforts should be made to avoid physical restraints. If restraints are required, in the second half of pregnancy, a woman should not be restrained in supine position given potential for obstruction of venous return to the heart by the gravid uterus [26]; left lateral or Fowler’s position would be preferred. There is no pharmacologic intervention necessary for stimulant withdrawal; however, the possibility of depressed mood may prompt screening for safety issues during this period [27].
Nicotine
Smoking during pregnancy has been associated with a number of negative outcomes, including spontaneous abortion, impaired fetal growth , placenta previa, placental abruption, and preterm delivery [28]. Recommendations on the use of nicotine replacement therapy during pregnancy are not yet clear; data on the efficacy of nicotine replacement therapy in aiding smoking cessation are not consistent [29]. Nicotine replacement therapy exposes the mother to continuous low doses of nicotine thus avoiding acute nicotine spikes, which may be safer to the fetus, given that concentrations of nicotine are higher in the placenta, amniotic fluid, and fetal serum than in maternal serum [28]. While nicotine replacement therapy may carry some risks itself during pregnancy, in general, nicotine replacement is considered less harmful to the fetus than smoking [30]. The American College of Obstetrics and Gynecologists (ACOG ) published recommendations in 2010 advising that nicotine replacement should only be used with clear resolve of the patient to quit smoking, and with discussion of the known risks of continued smoking, as well as the possible risks of nicotine replacement therapy [28]. Acutely in the ED, a decision regarding the use of nicotine replacement therapy should also take into account the potential for nicotine withdrawal to impair the patient’s ability to participate in important care of comorbid conditions, often making it an appropriate intervention (Table 13.1).
Conclusion
Substance use disorders during pregnancy are common – in 2012, a large survey indicated that in the USA approximately 6% of pregnant women used illicit drugs, 8.5% drank alcohol, and 16% smoked cigarettes [31]. In addition to the risks discussed above, women with substance use disorders during pregnancy are more likely to receive inadequate prenatal care, have poor nutrition, experience poverty and domestic violence, and have comorbid psychiatric illness [32] – all of which should be screened for during the emergency department visit in addition to treatment of acute medical conditions related to substance use.
An encounter in the emergency department offers enormous potential for identifying at-risk pregnant women struggling with substance use disorders, and engaging them in treatment. Given that many of these patients experience shame and guilt about their use, and with the awareness that some will avoid medical or addiction treatment as a result, the ED provider has an opportunity to offer a nonjudgmental introduction to treatment. Some women will also avoid care due to concerns about legal ramifications, not without reason. It is important as a provider to have a familiarity with relevant state laws regarding substance use during pregnancy – some states have declared substance use during pregnancy to be child abuse under civil child welfare statutes, and a few states consider substance use as grounds for civil commitment of pregnant women; some states also require providers to report suspected prenatal drug use [33]. While these laws may be intended to protect the fetus and possibly compel maternal treatment, they often pose yet another challenge for the provider in developing rapport and trust with the patient at a time when the treatment relationship is perhaps needed most.
Overall, goals in the emergency department treatment of a pregnant patient with a substance use disorder include safely managing acute intoxication/withdrawal; engaging the patient with a nonjudgmental empathic approach; screening for comorbid medical, psychiatric, and social problems; and connecting the patient to ongoing addiction care.
References
Center for Substance Abuse Treatment. Substance abuse treatment for persons with co-occurring disorders. Treatment Improvement Protocol (TIP) Series 42. DHHS Publication No. (SMA) 05-3922. Rockville: Substance Abuse and Mental Health Services Administration; 2005.
Wilson J, Thorp Jr. J. Glob libr women’s med, (ISSN: 1756-2228) 2008. https://doi.org/10.3843/GLOWM.10115.
Whitlock EP, Polen MR, Green CA, Orleans T, Klein J, U. S. Preventive Services Task Force. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):557–68.
Stinson FS, Grant BF, Dawson DA, Ruan WJ, Huang B, Saha T. Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2005;80(1):105–16. https://doi.org/10.1016/j.drugalcdep.2005.03.009.
World Health Organization (WHO). Guidelines for the identification and management of substance use and substance use disorders in pregnancy. Geneva: World Health Organization (WHO); 2014.
Bertrand J, Floyd RL, Weber MK, O’Connor M, Riley P, Johnson KA, Cohen DE, National Task Force on FAS/FAE. Fetal alcohol syndrome: guidelines for referral and diagnosis. Atlanta: Centers for Disease Control and Prevention; 2004.
Bellantuono C, Tofani S, Di sciascio G, Santone G. Benzodiazepine exposure in pregnancy and risk of major malformations: a critical overview. Gen Hosp Psychiatry. 2013;35(1):3–8.
Chisolm MS, Payne JL. Management of psychotropic drugs during pregnancy. BMJ. 2016;532:h5918.
National Guideline Clearinghouse (NGC). Guideline summary: Guidelines for the identification and management of substance use and substance use disorders in pregnancy. In: National Guideline Clearinghouse (NGC) [Web site]. Rockville: Agency for Healthcare Research and Quality (AHRQ); 2014 Jan 01. Available: https://www.guideline.gov.
McElhatton PR. The effects of benzodiazepine use during pregnancy and lactation. Reprod Toxicol. 1994;8(6):461–75.
National Institute on Drug Abuse. Trends & Statistics. Retrieved from https://www.drugabuse.gov/related-topics/trends-statistics on 28 Aug 2016.
Passey ME, Sanson-Fisher RW, D’Este CA, Stirling JM. Tobacco, alcohol and cannabis use during pregnancy: clustering of risks. Drug Alcohol Depend. 2014;134:44–50.
Marijuana use during pregnancy and lactation. Committee Opinion No. 637. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2015;126:234–8.
van Gelder MM, Reefhuis J, Caton AR, Werler MM, Druschel CM, Roeleveld N, National Birth Defects Prevention Study. Characteristics of pregnant illicit drug users and associations between cannabis use and perinatal outcome in a population-based study. Drug Alcohol Depend. 2010;109:243–7.
Maeda A, Bateman BT, Clancy CR, Creanga AA, Leffert LR. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology. 2014;121(6):1158–65.
Wilder CM, Winhusen T. Pharmacologic management of opioid use disorder in pregnant women. CNS Drugs. 2015;29(8):625–36.
Forray A, Foster D. Substance use in the perinatal period. Curr Psychiatry Rep. 2015;17:91.
The American College of Obstetricians and Gynecologists (ACOG): Committee Opinion. Opioid Abuse, Dependence, and Addiction in Pregnancy. 2014. Number 524.
Mozurkewich EL, Rayburn WF. Buprenorphine and methadone for opioid addiction during pregnancy. Obstet Gynecol Clin N Am. 2014;41(2):241–53.
Noormohammadi A, Forinash A, Yancey A, Crannage E, Campbell K, Shyken J. Buprenorphine versus methadone for opioid dependence in pregnancy. Ann Pharmacother. 2016;50(8):666–72.
Zedler BK, Mann AL, Kim MM, Amick HR, Joyce AR, Murrelle EL, et al. Buprenorphine compared with methadone to treat pregnant women with opioid use disorder: a systematic review and meta-analysis of safety in the mother, fetus, and child. Addiction. 2016;111:2115. https://doi.org/10.1111/add.13462. [Epub ahead of print].
D’Apolito K. Breastfeeding and substance abuse. Clin Obstet Gynecol. 2013;56(1):202–11.
Bagley SM, Wachman EM, Holland E, Brogly SB. Review of the assessment and management of neonatal abstinence syndrome. Addict Sci Clin Pract. 2014;9(1):19.
Young JL, Martin PR. Treatment of opioid dependence in the setting of pregnancy. Psychiatr Clin N Am. 2012;35(2):441–60.
Kwiatkowski MA, Roos A, Stein DJ, Thomas KG, Donald K. Effects of prenatal methamphetamine exposure: a review of cognitive and neuroimaging studies. Metab Brain Dis. 2014;29(2):245–54.
Ladavac AS, Dubin WR, Ning A, Stuckeman PA. Emergency management of agitation in pregnancy. Gen Hosp Psychiatry. 2007;29(1):39–41.
Rayburn WF, Bogenschutz MP. Pharmacotherapy for pregnant women with addictions. Am J Obstet Gynecol. 2004;191(6):1885–97.
The American College of Obstetricians and Gynecologists (ACOG): Committee Opinion. Smoking Cessation During Pregnancy. 2010. Number 471.
Coleman T, Chamberlain C, Davey MA, Cooper SE, Leonardi-Bee J. Pharmacological interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev. 2015;(12):CD010078.
Berard A, Zhao JP, Sheehy O. Success of smoking cessation interventions during pregnancy. Am J Obstet Gynecol 2016. pii: S0002-9378(16)30432-X. https://doi.org/10.1016/j.ajog.2016.06.059. [Epub ahead of print].
Forray A. Substance use during pregnancy. F1000Res. 2016;5:F1000 Faculty Rev-887.
Gopman S. Prenatal and postpartum care of women with substance use disorders. Obstet Gynecol Clin N Am. 2014;41(2):213–28.
McLafferty LP, Becker M, Dresner N, Meltzer-Brody S, Gopalan P, Glance J, et al. Guidelines for the management of pregnant women with substance use disorders. Psychosomatics. 2016;57(2):115–30.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Baker, A.S., Hogan, C.S. (2019). Emergency Management of Substance Use in Pregnant Patients. In: Donovan, A., Bird, S. (eds) Substance Use and the Acute Psychiatric Patient. Current Clinical Psychiatry. Humana, Cham. https://doi.org/10.1007/978-3-319-23961-3_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-23961-3_13
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-319-23960-6
Online ISBN: 978-3-319-23961-3
eBook Packages: MedicineMedicine (R0)