Abstract
Introduction
Outpatient thyroidectomy has been demonstrated in recent years as safe and feasible by a number of endocrine surgery centers. However, despite the inherent benefits of doing surgery with the same day discharge, the acceptance of thyroidectomy as an outpatient procedure has been slow and regarded by some as still controversial.
Methods
This manuscript addresses the logistics as well as the pros and cons of doing thyroidectomy with the same day discharge from the reported experience in the literature in the past decade and the perspective of the author’s approximate 20-year experience with outpatient thyroidectomy. Special emphasis is given to the diagnosis, prevention, and management of post-thyroidectomy cervical hematoma in the outpatient setting.
Conclusion
Outpatient thyroidectomy is feasible and safe for the majority of thyroid operations while providing similar health-care cost savings to society as other outpatient operations. It seems reasonable to anticipate increasing utilization of outpatient thyroidectomy by experienced thyroid surgeons in the future. Ultimately, the majority of thyroidectomy procedures will be accomplished in the outpatient setting to the benefit of the patient, hospital, surgeon, insurance company, and society.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Outpatient thyroidectomy
- Thyroidectomy same day discharge
- Post-thyroidectomy cervical hematoma
- Diagnosis of post-thyroidectomy cervical hematoma
- Prevention of post-thyroidectomy cervical hematoma
- Management of post-thyroidectomy cervical hematoma
- Thyroidectomy hemostasis
Introduction
Outpatient thyroidectomy has been demonstrated in recent years as safe and feasible by a number of endocrine surgery centers (Table 6.1) [1–14]. However, despite the inherent benefits of doing surgery with the same day discharge, the acceptance of thyroidectomy as an outpatient procedure has been slow and still regarded by some as controversial [15, 16]. The American Thyroid Association has recently released a statement on outpatient thyroidectomy that serves as an excellent reference for evaluating the logistics as well as the pros and cons of doing thyroidectomy with the same day discharge [17]. This manuscript addresses the same issues from the perspective of the author’s approximate 20-year experience with outpatient thyroidectomy.
Pros and Cons of Outpatient Thyroidectomy
It is important to understand that for most surgeons who perform endocrine surgery, the accomplishment of thyroidectomy in the outpatient setting is a gradual and evolutionary process. It starts with the least risky procedures, parathyroidectomy and/or partial thyroidectomy, and then evolves to include thyroid lobectomy, then total thyroidectomy for a diverse array of pathologies, and finally total thyroidectomy with central lymph node dissection. The safety of the procedure to the patient is paramount and rests primarily in avoiding the risk of life-threatening postoperative bleeding. Each surgeon must evaluate their personal experience with thyroidectomy to assess whether in their hands, it can be done safely in the outpatient setting. Outpatient thyroidectomy is not for every patient, but in the author’s experience, with careful patient selection, it can be accomplished for between 80 and 90 % of procedures [8]. It is appropriate to examine the advantages and disadvantages of outpatient thyroidectomy from the perspectives of the patient, hospital, surgeon, insurance company, and society.
Patient
There are advantages of being in the comfort of a familiar home environment with family or a caring friend. Even a hotel room can provide a quiet environment with fewer interruptions, a comfortable bed, and personal food choices. It can even be less costly if the patient must pay a remaining percentage of insurance charges and/or required co-payments. Finally, being outside the hospital environment can avoid rare hospital acquired infection risks, medication errors, or service and medication delays from caregivers. The disadvantages include losing the presumed safety net of the hospital environment with prompt attention for emergency care. Access to emergency evaluation may be compromised or delayed outside of the hospital. The fear of this unknown problem prompts some patients and their family or friends to be wary of outpatient surgery. In the author’s experience, however, the vast majority of patients are relieved and very receptive to having their surgery as an outpatient procedure.
Hospital
Outpatient surgery opens up hospital beds to utilization for the care of sicker patients, ultimately reducing the overall physical plant needs, staffing, and overhead costs. The hospital, however, may lose potential reimbursable charges.
Surgeon
The benefits of outpatient surgery accrue primarily with the more efficient use of time by eliminating hospital rounding, charting, etc. The surgeon, however, may lose the comfort of knowing that any problems with the patient’s recovery are being readily addressed within the hospital environment.
Insurance Company
Outpatient surgery saves expenditures. Government restrictions, reasonable or not, can sometimes mandate inpatient care.
Society
The penultimate global concern is how to reduce the burden of health-care expenditures while still providing quality health care. Outpatient surgery clearly saves health-care dollars.
Developing an Outpatient Thyroidectomy Program
Outpatient thyroidectomy is not universally applicable to all patients. The surgeon must determine if patient comorbidities require in-hospital postoperative care. The surgeon must also determine if the difficulty and extent of the thyroidectomy procedure increases the risk of postoperative complications that are best addressed in the hospital environment. Social concerns for adequate family support and travel restrictions may limit the feasibility of outpatient surgery. The hospital or outpatient surgery center must have a system designed to promote outpatient surgery with adequate patient evaluation and counseling prior to discharge. In the author’s main hospital, the same day discharge center will stay open to midnight to facilitate outpatient surgery.
The experience with laparoscopic cholecystectomy as an outpatient procedure in the last decade of the twentieth century is analogous to doing outpatient thyroidectomy currently. Historically, open cholecystectomy required a hospital stay for a few days before discharge. There were financial pressures to increasingly shorten the hospital stay. Then laparoscopic cholecystectomy was developed, which made the recovery less painful. It became apparent that the surgery could be tolerated as an outpatient procedure for most patients. The risk of postoperative bile leak, bleeding, or other serious complications was very rare, but not to be overlooked. Eventually, the standard of care favored outpatient laparoscopic cholecystectomy. A culture of expectation of outpatient surgery for this procedure by patients and health-care providers developed, such that patients are now dismissed from the same day surgery center as soon as they meet discharge criteria, usually within a few hours.
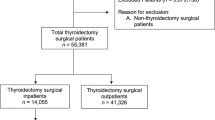
The evolution of outpatient thyroidectomy has been much slower than it was for laparoscopic cholecystectomy. This has occurred despite the awareness that most patients tolerate thyroidectomy as well as laparoscopic cholecystectomy from a discomfort point of view. Serious life-threatening complications are similarly rare, but again not to be overlooked. The author’s personal evolution toward doing outpatient thyroidectomy began in the last decade of the twentieth century with the experience of using local anesthesia with intravenous sedation for parathyroidectomy that allowed the patient to be dismissed the same day. Some patients had a dominant thyroid nodule that needed to be addressed at the same time as the parathyroidectomy. It was impressive how well they tolerated the additional partial thyroidectomy under local anesthesia. The experience of Dr. LoGerfo with thyroidectomy under local anesthesia with intravenous sedation [18] led the author to further utilize this approach with thyroid lobectomy, total thyroidectomy, and eventually total thyroidectomy with a central level VI lymph node dissection. The main advantage of local anesthesia surgery is the rapid postoperative recovery, which makes discharge of the patient the same day more feasible, much like the same day thyroidectomy discharge as promoted by Dr. LoGerfo [18]. A randomized prospective comparison of thyroidectomy under local anesthesia with intravenous sedation versus general anesthesia was conducted, and both groups were planned for outpatient thyroidectomy to see if there was an advantage to the local anesthesia approach. Patient satisfaction and results were surprisingly nearly identical. Complications occurred but could still be managed safely when they developed [1]. This led to the increasing utilization of outpatient thyroidectomy until approximately 80–90 % of thyroidectomies presently are done as outpatient procedures [8]. The author’s outpatient surgery center and main hospital center are geared toward providing the immediate postoperative support that allows the patient to be discharged home the same day. With this creation of a culture of outpatient thyroidectomy, the patient response to proposed outpatient surgery is universally positive. There is occasional push back from the patient and family for social and health-care concerns, but it is rare to have a patient be adamant about being hospitalized after surgery.
So why is there so much resistance by surgeons for doing outpatient thyroidectomy when the feasibility seems so evident? The answer rests in the overriding concern for postoperative hemorrhage in the central neck resulting in airway compromise from a life-threatening hematoma. Other major complications include symptomatic hypocalcemia from hypoparathyroidism and recurrent laryngeal nerve injury. A secondary overriding concern relates to problems with timely access to qualified emergency care, if needed. It is relevant to address each of these concerns in depth.
Postoperative Central Neck Hematoma: Incidence and Timing
Despite intensive efforts by the surgeon to avoid postoperative central neck hematoma, this complication predictably will occur in a very small percentage of patients. A number of studies have evaluated the incidence and timing of postoperative hematoma to formulate recommendations on the feasibility and safety of doing outpatient thyroidectomy (Table 6.2) [19–32]. The frequency of postoperative hematoma is approximately 1 % or less. Patient factors that increase the risk of postoperative bleeding have not been clearly defined although the author found a tendency toward increased bleeding risk in patients on anticoagulants [32]. It is important to keep in mind that most studies that report on postoperative central neck hematoma include all thyroidectomy procedures. Since outpatient thyroidectomy is done for selected patients deemed by the surgeon to have a lower risk for postoperative bleeding, the incidence of this complication then should be less. The author reported on all thyroidectomy procedures over a 6-year period of time during which postoperative bleeding occurred in 0.19 % (2/1064) outpatient thyroidectomies and 1.4 % (3/208) inpatient thyroidectomies [8]. The timing of postoperative bleeding varies among reported case series (Table 6.2). In general, about half will occur within 6 h of the surgery, a third within 7–23 h of the surgery, and the remaining 24 h or more after surgery. The author with coauthors Dixon, Lairmore, and Govednik reported on an institutional 17-year experience with postoperative hematoma following thyroidectomy and/or parathyroidectomy procedures and noted an incidence of 0.51 % (17/3357) after thyroidectomy; 38.9 % of bleeding overall occurred within 6 h after the surgery, 38.9 % between 7 and 23 h after the surgery, and 22.2 % from 24 to 96 h after the surgery [32]. Only two patients needed emergency bedside decompression of the cervical hematoma as a life-saving effort, and both occurred in the postoperative anesthesia care unit (PACU) within 2 h of the surgery. The remaining hematomas were surgically managed in the operating room. Half of the hematomas occurred in patients that had outpatient thyroidectomy. It is noteworthy that a predictable percentage of hematomas occur after 23 h following surgery. There are a number of studies that advocate a 23-h observation period following surgery as the optimal observation period before safely discharging the patients [15, 16, 33]. Yet this policy will still miss a defined percentage of postoperative bleeding episodes. A purist assessment would advocate a 2–4-day postoperative hospitalization to have every bleeding episode occur within the hospital environment. If outpatient thyroidectomy is contemplated, how long should the patient be observed in the day surgery unit prior to discharge? This is a judgment decision by the surgeon and relates to the perceived risk of postoperative bleeding. Six hours has been used by some surgeons [2, 5]. The author with coauthor’s reported experience on postoperative hematoma indicated that only bleeding occurring in the PACU needed emergency bedside decompression as a life-saving effort [32]. Therefore, in the author’s experience, patients deemed appropriate for outpatient thyroidectomy are dismissed from the day surgery unit when they meet the usual dismissal criteria plus observational evidence of no deep cervical wound bleeding. Trained nursing staff should be able to make that determination with surgeon input only as deemed necessary. Essentially, dismissal criteria are not much different from what would be used for a laparoscopic cholecystectomy with the exception of the assessment of the cervical wound. The author reported an average postoperative observation period of 2 h and 42 min prior to dismissal from the day surgery unit [8].
The relative risk of postoperative hematoma for an individual patient should be less for unilateral thyroidectomy than bilateral thyroidectomy, since the latter surgery requires hemostasis of almost twice as many blood vessels. Reported results seem to bear this out. A large Austrian study reported a significantly higher risk of postoperative hematoma for total thyroidectomy versus thyroid lobectomy (2.0 % vs. 1.0 %, p < 0.001) [31]. The author’s experience also demonstrated a 0.62 % occurrence of postoperative central neck hematoma after bilateral thyroidectomy procedures with or without parathyroidectomy versus a 0.38 % occurrence following unilateral thyroidectomy procedures with or without parathyroidectomy [32]. This has led some surgeons to be more willing to do outpatient thyroidectomy for thyroid lobectomy than total thyroidectomy [34]. The increased risk of postoperative cervical hematoma after total thyroidectomy appears to be just related to the more extensive surgery. There is no reported evidence that a cervical hematoma after total thyroidectomy is more life-threatening than a cervical hematoma after thyroid lobectomy. A central lymph node dissection plus total thyroidectomy should add minimal extra risk to the development of a postoperative cervical hematoma. The additional risk is mainly from thymic veins and small segmental tracheal arteries that need additional hemostasis.
Postoperative Central Neck Hematoma: Prevention
Complete hemostasis to prevent post-thyroidectomy central neck hematoma is the obvious solution to accomplishing outpatient thyroidectomy safely. Some technical considerations to achieve hemostasis deserve emphasis. Traditionally, the patient was placed in the slightly head-up or “beach chair” position to reduce venous pressure and therefore reduce intraoperative venous bleeding. However, this may obscure venous bleeding sites. The amount of blood loss during thyroidectomy is rarely substantial enough to have hemodynamic consequences. The author prefers the supine position for thyroidectomy to allow venous bleeding sites to be more readily identified for hemostasis during the operation. Traditionally, subplatysmal flaps are advocated by thyroid surgeons to augment the exposure of the thyroid gland. This requires dissection along the anterior jugular veins, which can place the subcutaneous wound at increased risk of postoperative venous bleeding with Valsalva maneuvers. Thyroidectomy can be accomplished readily without active subplatysmal flap dissection just by maximizing the midline exposure, which is the author’s preference. The frequently present midline anterior jugular veins can be ligated at wound opening or closure as indicated.
During thyroidectomy, there are a multitude of vessels that require hemostasis to prevent postoperative hematoma, many of which are not detailed in anatomy textbooks. The major venous channels are the isthmus, middle thyroid, superior thyroid, and thymic veins. As lower pressure blood vessels, they less often contribute to postoperative hematoma. The arterial blood vessels deserve more attention intraoperatively. In addition to the inferior thyroid, superior thyroid, and infrequent thyroid ima arteries, substantial arterial vessels are frequently located at the medial border of the cricothyroid muscle, the junction of the cricoid cartilage, and the trachea that the author likes to refer to as the “thyroid uma arteries,” ligament of Berry area, and segmental tracheal arterioles (Fig. 6.1a). The author has witnessed a resulting postoperative hematoma from each of these sites. All of these potential arterial bleeding sites become more evident in patients with Graves’ disease. The use of loupe magnification during thyroidectomy enhances the visualization of potential bleeding sites, particularly small vessel side branches that may be in spasm during wound exploration but at risk of initiating postoperative bleeding (Fig. 6.1b). Careful inspection of the entire wound for these enumerated major bleeding sites following completion of the thyroidectomy is paramount to avoiding postoperative bleeding. The author likes to place additional small ligaclips on these at-risk bleeding sites, particularly in the ligament of Berry area and “thyroid ima arteries” prior to completing wound closure. It is helpful to do the larger, more vascular, and more difficult thyroid lobe first when planning a total thyroidectomy to allow for a greater lapse of time to ensure adequate hemostasis prior to wound closure. The presence of a small hematoma on the first thyroid lobectomy side indicates the location of a residual bleeding site that needs further hemostasis. Other measures to assist in identifying potential residual bleeding sites following completion of the thyroidectomy include an induced Valsalva maneuver by anesthesia to raise venous pressure, wound dabbing, and/or gentle rubbing combined with irrigation.
Hemostasis can be effectively accomplished with vessel suture ligation, vessel clips, electrocautery, or other high-energy devices. The author uses all of these methods but prefers mechanical hemostasis of major blood vessels. A significant difference in effective hemostasis has not been demonstrated between these hemostatic methods [35, 36]. The recently published large study from Austria indicated a small rise in the incidence of postoperative hematoma after thyroidectomy in recent years (1979–1983 1.0 %, 1989–1998 1.7 %, 2004–2008 2.4 %), but the cause of this is open to speculation [31]. It is unclear whether hemostatic techniques played a significant role in this observation. Perhaps a more telling result was the demonstration by the Austrian study of significant differences in the rate of postoperative hematoma among surgeons (0.4–2.8 %, p < 0.001) [31]. Individual surgeons contemplating doing outpatient thyroidectomy need to demonstrate a correspondingly very low postoperative hematoma rate, if any. A variety of hemostatic pads or clotting aids are commercially available to apply to the thyroidectomy bed to augment principally small vessel hemostasis before wound closure. There is unlikely to be any statistical evidence to support this endeavor, but the practice of adding hemostatic agents to the thyroidectomy bed seems reasonable.
A wound closure method for the strap muscles that is minimal with a single figure-of-eight suture or by leaving the lower portion of the strap muscles open has been proposed to enhance earlier recognition of significant deeper postoperative bleeding as the blood diffuses into the subcutaneous spaces [3, 18]. The use of drains left in the thyroidectomy bed to also enhance earlier recognition of postoperative bleeding has not been proven to be useful [17]. These have the theoretical potential to disturb hemostasis at the time of drain removal. The author does not use drains. Coughing and straining are to be avoided during extubation at the end of the operation [37]. Deep extubation by anesthesia, if reasonable, can accomplish this. Avoiding nausea and vomiting in the early postoperative recovery is also desirable. A number of pharmacological agents given during and after the operation can assist in this. A final practical measure to facilitating outpatient discharge is to anesthetize the wound with a long-acting local anesthetic, which may help minimize the early need for narcotic pain medication and thus side effects associated with pain medication.
Postoperative Central Neck Hematoma: Management
It is important to keep in mind the evolution of neck wound dressings over time. Historically, patients having thyroidectomy decades ago had bulky dressings, e.g., Queen Anne’s dressing, to apply a modicum of pressure to the wound to limit postoperative bleeding. At the author’s institution in 1980, it was a standard practice for older surgeons to use this kind of dressing while placing every thyroidectomy patient in the intensive care unit with a tracheostomy set at the bedside for fear of a postoperative hematoma. However, the anterior neck is not an area that can be adequately compressed to contribute to hemostasis. The bulky dressings merely hid a developing hematoma until the patient was extremely symptomatic, potentially contributing to the morbidity of this complication. Older studies on the incidence, timing, and severity of postoperative hematoma likely included patients managed with bulky dressings. Today, the optimal wound coverage is a minimal gauze dressing barely covering the wound or perhaps no dressing with a plastic sealant dressing. This gives ready visual access to the anterior neck to detect a developing hematoma, sometimes even before it becomes symptomatic.
Postoperative central neck hematoma can be a lethal complication. A rapidly expanding hematoma from major arterial bleeding can produce significant tracheal pressure to compromise the airway. This is verified by decreasing oxygen saturation and the patient’s waning ventilatory status. The classic management of this clinical situation is bedside decompression by promptly opening the wound, removing closing sutures, evacuating the hematoma, and even performing a tracheostomy in extremis conditions to reestablish an airway. Attempts at endotracheal intubation in this clinical situation are fraught with difficulty and serve only to delay proper life-saving treatment. Most reported studies do not indicate how often bedside decompression was necessary or the mortality of postoperative hematoma. In the author’s experience, bedside decompression of a hematoma is rarely necessary and primarily limited to a rapidly enlarging hematoma that becomes evident shortly after surgery is completed while the patient is in the postoperative anesthesia care unit (PACU) [32].
The more common clinical scenario is a slowly expanding central neck hematoma from small arteriole or venous bleeding that produces a mild- to moderate-size hematoma. The gradually increasing central neck compartment pressure leads to laryngeal edema that can contribute to compromising the airway. The patient complains of progressive neck swelling and/or tightness. The patient has difficulty putting the chin down on the chest without experiencing increased tightness or a choking sensation. As the swelling increases, the patient has difficulty lying flat, because of increased shortness of breath. The patient prefers sitting upright with the neck slightly extended, which maximizes the airway opening. With increasing laryngeal edema, the patient may develop stridorous breathing. The diagnosis of postoperative central neck hematoma is generally a clinical one. Ultrasound of the central neck is difficult to interpret secondary to postoperative swelling and the interference from hemostatic pads that may have been placed at the time of wound closure. Computerized tomography scan of the neck can be helpful to establish the diagnosis, but usually it delays proper treatment, which is wound decompression. Attempts at endotracheal intubation are again fraught with danger, because of the risk of inducing laryngeal spasm and life-threatening airway compromise.
The initial management of the patient with a central neck hematoma requires confirming adequate oxygenation with O2 saturation measurements, with or without supplemental oxygen. Keeping the patient in the upright position promotes this. The patient needs urgent central neck decompression. The author prefers to accomplish this in the controlled environment of the operating room. Anesthesia and the operating room staff are aware of the emergency nature of this intervention. Surgical staff accompanies the patient to the operating room, maintaining the upright position. The patient is prepped awake in 45° upright position. Using local anesthesia, the cervical wound is opened and hematoma evacuated. The patient can now tolerate the supine position without respiratory difficulty. Continuing under local anesthesia with some mild sedation, the wound can be searched for the bleeding source. Irrigation of the wound with a dilute hydrogen peroxide solution helps clear residual blood clot. Hemostasis is established with ligation of the bleeding site or confirmed by excluding a persistent active bleeding site, which is frequently the end result of wound exploration. If successful, the operation can be completed safely under local anesthesia with mild sedation. If general anesthesia is felt necessary to facilitate an adequate wound exploration for hemostasis, the patient can be intubated once they can tolerate the supine position. It is reasonable for the anesthesia team to consider pursuing awake intubation with endoscopic guidance as the safest approach in this situation, because of the anticipated laryngeal edema that makes securing the airway more difficult. The irritated larynx appears to be more susceptible to develop laryngeal spasm with endotracheal intubation attempts. If the patient has been paralyzed already with succinylcholine, an emergency surgical airway with tracheostomy is needed. The author has experienced just this set of circumstances on one occasion. Tracheostomy is readily accomplished, however, with the wound already opened and trachea exposed. If concern about maintaining an adequate airway remains following completion of the wound exploration, the patient can be left intubated for a period of time, maintained in a semi-upright position, and given steroids to reduce laryngeal edema before extubation can later be safely accomplished. This sequence of events for management of the central neck hematoma can be accomplished similarly for the hospitalized patient or for the outpatient from the emergency room. Again, in the author’s experience, the vast majority of patients with central neck hematoma can be managed without initial bedside decompression of the cervical wound [32].
Postoperative Hypoparathyroidism
The development of symptomatic hypocalcemia secondary to hypoparathyroidism is not really an impediment to successful outpatient thyroidectomy. It is a risk factor only after total thyroidectomy or completion total thyroidectomy. The nadir of postoperative hypocalcemia is typically 48–72 h postoperatively when symptoms become more evident. The short half-life of parathyroid hormone in the blood allows measuring PTH in the day surgery unit or PACU to select patients for oral supplemental calcium plus calcitriol [38]. Various time frames from immediately after surgery to 6 h postoperatively have been reported to correctly predict significant hypocalcemia [39]. Generally, an intact parathyroid hormone level below 10–15 is used to prescribe postoperative calcium medication [40]. The alternative approach is to recommend routine oral calcium supplementation postoperatively for total thyroidectomy [41]. The medication is inexpensive and highly unlikely to result in significant hypercalcemia. It is helpful to keep in mind that there are differences among calcium medications as to the elemental calcium content, which is 40 % for the more commonly used calcium carbonate. Oscal brand does specify a level of 500 mg of elemental calcium with each tablet. Calcium citrate preparations are more readily absorbed in patients with altered gastrointestinal function, i.e., Roux-en-y gastric bypass. Calcitriol can be added at the surgeon’s discretion, if there is increased concern for less than ideal blood supply to parathyroid glands intraoperatively or very low postoperative parathyroid hormone levels (<10). The need for autotransplantation of only one parathyroid gland has not been shown to increase the risk of early postoperative symptomatic hypocalcemia [42]. If symptomatic hypocalcemia does develop despite supplemental oral calcium, it can frequently be successfully managed in the outpatient setting with only a very small percentage of patients needing in-hospital treatment [8].
Recurrent Laryngeal Nerve Injury
Bilateral recurrent laryngeal nerve injury is a contraindication to outpatient thyroidectomy and should be immediately evident following extubation in the operating room or PACU. Unilateral recurrent laryngeal nerve injury is not a contraindication to outpatient thyroidectomy [8]. Patients, however, are at increased risk for aspiration, particularly with oral liquids. This leads to frequent coughing that can then foment postoperative internal bleeding in the central neck compartment. Patients can reduce the risk of aspiration by taking oral liquids in small amounts (drinking through a straw) and tilting the head down and to the side of the injury to mechanically protect the airway during swallowing.
The patient’s voice quality is a poor diagnostic aid to identify unilateral recurrent laryngeal nerve injury in the immediate postoperative period. Intraoperative recurrent laryngeal nerve monitoring, particularly using electrode-bearing endotracheal tubes with an electromyographic monitor, can indicate the presence of a recurrent laryngeal nerve injury [43]. If a total thyroidectomy is planned and the first lobectomy side indicates a recurrent laryngeal nerve that is anticipated to recover within the next few months, then a completion total thyroidectomy with contralateral lobectomy is delayed until adequate vocal cord function returns on the initial affected side [44]. This avoids the risk of bilateral recurrent laryngeal nerve injury and still allows the thyroidectomy surgery to be done as an outpatient procedure. When intraoperative nerve monitoring indicates the presence of a recurrent laryngeal nerve injury, the surgeon can now counsel the patient about the altered voice function that is anticipated and the proper maneuvers to avoid aspiration of liquids with swallowing [44]. This knowledge allows safe discharge of the patient from the day surgery unit and avoids increased risk of postoperative bleeding associated with aspiration-induced coughing.
Outpatient Thyroidectomy: Social Concerns
A program of outpatient thyroidectomy requires detailed oral and written instructions about potential postoperative complications, particularly the signs and symptoms of bleeding into the thyroidectomy bed, the response to these complications in seeking emergency evaluation when indicated, where to seek emergency evaluation, and contact information during the day or night for advice concerning possible complications. All of these instructions can be covered before and once again after the surgery. The patient needs involved family or friends that appear to understand instructions about potential complications and are readily able to provide assistance, especially in the early postoperative period.
Adequate transportation to an emergency facility is a necessary consideration for outpatient thyroidectomy. Ideally, this would be to the institution where the surgery took place. If travel from home would be considered too distant or too difficult from the hospital to be safe, then the patient, family, and/or friends are counseled to stay in a nearby hotel or motel for at least the first postoperative night. How far is too far is a judgment decision between the surgeon and patient, family, and/or friends. The author’s experience with patients that have had a postoperative cervical hematoma following outpatient thyroidectomy has not identified a prohibitive distance from the hospital. Intuitively, a separation of greater than 1–2 h would be considered problematic. All these social concerns, if not adequately resolved, could contraindicate proceeding with outpatient thyroidectomy.
Patient Selection
So which thyroid operations and which pathologies should or should not be done as outpatient procedures? There are no absolute contraindications, meaning even a multinodular goiter with substernal extension, Graves’ disease, or thyroid cancer can be considered a candidate for outpatient thyroidectomy. Patients needing a lateral cervical lymph node neck dissection, however, are excluded from this consideration. It is a judgment decision by the surgeon concerning the extent of the operative procedure, relative risk of postoperative bleeding, patient comorbidities, adequate initial postoperative observation in the day surgery unit, and adequate supportive outpatient social circumstances. It is not related to how much blood loss occurred during the operation, but how thorough and complete hemostasis appears at the end of the operation. While the surgeon cannot universally predict who will develop postoperative bleeding, the relative risk can be assessed, so that patients felt to be at significantly increased risk can be observed in the hospital setting. The author reported an incidence of postoperative cervical hematoma of 0.19 % for outpatient procedures and 1.4 % for inpatient procedures that indicates prudent patient selection [8].
Conclusion
With all these considerations in mind, outpatient thyroidectomy is feasible and safe for the majority of thyroid operations while providing similar health-care cost savings to society as other outpatient operations. It seems reasonable to anticipate increasing utilization of outpatient thyroidectomy by experienced thyroid surgeons in the future. A recent study confirms that this is already taking place at major university hospitals [45]. Ultimately, the majority of thyroidectomy procedures will be accomplished in the outpatient setting to the benefit of the patient, hospital, surgeon, insurance company, and society.
References
Snyder SK, Roberson CR, Cummings CC, Rajab MH. Local anesthesia with monitored anesthesia care vs general anesthesia in thyroidectomy: a randomized study. Arch Surg. 2006;141(2):167–73.
Spanknebel K, Chabot JA, DiGiorgi M, Cheung K, Curty J, Allendorf J, LoGerfo P. Thyroidectomy using monitored local or conventional general anesthesia: an analysis of outpatient surgery, outcome and cost in 1,194 consecutive cases. World J Surg. 2006;30(5):813–24.
Terris DJ, Moister B, Seybt MW, Gourin CG, Chin E. Outpatient thyroid surgery is safe and desirable. Otolaryngol Head Neck Surg. 2007;136(4):556–9.
Inabnet WB, Shifrin A, Ahmed L, Sinha P. Safety of same day discharge in patients undergoing sutureless thyroidectomy: a comparison of local and general anesthesia. Thyroid. 2008;18(1):57–61.
Champault A, Vons C, Zilberman S, Labaille T, Brosseau S, Franco D. How to perform a thyroidectomy in an outpatient setting. Langenbecks Arch Surg. 2009;394(5):897–902.
Trottier DC, Barron P, Moonje V, Tadros S. Outpatient thyroid surgery: should patients be discharged on the day of their procedures? Can J Surg. 2009;52(3):182–6.
Seybt MW, Terris DJ. Outpatient thyroidectomy: experience in over 200 patients. Laryngoscope. 2010;120(5):959–63.
Snyder SK, Hamid KS, Roberson CR, Rai SS, Bossen AC, Luh JH, Scherer EP, Song J. Outpatient thyroidectomy is safe and reasonable: experience with more than 1,000 planned outpatient procedures. J Am Coll Surg. 2010;210(5):575–82. 5.
Hessman C, Fields J, Schuman E. Outpatient thyroidectomy: is it safe and reasonable option? Am J Surg. 2011;201(5):565–8.
Houlton JJ, Pechter W, Steward DL. PACU PTH facilitates safe outpatient total thyroidectomy. Otolaryngol Head Neck Surg. 2011;144(1):43–7.
Sklar M, Ali MJ, Solomon P. Outpatient thyroid surgery in a Toronto community hospital. J Otolaryngol Head Neck Surg. 2011;40(6):458–61.
Tuggle CT, Roman S, Udelsman R, Sosa JA. Same-day thyroidectomy: a review of practice patterns and outcomes for 1,168 procedures in New York State. Ann Surg Oncol. 2011;18(4):1035–40.
Mazeh H, Khan Q, Schneider DF, Schaefer S, Sippel RS, Chen H. Same-day thyroidectomy program: eligibility and safety evaluation. Surgery. 2012;152(6):1133–41.
Sahmkow SI, Audet N, Nadeau S, Camiré M, Beaudoin D. Outpatient thyroidectomy: safety and patient’s satisfaction. J Otolaryngol Head Neck Surg. 2012;41 Suppl 1:S1–12.
Doran HE, England J, Palazzo F. British association of endocrine and thyroid surgeons. Questionable safety of thyroid surgery with same day discharge. Ann R Coll Surg Engl. 2012;94(8):543–7.
Menegaux F. Ambulatory thyroidectomy: recommendations from the Association Francophone de Chirurgie Endocrinienne (AFCE). Investigating current practices. J Visc Surg. 2013;150(3):165–71.
Terris D, Snyder S, Carneiro-Plus D, Inabnet W, Kandil E, Orloff L, Shindo M, Tufano R, Tuttle M, Urken M, Yeh M. American Thyroid Association statement on outpatient thyroidectomy. Thyroid. 2013;23(10):1193–202.
Lo GP. Local/regional anesthesia for thyroidectomy: evaluation as an outpatient procedure. Surgery. 1998;124(12):975–9.
Shaha AR, Jaffe BM. Practical management of post-thyroidectomy hematoma. J Surg Oncol. 1994;57:235–8.
Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP. Morbidity of thyroid surgery. Am J Surg. 1998;176:71–5.
Reeve T, Thompson NW. Complications of thyroid surgery: how to avoid them, how to manage them, and observations on their possible effect on the whole patient. World J Surg. 2000;24:971–5.
Burkey SH, van Heerden JA, Thompson GB, Grant CS, Schleck CD, Farley DR. Reexploration for symptomatic hematomas after cervical exploration. Surgery. 2001;130:914–20.
Zambudio AR, Rodriguez J, Riquelme J, Soria T, Canteras M, Parrilla P. Prospective study of postoperative complications after total thyroidectomy for multinodular goiters by surgeons with experience in endocrine surgery. Ann Surg. 2004;240:18–25.
Materazzi G, Dionigi G, Berti P, Rago R, Frustaci G, Docimo G, Puccini M, Miccoli P. One-day thyroid surgery: retrospective analysis of safety and patient satisfaction on a consecutive series of 1,571 cases over a three-year period. Eur Surg Res. 2007;39:182–8.
Bergenfelz A, Jansson S, Kristoffersson A, Martensson H, Reihner E, Wallin G, Lausen I. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg. 2008;393:667–73.
Leyre P, Desurmont T, Lacoste L, Odasso C, Bouche G, Beaulieu A, Valagier A, Charalambous C, Gibelin H, Debaene B, Kraimps JL. Does the risk of compressive hematoma after thyroidectomy authorize 1-day surgery? Langenbecks Arch Surg. 2008;393(5):733–7.
Rosenbaum MA, Haridas M, McHenry CR. Life-threatening neck hematoma complicating thyroid and parathyroid surgery. Am J Surg. 2008;195(3):339–43.
Bononi M, Amore Bonapasta S, Vari A, Scarpini M, De Cesare A, Miccini M, Meucci M, Tocchi A. Incidence and circumstances of cervical hematoma complicating thyroidectomy and its relationship to postoperative vomiting. Head Neck. 2010;32(9):1173–7.
Chang LY, O’Neill C, Suliburk J, Sidhu S, Delbridge L, Sywak M. Sutureless total thyroidectomy: a safe and cost-effective alternative. ANZ J Surg. 2011;81:510–4.
Lang B, Yih P, Lo CY. A review of risk factors and timing for postoperative hematoma after thyroidectomy: is outpatient thyroidectomy really safe? World J Surg. 2012;36:2497–502.
Promberger R, Ott J, Kober F, Koppitsch C, Seemann R, Freissmuth M, Hermann M. Risk factors for postoperative bleeding after thyroid surgery. Br J Surg. 2012;99(3):373–9.
Dixon JL, Snyder SK, Lairmore TC, Jupiter DC, Govednik CM, Hendricks JC. A novel method for the management of post-thyroidectomy or parathyroidectomy hematoma: a single institution experience after over 4000 central neck operations. World J Surg. 2014;38(6):1262–7.
Materazzi G, Dionigi G, Berti P, et al. One-day thyroid surgery: retrospective analysis of safety and patient satisfaction on a consecutive series of 1571 cases over a three-year period. Eur Surg Res. 2007;39:182–8.
Torfs A, Laureyns G, Lemkens P. Outpatient hemithyroidectomy: safety and feasibility. B-ENT. 2012;8(4):279–83.
Inabnet WB, Shifrin A, Ahmed L, Sinha P. Safety of same day discharge in patients undergoing sutureless thyroidectomy: a comparison of local and general anesthesia. Thyroid. 2008;18(1):57–61.
Siperstein AE, Berber E, Morkoyun E. The use of the harmonic scalpel vs conventional knot tying for vessel ligation in thyroid surgery. Arch Surg. 2002;137:137–42.
Morgan Jr GE, Mikhail MS, Murray MJ. Chapter 5. Airway management. In: Morgan Jr GE, Mikhail MS, Murray MJ, editors. Clinical anesthesiology. 4th ed. New York: McGraw-Hill; 2006.
Houlton JJ, Pechter W, Steward DL. PACU PTH facilitates safe outpatient total thyroidectomy. Otolaryngol Head Neck Surg. 2011;144(1):43–7.
Wiseman JE, Mossanen M, Ituarte PH, Bath JM, Yeh MW. An algorithm informed by the parathyroid hormone level reduces hypocalcemic complications of thyroidectomy. World J Surg. 2010;34(3):532–7.
McCullough M, Weber C, Leong C, Sharma J. Safety, efficacy, and cost savings of single parathyroid hormone measurement for risk stratification after total thyroidectomy. Am Surg. 2013;79:768–74.
Singer MC, Bhakta D, Seybt MW, Terris DJ. Calcium management after thyroidectomy: a simple and cost-effective method. Otolaryngol Head Neck Surg. 2012;146:362–5.
Karakas E, Osei-Agyemang T, Schlosser K, Hoffmann S, Zielke A, Rothmund M, Hassan I. The impact of parathyroid auto transplantation during bilateral surgery for Graves’ disease on postoperative hypocalcemia. Endocr Regul. 2008;42:39–44.
Snyder SK, Lairmore TC, Hendricks JC, Roberts JW. Elucidating mechanisms of recurrent laryngeal nerve injury during thyroidectomy and parathyroidectomy. J Am Coll Surg. 2008;206(1):123–30.
Snyder SK, Hendricks JC. Intraoperative neurophysiology testing of the recurrent laryngeal nerve: plaudits and pitfalls. Surgery. 2005;138(12):1183–92.
Stack Jr BC, Moore E, Spencer H, Medvedev S, Bodenner DL. Outpatient thyroid surgery data from the University Health System (UHC) consortium. Otolaryngol Head Neck Surg. 2013;148(5):740–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Snyder, S.K. (2016). Ambulatory Thyroid Surgery: Is This the Way of the Future?. In: Hanks, J., Inabnet III, W. (eds) Controversies in Thyroid Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-20523-6_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-20523-6_6
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20522-9
Online ISBN: 978-3-319-20523-6
eBook Packages: MedicineMedicine (R0)