Abstract
Several forces will progressively change the current US healthcare system. First, patient factors will likely exert the greatest impact. The rapidly growing US population, a growing percentage of seniors, increasing prevalence of chronic disease, increasing racial/ethnic diversity and persisting healthcare disparities will strain an already overloaded system. Second, healthcare system factors are also contributing to challenges. Shortages in the healthcare workforce, the rising costs, complexity and chronicity of care, the burdens of caregivers as primary health providers, the failure to address social determinants of health and the emergence of retail healthcare will exacerbate that strain. This chapter discusses implications of these forces in the context of health information systems evolving to meet these healthcare challenges. We conclude with a case study of a potential future patient-centered health information system and a discussion of patient-oriented features of effective health information systems.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Consumer health technology
- Population health
- Prevention and wellness
- On demand healthcare
- Health innovation
- Caregivers
- Chronic disease self management
- Populomics
- Telehealth
- Telemedicine
1 Changes in Patient Populations and Health Care
1.1 Introduction
A fundamental premise of this chapter is the notion that healthcare systems in the future will be very different than they are now or have been. Patients will interact with future healthcare systems in some ways that are similar to historic and current practices, but undoubtedly they will need to do so in many new ways in the future. To be useful, health information systems must be responsive to current healthcare realities, and also to new and unique interactions, tasks, behaviors and needs of patients, providers and others who will engage patients, to help them achieve their personal health goals.
The chapter starts with patient and population factors which will likely exert the largest impact on healthcare, and a look at changes in healthcare itself. This is followed by a discussion on the implications of changes on health information. These factors have the potential to change many aspects of care: access, quality, costs and patients’ experience and satisfaction with its delivery. Advances in information and computer technologies, especially remote clinical sensing, will facilitate the care of individuals to empower patients and to meet emerging healthcare challenges. New, more powerful health information systems will also shape the scope and practice of the healthcare processes they will support. The chapter closes with a case study of a potential health information system of the future, from the patient perspective.
1.2 The Changing US Healthcare Landscape
1.2.1 Changes in the Patient Population
An Increasing US Population – The US population has grown since 1950 from a base of 152 million Americans, with an additional 156 million added between 1950 and 2009 [1). Projections suggest the number of people living in the US will increase to 400–450 million people by 2050 [1, 2]. The doubling of the US population (152 million in 1950 to 308 million in 2009) has been remarkable compared with other industrialized countries. Germany and Italy, for instance, grew by only 21 % and 30 % respectively during the same period. Several other countries particularly in Eastern Europe, have actually had reductions in population [1].
An Aging US Population – Since 1950, the US population has aged, with increases in the total number of seniors (those over age 65 years) and the proportion of seniors relative to the total population. In 1950, the median age of US was 30.2 years with children under the age of 5 accounting for 10.8 %. By 2000, the median age had risen to 35.3 years while children under the age of 5 accounted for only 6.8 % [1]. By 2010 the median age increased to 37.2 years with those under the age of 5 dropped to 6.5 % [3]. On the other end of the age spectrum: in 1950, seniors represented 8.1 % of the US population, increasing to 12.8 % in 2009 and projected to reach 20.2 % by 2050. By then, one in five persons or over 88 million people will be age 65 or older. Of these, 32.5 million or approximately 7.5 % of the US population are projected to be over the age of 80 [1].
Increasing Prevalence Of Chronic Disease – In the US, chronic diseases are the leading cause of illness, morbidity and mortality, accounting for most of health-care expenditures [4]. Half (50.9 %) of all adults in the US have at least one chronic disease and over a quarter (26 %) of all adults and more than 50 % of seniors will have two or more chronic conditions [5]. In 2011, seven of the top ten causes of death in the US were chronic conditions, including (heart disease, cancer, chronic lung diseases, stroke, Alzheimer disease, diabetes, and kidney diseases). Individuals with chronic diseases need and utilize a significant amount of health care services and resources. In addition, chronic conditions puts a tremendous burden on patients, their families and employers, among patients who stay in the workforce and those who must leave it prematurely due to disability [4].
Increasing Racial and Ethnic Diversity – According the Census Bureau, the US population is becoming progressively diverse, racially and ethnically. Minorities who now comprise 37 % of the population are projected to become 57 % by 2060 [2]. The non-Hispanic white population is projected to peak by 2024, at 199.6 million, and then to decrease slowly, falling by 20.6 million during 2024–2060. The overall Hispanic population is projected to more than double to 128.8 million by 2060. By 2060, nearly one in three US residents will be of Hispanic descent, up from one in six today. The Asian population is also projected also to more than double, from 15.9 million (5.1 %) in 2012 to 34.4 million (8.2 %) in 2060. The African American population is expected to increase to 61.8 million (14.7 %) over the same time period. American Indian and Alaska Native and Hawaiian and Other Pacific Islander populations are also projected to increase substantially, but will comprise about 1.5 % each of the total population over the same time frame. The number of people who identify themselves as being of two or more races is projected to more than triple, from 7.5 million to 26.7 million over the same period [2].
The cumulative effect of these changes on the total US minority population by 2060 will result in older consumers being predominately non-Hispanic white. Younger individuals will be increasingly minority and the US will become a majority-minority nation for the first time by the year 2043. At that time, the non-Hispanic white population will still be the largest single group, but no single racial group will form a majority of the total US population [2].
Persisting Healthcare Disparities – Racial and ethnic demographic shifts are important to consider because patients and consumers from these population groups tend to have poorer health outcomes, less access to health care, lower adoption of healthy behaviors and lower exposure to health-promoting environments. For example, non-Hispanic black adults are at least 50 % more likely to die of heart disease or stroke prematurely (i.e., before age 75 years) than their non-Hispanic white counterparts [6]. The prevalence of adult diabetes is higher among Hispanics, non-Hispanic blacks, and those of other or mixed races than among Asians and non-Hispanic whites [7]. Infant mortality is more than double the rate for non-Hispanic blacks than for non-Hispanic whites [8]. Because individuals from racial and ethnically diverse populations have and continue to experience poorer access to and quality of healthcare services than their white counterparts, they are, by definition, medically underserved and disenfranchised.
Each year since 2003, the Agency for Healthcare Research and Quality (AHRQ) has reported on the status of health care disparities in the US. The National Healthcare Disparities Report (NHDR) focuses on more than 200 health care process, outcome, and access measures, covering a wide variety of conditions and settings [9]. As in previous years, the most recent report found disparities in access to and quality of care to be common across racial and ethnic populations and that most of these are not changing [9]. A few measures of disparities have changed unevenly and inconsistently, but over time, there have been no sustained improvements [9].
The reasons for the existence and persistence of health disparities are complex and thought to be related to sociocultural, socioeconomic, behavioral and environmental factors within the context of current and historical biases and prejudices found within the healthcare system and within the larger society [10]. In addition, significant levels of mistrust and challenges in cross cultural communication have been found among many racial and ethnic minority patients and their health care providers [11–14].
1.2.2 Changes in Healthcare
Shortages in Healthcare Manpower – The core of US healthcare system has been historically comprised of physicians, nurses and other professionals employed within hospitals/health centers. Studies project shortages in the numbers of US healthcare providers:
-
Demand for physicians continues to grow faster than supply. This will lead to a projected shortfall of between 46,100 and 90,400 physicians by 2025 [15].
-
Projected shortfalls in primary care will range between 12,500 and 31,100 physicians by 2025, while demand for non-primary care physicians will range between 28,200 and 63,700 physicians [15].
-
Expanded medical coverage achieved under the Affordable Care Act (ACA) once fully implemented will likely increase demand by about 16,000–17,000 physicians (2.0 %) over the increased demand resulting from changing population demographics and an aging physician workforce [15].
The greatest shortfall, percentage-wise, will be among surgical specialties (excluding obstetrics and gynecology) reflecting little projected growth in the supply of surgeons and limitations on the ability to augment staffing with other types of clinicians. While the shortfall is expected to affect everyone, it will likely be more harmful to vulnerable and underserved consumers and patients in rural or inner-city areas [16]. Some experts believe the physician shortage to be relative, a result of inadequate distribution of physicians across the country, rather than an actual overall shortage [17, 18].
Experts have also indicated that a nursing shortage exists [19]. In 2002, the shortage of registered nurses was estimated to be approximately 125,000. Primary drivers of this shortage are: an aging nursing workforce, increased demands due to population demographic shifts and expansion of government sponsored insurance. It is expected that the trend will progress over time, with a projected shortage of 400,000–808,000 RNs by 2020 [20]. Regardless of cause, whether referring to specialists, primary care providers or nurses, many patients and consumers live without adequate access to the core medical providers of our healthcare system.
Caregivers as Providers – The bulk of health care services to patients over the course of their lives is delivered by family members and friends, not healthcare professionals [21]. Nearly four out of ten adult Americans (39 %) report “providing care to an adult relative or friend”. In addition, nearly half (47 %) of adults say that they expect to be a caregiver for an aging parent or other elderly relative at some point in their lives [21].
Caregiver activities range from providing simple assistance with routine household tasks or providing emotional support to carrying out complex medical procedures. More than half of all caregivers report having to perform medical/nursing tasks for patients with multiple chronic physical and cognitive conditions. Caregiver provided medical tasks include: managing and administering multiple medications, caring for wounds, giving injections or intravenous therapy, providing incontinence support and/or care coordination [21]. Most caregivers receive little training or support from medical professionals, having to learn to perform tasks on their own, with many reporting fear about their ability to carry out tasks properly [21]. Caregiving can be stressful and time consuming, with tremendous impacts on the physical, mental, financial and social health of caregivers. As the US population continues to age, the need for caregivers will undoubtedly continue to rise [21].
Rising Healthcare Costs – US health care costs have risen, largely unabated, for more than 20 years. Projections suggest that US health care spending will surpass $10,000 per person in 2015 [22] and that national health expenditures will consume more than 20 % of the US Gross Domestic Product by 2018 [23]. At the current rate, healthcare spending threatens the integrity of the Medicare and Medicaid programs and makes health care unaffordable for those with low incomes and/or without insurance. The rising rate drives employers, particularly of smaller businesses, to reduce or discontinue providing health insurance for employees because they can no longer afford premiums [23]. To help manage costs, employers and other payers are increasingly shifting costs to employees and their families by offering modest benefit packages with out-of- pocket costs. Enhanced benefits may be possible, but only at higher costs [23].
Recognition of the Impact of Social Determinants on Health – It has been increasingly recognized that social factors play an important role in determining morbidity, mortality, disability and health outcomes [24–32]. Growing evidence suggests that medical care, while critical to health, is not the only influence. Experts suggest that the independent influence of medical care alone on mortality may in fact be as low 10–15 % in the US [33, 34], and there is increasing acceptance of the importance of social factors in health and well-being [35, 36]. It is estimated that as many as 50 % of all deaths in the US involve behavioral causes. Health-related behaviors have been shown to be strongly shaped by social factors, including income, education, employment, isolation, social support, socioeconomic status and stress [37], and the effects of any single social factor are often contingent on a host of other factors [37].
Emerging evidence suggests that social and genetic causes of disease are not mutually exclusive and that genetic endowment is not unalterable as once thought. Gene expression may occur only when impacted by social or environmental factors. In turn, physical and social environments may be impacted by social policy [37].
Retail Healthcare in America – Patients and consumers can be frustrated by poor access to care, unclear or confusing health information, long wait times for physician office appointments and overcrowded emergency departments. Utilization data indicates that patients are increasingly demanding care that meets their needs [38]. Retail clinics, commercial acute care facilities that provide services evenings and weekends in convenient locations (groceries, drugstores, general retailers, etc.) have emerged as viable sources of acute and preventive care with predictable wait times, easy access, lower costs and clear, transparent patient information [38]. Growing data shows consumers satisfaction with retail clinics. In 2011, 19 % of consumers reported using a retail clinic vs 15 % in 2010 and 13 % in 2009; 30 % of consumers said that they would use a retail clinic if it considerably reduced their wait time [38]. A recent analysis of retail clinic services found they outperformed emergency departments and ambulatory care facilities in 7 measures of quality [39].
2 Implications of Change on Health Information Systems
Changes in the US population and in healthcare will affect health information systems. Systems of the future must support the needs of a rapidly expanding population of patients, caregivers and healthcare in the face of decreasing healthcare manpower. Experience with telemedicine and tele-health suggests it will be impractical, inconvenient and unnecessary for patients to see a physician for every problem.
An aging population with chronic disease will require health information systems and other information tools to support longitudinal care of increasing complexity as patients accumulate physical and cognitive limitations caused by the co-morbidities of multiple conditions over decades. Future systems will need to aggregate clinical information and data from a wide variety of sources and process as well as interpret data and provide feedback to support patients’ adherence, education and health behavior changes.
Increasing racial and ethnic diversity of the population will require health information systems to facilitate and support socio-culturally and linguistically competent interactions between patients and providers. In addition to anticipating and supporting language, literacy, numeracy and health literacy needs, systems and providers will need to help patients make informed inferences, choices and decisions about their health to prevent and mitigate delays and errors in care or communication and enable truly informed consent.
The reduction of healthcare disparities presents special challenges to future health information systems and providers:
-
Although patient education and training are necessary and are important means of addressing healthcare disparities, their current implementation has not resulted in discernable or sustained change or reduction. Therefore, alternatives, improvements and new techniques in teaching and training patients and their caregivers are needed if these are to have any impact on disparities.
-
The assessment of social, behavioral and environmental determinants of health may require discovery and inference from new types of patient data that are currently not being collected, including those generated by patients, either actively and/or passively.
-
Emerging health information systems may not reduce disparities, and in fact, may exacerbate existing and/or introduce new disparities due to differential abilities of populations to utilize and/or benefit from them.
Understanding how health information and systems, their design, implementation and deployment can impact population health to reduce disparities is a frontier in clinical and population health informatics and healthcare services research.
Health information systems of the future must support all stakeholders that comprise patient-centered care teams. As part of supporting the functions of the Patient Centered Medical Home (PCMH), systems must support the needs and activities of informal caregivers (as an integral part of care coordination). Without recognition and support in the form of (education, training and communication with the medical team), caregivers (and the patients for whom they provide services) are vulnerable to poor outcomes due to unseen, unaddressed and undocumented needs. Rather than lowering costs, this will likely increase costs because patients will continue to use expensive services emergently (i.e., emergency departments and hospitals) and unnecessarily.
Retail healthcare can provide both competition and solutions for improving support for PCMHs. Healthcare retailers have financial incentive to encourage patients to use their facilities. In the future, retail healthcare will include the deployment of information tools for patients to augment their care and deepen patient health engagement. One possible evolution is for retail clinics to become part of the medical neighborhood of a PCMH and its health information network to make all care transparent.
2.1 Patient Centered Health Information Management
The evolution of patient-centered health information management will require EHR system interoperability with a vast array of clinical, patient and consumer oriented tools, sensors and devices. Future systems must enable providers to manage these devices and their data while providing the patient culturally and linguistically appropriate just-in-time assistance and support that fits into (rather than disrupts) patient lifestyles.
Smartphones provide new opportunities for patient-centered health information support as many patients try and use personal digital health tools. It is reported that over one million “apps” are available through Android, Google and Apple [40], with 40,000 health apps being available on the iTunes (Apple) store alone! [41]. In addition, while consumers are increasingly turning to online resources for first-line health information and support, possibly because access is easier than for providers [42]. Many patients also engage in online communities of care (i.e. Patients like me, Cure Together) that connect patients with similar illnesses and/or problems.
Consumer-targeted health information technologies [43, 44] help patients manage their own care and decisions and can be beneficial in improving health [43–45]:
-
Web-based interventions have been shown to improve depression, anxiety or stress [46].
-
Mobile messaging supports chronic disease self-management [47] with a variety of tools aimed at helping patients to control asthma [48].
-
Social media and/or video-based digital health tools also augment in-person interactions with peers and health professionals as patients navigate their conditions and search for support.
-
Social media is also challenging fundamental notions of medical research:
-
Electronic recruitment of geographically dispersed or sparse cohorts can occur quickly.
-
“Citizen science” (patient originated and conducted “studies”) conducted in online communities (Patients like me, Cure Together, Association of Cancer Online Registries, Smart Patients) may ignore traditional constraints of research: evidence-based hypotheses, theory-based intervention design, peer review and even informed consent. Many patients, caregivers and consumers view the ability to conceive and conduct these “studies”, independent of formal research communities, as empowering and able to challenge traditional research processes. “Citizen science” does not wait for the approval of the scientific community and may provide the patient’s voice in hypothesis generation.
-
The rapid growth of the use of these platforms and innovations suggests that these trends will continue for the foreseeable future and that future health information systems could benefit by incorporating these technologies into care to better engage and empower patients [49–51], and to meet the IHI “Triple Aim” of (a) improving the patient experience of care (including quality and satisfaction), (b) improving the health of populations and (c) reducing the per capita cost of health care [52].
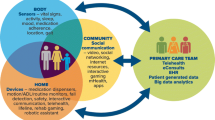
3 The Patient of the Future: Care, Self-Care and Technology
Understanding how patients, consumers, providers and organizations located in different places may work together in an integrated and coordinated fashion may be facilitated by an “ecosystem” organizational perspective. Serbanati defines a healthcare ecosystem as a collaborative, multidisciplinary and cross-organizational medical and social care delivery network, with the patient or consumer at the center. Using an Internet-based broadband infrastructure, participants share electronic information, use e-services and collaborate as needed and as directed by the patient to address health concerns [53]. Marschollek [54] refers to such systems as sensor enabled Health Information Systems, highlighting the need for such systems to support decentralized, patient-centered and personalized care while seamlessly interfacing with the many sources of information in a person’s environment.
At least three types of benefits will be realized by patients using these systems:
-
First: Patients will be in constant connection with digital sensors and tools. These tools will provide real time decision support, enhance patient engagement in health and enable them to stay in contact with the people, information and resources they need to become healthy and stay well. Patients will live in constant contact with medical, social and behavioral supports to reach their health goals. These virtual “health and care” ecosystems will be accessible by patients “on demand”, anytime, anywhere they need them. Providers will be able to manage patient-generated health data using emerging big data techniques to study the health of populations for care and research.
-
Second: Patients will benefit when data from multiple sources are integrated to yield new insights (“smart” environments). For example, it may be useful to know an asthmatic patient’s respiratory rate heart rate and blood pressure during exercise. A clinician (using an algorithmically generated display) can calculate the patient’s work of breathing. This information can enable real time predictions for the likelihood of an impending asthma attack.
-
Third: “Smart” environments will be able to respond to real-time patient sensor data and adjust to benefit the patient. To illustrate this point, imagine that our asthma patient lives in a “smart” home (a residence equipped with technology that facilitates monitoring of residents aiming to improve health, quality of life and promote independence) [55]. Mobile sensor and wireless network technologies can extend monitoring beyond the “smart” home into external activities. Such ubiquitous computing provides the basis for “ambient” assisted living technologies [55]. The “smart” home can be networked to a broader “health and care” ecosystem to become part of the patient’s personal ecosystem in which clinical algorithms detect when the patient’s work of breathing is consistent with an impending asthma attack and can assess measures of contributory factors such as temperature, medication utilization and patient activity to determine the need for an intervention such as raising the humidity of the home environment, delivering a dose of rescue medication and/or alerting an on-call nurse to the potential of an emerging asthma attack.
This “network of networks” of wireless body sensors, “smart” home, “ambient” assisted living environment and the broader “health and care” network (medical and social information, services and providers) can (using big data and cloud technologies) allow processing of immense amounts of data [56] and integration of that data from a wide variety of sources (i.e., all asthmatic patients within a geographic region) in real time [56]. Over time, these “health and care” ecosystems will be able to “learn and predict” patient behaviors, needs and outcomes, and automatically respond in ways to prevent acute events or to optimize health outcomes based on aggregated patient data.
4 Case Study: The “Interactive Remote Lifestyle Assistant” (Irla)
To illustrate these benefits, we present a case study of a hypothetical sensor- enabled health information system for supporting chronic disease management:
Ruby C.
is a 76 year old Hispanic patient with congestive heart failure (CHF). She lives alone in a semi-urban mid-western state. Her husband died of a heart attack three years ago. Their three adult children have done well for themselves, but now live in other states with their own families. For many years Ruby struggled, requiring at least 3 hospitalizations a year. Even though she was doing her best, Ruby and her children constantly lived in fear of the worst. But now, things are much better. Ruby’s new bathroom carpet automatically records her weight, just before she gets in the shower each day and the information is automatically sent to her health information system and appropriate information forwarded to her electronic medical record. As Ruby tells it:
Whenever I gain 5 pounds or more, this “magic” carpet contacts IRLA. IRLA (the Interactive Remote Lifestyle Assistant) analyzes my eating patterns over the last week. Depending on the results, IRLA will suggest simple ways I can adjust my diet or cooking. IRLA also is able to contact the local grocery store and order foods I like and need and have them delivered right to my door or make a reservation for me at the neighborhood YMCA so I can get the exercise I need. Whenever my kids want to know how I am doing, IRLA keeps track of everything and can tell them anything they want to know. Whenever I need her or just want to talk, all I have to do is turn on the TV and press this button on one of my grandson’s game boxes and there she is. We talk and chat for as short or as long as I would like, day or night! If IRLA gets real worried, she will actually call my children to let them know what is going on, set up an appointment with my doctor and arrange for my church van to pick me up and bring me home after the visit.
In addition to CHF, Ruby also has asthma. Her doctor recently gave her a new digital asthma inhaler that automatically records the temporal and geospatial context of each use then sends the data back to Ruby’s smartphone, IRLA and other connected devices within the network. IRLA automatically integrates this information with data from these data streams are then utilized by an algorithm to identify patterns highly related to an asthma exacerbation. IRLA then activates connected devices such as humidifiers, air filters and heaters in Ruby’s home to optimize her environment and decrease the likelihood of an asthma attack.
Over time IRLA “learned” that Ruby’s asthma triggers include, among other things, the spicy foods that she loves so much. Using this information, IRLA suggested flavorful recipes and foods that Ruby could cook, without the spicy ingredients that lead to asthma attacks, based on what was already in her refrigerator and kitchen cabinets. In addition, IRLA noticed that Ruby usually ate out at a restaurant once a month, usually between the 1st and 5th of the month. Using this information, IRLA provided Ruby, on the last week of each month, with local restaurant and menu suggestions that avoided the spicy foods that often triggered her asthma attacks.
In this example, IRLA is the convenient, culturally and linguistically appropriate and competent, patient-facing interface to a sensor enabled health information system. IRLA is managed by Ruby’s providers but under her control. IRLA is more than a database that collects and transmits data. IRLA relys on data from Ruby’s total environment:
-
Ruby’s medical history, encoded in her electronic health record
-
Data from multiple sensors and sources including:
-
Weight scale in the Bluetooth-enabled bathroom mat that wirelessly and automatically transmits weight data to a “cloud” repository
-
Radio frequency identification (RFID) tags embedded in food labels and bottle caps of the food items she buys to help monitor sodium and nutritional intake
-
Continuously indoor and outdoor atmospheric pollution sensors
-
Humidity and temperature sensors
-
Local traffic conditions (for diesel exhaust fumes) and weather patterns
-
Direct input from Ruby
-
Information from her internist
-
The Bluetooth enabled peak flow meter attached to her asthma inhaler to monitor potential airway obstruction
-
Ruby’s activity and appointment calendar and diet tracker
-
Food databases from her favorite restaurant and grocer
-
IRLA helps coordinate Ruby’s health and social care activities and provides culturally appropriate behavioral feedback to motivate long term behavior change. With data streams from Ruby’s ecosystem of devices and doctor, IRLA can then use machine learning and artificial intelligence, initiate certain actions autonomously and automatically record these actions in Ruby’s electronic health record for viewing by caregivers to whom Ruby has granted access (her physician, her pastor and her adult children).
Prior to IRLA, Ruby and her children always worried about keeping up with everything the doctor told them the last time they saw him. It was difficult because he always had to rush and the paperwork was always confusing. IRLA simplifies the paperwork Ruby receives from her doctor and provides verbal reinforcement to help Ruby to become and stay healthy. Ruby’s children no longer worry about not knowing what is going on because they can obtain understandable online summaries of her activities, eating patterns or doctor’s instructions at any time without having to take off valuable time from work and loose income.
Finally, IRLA provides Ruby with suggestions and regular behavioral feedback. Timely practical feedback and instruction is a powerful form of reinforcement based on the data from recent patient actions. Regular behavior feedback has been shown to be critical to initiating and sustaining behavior change and has been found to be a key component of successful consumer health informatics tools. This form of teaching has its roots in so-called “edutainment” and “health gaming”. Time and rigorous evaluation will be needed to determine the superiority of these approaches to traditional methods (which have not worked).
5 Conclusions
As healthcare systems evolve, so too must health information systems and tools to meet the changing needs of patients and healthcare systems. The story of IRLA is hypothetical but the described technologies are currently possible or being developed. Their implementation into publicly or commercially available connected health information ecosystems is only a matter of time as industry and federal efforts are underway to lay the foundation for realizing these possibilities.
Health information systems of the future must provide much more than just a mechanism for health information exchange with a provider or health system. Robust health information systems of the future will likely share the following characteristics:
-
Systems will consist of distributed networked devices, tools, sensors and technologies, working together to provide alignment of decision support, behavioral motivation, education and health task support, while maintaining awareness of patient activity, response and needs. They will need to automate pre-programmable tasks where and when possible within patient home environments, in response to real time aggregated data.
-
Systems must be interoperable with any patient’s health information ecosystem. They will need to receive and share data with a variety of clinical and nonclinical sources (including patient generated health data), based on patient preferences, information needs and tools (apps, consumer devices, fitness trackers and other emerging technology), in human accessible/readable forms.
-
Systems must put patients at the center of care. They must:
-
Integrate and incorporate tele-health and remote technologies to make healthcare accessible, usable and convenient for patients
-
They must facilitate communication and other interactions among all stakeholders in a patient’s care
-
They must summarize data and present it in forms that meet the literacy, numeracy and health literacy needs of patients at all levels in a culturally acceptable fashion.
-
It is challenging to conceive how healthcare services will be delivered to meet the needs of all Americans, but the evolving US patient population will require evolving ways of managing health information. Networked, sensor-enhanced, patient-centered health information systems hold great promise to facilitate this evolution, to empower patients and to make the work of providers care teams and families more efficient, more cost-effective and more responsive to patient needs to help the nation achieve its national health goals.
References
Shrestha LB, Heisler EJ. The changing demographic profile of the United States. Washington, DC: Congressional Research Service; 2011. Report No.: 7-5700.
U.S.Census Bureau. Projections show a slower growing, older, more diverse nation a half century from now. https://www.census.gov/newsroom/releases/archives/population/cb12-243.html. 2012.
Howden LM, Meyer JA. Age and sex composition 2010: 2010 Census brief # C2010BR-03. https://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf. 2011.
Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384(9937):45–52.
Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis. 2013;10, E65.
Gillespie CD, Wigington C, Hong Y. Coronary heart disease and stroke deaths – United States, 2009. MMWR Surveill Summ. 2013;62 Suppl 3:157–60.
Beckles GL, Chou CF. Diabetes – United States, 2006 and 2010. MMWR Surveill Summ. 2013;62 Suppl 3:99–104.
MacDorman MF, Mathews TJ. Infant deaths – United States, 2005–2008. MMWR Surveill Summ. 2013;62 Suppl 3:171–5.
Agency for Healthcare Research and Quality. National healthcare disparities report 2013. Washington, DC: AHRQ; 2014.
Institute of Medicine. Unequal treatment: understanding racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2002.
Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118(4):358–65.
Casagrande SS, Gary TL, LaVeist TA, Gaskin DJ, Cooper LA. Perceived discrimination and adherence to medical care in a racially integrated community. J Gen Intern Med. 2007;22(3):389–95.
LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009;44(6):2093–105.
LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57 Suppl 1:146–61.
Dall T, West T, Chakrabarti R, Iacobucci W. The complexities of physician supply and demand: projections from 2013 to 2025. Washington, DC: IHS; 2015.
Association of American Medical Colleges. Physician shortages to worsen without increases in residency training. https://www.aamc.org/download/153160/data/physician_shortages_to_worsen_without_increases_in_residency_tr.pdf. 2010.
Council on Graduate Medical Education. Physician distribution and health care challenges in rural and inner-city areas. Washington, DC: HRSA; 1998. Report No.: 10th.
Petterson SM, Liaw WR, Phillips Jr RL, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010–2025. Ann Fam Med. 2012;10(6):503–9.
Goodin HJ. The nursing shortage in the United States of America: an integrative review of the literature. J Adv Nurs. 2003;43(4):335–50.
Keenan P. The nursing workforce shortage: causes, consequences, proposed solutions. The Commonwealth Fund; Report No.: Issue Brief #619. 2003.
Adler R, Mehta R. Catalyzing technology to support family caregiving. Washington, DC: National Alliane for Caregiving; 2014.
Centers for Medicare & Medicaid Services. National health expenditure fact sheet. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet.html. 2014.
Battani J, Zywiak W. US healthcare in the year 2015. Falls Church: Computer Sciences Corporation; 2015.
Ferrie JE, Shipley MJ, Davey SG, Stansfeld SA, Marmot MG. Change in health inequalities among British civil servants: the Whitehall II study. J Epidemiol Community Health. 2002;56(12):922–6.
Marmot M. Income inequality, social environment, and inequalities in health. J Policy Anal Manage. 2001;20(1):156–9.
Marmot MG, Smith GD, Stansfeld S, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337(8754):1387–93.
Kawachi I, Kennedy BP, Wilkinson RG. Crime: social disorganization and relative deprivation. Soc Sci Med. 1999;48(6):719–31.
Pickett KE, Wilkinson RG. Income inequality and health: a causal review. Soc Sci Med. 2015;128:316–26.
Wilkinson RG, Pickett KE. Income inequality and population health: a review and explanation of the evidence. Soc Sci Med. 2006;62(7):1768–84.
Wilkinson RG. Income inequality and population health. Soc Sci Med. 1998;47(3):411–2.
Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–98.
Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010;51(Suppl):S15–27.
McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207–12.
McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood). 2002;21(2):78–93.
Mackenbach JP. The contribution of medical care to mortality decline: McKeown revisited. J Clin Epidemiol. 1996;49(11):1207–13.
Mackenbach JP, Stronks K, Kunst AE. The contribution of medical care to inequalities in health: differences between socio-economic groups in decline of mortality from conditions amenable to medical intervention. Soc Sci Med. 1989;29(3):369–76.
Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129 Suppl 2:19–31.
Kaissi A, Charland T. The evolution of retail clinics in the United States, 2006–2012. Health Care Manag (Frederick). 2013;32(4):336–42.
Shrank WH, Krumme AA, Tong AY, et al. Quality of care at retail clinics for 3 common conditions. Am J Manag Care. 2014;20(10):794–801.
Freierman S. One million apps and counting at a fast pace. New York Times. 2011 Dec 12 pB3.
Aitken M, Gauntlet C. Patient apps for improved healthcare: from novelty to mainstream. Parsippany: IMS Institute for Healthcare Informatics; 2013.
Cybercitizen Health v8.0. New York: Manhattan Research; 2008.
Gibbons MC. Personal health and consumer informatics. The impact of health oriented social media applications on health outcomes. Yearb Med Inform. 2013;8(1):159–61.
Gibbons MC, Wilson RF, Samal L, et al. Impact of consumer health informatics applications. Evid Rep Technol Assess (Full Rep). 2009;(188):1–546. AHRQ Publication No. 09(10)-E019
Gibbons MC, Wilson RF, Samal L, et al. Consumer health informatics: results of a systematic evidence review and evidence based recommendations. Transl Behav Med. 2011;1(1):72–82.
Davies EB, Morriss R, Glazebrook C. Computer-delivered and web-based interventions to improve depression, anxiety, and psychological well-being of university students: a systematic review and meta-analysis. J Med Internet Res. 2014;16(5), e130.
de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev 2012;(12):CD007459.
Morrison D, Wyke S, Agur K, et al. Digital asthma self-management interventions: a systematic review. J Med Internet Res. 2014;16(2), e51.
Househ M, Borycki E, Kushniruk A. Empowering patients through social media: the benefits and challenges. Health Informatics J. 2014;20(1):50–8.
Winbush GB, McDougle L, Labranche L, Khan S, Tolliver S. Health empowerment technologies (HET): building a web-based tool to empower older African American patient-doctor relationships. J Health Care Poor Underserved. 2013;24(4 Suppl):106–17.
Calvillo J, Roman I, Roa LM. How technology is empowering patients? A literature review. Health Expect. 2013. doi:10.1111/hex.12089.
Dahl D, Reisetter JA, Zismann N. People, technology, and process meet the triple aim. Nurs Adm Q. 2014;38(1):13–21.
Serbanati LD, Ricci FL, Mercurio G, Vasilateanu A. Steps towards a digital health ecosystem. J Biomed Inform. 2011;44(4):621–36.
Marschollek M. Recent progress in sensor-enhanced health information systems - slowly but sustainably. Inform Health Soc Care. 2009;34(4):225–30.
Demiris G, Thompson H. Smart homes and ambient assisted living applications: from data to knowledge-empowering or overwhelming older adults? Contribution of the IMIA Smart Homes and Ambiant Assisted Living Working Group. Yearb Med Inform. 2011;6(1):51–7.
Bryant R, Katz RH, Lazowska ED. Big data computing: creating revolutionary breakthroughs in commerce, Science and Society. Washington, DC: Computing Research Association; 2008.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Gibbons, M.C., Shaikh, Y. (2016). The Patient of the Future: Participatory Medicine and Enabling Technologies. In: Weaver, C., Ball, M., Kim, G., Kiel, J. (eds) Healthcare Information Management Systems. Health Informatics. Springer, Cham. https://doi.org/10.1007/978-3-319-20765-0_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-20765-0_17
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20764-3
Online ISBN: 978-3-319-20765-0
eBook Packages: MedicineMedicine (R0)