Abstract
Lung cancer is currently the leading global cause of cancer death, accounting for 18 % of all cancer deaths (CA Cancer J Clin; 61(2):69–90, 2011). The global lung cancer epidemic is largely due to a single predominant cause: cigarette smoking. In addition to cigarette smoking and other forms of combustible tobacco, many other environmental risk factors and clinical risk indicators for lung cancer have been identified. The potential influence of dietary factors on lung cancer risk has been a topic of considerable interest in recent decades, and a substantial body of evidence has now been generated on this topic.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Lung cancer
- Epidemiology
- Cigarette smoking
- Tobacco
- Diet
- Nutrition
- Fruits
- Vegetables
- Micronutrients
- Chemoprevention
- Body mass index
- Beverages
-
Cigarette smoking is the single major determinant of lung cancer risk.
-
Cigarette smokers are more likely to have unhealthful diets than nonsmokers, which makes it complex to study nutrition and diet in relation to lung cancer.
-
Higher dietary intakes of fruits, and to a lesser extent vegetables, are inversely associated with the risk of lung cancer.
-
Factors with weak evidence of association with increased risk of lung cancer include consumption of red and processed meat, total fat, and lower body mass index.
1 Introduction
Lung cancer is currently the leading global cause of cancer death, accounting for 18 % of all cancer deaths [1]. The global lung cancer epidemic is largely due to a single predominant cause: cigarette smoking. In addition to cigarette smoking and other forms of combustible tobacco, many other environmental risk factors and clinical risk indicators for lung cancer have been identified. The potential influence of dietary factors on lung cancer risk has been a topic of considerable interest in recent decades, and a substantial body of evidence has now been generated on this topic.
2 Descriptive Epidemiology of Lung Cancer
Lung cancer is a significant public health problem. In the USA, lung cancer is the third most common form of cancer and is by far the leading cause of cancer mortality. Approximately 224,000 new cases of lung cancer were diagnosed in the USA in 2014 [2]. By itself, lung cancer accounts for as many deaths as the next four leading causes of cancer death (breast, prostate, colorectal, and pancreatic cancer) combined [2]. Lung cancer is the leading cause of cancer death among both men and women [3]. Lung cancer is a leading global health problem as the leading cause of cancer death in world [1].
The high mortality rate for lung cancer is a function of a high incidence rate combined with a poor survival rate. The 5-year relative survival rate for lung cancer has improved only slightly during the past decades, increasing from 14 % in 1985–1989 to 18 % in 2004–2010 [3]. Five-year relative survival is considerably better for local disease (54 %) compared to a lung cancer diagnosis with regional spread (27 %) or distant disease (4 %) [3].
Lung cancer rarely occurs in individuals younger than 45 years of age, but the incidence rates start to increase among those 45–64 years old and peak in the elderly, with rates of 272 per 100,000 or higher for all age groups 65 and older [3]. Men have greater risk of developing and dying from lung cancer than women. This is not due to an inherent difference in susceptibility to lung cancer risk factors, but rather due to gender differences in historical patterns of smoking prevalence and exposure to other lung cancer risk factors [4]. African Americans have the highest lung cancer incidence rates of any racial/ethnic group, which is due specifically to extremely high rates in African American men [5]. With respect to trends over time in the USA, there has been a steady decrease in the age-adjusted incidence rates (per 100,000) from 69.5 in 1992 to 56.6 in 2011 [3]. This decrease can largely be attributed to the decreased smoking prevalence that began in the mid-1960s [6].
3 Socioeconomic Status
Indicators of lower socioeconomic status (SES) such as lower income and education have been consistently associated with increased lung cancer risk. The association between lower SES and increased lung cancer risk was observed decades ago in the USA [7], but is also a consistent finding across countries and cultures [8–11]. Lower SES is associated with a high-risk profile for many factors associated with lung cancer risk including smoking and exposures to inhaled carcinogens in the workplace and general environment. Lower SES is also associated with less healthful diets [12]. Nutrition and dietary factors may therefore be a contributing factor to the disproportionate burden of lung cancer observed in the lower socioeconomic status groups.
4 Histopathology
As classified by light microscopy, the four major histologic types of lung cancer are adenocarcinoma, squamous cell carcinoma, large cell carcinoma, and small cell carcinoma. All four histologic types are caused by cigarette smoking, but the magnitude of risks across types varies [13, 14]. Clinically, diagnosis is dichotomized into classifications of small cell (about 15 % of lung cancers) or non-small cell lung cancer (about 85 %) because small cell lung cancer has high metastatic potential to the central nervous system and, as opposed to non-small cell lung cancer, surgery is not the backbone of curative intent therapy.
The histologic characteristics of lung cancer have changed in recent decades, with an increase in adenocarcinoma and decrease in squamous cell carcinoma. The shift to adenocarcinoma is thought to be due to alterations in cigarette manufacturing over time leading to changes in (1) smoking-delivered carcinogens and (2) how cigarettes are smoked, such as depth of inhalation [14].
Beyond the histopathologic definitions of cancer, molecular characterization plays an increasingly important role in the definition of cancers of the lung and guiding its treatment. Adenocarcinoma of the lung is now routinely tested for mutations and genetic events in genes such as the epidermal growth factor receptor (EGFR) and translocations involving anaplastic lymphoma kinase (ALK) and c-ros oncogene 1 (ROS1) which predict clinical sensitivity to oral tyrosine kinase inhibitors.
5 Risk Factors for Lung Cancer
Epidemiologic research has succeeded in identifying several environmental risk factors that are causally associated with the risk of developing lung cancer. A brief consideration of well-established risk factors for lung cancer is essential to provide context for interpreting the evidence on the potential role of diet and nutrition in human lung carcinogenesis.
5.1 Tobacco Products
5.1.1 Cigarette Smoking
Cigarette smoking is the predominant cause of lung cancer [15]. The link between cigarette smoking and lung cancer is so strong that after accounting for a latency period of approximately 20 years, smoking prevalence and rates of lung cancer track closely at the population level [16]. Cigarette smoking is primarily responsible for the worldwide lung cancer epidemic as it is associated with such enormous increases in risk of developing lung cancer and cigarette smoking is so common [17].
The risk of lung cancer associated with cigarette smoking follows clear dose-response relationships [14]. This remains true with respect to the number of cigarettes smoked per day and the duration of smoking. Lung cancer risk decreases in those who quit smoking compared to persistent smokers, but not to the level of those who never smoked [18].
Menthol is a flavoring agent added to cigarettes, and menthol cigarettes have been hypothesized to be associated with higher risk of lung cancer than non-menthol cigarettes. The evidence, however, does not support this hypothesis. Numerous case–control [19–23] and cohort [24–26] studies indicate that menthol cigarettes are not associated with a greater risk of lung cancer than non-menthol cigarettes.
The trends in the composition of cigarettes over time, such as the addition of filters and advertised lower tar and nicotine concentrations, would suggest the hypothesis that risks of lung cancer associated with cigarette smoking would have decreased over time. However, contrary to expectation, the smoking-associated risks of lung cancer have actually increased over time [27]. Three US cohorts were followed from 1959 to 1965, 1982 to 1988, and 2000 to 2010. Among women, the relative risks of lung cancer in current versus never smokers increased across these time periods from 2.7 to 12.6 to 26.2, respectively; among men, the relative risks increased from 12.5 to 25.3 to 27.3, respectively. The reasons underlying the increase in risk over time are uncertain, but are hypothesized to be related to changes in tobacco processing and additives.
5.1.2 Other Combustible Tobacco Products
Combustible tobacco products other than cigarettes are also associated with increased risk of lung cancer. Pipes and cigars are causally associated with lung cancer, even though the risks are less than observed for cigarette smoking due to differences in smoking frequency and smoking topography in pipe/cigar smokers compared to cigarette smokers [15]. Pipe and cigar smoke contain a similar profile of harmful toxins as cigarette smoke, but a key determinant of the observed epidemiologic differences in health risks is that compared to cigarette smokers, the tendency is for pipe and cigar smokers to smoke less frequently and to inhale the smoke less deeply. As a result of the difference in the way pipes and cigars are smoked compared with cigarettes, the end result is that the dose of toxins delivered to the smoker is often less for pipes and cigars than for cigarettes [15].
Smoking tobacco through a waterpipe is referred to by a number of terms including “hookah .” In a meta-analysis of data from four studies waterpipe tobacco smoking was significantly associated with increased lung cancer risk (OR 2.1; 95 % CI 1.3–4.2) [28]. The relatively sparse evidence thus far indicates that waterpipe tobacco smoking is associated with a significantly increased risk of lung cancer, but further research on this topic is needed.
5.1.3 Vaporized Nicotine Products
The marketplace for tobacco products and devices that deliver nicotine has been expanding during the past decade [29–32]. Vaporized nicotine products such as electronic cigarettes (or “e-cigarettes”) are nicotine delivery devices that have experienced a rapid upsurge in use and are now marketed by the major US tobacco companies [29, 30]. There is currently a lack of data on whether these products are associated with lung cancer risk. A product such as the e-cigarette that would decrease delivery of tobacco toxins would ostensibly also reduce the risk of developing lung cancer if current cigarette smokers were to switch from cigarettes to exclusive use of the e-cigarette. By contrast, however, the risk of lung cancer could be increased if the e-cigarette maintained nicotine addiction and its users also continued to smoke cigarettes as well as use multiple products that deliver nicotine or if e-cigarette use served as a gateway to the uptake of combustible tobacco products such as cigarettes. Additionally, the risks of nicotine exposure are not eliminated by electronic nicotine delivery systems as nicotine itself has been reported to promote tumor growth and the nonuniform standard of manufacture of device refills and vaporizer delivery technology has led to concerns about the generation of delivery of carcinogenic materials and combustible toxins [33, 34].
5.1.4 Secondhand Tobacco Smoke Exposure
There is currently no “safe level” of exposure to cigarette smoke, as even the secondhand tobacco smoke inhaled by nonsmokers involuntarily in ambient air is causally associated with lung cancer [35]. As expected given the fact that the doses of exposure to cigarette smoke are much lower for secondhand smoke exposure than for active cigarette smoking, the risk of lung cancer is also much less than for active cigarette smoking. This association has had major policy implications such as by providing justification for smoke-free workplace legislation.
5.2 Factors Other than Tobacco
Smoking cigarettes and other combustible tobacco products are the major determinants of the population burden of lung cancer. However, many other risk factors for lung cancer have been identified. The most important of these are briefly summarized below.
5.2.1 Occupational Exposures
Numerous occupational lung carcinogens have been identified; the substances involved include radon, arsenic, asbestos, chromium, chloromethyl ethers, nickel, and polycyclic aromatic hydrocarbons [36, 37]. Synergism with smoking has been shown for several of these agents, such as asbestos and radon [38]. Many other agents are suspected occupational carcinogens.
5.2.2 Indoor and Outdoor Air Pollution
By exposing the lung to air contaminants from combustion sources that generate polycyclic aromatic hydrocarbons and radionuclides, outdoor air pollution is associated with increased risk of lung cancer [39]. Indoor air pollution is also associated with lung cancer risk. The sources and composition of lung carcinogen exposure in indoor air vary with the setting but may include radon, tobacco smoke, smoke from wood or coal burning, and cooking fumes [40–43].
5.2.3 Family History and Inherited Predisposition
A positive family history of lung cancer is a clinically useful risk indicator. In analyses of pooled data from 24 case–control studies, those with a positive history of lung cancer in a first-degree relative had a 1.5-fold increased risk of lung cancer (95 % CI 1.4–1.6). When analyses were limited to never smokers the association was weaker but still statistically significant (OR 1.3; 95 % CI 1.03–1.5) [44].
The observed familial aggregation of lung cancer suggests that genetic factors may influence susceptibility. There have been no clinically relevant high-risk mutations with high penetrance for lung cancer identified as with disease-conferring BRCA1 and BRCA2 mutations in breast cancer. However, data from genome-wide association studies (GWAS) have provided promising leads with respect to low-penetrance germline variants that are associated with small increases in lung cancer risk [45]. For example, the results of GWAS have been remarkably consistent in identifying genetic variants within a region on the long arm of chromosome 15 that are associated with lung cancer risk; those with at least one variant allele of a specific SNP in this region (rs8034191) had a 1.3-fold greater risk of lung cancer than those homozygous for the wild-type allele.
5.2.4 Physical Activity
In a consideration of the role of diet in relation to lung cancer it is important to consider the evidence on physical activity because it is also a lifestyle factor and because of the interrelationship between diet and physical activity. A meta-analysis of leisure-time activity observed that both moderate and high levels of physical activity were associated with a 13–30 % decrease in lung cancer risk [46]. In a meta-analysis of physical activity and lung cancer specific to smokers, the overall association was consistent with an 18 % reduction in risk; there was some heterogeneity in the magnitude of the associations across categories of physical activity, smoking intensity, and gender but the associations remained statistically significant in all of these subgroups [47]. In a thorough narrative review of the epidemiologic evidence, physical activity was consistently observed to be associated with a >20 % reduction in lung cancer risk across studies [48]. The mechanistic basis for how physical activity could protect against lung cancer remains to be established, but current hypotheses include (1) improved lung function accelerating clearance of carcinogens; (2) reduced inflammation and enhanced immune status; and (3) changes in concentrations of growth factors [48].
An inverse and relatively strong statistical relationship between physical activity and lung cancer risk has clearly been documented. The inferences from this evidence will be strengthened if the specific biologic mechanism whereby physical activity reduces lung cancer risk can be pinpointed and the potential for residual confounding by cigarette smoking is more strongly addressed.
5.2.5 Clinical Risk Indicators for Lung Cancer
Several clinical risk indicators have been documented to be more prevalent in lung cancer patients than the general population. Even though the exact etiologic significance of these associations has yet to be clearly elucidated, these are useful clinically. In addition to a family history of lung cancer, increased risk of lung cancer has been noted for several acquired lung diseases. This includes obstructive lung disease, such as chronic obstructive pulmonary disease, as well as fibrotic disease, such as idiopathic pulmonary fibrosis and systemic sclerosis [36]. Further, the presence of infections, such as with tuberculosis or HIV, is associated with increased risk of lung cancer [36]. Known risk factors and clinical risk indicators for lung cancer are summarized in Table 8.1.
5.3 Diet and Nutrition
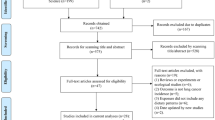
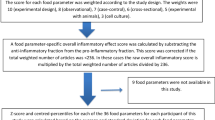
The background provided above has emphasized the known risk factors for lung cancer outside the domain of diet and nutrition. This background provides essential contextual information for considering the potential role of dietary factors in the etiology of lung cancer, highlighting the fact that many well-established risk factors for lung cancer have been identified (Fig. 8.1). The key message from this background information is that cigarette smoking is far and away the leading cause of lung cancer. This is of central importance to a consideration of the role of diet and lung cancer for several reasons. Not only is cigarette smoking the overwhelming cause of lung cancer, but smokers also tend to eat less healthful diets than nonsmokers [49]. Cigarette smoking thus poses significant inferential challenges to establishing a clear role for dietary factors in the etiology of lung cancer. Specifically, this set of circumstances means that cigarette smoking is a major potential confounder that needs to be carefully considered when evaluating a potential role for dietary factors in relation to lung cancer risk, making it difficult to disentangle the potential impact of cigarette smoking on any observed association between a dietary factor and lung cancer (Fig. 8.2). Complicating matters further is that cigarette smoke can directly affect nutritional biomarkers; for example, smokers tend to have lower levels of circulating antioxidant micronutrients even after accounting for differences in dietary intake, implying that the oxidative stress from cigarette smoke leads to depletion of antioxidant micronutrients [49, 50]. Similar associations have even been noted for secondhand smoke exposure [50, 51].
Additionally, associations between dietary factors and lung cancer risk are likely to be far weaker than the association with active smoking. As discussed below, even for dietary factors that have a robust inverse association with lung cancer the associations are very weak compared to the strong increased risk caused by cigarette smoking. Thus, in interpreting evidence on the associations between dietary factors and lung cancer, residual confounding by cigarette smoking is not easily dismissed as a potential explanation. The facts that cigarette smoking is so closely intertwined with risk of lung cancer and with diet and biomarkers of diet underscore not only the complexities involved in studies of diet in relation to lung cancer, but also the imperative to control cigarette smoking as carefully as possible.
The potential role of dietary factors on risk of lung cancer has been extensively investigated. To provide a synopsis of the research in this area, evidence concerning relationships between lung cancer and fruits, vegetables, micronutrients, phytochemicals, fat, body mass index, beverages, and meat intake is described below. To provide a guide for assessing the evidence for each dietary factor, evidence ratings from an objective assessment of the world’s evidence on these topics, summarized in a seminal 2007 report of the World Cancer Research Fund (WCRF), are used for factors that were assigned evidence ratings. The rating scale used included evidence ratings of “convincing,” “probable,” and “limited—suggestive” for whether a dietary factor was associated with increased or decreased risk of lung cancer. Key research published since the 2007 WCRF report are used to augment the review.
5.4 Fruit Intake
In total, the epidemiologic evidence strongly points toward greater levels of fruit consumption being inversely associated with lung cancer risk. Based on a large and consistent body of data, the WCRF systematic review rated the evidence on this topic as “probable” that fruit consumption is associated with decreased risk of lung cancer [52]. Prospective cohort studies published since the 2007 WCRF report provide at least modest support for the premise that fruit consumption protects against lung cancer [53–55]. In the Shanghai Men’s Health Study, any level of fruit consumption above the lowest fourth of total fruit intake was associated with a 24–25 % reduction in lung cancer risk [53]. In the European Prospective Investigation into Cancer and Nutrition (EPIC), the RR for the highest-versus-lowest fifth comparison was 0.80 (95 % CI 0.66–0.96, p-for-trend 0.01). In the NIH-AARP Diet and Health Study, the highest-versus-lowest fifth of total fruit consumption relative risk (RR) was 0.91 (p-for-trend 0.10) in men and 0.97 (p-for-trend 0.70) in women [55]. In the studies that stratified by smoking status, there was no clear pattern in the associations across the categories of never, former, and current smokers [54, 55]. In the EPIC study the results were stratified by histologic type, but no clear pattern emerged to suggest that fruit intake was clearly more strongly associated with specific histologic types of lung cancer than other histologic types [54].
In general, no clear pattern emerges when studies have examined specific fruits or classes of fruits. For example, in the studies cited above, berry intake was significantly associated with lower lung cancer risk in the EPIC Cohort [54] whereas in the Shanghai Men’s Health Study a significant inverse association was observed for watermelon intake and a borderline association with citrus fruits [53].
5.5 Vegetable Intake
Paralleling the evidence for fruit consumption, the overall body of epidemiologic evidence suggests vegetable consumption is inversely associated with lung cancer risk. However, the results for a link between vegetable intake and lung cancer have been less consistent and the observed associations have been weaker than for fruit. Reflecting the more equivocal evidence that vegetable intake may exert protection against lung cancer, the WCRF report rated the overall evidence for vegetables as “limited—suggestive” [52].
Since the publication of the 2007 WCRF report, results of prospective cohort studies have been published in the same reports that catalogued results for fruit intake [53–55]. In the Shanghai Men’s Health Study, any level of vegetable consumption above the lowest fourth of total vegetable intake was associated with a 10–12 % reduction in lung cancer risk that was not statistically significant [53]. In the European Prospective Investigation into Cancer and Nutrition (EPIC), the RR for the highest-versus-lowest fifth comparison was 0.96 (95 % CI 0.79–1.17, p-for-trend 0.58). In the NIH-AARP Diet and Health Study, the highest-versus-lowest fifth of total vegetable consumption relative risk (RR) was 0.93 (p-for-trend 0.08) in men and 1.05 (p-for-trend 0.23) in women [55]. The results of these three more recently published data from prospective cohort studies reinforce an overall body of evidence that demonstrates much less compelling evidence to support an inverse association between vegetable intake and lung cancer risk than which exists for fruit intake. This same observation was noted in a review limited to data from Japan [56].
In one study that stratified by smoking status a strong and statistically significant inverse dose–response trend was evident in former smokers [55], but this finding was not replicated in another study that stratified according to never, former, and current smokers [54]. In the EPIC study the results were stratified by histologic type and no clear pattern emerged to suggest a differential impact of vegetable intake by histologic type [54].
For specific classes of vegetables, such as cruciferous vegetables, the results have been more strongly and consistently associated with a reduced risk of lung cancer than for total vegetable intake. A systematic review and meta-analysis revealed a consistent body of evidence has been observed across studies indicating that cruciferous vegetable intake is inversely associated with lung cancer risk [57]. In studies published since the systematic review, the inverse association between cruciferous vegetable intake and lung cancer risk has persisted even when cigarette smoking has been carefully controlled for in the study design by matching [58, 59]. In the Shanghai Women’s Health Study, a prospective cohort study, cruciferous vegetable intake was only marginally associated with lung cancer risk, with fully adjusted RRs across quartiles of 1.0, 0.81 (95 % CI 0.62–1.07), 1.00 (95 % CI 0.76–1.30), and 0.73 (95 % CI 0.54–1.00) [60]. As discussed below, the growing evidence of an inverse association between cruciferous vegetable intake and lung cancer risk has generated enthusiasm for isothiocyanates, bioactive phytochemicals abundant in cruciferous vegetables, as a promising chemopreventive agent.
5.6 Intake and Biomarkers of Micronutrients
The inverse associations observed between fruit and vegetable consumption and lung cancer risk spurred investigation into what the specific constituents may be that were linked to protection against lung cancer. Fruits and vegetables are the major dietary source of specific antioxidant micronutrients, and antioxidant micronutrients have been hypothesized to exert broad protection against malignancies by protecting DNA from the damaging effects of oxidative stress [50]. Two alternative strategies have been used to assess the potential role of micronutrients in lung cancer. One approach is to measure reported micronutrient intake using food-frequency questionnaires. A second approach is biomarker based, measuring the circulating concentrations of micronutrients. When comparing the evidence provided by these two measurement approaches, food-frequency questionnaires provide a better average measure of micronutrient intake, whereas assaying circulating micronutrient concentrations provides a biological measure that is more proximal to the cellular level where the biologic effect is postulated to occur. However, circulating micronutrient concentrations will vary based on numerous factors including recent diet and thus are transient in nature and may therefore have limited relevance to the most biologically important exposure period. The strongest evidence for the biomarker approach is generated from prospective cohort studies, where blood is collected from a population that is initially cancer free and the population is then followed for the occurrence of lung cancer. For these reasons, these measurement approaches are best viewed as complementary.
The example of carotenoids exemplifies the complexities involved in attempting to determine the role of diet in the etiology of lung cancer. A systematic review of prospective studies of both dietary intake and prediagnostic blood concentrations indicated there was an inverse association between carotenoids and lung cancer [61]. For example, both dietary intake and circulating concentrations of total carotenoids were associated with 20–30 % lower risk of lung cancer in the highest-versus-lowest exposure categories [61]. In addition to these results for total carotenoids, prospective studies also showed that circulating concentrations of specific carotenoids (α-carotene, β-carotene, β-cryptoxanthin, lutein, and lycopene) were consistently inversely associated with future lung cancer risk [61]. This body of evidence prompted the WCRF to rate foods containing carotenoids as “probable” protective factors for lung cancer [52]. However, it cannot be determined with certainty if the inverse association between carotenoids and lung cancer is directly due to carotenoid intake, or whether carotenoid intake merely serves as a marker of the intake of other protective substances or healthier dietary habits in general. As described in the section below on chemoprevention, this point is amplified by the fact that the results of large-scale randomized controlled trials conclusively demonstrated that β-carotene consumption is associated with increased risk of lung cancer in smokers [61].
The emphasis of this section on carotenoids is useful to illustrate the issues facing the study of micronutrients in relation to lung cancer in general. With respect to other micronutrients, for dietary intake the evidence is most abundant for vitamins A, C, and E. The evidence relating measures of retinol intake to lung cancer risk was rated by WCRF as providing “limited—suggestive” evidence that retinol is actually associated with increased risk of lung cancer [52]. The evidence for foods containing selenium was judged to be “limited—suggestive” of a protective association [52]. Studies of vitamin C have tended to consistently point toward an inverse association, but the evidence was judged insufficient for a conclusion by WCRF, as was the evidence for vitamin A, the B vitamins, and vitamin E/tocopherol [52].
With respect to updates of the evidence since the 2007 WCRF report, strong inverse associations were observed between serum B vitamin concentrations and subsequent lung cancer risk in the EPIC Cohort [62], particularly for vitamin B6 and methionine. In the Melbourne Collaborative Cohort Study, dietary intake of riboflavin was inversely associated with lung cancer risk in current smokers (highest-versus-lowest RR 0.53 95 % CI 0.29–0.94) but not in never and former smokers; null associations were observed for the B vitamins or methionine [63]. In the Women’s Health Initiative Cohort Study, a study of postmenopausal women, dietary vitamin D intake was not associated with lower lung cancer risk overall, but a statistically significant inverse association was observed in never smokers [64]. In the Shanghai Women’s Health Study the RRs of lung cancer were 1.0 (referent), 0.87 (95 % CI 0.8–1.11), and 0.78 (95 % CI 0.58–1.07) according to the low, middle, and high thirds of dietary vitamin E intake (p-for-trend 0.12) [65]. These more recent results highlight the challenges to making strong inferences about the associations between many micronutrients and lung cancer. If associations are observed at all, they are not always statistically significant associations for the main results, and if associations are observed they may only emerge in specific population subgroups. Evidence of this nature makes it difficult to discern whether these associations are genuine or chance findings.
5.7 Phytochemicals
Phytochemicals are low molecular weight molecules produced by plants. Of the many classes of phytochemicals, those most commonly studied in relation to lung cancer include phytoestrogens, flavonoids, and glucosinoids.
The tumor promoting effects of steroid hormones can be blocked by phytoestrogens. Soya beans are a primary source of a specific class of phytoestrogens known as isoflavonoids . The relatively few studies to date of isoflavonoids in relation to lung cancer have not provided evidence of a link, and the WCRF report found the evidence too limited to reach a conclusion [52]. Data from the Shanghai Women’s Health Study have since been published indicating a strong inverse association between soy food intake and lung cancer [66]. Yang et al. also carried out a meta-analysis of 7 case–control and 4 cohort studies of soy intake in relation to lung cancer and calculated a summary relative risk estimate of 0.83 (95 % CI 0.72–0.96) for the highest-versus-lowest category comparisons.
Flavonoids are polyphenolic compounds found in many foods derived from plants; flavonoids often exhibit potent antioxidant activity. Some fruits contain high levels of flavonoids, such as apples (quercetin) and white grapefruit (naringin). Flavonoid intake has been at least weakly associated with reduced risk of lung cancer in many, but not all, of the studies to date but the evidence was too limited for a conclusion to be drawn in the WCRF report. The evidence that flavonoid intake from food sources may be inversely associated with lung cancer risk continues to accrue [67].
Isothiocyanates are metabolites of the class of phytochemicals known as glucosinolates. Isothiocyanates could exert anticancer effects by blocking carcinogens via induction of phase II detoxification enzymes, such as glutathione S-transferase. Cruciferous vegetables contain high concentrations of glucosinolates, so that cruciferous vegetable intake is positively correlated with higher endogenous isothiocyanate concentrations. As with cruciferous vegetables, lung cancer risk is also consistently lower with higher intakes or urinary concentrations of isothiocyanates [68–70].
A postulated biologic relationship between isothiocyanates and a common polymorphism in the GSTM1 gene provides an example of a potential gene–diet interaction relevant to lung carcinogenesis. A growing focus in cancer epidemiology is to characterize interindividual susceptibility to cancer by studying polymorphisms in genes involved in carcinogenic pathways, including how these genetic markers interact with environmental exposures to contribute to cancer risk. The role of glutathione S-transferase as a phase II detoxification enzyme has made a common polymorphism in the glutathione S-transferase M1 (GSTM1) gene of interest in relation to lung cancer. Compared to persons with the GSTM1 present genotype, those with the GSTM1 null genotype have a small but statistically significantly higher risk of lung cancer [71].
When isothiocyanates have been studied in combination with GSTM1, the decreased risk of lung cancer associated with isothiocyanates has been especially pronounced in persons with the GSTM1 null genotype [57]. This association could represent the cancer blocking activity of isothiocyanates being allowed to play an enhanced role in GSTM1 null individuals because they are not being metabolized as quickly as in those with the GSTM1 present genotype. This example illustrates the potential interactions between genetic and dietary factors. Integrating genetic and epigenetic markers into the study of nutritional factors provides a mechanistically based approach that holds promise for advancing understanding of the complex role of diet in the etiology of lung cancer.
5.8 Fat
Evidence that dietary fat may facilitate tumor growth was reported as early as 1940. In case–control studies, total fat intake is consistently associated with lung cancer risk, with less consistent results for saturated fat, unsaturated fat, and cholesterol intake [72–75]. The prospective evidence shows a different picture, with some cohort studies observing lung cancer risk to increase with total fat and saturated fat intake but not unsaturated fat and cholesterol, but the results of an important study that was a large, pooled cohort study found lung cancer risk was not strongly associated with fat (total, saturated or unsaturated) or cholesterol intake [76]. The evidence is equivocal, but the hint of associations in the direction of increased risk in some studies is reflected in the assessment of the overall evidence rating in the WCRF report that the evidence is “limited—suggestive” that total dietary fat is associated with increased lung cancer risk [52]. With respect to specific food sources of fats, the same level of evidence was applied to butter [52].
5.9 Body Mass Index
In contrast to the association seen for most types of cancer, prospective cohort studies consistently show a strong inverse association between body mass index (BMI) and lung cancer risk. These remarkably strong, consistent findings clearly demonstrate that leanness is statistically associated with lung cancer risk. The key remaining question is whether this association is genuine or whether it is indirect. Confounding by cigarette smoking is a viable explanation for these findings because cigarette smoking is strongly associated both with the risk of lung cancer and with leanness. The WCRF report thus rated the evidence as “limited—suggestive” that “low body fatness” is associated with increased risk of lung cancer [52].
However, the need to further test the hypothesis that leanness is a susceptibility factor for lung cancer is indicated by the results of studies in which this association persists even after careful control for cigarette smoking. As investigators continue to pursue this question further, the evidence continues to amass indicating that residual confounding by cigarette smoking may not completely explain away this association. Since the WCRF report, evidence from case–control [77, 78] and cohort studies [79–81] that have attempted to carefully control cigarette smoking still observe strong associations between leanness and lung cancer risk. Interestingly, hints that higher body mass index may also be associated with longer survival in lung cancer patients have also been observed [82, 83].
5.10 Beverages
Potential confounding by cigarette smoking recurs for the topic of beverage consumption. Many beverages, including alcohol, coffee, tea, and milk have been studied for a possible link to lung cancer [52]. The majority of studies of alcohol drinking in relation to lung cancer risk that have been adjusted for age and cigarette smoking have observed either null or weak associations [84, 85].
Some studies have observed heavy coffee consumption to be associated with an elevated risk of lung cancer after adjustment for cigarette smoking, but a host of case–control studies have generated findings that fluctuate around the null [52]. The issue of confounding between coffee drinking and other health behaviors, particularly cigarette smoking, has not been addressed adequately, indicating that much stronger evidence is needed for coffee drinking to be considered a risk factor for lung cancer. Despite numerous in vitro and in vivo studies that have observed potential tumor-inhibitory effects of tea [86], the epidemiologic evidence does not presently provide strong support for a link between tea drinking and lung cancer risk [87, 88].
The associations observed between milk drinking and lung cancer have varied considerably. For example, in a cohort followed up since childhood, milk drinking during childhood was significantly inversely associated with lung cancer risk, suggesting drinking milk was protective [89]. On the other hand, in a large prospective study in Sweden, lactose intolerance was associated with nearly a halving in the risk of developing lung cancer, suggesting that avoidance of milk and dairy products led to a reduction in lung cancer risk [90]. The lack of data on cigarette smoking in both of these studies imposes a barrier to clear-cut inferences. Consistent with the equivocal nature of the evidence and concerns about confounding by cigarette smoking, the WCRF report did not provide evidence ratings for any of these beverages in relation to lung cancer risk [52].
Drinking water can be a route of exposure to environmental contaminants. This is exemplified by the clear increase in lung cancer risk associated with drinking water that is contaminated with high levels of arsenic [91]. Based on studies conducted in geographic regions where drinking water is contaminated with high concentrations of arsenic, the WCRF report rated the evidence as “convincing” that high concentrations of arsenic in drinking water is a risk factor for lung cancer [52].
5.11 Meat and Fish
Increased lung cancer risk has been observed to be associated with greater intakes of red meat and processed meat, but this evidence is counterbalanced by some null studies. The cooking method may play a role, as heterocyclic amines from cooked meat may contribute to an increased lung cancer risk. Based on the slight trending of the results toward increased risk, the WCRF report rated the evidence for both red meat intake and processed meat intake to be “limited—suggestive” of increased risk. The current evidence does not support a strong link between fish consumption and lung cancer; the WCRF report did not rate this evidence.
Since the WCRF report, large-scale prospective cohort studies such as the PLCO Study, the EPIC Study, and the NIH-AARP Diet and Health Study have published findings on the association of intake of red meat and processed meat on lung cancer risk [92–94]. None of the results from these studies showed strong associations, but the results from the NIH-AARP Diet and Health Study were statistically significant [94] whereas the results of the EPIC Study and the PLCO Study were not statistically significant [92, 93]. Even in the studies when the results were not statistically significant the associations tend to be in the direction of red meat and processed meat being associated with increased lung cancer risk. Thus, when the evidence is combined across studies in meta-analyses, the results show statistically significantly increased risk of lung cancer for consumption of red meat and processed meat [95, 96]. It remains to be clearly established whether or not red meat and processed meat genuinely contribute to the etiology of lung cancer.
5.12 Diet and Prevention: Chemoprevention Trials
The promising data from observational epidemiologic studies seen for fruit and vegetable consumption and for specific micronutrients led to interest in testing if antioxidant micronutrients delivered in concentrated form as dietary supplements could prevent against lung cancer. The two examples considered here are β-carotene, for which there was relatively strong a priori evidence for protection, and vitamin E (α-tocopherol), for which there was not strong a priori evidence for protection.
With respect to β-carotene , four large-scale, randomized, double-blind, placebo-controlled trials were undertaken to test the hypothesis that β-carotene supplementation protects against lung cancer [97–100]. Two of the trials were implemented in populations at high risk of lung cancer [97, 98] and two of the studies were in populations at average risk of lung cancer [99, 100]. All four studies indicated that β-carotene supplementation in later adulthood does not protect against lung cancer. To the contrary, β-carotene supplementation was associated with an increased risk of lung cancer among the high-risk populations of heavy smokers in the ATBC Cancer Prevention Study [97] and smokers and asbestos-exposed workers in the CARET Study [98]. The WCRF thus rated this strong, consistent evidence from two randomized controlled trials as “convincing” that β-carotene increases lung cancer risk in current smokers. These experimental results thus not only failed to corroborate the evidence from observational studies, but also clearly demonstrated that β-carotene supplementation increased risk in groups at the highest risk of lung cancer.
In the two randomized controlled trials of β-carotene that comprised participants who were not at excess lung cancer risk, the Physicians Health Study and the Women’s Health Study, neither trial showed evidence the β-carotene supplements protected against the development of lung cancer [99, 100]. In fact, in the Women’s Health Study, more lung cancer cases were observed in the β-carotene arm (n = 30) than the placebo arm (n = 21) [100]. Considered in total, large-scale randomized, placebo-controlled trials have been carried out and provide very strong and consistent evidence that β-carotene supplementation increases the risk of lung cancer in populations at high risk of lung cancer and does not protect against lung cancer in more average-risk populations.
A substantial amount of evidence has amassed on the potential chemopreventive effect of vitamin E supplementation for lung cancer. This evidence has been generated mostly from multiple randomized trials of vitamin E supplementation whose primary endpoints were cardiovascular disease. In the Heart Outcomes Prevention Evaluation (HOPE) trial , the group randomly assigned to vitamin E had a significantly lower lung cancer incidence rate (1.4 %) than the placebo group (2.0 %) (RR = 0.72; 95 % CI, 0.53–0.98) [101]. In the ATBC study, α-tocopherol supplements had no impact on lung cancer risk (RR = 0.99; 95 % CI, 0.87–1.13) [97]. In the Women’s Health Study, vitamin E supplementation did not lower lung cancer risk (RR = 1.09; 95 % CI, 0.83–1.44) [102]. There has also been interest in combining mixtures of antioxidant micronutrients. For example, the Medical Research Council/British Heart Foundation Heart Protection Study (HPS) was a randomized placebo-controlled trial to test antioxidant vitamin supplementation with vitamin E, vitamin C, and β-carotene. Compared with the placebo group, the lung cancer rate was slightly higher in the intervention arm (1.6 % vs. 1.4 %) [103].
In the HOPE Study, vitamin E supplements showed evidence of protecting against lung cancer, but when all these randomized trials are considered together, the combined results of multiple randomized controlled trials of vitamin E supplements are consistent with no effect on lung cancer risk.
5.12.1 Observational Versus Experimental Evidence
The evidence for vitamin E supplements to provide protection against lung cancer was not strongly supported by human data, but the epidemiologic evidence for β-carotene, as reviewed above, was robust. Thus, the discordance between the results of observational epidemiologic studies that consistently showed an inverse association between dietary intake and circulating concentrations of β-carotene and lung cancer risk and the results of the large-scale chemoprevention trials provoked considerable introspection about potential underlying explanations. Among the factors that have been considered include: (1) the protective effect may apply more to the earlier stages of carcinogenesis, so β-carotene was administered too late to impede lung carcinogenesis particularly in the trials that focused at those at high risk of lung cancer; (2) the supplemental doses administered were far higher than the normal dietary range; and (3) compounds present in fruits and vegetables other than β-carotene may protect against lung cancer. Clearly, fruits and vegetables comprise complex mixtures of antioxidants, phytochemicals, and other compounds that may each exert anticancer properties. This is not a comprehensive list, but still provides insights into the complexity involved in taking the findings from basic and epidemiological research to characterize the nutritional factors that influence lung carcinogenesis and translating this information into strategies to prevent lung cancer.
6 Conclusions
Key questions concerning the relationship between diet and lung cancer continue to progress toward resolution. As summarized in Table 8.2, several promising leads have emerged to suggest that nutritional factors could have a substantial impact on lung cancer risk in humans. For example, persons who eat more fruits and vegetables clearly have a lower risk of lung cancer than persons who consume less of these foods. In observational studies, the same holds true for intake of specific micronutrients, such as carotenoids. The specific constituents of fruits and vegetables that may confer protection are unknown. An important unanswered question is whether fruits and vegetables directly confer protection against lung cancer. An alternative explanation that is difficult to dismiss is that fruit and vegetable consumption is a marker of other differences between individuals who eat healthy and unhealthy diets that are leading to uncontrolled confounding. The association between fruit and vegetable consumption and lower risk of lung cancer has the potential to contribute to prevention.
In recent years, published epidemiologic studies have improved considerably in using methods to provide the strictest possible control for cigarette smoking, such as matching cases and controls in the study design, limiting the study population to never smokers, and carefully stratifying by smoking history in the analyses. Continued movement in this direction will help to resolve long-standing questions about dietary factors and lung cancer by addressing head-on the persistent concern about residual confounding by cigarette smoking.
Research that continues to provide fresh insights into the influence of diet and nutrition on the occurrence of lung cancer is critical to move the field forward, helping to define new strategies to prevent lung cancer. Increased mechanistic understanding about the complex interactions micronutrients play in the pathogenesis of malignancies may contribute to focusing on particular dietary components most relevant for study. As an example, various micronutrients have been shown to modify the action of enzymes responsible for methylating DNA and creating various histone modifications, the types of epigenetic modifications that have been demonstrated to be associated with the pathogenesis of lung cancer and other solid tumor malignancies. Additionally, a promising research strategy to more thoroughly investigate across food and nutrient categories is to study dietary patterns as opposed to individual dietary constituents. In this approach investigators are able to categorize overall diets according to whether they meet a predefined definition of “healthy eating” or “mixed dishes” pattern of eating [104, 105].
As progress is made in further understanding the role of diet and nutrition in lung cancer etiology, this progress should not obscure the fact that cigarette smoking is the predominant cause of lung cancer. Many important questions remain concerning the role of diet and nutrition in relation to lung cancer, but the primary way that the lung cancer epidemic will be controlled is to prevent the uptake of cigarette smoking among children and effectively assist addicted smokers to stop smoking cigarettes.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107.
American Cancer Society. Cancer facts and figures 2014. Atlanta: American Cancer Society; 2014.
Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF et al. SEER Cancer Statistics Review, 1975-2011. National Cancer Institute.Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.
Alberg AJ, Wallace K, Silvestri GA, Brock MV. Invited commentary: the etiology of lung cancer in men compared with women. Am J Epidemiol. 2013;177(7):613–6. doi:10.1093/aje/kws444.
Alberg AJ, Horner MJ, Daguise VG, Carpenter MJ, Mosley CM, Vincent B et al. Lung and bronchus cancer disparities in South Carolina: epidemiology and strategies for prevention. J S C Med Assoc. 2006;102(7):183–91.
Holford TR, Meza R, Warner KE, Meernik C, Jeon J, Moolgavkar SH, et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964-2012. JAMA. 2014;311(2):164–71. doi:10.1001/jama.2013.285112.
Devesa SS, Diamond EL. Socioeconomic and racial differences in lung cancer incidence. Am J Epidemiol. 1983;118:818–31.
Mao Y, Hu J, Ugnat AM, Semenciw R, Fincham S. Socioeconomic status and lung cancer risk in Canada. Int J Epidemiol. 2001;30:809–17.
Li K, Yu S. Economic status, smoking, occupational exposure to rubber, and lung cancer: a case-cohort study. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2002;20(1):21–8. doi:10.1081/gnc-120003926.
Booth CM, Li G, Zhang-Salomons J, Mackillop WJ. The impact of socioeconomic status on stage of cancer at diagnosis and survival: a population-based study in Ontario, Canada. Cancer. 2010;116(17):4160–7. doi:10.1002/cncr.25427.
van Loon AJ, Goldbohm RA, Kant IJ, Swaen GM, Kremer AM, van den Brandt PA. Socioeconomic status and lung cancer incidence in men in The Netherlands: is there a role for occupational exposure? J Epidemiol Community Health. 1997;51(1):24–9.
Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM. Income and race/ethnicity are associated with adherence to food-based dietary guidance among US adults and children. J Acad Nutr Dietetics. 2012;112(5):624–35.e6. doi:10.1016/j.jand.2011.11.012.
Khuder SA. Effect of cigarette smoking on major histological types of lung cancer: a meta-analysis. Lung Cancer. 2001;31(2-3):139–48.
Alberg AJ, Samet JM. Epidemiology of lung cancer. Chest. 2003;123(1 Suppl)):21s–49s.
US Department of Health and Human Services (USDHHS). The health consequences of smoking—50 years of progress. Atlanta: USDHHS Office on Smoking and Health; 2014.
Alberg AJ, Nonemaker J. Who is at high risk for lung cancer? Population-level and individual-level perspectives. Semin Respir Crit Care Med. 2008;29(3):223–32. doi:10.1055/s-2008-1076742.
Alberg AJ. Cigarette smoking: health effects and control strategies. Drugs Today(Barc). 2008;44(12):895–904. doi:10.1358/dot.2008.44.12.1308898.
Alberg AJ, Ford JG, Samet JM. Epidemiology of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007;132(3 Suppl):29s–55s. doi:10.1378/chest.07-1347.
Kabat GC, Hebert JR. Use of mentholated cigarettes and lung cancer risk. Cancer Res. 1991;51(24):6510–3.
Muscat JE, Richie Jr JP, Stellman SD. Mentholated cigarettes and smoking habits in whites and blacks. Tob Control. 2002;11(4):368–71.
Stellman SD, Chen Y, Muscat JE, Djordjevic MV, Richie Jr JP, Lazarus P, et al. Lung cancer risk in white and black Americans. Ann Epidemiol. 2003;13(4):294–302.
Brooks DR, Palmer JR, Strom BL, Rosenberg L. Menthol cigarettes and risk of lung cancer. Am J Epidemiol. 2003;158(7):609–16. discussion 17-20.
Carpenter CL, Jarvik ME, Morgenstern H, McCarthy WJ, London SJ. Mentholated cigarette smoking and lung-cancer risk. Ann Epidemiol. 1999;9(2):114–20.
Sidney S, Tekawa IS, Friedman GD, Sadler MC, Tashkin DP. Mentholated cigarette use and lung cancer. Arch Intern Med. 1995;155(7):727–32.
Murray RP, Connett JE, Skeans MA, Tashkin DP. Menthol cigarettes and health risks in Lung Health Study data. Nicotine Tob Res. 2007;9(1):101–7. doi:10.1080/14622200601078418.
Blot WJ, Cohen SS, Aldrich M, McLaughlin JK, Hargreaves MK, Signorello LB. Lung cancer risk among smokers of menthol cigarettes. J Natl Cancer Inst. 2011;103(10):810–6. doi:10.1093/jnci/djr102.
Thun MJ, Carter BD, Feskanich D, Freedman ND, Prentice R, Lopez AD, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368(4):351–64. doi:10.1056/NEJMsa1211127.
Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. 2010;39(3):834–57. doi:10.1093/ije/dyq002.
Popova L, Ling PM. Alternative tobacco product use and smoking cessation: a national study. Am J Public Health. 2013;103(5):923–30. doi:10.2105/ajph.2012.301070.
Kamerow D. Big Tobacco lights up e-cigarettes. BMJ. 2013;346:3418. doi:10.1136/bmj.f3418.
Schuster RM, Hertel AW, Mermelstein R. Cigar, cigarillo, and little cigar use among current cigarette-smoking adolescents. Nicotine Tob Res. 2013;15(5):925–31. doi:10.1093/ntr/nts222.
Jawad M, McEwen A, McNeill A, Shahab L. To what extent should waterpipe tobacco smoking become a public health priority? Addiction. 2013;108(11):1873–84. doi:10.1111/add.12265.
Schaal C, Chellappan SP. Nicotine-mediated cell proliferation and tumor progression in smoking-related cancers. Mol Cancer Res. 2014;12(1):14–23. doi:10.1158/1541-7786.mcr-13-0541.
Cheng T. Chemical evaluation of electronic cigarettes. Tob Control. 2014;23 Suppl 2:11–7. doi:10.1136/tobaccocontrol-2013-051482.
US Department of Health and Human Services (USDHHS). The health consequences of involuntary exposure to tobacco smoke. Atlanta: USDHHS Office on Smoking and Health; 2006.
Alberg AJ, Brock MV, Ford JG, Samet JM, Spivack SD. Epidemiology of lung cancer: diagnosis and management of lung cancer, 3rd ed: american college of chest physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e1s–29s. doi:10.1378/chest.12-2345.
Alberg AJ, Yung RC, Strickland PT, Nelson J. Respiratory cancer and exposure to arsenic, chromium, nickel and polycyclic aromatic hydrocarbons. Clin Occup Environ Med. 2002;2:779–801.
Alberg AJ, Samet JM. Chapter 46: Epidemiology of lung cancer. In: Mason RJ, Broaddus VC, Martin T, King T, Schraufnagel D, Murray JF, Nadel JA, editors. Murray and Nadel’s textbook of respiratory medicine. 5th ed. Philadelphia: Elsevier Science; 2010. p. 1098–115.
Hamra GB, Guha N, Cohen A, Laden F, Raaschou-Nielsen O, Samet JM, et al. Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect. 2014;122(9):906–11. doi:10.1289/ehp.1408092.
Chen BH, Hong CJ, Pandey MR, Smith KR. Indoor air pollution in developing countries. World Health Stat Q. 1990;43(3):127–38.
Hosgood 3rd HD, Boffetta P, Greenland S, Lee YC, McLaughlin J, Seow A, et al. In-home coal and wood use and lung cancer risk: a pooled analysis of the International Lung Cancer Consortium. Environ Health Perspect. 2010;118(12):1743–7. doi:10.1289/ehp.1002217.
Lin HH, Murray M, Cohen T, Colijn C, Ezzati M. Effects of smoking and solid-fuel use on COPD, lung cancer, and tuberculosis in China: a time-based, multiple risk factor, modelling study. Lancet. 2008;372(9648):1473–83. doi:10.1016/s0140-6736(08)61345-8.
Kurmi OP, Arya PH, Lam KB, Sorahan T, Ayres JG. Lung cancer risk and solid fuel smoke exposure: a systematic review and meta-analysis. Eur Respir J. 2012;40(5):1228–37. doi:10.1183/09031936.00099511.
Cote ML, Liu M, Bonassi S, Neri M, Schwartz AG, Christiani DC, et al. Increased risk of lung cancer in individuals with a family history of the disease: a pooled analysis from the International Lung Cancer Consortium. Eur J Cancer. 2012;48(13):1957–68. doi:10.1016/j.ejca.2012.01.038.
Brennan P, Hainaut P, Boffetta P. Genetics of lung-cancer susceptibility. Lancet Oncol. 2011;12(4):399–408. doi:10.1016/s1470-2045(10)70126-1.
Tardon A, Lee WJ, Delgado-Rodriguez M, Dosemeci M, Albanes D, Hoover R, et al. Leisure-time physical activity and lung cancer: a meta-analysis. Cancer causes & control : CCC. 2005;16(4):389–97. doi:10.1007/s10552-004-5026-9.
Buffart LM, Singh AS, van Loon EC, Vermeulen HI, Brug J, Chinapaw MJ. Physical activity and the risk of developing lung cancer among smokers: a meta-analysis. J Sci Med Sport. 2014;17(1):67–71. doi:10.1016/j.jsams.2013.02.015.
Emaus A, Thune I. Physical activity and lung cancer prevention. Recent Results Cancer Res. 2011;186:101–33. doi:10.1007/978-3-642-04231-7_5.
Alberg AJ. The influence of cigarette smoking on circulating concentrations of antioxidant micronutrients. Toxicology. 2002;180(2):121–37.
Alberg AJ, Byers P. Cigarette smoking and endogenous antioxidants. In: Laher I, editor. Systems biology of free radicals and antioxidants. Berlin: Springer; 2014. p. 1633–42.
Alberg AJ, Chen JC, Zhao H, Hoffman SC, Comstock GW, Helzlsouer KJ. Household exposure to passive cigarette smoking and serum micronutrient concentrations. Am J Clin Nutr. 2000;72(6):1576–82.
World Cancer Research Fund. Food, nutrition and the prevention of cancer: a global perspective. Washington, DC: American Institutes of Cancer Research; 2007.
Takata Y, Xiang YB, Yang G, Li H, Gao J, Cai H, et al. Intakes of fruits, vegetables, and related vitamins and lung cancer risk: results from the Shanghai Men’s Health Study (2002-2009). Nutr Cancer. 2013;65(1):51–61. doi:10.1080/01635581.2013.741757.
Buchner FL, Bueno-de-Mesquita HB, Linseisen J, Boshuizen HC, Kiemeney LA, Ros MM, et al. Fruits and vegetables consumption and the risk of histological subtypes of lung cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC). Cancer Causes Control. 2010;21(3):357–71. doi:10.1007/s10552-009-9468-y.
Wright ME, Park Y, Subar AF, Freedman ND, Albanes D, Hollenbeck A, et al. Intakes of fruit, vegetables, and specific botanical groups in relation to lung cancer risk in the NIH-AARP Diet and Health Study. Am J Epidemiol. 2008;168(9):1024–34. doi:10.1093/aje/kwn212.
Wakai K, Matsuo K, Nagata C, Mizoue T, Tanaka K, Tsuji I, et al. Lung cancer risk and consumption of vegetables and fruit: an evaluation based on a systematic review of epidemiological evidence from Japan. Jpn J Clin Oncol. 2011;41(5):693–708. doi:10.1093/jjco/hyr027.
Lam TK, Gallicchio L, Lindsley K, Shiels M, Hammond E, Tao XG, et al. Cruciferous vegetable consumption and lung cancer risk: a systematic review. Cancer Epidemiol Biomarkers Prev. 2009;18(1):184–95. doi:10.1158/1055-9965.epi-08-0710.
Lam TK, Ruczinski I, Helzlsouer KJ, Shugart YY, Caulfield LE, Alberg AJ. Cruciferous vegetable intake and lung cancer risk: a nested case-control study matched on cigarette smoking. Cancer Epidemiol Biomarkers Prev. 2010;19(10):2534–40. doi:10.1158/1055-9965.epi-10-0475.
Tang L, Zirpoli GR, Jayaprakash V, Reid ME, McCann SE, Nwogu CE, et al. Cruciferous vegetable intake is inversely associated with lung cancer risk among smokers: a case-control study. BMC Cancer. 2010;10:162. doi:10.1186/1471-2407-10-162.
Wu QJ, Xie L, Zheng W, Vogtmann E, Li HL, Yang G, et al. Cruciferous vegetables consumption and the risk of female lung cancer: a prospective study and a meta-analysis. Ann Oncol. 2013;24(7):1918–24. doi:10.1093/annonc/mdt119.
Gallicchio L, Boyd K, Matanoski G, Tao XG, Chen L, Lam TK, et al. Carotenoids and the risk of developing lung cancer: a systematic review. Am J Clin Nutr. 2008;88(2):372–83.
Johansson M, Relton C, Ueland PM, Vollset SE, Midttun O, Nygard O, et al. Serum B vitamin levels and risk of lung cancer. JAMA. 2010;303(23):2377–85. doi:10.1001/jama.2010.808.
Bassett JK, Hodge AM, English DR, Baglietto L, Hopper JL, Giles GG, et al. Dietary intake of B vitamins and methionine and risk of lung cancer. Eur J Clin Nutr. 2012;66(2):182–7. doi:10.1038/ejcn.2011.157.
Cheng TY, Lacroix AZ, Beresford SA, Goodman GE, Thornquist MD, Zheng Y, et al. Vitamin D intake and lung cancer risk in the Women’s Health Initiative. Am J Clin Nutr. 2013;98(4):1002–11. doi:10.3945/ajcn.112.055905.
Wu QJ, Xiang YB, Yang G, Li HL, Lan Q, Gao YT, et al. Vitamin E intake and the lung cancer risk among female nonsmokers: a report from the Shanghai Women’s Health Study. Int J Cancer. 2015;136(3):610–7. doi:10.1002/ijc.29016.
Yang G, Shu XO, Chow WH, Zhang X, Li HL, Ji BT, et al. Soy food intake and risk of lung cancer: evidence from the Shanghai Women’s Health Study and a meta-analysis. Am J Epidemiol. 2012;176(10):846–55. doi:10.1093/aje/kws168.
Christensen KY, Naidu A, Parent ME, Pintos J, Abrahamowicz M, Siemiatycki J, et al. The risk of lung cancer related to dietary intake of flavonoids. Nutr Cancer. 2012;64(7):964–74. doi:10.1080/01635581.2012.717677.
Spitz MR, Duphorne CM, Detry MA, Pillow PC, Amos CI, Lei L, et al. Dietary intake of isothiocyanates: evidence of a joint effect with glutathione S-transferase polymorphisms in lung cancer risk. Cancer Epidemiol Biomarkers Prev. 2000;9(10):1017–20.
Zhao B, Seow A, Lee EJ, Poh WT, Teh M, Eng P, et al. Dietary isothiocyanates, glutathione S-transferase -M1, -T1 polymorphisms and lung cancer risk among Chinese women in Singapore. Cancer Epidemiol Biomarkers Prev. 2001;10(10):1063–7.
London SJ, Yuan JM, Chung FL, Gao YT, Coetzee GA, Ross RK, et al. Isothiocyanates, glutathione S-transferase M1 and T1 polymorphisms, and lung-cancer risk: a prospective study of men in Shanghai, China. Lancet. 2000;356(9231):724–9. doi:10.1016/s0140-6736(00)02631-3.
Lam TK, Ruczinski I, Helzlsouer K, Shugart YY, Li KE, Clipp S, et al. Copy number variants of GSTM1 and GSTT1 in relation to lung cancer risk in a prospective cohort study. Ann Epidemiol. 2009;19(8):546–52. doi:10.1016/j.annepidem.2009.03.003.
Goodman MT, Kolonel LN, Yoshizawa CN, Hankin JH. The effect of dietary cholesterol and fat on the risk of lung cancer in Hawaii. Am J Epidemiol. 1988;128(6):1241–55.
Goodman MT, Hankin JH, Wilkens LR, Kolonel LN. High-fat foods and the risk of lung cancer. Epidemiology. 1992;3(4):288–99.
De Stefani E, Brennan P, Boffetta P, Mendilaharsu M, Deneo-Pellegrini H, Ronco A, et al. Diet and adenocarcinoma of the lung: a case-control study in Uruguay. Lung Cancer. 2002;35(1):43–51.
Hu J, Mao Y, Dryer D, White K. Risk factors for lung cancer among Canadian women who have never smoked. Cancer Detect Prev. 2002;26(2):129–38.
Smith-Warner SA, Ritz J, Hunter DJ, Albanes D, Beeson WL, van den Brandt PA, et al. Dietary fat and risk of lung cancer in a pooled analysis of prospective studies. Cancer Epidemiol Biomarkers Prev. 2002;11(10 Pt 1):987–92.
Tarnaud C, Guida F, Papadopoulos A, Cenee S, Cyr D, Schmaus A, et al. Body mass index and lung cancer risk: results from the ICARE study, a large, population-based case-control study. Cancer Causes Control. 2012;23(7):1113–26. doi:10.1007/s10552-012-9980-3.
El-Zein M, Parent ME, Nicolau B, Koushik A, Siemiatycki J, Rousseau MC. Body mass index, lifetime smoking intensity and lung cancer risk. Int J Cancer. 2013;133(7):1721–31. doi:10.1002/ijc.28185.
Everatt R, Virviciute D, Kuzmickiene I, Tamosiunas A. Body mass index, cholesterol level and risk of lung cancer in Lithuanian men. Lung Cancer. 2014;85(3):361–5. doi:10.1016/j.lungcan.2014.07.009.
Bethea TN, Rosenberg L, Charlot M, O’Connor GT, Adams-Campbell LL, Palmer JR. Obesity in relation to lung cancer incidence in African American women. Cancer Causes Control. 2013;24(9):1695–703. doi:10.1007/s10552-013-0245-6.
Smith L, Brinton LA, Spitz MR, Lam TK, Park Y, Hollenbeck AR, et al. Body mass index and risk of lung cancer among never, former, and current smokers. J Natl Cancer Inst. 2012;104(10):778–89. doi:10.1093/jnci/djs179.
Leung CC, Lam TH, Yew WW, Chan WM, Law WS, Tam CM. Lower lung cancer mortality in obesity. Int J Epidemiol. 2011;40(1):174–82. doi:10.1093/ije/dyq134.
Dahlberg SE, Schiller JH, Bonomi PB, Sandler AB, Brahmer JR, Ramalingam SS, et al. Body mass index and its association with clinical outcomes for advanced non-small-cell lung cancer patients enrolled on Eastern Cooperative Oncology Group clinical trials. J Thorac Oncol. 2013;8(9):1121–7. doi:10.1097/JTO.0b013e31829cf942.
Korte JE, Brennan P, Henley SJ, Boffetta P. Dose-specific meta-analysis and sensitivity analysis of the relation between alcohol consumption and lung cancer risk. Am J Epidemiol. 2002;155(6):496–506.
Bandera EV, Freudenheim JL, Vena JE. Alcohol consumption and lung cancer: a review of the epidemiologic evidence. Cancer Epidemiol Biomarkers Prev. 2001;10(8):813–21.
Clark J, You M. Chemoprevention of lung cancer by tea. Mol Nutr Food Res. 2006;50(2):144–51. doi:10.1002/mnfr.200500135.
Fritz H, Seely D, Kennedy DA, Fernandes R, Cooley K, Fergusson D. Green tea and lung cancer: a systematic review. Integr Cancer Ther. 2013;12(1):7–24. doi:10.1177/1534735412442378.
Arts IC. A review of the epidemiological evidence on tea, flavonoids, and lung cancer. J Nutr. 2008;138(8):1561s–6.
van der Pols JC, Bain C, Gunnell D, Smith GD, Frobisher C, Martin RM. Childhood dairy intake and adult cancer risk: 65-y follow-up of the Boyd Orr cohort. Am J Clin Nutr. 2007;86(6):1722–9.
Ji J, Sundquist J, Sundquist K. Lactose intolerance and risk of lung, breast and ovarian cancers: aetiological clues from a population-based study in Sweden. Br J Cancer. 2015;112(1):149–52. doi:10.1038/bjc.2014.544.
Celik I, Gallicchio L, Boyd K, Lam TK, Matanoski G, Tao X, et al. Arsenic in drinking water and lung cancer: a systematic review. Environ Res. 2008;108(1):48–55. doi:10.1016/j.envres.2008.04.001.
Tasevska N, Cross AJ, Dodd KW, Ziegler RG, Caporaso NE, Sinha R. No effect of meat, meat cooking preferences, meat mutagens or heme iron on lung cancer risk in the prostate, lung, colorectal and ovarian cancer screening trial. Int J Cancer. 2011;128(2):402–11. doi:10.1002/ijc.25327.
Linseisen J, Rohrmann S, Bueno-de-Mesquita B, Buchner FL, Boshuizen HC, Agudo A, et al. Consumption of meat and fish and risk of lung cancer: results from the European Prospective Investigation into Cancer and Nutrition. Cancer Causes Control. 2011;22(6):909–18. doi:10.1007/s10552-011-9764-1.
Tasevska N, Sinha R, Kipnis V, Subar AF, Leitzmann MF, Hollenbeck AR, et al. A prospective study of meat, cooking methods, meat mutagens, heme iron, and lung cancer risks. Am J Clin Nutr. 2009;89(6):1884–94. doi:10.3945/ajcn.2008.27272.
Yang WS, Wong MY, Vogtmann E, Tang RQ, Xie L, Yang YS, et al. Meat consumption and risk of lung cancer: evidence from observational studies. Ann Oncol. 2012;23(12):3163–70. doi:10.1093/annonc/mds207.
Xue XJ, Gao Q, Qiao JH, Zhang J, Xu CP, Liu J. Red and processed meat consumption and the risk of lung cancer: a dose-response meta-analysis of 33 published studies. Int J Clin Exp Med. 2014;7(6):1542–53.
Albanes D, Heinonen OP, Taylor PR, Virtamo J, Edwards BK, Rautalahti M, et al. Alpha-Tocopherol and beta-carotene supplements and lung cancer incidence in the alpha-tocopherol, beta-carotene cancer prevention study: effects of base-line characteristics and study compliance. J Natl Cancer Inst. 1996;88(21):1560–70.
Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, et al. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med. 1996;334(18):1150–5. doi:10.1056/nejm199605023341802.
Hennekens CH, Buring JE, Manson JE, Stampfer M, Rosner B, Cook NR, et al. Lack of effect of long-term supplementation with beta carotene on the incidence of malignant neoplasms and cardiovascular disease. N Engl J Med. 1996;334(18):1145–9. doi:10.1056/nejm199605023341801.
Lee IM, Cook NR, Manson JE, Buring JE, Hennekens CH. Beta-carotene supplementation and incidence of cancer and cardiovascular disease: the Women’s Health Study. J Natl Cancer Inst. 1999;91(24):2102–6.
Lonn E, Bosch J, Yusuf S, Sheridan P, Pogue J, Arnold JM, et al. Effects of long-term vitamin E supplementation on cardiovascular events and cancer: a randomized controlled trial. JAMA. 2005;293(11):1338–47. doi:10.1001/jama.293.11.1338.
Lee IM, Cook NR, Gaziano JM, Gordon D, Ridker PM, Manson JE, et al. Vitamin E in the primary prevention of cardiovascular disease and cancer: the Women’s Health Study: a randomized controlled trial. JAMA. 2005;294(1):56–65. doi:10.1001/jama.294.1.56.
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360(9326):23–33. doi:10.1016/s0140-6736(02)09328-5.
Balder HF, Goldbohm RA, van den Brandt PA. Dietary patterns associated with male lung cancer risk in the Netherlands Cohort Study. Cancer Epidemiol Biomarkers Prev. 2005;14(2):483–90. doi:10.1158/1055-9965.epi-04-0353.
Gorlova OY, Weng SF, Hernandez L, Spitz MR, Forman MR. Dietary patterns affect lung cancer risk in never smokers. Nutr Cancer. 2011;63(6):842–9. doi:10.1080/01635581.2011.589958.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Alberg, A.J., Wrangle, J.M. (2015). The Role of Diet and Nutrition in Lung Cancer. In: Bendich, A., Deckelbaum, R. (eds) Preventive Nutrition. Nutrition and Health. Springer, Cham. https://doi.org/10.1007/978-3-319-22431-2_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-22431-2_8
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22430-5
Online ISBN: 978-3-319-22431-2
eBook Packages: MedicineMedicine (R0)