Abstract
Patients’ acceptance of their dentures and their satisfaction are affected by esthetic factor. The appearance of the metal clasps in the esthetic zone can be objectionable for many patients. To overcome the esthetic problem, different solutions have been presented in the literature. The use of precision attachments, double-crown systems, and implants in removable partial dentures (described in part IV) can be esthetic treatment options, but these options require tooth preparation to fabricate crown restoration and a surgical operation. As a result, the increased cost is inevitable. Different metal clasp designs presented in Chap. 11 can also be esthetic alternatives in removable partial dentures. In this chapter, widely accepted and used other treatment alternatives, which are thermoplastic resins for nonmetal clasp dentures and rotational path removable partial denture design, are described. The advantages, disadvantages, and the basic principles in clinical usage are presented.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Esthetic
- Nonmetal clasp
- Nonmetal clasp denture
- Thermoplastic resin
- Rotational path
- Removable denture
- Removable partial denture
- Denture design
- RPD
- Rotational path RPD
1 Definitions
- Thermoplastic :
-
A characteristic or property of a material that allows it to be softened by the application of heat and return to the hardened state on cooling.
- Resin :
-
1: Any of various solid or semisolid amorphous natural organic substances that usually are transparent or translucent and brown to yellow; usually formed in plant secretions; are soluble in organic solvents but not in water; are used chiefly in varnishes, inks, plastics, and medicine; and are found in many dental impression materials 2: a broad term used to describe natural or synthetic substances that form plastic materials after polymerization. They are named according to their chemical composition, physical structure, and means for activation of polymerization.
- Nonmetal clasp dentures (NMCDs):
-
It is used to refer not only to dentures that do not contain any metal elements but also to dentures that incorporate a metal rest or framework and is defined as “the general name for removable partial dentures (RPDs) using denture base resins as the denture retentive parts.”
- Rotational path removable partial denture (rotational path RPD):
-
A partial removable dental prosthesis that incorporates a curved, arcuate, or variable path of placement allowing one or more of the rigid components of the framework to gain access to and engage an undercut area.
Patients’ acceptance of their dentures and their satisfaction are affected by aesthetic factors. The appearance of the metal clasps in the aesthetic zone can be objectionable for many patients. To overcome the aesthetic problem, different solutions have been presented in the literature. The use of precision attachments, double-crown systems, and implants in removable partial dentures (described in part IV) can be aesthetic treatment options, but these options require tooth preparation to fabricate crown restoration and a surgical operation. As a result, the increased cost is inevitable. Different metal clasp designs presented in Chap. 11 can also be aesthetic alternatives in removable partial dentures. In this chapter, widely accepted and used other treatment alternatives, which are thermoplastic resins for nonmetal clasp dentures and rotational path removable partial denture design, are described. The advantages, disadvantages, and the basic principles in clinical usage are presented.
2 Nonmetal Clasp Dentures
Thermoplastic resins are used for nonmetal clasp dentures (NMCDs). They can be used both as a denture base material (such as polyamides, polyesters, polycarbonates, polypropylenes, polyacetal resin) and as a preformed clasp (such as polyetheretherketon, polyetherketonketon, polyoxymethylene/acetal resin) for the fabrication of NMCDs. Although there are no sufficient studies related to the physical properties and clinical follow-up of all the thermoplastic materials, they are used in dental practice. Therefore, their mechanical and physical properties, as well as their clinical usage, maintenance, and complications, will be described in the light of the studies carried out up to now. Also manufacturer brands will be mentioned when presenting study results.
It should be kept in mind that the following advantages and disadvantages may vary according to material selection.
General advantages of nonmetal clasp dentures and thermoplastic resin materials
-
1.
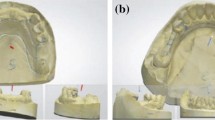
Aesthetic appearance of NMCDs is more satisfactory than the metal clasp dentures (Fig. 12.1a, b).
-
2.
Wearing and fitting of NMCDs with thermoplastic base can be more suitable for patients due to the flexibility and softer surface of thermoplastic resins compared to acrylic resins.
-
3.
Thermoplastic resins can be used in patients who have an allergy to metal.
-
4.
Thermoplastic resins have hygienic advantages due to their low water absorption and solubility.
-
5.
Thermoplastic resins contain very little or almost no free monomer.
-
6.
Creep resistance and fatigue endurance of thermoplastic materials are very high, and they are also resistant to wear and solvent materials.
-
7.
Although the flexural strength and modulus of elasticity (ME) were relatively low in the thermoplastic resins, they demonstrated great toughness and strong resistance to fracture. Their flexibility can be enhanced by adding elastomeric resins. They can be also reinforced by adding glass filler or fibers.
General disadvantages of nonmetal clasp dentures
-
1.
Thermoplastic materials need special attention because they are affected by heat generation during polishing. If the glass transition temperature is exceeded, the structure may become rubbery.
It was shown that a polyamide denture base becomes more than 7 times smoother and a processed polymethylmethacrylate becomes more than 20 times smoother when they are polished with the same conventional polishing technique.
-
2.
The polished surface of the thermoplastic resins may lose their brightness over time because they are softer than acrylic resin and more easily damaged by the scratch test. Therefore, NMCDs should be brushed with soft materials and checked at short-term intervals. Discoloration and degradation of thermoplastic resin may also be observed. Although thermoplastic resins need more care in terms of oral hygiene, in patients with good oral hygiene, candida growth will not be a problem.
-
3.
It is difficult to adjust and repair NMCDs because generally they do not adhere to the self-cure acrylic resin. It should be remembered that distal extension NMCDs should have maximum tissue support. An altered cast impression technique (see Chap. 8) can improve support in distal extension NMCDs and delay relining requirement.
-
4.
If the resin clasp is in the form of extending a part of the thermoplastic denture base resin, it covers the cervical area of the abutment teeth. This design may lead to periodontal problems. Additionally, the thickness of the preformed clasps may cause the same problems. Therefore, careful cleaning is very important.
It can be easily understood from the abovementioned disadvantages that thermoplastic resin materials have different limitations and their properties need to be modified. More clinical studies are needed for their improved usage.
2.1 The Basic Principles for Clinical Use of Nonmetal Clasp Dentures with Different Thermoplastic Materials
The basic requirement of a major connector is rigidity. NMCDs which do not include a metal structure lead to traumatic damage to the periodontal tissue of the abutment teeth and impingement of the underlying tissue due to their flexibility. NMCDs with a metal framework are rigid. Therefore, NMCDs including a metal structure with metal rest are recommended to avoid sinking and flexion of the denture base, and they can be used for all patients whose priority is aesthetics. It is very important to remember that the NMCDs should follow the same design principles as conventional RPDs with metal clasps (Fig. 12.2a, b).
However, nonmetal clasp dentures that do not include a metal structure can be a treatment option in patients with metal allergy and in patients with few missing anterior teeth or few missing teeth with occlusal support. Additionally, they can be used as epithesis for patients for whom the dentures carry no functional burden and for patients who do not consent to the preparation of their abutment teeth even for rest seats and, for implant patients, as an interim denture.
As mentioned above, thermoplastic resin clasps can be fabricated in two ways. The design criteria of thermoplastic resin retainers depend on the ME of the resin. As the ME of the material increases, rigidity also increases. Hence, the material with the lower modulus of elasticity will be more flexible and can be used in the deeper undercut (e.g., polyamides have lower ME than polyoxymethylenes).
In the first design, the resin clasp is in the form of extending a part of the thermoplastic denture base resin, and in the second design, a preformed resin clasp is used with a polymethylmethacrylate denture base material.
Polyoxymethylene (acetal resin) is the most commonly used preformed clasp material in dentistry. It is also used as a base material for patients with an allergic reaction to chrome-cobalt framework because it is monomer free. Although manufacturers suggest the use of this material without a metal framework, a metal framework offers better rigidity as can be seen with other thermoplastic materials.
This material is very strong and resists wear and fracture. It also exhibits high creep resistance and high fatigue endurance. It has clinically acceptable discoloration values. It is also reported that the water sorption and the solubility of acetal resins were within ISO specification limits, and an acetal resin showed clinically acceptable color changes for peroxide cleanser but unacceptable for hypochlorite cleanser.
It is more flexible but has a lower retentive force when compared to the chrome-cobalt clasp. Thus, it should be placed in deeper undercuts (approximately 0.5 mm) on abutments rather than chrome-cobalt. It has been recommended that an acetal resin clasp should be fabricated shorter with a larger cross-sectional diameter in order to have a stiffness similar to a cast chrome-cobalt clasp (if all other variables are equal, an acetal resin clasp should be 5 mm long and 1.4 mm in diameter, instead of 15 mm long and 1 mm in diameter chrome-cobalt clasp – Dental D). A study result showed that a 1 kg force was required to dislodge Dental D clasp’s tips by 0.5 mm, using its dimensions according to the manufacturer recommendation (length 12 mm, thickness 1.9 mm tapering to 1.25 mm at the tip, width 2.8 mm tapering to 2.2 mm at the tip).
If plaque control is established, a thicker clasp will not be harmful to oral health. It is also recommended to benefit from guiding planes in order to provide more retention. Retention will also be affected by the number of clasps, the fit of the framework, and the depth of undercut (Fig. 12.3).
Acetal resin does not have natural translucency but is available in various color shades. It can be fabricated in the same shape as a metal clasp without covering the gingiva. A metal framework is fabricated in a conventional manner. After intraoral try-in of the framework, the jaw relations are recorded. In laboratory procedures, a wax pattern of an acetal resin clasp is manufactured and an injection carried out and shaped in the metal framework’s mesh. Thus, it is possible to check the retention and color harmony of acetal resin clasps during the aesthetic try-in (Fig. 12.4).
Polyetheretherketon and polyetherketonketon have also been used as a material for clasp fabrication in the same manner as polyoxymethylene. It was found that all three thermoplastic resin clasps (Bio XS, PEEKtone A, Acetal Dental) showed their greatest retentive force at 1.5 mm thickness with a 0.50 mm undercut and provided adequate retention for RPDs even after 10 years of simulated use. It was concluded that the retention of adequately designed resin clasps might be sufficient for clinical use.
Although a clinical study showed that the acetal resin clasps were superior to chrome-cobalt clasps as they produced fewer reductions in bone height and in bone density around the abutment teeth, it should be noted that more randomized clinical studies are needed.
Thermoplastic polyamides, commonly known as nylon/flexible dentures, have also become widely used in dentistry. Although there are not enough studies of all brands, it is shown that the characteristics of polyamides differ from brand to brand. The most noteworthy and clinically important additional differences from the abovementioned advantages and disadvantages based on some studies are as follows for commonly used materials: Valplast’s and Deflex’s colors harmonize well with the color shades of the gums (Fig. 12.5a–c). Valplast can be disinfected with glutaraldehyde or sodium hypochlorite without changing its surface roughness. But a study showed that all three sodium perborate-containing denture cleansers (Corega, Protefix, Valclean) increased surface roughness of the polyamide materials (Valplast, Deflex). Color changes (Valplast) can occur with some foods and beverages such as curry, coffee, and wine. A study result showed that Deflex also has displayed more color changes when compared to polymethylmethacrylate and tea was the most effective beverage on color changes for all base materials. As Valplast does not bond to acrylic resins, treating the surface with 4-META/MMA-TBB resin after sandblasting has been recommended.
Polishing and grinding are easier for Lucitone FRS because it is harder than Valplast and highly resistant to abrasion. But the risk of fracture, color instability, and the difficulty of relining and repairing are considered disadvantages. It should be noted that the preparation of appropriate retention holes for artificial teeth is very important for the two of them. Ultimate is a new material about which there is little information. Relining and repairing can be fabricated by reinjection of the material, and it can also be used for the relining and repairing of the Lucitone FRS.
Polyesters (EstheShot, EstheShot Bright) are thermoplastic base materials which are relatively new. They have lower resilience and better fitting than polyamides and polycarbonates. Unlike polyamides, repairing is possible with self-curing resin. Alkaline denture cleaners may lead to degradation on the surface of the polyesters.
Reigning which is polycarbonate has similar physical properties to polyesters but lower water absorbency. Denture cleaners do not affect the material. Relining with self-curing resins may result in peeling. It can be reinjected to repair the broken clasp, and also repairs can be done with special repair materials. Another polycarbonate material Reigning N’s surface is harder than polyamides and polyesters. Discoloration is less than other resins. It bonds to self-cure resin. There are artificial teeth made of the same material which therefore do not need special retention for both materials.
The retentive forces of all thermoplastic resin clasps depended on the different factors such as ME, thickness, and the width of the resin and the amount of the undercut. If a thermoplastic clasp is fabricated as an extending part of the denture base, the recommended width of the retentive arm is approximately 5.0–6.0 mm and the thickness of the clasp arm is 1.0 mm (Fig. 12.6a, b). Thus, in clinically short crowns with inadequate sulcus depth and/or an excessive undercut in the tissue part, the width of the retentive arm may not be properly designed. In the case of missing molars, a study indicated that if there is presence of a 0.75 mm undercut on the second premolar, a polyamide resin clasp covering only the buccal surface is desirable, but in the presence of a 0.50 mm undercut, a resin clasp should also be extended to the buccal surface of the first premolar (Fig. 12.7). As a deeper undercut was found more effective than that of a design covering the anterior abutment tooth, it is also necessary to use lingual and proximal undercuts to increase retention. However, it should be kept in mind that further studies on the design of the resin clasps are still needed.
In clinical steps, the metal framework is fabricated. Jaw relations are recorded. Artificial teeth are arranged. After completing the aesthetic try-in, the denture is forwarded to the laboratory. The denture base, including the clasps, is manufactured with thermoplastic resin.
In light of the above data, it is clear that the dentist should have detailed information about the material before its clinical application.
3 Rotational Path Removable Partial Dentures
It is possible to eliminate the clasps in the aesthetic zone by using the rotational path of placement (Fig. 12.8). Additionally, in the presence of severely tilted teeth, the placement of the RPD is possible by using the rotational path design. A straight path of placement is used in the conventional design. But in the rotational path design, one portion of the framework is seated first, and later the other portion of the framework is seated (Fig. 12.9). Retention is obtained from the proximal undercuts adjacent to the edentulous spaces. Rigid retentive units consist of a rest and a minor connector. The retentive minor connector is frequently formed with a gingival extension on the teeth.
Placement of a rotational path RPD is different from a conventional RPD. While straight path of placement is used in conventional RPDs, rotational path RPD’s one portion is placed first, and later the other portion is placed. Path of placement shows differences according to the rotational centers (Video 12.1)
The primary indication of the rotational path design is for tooth-bounded partially edentulous arches. Namely, applying this design is more suitable for Kennedy Class III and IV cases. Although one clinical study that evaluated Kennedy Class III and II (without anterior modification) case results revealed that the rigid retainers demonstrated support, stability, retention, adequate encirclement, and passivity at the end of 10 years or more follow-up, further clinical studies are still needed in order to expand the indications for this design.
Advantages of the rotational path RPD design
-
1.
The clasps can be eliminated in the aesthetic zone.
-
2.
Plaque accumulation may be decreased by reducing tooth coverage.
-
3.
Preparation on the abutment teeth is minimally invasive.
-
4.
Facial or lingual undercuts are not necessary for retention.
-
5.
Further tipping of the abutment tooth can be prevented by a rigid retainer.
Disadvantages of the rotational path RPD design
-
1.
Fabrication and adjustment may be more difficult when compared to conventional design because technicians are less familiar with this design and processing errors are less tolerable.
-
2.
The well-prepared rest seat preparation is vital.
There are two categories of rotational path designs. In category I design, the rotational centers of the framework are located at the ends of the rests of the rigid retainers. The rotational centers are seated first, and then the entire prosthesis is placed to its final position. Depending on aesthetic and periodontal considerations, the anterior or posterior portion of the RPD is placed first. Elimination of either anterior or posterior clasps with this design is possible. If the anterior portion of the prosthesis is placed first, the path of placement is termed anteroposterior, and generally it is used to eliminate the anterior clasp (Fig. 12.10a, b). If the posterior portion is placed first, the path is termed posteroanterior, and generally it is used to eliminate the posterior clasp (Fig. 12.11a, b). When molar abutments are tipped mesially, this design offers a great advantage (Fig. 12.12).
In category II designs, rotational centers are placed gingivally as rigid extensions of the minor connectors and are primarily used to replace the anterior teeth with the elimination of anterior clasps (Fig. 12.13). This category includes all lateral paths.
Rests in the rotational path design show small differences from conventional design. In molars, rest seats should be prepared 1.5–2 mm deep occlusogingivally with nearly parallel buccal and lingual walls on the molar abutments. Rest seat preparation should be extended to more than half the mesiodistal width of the occlusal surface to provide bracing and vertical distribution of the forces to the abutment teeth and to prevent tooth migration. Preparation of the irregular outline form also prevents migration (Fig. 12.14). If molars are also tipped lingually, their rest seat walls should be prepared parallel to each other.
A cingulum rest seat on the anterior teeth should be prepared. When suitable cingulum does not exist, it can be provided by acid-etched composite resin or fabricating a crown restoration. The outline form of the preparation should be an inverted “U” or “V” and extended to more than one half the mesiodistal width of the anterior tooth.
Conventional clasping and rest can be used wherever necessary in all designs.
Regardless of the design category, rigid retainers should be passive during and after seating of the framework, and therefore they do not require reciprocation.
It is important to remember that the lingual bar design causes fewer problems when establishing a rotational path of insertion in the mandible. The lingual plate is more likely to cause interferences as the surface covered is much greater. So if possible a lingual bar should be preferred over a lingual plate.
Steps of clinical and surveying procedures
-
1.
The patient’s acceptance and coordination are assessed. Intraoral evaluation is performed to determine whether a rotational path design is possible or the presence of proximal undercuts, the location and number of edentulous areas, and the arch form. Occlusal relationships are evaluated both clinically and on the mounted casts. Then the study casts are investigated in terms of adequate undercuts when the cast is surveyed with a zero-degree tilt. Rest and retentive areas are also investigated. The amount of undercut should be approximately 0.5 mm in the retentive area. Although guiding plates are not usually recommended for this design, recontouring in the required areas is performed to minimize the amount of relief.
-
2.
Rest seat preparation is performed. If there is no proper cingulum to prepare the rest seat and/or adequate undercut, crown or bonded composite resin restorations can be provided. Composite restorations are generally recommended in completing rest seats to improve contours and to alleviate the patient’s financial constraints.
After the final impression, the cast is surveyed again. The heights of the contours are drawn at two different positions (at the zero-degree and tilted positions) (Fig. 12.15a–c). Retentive areas and undercuts are indicated on the cast. The analyzing rod is utilized to assess whether access exists for the rests to be seated. If not, extra preparation is required which eventually needs a new impression.
-
3.
An acrylic prototype resembling the metal framework may be helpful to check the rotational path of insertion. Thus, any obstacles detected during try-in can be handled before casting.
-
4.
During the adjustment of the metal framework, care should be given to preserve the surface of minor connectors that are facing the abutment teeth and act as rigid retainers. If necessary, these surfaces should be adjusted chairside by the dentist (Fig. 12.16a, b). However, any interference with the framework regarding the rotational path of insertion has to be eliminated during laboratory finishing.
-
5.
In order to determine the shape and amount of blockout under the minor connector and whether there is adequate undercut for the rigid retentive component, a pair of compasses can be used (Fig. 12.17).The free arm tip of the compass is used to evaluate the undercut area during motion around the other arm tip which is fixed at the rotation axis. If multiple edentulous areas exist, a sufficient blockout of undesirable undercuts should be planned for all minor connectors.
Bibliography
Arda T, Arıkan A. An in vitro comparison of retentive force and deformation of acetal resin and cobalt-chromium clasps. J Prosthet Dent. 2005;94:267–74.
Arikan A, Kulak Ozkan Y, Arda T, Akalın B. Effect of 180 days of water storage on the transverse strength of acetal resin denture base material. J Prosthodont. 2010;19:47–51.
Arikan A, Ozkan YK, Arda T, Akalın B. An in vitro investigation of water sorption and solubility of two acetal denture base materials. Eur J Prosthodont Restor Dent. 2005;13:119–22.
Aysan I, Uçar Y, Usumez A. A comparison of the color stability of three different base materials in the different solutions. J Dent Fac Atatürk Uni. 2011;21:219–25.
Baharav H, Ben-Ur Z, Laufer BZ, Cardash HS. Removable partial denture with a lateral rotational path of insertion. Quintessence Int. 1995;26:531–3.
Carreiro Ada F, Machado AL, Giampaolo ET, Santana IL, Vergani CE. Dual path: a concept to improve the esthetic replacement of missing anterior teeth with a removable partial denture. J Prosthodont. 2008;17:586–90.
Chow TW, Clark RKF, Clarke DA. Improved designs for removable partial dentures in Kennedy Class IV cases. Quintessence Int. 1988;19:797–800.
Donovan T. Use of the rotational path removable partial denture concept in a Kennedy Class II Patient: a case report. J Esthet Restor Dent. 2008;20:294–9.
Durkan R, Ayaz EA, Bagis B, Gurbuz A, Ozturk N, Korkmaz FM. Comparative effects of denture cleansers on physical properties of polyamide and polymethyl methacrylate base polymers. Dent Mater J. 2013;32:367–75.
Firtell DN, Jacobson TE. Removable partial dentures with rotational paths of insertion: problem analysis. J Prosthet Dent. 1983;50:8–15.
Fitton JS, Davies EH, Howlett JA, Pearson GJ. The physical properties of a polyacetal denture resin. Clin Mater. 1994;17:125–9.
Fueki K, Ohkubo C, Yatabe M, Arakawa I, Arita M, Ino S, Kanamori T, Kawai Y, Kawara M, Komiyama O, Suzuki T, Nagata K, Hosoki M, Masumi S, Yamauchi M, Aita H, Ono T, Kondo H, Tamaki K, Matsuka Y, Tsukasaki H, Fujisawa M, Baba K, Koyano K, Yatani H. Clinical application of removable partial dentures using thermoplastic resin-Part I: definition and indication of non-metal clasp dentures. J Prosthodont Res. 2014;58:3–10.
Ito M, Wee AG, Miyamoto T, Kawai Y. The combination of a nylon and traditional partial removable dental prosthesis for improved esthetics: a clinical report. J Prosthet Dent. 2013;109:5–8.
Jacobson TE. Rotational path partial denture design: a 10-year clinical follow –up-Part I. J Prosthet Dent. 1994a;71:271–7.
Jacobson TE. Rotational path partial denture design: a 10-year clinical follow-up – Part II. J Prosthet Dent. 1994b;71:278–82.
Kawara M, Iwata Y, Iwasaki M, Komoda Y, Iida T, Asano T, Komiyama O. Scratch test of thermoplastic denture base resins for non-metal clasp dentures. J Prosthodont Res. 2014;58:35–40.
Kim MH, Heo SJ, Kim SK, Koak JY. Full mouth rehabilitation of destroyed dentition with rotational path removable partial denture: a case report. J Adv Prosthodont. 2010;2:46–9.
Krol AJ, Finzen FC. Rotational path removable partial dentures: part 1. Replacement of posterior teeth. Int J Prosthodont. 1988a;1:17–27.
Krol AJ, Finzen FC. Rotational path removable partial dentures: part 2. Replacement of anterior teeth. Int J Prosthodont. 1988b;1:135–42.
Kurtulmus H, Kumbuloglu O, Aktas RT, Kurtulmus A, Boyacioglu H, Oral O, User A. Effects of saliva and nasal secretion on some physical properties of four different resin materials. Med Oral Patol Oral Cir Bucal. 2010;15:e969–75.
Lekha K, Savitha NP, Roseline M, Nadiger RK. Acetal resin as an esthetic clasp material. J Interdiscip Dent. 2012;2:11–4.
Mohamed T, Baraka OA, Badawy MM. Comparison between acetal resin and cobalt-chromium removable partial denture clasps: Effect on abutment teeth supporting structures. IJOPRD. 2011;1:147–54.
Negrutiu M, Sinescu C, Romanu M, Pop D, Lakatos S. Thermoplastic resins for flexible framework removable partial dentures. TMJ. 2005;55:295–9.
Osada H, Shimpo H, Hayakawa T, Ohkubo C. Influence of thickness and undercut of thermoplastic resin clasps on retentive force. Dent Mater J. 2013;32:381–9.
Ozkan Y, Arikan A, Akalin B, Arda T. A study to assess the colour stability of acetal resins subjected to thermocycling. Eur J Prosthodont Restor Dent. 2005;13:10–4.
Polyzois G, Niarchou A, Ntala P, Pantopoulos A, Frangou M. The effect of immersion cleansers on gloss, colour and sorption of acetal denture base material. Gerodontology. 2013;30:150–6.
Suh JS, Billy EJ. Rotational path removable partial denture (RPD): conservative esthetic treatment option for the edentulous mandibular anterior region: a case report. J Esthet Restor Dent. 2008;20:98–107.
Taguchi Y, Shimamura I, Sakurai K. Effect of buccal part designs of polyamide resin partial removable dental prosthesis on retentive force. J Prosthodont Res. 2011;55:44–7.
Takabayashi Y. Characteristics of denture thermoplastic resins for non-metal clasp dentures. Dent Mater J. 2010;29:353–61.
Tannous F, Steiner M, Shahin R, Kern M. Retentive forces and fatigue resistance of thermoplastic resin clasps. Dent Mater. 2012;28:273–8.
The glossary of prosthodontics terms. J Prosthet Dent. 2005;94:10–92.
Turner JW, Radford DR, Sherriff M. Flexural properties and surface finishing of acetal resin denture clasps. J Prosthodont. 1999;8:188–95.
Ucar Y, Akova T, Aysan I. Mechanical properties of polyamide versus different PMMA denture base materials. J Prosthodont. 2012;21:173–6.
Wada J, Fueki K, Yatabe M, Takahashi H, Wakabayashi N. A comparison of the fitting accuracy of thermoplastic denture base resins used in non-metal clasp dentures to a conventional heat-cured acrylic resin. Acta Odontol Scand. 2014;14:1–5.
Wieckiewicz M, Opitz V, Richter G, Boening KW. Physical properties of polyamide-12 versus PMMA denture base material. Biomed Res Int. 2014;2014:150298. doi:10.1155/2014/150298.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Video 12.1
(MP4 8631 kb)
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Şakar, O. (2016). Esthetic Solutions for Removable Partial Dentures. In: Şakar, O. (eds) Removable Partial Dentures. Springer, Cham. https://doi.org/10.1007/978-3-319-20556-4_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-20556-4_12
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20555-7
Online ISBN: 978-3-319-20556-4
eBook Packages: MedicineMedicine (R0)