Abstract
A large body of evidence shows that cannabinoids, in addition to their well-known palliative effects on some cancer-associated symptoms, can reduce tumour growth in animal models of cancer. They do so by modulating key cell signalling pathways involved in the control of cancer cell proliferation and survival. In addition, cannabinoids inhibit angiogenesis and cell proliferation in different types of tumours in laboratory animals. By contrast, little is known about the biological role of the endocannabinoid system in cancer physio-pathology, and several studies suggest that it may be over-activated in cancer. In this review, we discuss our current understanding of cannabinoids as antitumour agents, focusing on recent advances in the molecular mechanisms of action, including resistance mechanisms and opportunities for combination therapy approaches.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Angiogenesis
- Apoptosis
- Autophagy
- Cancer
- Cannabinoid
- Cell proliferation
- Cell signalling
- Combinational therapy
1 Introduction
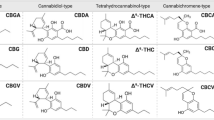
Preparations from Cannabis sativa L. (marijuana) have been used for many centuries both medicinally and recreationally. However, the chemical structures of their unique active components—the cannabinoids—were not elucidated until the 1960s. Three decades later the first solid clues on cannabinoid molecular action were established, which led to an impressive expansion of basic cannabinoid research and to a renaissance in the study of the therapeutic effects of cannabinoids in various fields, including oncology. Today, it is widely accepted that, out of the ~108 cannabinoids produced by C. sativa, Δ9-tetrahydrocannabinol (THC) is the most relevant owing to its high potency and abundance in plant preparations (Gaoni and Mechoulam 1964; Pertwee 2008). THC exerts a wide variety of biological effects by mimicking endogenous substances—the endocannabinoids anandamide (Devane et al. 1992) and 2-arachidonoylglycerol (2-AG) (Mechoulam et al. 1995; Sugiura et al. 1995)—that engage specific cell-surface cannabinoid receptors (Pertwee et al. 2010). So far, two major cannabinoid-specific receptors—CB1 and CB2—have been cloned and characterized from mammalian tissues (Matsuda et al. 1990; Munro et al. 1993). In addition, other receptors such as the transient receptor potential cation channel subfamily V member 1 (TRPV1) and the orphan G protein-coupled receptor GPR55 have been proposed to act as endocannabinoid receptors (Pertwee et al. 2010). Most of the effects produced by cannabinoids in the nervous system and in non-neural tissues rely on CB1 receptor activation. In contrast, the CB2 receptor was initially described to be present in the immune system (Pertwee et al. 2010), but more recently it has been shown to be expressed as well in cells from other origins (Atwood et al. 2010; Fernandez-Ruiz et al. 2007). Of note, expression of CB1 and CB2 receptors has been found in many types of cancer cells, which does not necessarily correlate with the expression of these receptors in the tissue type of origin (Fernandez-Ruiz et al. 2007; Guzman et al. 2006; Sarfaraz et al. 2008).
The endocannabinoids, together with their receptors and the proteins responsible for their synthesis, transport and degradation, constitute the endocannabinoid system. Aside from its pivotal neuromodulatory activity (Katona and Freund 2008), the endocannabinoid system exerts other regulatory functions in the body such as the control of cardiovascular tone, energy metabolism, immunity and reproduction (Pacher et al. 2006; Pertwee 2009). This miscellaneous activity makes the pharmacological manipulation of the endocannabinoid system a promising strategy for the management of many different diseases. Specifically, cannabinoids are well known to exert palliative effects in cancer patients (Pacher et al. 2006; Pertwee 2009). The best-established use is the inhibition of chemotherapy-induced nausea and vomiting (Guzman 2003; Pertwee 2009). Today, capsules of THC (Marinol) and its synthetic analogue nabilone (Cesamet) are approved for this purpose. Cannabinoids also inhibit pain, and thus a standardized cannabis extract (Sativex) has been already approved in Canada and is currently subject of large-scale Phase III clinical trials for managing cancer-associated pain. Another potential palliative effect of cannabinoids in oncology, supported by Phase III clinical trials, includes appetite stimulation and attenuation of wasting. In relation to this, Marinol can currently be prescribed for anorexia associated with weight loss in AIDS patients.
The therapeutic potential of cannabinoids in oncology may not be restricted to their aforementioned palliative actions. Thus, numerous studies have provided evidence that THC and other cannabinoids exhibit antitumour effects on a wide array of animal models of cancer (Guzman 2003; Sarfaraz et al. 2008; Velasco et al. 2012) Moreover, these observations have led to the development of two clinical studies to investigate the antitumour activity of cannabinoids in human patients (see Sect. 7). Nonetheless, a few studies have shown that, under certain conditions, cannabinoid treatment can stimulate cancer cell proliferation in vitro (Cudaback et al. 2010; Hart et al. 2004) and interfere with the tumour-suppressor role of the immune system (McKallip et al. 2002; Zhu et al. 2000). Likewise, there are conflicting reports regarding the role (tumour-suppressor or oncogenic) of the endocannabinoid system in cancer (Malfitano et al. 2011) (Box 1).
Box 1. Biological Role of the Endocannabinoid System in Tumour Generation and Progression
To date, little is known about the biological role of the endocannabinoid system in cancer physio-pathology. Although there are some exceptions that may be tumour type-specific, both cannabinoid receptors and their endogenous ligands are generally up-regulated in tumour tissue compared with non-tumour tissue (Caffarel et al. 2006; Guzman 2003; Malfitano et al. 2011; Sanchez et al. 2001). Additionally, different studies have associated the expression levels of cannabinoid receptors, endocannabinoids and/or endocannabinoid-metabolizing enzymes with tumour aggressiveness (Malfitano et al. 2011; Nomura et al. 2010; Thors et al. 2010), which suggests that the endocannabinoid system may be over-activated in cancer and hence pro-tumourigenic (Malfitano et al. 2011). In support of this, in mouse models of cancer, genetic ablation of CB1 and CB2 receptors reduces ultraviolet light-induced skin carcinogenesis (Zheng et al. 2008), and CB2 receptor over-expression enhances the predisposition to leukaemia after leukaemia virus infection (Joosten et al. 2002).
Conversely, and in line with the evidence supporting the hypothesis that pharmacological activation of cannabinoid receptors reduces tumour growth (Guzman 2003; Sarfaraz et al. 2008), the up-regulation of endocannabinoid-degrading enzymes has been observed in aggressive human tumours and cancer cell lines (Nomura et al. 2010; Thors et al. 2010), indicating that endocannabinoid signalling can also have a tumour-suppressive role. In support of this, deletion of CB1 receptors accelerates intestinal tumour growth in a genetic mouse model of colon cancer (Wang et al. 2008), increased endocannabinoid levels diminish azoxymethane-induced precancerous lesions in the mouse colon (Izzo et al. 2008), and a reduction in the expression of the endocannabinoid-degrading enzyme monoacylglycerol lipase reduces tumour growth in xenografted mice (Nomura et al. 2010).
Further studies, including those analysing the activation of the precise signalling mechanisms involved in the regulation of cannabinoid-induced cell death or cell proliferation upon genetic or pharmacological manipulation of the endocannabinoid system, are therefore needed to clarify which are the contextual determinants for this system to act as either a guardian or an inducer of tumourigenesis or tumour progression.
This review summarizes these observations and provides an integrated view of the molecular mechanisms responsible for cannabinoid antitumour activity. It also discusses the experimental evidence supporting the existence of mechanisms of resistance to the cell death-promoting actions of THC in certain types of cancer cells, the possible strategies that could be undertaken to overcome such resistance, and the preclinical data supporting that the combined administration of cannabinoids and other drugs could be useful in anticancer therapies.
2 The Endocannabinoid System and Cancer
To date, little is known about the precise biological role of the endocannabinoid system in cancer physio-pathology. Although there are some exceptions that may be tumour type-specific, both cannabinoid receptors and their endogenous ligands are generally up-regulated in tumour tissue compared with non-tumour tissue (Caffarel et al. 2006; Guzman 2003; Malfitano et al. 2011; Sanchez et al. 2001). Additionally, different studies have associated the expression levels of cannabinoid receptors, endocannabioids and/or endocannabinoid-metabolizing enzymes with tumour aggressiveness (Malfitano et al. 2011; Nomura et al. 2010; Thors et al. 2010), which suggests that the endocannabinoid system may be over-activated in cancer and hence pro-tumourigenic (Malfitano et al. 2011). In support of this, in mouse models of cancer, genetic ablation of CB1 and CB2 receptors reduces ultraviolet light-induced skin carcinogenesis (Zheng et al. 2008), and CB2 receptor over-expression enhances the predisposition to leukaemia after leukaemia virus infection (Joosten et al. 2002).
Conversely, and in line with the evidence supporting that pharmacological activation of cannabinoid receptors reduces tumour growth (Guzman 2003; Sarfaraz et al. 2008), the up-regulation of endocannabinoid-degrading enzymes has been observed in aggressive human tumours and cancer cell lines (Nomura et al. 2010; Thors et al. 2010), indicating that endocannabinoid signalling can also have a tumour-suppressive role. In support of this, deletion of CB1 receptors accelerates intestinal tumour growth in a genetic mouse model of colon cancer (Wang et al. 2008), increased endocannabinoid levels diminish azoxymethane-induced precancerous lesions in the mouse colon (Izzo et al. 2008), and a reduction in the expression of the endocannabinoid-degrading enzyme monoacylglycerol lipase reduces tumour growth in xenografted mice (Nomura et al. 2010).
Further studies, including those analysing the activation of the precise signalling mechanisms involved in the regulation of cannabinoid-induced cell death or cell proliferation upon genetic or pharmacological manipulation of the endocannabinoid system, are therefore needed to clarify which are the contextual determinants for this system to act as a guardian or an inducer of tumourigenesis or tumour progression
3 Preclinical Antitumour Activity
Since the late 1990s, a large body of evidence has accumulated demonstrating that various cannabinoids exert antitumour effects in a wide variety of experimental models of cancer , ranging from cancer cell lines in culture to genetically engineered mice [reviewed by Velasco et al. (2012)]. Multiple cannabinoids have shown this activity, including THC; the endocannabinoids 2-AG and anandamide; and different synthetic cannabinoid receptor agonists that have either comparable affinity for CB1 and CB2 receptors (e.g. WIN 55212-2 or HU-210), higher affinity for CB1 (e.g. methanandamide) or higher affinity for CB2 (e.g. JWH-133). These findings strongly support that, aside from the role played by the endogenous cannabinoid system in cancer, pharmacological stimulation of CB receptors is in most cases antitumourigenic. Nonetheless, a few reports have proposed a tumour-promoting effect of cannabinoids (Cudaback et al. 2010; Hart et al. 2004; McKallip et al. 2002; Zhu et al. 2000). These apparently conflicting observations are discussed below.
Cannabinoids impair tumour progression at different levels. Their most prevalent effect is the induction of cancer cell death by apoptosis and the inhibition of cancer cell proliferation . At least one of these actions has been demonstrated in virtually all cancer cell types tested (Velasco et al. 2012). In addition, in vivo experiments have shown that cannabinoids impair tumour angiogenesis and block invasion and metastasis.
4 Mechanisms of Antitumour Effects
4.1 Induction of Cancer Cell Death
A significant amount of the research conducted so far on the mechanism of cannabinoid antitumour activity has focussed on glioma cells. Initial studies showed that THC and other cannabinoids induce the apoptotic death of glioma cells via CB1- and CB2-dependent stimulation of the de novo synthesis of the pro-apoptotic sphingolipid ceramide (Blazquez et al. 2004; Galve-Roperh et al. 2000; Gomez del Pulgar et al. 2002; Sanchez et al. 2001). Further studies, based on the analysis of the gene expression profile of THC-sensitive and resistant glioma cells, gave further insight into the specific signalling events downstream of ceramide that are activated in cancer cells by CB1 and CB2 cannabinoid receptor agonists (Carracedo et al. 2006b). THC acutely up-regulates the expression of the stress-regulated protein p8 (also named NUPR1), a transcriptional regulator that has been implicated in the control of tumourigenesis and tumour progression (Encinar et al. 2001), together with several of its downstream targets such as the endoplasmic reticulum (ER) stress-related transcription factors ATF4 and CHOP and the pseudokinase tribbles-homologue 3 (TRIB3) (Carracedo et al. 2006b) (Fig. 1).
Cannabinoid -induced apoptosis relies on the stimulation of ER stress and autophagy . Scheme depicting the mechanism of cannabinoid-induced apoptosis in glioma, pancreatic and hepatocellular carcinoma cells. This signalling route may constitute the main mechanism of cannabinoid-induced cell death, with some variations inherent to different types of cancer cells. Cannabinoid agonists bind to CB1 and/or CB2 receptors (CBR) to stimulate de novo synthesis of ceramide (Carracedo et al. 2006b; Galve-Roperh et al. 2000; Gomez del Pulgar et al. 2002; Herrera et al. 2006; Salazar et al. 2009), which triggers the induction of an endoplasmic reticulum (ER) stress-related response that promotes the up-regulation of the transcription factor p8 and several of its downstream targets, including the pseudokinase Tribbles 3 (TRIB3) (Carracedo et al. 2006b; Salazar et al. 2009). This favours the interaction of TRIB3 with AKT (Du et al. 2003; Salazar et al. 2009), thus leading to the inhibition of the AKT-mechanistic target of rapamycin C1 (mTORC1) axis and the subsequent induction of autophagy (Salazar et al. 2009). Autophagy is upstream of intrinsic mitochondrial apoptosis in the process of cannabinoid-induced cell death. The importance of this pathway is highlighted by the ability of different chemical and genetic manipulations to block cannabinoid-induced cell death. In hepatocellular carcinoma cells, the cannabinoid-evoked and ER stress-dependent activation of calcium/calmodulin-dependent protein kinase kinase 2-beta (CaCMKKβ) and AMP-activated protein kinase (AMPK) leads, together with the p8–TRIB3 pathway, to autophagy and apoptosis (Vara et al. 2011). The cannabinoid-evoked inhibition of AKT could promote cycle arrest in breast cancer and melanoma cells, as well as apoptosis, through additional mechanisms, including the decreased phosphorylation of the pro-apoptotic protein BCL2-associated agonist of cell death (BAD) (Ellert-Miklaszewska et al. 2005) and the activation of the cyclin-dependent kinase (CDK) inhibitory proteins p21 and p27 (Blazquez et al. 2006; Caffarel et al. 2008; Caffarel et al. 2006). This would lead to the subsequent decreased phosphorylation of the retinoblastoma protein (pRB), which thus would be active to arrest cell cycle. ATF4 activating transcription factor 4, CHOP C/EBP homology protein, eIF2α eukaryotic translation initiation factor 2 alpha, SPT serine palmitoyltransferase
ER stress, as induced by different anticancer agents, can also lead through different mechanisms (Verfaillie et al. 2010) to the stimulation of autophagy , an essential cellular process participating in a number of physiological functions within the cell (Mizushima et al. 2008; Verfaillie et al. 2010). During autophagy, organelles and other cytoplasmic components are engulfed within double-membrane vesicles designated autophagosomes. The maturation of these vesicles involves their fusion with lysosomes, which leads in turn to the degradation of the autophagosome components by lysosomal enzymes (Mizushima et al. 2008). Autophagy is primarily a cytoprotective mechanism, although its activation can also lead to cell death (Eisenberg-Lerner et al. 2009; Mizushima et al. 2008). Indeed, THC-triggered stimulation of the p8-regulated pathway enhances the inhibitory interaction of TRIB3 with a pro-survival kinase, AKT, which leads to the inhibition of the mammalian target of rapamycin complex 1 (mTORC1) and the subsequent stimulation of autophagy-mediated cell death (Salazar et al. 2009, 2013) (Fig. 1). CB1 and/or CB2 cannabinoid receptor agonists induce autophagy in different types of cancer cells in culture, and pharmacological or genetic inhibition of autophagy prevents the antitumour action of these agents in different animal models of cancer (Fig. 1), thus demonstrating that autophagy is important for the antineoplastic activity of cannabinoid receptor agonists (Salazar et al. 2009; Vara et al. 2011). Moreover, autophagy blockade prevents cannabinoid receptor agonist-induced apoptosis and cell death whereas apoptosis blockade prevents cell death but not autophagy induced by these compounds (Salazar et al. 2009; Vara et al. 2011). This indicates that autophagy is upstream of apoptosis in the process of cannabinoid receptor agonist-induced cell death (Fig. 1).
The direct participation of the p8-mediated autophagy pathway in the antitumour action of THC and other CB1 and/or CB2 receptor agonists has been clearly demonstrated in glioma cells and pancreatic and hepatic cancer cells (Carracedo et al. 2006a; Carracedo et al. 2006b; Salazar et al. 2009; Vara et al. 2011). At least part of this signalling route has also been found to be up-regulated after cannabinoid treatment in other types of cancer cells. This suggests that—with some variations—this could be a general mechanism by which activation of CB1 and CB2 receptors promotes cancer cell death.
Additional mechanisms may nonetheless cooperate with the p8-mediated autophagy pathway to evoke cancer cell death (Fig. 1). For example, in hepatocellular carcinoma cells, THC and the CB2 receptor agonist JWH-015 can trigger an ER stress-dependent activation of AMPK that cooperates with the TRIB3-mediated inhibition of the AKT–mTORC1 axis in the stimulation of autophagy–mediated cell death (Vara et al. 2011). In melanoma (Blazquez et al. 2006), breast carcinoma (Caffarel et al. 2006, 2012) and prostate carcinoma (Sarfaraz et al. 2006) cells, cannabinoid receptor agonists can induce cell cycle arrest in concert with apoptosis (Blazquez et al. 2006; Caffarel et al. 2006; Sarfaraz et al. 2006). Of note the antiproliferative action—at least in melanoma (Blazquez et al. 2006) and breast cancer (Caffarel et al. 2006) cells—of THC and CB2 receptor agonists also relies on AKT inhibition.
Likewise, the effect of cannabinoid receptor agonists in hormone-dependent tumours may rely, at least in part, on their ability to interfere with the activation of growth factor receptors (Guzman 2003; Sarfaraz et al. 2008). This interference and other mechanisms (Guindon and Hohmann 2011) may participate in the cytotoxic action of cannabinoid receptor agonists in different types of cancer cells together with the autophagy -mediated cell death pathway. However, further investigation is required to clarify this issue (Box 2).
Box 2. Mechanism of Cannabinoid Receptor-Mediated Cancer Cell Death: Some Important Unanswered Questions
Research conducted during the last few years has shed light onto the intracellular signalling mechanisms underlying cannabinoid anticancer action. However, a number of important observations—in particular ones related to the role played by cannabinoid receptors in the triggering of these signals—remain to be clarified. For some examples of these, see below.
-
Unlike the cell death-promoting action of cannabinoids on cancer cells, the viability of normal (non-transformed) cells is unaffected or—under certain conditions—even enhanced by cannabinoid challenge (Carracedo et al. 2006b; Galve-Roperh et al. 2000, 2008; Gomez del Pulgar et al. 2002; Salazar et al. 2009). For example, THC treatment of astrocytes (a cell type that expresses functional CB1 receptors) does not trigger the activation of ER stress, the up-regulation of the p8 pathway, the inhibition of the AKT–mTORC1 axis or the stimulation of autophagy and apoptosis , even when concentrations of THC higher than those that promote glioma cell death are used (Carracedo et al. 2006b; Salazar et al. 2009). Similar results were obtained with primary embryonic fibroblasts (Carracedo et al. 2006b; Salazar et al. 2009) and other types of non-transformed cells expressing functional cannabinoid receptors when compared with their transformed counterparts (Blazquez et al. 2006; Caffarel et al. 2006; Casanova et al. 2003; Chan et al. 1996). Thus, stimulation of cannabinoid receptors seems to be coupled to the activation of different signalling mechanisms in transformed and non-transformed cells. The precise molecular reasons for this different behaviour remain as an important open question in the cannabinoid field.
-
Another intriguing observation is that, in some types of cancer cells, such as glioma cells, pharmacological blockade of either CB1 or CB2 receptors prevents cannabinoid-induced cell death with similar efficacy (Galve-Roperh et al. 2000; Lorente et al. 2011), while in other types of cancer cells, for example, pancreatic (Carracedo et al. 2006a), breast (Caffarel et al. 2006) or hepatic (Vara et al. 2011) carcinoma cells, antagonists of CB2 but not of CB1 receptors inhibit cannabinoid antitumour actions. Why cannabinoids produce their antitumour actions through one or other of these receptor types depending on the type of cancer cell studied has yet to be established.
-
Some cannabinoid receptor agonists promote cancer cell death more efficiently than other agonists that exhibit similar or even higher affinity for CB1 or CB2 receptors. For example, THC promotes cancer cell death in a CB1 and/or CB2-dependent manner at lower concentrations than the synthetic cannabinoid receptor agonist WIN-55,212-2, although the latter agent displays significantly higher affinity for CB1 and CB2 receptors in binding assays (Pertwee et al. 2010).
Further work aimed at investigating, for example, CB receptor homo or hetero-oligomerization in response to different cannabinoid agonists, their association with specific domains in the plasma membrane such as lipid rafts, changes in the subcellular location of CB receptors, and the selective coupling to different G proteins and other signalling proteins will be essential to answer these questions and precisely define the role played by each cannabinoid receptor type as an anticancer signalling platform.
Of note, cannabidiol (CBD), a phytocannabinoid with low affinity for cannabinoid receptors (Pertwee 2009), and other marijuana-derived cannabinoids (Ligresti et al. 2006) have also been proposed to promote the apoptotic death of cancer cells acting independently of CB1 and CB2 receptors. The mechanism by which CBD produces this effect has not been completely clarified as yet, but seems to rely—at least in part—on its ability to enhance the production of reactive oxygen species in cancer cells (Massi et al. 2008; Shrivastava et al. 2011). It has also been proposed that CBD may activate TRPV2 receptors to promote glioma cell death (Nabissi et al. 2012).
4.2 Inhibition of Angiogenesis, Invasion and Metastasis
In cancer cells, cannabinoid receptor agonists block the activation of the vascular endothelial growth factor (VEGF) pathway, an inducer of angiogenesis . Specifically, different elements of this cascade, such as the main ligand (VEGF) and the active forms of its main receptors (VEGFR1 and VEGFR2), are down-regulated upon treatment of skin carcinomas (Casanova et al. 2003), gliomas (Blazquez et al. 2003; Blazquez et al. 2004) and thyroid carcinomas (Portella et al. 2003) with CB1 and/or CB2 receptor agonists. In vascular endothelial cells, CB1 and/or CB2 receptor activation inhibits proliferation and migration and induces apoptosis (Blazquez et al. 2003; Pisanti et al. 2007). These and perhaps other cannabinoid-evoked actions result in a normalized tumour vasculature; that is, smaller and/or fewer vessels that are more differentiated and less leaky.
Likewise, CB1 and/or CB2 receptor agonists reduce the formation of distant tumour masses in animal models of both induced and spontaneous metastasis and inhibit adhesion, migration and invasiveness of glioma (Blazquez et al. 2008), breast (Grimaldi et al. 2006; Qamri et al. 2009), lung (Preet et al. 2008; Ramer and Hinz 2008), and cervical (Ramer and Hinz 2008) cancer cells in culture. These effects depend, at least in part, on the modulation of extracellular proteases [such as matrix metalloproteinase 2 (MMP2)] (Blazquez et al. 2008) and their inhibitors [such as tissue inhibitor of matrix metalloproteinases 1 (TIMP1)] (Ramer and Hinz 2008).
Of note, pharmacological inhibition of ceramide biosynthesis abrogates the antitumour and anti-angiogenic effect of CB1 and/or CB2 receptor agonists in glioma xenografts and decreases VEGF production by glioma cells in vitro and in vivo (Blazquez et al. 2004). Likewise, inhibition of MMP-2 expression and glioma cell invasion is prevented by blocking ceramide biosynthesis and by knocking down p8 expression (Blazquez et al. 2008). Although further research is still necessary to precisely define the molecular mechanisms responsible for these actions of cannabinoids, these observations indicate that the ceramide/p8-regulated pathway plays a general role in the antitumour activity of cannabinoids targeting CB1 and CB2 receptors.
It is worth noting that CBD, by acting independently of CB1 and CB2 receptors, produces a remarkable antitumour effect—including reduction of invasiveness and metastasis—in different animal models of cancer . This effect of CBD seems to rely—at least in part—on the down-regulation of the helix-loop-helix transcription factor inhibitor of DNA binding-1 (ID-1) (McAllister et al. 2011; Soroceanu et al. 2012).
4.3 Regulation of Antitumour Immunity
Of note, stimulation of cannabinoid receptors may lead to important changes in the processes that regulate antitumour immunity. Thus, for example, treatment of mice with THC triggers a shift (from Th1 to Th2) on the cytokine profile (Lu et al. 2006; McKallip et al. 2005; Newton et al. 2009; Steffens et al. 2005) and induces mobilization of myeloid-derived suppressor cells (Hegde et al. 2010), two events that play a critical role in the suppression of antitumour immunity. In agreement with this notion, stimulation of CB2 receptors has been proposed in some reports to enhance tumourigenesis by interfering with tumour surveillance by the immune system (McKallip et al. 2005; Zhu et al. 2000). By contrast, cannabinoids may also enhance immune system-mediated tumour surveillance in some contexts: the antitumour action of WIN 55212-2 (a CB1/CB2-mixed agonist) or JWH-133 (a CB2-selective agonist) was more pronounced in melanoma xenografts generated in immunocompetent mice compared with those in immunodeficient mice (Blazquez et al. 2006). This also indicates that, at least in this model, stimulation of CB2 receptors primarily inhibits tumour growth through direct effects on cancer cells rather than necessarily through interfering with the normal antitumour function of the immune system. In line with this idea, treatment for 2 years of immunocompetent rats with very high doses (50 mg/kg/day 5 times a week) of THC decreased the incidence of several types of tumours and enhanced the overall survival of these animals (Chan et al. 1996). These observations might be related to the ability of THC to reduce inflammation (Burstein and Zurier 2009; Liu et al. 2010), an effect that may prevent certain types of cancer (Liu et al.). For cannabinoid use to be clinically successful, antitumour effects will need to overcome immunosuppressive (potentially tumour-promoting) effects. Additional studies should clarify this issue. For example, it could be conceivable to study the effect of cannabinoid administration on the generation and progression of tumours exhibiting different sensitivity to CB1 and/or CB2 receptor agonists and generated in immunocompetent or immunodeficient mice in which the expression of CB1 and/or CB2 receptors in cells from the immune system has been genetically manipulated.
5 Resistance Mechanisms
Numerous studies have contributed to our appreciation of the heterogeneity of cancer , whereby each subtype of cancer, and even each individual tumour, exhibits a series of molecular characteristics that determines its behaviour and, in particular, its responsiveness to different anticancer drugs. In agreement with this line of reasoning, are results obtained in a recent investigation into the molecular features associated with the resistance of a collection of human glioma cell lines and primary cultures to cannabinoid antitumour action (Lorente et al. 2011). This study showed that, although the apoptotic effect of THC on glioma cells relied on the stimulation of cannabinoid receptors and the activation the p8-mediated autophagy pathway, the differences in the sensitivity to THC-induced cell death correlated with the enhanced expression of a particular set of genes in the THC-resistant glioma cells rather than with the presence of different expression levels of CB1 or CB2 receptors (Lorente et al. 2011). Of interest, up-regulation of one of these genes, midkine (MDK), that encodes a growth factor that has been previously associated with increased malignancy and resistance to anticancer therapies in several types of tumours (Kadomatsu 2005; Mirkin et al. 2005), correlates with a lower overall survival of patients with glioblastoma (Lorente et al. 2011). Moreover, MDK plays a direct role in the resistance to THC action via stimulation of the anaplastic lymphoma kinase [ALK (Palmer et al. 2009)]. Thus, the stimulation of ALK by MDK inhibits the THC-evoked autophagy-mediated cell death pathway. Further research should clarify whether this mechanism could also be responsible for the resistance of cancer cells expressing high levels of MDK to other therapies. Interestingly, in vivo silencing of MDK or pharmacological inhibition of ALK in a mouse xenograft model abolishes the resistance to THC treatment of established tumours derived from cannabinoid-resistant glioma cells (Lorente et al. 2011).
Taken together, these findings support the idea that stimulation of the MDK–ALK axis promotes resistance to THC antitumour action in gliomas and could help to set the basis for the potential clinical use of THC in combination with inhibitors of this axis (Fig. 2). In line with this idea, ALK inhibitors have started to be used in clinical trials for the management of non-small-cell lung cancer and other types of tumours (de Bono and Ashworth 2010; Grande et al. 2011). Future research should clarify whether this mechanism of resistance to cannabinoid action operates in other types of tumours. In agreement with this possibility, MDK silencing enhanced the sensitivity of cannabinoid-resistant pancreatic cancer cells to THC-induced cell death (Lorente et al. 2011).
Possible strategies aimed at optimizing cannabinoid-based therapies against gliomas. Glioblastoma is highly resistant to current anticancer therapies (Lonardi et al. 2005; Nieder et al. 2006; Purow and Schiff 2009). Specifically, resistance of glioma cells to cannabinoid-induced cell death relies, at least in part, on the enhanced expression of the growth factor midkine (MDK) and the subsequent activation of the anaplastic lymphoma receptor tyrosine kinase (ALK) (Lorente et al. 2011). Likewise, enhanced expression of the heparin-bound EGFR-ligand amphiregulin (AREG) can promote resistance to THC antitumour action via ERK stimulation (Lorente et al. 2009). Combination of THC with pharmacological inhibitors of ALK (or genetic inhibition of MDK) enhances cannabinoid action in resistant tumours, which provides the rationale for the design of targeted therapies capable of increasing cannabinoid antineoplastic activity (Lorente et al. 2011). Combinations of cannabinoids with classical chemotherapeutic drugs such as the alkylating agent temozolomide [TMZ; the benchmark agent for the management of glioblastoma (Lonardi et al. 2005; Stupp et al. 2005)] have been shown to produce a strong anticancer action in animal models (Torres et al. 2011). Combining cannabinoids and TMZ is thus a very attractive possibility for clinical studies aimed at investigating cannabinoids antitumour effects in glioblastoma. Other potentially interesting strategies to enhance cannabinoid anticancer action (still requiring additional experimental support from data obtained using preclinical models) could be combining cannabinoids with endoplasmic reticulum (ER) stress and/or autophagy inducers or with inhibitors of the AKT-mechanistic target of rapamycin C1 (mTORC1) axis. Abs antibodies, EGFR epidermal growth factor receptor, ERK extracellular signal-regulated kinase, GF growth factors, RTK receptor tyrosine kinase, TRIB3 tribbles 3, VEGF vascular endothelial growth factor
The release by cancer cells of other growth factors has also been implicated in the mechanism of resistance to cannabinoid antitumour action. Thus, increased expression of the heparin-bound epidermal growth factor receptor (EGFR) ligand amphiregulin is associated with enhanced resistance to THC antitumour action in glioma xenografts (Lorente et al. 2009). Of note, illustrating that the dose of cannabinoids could be crucial for their optimal therapeutic effect, low (sub-micromolar) concentrations of THC or other synthetic cannabinoid agonists enhance the proliferation of several cancer cell lines in vitro. This effect relies on the activation of the protease ADAM17, the shedding of heparin-bound EGFR ligands, including amphiregulin, and the subsequent stimulation of extracellular signal-regulated kinase (ERK) and AKT pathways (Hart et al. 2004). In line with this idea, a recent report has shown that treatment with the synthetic cannabinoid, CP-55,940, increases the proliferation of murine glioma cells engineered to express CB1 or CB2 receptors only when these receptors were coupled to AKT activation (Cudaback et al. 2010). Although a pro-tumourigenic effect has not been observed on the growth of tumour xenografts generated with glioma cells and treated with low doses of THC (Torres et al. 2011), increased expression of amphiregulin promotes resistance to THC antitumour action through a mechanism that involves the EGFR-dependent stimulation of ERK and the subsequent inhibition of p8 and TRB3 expression. Likewise, pharmacological inhibition of EGFR, ERK (Lorente et al. 2009) or AKT (authors’ unpublished observations) enhances the cell death-promoting action of THC in cultures of glioma cells. These observations suggest that targeting EGFR and the AKT and ERK pathways could enhance the antitumour effect of cannabinoids.
6 Cannabinoid -Based Combinational Therapies
The use of combinational anticancer therapies has a number of theoretical advantages over single-agent-based strategies as they allow the simultaneous targeting of tumour growth, progression and spreading at different levels. In line with this idea, recent observations suggest that the combined administration of cannabinoids with other anticancer drugs acts synergistically to reduce tumour growth. For example, the administration of THC and temozolomide (the benchmark agent for the management of glioblastoma) exerts a strong antitumour action in glioma xenografts, an effect that is also evident in temozolomide-resistant tumours (Torres et al. 2011). Of interest, no toxicity was observed in mice treated with combinations of THC and temozolomide (Torres et al. 2011). As most patients with glioblastoma undergo temozolomide treatment, these findings indicate that the combined administration of temozolomide and cannabinoids could be therapeutically exploited for the management of glioblastoma (Fig. 2).
Likewise, another study has recently shown that the combined administration of gemcitabine (the benchmark agent for the treatment of pancreatic cancer ) and different cannabinoid agonists synergistically reduces the viability of pancreatic cancer cells (Donadelli et al. 2011). Other reports indicate that anandamide and HU-210 may also enhance the anticancer activity of paclitaxel (Miyato et al. 2009) and 5-fluorouracil (Gustafsson et al. 2009), respectively.
An additional approach has been to combine THC with CBD, a phytocannabinoid that reduces—although to a lower extent than THC—the growth of several types of tumour xenografts through a still poorly defined mechanism (Massi et al. 2006; McAllister et al. 2007; Shrivastava et al. 2011). Combined administration of THC and CBD enhances the anticancer activity of THC and reduces the doses of THC needed to induce its tumour growth-inhibiting activity (Marcu et al. 2010; Torres et al. 2011). Moreover, the combination of THC and CBD together with temozolomide produces a striking reduction in the growth of glioma xenografts even when low doses of THC are used (Torres et al. 2011). Of note, CBD has also been shown to alleviate some of the undesired effects of THC administration, such as convulsions, discoordination and psychotic events, and therefore improves the tolerability of cannabis-based medicines (Pertwee 2009). As mentioned above, C. sativa produces ~108 different cannabinoids and, apart from CBD, some of the other cannabinoids present in marijuana might attenuate the psychoactive side effects of THC or even produce other therapeutic benefits (Pertwee 2009). Thus, we think that clinical studies aimed at analysing the efficacy of cannabinoids as antitumour agents should be based on the use both of pure substances, such as THC and CBD, and of cannabis extracts containing controlled amounts of THC, CBD and other cannabinoids.
7 Clinical Antitumour Effects of Cannabinoids
Although the clinical approval of cannabinoids is largely restricted to palliative uses in various diseases, following promising preclinical data, the antitumour effects of cannabinoids are beginning to be clinically assessed. In a pilot Phase I clinical study, nine patients with actively-growing recurrent glioblastoma that had previously failed standard therapy underwent intracranial THC administration (Guzman et al. 2006). Under these conditions, cannabinoid delivery was safe and could be achieved without significant unwanted effects. In addition, although no statistically significant conclusions can be extracted from a cohort of nine patients, the results obtained in that study suggested that some patients responded—at least partially—to THC treatment in terms of decreased tumour growth rate, as evaluated by magnetic resonance imaging (Guzman et al. 2006). Importantly, analyses of samples obtained from two patients in this study before and after THC administration indicate that the molecular mechanism of cannabinoid antitumour action delineated in the previous sections, namely p8 and TRIB3 up-regulation (Carracedo et al. 2006b; Salazar et al. 2009), mTORC1 inhibition (Salazar et al. 2009), stimulation of autophagy and apoptosis (Carracedo et al. 2006b; Guzman et al. 2006; Salazar et al. 2009), inhibition of cell proliferation (Guzman et al. 2006), decreased VEGF signalling (Blazquez et al. 2004) and MMP-2 down-regulation (Blazquez et al. 2008), also operates in cancer patients. These findings were encouraging and reinforced the interest on the potential use of cannabinoids in cancer therapies. However, they also highlighted the need for further research aimed at optimizing the use of cannabinoids in terms of patient selection, combination with other anticancer agents and use of other routes of administration (see Box 3). Two clinical trials that are currently ongoing could shed some light on these issues. One of these studies is a Phase I/II trial aimed at evaluating the combined effect of Sativex (an oro-mucosal cannabis extract whose main active components are THC and CBD in a ca. 1:1 ratio) and temozolomide in patients with recurrent glioblastoma multiforme (http://clinicaltrials.gov/show/NCT01812603). The other study is a Phase II trial aimed at evaluating the effect of CBD as single treatment in patients with solid tumours (http://clinicaltrials.gov/ct2/show/NCT02255292?term=cbd+solid+tumour&rank=1). Hopefully, more clinical trials will add in the near future to these two to allow determining whether cannabinoids can be used, other than for their palliative effects, to treat cancer patients
Box 3. Different Pharmacological Approaches to Target Cancer Cells with Cannabinoids
Cannabinoid agonists or enhancers of endocannabinoid tone?
Administration of endocannabinoids or inhibitors of endocannabinoid-degrading enzymes has been shown to reduce the growth of different types of tumour xenografts (Bifulco et al. 2001; Ligresti et al. 2003) and, therefore, could be a reasonable strategy for targeting cannabinoid receptors for anticancer purposes. However, as discussed in Box 1, the role of the endocannabinoid system, including the endocannabinoid-degrading enzymes, in the control of tumour generation and progression is not well understood. Since enhancing endocannabinoid tone only has mild anti-tumour effects in mice and since no inhibitor of endocannabinoid degradation has been approved as yet for use in humans, clinical studies aimed at analysing the efficacy of cannabinoids as anti-tumour agents should be based on the use of plant-derived or synthetic agonists of cannabinoid receptors rather than on endocannabinoids or inhibitors of endocannabinoid degradation.
Cannabis extracts or pure cannabinoids?
The long-known therapeutic properties of Cannabis sativa—including amelioration of symptoms associated with cancer and its chemotherapy—have led to the authorization of the medical use of this plant and its extracts in several countries. As mentioned in the text, C. sativa produces ~108 different cannabinoids, including THC and CBD. Some of the other cannabinoids present in marijuana may contribute to the attenuation of THC psychoactive-side effects or even to the production of other therapeutic benefits (Pertwee 2009). However, pure drugs are more prone to standardization than complex molecular cocktails. Thus, it would be ideal that studies aimed at investigating the anticancer actions of cannabinoids in patients were performed comparatively with both pure substances and cannabis extracts containing controlled amounts of THC, CBD and other cannabinoids.
Which routes of cannabinoid administration?
The most widely used route of administration of recreational and self-medicated marijuana is smoking. Although THC and other phytocannabinoids are rapidly absorbed by inhalation, smoking is an unattractive clinical option. Preclinical work in animal models has typically administered cannabinoids intra peri-tumourally. Likewise, in the only clinical trial in which a cannabinoid has been assayed as an anti-tumour agent, THC was administered locally (intracranial delivery to Glioblastoma patients) (Guzman et al. 2006). Nevertheless, this route of administration has many obvious limitations. Currently available cannabis-based medicines are administered as capsules or using an oro-mucosal spray (Pertwee 2009). Preclinical animal models have yielded data indicating that systemic (oral or intraperitoneal) administration of cannabinoids effectively reduces tumour growth (author’s unpublished observations), so it seems reasonable that future clinical studies directed at determining the efficacy of cannabinoids as anti-tumour agents use oral or oro-mucosal routes of administration.
8 Conclusions and Future Directions
It is widely believed that strategies aimed at reducing mortality from cancer should consist of targeted therapies capable of providing the most efficacious and selective treatment for each individual tumour and patient. Thus, the major focus of anticancer-drug development has progressively moved from non-specific chemotherapies to molecularly targeted inhibitors. However, despite the huge amount of preclinical literature on how these rationally designed compounds work, the advance of most of these drugs into the clinic is still limited.
How do cannabinoid-based medicines fit into this ongoing scenario? Let us consider gliomas, the type of cancer on which the most detailed cannabinoid research has been conducted to date. As discussed above, engagement of a molecular target (CB receptors) by a family of selective drugs (THC and other cannabinoid agonists) inhibits tumour growth in animal models through a well-established mechanism of action that seems to operate in patients. Moreover, cannabinoids potentiate the antitumour efficacy of temozolomide and ALK inhibitors in mice harbouring gliomas. These findings provide preclinical proof-of-concept that “cannabinoid sensitizers” could improve the clinical efficacy of classical cytotoxic drugs in glioblastoma (Fig. 2) and perhaps other highly malignant tumours such as pancreatic cancer, melanoma and hepatocellular carcinoma. However, further research is required to define the precise molecular crosstalk between cannabinoids and chemotherapeutic drugs and to optimize the pharmacology of preclinical cannabinoid-based combinational therapies. Of note, the role of the endocannabinoid system in cancer generation and progression needs to be explored in further detail as—depending on the experimental model—genetic inactivation of cannabinoid receptors may enhance or decrease tumourigenesis in animal models of cancer. Accordingly, whether pharmacological manipulation of endocannabinoid levels (e.g. by using inhibitors of the enzymes involved in the degradation of these local mediators) could be used alone or in combination with other anticancer agents as an anticancer strategy needs to be clarified.
Regarding patient stratification, we should unequivocally determine which particular individuals are potentially responsive to cannabinoid administration. For this purpose, high-throughput approaches should be implemented to find cannabinoid therapy-associated biomarkers in tumour biopsies or, ideally, in easily acquired fluids containing circulating cancer cells or enhanced levels of resistance factors that could have been released by cancer cells. These biomarkers would conceivably relate to cannabinoid pharmacodynamics—namely expression and activity of cannabinoid receptors and their downstream cell-death inducing effectors. This would be analogous to the biochemical evaluation of oestrogen and ERBB2 receptors, which predict the benefit from endocrine therapies and trastuzumab, respectively, in breast cancer. Predictive markers to define the sensitivity of a particular tumour to cannabinoid-based therapies could also include the status of growth factors, such as MDK in gliomas, as well as their receptors and signalling partners.
In conclusion, cannabinoids induce tumour cell death and inhibit tumour angiogenesis and invasion in animal models of cancer , and there are indications that they do so as well in patients with glioblastoma. As cannabinoids show an acceptable safety profile, clinical trials testing them as single drugs or, ideally, in combination therapies in glioblastoma and other types of cancer are both warranted and urgently needed.
Abbreviations
- 2-AG:
-
2-Arachidonoylglycerol
- ALK:
-
Anaplastic lymphoma kinase
- ATF-4:
-
Activating transcription factor 4
- CB1 :
-
Cannabinoid CB1 receptor
- CB2 :
-
Cannabinoid CB2 receptor
- CBD:
-
Cannabidiol
- CHOP:
-
C/EBP homologous protein
- EGFR:
-
Epidermal growth factor receptor
- ER:
-
Endoplasmic reticulum
- ERK:
-
Extracellular signal-regulated kinase
- MDK:
-
Midkine
- mTORC1:
-
Mammalian target of rapamycin complex 1
- mTORC2:
-
Mammalian target of rapamycin complex 2
- THC:
-
Δ9-tetrahydrocannabinol
- TRIB3:
-
Tribbles-homologue 3
- TRPV1:
-
Transient receptor potential cation channel subfamily V member 1
- VEGF:
-
Vascular endothelial growth factor
References
Atwood BK, Huffman J, Straiker A, Mackie K (2010) JWH018, a common constituent of ‘Spice’ herbal blends, is a potent and efficacious cannabinoid CB receptor agonist. Br J Pharmacol 160:585–593
Bifulco M, Laezza C, Portella G, Vitale M, Orlando P, De Petrocellis L, Di Marzo V (2001) Control by the endogenous cannabinoid system of ras oncogene-dependent tumor growth. FASEB J 15:2745–2747
Blazquez C, Casanova ML, Planas A, Gómez del Pulgar T, Villanueva C, Fernandez-Acenero MJ, Aragones J, Huffman JW, Jorcano JL, Guzman M (2003) Inhibition of tumor angiogenesis by cannabinoids. FASEB J 17:529–531
Blazquez C, Gonzalez-Feria L, Alvarez L, Haro A, Casanova ML, Guzman M (2004) Cannabinoids inhibit the vascular endothelial growth factor pathway in gliomas. Cancer Res 64:5617–5623
Blazquez C, Carracedo A, Barrado L, Real PJ, Fernandez-Luna JL, Velasco G, Malumbres M, Guzman M (2006) Cannabinoid receptors as novel targets for the treatment of melanoma. FASEB J 20:2633–2635
Blazquez C, Salazar M, Carracedo A, Lorente M, Egia A, Gonzalez-Feria L, Haro A, Velasco G, Guzman M (2008) Cannabinoids inhibit glioma cell invasion by down-regulating matrix metalloproteinase-2 expression. Cancer Res 68:1945–1952
Burstein SH, Zurier RB (2009) Cannabinoids, endocannabinoids, and related analogs in inflammation. AAPS J 11:109–119
Caffarel MM, Sarrio D, Palacios J, Guzman M, Sanchez C (2006) Delta9-tetrahydrocannabinol inhibits cell cycle progression in human breast cancer cells through Cdc2 regulation. Cancer Res 66:6615–6621
Caffarel MM, Moreno-Bueno G, Cerutti C, Palacios J, Guzman M, Mechta-Grigoriou F, Sanchez C (2008) JunD is involved in the antiproliferative effect of Delta9-tetrahydrocannabinol on human breast cancer cells. Oncogene 27:5033–5044
Caffarel MM, Andradas C, Perez-Gomez E, Guzman M, Sanchez C (2012) Cannabinoids: a new hope for breast cancer therapy? Cancer Treat Rev 38:911–918
Carracedo A, Gironella M, Lorente M, Garcia S, Guzman M, Velasco G, Iovanna JL (2006a) Cannabinoids induce apoptosis of pancreatic tumor cells via endoplasmic reticulum stress-related genes. Cancer Res 66:6748–6755
Carracedo A, Lorente M, Egia A, Blazquez C, Garcia S, Giroux V, Malicet C, Villuendas R, Gironella M, Gonzalez-Feria L, Piris MA, Iovanna JL, Guzman M, Velasco G (2006b) The stress-regulated protein p8 mediates cannabinoid-induced apoptosis of tumor cells. Cancer Cell 9:301–312
Casanova ML, Blazquez C, Martinez-Palacio J, Villanueva C, Fernandez-Acenero MJ, Huffman JW, Jorcano JL, Guzman M (2003) Inhibition of skin tumor growth and angiogenesis in vivo by activation of cannabinoid receptors. J Clin Invest 111:43–50
Chan PC, Sills RC, Braun AG, Haseman JK, Bucher JR (1996) Toxicity and carcinogenicity of delta 9-tetrahydrocannabinol in Fischer rats and B6C3F1 mice. Fundam Appl Toxicol 30:109–117
Cudaback E, Marrs W, Moeller T, Stella N (2010) The expression level of CB1 and CB2 receptors determines their efficacy at inducing apoptosis in astrocytomas. PLoS One 5, e8702
de Bono JS, Ashworth A (2010) Translating cancer research into targeted therapeutics. Nature 467:543–549
Devane WA, Hanus L, Breuer A, Pertwee RG, Stevenson LA, Griffin G, Gibson D, Mandelbaum A, Etinger A, Mechoulam R (1992) Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 258:1946–1949
Donadelli M, Dando I, Zaniboni T, Costanzo C, Dalla Pozza E, Scupoli MT, Scarpa A, Zappavigna S, Marra M, Abbruzzese A, Bifulco M, Caraglia M, Palmieri M (2011) Gemcitabine/cannabinoid combination triggers autophagy in pancreatic cancer cells through a ROS-mediated mechanism. Cell Death Dis 2, e152
Du K, Herzig S, Kulkarni RN, Montminy M (2003) TRB3: a tribbles homolog that inhibits Akt/PKB activation by insulin in liver. Science 300:1574–1577
Eisenberg-Lerner A, Bialik S, Simon HU, Kimchi A (2009) Life and death partners: apoptosis, autophagy and the cross-talk between them. Cell Death Differ 16:966–975
Ellert-Miklaszewska A, Kaminska B, Konarska L (2005) Cannabinoids down-regulate PI3K/Akt and Erk signalling pathways and activate proapoptotic function of Bad protein. Cell Signal 17:25–37
Encinar JA, Mallo GV, Mizyrycki C, Giono L, Gonzalez-Ros JM, Rico M, Canepa E, Moreno S, Neira JL, Iovanna JL (2001) Human p8 is a HMG-I/Y-like protein with DNA binding activity enhanced by phosphorylation. J Biol Chem 276:2742–2751
Fernandez-Ruiz J, Romero J, Velasco G, Tolon RM, Ramos JA, Guzman M (2007) Cannabinoid CB2 receptor: a new target for controlling neural cell survival? Trends Pharmacol Sci 28:39–45
Galve-Roperh I, Sanchez C, Cortes ML, Gómez del Pulgar T, Izquierdo M, Guzman M (2000) Anti-tumoral action of cannabinoids: involvement of sustained ceramide accumulation and extracellular signal-regulated kinase activation. Nat Med 6:313–319
Galve-Roperh I, Aguado T, Palazuelos J, Guzman M (2008) Mechanisms of control of neuron survival by the endocannabinoid system. Curr Pharm Des 14:2279–2288
Gaoni Y, Mechoulam R (1964) Isolation, structure and partial synthesis of an active constituent of hashish. J Am Chem Soc 86:1646–1647
Gomez del Pulgar T, Velasco G, Sanchez C, Haro A, Guzman M (2002) De novo-synthesized ceramide is involved in cannabinoid-induced apoptosis. Biochem J 363:183–188
Grande E, Bolos MV, Arriola E (2011) Targeting oncogenic ALK: a promising strategy for cancer treatment. Mol Cancer Ther 10:569–579
Grimaldi C, Pisanti S, Laezza C, Malfitano AM, Santoro A, Vitale M, Caruso MG, Notarnicola M, Iacuzzo I, Portella G, Di Marzo V, Bifulco M (2006) Anandamide inhibits adhesion and migration of breast cancer cells. Exp Cell Res 312:363–373
Guindon J, Hohmann AG (2011) The endocannabinoid system and cancer: therapeutic implication. Br J Pharmacol 163:1447–1463
Gustafsson SB, Lindgren T, Jonsson M, Jacobsson SO (2009) Cannabinoid receptor-independent cytotoxic effects of cannabinoids in human colorectal carcinoma cells: synergism with 5-fluorouracil. Cancer Chemother Pharmacol 63:691–701
Guzman M (2003) Cannabinoids: potential anticancer agents. Nat Rev Cancer 3:745–755
Guzman M, Duarte MJ, Blazquez C, Ravina J, Rosa MC, Galve-Roperh I, Sanchez C, Velasco G, Gonzalez-Feria L (2006) A pilot clinical study of Delta9-tetrahydrocannabinol in patients with recurrent glioblastoma multiforme. Br J Cancer 95:197–203
Hart S, Fischer OM, Ullrich A (2004) Cannabinoids induce cancer cell proliferation via tumor necrosis factor alpha-converting enzyme (TACE/ADAM17)-mediated transactivation of the epidermal growth factor receptor. Cancer Res 64:1943–1950
Hegde VL, Nagarkatti M, Nagarkatti PS (2010) Cannabinoid receptor activation leads to massive mobilization of myeloid-derived suppressor cells with potent immunosuppressive properties. Eur J Immunol 40:3358–3371
Herrera B, Carracedo A, Diez-Zaera M, Gomez del Pulgar T, Guzman M, Velasco G (2006) The CB2 cannabinoid receptor signals apoptosis via ceramide-dependent activation of the mitochondrial intrinsic pathway. Exp Cell Res 312:2121–2131
Izzo AA, Aviello G, Petrosino S, Orlando P, Marsicano G, Lutz B, Borrelli F, Capasso R, Nigam S, Capasso F, Di Marzo V (2008) Increased endocannabinoid levels reduce the development of precancerous lesions in the mouse colon. J Mol Med (Berl) 86:89–98
Joosten M, Valk PJ, Jorda MA, Vankan-Berkhoudt Y, Verbakel S, van den Broek M, Beijen A, Lowenberg B, Delwel R (2002) Leukemic predisposition of pSca-1/Cb2 transgenic mice. Exp Hematol 30:142–149
Kadomatsu K (2005) The midkine family in cancer, inflammation and neural development. Nagoya J Med Sci 67:71–82
Katona I, Freund TF (2008) Endocannabinoid signaling as a synaptic circuit breaker in neurological disease. Nat Med 14:923–930
Ligresti A, Bisogno T, Matias I, De Petrocellis L, Cascio MG, Cosenza V, D’Argenio G, Scaglione G, Bifulco M, Sorrentini I, Di Marzo V (2003) Possible endocannabinoid control of colorectal cancer growth. Gastroenterology 125:677–687
Ligresti A, Moriello AS, Starowicz K, Matias I, Pisanti S, De Petrocellis L, Laezza C, Portella G, Bifulco M, Di Marzo V (2006) Antitumor activity of plant cannabinoids with emphasis on the effect of cannabidiol on human breast carcinoma. J Pharmacol Exp Ther 318:1375–1387
Liu WM, Fowler DW, Dalgleish AG (2010) Cannabis-derived substances in cancer therapy—an emerging anti-inflammatory role for the cannabinoids. Curr Clin Pharmacol 5:281–287
Lonardi S, Tosoni A, Brandes AA (2005) Adjuvant chemotherapy in the treatment of high grade gliomas. Cancer Treat Rev 31:79–89
Lorente M, Carracedo A, Torres S, Natali F, Egia A, Hernandez-Tiedra S, Salazar M, Blazquez C, Guzman M, Velasco G (2009) Amphiregulin is a factor for resistance of glioma cells to cannabinoid-induced apoptosis. Glia 57:1374–1385
Lorente M, Torres S, Salazar M, Carracedo A, Hernandez-Tiedra S, Rodriguez-Fornes F, Garcia-Taboada E, Melendez B, Mollejo M, Campos-Martin Y, Lakatosh SA, Barcia J, Guzman M, Velasco G (2011) Stimulation of the midkine/ALK axis renders glioma cells resistant to cannabinoid antitumoral action. Cell Death Differ 18:959–973
Lu T, Newton C, Perkins I, Friedman H, Klein TW (2006) Cannabinoid treatment suppresses the T-helper cell-polarizing function of mouse dendritic cells stimulated with Legionella pneumophila infection. J Pharmacol Exp Ther 319:269–276
Malfitano AM, Ciaglia E, Gangemi G, Gazzerro P, Laezza C, Bifulco M (2011) Update on the endocannabinoid system as an anticancer target. Expert Opin Ther Targets 15:297–308
Marcu JP, Christian RT, Lau D, Zielinski AJ, Horowitz MP, Lee J, Pakdel A, Allison J, Limbad C, Moore DH, Yount GL, Desprez PY, McAllister SD (2010) Cannabidiol enhances the inhibitory effects of delta9-tetrahydrocannabinol on human glioblastoma cell proliferation and survival. Mol Cancer Ther 9:180–189
Massi P, Vaccani A, Bianchessi S, Costa B, Macchi P, Parolaro D (2006) The non-psychoactive cannabidiol triggers caspase activation and oxidative stress in human glioma cells. Cell Mol Life Sci 63:2057–2066
Massi P, Valenti M, Vaccani A, Gasperi V, Perletti G, Marras E, Fezza F, Maccarrone M, Parolaro D (2008) 5-Lipoxygenase and anandamide hydrolase (FAAH) mediate the antitumor activity of cannabidiol, a non-psychoactive cannabinoid. J Neurochem 104:1091–1100
Matsuda LA, Lolait SJ, Brownstein MJ, Young AC, Bonner TI (1990) Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature 346:561–564
McAllister SD, Christian RT, Horowitz MP, Garcia A, Desprez PY (2007) Cannabidiol as a novel inhibitor of Id-1 gene expression in aggressive breast cancer cells. Mol Cancer Ther 6:2921–2927
McAllister SD, Murase R, Christian RT, Lau D, Zielinski AJ, Allison J, Almanza C, Pakdel A, Lee J, Limbad C, Liu Y, Debs RJ, Moore DH, Desprez PY (2011) Pathways mediating the effects of cannabidiol on the reduction of breast cancer cell proliferation, invasion, and metastasis. Breast Cancer Res Treat 129:37–47
McKallip RJ, Lombard C, Fisher M, Martin BR, Ryu S, Grant S, Nagarkatti PS, Nagarkatti M (2002) Targeting CB2 cannabinoid receptors as a novel therapy to treat malignant lymphoblastic disease. Blood 100:627–634
McKallip RJ, Nagarkatti M, Nagarkatti PS (2005) Delta-9-tetrahydrocannabinol enhances breast cancer growth and metastasis by suppression of the antitumor immune response. J Immunol 174:3281–3289
Mechoulam R, Ben-Shabat S, Hanus L, Ligumsky M, Kaminski NE, Schatz AR, Gopher A, Almog S, Martin BR, Compton DR, Pertweee RG, Griffine G, Bayewitchf M, Bargf J, Vogelf Z (1995) Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem Pharmacol 50:83–90
Mirkin BL, Clark S, Zheng X, Chu F, White BD, Greene M, Rebbaa A (2005) Identification of midkine as a mediator for intercellular transfer of drug resistance. Oncogene 24:4965–4974
Miyato H, Kitayama J, Yamashita H, Souma D, Asakage M, Yamada J, Nagawa H (2009) Pharmacological synergism between cannabinoids and paclitaxel in gastric cancer cell lines. J Surg Res 155:40–47
Mizushima N, Levine B, Cuervo AM, Klionsky DJ (2008) Autophagy fights disease through cellular self-digestion. Nature 451:1069–1075
Munro S, Thomas KL, Abu-Shaar M (1993) Molecular characterization of a peripheral receptor for cannabinoids. Nature 365:61–65
Nabissi M, Morelli MB, Santoni M, Santoni G (2012) Triggering of the TRPV2 channel by cannabidiol sensitizes glioblastoma cells to cytotoxic chemotherapeutic agents. Carcinogenesis 34:48–57
Newton CA, Chou PJ, Perkins I, Klein TW (2009) CB(1) and CB(2) cannabinoid receptors mediate different aspects of delta-9-tetrahydrocannabinol (THC)-induced T helper cell shift following immune activation by Legionella pneumophila infection. J Neuroimmune Pharmacol 4:92–102
Nieder C, Adam M, Molls M, Grosu AL (2006) Therapeutic options for recurrent high-grade glioma in adult patients: recent advances. Crit Rev Oncol Hematol 60:181–193
Nomura DK, Long JZ, Niessen S, Hoover HS, Ng SW, Cravatt BF (2010) Monoacylglycerol lipase regulates a fatty acid network that promotes cancer pathogenesis. Cell 140:49–61
Pacher P, Batkai S, Kunos G (2006) The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol Rev 58:389–462
Palmer RH, Vernersson E, Grabbe C, Hallberg B (2009) Anaplastic lymphoma kinase: signalling in development and disease. Biochem J 420:345–361
Pertwee RG (2008) The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br J Pharmacol 153:199–215
Pertwee RG (2009) Emerging strategies for exploiting cannabinoid receptor agonists as medicines. Br J Pharmacol 156:397–411
Pertwee RG, Howlett AC, Abood ME, Alexander SP, Di Marzo V, Elphick MR, Greasley PJ, Hansen HS, Kunos G, Mackie K, Mechoulam R, Ross RA (2010) International union of basic and clinical pharmacology. LXXIX. Cannabinoid receptors and their ligands: beyond CB1 and CB2. Pharmacol Rev 62:588–631
Pisanti S, Borselli C, Oliviero O, Laezza C, Gazzerro P, Bifulco M (2007) Antiangiogenic activity of the endocannabinoid anandamide: correlation to its tumor-suppressor efficacy. J Cell Physiol 211:495–503
Portella G, Laezza C, Laccetti P, De Petrocellis L, Di Marzo V, Bifulco M (2003) Inhibitory effects of cannabinoid CB1 receptor stimulation on tumor growth and metastatic spreading: actions on signals involved in angiogenesis and metastasis. FASEB J 17:1771–1773
Preet A, Ganju RK, Groopman JE (2008) Delta9-Tetrahydrocannabinol inhibits epithelial growth factor-induced lung cancer cell migration in vitro as well as its growth and metastasis in vivo. Oncogene 27:339–346
Purow B, Schiff D (2009) Advances in the genetics of glioblastoma: are we reaching critical mass? Nat Rev Neurol 5:419–426
Qamri Z, Preet A, Nasser MW, Bass CE, Leone G, Barsky SH, Ganju RK (2009) Synthetic cannabinoid receptor agonists inhibit tumor growth and metastasis of breast cancer. Mol Cancer Ther 8:3117–3129
Ramer R, Hinz B (2008) Inhibition of cancer cell invasion by cannabinoids via increased expression of tissue inhibitor of matrix metalloproteinases-1. J Natl Cancer Inst 100:59–69
Salazar M, Carracedo A, Salanueva IJ, Hernandez-Tiedra S, Lorente M, Egia A, Vazquez P, Blazquez C, Torres S, Garcia S, Nowak J, Fimia GM, Piacentini M, Cecconi F, Pandolfi PP, Gonzalez-Feria L, Iovanna JL, Guzman M, Boya P, Velasco G (2009) Cannabinoid action induces autophagy-mediated cell death through stimulation of ER stress in human glioma cells. J Clin Invest 119:1359–1372
Salazar M, Lorente M, Garcia-Taboada E, Hernandez-Tiedra S, Davila D, Francis SE, Guzman M, Kiss-Toth E, Velasco G (2013) The pseudokinase tribbles homologue-3 plays a crucial role in cannabinoid anticancer action. Biochim Biophys Acta 1831:1573–1578
Sanchez C, de Ceballos ML, del Pulgar TG, Rueda D, Corbacho C, Velasco G, Galve-Roperh I, Huffman JW, Ramon y Cajal S, Guzman M (2001) Inhibition of glioma growth in vivo by selective activation of the CB(2) cannabinoid receptor. Cancer Res 61:5784–5789
Sarfaraz S, Afaq F, Adhami VM, Malik A, Mukhtar H (2006) Cannabinoid receptor agonist-induced apoptosis of human prostate cancer cells LNCaP proceeds through sustained activation of ERK1/2 leading to G1 cell cycle arrest. J Biol Chem 281:39480–39491
Sarfaraz S, Adhami VM, Syed DN, Afaq F, Mukhtar H (2008) Cannabinoids for cancer treatment: progress and promise. Cancer Res 68:339–342
Shrivastava A, Kuzontkoski PM, Groopman JE, Prasad A (2011) Cannabidiol induces programmed cell death in breast cancer cells by coordinating the cross-talk between apoptosis and autophagy. Mol Cancer Ther 10:1161–1172
Soroceanu L, Murase R, Limbad C, Singer E, Allison J, Adrados I, Kawamura R, Pakdel A, Fukuyo Y, Nguyen D, Khan S, Arauz R, Yount GL, Moore DH, Desprez PY, McAllister SD (2012) Id-1 is a key transcriptional regulator of glioblastoma aggressiveness and a novel therapeutic target. Cancer Res 73:1559–1569
Steffens S, Veillard NR, Arnaud C, Pelli G, Burger F, Staub C, Karsak M, Zimmer A, Frossard JL, Mach F (2005) Low dose oral cannabinoid therapy reduces progression of atherosclerosis in mice. Nature 434:782–786
Stupp R, Pavlidis N, Jelic S (2005) ESMO minimum clinical recommendations for diagnosis, treatment and follow-up of malignant glioma. Ann Oncol 16(Suppl 1):i64–i65
Sugiura T, Kondo S, Sukagawa A, Nakane S, Shinoda A, Itoh K, Yamashita A, Waku K (1995) 2-Arachidonoylglycerol: a possible endogenous cannabinoid receptor ligand in brain. Biochem Biophys Res Commun 215:89–97
Thors L, Bergh A, Persson E, Hammarsten P, Stattin P, Egevad L, Granfors T, Fowler CJ (2010) Fatty acid amide hydrolase in prostate cancer: association with disease severity and outcome, CB1 receptor expression and regulation by IL-4. PLoS One 5, e12275
Torres S, Lorente M, Rodriguez-Fornes F, Hernandez-Tiedra S, Salazar M, Garcia-Taboada E, Barcia J, Guzman M, Velasco G (2011) A combined preclinical therapy of cannabinoids and temozolomide against glioma. Mol Cancer Ther 10:90–103
Vara D, Salazar M, Olea-Herrero N, Guzman M, Velasco G, Diaz-Laviada I (2011) Anti-tumoral action of cannabinoids on hepatocellular carcinoma: role of AMPK-dependent activation of autophagy. Cell Death Differ 18:1099–1111
Velasco G, Sanchez C, Guzman M (2012) Towards the use of cannabinoids as antitumour agents. Nat Rev Cancer 12:436–444
Verfaillie T, Salazar M, Velasco G, Agostinis P (2010) Linking ER stress to autophagy: potential implications for cancer therapy. Int J Cell Biol 2010:930509
Wang D, Wang H, Ning W, Backlund MG, Dey SK, DuBois RN (2008) Loss of cannabinoid receptor 1 accelerates intestinal tumor growth. Cancer Res 68:6468–6476
Zheng D, Bode AM, Zhao Q, Cho YY, Zhu F, Ma WY, Dong Z (2008) The cannabinoid receptors are required for ultraviolet-induced inflammation and skin cancer development. Cancer Res 68:3992–3998
Zhu LX, Sharma S, Stolina M, Gardner B, Roth MD, Tashkin DP, Dubinett SM (2000) Delta-9-tetrahydrocannabinol inhibits antitumor immunity by a CB2 receptor-mediated, cytokine-dependent pathway. J Immunol 165:373–380
Acknowledgements
Research in the groups of the authors is supported by grants from Spanish Ministry of Economy and Competitiveness (MINECO) (PI12/02248, FR2009-0052 and IT2009-0053 to GV; and PI11/00295 to CS), Comunidad de Madrid (S2011/BMD-2308 to MG), GW Pharmaceuticals (to GV, CS and MG); Fundación Mutua Madrileña (AP101042012 to GV) and Fundació Telemarató (20134031 to GV)
Potential Conflict of Interest
We declare that GW Pharmaceuticals funded part of the research of our laboratory. Likewise, part of the data obtained by the authors in relation with the antitumour action of cannabinoids is included in three patent applications presented by GW Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Velasco, G., Sánchez, C., Guzmán, M. (2015). Endocannabinoids and Cancer. In: Pertwee, R. (eds) Endocannabinoids. Handbook of Experimental Pharmacology, vol 231. Springer, Cham. https://doi.org/10.1007/978-3-319-20825-1_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-20825-1_16
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20824-4
Online ISBN: 978-3-319-20825-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)