Abstract
Over the last 30 years, numerous patient registries in pulmonary arterial hypertension (PAH) have been conducted primarily in the United States and Western Europe. The registries provide extensive information about this rare and deadly disease. In addition, survival estimates and risk factors associated with mortality have been spotlighted. Several predictive equations have been generated from these large registries, such as the National Institutes of Health, French National, Pulmonary Hypertension Connection, and REVEAL. These equations have been designed to forecast survival of PAH cohorts and have been useful tools in clinical research. Adding to this experience, the REVEAL survival equation and risk calculator have been shown to reliably predict short-term survival of individual PAH patients. But, several factors, including regional differences in PAH sub-populations, access to care and a rapidly evolving therapeutic approach, limit the usefulness of these predictive equations in routine clinical practice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Pulmonary arterial hypertension (PAH) is a rare and incurable disease with an estimated prevalence of 10–25 cases per million. As a consequence of chronically elevated right ventricular afterload, patients develop progressive right-sided heart failure, which is the primary mode of death. Many advances have been appreciated with PAH during the last three decades, thanks to improved awareness, more refined classification schemes, better understanding and management of right-sided heart failure and, most importantly, the availability of numerous PAH-specific therapies.
During this period, many observational registries have been conducted in different parts of the world, providing a global perspective of this rare disease. These efforts have characterized the presentation of PAH, documented the changing phenotype of PAH patients, updated survival rates and identified predictors of death. Some registries have also developed predictive equations that estimate survival rates; and when eventually validated, could assist clinicians with patient assessment and clinical decision-making.
In this chapter, some general aspects of patient registries will be introduced, followed by a review of some of the major PAH registries conducted in the last 30 years, emphasizing observations on survival and associated risk factors. Discussion will center on several predictive equations developed from four different large registries – National Institutes of Health (NIH), French National, Pulmonary Hypertension Connection (PHC), and Registry to Evaluate Early and Long-term Pulmonary Arterial Hypertension Disease Management (REVEAL). Next, the challenges of applying these predictive equations in clinical practice will be covered. Lastly, lessons learned from PAH registries and survival equations, as they pertain to improving the allocation of lungs for transplantation of PAH patients, will be introduced.
Observational Patient Registries
Registries provide information about a select group of patients, who ideally, represent individuals with similar disease characteristics in the general population. A major aim of clinical registries is to provide information about the natural history and prognosis of the patient cohort. Such registries have high generalizability and are especially useful for characterizing populations, assessing the burden of illness, and developing prognostic models [1, 2]. However, the observational nature of registries means that there is neither randomization nor a rigorous way to compare effectiveness of therapies, and it is difficult to account for confounding variables [3]. Furthermore, there are no hypotheses at the initiation of a registry, but the breadth of clinical information collected makes registries a rich medium for generating new hypotheses.
Registries can be used to complement randomized controlled trials in determining outcomes. The Effective Health Care Program of the Agency for Healthcare Research and Quality defines a patient registry as “an organized system that uses observational study methods to collect uniform data (clinical and other) to evaluate specified outcomes for a population defined by a particular disease, condition or exposure and that serves a predetermined scientific, clinical or policy purpose(s)” [1]. Registries describe the natural history of the disease and can help determine clinical effectiveness. The European Medicine Agency also defines registry as “an organized system that uses observational methods to collect uniform data on specified outcomes in a population defined by a particular disease, condition or exposure” [4].
Registries examine the epidemiology of prevalent or incident cases. Prevalent cases comprise individuals who have previously been diagnosed. The term incident refers to cases that are newly diagnosed during a pre-defined time period. Generally, patients are considered incident on the day of diagnosis and prevalent the following day [3]. But, registries can differ even in their definition of incident and prevalent cases. Methodological differences can account for some variation in incidence and prevalence across registries. For example, the allowable time elapsed between the diagnostic right heart catheterization (RHC) and enrollment in a registry can vary when differentiating an incident from a prevalent case. Prevalent patients are enrolled after enduring the disease for varying periods of time. This may lead to underestimation of true mortality since the sickest patients may have already died and not had the opportunity to be enrolled, while less severely affected patients survive the pre-enrollment period to become eligible for a registry. In essence, patients who die before study initiation are precluded from enrollment and patients who survive to study initiation are included, leading to an immortal time bias, which is a form of survivor bias that potentially inflates survival estimates. If the mortality rate for a condition were constant over time, as might be encountered in a natural history study of a condition without any available interventions, then the differentiation between prevalent and incident cases may not impact the estimation of mortality. But active treatment of PAH patients through management of right ventricular failure and PAH-specific medications, has impacted survival for many, but not all, individuals. Therefore, it is important to understand if a particular registry includes incident and prevalent cases because information derived from incident cases may not be generalizable to prevalent patients and vice versa.
Each registry defines specific inclusion and exclusion criteria. Although there are no standard inclusion and exclusion criteria amongst registries, the goal is to maximize generalizability, identify clear objectives for data collection, and minimize bias [2, 3]. These criteria vary depending on the objective of the registry, such as evaluating only Idiopathic Pulmonary Arterial Hypertension (IPAH) or including PAH associated with other conditions as most modern PAH registries have done (Table 20.1). The definition of PAH and World Health Organization (WHO) classification of PAH has evolved over time, leading to modifications in the inclusion-exclusion criteria across registries in different eras. For example, the NIH registry used a PAWP ≤ 12 mmHg with a PAP > 25 mmHg; whereas the REVEAL registry used a pulmonary arterial wedge pressure (PAWP) or left ventricular end-diastolic pressure (LVEDP) ≤ 18 mmHg as an inclusion criteria [5, 6]. And even though RHC is the gold standard for diagnosis, some have used echocardiographic measurement of pulmonary pressures for diagnosis as RHC may be infrequently performed within a region [7]. These factors are important to recognize when applying the results of a particular registry to another patient population.
Another key distinguishing design aspect of registries is the method of data collection – prospective, retrospective, or a mixture of the two. Clearly prospective and standardized data collection is superior, in order to minimize biases and missing or inaccurate data, but requires a much greater investment in time and resources.
PAH Registries
PAH Registries have a number of distinguishing characteristics, including the population recruited, the method of data collection, allowance of prevalent patients, era and region of data collection, timing of diagnosis, and period of observation. Table 20.1 displays the major PH registries conducted during the last 30 years. Starting with the landmark NIH registry of the early 1980s, PAH registries have been analyzed across the globe, allowing for comparison between populations in different eras and regions [3]. Important prognostic information has also been obtained. Systematic clinical surveillance of PAH is important especially as the field advances the knowledge of pathophysiology and therapeutics. Registries have importantly identified the changing phenotype of PAH over time. The continual reassessment of patient demographics and survival are essential in the aging population and in the ever-changing climate of improved PAH targeted therapies. New assessments of survival in the modern era helped develop predictive survival equations. Furthermore, epidemiological data and practice patterns from different countries with diverse healthcare systems and variable availability to expert centers and drugs provide a more widespread view of the current management of PAH.
Several registries that are either historically relevant or provide vital survival data in PAH will be spotlighted, including ones that have generated equations for predicting survival [5, 6, 8–13]. Fundamental information about other registries, from China, Switzerland, United Kingdom-Ireland, and the United States (PAH-QuERI) are also listed in Tables 20.1 and 20.2 [7, 14–18].
National Institutes of Health (NIH) Registry
The Patient Registry for the Characterization of Primary Pulmonary Hypertension was the first national registry [5]. This landmark registry, sponsored by the NIH, began in 1981 and prospectively collected clinical data on 194 patients from 32 centers in the United States with primary pulmonary hypertension (corresponding to idiopathic PAH in recent classification schemes), familial PAH (now heritable PAH), or anorexigen-induced PAH. Prior to the registry, there were many questions regarding the epidemiology and natural history of the disease. Data were collected on patients prospectively according to standardized protocol from July 1981 to Sept 1985 and patients were followed through August 1988. The registry did not address prevalence of PAH. Pulmonary hypertension was defined by catheterization as a mean pulmonary arterial pressure of >25 mmHg at rest or >30 mmHg with exercise. Primary pulmonary hypertension was only diagnosed after exclusion of other potential causes of pulmonary hypertension, including collagen vascular disease and elevated left-sided filling pressures, defined as pulmonary capillary wedge pressure >12 mmHg. Demographic data, hemodynamic measures, pulmonary function, and gas exchange variables were obtained at baseline and assessed at 6-month intervals.
There were 187 patients with mean age of 36 ± 15 years with a female to male ratio of 1.7:1. Five percent had a history of appetite suppressant use and 6 % were familial pulmonary hypertension. Female patients tended to have more severe symptoms at presentation with 75 % being in New York Heart Association (NYHA) functional class III or IV compared with 64 % of male patients. The median time from onset of symptoms to diagnosis was 2.0 ± 4.9 years (median 1.27). This landmark registry helped correlate hemodynamic findings to severity of symptoms and survival. As expected, patients with NYHA functional class III or IV symptoms had higher mean pulmonary artery pressures, higher right atrial pressures and lower cardiac indices compared to less symptomatic patients. By the time of diagnosis, the clinical and hemodynamic findings were advanced in most cases.
The NIH registry also characterized mortality and identified factors associated with survival for this select group of PAH patients. Because only incident cases were recruited and catheterizations were part of the initial evaluation, the date of diagnostic catheterization served as the baseline from which survival was measured. The estimated median survival was 2.8 years [19]. Variables associated with poor survival included NYHA functional class III or IV, presence of Raynaud’s phenomenon, elevated right atrial pressure (RAP), elevated mean pulmonary artery pressure (PAP), decreased cardiac index (CI) and decreased diffusing capacity (of the lung) for carbon monoxide (DLCO) (Table 20.3). Estimated survival rates at 1-, 3- and 5-years were 68 %, 48 % and 34 % respectively. By the end of the registry, 106 of the 194 patients had died, including 26 % with sudden or unexpected death and 47 % from right ventricular failure. Symptom duration did not correlate with disease severity implying that disease progression differs among patients. Of the 36 patients (19 %) receiving long-term (non PAH-specific) medication at study entry, there was no significant difference in survival time compared with patients not receiving therapy. However, the design of the study did not allow for valid assessment of differences in therapeutic interventions. This study certainly confirmed the poor prognosis of patients with pulmonary arterial hypertension.
The NIH registry gave the first national characterization of a rare disease with detailed evaluation of symptoms, laboratory, imaging and hemodynamic findings as well as providing prognostic indicators. This registry provided the foundation for subsequent studies of PAH.
French National Registry
The French National Registry is considered the first PAH registry in the modern treatment era. Disease-specific therapies were absent at the time of the NIH registry and the classification of pulmonary hypertension had changed since the late 1980s. In the nearly two decades since the NIH registry, prostanoids, endothelin receptor antagonists (ERA) and phosphodiesterase-5 (PDE5) inhibitors became specifically available for PAH. Despite these significant advances, there had not been a large-scale, national-level registry to update clinical and hemodynamic parameters of patients, prevalence of the disease or estimates of survival.
The prospective registry included 17 university hospitals with a total of 674 patients (121 incidence cases, 553 prevalent cases) through the French Network on PAH with 3-year follow-up [10]. Adult PAH patients, including idiopathic, familial, anorexigen-induced, or PAH associated with CTDs, congenital heart diseases (CHD), portal hypertension and HIV were seen between October 2002 and October 2003. Diagnosis was considered to be the time of RHC, which was a pre-requisite for enrollment. Because prevalent cases were catheterized before study entry, Humbert et al. accounted for immortal time bias by using survival estimates and a Cox proportional hazards model from the time of diagnosis. In addition, prevalent cases were entered into the risk set in delayed fashion (i.e. left truncation), by the same amount of time that had elapsed between diagnostic catheterization and registry entry. For example, if 12 months had elapsed between an individual’s diagnostic catheterization and recruitment into the registry, that individual’s subsequent time alive in the registry and contribution to the cohort’s survival estimate did not begin until the 12 month point of the cohort’s survival curve and was not included in the first 12 months. There were also 121 incident cases (newly diagnosed), who were patients diagnosed during the registry’s recruitment phase and none of these patients were lost to follow-up.
Mean age was 50 ± 15 years, much older than in the NIH registry due to a more diverse group of enrolled PAH patients; female to male ratio was 1.9. The delay between the onset of symptoms and diagnosis was still 27 months. At diagnosis, 75 % of patients had NYHA functional class III or IV symptoms. Hemodynamic evaluation demonstrated severe compromise with RAP 8 ± 5 mmHg, mean PAP 55 ± 15 mmHg and pulmonary vascular resistance index 20.5 ± 10.2 WU · m2 with correlation to the NYHA functional class. IPAH comprised 39.2 % of patients and familial cases represented 3.9 % of the population. At that time, epoprostenol, bosentan, iloprost and sildenafil were the available approved therapies. No mandatory specific treatment algorithm was used; thus, use of PAH targeted therapies was at the discretion of the treating physician.
Prevalence in France was calculated to be 15.0 cases per million adults, although a significant range (5–25 cases per million population) was noted across regions of the country. Unfortunately, this registry identified that despite the increased awareness of PAH since the NIH registry 20 years prior, patients were still being diagnosed with clinical impairment as severe as during the time of the NIH registry.
The French PAH network followed patients for 3 years after study entry and demonstrated 1-, 2- and 3- year survival of 87 %, 76 % and 67 %, respectively in the overall cohort [20]. In a combined incident and prevalence (i.e. diagnosed <3 years from study entry) cohort of idiopathic, familial and anorexigen-associated PAH cases, survival for 1-, 2-, and 3-year survival rates were slightly lower, 83 %, 67 % and 58 % respectively, but still considerably better than NIH registry’s estimates [19]. The prevalent patients with idiopathic, familial and anorexigen associated PAH had higher survival rates than incident patients. Even though the registry made efforts to eliminate survivor bias (as described earlier), this finding may still reflect such a bias. There was better 3-years survival rate in patients with congenital heart disease, but poorer survival in CTD; these observations were subsequently confirmed by the REVEAL registry [21]. Multivariate analysis identified female sex, higher six minute walk distances, and higher cardiac output at time of diagnosis as independent prognostic factors for survival (Table 20.3).
Pulmonary Hypertension Connection (PHC) Registry
The Pulmonary Hypertension Connection registry (PHC) was a large U.S. based registry conducted at three sites by essentially one group of researchers. From 1982 to 2006, 578 patients with WHO Group 1 Pulmonary Arterial Hypertension were included [8]. The goal was to define clinical characteristics and prognosis of WHO Group 1 PAH patients and compare groups by etiology and across treatment eras.
Patients were segregated into prevalent (1982–2004) versus incident (2004–2006) groups, with only the latter group’s data being collected prospectively. Patients were also compared by treatment era: pre-1996 (before approved therapies), 1996–2002 (only IV epoprostenol) and post-2002 (IV, subcutaneous or inhalational prostacyclins, ERAs and PDE5 inhibitors). Seventy-seven percent of the PHC cohort was female, confirming again the female predominance of PAH; the only subgroup without female predominance was Human Immunodeficiency Virus (HIV) -associated PAH. The PHC registry again recognized that patients with PAH are referred to specialty centers far into the disease course, as 80 % of patients had NYHA functional class III or IV symptoms at presentation.
PHC included all types of Group 1 PAH patients, including 44 % idiopathic, 4 % heritable PAH (HPAH) and 3 % anorexigen, along with several associated PAH groups – 30 % CTD, 11 % CHD, 7 % porto-pulmonary hypertension and 1 % HIV-associated PAH. These frequencies were similar to the French registry, but differed from the NIH registry which only included IPAH, HPAH and anorexigen-related PAH. Compared with other subgroups, patients with connective tissue disease (CTD) had more severe disease: poorer exercise capacity, a worse functional class, a higher mean PAP, higher pulmonary vascular resistance (PVR) and lower CI. Meanwhile, higher functional class, better exercise capacity, lower mean PAP, lowered PVR and higher CI were seen with porto-pulmonary hypertension and congenital heart disease (CHD) -associated PAH.
For the entire cohort, median survival time was 3.6 years. The 1-, 3-, and 5- year survival rates were 84 %, 67 % and 58 %, respectively. The 1-year survival for the incident cohort was 85 %, which is similar to the French registry (88 % 1 year survival) but improved from NIH registry [10, 19]. Using Cox proportional hazards analysis, increasing age, CTD as the etiology for PAH, higher functional class, higher RAP and lower CI were identified as significant and independent predictors of mortality (Table 20.3) [22]. In essence, PHC confirmed some of the NIH findings but once again highlighted how advancements in care had improved survival.
Scottish Registry
The Scottish registry described the epidemiologic features of PAH in a population over a prolonged period of time (1986–2001), by reporting data from the Scottish Morbidity Record (SMR) and the Scottish Pulmonary Vascular Unit (SPVU) [11]. This retrospective population cohort study used records from a national hospitalization database for Scotland; the SMR relied on systematic coding of hospital admissions and assembled a cohort of 374 incident patients, aged 16–65 years with diagnosis of IPAH, CTD-PAH or CHD-PAH. The overall population prevalence was 52 cases per million. The median survival of incident patients with IPAH was 3.8 years in females and 5.6 years in males, which is contrary to the poorer survival in male patients in the NIH, French, PHC and REVEAL registries [8, 19, 20, 23]. These lengthier survival times cast doubt on the PAH diagnosis in some of the patients from the SMR group.
The incidence and prevalence was also examined from the SPVU (1997–2005), which is a national specialist center for PAH management and is responsible for diagnosis and treatment of all cases of PAH in Scotland. All patients with PAH were diagnosed by standardized protocol, including RHC. The prevalence was 26 cases per million adult inhabitants.
The Scottish registry collected epidemiologic data from two perspectives. The SMR identified patients simply by ICD-9 code. The accuracy of the diagnosis was not confirmed by standardized protocol, like the SPVU data. As a result, there was a lower prevalence of PAH from the SPVU than from the SMR analysis (52 versus 26 cases per million adult inhabitants). Even though the data from SMR represents a survey of inexpert diagnoses, it still suggests that registries conducted at specialized centers may underestimate prevalence rates due to numerous challenges precluding some individuals from being evaluated at distant expert-based referral centers. In addition, the lower prevalence rate from SPVU is still significantly higher than the French National Registry (26 versus 15 cases per million) [10]. Considering these two large national experiences, differences in prevalence likely exist in various regions of the world, but also depend on the method of case identification and data collection [24].
Spanish Registry of PAH (REHAP)
The Spanish Registry of Pulmonary Arterial Hypertension (REHAP) examined the prevalence, incidence and survival of PAH and chronic thromboembolic pulmonary hypertension (CTEPH) in Spain from January 1998 to June 2008 [12]. One of its objectives was to assess the applicability of recently developed predictive equations (for survival). Demographic, functional and hemodynamic variables were evaluated in 866 PAH and 162 patients with CTEPH. Patients were diagnosed as incident if diagnostic RHC took placed within 6 months of the Registry’s inception. PAH prevalence was estimated to be 16 cases per million. The prevalence for CTEPH was only 3.2 cases per million. With incident PAH cases, the delay between the onset of symptoms and diagnosis was 2.2 years and in previously diagnosed patients was 3.7 years, possibly suggesting some improvement in disease awareness over the period of the recruitment. Sixty-nine percent of patients in the PAH group were in WHO functional class III or IV, which was similar to the 77 % of the CTEPH group. Interestingly, only 30 % of CTEPH patients underwent pulmonary thromboendarterectomy, the treatment of choice for CTEPH. This was also the first registry to describe pulmonary veno-occlusive disease (PVOD) within a larger PAH cohort. PVOD only made up 1.5 % of the cohort and prevalence was estimated to be 0.16 cases per million adults; but the authors speculated an underestimation of true prevalence. Patients with PVOD had more severe hypoxemia, lower DLCO, absence of vasodilator response and poorer survival compared with patients with IPAH.
Observed survival at 1- and 3- years was 87 % and 75 %, respectively with no significant differences between the PAH and CTEPH cohorts. Corresponding survival in IPAH patients was 89 % and 77 % at 1- and 3- years respectively. In multivariate analysis, PAH associated with connective tissue disease, portal hypertension and pulmonary veno-occlusive disease were independently associated with death. Again, males, higher WHO functional class, higher mean RAP and lower CI were also independent predictors of death in PAH (Table 20.3). As defined in their objectives, Spanish investigators explored the accuracy of predictive equations from NIH, PHC, French National and REVEAL. While estimates from the PHC equation fit fairly well with the REHAP observations, significant differences between projected and observed survival were noted with the NIH, French, and REVEAL equations.
Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL)
REVEAL is the largest PAH registry to date and provided updated WHO Group 1 patient demographics in the U.S. The observational REVEAL registry also characterized the landscape of PAH in the modern era, by enrolling ~3500 patients from 54-centers between 2006 and 2009 [6]. Of note, the publication of REVEAL was prior to the fourth World Symposium on Pulmonary Hypertension; therefore, PAH was diagnosed based on criteria from third World Symposium on Pulmonary Hypertension (i.e. mean PAP > 25 mmHg at rest or >30 mmHg with exercise; PAWP or LVEDP ≤ 15 mmHg and PVR > 240 dyne/s/cm5).
Importantly, REVEAL only included 14 % recently-diagnosed (incident) cases, whereas 86 % were previously-diagnosed (prevalent) patients, most of whom were already receiving PAH-specific treatment at enrollment. Patients must have been diagnosed by catheterization, but REVEAL did expand the PAWP cut-off for enrollment to 18 mmHg. The higher PAWP facilitated enrollment of a more typical ‘real-world’ population of PH patients, thus separating it from previous registries.
REVEAL explored questions of whether population demographics in the current era differ from those encountered in previous registries. The registry included 2,955 patients with IPAH, HPAH and PAH- associated with other disorders, in contrast to the NIH registry. Prospectively collected data illustrated an older cohort (mean age at diagnosis 47 years) with an even greater female predominance (3.6:1) compared to the NIH registry (mean age 36 years and 1.7:1 female to male ratio). Compared to the French registry, the REVEAL cohort had a higher percentage of obesity (32.5 % versus 14.8 % with body mass index ≥ 30 kg/m2) [25]. REVEAL also recruited a larger percentage of anorexigen-related PAH than the NIH or French registries (15.3 % versus 5 % versus 9/5 %, respectively), which may reflect the increasing obesity epidemic in the United States, availability of anorexigen compounds in the 1990s and the potential latent effects of anorexigen exposure on PAH pathogenesis. Hemodynamic parameters at time of diagnosis had not changed significantly since the NIH registry. Despite increased physician awareness, there was little change in severity of PAH at time of diagnosis: 72 % classified as being in NYHA functional class III/IV similar to the 70–80 % range of other registries, including NIH. REVEAL essentially followed a large cohort of diverse PAH patients in the modern treatment era.
Survival in REVEAL was determined from the date of the diagnostic catheterization, similar to the French National Registry. Immortal time bias was also addressed in a manner similar to the French National Registry, i.e. left-truncation of prevalent cases during survival analysis. But unlike the French National Registry, REVEAL investigators incorporated factors for their multivariable predictor analysis from the time of registry enrollment and not the time of diagnosis (or catheterization) [6, 10, 23, 26]. One-, 3-, 5- and 7- year survival estimates were 85 %, 68 %, 57 % and 49 % respectively. In addition, survival in the IPAH/HPAH subset, which was matched to NIH registry entry criteria, was 91 %, 74 %, 65 % and 59 % at 1-, 3-, 5-, 7- years, which was considerably higher at all time points than the projected survival from the NIH equation [26]. REVEAL identified 19 prognostic variables, some favorable and some unfavorable, such as sub-type of PAH, age, PVR, RAP, renal insufficiency, resting systolic blood pressure, resting heart rate, brain natriuretic peptide, presence of pericardial effusion and DLCO. Similar to the French registry, sex, functional class and 6-minute walk distance were significant predictors (Table 20.3) [23]. It is noteworthy that PVR, and not mean PAP or cardiac output was a significant predictor of survival; even though PVR is a derived measure (i.e. the ratio of pressure and flow) with potential for inaccuracy in certain clinical condition such as a low cardiac output state, severe tricuspid regurgitation, etc.
Mayo Clinic Registry
The Mayo Clinic registry prospectively evaluated 484 patients with WHO group 1 pulmonary hypertension from January 1995 to December 2004 followed at the Mayo Clinic pulmonary hypertension specialty clinic in Rochester, MN [9]. The objective was to evaluate survival patterns in patients with PAH and establish clinical and hemodynamic prognostic factors. Unlike other modern registries, only newly diagnosed or incident cases were included. The time of diagnosis was the date of evaluation by the PH physician and generally corresponded to the date of the pre-requisite heart catheterization. The mix of PAH patients was broad and similar to other contemporary registries, including 56 % percent idiopathic, familial or anorexigen-related PAH, 24 % PAH associated with CTD and remaining 20 % were congenital systemic to pulmonary shunts, portal hypertension and HIV. Mean age was 52 years and similar for men and women. The mean disease duration from onset of symptoms to Mayo Clinic evaluation was 1.8 years. Seventy-one percent of patients were in NYHA functional class III/IV. Patients with CTDs were older, predominately female, exhibited greater markers of disease severity and worse hemodynamic parameters than IPAH patients.
Overall cohort’s mean survival was 4.56 years with 1-, 3-, and 5-year survival rates of 81.1 %, 61.1 %, 47.9 %, respectively. Males had a poorer prognosis and mortality increased by 27 % with every decade of increasing age. Patients with PAH associated with CTD had two-fold higher risk of death compared to other PAH sub-groups. Higher WHO functional class, lower CI and higher RAP were associated with mortality. Renal insufficiency (serum creatinine level >1.5 mg/dL) was also associated with a higher mortality rate. Interestingly, the Mayo Registry showed that survival predictions were enhanced when the functional class was supplemented by additional factors, such as demographics and objective measures (i.e. labs, 6MW distance, pulmonary function testing, echocardiogram, and heart catheterization) (Table 20.3).
Comparative, Prospective Registry of Newly Initiated Therapies for Pulmonary Hypertension (COMPERA)
COMPERA is an ongoing European registry started in July 2007. A total of 1283 PAH patients, including 800 IPAH, have been enrolled from 41 pulmonary hypertension centers from 7 European countries (Germany, Belgium, Netherlands, Italy, Austria, Switzerland, and United Kingdom) [13, 27]. All patients were newly diagnosed with PAH and no one diagnosed prior to May 2007 was entered. Interestingly, median ages of the entire cohort (68 years [IQR 55–75]) and the IPAH/HPAH/drug-associated subgroups (71 years [IQR 55–87]) were considerably higher than other historic or even contemporary registries, which in part reflects the changing demographics of the PAH population or that COMPERA may also be including patients with heart failure with preserved ejection fraction (Group 2 PH) rather than traditional PAH (or Group 1 PH) patients. The registry also evaluated initial PAH treatment and found that the majority of patients received PDE5 inhibitors (58 %). Forty-four percent of patients were treated with ERAs and 2 % of patients were receiving prostacyclin analogues. Forty-five percent of patients were treated with combination therapy during follow-up. In multivariable analysis, males, increasing age and NYHA functional class IV were independent predictors of poor prognosis in IPAH (Table 20.3). COMPERA also utilized registry data to compare survival rates in patients with IPAH and other forms of PAH stratified by the use of anticoagulation [27].
Considering all these registries collectively, several points and trends are apparent. PAH remains a very serious and lethal condition with the majority of patients being in functional class III or IV at the time of diagnosis. PAH afflicts women much more than men. The largest PAH sub-groups remain IPAH and CTD-PAH. The mean age of PAH cohorts has increased considerably, partly due to inclusion of a more heterogeneous patients, but perhaps also because of a burgeoning group of older individuals diagnosed with IPAH. The severity of initial cardiopulmonary hemodynamics has changed very little over time. Consistent and significant predictors of survival include demographic factors (age, males), hemodynamics (RAP, CI) and functional assessments (NYHA or WHO functional class, 6MW distance). In particular CTD-PAH and porto-pulmonary PAH patients have the poorest survival. Most importantly, survival from the registries has improved over time, presumably due to the availability of PAH-specific therapies; but a significant caveat is the inclusion of prevalent patients into registries and the resulting impact of immortal time bias.
Survival Prediction and Prognosis
One potential use of registry data is to develop risk equations that predict mortality or, stated differently, forecast survival. Ideally, a predictive equation should have broad applicability to diverse patients with the same diagnosis and at different times in an individual’s course. And, since some components of an equation may not be available, the equation should still be usable in the face of some missing data. An equation should exhibit good calibration for estimating survival in cohorts of patients. But for clinical practice, a survival equation also needs to reliably discriminate between survivors and non-survivors.
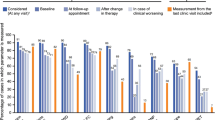
PAH registries have generally collected a wide range of clinical data, including demographics, physiologic variables (e.g. right-heart catheterization data, DLCO), laboratory measurements (e.g. BNP), and co-morbidities. These data have then been used to create multivariate equations for predicting survival. The NIH and PHC equations are based entirely on the hemodynamic parameters mean PAP, mean RAP, and CI [5, 8, 19, 22]. By contrast, the French survival equation also included 6 MW distance and sex along with the cardiac output [10, 20]. The REVEAL equation also includes hemodynamic measures, but instead of the mean PAP or cardiac output, PVR and mean RAP were incorporated. Importantly, the REVEAL equation also factors in numerous non-hemodynamic variables, including demographics, etiologies of PAH, functional class, laboratory markers, renal insufficiency and presence of a pericardial effusion among others; all items were found to be significant to the model through a multivariate Cox proportional hazards analysis (Table 20.4) [21, 23, 28]. Additional details of the four equations, efforts at their validation, and their respective strengths and weaknesses are described below and summarized in Table 20.5.
NIH Equation
As noted earlier, the NIH registry enrolled patients with IPAH in an era before modern therapies for pulmonary hypertension were available. This model was developed by multivariate regression analysis of the variables that independently predicted mortality. Estimated percentages of patient survival at 1, 3, and 5 years using this equation are 68 %, 48 %, and 34 %, respectively [19].
-
P (t) indicates the patient’s chances of survival and t = 1, 2 or 3 years
-
x = mean pulmonary artery pressure
-
y = mean right atrial pressure
-
z = cardiac index
Sandoval et al. demonstrated good correlation between survival estimates from the NIH equation and observed survival in an external cohort of IPAH patients from Mexico in essentially the same treatment era as the NIH registry. The NIH equation appeared to have greater accuracy when applied to the sub-group of patients that were not acutely responsive to vasodilators [29]. A number of clinical trials have subsequently utilized NIH equation-predicted survival as the comparator to the observed survival on that specific medication [14, 30–34]. But when applied to more contemporary cohorts, the NIH equation has underestimated survival, even when limited to cohorts of IPAH, HPAH and anorexigen patients [14, 23, 35, 36]. This has been attributed to change in awareness, updated management strategies, availability of PAH-specific therapies, and possibly a change in the phenotype of pulmonary hypertension [3]. Improvements to the NIH equation have been proposed from data collected by recent PH registries [22, 35].
French National Registry Equation
Although the French National Registry included patients with all types of Group 1 PAH, the equation was developed from a subset of incident and prevalent cohorts (diagnosed less than 3 years before enrollment) with idiopathic, familial or anorexigen-associated PAH (n = 190 – 56 incident and 134 prevalent), and importantly left out patients with CTD, congenital heart disease, portal hypertension, and HIV [10, 20]. This subset of patients was chosen to better control for the presence or absence of associated conditions that would independently affect mortality. For this PAH subgroup, 1-, 2-, and 3- year survival was 83 %, 67 % and 58 % respectively. The French equation included factors which independently influenced survival as determined by the multivariate regression model. Probability of survival with this equation is estimated as:
-
t = time since diagnosis
-
x = 6MWD at diagnosis
-
y = 1 if female, y = 0 if male
-
z = cardiac output at diagnosis
The French registry has been prospectively validated and shown to have adequate predictive power when tested in a matched cohort from the U.S.-based REVEAL registry [37]. But when tested in the U.K. and Spanish Registries, the French equation tended to overestimate the risk of death [12, 38].
Pulmonary Hypertension Connection (PHC) Equation
Similar to the French equation, the PHC equation was developed to predict survival in a subgroup of patients with idiopathic, familial or anorexigen-associated PAH enrolled in the PHC Registry [8, 22]. For this subgroup, 1-, 3-, and 5-year survival was 91 %, 75 % and 65 % respectively, whereas survival predicted by NIH equation was 65, 43 and 32 %, respectively. Again, these mortality differences likely represent the recent availability of targeted PAH therapies. PHC equation predicts the probability of survival primarily by hemodynamic values:
-
\( \mathrm{A}\left(\mathrm{x,y,z}\right)={\mathrm{e}}^{\left(-1.270-0.0148\mathrm{x}+0.0402\mathrm{y}-0.361\mathrm{z}\right)} \) in non-responders to calcium-channel blocker
-
\( \mathrm{A}\left(\mathrm{x,y,z}\right)={\mathrm{e}}^{\left(-3.012-0.0148\mathrm{x}+0.0402\mathrm{y}-0.361\mathrm{z}\right)} \) in responders to calcium-channel blocker
-
t = time since diagnosis
-
x = mean pulmonary arterial pressure (mean PAP)
-
y = mean right atrial pressure
-
z = cardiac index
Although only seen in approximately 3 % of patients, an acute vasodilator response was noted to be a strong prognostic indicator. Thenappan et al. externally validated the PHC and the French equations in a dataset of 449 patients with IPAH, HPAH or anorexigen-PAH prospectively assembled from four different clinical trials of investigational prostanoid therapy [35].
REVEAL Prognostic Equation and Risk Score
The REVEAL prognostic equation was derived from variables independently associated with mortality through multivariable analysis (with Cox proportional hazards) in 2716 patients enrolled in the REVEAL registry [21, 23, 28]. Because REVEAL’s enrollment was several-fold larger than the other registries, the predictor analysis was much more robust, leading to quite a few more predictors. The equation predicts 1- year survival as:
-
S0(1) = baseline survivor function (0.9698)
-
γ = shrinkage coefficient (0.939)
-
Z’β = linear component.
The linear component of this complex equation is dependent on 19 variables (Table 20.4). Variables that add to the linear component are risk factors (total 15), whereas the ones which subtract from it are protective factors (total 4).
Benza et al. validated the prediction equation in a subgroup of 504 recently diagnosed PAH patients (catheterization <3 months of registry enrollment) from REVEAL. Survival estimates from the REVEAL equation were stratified into 5 groups, ranging from low to very high risk of death; and the model calibrated extremely well with observed 1-year survival [21]. The full REVEAL survival equation also showed good external calibration for predicting 1-year survival in a relatively small cohort of PAH patients from a single U.S. center [39]. Furthermore, the REVEAL risk calculator was developed by assigning weighted values to the independent prognostic variables of the full survival equation (Table 20.4), in order to develop a more facile tool for routine clinical practice. The simplified risk calculator was also shown to have excellent calibration for predicting 1- year survival across the same 5 risk groups [40]. Prognostic abilities of the REVEAL risk calculator has also been externally validated in a cohort of matched patients from the French Registry [39, 41, 42].
Applying Survival Equations
An important aspect of a risk equation is its intended use – projecting survival estimates for cohorts or an individual. As described above, the French, PHC and REVEAL predictive equations have been shown through external validation to provide accurate survival estimates in cohorts of PAH patients. However, reliability of these equations for predicting the survival of an individual patient is not robust. For example, Sandoval’s analysis demonstrated that the NIH equation was highly predictive of which individuals would survive (i.e. highly sensitive) but struggled to identify which individuals would die (i.e. low specificity) when using a rigid survival prediction cutoff of 50 % [29]. In Thenappan’s analysis, the PHC equation also had high sensitivity for predicting individual’s survival, but again lacked specificity (i.e. identifying likely deaths). The NIH equation had high specificity at the expense of low sensitivity. Meanwhile, the French equation predicted individual survival with intermediate sensitivity and specificity. Moreover, the area under the receiver operator characteristic (ROC) curve for all 3 equations was similar (only ~0.55), indicating a lack of predictive accuracy. The authors concluded that none of these three equations could be applied to predicting an individual patient’s survival [35].
Benza et al. demonstrated better discrimination of survivors and non-survivors by the REVEAL survival equation and the REVEAL risk score through a validation cohort from within the REVEAL registry. The probability of concordance (or c-index) was 0.72, thus confirming good discrimination (of survivors from non-survivors at 1 year) for both tools [21]. The c-index, which approximates the area under an ROC curves, is a different statistical evaluation of an equation’s discriminatory capability. In essence, an equation’s c-index is the probability that a randomly chosen survivor will have a higher projected survival estimate than a randomly chosen deceased subject; a c-index equaling 1.0 is perfectly discriminatory, while 0.5 represents chance prediction [43]. The REVEAL equation was also able to discriminate effectively when tested for specific subgroups of maximally treated patients (i.e. on parenteral prostanoids), newly diagnosed patients, patients with a pulmonary capillary wedge pressure ≤ 12 mmHg (NIH registry definition), as well as IPAH/HPAH or other forms of PAH. Cogswell et al. demonstrated very good discrimination of 1-year survival, using the original REVEAL equation, in their single-center cohort of 140 PAH patients with a reported c-index of 0.77. The concordance index held up even though there were significant differences in the composition of PAH sub-types (from REVEAL) and a substantial number of patients with missing data for some key variables in the equation [39]. Meanwhile, Kane et al. studied the REVEAL risk score in the much larger Mayo cohort and determined a comparable c-index of 0.71 [9]. Therefore, the REVEAL risk calculator has discriminatory power similar to the full survival equation and has the potential to be used in everyday clinical practice (pending further studies and validation).
Another important test characteristic of predictive equations is the time-frame for predicting survival. While the NIH, French, and PHC equations may not offer as strong discriminatory power as the REVEAL equation or the risk score, these older equations are designed to estimate survival as a function of time. Therefore, an individual’s survival can be estimated at 1, 2 and 3 years, etc. The REVEAL equation and simplified risk calculator were designed to estimate survival 1 year from the point of acquisition of the variables entered into the risk calculator. One analysis of the Mayo registry cohort did note good discrimination of 5 year survival with the REVEAL risk score [9]. In another report though, the discriminatory ability of the full REVEAL equation for predicting 5 year survival was not as good as the 1 year projection, and particularly overestimated risk in patients in the intermediate risk category [39]. Additional experience is needed before the REVEAL equation or risk calculator can be used reliably to forecast survival beyond 1 year, especially as therapeutic options in PAH continue to expand.
In total, numerous analyses demonstrate that currently available modern survival equations, notwithstanding the NIH equation, are best suited to estimate survival in cohorts of patients. In addition, the REVEAL survival equation and risk score, which are also able to discriminate between survivors and non-survivors, can be used at the individual level but are best limited to predicting short term or 1-year survival.
Challenges to Applying Survival Equations in Clinical Practice
Heterogeneity of PAH
At its core, PAH is a heterogeneous group of disorders that share some common pathologic features and, presumably, underlying mechanisms of disease. But PAH disorders have largely been linked together by a clinical classification system based on the severity of hemodynamic derangements, clinical presentation, and disease course in the late stages. Given the rarity of Group 1 PAH conditions, such as IPAH, HPAH, and HIV-associated PAH, it is understandable to aggregate data from potentially diverse subgroups. By assembling a larger cohort of patients, a registry’s statistical power increases and predictive value enhanced. Modern PAH registries have incorporated several hundred to several thousand PAH patients with the majority of patients having either IPAH or CTD-associated PAH, while less frequent representation from rarer subgroups such as porto-pulmonary HTN, HIV-PAH and CHD-PAH. But, these subgroups behave quite differently and exhibit different survival curves, especially in the long-term [21]. Accordingly, caution has to be exercised when applying survival equations to rarer PAH sub-groups, which sorely need dedicated registries.
Age is an important discriminator of outcome in PAH, with older adults faring worse [9, 13, 16, 22, 26]. Furthermore, PAH subgroups can also be differentiated by age at PAH diagnosis. In the NIH registry of the 1980s, patients with IPAH typically presented in the third or fourth decade of life with an average age of 36 ± 15 years [5]. PAH patients with CHD are often recognized during childhood or present in young adulthood, depending on the complexity and size of the defect [44]. On the other end of the spectrum, patients with systemic sclerosis, which is the most common form of CTD-PAH, present much later in life as one large series from the United Kingdom demonstrated (mean age of 63.9 ± 10.5 years) [45]. With more diverse enrollment, modern PAH registries typically report an average age in the fifties, which is much older than the average age of the more homogeneous cohort of IPAH patients entered into the NIH registry 30 years ago [5, 6, 8, 10]. Age alone challenges the use of older survival equations as the population of PAH evolves.
Co-morbidities, which are often associated with the underlying disorder implicated in PAH pathogenesis, also factor into survival and are often not captured in large registry efforts. For example, renal dysfunction appears to be an important predictor of outcome in PAH; in fact, the relatively crude creatinine value (as an estimate of renal function) is part of the REVEAL risk calculator [9, 21, 46]. However, other registries have failed to capture information on renal function. Patients with systemic sclerosis not infrequently exhibit concomitant pulmonary conditions, such as interstitial lung disease, or cardiac issues, including diastolic dysfunction, arrhythmias and valvular disease, that may impact response to PAH therapies and survival [45, 47–49]. Individuals with CHD, ultimately develop Eisenmenger’s physiology with irreversible pulmonary vasculopathy leading to right-to-left circulatory shunting and severe chronic hypoxemia. Eisenmenger’s syndrome is a multi-system disorder with intrinsic cardiac, hematologic, musculoskeletal, renal, and cerebrovascular manifestations [50]. Similarly, non-PAH manifestations of liver disease and portal hypertension, certainly impact the course of patients with porto-pulmonary hypertension and likely lead to the noticeably poor survival of that PAH sub-group [21, 51]. This level of comorbidity detail has not been captured in large-scale PAH registries and therefore challenge the ability of predictive equations to equally forecast survival in diverse PAH subgroups, many of which only make up a small portion of registry enrollment.
Measurement of Predictors and the Use of Survival Equations
The REVEAL survival equation and risk calculator represent a significant advancement from earlier risk equations. Thanks to a richer body of variables that are entered in the REVEAL equations, a more thorough assessment of an individual is undertaken, leading to better discrimination of individual’s short-term survival. But the cost of implementing the equation in routine clinical practice cannot be overlooked, as the full dataset requires recent data from an echocardiogram, laboratory tests, pulmonary function tests, and RHC. This burden of testing will limit use of the equation or the risk calculator on a repetitive and longitudinal basis. Developers of the risk equation and calculator note that absence of some data does not hinder the equation’s ability to provide reliable predictions, but its discriminatory value does diminish with incremental missing data [23]. Efforts are underway to simplify the REVEAL risk calculator without compromising its predictive power, but additional validation will be needed [41].
Once data are collected, the operational aspects of the various equations come into play. None of the equations is particularly user-friendly in the routine clinical environment and require a fair degree of computation. For this reason, the REVEAL risk calculator is much more ideally suited for routine clinical use as the weighted values for individual risk factors can be easily calculated.
Another challenge to applying survival equations stems from inaccuracy and variability of the actual variables needed to compute survival. The NIH, French, and PHC equations rely heavily on hemodynamic measures, such as the cardiac output (or index), RAP and PAP. Even the elaborate REVEAL risk calculator relies on two key hemodynamic measures, RAP and PVR. Although RHC remains critical for diagnosing PAH and assessing prognosis, there are concerns about the accuracy and consistency of these fundamental measurements as routine clinical practices vary considerably [52–54]. Efforts to better standardize hemodynamic measurement in PAH have been published [55]. The 6 MW distance is another important variable in the French and REVEAL equations. While the 6 minute walk test is designed to measure an individual’s exercise capacity and thereby providing an inferential assessment of one’s pulmonary vascular disease and right ventricular function, co-morbidities can influence the test’s output. This is particularly relevant in older patients with peripheral musculoskeletal impairments (e.g. individuals with systemic sclerosis), whose walk distance is limited by more than just cardio-pulmonary issues. Other factors, such as patient’s motivation and cognitive abilities can also influence the six minute walk test output. Another frequently cited measure is the NYHA or WHO functional class, which is a subjectively assigned measure based on somewhat vague definitions. One study demonstrated poor inter-grader agreement, even among experts, for assigning functional class in PAH patients [56]. As a result of challenges in measuring some of these variables that are incorporated into survival equations, the generalizability of survival equations into diverse clinical settings may be impacted.
Newer and promising measures of cardiac function obtained from echocardiography (e.g. tricuspid annular systolic plane excursion, right ventricular strain, etc.) or cardiac MRI (e.g. RV ejection fraction, stroke volume index, myocardial mass, etc.), as well as other exercise indices, such as peak oxygen consumption and the heart rate recovery (after the 6MWT) among others, have not yet been investigated as predictors of survival in large-scale registries. These non-invasive measures might improve the predictive power and discriminatory capabilities of survival prediction equations and, in some cases, are more easily attained [57–61].
All of the survival equations and risk calculators rely on measurements at a single time-point. None of the equations is adaptive and incorporate favorable or unfavorable time-dependent changes of key clinical measures, e.g. improvement in functional class, % decline in six minute walk distance, change in key hemodynamic measures etc., even though clinical experience suggests that changes to these dynamic measures offer predictive value [59, 62–65]. Using relevant trends of key variables in predictive models, intuitively, should better track an individual’s or cohort’s trajectory over time.
Rapidly Evolving PAH Field Leads to Antiquated Survival Equations
An important impediment to applying registry-derived prediction equations to clinical practice is the out-datedness of registry data, which is especially relevant when a condition’s management evolves rapidly. PAH management has been transformed dramatically in the last 20 years and most of the registries in listed Table 20.1 observed patients in earlier eras. PAH-specific therapies were non-existent during the time of the NIH registry. Then, intravenous epoprostenol followed by early oral agents had just become treatment options during the period of the PHC and French registries. More contemporary registries, such as REVEAL and COMPERA, mark the beginning of the era of sequential (or “add-on”) combination therapy. Accordingly survival rates were dismal in the NIH registry with median survival of 2.8 years; but the REVEAL Registry reported a median survival of 7 years [19, 21, 23]. While inclusion of prevalent patients in REVEAL (as opposed to only incident cases enrolled in the NIH registry) likely accounted for some of the improvement in median survival, the availability of PAH therapies and a better general approach to right-sided heart failure also likely influenced the improved survival shown in REVEAL [26].
As of 2015, there are 12 approved PAH therapies in the United States, including approval of three new agents between late 2013 and early 2014. Moreover, another shift in the treatment paradigm will likely occur in 2015, based on the increasing number of oral agents and the positive results of a large, rigorous study that demonstrated a reduction in the risk of “Clinical Failure” with upfront dual oral therapies as opposed to (traditional) monotherapy in newly diagnosed and treatment naive PAH patients [66]. There is even early experience with upfront triple therapy with agents from each of the major classes of therapy – prostanoid, ERA, and PDE5-inhibitor in functional class IV patients [67]. Beyond the use of PAH specific therapies, management of right ventricular failure and more appropriate use of background therapies, including diuretics, inotropes, anticoagulants and calcium-channel blockers have also evolved over the last few decades. Therefore, survival estimates displayed in registries and their derived prediction equations are pertinent to their respective eras, but quickly become outdated as the PAH therapeutic landscape continues to evolve with new classes of medications and treatment strategies. Accordingly, more modern registries have shown that the older NIH equation significantly underestimates observed survival [15, 22]. These reports should inform clinicians and researchers that a survival equation’s clinical application should be in the same era of the equation’s originating Registry, in order to assure similar therapeutic options and management approaches.
PAH Is a Global Condition
PAH is a global problem but its makeup is not the same around the world. In the U.S., Canada, and Europe, IPAH and CTD-related PAH predominate in large patient cohorts and in clinical practice. But, CHD-PAH and Schistosomiasis-associated PAH are much more relevant in under-developed regions of the world, including Latin America, Africa, China and India. Even though all of these conditions are still viewed as PAH under the Nice Classification, PAH cohorts from these regions are distinct and their natural history and response to treatment are not likely similar [68]. And with the exception of two reports from China, all registry-based published experiences emanate from the United States or Europe (Table 20.1) [7, 14].
PAH patients in under-developed regions of the world also face numerous obstacles that patients in more developed areas generally do not face, such as access to health-care (let alone experienced PH physicians) and availability of expensive and complicated PAH medications. Most Western countries, including France, United Kingdom, and Canada, have developed a few national PH referral centers, staffed by PH experts that have concentrated the care of PAH patients originating throughout their respective countries. In the United States, such a program is in its infancy, but there are many large and small PH Centers throughout the country that offer expert management of PH patients [69]. In most under-developed countries, expert PH care is offered at only a handful of locations; unfortunately, geography and economics greatly hinder access to these specialized care centers. As a result, early disease recognition and appropriate comprehensive evaluations, including catheterization, are significant challenges [7]. Finally, PAH-specific therapies are quite expensive and advanced therapies, namely parenteral prostanoids, are extremely complex to administer. Even though parenteral prostanoids have tremendous potential and are often the treatment of choice for the most compromised PAH individuals or for patients failing simpler therapies, prostanoid usage is essentially nil in under-developed regions of the world due to a combination of exorbitant costs, limited understanding of safe infusion practices, or lack of pre-requisite infrastructure to safely administer [70].
Many of these points are nicely corroborated by efforts in China and illustrated through two separate registries, spanning altogether a 10 year period from 1999 to 2009 [7, 14]. In the first registry, 72 incident or prevalent IPAH and HPAH patients were recruited from two facilities between 1999 and 2004. The majority of patients were diagnosed by echocardiogram and 90 % of patients received calcium-channel blocker therapy even though acute vaso-responsiveness was only confirmed in a few individuals. Survival estimates at 1, 3, and 5 years were 68.0 %, 38.9 %, 20.8 % respectively [7]. In essence, this early Chinese Registry provided natural history data (i.e. without PAH-specific therapy) on a sub-population of PAH patients, similar to the NIH Registry conducted 15 years earlier. By 2007, a number of PH referral centers were established throughout China [14]. Zhang subsequently provided a more modern account of PAH in China by reporting on 276 IPAH and CTD-PAH patients, recruited from five centers throughout the country between 2007 and 2009. Even though data collection was retrospective, all patients underwent a standardized and comprehensive evaluation including RHC. Importantly, the mean age for the IPAH cohort in both Chinese registries was in the low 30s, similar to the NIH registry but far younger than COMPERA [5, 27]. This finding may stem from regional population differences but probably also indicates a referral bias against older individuals being evaluated at the few PH referral centers in China. Majority of patients in the modern Chinese registry received PAH specific therapy, either a PDE5-I or an ERA and only a handful of patients received a calcium channel blocker, but prostanoids were not utilized due to reasons mentioned earlier [14]. Survival estimates for IPAH patients improved considerably in the second registry to 92.1 % and 75.1 % at 1 and 3 years, respectively. Zhang also confirmed poorer survival estimates for the CTD-PAH cohort, as opposed to IPAH, which has also been shown in other registries [14].
Significant obstacles, including accuracy of diagnosis, limited access to expert PH care and limited availability of PAH-specific therapies, especially advanced prostanoids, hinder the use of modern survival equations generated from resource-laden countries to regions of the world without similar resources.
Use of Risk Calculators for Allocating Lung Transplants in PAH
Advances in medical therapies have dramatically improved the mortality and quality of life for PAH patients [14, 30–34, 62, 71–74]. However, the disease remains uniformly fatal, and the only curative measure is lung transplantation [75]. Scarce donor organs and chronic rejection necessitates that resources be carefully allocated to patients with the most urgent need and greatest likelihood of successful lung transplantation. For this reason, the Lung Allocation Score (LAS) was developed and weighs both wait-list urgency and post-transplant survival based on disease severity, physiologic reserve, and disease subgroup [76].
Evaluations of the LAS system indicate that overall wait times and wait-list mortality have decreased, and the total number of transplants has increased [77]. However, amongst IPAH patients, transplant rates are lower and wait-list mortality higher [78]. This likely reflects the fact that the LAS does not include many of the key variables that predict mortality in PAH, such as mean RAP and CI [19, 21, 22, 29]. Additionally, the 6 MW distance is included in LAS, but at a threshold level so low that it applies to few patients. The inability of the LAS to distinguish low- and high-risk IPAH patients at least partially reflects the difficulty in clinically identifying the sickest IPAH patients.
To address these issues, attempts have been made to modify the LAS by including key clinical and physiologic variables [79]. To study the effectiveness of modified prediction equations in a transplant population, data were analyzed from the Scientific Registry of Transplant Recipients files to compare wait-list mortality with predicted mortality. The PHC equation and LAS-predicted mortality were compared to observed mortality in 827 PAH patients, divided into pre- and post-2006 cohorts; the post-2006 cohort was substantially sicker than the pre-2006 cohort. The PHC equation underestimated and overestimated survival in the pre- and post-2006 cohorts, respectively; the LAS had similar accuracy. The authors developed a new equation that included elements of the LAS along with 6-MWD, resting oxygen requirements, invasive cardiac output, and functional class. The new equation outperformed the PHC equation. Among CTD-associated and secondary PAH patients, the new equation outperformed the LAS, but performed similarly in a subgroup analysis of IPAH patients [80]. These results point to the fact that including more relevant variables in predictive models of survival can indeed lead to higher accuracy in actual transplantable populations. This is similar to what was observed in the transformation from earlier PAH survival equations to the REVEAL prediction models. However, fine tuning of these transplant allocation equations for the PAH group and prospective validation are still needed. More research is needed to ensure that PAH patients in need of lung transplantation are appropriately ranked on wait-lists, as transplant offers the greatest chance of survival for the most advanced PAH patients, even in patients with systemic multi-organ diseases such as scleroderma [81].
Conclusion
Registries conducted around the world over the last 30 years have provided a wealth of information about PAH, including epidemiologic data, prevalence estimates, survival statistics, and risk factors for important long-term outcomes. These registries have chronicled remarkable improvement in outcomes, including survival, but have also reaffirmed the ongoing struggles of this incurable disease. Survival equations and risk calculators are important by-products of registry efforts and, when used in the appropriate sub-groups and therapeutic era, have proven adept at predicting outcomes of sizable cohorts and for producing comparator data to judge various therapeutic interventions. But application of these prediction equations is challenged by the global nature of PAH that leads to disparities in care, a rapidly evolving therapeutic landscape, and the equations’ limitations for predicting outcomes at an individual patient level. Progress has been made with the development and validation of a more robust and clinically relevant REVEAL risk calculator, but additional enhancements and validation is needed. Given how rapidly the PAH field is evolving though, it is unclear if a valid and reliable survival prediction tool will ever be widely implemented in clinical practice.
Abbreviations
- 6 MW:
-
6 minute walk
- CHD:
-
Congenital heart disease
- CI:
-
Cardiac index
- COMPERA:
-
Comparative Prospective Registry of Newly Initiated Therapies for Pulmonary Arterial Hypertension
- CTD:
-
Connective tissue disease
- CTEPH:
-
Chronic thromboembolic pulmonary hypertension
- DLCO:
-
Diffusing capacity of the lung for carbon monoxide
- ERA:
-
Endothelin receptor antagonist
- HIV:
-
Human immunodeficiency virus
- HPAH:
-
Heritable pulmonary arterial hypertension
- IPAH:
-
Idiopathic pulmonary arterial hypertension
- LAS:
-
Lung Allocation Score
- LVEDP:
-
Left ventricular end-diastolic pressure
- MAI:
-
Million adult inhabitants
- NIH:
-
National Institutes of Health
- NYHA:
-
New York Heart Association
- PAH:
-
Pulmonary arterial hypertension
- PAP:
-
Pulmonary arterial pressure
- PAWP:
-
Pulmonary arterial wedge pressure
- PDE5:
-
Phosphodiesterase 5
- PHC:
-
Pulmonary Hypertension Connection
- PVOD:
-
Pulmonary veno-occulsive disease
- PVR:
-
Pulmonary vascular resistance
- QuERI:
-
Quality Enhancement Research Initiative
- RAP:
-
Right atrial pressure
- REHAP:
-
Spanish Registry of Pulmonary Arterial Hypertension
- REVEAL:
-
Registry to evaluate early and long-term pulmonary arterial hypertension management
- RHC:
-
Right heart catheterization
- ROC:
-
Receiver operator characteristic
- SMR:
-
Scottish Morbidity Record
- SPVU:
-
Scottish Pulmonary Vascular Unit
- WHO:
-
World Health Organization
References
Gliklich R, Dreyer N, editors. Registries for evaluating patient outcomes: a user’s guide. 2nd ed. (Prepared by Outcome DEcIDE Center [Outcome Sciences, Inc. d/b/a Outcome] under Contract No. HHSA29020050035I TO3.) AHRQ Publication No. 10-EHC049. Rockville: Agency for Healthcare Research and Quality; 2010.
Dreyer NA, Schneeweiss S, McNeil BJ, Berger ML, Walker AM, Ollendorf DA, et al. GRACE principles: recognizing high-quality observational studies of comparative effectiveness. Am J Manag Care. 2010;16(6):467–71. PubMed.
McGoon MD, Benza RL, Escribano-Subias P, Jiang X, Miller DP, Peacock AJ, et al. Pulmonary arterial hypertension: epidemiology and registries. J Am Coll Cardiol. 2013;62(25 Suppl):D51–9. PubMed.
Guidelines on Pharmacovigilance for Medicinal Products for Human Use. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2013/05/WC500143294.pdf. European Medicines Agency; 2013 [cited 25 Aug 2014].
Rich S, Dantzker DR, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, et al. Primary pulmonary hypertension. A national prospective study. Ann Intern Med. 1987;107(2):216–23. PubMed.
Badesch DB, Raskob GE, Elliott CG, Krichman AM, Farber HW, Frost AE, et al. Pulmonary arterial hypertension: baseline characteristics from the REVEAL Registry. Chest. 2010;137(2):376–87. PubMed.
Jing ZC, Xu XQ, Han ZY, Wu Y, Deng KW, Wang H, et al. Registry and survival study in chinese patients with idiopathic and familial pulmonary arterial hypertension. Chest. 2007;132(2):373–9. PubMed.
Thenappan T, Shah SJ, Rich S, Gomberg-Maitland M. A USA-based registry for pulmonary arterial hypertension: 1982–2006. Eur Respir J. 2007;30(6):1103–10. PubMed.
Kane GC, Maradit-Kremers H, Slusser JP, Scott CG, Frantz RP, McGoon MD. Integration of clinical and hemodynamic parameters in the prediction of long-term survival in patients with pulmonary arterial hypertension. Chest. 2011;139(6):1285–93. PubMed.
Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med. 2006;173(9):1023–30. PubMed.
Peacock AJ, Murphy NF, McMurray JJ, Caballero L, Stewart S. An epidemiological study of pulmonary arterial hypertension. Eur Respir J. 2007;30(1):104–9. PubMed.
Escribano-Subias P, Blanco I, Lopez-Meseguer M, Lopez-Guarch CJ, Roman A, Morales P, et al. Survival in pulmonary hypertension in Spain: insights from the Spanish registry. Eur Respir J. 2012;40(3):596–603. PubMed.
Hoeper MM, Huscher D, Ghofrani HA, Delcroix M, Distler O, Schweiger C, et al. Elderly patients diagnosed with idiopathic pulmonary arterial hypertension: results from the COMPERA registry. Int J Cardiol. 2013;168(2):871–80. PubMed.
Zhang R, Dai LZ, Xie WP, Yu ZX, Wu BX, Pan L, et al. Survival of Chinese patients with pulmonary arterial hypertension in the modern treatment era. Chest. 2011;140(2):301–9. PubMed.
Fischler M, Speich R, Dorschner L, Nicod L, Domenighetti G, Tamm M, et al. Pulmonary hypertension in Switzerland: treatment and clinical course. Swiss Med Wkly. 2008;138(25–26):371–8. PubMed.
Ling Y, Johnson MK, Kiely DG, Condliffe R, Elliot CA, Gibbs JS, et al. Changing demographics, epidemiology, and survival of incident pulmonary arterial hypertension: results from the pulmonary hypertension registry of the United Kingdom and Ireland. Am J Respir Crit Care Med. 2012;186(8):790–6. PubMed.
Khanna D, Tan M, Furst DE, Hill NS, McLaughlin VV, Silver RM, et al. Recognition of pulmonary hypertension in the rheumatology community: lessons from a Quality Enhancement Research Initiative. Clin Exp Rheumatol. 2014;32:s-21–7.
McLaughlin VV, Langer A, Tan M, Clements PJ, Oudiz RJ, Tapson VF, et al. Contemporary trends in the diagnosis and management of pulmonary arterial hypertension: an initiative to close the care gap. Chest. 2013;143(2):324–32. PubMed.
D’Alonzo GE, Barst RJ, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, et al. Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med. 1991;115(5):343–9. PubMed.
Humbert M, Sitbon O, Yaici A, Montani D, O’Callaghan DS, Jais X, et al. Survival in incident and prevalent cohorts of patients with pulmonary arterial hypertension. Eur Respir J. 2010;36(3):549–55. PubMed.
Benza RL, Miller DP, Barst RJ, Badesch DB, Frost AE, McGoon MD. An evaluation of long-term survival from time of diagnosis in pulmonary arterial hypertension from the REVEAL Registry. Chest. 2012;142(2):448–56. PubMed.
Thenappan T, Shah SJ, Rich S, Tian L, Archer SL, Gomberg-Maitland M. Survival in pulmonary arterial hypertension: a reappraisal of the NIH risk stratification equation. Eur Respir J. 2010;35(5):1079–87. PubMed.
Benza RL, Miller DP, Gomberg-Maitland M, Frantz RP, Foreman AJ, Coffey CS, et al. Predicting survival in pulmonary arterial hypertension: insights from the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL). Circulation. 2010;122(2):164–72. PubMed.
McLaughlin VV, Suissa S. Prognosis of pulmonary arterial hypertension: the power of clinical registries of rare diseases. Circulation. 2010;122(2):106–8. PubMed.
Frost AE, Badesch DB, Barst RJ, Benza RL, Elliott CG, Farber HW, et al. The changing picture of patients with pulmonary arterial hypertension in the United States: how REVEAL differs from historic and non-US Contemporary Registries. Chest. 2011;139(1):128–37. PubMed.
Benza RL, Gomberg-Maitland M, Frost AE, Frantz RP, Humbert M, McGoon MD. Development of prognostic tools in pulmonary arterial hypertension: lessons from modern day registries. Thromb Haemost. 2012;108(6):1049–60. PubMed.
Olsson KM, Delcroix M, Ghofrani HA, Tiede H, Huscher D, Speich R, et al. Anticoagulation and survival in pulmonary arterial hypertension: results from the Comparative, Prospective Registry of Newly Initiated Therapies for Pulmonary Hypertension (COMPERA). Circulation. 2014;129(1):57–65. PubMed.
McGoon MD, Krichman A, Farber HW, Barst RJ, Raskob GE, Liou TG, et al. Design of the REVEAL registry for US patients with pulmonary arterial hypertension. Mayo Clin Proc Mayo Clin. 2008;83(8):923–31. PubMed.
Sandoval J, Bauerle O, Palomar A, Gomez A, Martinez-Guerra ML, Beltran M, et al. Survival in primary pulmonary hypertension. Validation of a prognostic equation. Circulation. 1994;89(4):1733–44. PubMed.
Rubin LJ, Badesch DB, Barst RJ, Galie N, Black CM, Keogh A, et al. Bosentan therapy for pulmonary arterial hypertension. N Engl J Med. 2002;346(12):896–903. PubMed.
McLaughlin VV, Shillington A, Rich S. Survival in primary pulmonary hypertension: the impact of epoprostenol therapy. Circulation. 2002;106(12):1477–82. PubMed.
McLaughlin VV, Sitbon O, Badesch DB, Barst RJ, Black C, Galie N, et al. Survival with first-line bosentan in patients with primary pulmonary hypertension. Eur Respir J. 2005;25(2):244–9. PubMed.
Provencher S, Sitbon O, Humbert M, Cabrol S, Jais X, Simonneau G. Long-term outcome with first-line bosentan therapy in idiopathic pulmonary arterial hypertension. Eur Heart J. 2006;27(5):589–95. PubMed.
Barst RJ, Galie N, Naeije R, Simonneau G, Jeffs R, Arneson C, et al. Long-term outcome in pulmonary arterial hypertension patients treated with subcutaneous treprostinil. Eur Respir J. 2006;28(6):1195–203. PubMed.
Thenappan T, Glassner C, Gomberg-Maitland M. Validation of the pulmonary hypertension connection equation for survival prediction in pulmonary arterial hypertension. Chest. 2012;141(3):642–50. PubMed.
Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, et al. Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation. 2010;122(2):156–63. PubMed.
McGoon M, Benza R, Frost A. External validation of the French predictive model to estimate PAH survival: a REVEAL analysis (abstr). Eur Respir J. 2012;40(41S).
Lee WT, Ling Y, Sheares KK, Pepke-Zaba J, Peacock AJ, Johnson MK. Predicting survival in pulmonary arterial hypertension in the UK. Eur Respir J. 2012;40(3):604–11. PubMed.
Cogswell R, Kobashigawa E, McGlothlin D, Shaw R, De Marco T. Validation of the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL) pulmonary hypertension prediction model in a unique population and utility in the prediction of long-term survival. J Heart Lung Transplant. 2012;31(11):1165–70. PubMed.
Benza RL, Gomberg-Maitland M, Miller DP, Frost A, Frantz RP, Foreman AJ, et al. The REVEAL Registry risk score calculator in patients newly diagnosed with pulmonary arterial hypertension. Chest. 2012;141(2):354–62. PubMed.
Cogswell R, Pritzker M, De Marco T. Performance of the REVEAL pulmonary arterial hypertension prediction model using non-invasive and routinely measured parameters. J Heart Lung Transplant. 2014;33(4):382–7. PubMed.
Sitbon O, Humbert M, Simonneau G. External validation of the REVEAL risk score calculator for PAH survival: a French pulmonary hypertension network analysis (abstr). Eur Respir J. 2012;40(41S).
Pencina MJ, D’Agostino RB. Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Stat Med. 2004;23(13):2109–23. PubMed.
Duffels MG, Engelfriet PM, Berger RM, van Loon RL, Hoendermis E, Vriend JW, et al. Pulmonary arterial hypertension in congenital heart disease: an epidemiologic perspective from a Dutch registry. Int J Cardiol. 2007;120(2):198–204. PubMed.
Condliffe R, Kiely DG, Peacock AJ, Corris PA, Gibbs JS, Vrapi F, et al. Connective tissue disease-associated pulmonary arterial hypertension in the modern treatment era. Am J Respir Crit Care Med. 2009;179(2):151–7. PubMed.
Shah SJ, Thenappan T, Rich S, Tian L, Archer SL, Gomberg-Maitland M. Association of serum creatinine with abnormal hemodynamics and mortality in pulmonary arterial hypertension. Circulation. 2008;117(19):2475–83. PubMed.
de Groote P, Gressin V, Hachulla E, Carpentier P, Guillevin L, Kahan A, et al. Evaluation of cardiac abnormalities by Doppler echocardiography in a large nationwide multicentric cohort of patients with systemic sclerosis. Ann Rheum Dis. 2008;67(1):31–6. PubMed.
Meune C, Avouac J, Wahbi K, Cabanes L, Wipff J, Mouthon L, et al. Cardiac involvement in systemic sclerosis assessed by tissue-doppler echocardiography during routine care: a controlled study of 100 consecutive patients. Arthritis Rheum. 2008;58(6):1803–9. PubMed.
Tongers J, Schwerdtfeger B, Klein G, Kempf T, Schaefer A, Knapp JM, et al. Incidence and clinical relevance of supraventricular tachyarrhythmias in pulmonary hypertension. Am Heart J. 2007;153(1):127–32. PubMed.
Vongpatanasin W, Brickner ME, Hillis LD, Lange RA. The Eisenmenger syndrome in adults. Ann Intern Med. 1998;128(9):745–55. PubMed.
Kawut SM, Taichman DB, Ahya VN, Kaplan S, Archer-Chicko CL, Kimmel SE, et al. Hemodynamics and survival of patients with portopulmonary hypertension. Liver Transpl. 2005;11(9):1107–11. PubMed.
Halpern SD, Taichman DB. Misclassification of pulmonary hypertension due to reliance on pulmonary capillary wedge pressure rather than left ventricular end-diastolic pressure. Chest. 2009;136(1):37–43. PubMed.
Ryan JJ, Rich JD, Thiruvoipati T, Swamy R, Kim GH, Rich S. Current practice for determining pulmonary capillary wedge pressure predisposes to serious errors in the classification of patients with pulmonary hypertension. Am Heart J. 2012;163(4):589–94. PubMed.
Pugh ME, Hemnes AR, Trammell A, Newman JH, Robbins IM. Variablity in hemodynamic evalution of pulmonary hypertension at large referral centers. Pulmonary circulation. 2014;2014:4(4).
Hoeper MM, Bogaard HJ, Condliffe R, Frantz R, Khanna D, Kurzyna M, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D42–50. PubMed.
Taichman DB, McGoon MD, Harhay MO, Archer-Chicko C, Sager JS, Murugappan M, et al. Wide variation in clinicians’ assessment of New York Heart Association/World Health Organization functional class in patients with pulmonary arterial hypertension. Mayo Clin Proc Mayo Clin. 2009;84(7):586–92. PubMed Pubmed Central PMCID: 2704130.
Forfia PR, Fisher MR, Mathai SC, Housten-Harris T, Hemnes AR, Borlaug BA, et al. Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med. 2006;174(9):1034–41. PubMed.
van Wolferen SA, Marcus JT, Boonstra A, Marques KM, Bronzwaer JG, Spreeuwenberg MD, et al. Prognostic value of right ventricular mass, volume, and function in idiopathic pulmonary arterial hypertension. Eur Heart J. 2007;28(10):1250–7. PubMed.
van de Veerdonk MC, Kind T, Marcus JT, Mauritz GJ, Heymans MW, Bogaard HJ, et al. Progressive right ventricular dysfunction in patients with pulmonary arterial hypertension responding to therapy. J Am Coll Cardiol. 2011;58(24):2511–9. PubMed.
Wensel R, Opitz CF, Anker SD, Winkler J, Hoffken G, Kleber FX, et al. Assessment of survival in patients with primary pulmonary hypertension: importance of cardiopulmonary exercise testing. Circulation. 2002;106(3):319–24. PubMed.
Minai OA, Gudavalli R, Mummadi S, Liu X, McCarthy K, Dweik RA. Heart rate recovery predicts clinical worsening in patients with pulmonary arterial hypertension. Am J Respir Crit Care Med. 2012;185(4):400–8. PubMed.
Sitbon O, Humbert M, Nunes H, Parent F, Garcia G, Herve P, et al. Long-term intravenous epoprostenol infusion in primary pulmonary hypertension: prognostic factors and survival. J Am Coll Cardiol. 2002;40(4):780–8. PubMed.
Nickel N, Golpon H, Greer M, Knudsen L, Olsson K, Westerkamp V, et al. The prognostic impact of follow-up assessments in patients with idiopathic pulmonary arterial hypertension. Eur Respir J. 2012;39(3):589–96. PubMed.
Hoeper MM, Markevych I, Spiekerkoetter E, Welte T, Niedermeyer J. Goal-oriented treatment and combination therapy for pulmonary arterial hypertension. Eur Respir J. 2005;26(5):858–63. PubMed.
Tiede H, Sommer N, Milger K, Voswinckel R, Bandorski D, Schermuly RT, et al. Short-term improvement in pulmonary hemodynamics is strongly predictive of long-term survival in patients with pulmonary arterial hypertension. Pulm Circ. 2013;3(3):523–32. PubMed Pubmed Central PMCID: 4070816.
Galie N, Barbera JA, Frost AE, Ghofrani HA, Hoeper MM, McLaughlin VV, et al. Initial use of Ambrisentan plus Tadalafil in Pulmonary Arterial Hypertension. N Eng J Med. 2015; 373(9):834–44.
Sitbon O, Jais X, Savale L, Cottin V, Bergot E, Macari EA, et al. Upfront triple combination therapy in pulmonary arterial hypertension: a pilot study. Eur Respir J. 2014;43(6):1691–7. PubMed.
Simonneau G, Gatzoulis MA, Adatia I, Celermajer D, Denton C, Ghofrani A, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D34–41. PubMed.
Chakinala MM, McGoon M. Pulmonary hypertension care centers. Adv Pulm Hyper. 2014;12(4):175–8.
Hiremath J, Thanikachalam S, Parikh K, Shanmugasundaram S, Bangera S, Shapiro L, et al. Exercise improvement and plasma biomarker changes with intravenous treprostinil therapy for pulmonary arterial hypertension: a placebo-controlled trial. J Heart Lung Transplant. 2010;29(2):137–49. PubMed.
Galie N, Olschewski H, Oudiz RJ, Torres F, Frost A, Ghofrani HA, et al. Ambrisentan for the treatment of pulmonary arterial hypertension: results of the ambrisentan in pulmonary arterial hypertension, randomized, double-blind, placebo-controlled, multicenter, efficacy (ARIES) study 1 and 2. Circulation. 2008;117(23):3010–9. PubMed.
Galie N, Ghofrani HA, Torbicki A, Barst RJ, Rubin LJ, Badesch D, et al. Sildenafil citrate therapy for pulmonary arterial hypertension. N Engl J Med. 2005;353(20):2148–57. PubMed.
Ghofrani HA, Galie N, Grimminger F, Grunig E, Humbert M, Jing ZC, et al. Riociguat for the treatment of pulmonary arterial hypertension. N Engl J Med. 2013;369(4):330–40. PubMed.
Awdish RL, Cajigas HR. Early initiation of prostacyclin in portopulmonary hypertension: 10 years of a transplant center’s experience. Lung. 2013;191(6):593–600. PubMed.
Orens JB. Lung transplantation for pulmonary hypertension. Int J Clin Pract Suppl. 2007;158:4–9. PubMed.
Davis SQ, Garrity Jr ER. Organ allocation in lung transplant. Chest. 2007;132(5):1646–51. PubMed.
Hachem RR, Trulock EP. The new lung allocation system and its impact on waitlist characteristics and post-transplant outcomes. Semin Thorac Cardiovasc Surg. 2008;20(2):139–42. PubMed.
Chen H, Shiboski SC, Golden JA, Gould MK, Hays SR, Hoopes CW, et al. Impact of the lung allocation score on lung transplantation for pulmonary arterial hypertension. Am J Respir Crit Care Med. 2009;180(5):468–74. PubMed Pubmed Central PMCID: 2742763.
Benza RL, Miller DP, Frost A, Barst RJ, Krichman AM, McGoon MD. Analysis of the lung allocation score estimation of risk of death in patients with pulmonary arterial hypertension using data from the REVEAL Registry. Transplantation. 2010;90(3):298–305. PubMed.
Gomberg-Maitland M, Glassner-Kolmin C, Watson S, Frantz R, Park M, Frost A, et al. Survival in pulmonary arterial hypertension patients awaiting lung transplantation. J Heart Lung Transplant. 2013;32(12):1179–86. PubMed.
Khan IY, Singer LG, de Perrot M, Granton JT, Keshavjee S, Chau C, et al. Survival after lung transplantation in systemic sclerosis. A systematic review. Respir Med. 2013;107(12):2081–7. PubMed.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
McEvoy, C.A., Sardana, M., Moll, M., Farber, H.W., Chakinala, M.M. (2016). Patient Registries in Pulmonary Arterial Hypertension: the Role of Survival Equations and Risk Calculators. In: Maron, B., Zamanian, R., Waxman, A. (eds) Pulmonary Hypertension. Springer, Cham. https://doi.org/10.1007/978-3-319-23594-3_20
Download citation
DOI: https://doi.org/10.1007/978-3-319-23594-3_20
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-23593-6
Online ISBN: 978-3-319-23594-3
eBook Packages: MedicineMedicine (R0)