Abstract
The human gut microbiota is critical for regulation of whole body metabolism and the immune system. Probiotics provide many benefits on human health by regulating this microbiota. In the prevention of infectious diseases, several probiotic Lactobacillus strains are shown to be effective to enhance the effects of influenza vaccine. These effects are mediated by increment of NK cell population, T-helper type 1 response, and production of virus-specific IgA, IgG, and IgM to inhibit the viral infection. Recently, we have shown that Lactobacillus gasseri LG2055 is effective to prevent influenza by induction of IFNβ production and expression of antiviral genes to inhibit the viral replication. In addition, the inflammatory response is inhibited, and cytokine production to stimulate B cells is induced by the administration of LG2055. Especially, IFNβ inhibits the replication of influenza virus and IFNβ production signal is mediated by IPS-1 through the activation of IRF3 and NF-κB. Therefore, in the future, the regulatory effects on the function or expression of these signaling molecules by the administration of probiotics should be studied. In addition, since the inhibition of FasL-induced apoptosis is effective to protect mice from death by the viral infection, the function of other death receptors, TNFR, DR4, and DR5, or signaling molecules, Siva-1, DAP3, and DELE, should be clarified in the viral replication and apoptosis induction. Further investigation for the regulatory effects of probiotics on the function of these molecules is required and might lead to the development of novel influenza drugs or vaccine adjuvants.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Gut microbiota is an important environmental factor for the regulation of hepatic lipogenesis and energy homeostasis in the host (Bäckhed et al. 2004; Nicholson et al. 2005). It is demonstrated that the functional members of the microbiome affect host metabolism regulating human health condition (Nicholson et al. 2005; Ley et al. 2006; Li et al. 2008). Gut microbiota is also critical for regulation of the immune system, to prevent immune disorders such as a chronic inflammatory bowel disease (Mazmanian et al. 2008), and contributes to the control of inflammatory responses in obesity or type II diabetes (Cani et al. 2008) and development of type I diabetes (Wen et al. 2008). Probiotics, live microorganisms, when administered in adequate amounts, provide many potential benefits on human health. Especially, intestinal and dairy species of lactobacilli and bifidobacteria are well known to be health-promoting microbes in the human gastrointestinal tract (Kleerebezem and Vaughan 2009). In fact, clinical trials show that certain microorganisms including these bacterial strains can prevent the intestinal infections of pathogens by reducing the duration of diarrhea, inflammatory bowel syndromes (Reid et al. 2003), and even the early atopic disease in children (Kalliomäki et al. 2001). Some probiotics are also demonstrated to be effective for enhancement of the effects of vaccination against influenza viruses (Olivares et al. 2007; Davidson et al. 2011).
Influenza A viruses are well known to cause highly contagious respiratory illness, influenza (Taubenberger and Morens 2010), and belong to the Orthomyxoviridae viruses, negative sense, single-stranded RNA viruses carrying eight segmented RNA genome (Fig. 1) (Medina & García-Sastre 2011). Infection of influenza A virus caused several pandemic diseases in the past and is also the cause of almost annual epidemics “seasonal flu.” In addition, influenza A virus is a cause of lethal infectious diseases culminating in severe pneumonia. Older adults, very young children, pregnant women, and patients with chronic diseases are higher risk groups to be exposed to serious illness or death by the viral infection. Therefore, development of drugs or vaccines for prevention or treatment of influenza is very important to protect these people from diseases that cause serious illness. Importantly, identifying the viral and host molecules, critical for the viral replication and pathogenesis, is very useful for the development of the effective drugs or vaccines. In addition to drugs or vaccines, probiotics are also good candidates to regulate the function of these molecules and that of immune cells to prevent or treat influenza.
Structure of influenza A virus and life cycle of the virus. Influenza A virus has eight RNA genomic segments, encoding the viral RNA polymerases (PB1, PB2, PA), nucleoproteins (NPs), hemagglutinin (HA), neuraminidase (NA), matrix protein (M1), and nonstructural protein (NS1). HA binds to the host cell surface receptors, and the virus is transported intracellularly by endocytosis. Low pH in the endosome induces fusion of the viral and endosomal membranes and also triggers releasing the viral RNP (vRNP) into the cytoplasm and transporting it into the nucleus. In the nucleus, the viral polymerase initiates viral mRNA synthesis. The mRNA is transported to the cytoplasm and is translated into proteins. NS1 has a critical role to inhibit the production of host mRNAs, including interferon (IFN) β mRNAs. The vRNP is transported to the cytoplasm, by a M1–NS2 complex. After the vRNP is translocated to the cell membrane, it is incorporated into new viruses and released after the budding on the host cell surface
Recently, we found that oral administration of a probiotic strain, Lactobacillus gasseri SBT2055 (LG2055) (1.6 × 109 cfu/mouse, administrated once a day for 21 days), was effective to prevent influenza by the inhibition of viral replication through upregulation of the expression of antiviral genes in mice (Nakayama et al. 2014). LG2055 is a probiotic lactic acid bacterium, shown to improve the intestinal environment, and has preventive effects on abdominal adiposity in humans (receiving 1.0 × 108 cfu /g/day of LG2055 in 200 g fermented milk for 12 weeks) (Sato et al. 2008). In addition, its oral administration to mouse dams was shown to prevent rotavirus infection in their pups (Kadooka et al. 2012). Interestingly, it was demonstrated that LG2055 induces TGF-β expression in dendritic cells and subsequently TGF-β induced IgA production by B cells in the small intestine (Sakai et al. 2014). Therefore, LG2055 as a probiotic strain plays a pivotal role in the prevention of rotavirus infection by produced IgA. In the lumen of the intestinal tract, secretory IgA is very important to constitute significant barriers to exclude pathogens from mucosal surfaces (Corthésy 2013). There is a possibility that IgA production is induced in the serum and bronchoalveolar lavage fluid (BALF) by the administration of LG2055 and secreted IgA protects the lung from the infection of influenza A virus.
In this chapter, the molecular mechanisms of influenza virus infection and host defense system against the viral replication are demonstrated, relating to the immunoregulatory effects of probiotics on the prevention of the viral infection. Based on these mechanisms, accumulated results by the functional analysis of the probiotics to regulate the host defense system could lead to the development of effective adjuvants of the influenza vaccine and drugs for the prevention and treatment of influenza.
2 Function of Cellular Signaling Molecules for the Infection of Influenza A Virus
Recently, it is demonstrated that the Ras–phosphoinositide 3-kinase (PI3K) signaling pathway mediates the entry of influenza A virus into the infected cells (Fig. 1) (Fujioka et al. 2011). Binding of Ras with PI3K is specifically involved in clathrin-independent endocytosis, endosomal maturation, and intracellular transport of the viruses. Influenza A virus infection activates Ras and subsequently PI3K in the early endosomes. Furthermore, it is shown that influenza A viruses enter cells via redundant pathways of clathrin-mediated and clathrin-independent endocytosis, and intracellular Ca (2+) increase is required for both signaling pathways (Fujioka et al. 2013). In addition, RhoA, Rho-kinase, phosphatidylinositol 4-phosphate 5-kinase (PIP5K), and phospholipase C (PLC) regulate this Ca (2+) signaling. The viral infection induces oscillations in the cytosolic Ca (2+) concentration of host cells, and this event is crucial for viral internalization and infection (Fig. 1). RhoA is activated at downstream of the virus-induced Ca (2+) response and induces Ca (2+) oscillations in a manner dependent on Rho-kinase and subsequent PIP5K-PLC signaling. This signaling circuit regulates both clathrin-mediated and clathrin-independent endocytoses and constitutes a key mechanism for regulation of the viral internalization and infection.
Influenza A virus consists of eight segmented minus stranded RNA, and among the proteins encoded by these segments, nonstructural protein 1 (NS1, encoded on segment 8) regulates suppression of apoptosis induction in host cells (Fig. 1), inhibition of nuclear export of mRNA, and splicing of mRNA by binding U6 small nuclear RNA (Hale et al. 2008). NS1 also binds to double-stranded RNA and, as a consequence, inhibits PKR kinase activity (Chen et al. 1998) and regulates apoptosis induction in host cells not through PI3K (Jackson et al. 2010). Recently, the functional interaction of NS1 with serine threonine kinase Akt, a core intracellular survival regulator, is reported (Fig. 1) (Matsuda et al. 2010). Akt is activated in response to PI3K by a wide variety of growth factors, antigens, and inflammatory stimuli. Activation of PI3K produces PtdIns (3,4,5)P3 (PIP3), which binds to the lipid-binding module of the PH domain of Akt, and induces activation of its downstream signals. It is demonstrated that NS1 directly interacts with Akt and the interaction is mediated primarily through the Akt-PH (pleckstrin homology) domain and the RNA-binding domain of NS1. NS1 preferentially interacts with phosphorylated Akt, but not with non-phosphorylated Akt. Interaction of NS1 with Akt enhances the kinase activity and phosphorylated Akt interacts with NS1 during the interphase of the cell cycle predominantly within the nucleus. Functionally, NS1 activates the signaling pathway to ensure efficient viral replication by enhancing anti-apoptotic responses (Fig. 1).
3 Significance of IFN and Apoptosis Signals During Influenza A Virus Infection
Viral proteins are translated from viral mRNA transcribed by the RNA-dependent RNA polymerase of influenza A virus. Viral polymerase complex is a heterotrimer consisting of polymerase acidic protein (PA), polymerase basic protein 1 (PB1) , and PB2, and each component is crucial for the replication of the virus (Fig. 1) (Neumann et al. 2004). In addition to the function of NS1, it is also shown that the viral polymerase plays an important role for regulating host antiviral response through inhibition of interferon (IFN) β production by the binding to IFNβ promoter stimulator 1 (IPS-1; also called MAVS, Cardif, or VISA) (Fig. 2) (Iwai et al. 2010). IFNβ is an important factor in the activation of host defensive mechanisms against influenza A virus. IPS-1 is a downstream mitochondrial adapter protein that transmits the signal to induce type I IFN through the activation of transcription factors IFN regulatory factor 3 (IRF3), IRF7, and nuclear factor κB (NF-κB) (Seth et al. 2005; Xu et al. 2005; Kawai et al. 2005; Meylan et al. 2005). PB2 or PB2-containing complex inhibits IPS-1-induced activation of IFNβ promoter after influenza A virus infection (Fig. 2) and this function is not competitive with the inhibitory action of NS1 (Pichlmair et al. 2006; Mibayashi et al. 2007; Guo et al. 2007; Opitz et al. 2007).
Inhibition of IPS-1-mediated IFN production by influenza A virus polymerase. The RNA helicase, retinoic acid-inducible gene 1 (RIG-I) is a RNA virus sensor for influenza A virus. Viral RNA is recognized by the helicase domain of RIG-I and interaction through homotypic caspase activation and recruitment domain (CARD) with the interferon promoter-stimulating factor 1 (IPS-1) induces the activation of transcriptional factors, IRF3, AP-1, and NF-kB, by phosphorylation. These activated transcription factors are translocated into the nucleus to induce IFNβ gene expression. Functions of IPS-1 to induce the gene expression are inhibited by the viral polymerase complex of influenza A virus by the direct interaction with IPS-1
Recently, regulation of cellular apoptosis is shown to be significantly important for the host defense system against influenza A virus infection (Iwai et al. 2013). For instance, apoptosis induction is critical for the virus elimination through the removal of the virus-infected cells, and tissue damage during the course of viral infection including multiple organ dysfunction is caused by apoptosis (Hinshaw et al. 1994; Chan 2002). Furthermore, abnormal apoptosis induction of alveolar epithelial cells and lymphocytes is related to the influenza disease symptoms.
Apoptosis is known as a programmed cell death in which the morphological features of apoptotic cells are associated with cytoplasmic shrinkage, plasma membrane blebbing, DNA fragmentation, and chromatin condensation. Finally, the cells form cell fragments, termed apoptotic bodies, and are engulfed by phagocytic cells. Two major apoptosis signals are known as death receptor-mediated signal and mitochondria-mediated signal (Gupta 2001). Death receptors, such as tumor necrosis factor α receptor 1 (TNF-α R1), Fas, death receptor 4 (DR4, TRAILR1), and death receptor 5 (DR5, TRAILR2), are defined by the death domain in their cytoplasmic region and mediate signals to activate caspase-8 (Fig. 3). On the other hand, mitochondrion is an important organelle for the host cells to determine the cell destiny, and generally the mitochondrial membrane potential is disrupted during apoptosis induction. After disruption of the mitochondrial membrane potential, the cytochrome c in the mitochondrial inner membrane is released into the cytoplasm, and caspase-9 is activated. Importantly, these two major apoptosis pathways are crucial for the elimination of influenza A virus by the removal of the virus-infected cells from the body. However, there is a possibility that excessive induction of apoptosis in lung tissue or other organs by influenza A virus infection induces severe illness often leading to death. In fact, we had shown that a variety of types of cells in the lung express FasL, a specific ligand of Fas, after the viral infection and the induction level of FasL gene expression was correlated with the severity of influenza (Fig. 3) (Fujikura et al. 2013). Furthermore, inhibition of Fas/FasL signal by treatment with a recombinant decoy receptor for FasL increases the survival rate of mice after the lethal viral infection. In the future, it might be an effective treatment method of influenza to inhibit the excessive apoptosis signal induced by the viral infection.
Apoptotic signaling pathways induced by influenza A virus infection. Infection of influenza A virus induces the expression of death receptor ligand, TRAIL or FasL on macrophages, DC cells, NK cells, or CD4 T cells, and these ligands stimulate their receptors, DR4/DR5 or Fas, to induce apoptosis in the alveolar epithelial cells. On the other hand, PB2 of influenza A virus binds to the host cellular molecule, Siva-1, to induce the activation of caspases 8 and 9. Siva-1 is involved in the effective viral replication through the activation of these caspases. In addition, DAP3 is essential for death receptor-mediated apoptosis induction and LKB1 or DELE and DAP3 associating protein also might be critical to regulate apoptosis induced by the viral infection
We also had shown that Siva-1, a proapoptotic protein, is crucial for effective replication of influenza A virus (Fig. 3) (Shiozaki et al. 2011). Since Siva-1 function in the viral replication completely disappears after treatment with a pan-caspase inhibitor, Z-VAD fmk, Siva-1 appears to modulate the viral replication by regulation of caspases activation. These results suggest that Siva-1 and caspases are critical targets for the inhibition of the viral propagation.
In addition, death-associated protein 3 (DAP3) is known to be crucial for apoptosis induced by the extrinsic death receptor stimulation (Fig. 3) (Miyazaki and Reed 2001; Kim et al. 2007) and is also related to other IPS-1 functions. A previous report has demonstrated that IPS-1 is also involved in the induction of anoikis (Li et al. 2009), known to be a form of apoptosis induced by anchorage-dependent cells detaching from the surrounding extracellular matrix. In anoikis induction, DAP3 binds to IPS-1 and recruits FADD for activation of caspase-8, and then apoptosis is executed. The DAP3 function in anoikis induction is inhibited by Akt-dependent phosphorylation (Miyazaki et al. 2004), and AKT is activated by the NS1 protein of influenza A virus. Therefore, the DAP3 function inducing anoikis is thought to be inhibited in the virus-infected cells. DAP3 is also crucial for apoptosis induced by TNF-α, FasL, and TRAIL stimulation (Miyazaki and Reed 2001; Kim et al. 2007). Therefore, DAP3 and signaling molecules to mediate the function of DAP3, such as liver kinase B1 (LKB1) (Takeda et al. 2007) and death ligand signal enhancer (DELE) (Harada et al. 2010), are thought to be involved in the viral replication and apoptosis induction caused by the viral infection (Fig. 3). Further investigation of the molecular mechanism of apoptosis induction mediated by these molecules during influenza A virus infection is required and might provide a strategy for the development of novel influenza drugs.
4 Beneficial Effects of Probiotics as Adjuvants of Influenza Vaccine
Oral consumption of Lactobacillus fermentum CECT5716 for co-adjuvant capability was performed to address the immunologic effects of vaccination in human clinical trial (50 volunteers aged 22–56 years, received an oral daily dose of probiotic bacteria 1.0 × 1010 cfu/day for 2 weeks before vaccination and 2 weeks after vaccination) (Olivares et al. 2007). Two weeks after vaccination, the proportion of natural killer cells was increased by the administration of CECT5716. The responses of T-helper type 1, antigen-specific immunoglobulin A and total immunoglobulin M were increased. The incidence of an influenza-like illness during 5 months after the vaccination was lower in the group consuming the probiotic bacteria. Lactobacillus rhamnosus GG (LGG) is also shown to be an important adjuvant to improve influenza vaccine immunogenicity by randomized double-blind placebo-controlled pilot study (42 healthy subjects aged 18–49 years, receiving 1.0 × 1010 cfu of LGG and 295 mg inulin in gelatin capsule, twice daily for 28 days after the vaccination) (Davidson et al. 2011). In the case of the H3N2 influenza A virus, 84 % subjects receiving LGG versus 55 % subjects receiving placebo had Hemagglutinin inhibition titers at day 28 after vaccination.
Infection of influenza A virus leads to lethal diseases, and especially, older adults are higher risk groups to cause serious illness or death by infection. Therefore, to develop drugs or vaccines for prevention or treatment of influenza in older people is very important. To investigate the effect of a probiotic dairy drink on the immune response to the vaccination against influenza viruses in an elderly population over 70 years of age, two randomized, multicenter, double-blind, controlled studies were performed (Boge et al. 2009). A fermented dairy drink, containing the probiotic strain Lactobacillus casei DN-114 001 was consumed twice daily for a period of 7 weeks for the pilot study or 13 weeks for the confirmatory study. These subjects took a vaccine after 4 weeks of the consumption of fermented dairy drink. Geometric mean antibody titers (GMT) against the three viral strains, influenza viruses A(H1N1), A(H3N2), and B, of the vaccine were measured at several time intervals post-vaccination by hemagglutination inhibition test.
The virus-specific antibody titers increased after vaccination, being consistently higher in the probiotic product group compared to the control group in the pilot study. Similarly, in the confirmatory study, antibody titers against the influenza virus B strain increased significantly more in the probiotic group than in the control group. Even 5 months after vaccination, significant differences in seroconversion between the groups were still found and also similar GMT results were observed for the influenza A virus H3N2 and H1N1 strains. These results demonstrate that in older people daily consumption of the probiotic product is effective for the increment of specific antibody responses to influenza vaccination.
Recently, Lactobacillus plantarum CECT7315/7316 is reported to have an immunostimulating effect and could be used to improve the response to the vaccination in elderly person (60 institutionalized volunteers aged 65–85 years, receiving 5.0 × 109 cfu/day of CECT 7315/7316 in 20 g powdered skim milk for 3 months after the vaccination) (Bosch et al. 2012). For the volunteers aged 65–85 years, a randomized, double-blind, placebo-controlled human trial was performed. The consumption of the probiotics strains during 3 months after the vaccination of trivalent influenza vaccine (A/Wisconsin/67/2005 NYMC X-161B (H3N2), A/Solomon Islands/3/2006 (H1N1), and B/Malaysia/2506/2004) increased the levels of virus-specific IgA and IgG antibodies. Moreover, a trend toward an increase in the virus-specific IgM antibodies was also observed. These results suggest that probiotics are good candidates for the effective adjuvants of influenza vaccine. In the future, effects of the probiotics should be examined as effective adjuvants of vaccines against a variety of pathogens.
5 Beneficial Effects of Probiotics on the Prevention of Influenza
In addition to the utility as an adjuvant of vaccine, the consumption of only probiotics is effective for the prevention of influenza virus infection. Heat-killed Lactobacillus plantarum L-137 (HK-LP) stimulates macrophage/dendritic cells to produce T-helper (Th) 1-related cytokines. The effect of oral administration of HK-LP on protection against H1N1 influenza virus A/FM/1/47 infection was examined in mice (Maeda et al. 2009). The survival time was significantly prolonged and the viral titers in the lung were significantly lower in mice treated with HK-LP administration. An appreciable level of IFNβ was detected in the serum of mice treated with HK-LP, suggesting that HK-LP is a potent IFNβ inducer.
Recently, from the screening of 158 bacterial strains, including a majority of lactic acid bacteria, using two different cellular models of tumor necrosis factor alpha (TNF-α) -activated human colon adenocarcinoma grade II cell, HT-29, and peripheral blood mononuclear cell (PBMC), novel candidate probiotics having an immunomodulatory function were identified (Kechaou et al. 2013). Different strains responsive to both models were selected, and their protective effects were tested against influenza virus infection in mice. With daily intragastric administrations after viral infection (H1N1 influenza virus A/Puerto Rico/8/1934 [A/PR8/34]), Lactobacillus plantarum CNRZ1997 was demonstrated to have functions reducing body weight loss, alleviating clinical symptoms, and inhibiting significantly viral replication in the lungs (daily administered intragastrically 1.0 × 109 cfu of each strain suspended in 200 μl of PBS, for 10 days before and 10 or 14 days after virus challenge). This screening method for the probiotic strains to have an immunomodulatory function might be useful strategy to identify the strain, effective for the prevention of influenza.
Since influenza A (H1N1) pdm virus caused the first human pandemic of the twenty-first century, to prevent the infection of this virus strain is very critical to save many people from the next influenza pandemic. The prophylactic efficacy of heat-killed Lactobacillus pentosus b240 against lethal influenza A (H1N1) pdm virus infection was examined in a mouse model. Mice were orally administered heat-killed b240 every day at a dose of 10 mg/mouse, which corresponds to 1.0 × 1010 cell counts in 200 μl of buffered saline for 5 weeks (Kiso et al. 2013). Expression of three acyl-CoA thioesterase (Acots) genes was significantly downregulated in mouse lungs by oral administration of b240. Acots play an important role in the generation of arachidonic acid, the precursor to eicosanoids, responsible for manifestations of inflammation. It suggests that the regulation of Acots expression by b240 might contribute to the recovery of mice from the viral infection by the regulation of inflammatory response. And the expression of the FBJ osteosarcoma oncogene (Fos), early growth response 1 (Egr1), and cysteine-rich, angiogenic inducer, 61 (Cyr61) genes was downregulated by b240 administration. Cyr61 activates IL-6 production, resulting in the progression of inflammation, and the transcription factors Egr1 and Fos are early responders during influenza virus infection. Egr1 is a critical regulator of host inflammatory chemokines and is associated with CD8+ T cell-mediated lung injury in the influenza virus infection. The downregulation of these genes induced by oral administration of b240 may play a role in alleviating pulmonary injury caused by the inflammatory response. In addition, expression of Rsad2 (radical S-adenosyl methionine domain-containing protein 2) gene was upregulated in the lungs of uninfected mice after oral administration of b240. Rsad2 is an interferon-stimulated gene (ISG), induced by IFNs after viral infection. These results suggest that inflammatory responses and ISG expression are regulated by the administration of heat-killed Lactobacillus pentosus b240.
We investigated the effect of lysozyme-treated Enterococcus faecalis FK-23 (LFK) , isolated from human intestinal tract, to prevent influenza in the virus-infected mice (Fukada et al. 2013). Mice were orally administered LFK and infected with influenza virus A/PR8/34 at lethal doses. After the viral infection, the survival rate of the LFK-administered mice was significantly higher than that of control mice. Oral administration of LFK suppressed the excessive infiltration of leukocytes into the lung after viral infection. The arrest was mediated by modulation of pulmonary alveolar–capillary permeability. In fact, expression levels of genes involved in matrix degradation, correlated with vascular permeability, were downregulated in LFK-administered mice. These results suggest that stabilizing the integrity of the alveolar–capillary barrier by the administration of LFK protects mice from death after the viral infection. Furthermore, we examined the efficacy of the water-soluble fraction (SLFK) of LFK against a lethal influenza A virus challenge (Kondoh et al. 2012). Mice were orally administered SLFK and intranasally infected with A/PR8/34 virus. The survival rate of SLFK-administered mice after the viral infection was significantly improved compared with that of control mice. In addition, the mRNA expression level of the anti-inflammatory cytokine interleukin-10 (IL-10 ) in the lung tissues was enhanced by the administration of SLFK. These observations suggest that the oral administration of SLFK exerts a protective effect against influenza virus infection through the activation of the anti-inflammatory response. Taken together, each component of probiotics has a different function to regulate the expression of anti-inflammatory cytokine or genes, critical for stabilizing the integrity of alveolar–capillary barrier. In the future, identification of the substances of these components is required for the development of influenza drugs.
Recently, we studied the immunomodulatory function of Lactobacillus gasseriLG2055 and demonstrated that oral administration of LG2055 increases in the survival rate of mice infected with the A/PR8/34 virus and decreases the ratio of body weight losses by the viral infection (Nakayama et al. 2014). The survival rate of mice tended to improve by the administration in a dose-dependent manner. The oral administration of LG2055 is effective to protect the mice from lethal virus infection, and it might be as a result of that the virus titer in the bronchoalveolar lavage fluid is significantly decreased by LG2055 administration after the virus infection. LG2055 administration induces the mRNA expression of the antiviral ISGs, myxovirus resistance 1 (Mx1), and 2′–5′ oligoadenylate synthetase 1A (Oas1a) in the lung tissues. In addition, Mx1 and IFNβ mRNA were strongly induced in macrophage-like cell, RAW264.7 after LG2055 treatment (Fig. 4). The intestinal cells were stimulated by LG2055 components, and type I IFN produced by these cells including macrophages in the intestine may secondarily stimulate the lung cells or macrophages in the lung for ISG production (Fig. 4). These results indicate that the oral administration of LG2055 is effective on the prevention of influenza by the inhibition of virus replication through upregulation of the expression of antiviral genes.
Induction of the antiviral responses in macrophages by LG2055. Phagocytosis of LG2055 by macrophages is mediated through the M (microfold) cells in the Peyer’s patches of the small intestine. Macrophages secrete pro-inflammatory mediators such as tumor necrosis factor (TNF)α, nitric oxide (NO), and IL-1β, critical for the activation of various antimicrobial mechanisms, including oxidative processes to kill the invading microorganisms. Activated macrophages produce IL-12 to induce the polarization to Th1 cells and NO or superoxide, highly toxic for microorganisms. In addition, transcription of mRNA of antiviral genes, Mx1 and IFNβ, is induced in macrophages by LG2055 stimulation. IFNβ produced by macrophages in the intestine may secondarily stimulate the lung epithelial cells or alveolar macrophages to induce ISG production in the lung
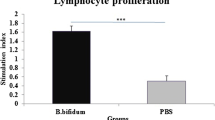
On the other hand, in mucosal immunity, IgA antibodies are very critical for preventing influenza virus transmission and the production of secretory IgA depends on the commensal bacteria and viral antigens in the gastrointestinal tract. IgA is produced by IgA(+) plasma cells, differentiated from IgA(+) B cells, and this differentiation is induced by the intestinal dendritic cells (DCs), stimulated by their antigens incorporated through M cells (Fig. 5). Recently, we have found that oral administration of LG2055 induced IgA production and increased the rate of IgA(+) cell population in Peyer’s patch lamina propria of the mouse small intestine (Fig. 6) (Sakai et al. 2014). This effect of LG2055 was significantly stronger than that of the L. gasseri type strain or of other Lactobacillus species. LG2055 administration markedly increased IgA amount in a co-culture of B cells and bone marrow-derived dendritic cells (BMDCs), and TLR2 signal was critical for this induction of IgA production. In addition, LG2055 stimulated BMDC to promote the production of TGF-β, BAFF, and IL-6, all critical for IgA production from B cells. B cells stimulated with both BAFF and LG2055 enhanced the induction of IgA production (Fig. 6). In these processes, TGF-β signal was critical for LG2055-induced IgA production in the B cell and BMDC co-culture system, but TGF-β did not induce IgA production by only B cells stimulated with LG2055. Furthermore, TGF-β was critical for the production of BAFF, IL-6, IL-10, and TGF-β itself from LG2055-stimulated BMDC. Therefore, TGF-β is produced by BMDC stimulated with LG2055 and it is essential for BMDC to induce the production of BAFF and IL-6 (Fig. 6). LG2055 is effective to induce IgA production by regulation of these cytokines. Induction of IgA production by LG2055 should play an important role in the control of the intestinal microflora and prevention of the infection of pathogenic bacteria and viruses. Other group also identified other probiotic strain, named as Lactobacillus plantarum AYA, stimulating induction of IgA production by murine Peyer’s patch cells (Kikuchi et al. 2014). IL-6 production was induced by this strain in Peyer’s patch dendritic cells, promoting IgA(+) B cells to differentiate into IgA-secreting plasma cells. Oral administration of this probiotic strain increased IgA production in the small intestine and lung in mice. The function of the induction of IgA production was strongly correlated with the activity to protect mice from death after lethal influenza virus infection.
Mechanism of the IgA secretion into the intestinal lumen. In mucosal immunity, IgA antibodies are very critical for preventing the infection of pathogens and maintaining the intestinal homeostasis. The production of secretory IgA by IgA(+) plasma cells and the differentiation from IgM(+) B cells to IgA(+) B cells are induced in the secondary lymphoid tissues (Peyer’s patches and mesenteric lymph nodes). This differentiation is activated by the intestinal DCs, stimulated by their antigens incorporated through M cells. The recruitment of DCs, T cells, and B cells is regulated in the process of immune responses to the microbiota. Stimulated DCs interact with T cells to induce T cell differentiation and T cell-dependent B cell maturation. Differentiated IgA(+) B cells migrate to the draining mesenteric lymph node. Subsequently, the development of IgA(+) plasma cells is induced and these cells leave the mesenteric lymph node and migrate to the blood circulation. IgA(+) plasma cells secrete IgA into the intestinal lumen. Secreted IgA has a function to control the intestinal homeostasis and to protect against the invasive pathogens
Mechanism of IgA production induced by LG2055 in the small intestine. LG2055 induces IgA production and increases the rate of IgA(+) B cell population in Peyer's patch and in the lamina propria of the small intestine. The production of BAFF, TGF-β, IL-6, and IL-10 is upregulated in LG2055-stimulated dendritic cells (DCs). TGF-β and BAFF induce an IgA class-switch recombination. IL-6 and IL-10 induce the differentiation of IgA-producing plasma cells in IgA(+) B cells. TGF-β signal contributes to the production of IL-6, IL-10, BAFF, and TGF-β itself by LG2055-stimulated DCs through the TLR2 signaling pathway. In addition, combined stimulation of B cells with BAFF and LG2055 enhanced the induction of IgA production
In summary, probiotic Lactobacillus strains are effective to prevent influenza as adjuvants of the vaccine, by different mechanisms depending on the strain such as increment of the population of natural killer cells, the response of T-helper type 1, and the amounts of virus-specific IgA, IgG, and IgM. Furthermore, administration of these probiotic strains in mice induced IFNβ production, expression of ISG and antiviral genes to inhibit the viral replication, inhibition of the inflammatory responses, and induction of BAFF, IL-6, and TGF-β to produce IgA by B cells.
Especially, IFNβ is an important factor against the replication of influenza virus. IPS-1 transmits the IFNβ induction through the activation of transcription factors IRF3, IRF7, and NF-κB. In contrast, viral polymerase complex inhibits IPS-1-induced activation of IFNβ promoter. Therefore, the effect and mechanism for the regulation of these signaling molecules by probiotics should be studied in the future. In addition, since inhibition of excessive apoptosis induction by Fas/FasL was effective to protect mice from death by the viral infection, significance of the function of other death receptors, such as TNFαR1, DR4, and DR5, should be clarified. Furthermore, signaling molecules, Siva-1, DAP3, and DELE, might be involved in the viral replication and apoptosis induction caused by the viral infection. Further investigation of the effects on the regulation of the function or expression of these molecules by the administration of probiotics during influenza virus infection is required and might lead to the development of novel influenza drugs or vaccine adjuvants.
References
Bäckhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, Semenkovich CF, Gordon JI (2004) The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci USA 101(44):15718–15723
Boge T, Rémigy M, Vaudaine S, Tanguy J, Bourdet-Sicard R, van der Werf S (2009) A probiotic fermented dairy drink improves antibody response to influenza vaccination in the elderly in two randomised controlled trials. Vaccine 27(41):5677–5684. doi:10.1016/j.vaccine.2009.06.094
Bosch M, Méndez M, Pérez M, Farran A, Fuentes MC, Cuñé J (2012) Lactobacillus plantarum CECT7315 and CECT7316 stimulate immunoglobulin production after influenza vaccination in elderly. Nutr Hosp 27(2):504–509. doi:10.1590/S0212-16112012000200023
Cani PD, Bibiloni R, Knauf C, Waget A, Neyrinck AM, Delzenne NM, Burcelin R (2008) Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57:1470–1481
Chan PK (2002) Outbreak of avian influenza A(H5N1) virus infection in Hong Kong in 1997. Clin Infect Dis 34(Suppl 2):S58–S64
Chen Z, Li Y, Krug RM (1998) Chimeras containing influenza NS1 and HIV-1 Rev protein sequences: mechanism of their inhibition of nuclear export of Rev protein–RNA complexes. Virology 241:234–250
Corthésy B (2013) Multi-faceted functions of secretory IgA at mucosal surfaces. Front Immunol 4:185
Davidson LE, Fiorino AM, Snydman DR, Hibberd PL (2011) Lactobacillus GG as an immune adjuvant for live-attenuated influenza vaccine in healthy adults: a randomized double-blind placebo-controlled trial. Eur J Clin Nutr 65(4):501–507. doi:10.1038/ejcn.2010.289
Fujikura D, Chiba S, Muramatsu D, Kazumata M, Nakayama Y, Kawai T, Akira S, Kida H, Miyazaki T (2013) Type-I interferon is critical for FasL expression on lung cells to determine the severity of influenza. PLoS One 8(2), e55321. doi:10.1371/journal.pone.0055321
Fujioka Y, Tsuda M, Hattori T, Sasaki J, Sasaki T, Miyazaki T, Ohba Y (2011) The Ras-PI3K signaling pathway is involved in clathrin-independent endocytosis and the internalization of influenza viruses. PLoS One 6(1), e16324. doi:10.1371/journal.pone.0016324
Fujioka Y, Tsuda M, Nanbo A, Hattori T, Sasaki J, Sasaki T, Miyazaki T, Ohba Y (2013) A Ca(2+)-dependent signalling circuit regulates influenza A virus internalization and infection. Nat Commun 4:2763. doi:10.1038/ncomms3763
Fukada K, Fujikura D, Nakayama Y, Kondoh M, Shimada T, Miyazaki T (2013) Enterococcus faecalis FK-23 affects alveolar-capillary permeability to attenuate leukocyte influx in lung after influenza virus infection. Springerplus 2(1):269. doi:10.1186/2193-1801-2-269
Guo Z, Chen LM, Zeng H, Gomez JA, Plowden J, Fujita T, Katz JM, Donis RO, Sambhara S (2007) NS1 protein of influenza A virus inhibits the function of intracytoplasmic pathogen sensor, RIG-I. Am J Respir Cell Mol Biol 36(3):263–269
Gupta S (2001) Molecular steps of death receptor and mitochondrial pathways of apoptosis. Life Sci 69(25-26):2957–2964
Hale BG, Randall RE, Ortin J, Jackson D (2008) The multifunctional NS1 protein of influenza A viruses. J Gen Virol 89:2359–2376
Harada T, Iwai A, Miyazaki T (2010) Identification of DELE, a novel DAP3-binding protein which is crucial for death receptor-mediated apoptosis induction. Apoptosis 15(10):1247–1255. doi:10.1007/s10495-010-0519-3
Hinshaw VS, Olsen CW, Dybdahl-Sissoko N, Evans D (1994) Apoptosis: a mechanism of cell killing by influenza A and B viruses. J Virol 68:3667–3673
Iwai A, Shiozaki T, Kawai T, Akira S, Kawaoka Y, Takada A, Kida H, Miyazaki T (2010) Influenza A virus polymerase inhibits type I interferon induction by binding to interferon beta promoter stimulator 1. J Biol Chem 285(42):32064–32074. doi:10.1074/jbc.M110.112458
Iwai A, Shiozaki T, Miyazaki T (2013) Relevance of signaling molecules for apoptosis induction on influenza A virus replication. Biochem Biophys Res Commun 441(3):531–537. doi:10.1016/j.bbrc.2013.10.100
Jackson D, Killip MJ, Galloway CS, Russell RJ, Randall RE (2010) Loss of function of the influenza A virus NS1 protein promotes apoptosis but this is not due to a failure to activate phosphatidylinositol 3-kinase (PI3K). Virology 396:94–105
Kadooka Y, Tominari K, Sakai F, Yasui H (2012) Prevention of rotavirus-induced diarrhea by preferential secretion of IgA in breast milk via maternal administration of Lactobacillus gasseri SBT2055. J Pediatr Gastroenterol Nutr 55:66–71
Kalliomäki M, Salminen S, Arvilommi H, Kero P, Koskinen P, Isolauri E (2001) Probiotics in primary prevention of atopic disease: a randomised placebo-controlled trial. Lancet 357(9262):1076–1079
Kawai T, Takahashi K, Sato S, Coban C, Kumar H, Kato H, Ishii KJ, Takeuchi O, Akira S (2005) IPS-1, an adaptor triggering RIG-I- and Mda5-mediated type I interferon induction. Nat Immunol 6(10):981–988
Kechaou N, Chain F, Gratadoux JJ, Blugeon S, Bertho N, Chevalier C, Le Goffic R, Courau S, Molimard P, Chatel JM, Langella P, Bermúdez-Humarán LG (2013) Identification of one novel candidate probiotic Lactobacillus plantarum strain active against influenza virus infection in mice by a large-scale screening. Appl Environ Microbiol 79(5):1491–1499. doi:10.1128/AEM.03075-12
Kikuchi Y, Kunitoh-Asari A, Hayakawa K, Imai S, Kasuya K, Abe K, Adachi Y, Fukudome S, Takahashi Y, Hachimura S (2014) Oral administration of Lactobacillus plantarum strain AYA enhances IgA secretion and provides survival protection against influenza virus infection in mice. PLoS One 9(1), e86416. doi:10.1371/journal.pone.0086416. eCollection 2014
Kim HR, Chae HJ, Thomas M, Miyazaki T, Monosov A, Monosov E, Krajewska M, Krajewski S, Reed JC (2007) Mammalian dap3 is an essential gene required for mitochondrial homeostasis in vivo and contributing to the extrinsic pathway for apoptosis. FASEB J 21(1):188–196
Kiso M, Takano R, Sakabe S, Katsura H, Shinya K, Uraki R, Watanabe S, Saito H, Toba M, Kohda N, Kawaoka Y (2013) Protective efficacy of orally administered, heat-killed Lactobacillus pentosus b240 against influenza A virus. Sci Rep 3:1563. doi:10.1038/srep01563
Kleerebezem M, Vaughan EE (2009) Probiotic and gut lactobacilli and bifidobacteria: molecular approaches to study diversity and activity. Annu Rev Microbiol 63:269–290. doi:10.1146/annurev.micro.091208.073341
Kondoh M, Fukada K, Fujikura D, Shimada T, Suzuki Y, Iwai A, Miyazaki T (2012) Effect of water-soluble fraction from lysozyme-treated Enterococcus faecalis FK-23 on mortality caused by influenza A virus in mice. Viral Immunol 25(1):86–90. doi:10.1089/vim.2011.0056
Ley RE, Turnbaugh PJ, Klein S, Gordon JI (2006) Microbial ecology: human gut microbes associated with obesity. Nature 444:1022–1023
Li M, Wang B, Zhang M, Rantalainen M, Wang S, Zhou H, Zhang Y, Shen J, Pang X, Zhang M, Wei H, Chen Y, Lu H, Zuo J, Su M, Qiu Y, Jia W, Xiao C, Smith LM, Yang S, Holmes E, Tang H, Zhao G, Nicholson JK, Li L, Zhao L (2008) Symbiotic gut microbes modulate human metabolic phenotypes. Proc Natl Acad Sci USA 105:2117–2122
Li HM, Fujikura D, Harada T, Uehara J, Kawai T, Akira S, Reed JC, Iwai A, Miyazaki T (2009) IPS-1 is crucial for DAP3-mediated anoikis induction by caspase-8 activation. Cell Death Differ 16(12):1615–1621. doi:10.1038/cdd.2009.97
Maeda N, Nakamura R, Hirose Y, Murosaki S, Yamamoto Y, Kase T, Yoshikai Y (2009) Oral administration of heat-killed Lactobacillus plantarum L-137 enhances protection against influenza virus infection by stimulation of type I interferon production in mice. Int Immunopharmacol 9(9):1122–1125. doi:10.1016/j.intimp.2009.04.015
Matsuda M, Suizu F, Hirata N, Miyazaki T, Obuse C, Noguchi M (2010) Characterization of the interaction of influenza virus NS1 with Akt. Biochem Biophys Res Commun 395(3):312–317. doi:10.1016/j.bbrc.2010.03.166
Mazmanian SK, Round JL, Kasper DL (2008) A microbial symbiosis factor prevents intestinal inflammatory disease. Nature 453:620–625
Medina RA, García-Sastre A (2011) Influenza A viruses: new research developments. Nat Rev Microbiol 9(8):590–603. doi:10.1038/nrmicro2613
Meylan E, Curran J, Hofmann K, Moradpour D, Binder M, Bartenschlager R, Tschopp J (2005) Cardif is an adaptor protein in the RIG-I antiviral pathway and is targeted by hepatitis C virus. Nature 437:1167–1172
Mibayashi M, Martínez-Sobrido L, Loo YM, Cárdenas WB, Gale M Jr, García-Sastre A (2007) Inhibition of retinoic acid-inducible gene I-mediated induction of beta interferon by the NS1 protein of influenza A virus. J Virol 81:514–524
Miyazaki T, Reed JC (2001) A GTP-binding adapter protein couples TRAIL receptors to apoptosis-inducing proteins. Nat Immunol 2(6):493–500
Miyazaki T, Shen M, Fujikura D, Tosa N, Kim HR, Kon S, Uede T, Reed JC (2004) Functional role of death-associated protein 3 (DAP3) in anoikis. J Biol Chem 279(43):44667–44672
Nakayama Y, Moriya T, Sakai F, Ikeda N, Shiozaki T, Hosoya T, Nakagawa H, Miyazaki T (2014) Oral administration of Lactobacillus gasseri SBT2055 is effective for preventing influenza in mice. Sci Rep 4:4638. doi:10.1038/srep04638
Neumann G, Brownlee GG, Fodor E, Kawaoka Y (2004) Orthomyxovirus replication, transcription, and polyadenylation. Curr Top Microbiol Immunol 283:121–143
Nicholson JK, Holmes E, Wilson ID (2005) Gut microorganisms, mammalian metabolism and personalized health care. Nat Rev Microbiol 3(5):431–438, Review
Olivares M, Díaz-Ropero MP, Sierra S, Lara-Villoslada F, Fonollá J, Navas M, Rodríguez JM, Xaus J (2007) Oral intake of Lactobacillus fermentum CECT5716 enhances the effects of influenza vaccination. Nutrition 23(3):254–260
Opitz B, Rejaibi A, Dauber B, Eckhard J, Vinzing M, Schmeck B, Hippenstiel S, Suttorp N, Wolff T (2007) IFN beta induction by influenza A virus is mediated by RIG-I which is regulated by the viral NS1 protein. Cell Microbiol 9(4):930–938
Pichlmair A, Schulz O, Tan CP, Näslund TI, Liljeström P, Weber F, Reis e Sousa C (2006) RIG-I-mediated antiviral responses to single-stranded RNA bearing 5'-phosphates. Science 314:997–1001
Reid G, Jass J, Sebulsky MT, McCormick JK (2003) Potential uses of probiotics in clinical practice. Clin Microbiol Rev 16(4):658–672
Sakai F, Hosoya T, Ono-Ohmachi A, Ukibe K, Ogawa A, Moriya T, Kadooka Y, Shiozaki T, Nakagawa H, Nakayama Y, Miyazaki T (2014) Lactobacillus gasseri SBT2055 induces TGF-β expression in dendritic cells and activates TLR2 signal to produce IgA in the small intestine. PLoS One 9(8), e105370. doi:10.1371/journal.pone.0105370. eCollection
Sato M, Uzu K, Yoshida T, Hamad EM, Kawakami H, Matsuyama H, Abd El-Gawad IA, Imaizumi K (2008) Effects of milk fermented by Lactobacillus gasseri SBT2055 on adipocyte size in rats. Br J Nutr 99:1013–1017
Seth RB, Sun L, Ea CK, Chen ZJ (2005) Identification and characterization of MAVS, a mitochondrial antiviral signaling protein that activates NF-kappaB and IRF 3. Cell 122:669–682
Shiozaki T, Iwai A, Kawaoka Y, Takada A, Kida H, Miyazaki T (2011) Requirement for Siva-1 for replication of influenza A virus through apoptosis induction. J Gen Virol 92(Pt 2):315–325. doi:10.1099/vir.0.028316-0
Takeda S, Iwai A, Nakashima M, Fujikura D, Chiba S, Li HM, Uehara J, Kawaguchi S, Kaya M, Nagoya S, Wada T, Yuan J, Rayter S, Ashworth A, Reed JC, Yamashita T, Uede T, Miyazaki T (2007) LKB1 is crucial for TRAIL-mediated apoptosis induction in osteosarcoma. Anticancer Res 27(2):761–768
Taubenberger JK, Morens DM (2010) Influenza: the once and future pandemic. Public Health Rep 125(Suppl 3):16–26
Wen L, Ley RE, Volchkov PY, Stranges PB, Avanesyan L, Stonebraker AC, Hu C, Wong FS, Szot GL, Bluestone JA, Gordon JI, Chervonsky AV (2008) Innate immunity and intestinal microbiota in the development of Type 1 diabetes. Nature 455:1109–1113
Xu LG, Wang YY, Han KJ, Li LY, Zhai Z, Shu HB (2005) VISA is an adapter protein required for virus-triggered IFN-beta signaling. Mol Cell 19:727–740
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Miyazaki, T. (2015). Efficacy of Probiotics in Prevention of Influenza. In: Liong, MT. (eds) Beneficial Microorganisms in Medical and Health Applications. Microbiology Monographs, vol 28. Springer, Cham. https://doi.org/10.1007/978-3-319-23213-3_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-23213-3_6
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-23212-6
Online ISBN: 978-3-319-23213-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)