Abstract
Fractures of the scaphoid are current, especially in young men, and represent 70–80 % of the traumas of the carpus. The large majority concerns the scaphoid waist, which is narrower and more fragile than the other parts of the bone.
The injury is most often caused by a trauma in compression/shearing during the hyperextension of the wrist combined with a radial or ulnar inclination, which explains the wide variety of fractures we can find.
Their consolidation is difficult because of the important constraints imposed on the scaphoid and its precarious vascularization (especially in its proximal part).
The efficiency of the treatment depends on an early diagnosis that avoids evolution towards a degenerative wrist (or scaphoid nonunion advanced collapse wrist).
Rehabilitation must improve mobility and strength without compromising the healing process, which remains the priority. After consolidation, reinforcing the flexor carpi radialis is an important element of treatment as it stabilizes efficiently the scaphoid, opposing to the palmar displacement of its distal part.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Fractures of the scaphoid are frequent, especially in young men, and represent 70–80 % of the traumas on the carpus [1].
Their consolidation is difficult because of the important constraints imposed on the scaphoid and its precarious vascularization [2].
The efficiency of the treatment depends on an early diagnosis, which allows avoiding evolutions towards a scaphoid nonunion advanced collapse [3].
1 Physiopathology [4–7]
The fractures of the scaphoid concern most of the times the waist of the bone that is narrower and more fragile than the rest of the bone.
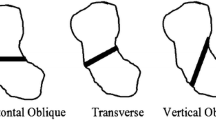
The injury is most often due to a trauma in compression/shearing in wrist hyperextension, combined with a radial or ulnar inclination.
This mechanism puts tension on the palmar radio-carpal ligaments that forbid the scaphoid from going frontward. The bone then suffers the shock from the posterior part of the radius at the level of the waist. The radioscaphocapitate ligament can increase the displacement in flexion of the distal fragment, causing a shortening of the bone (Fig. 3.1).
This mechanism only occurs in fractures of the waist and doesn’t concern the fractures of the proximal part [8].
The same mechanism puts important constraints on the scapholunate ligament, opposed to the differential gliding between the scaphoid and lunate.
That’s why in a trauma in hyperextension, we can observe a fracture of the scaphoid, an injury of the scapholunate ligament, or a fracture of the radial epiphysis. The combination of these injuries is rare (Fig. 3.2).
2 Clinical and Paraclinical Signs
With the patient interview only, we can determine if there has been a “risky” trauma.
The most suggestive clinical sign is pain when palpating the anatomical snuffbox, (Fig. 3.3) but if there’s an edema in this area or in the radial side of the wrist and pain when putting load on the scaphoid, we’ll have to realize X-rays [9].
Sometimes, the X-rays are clear and the diagnosis is easy, but it’s possible that the fracture isn’t visible on the X-ray on the day of the trauma.
In this case, a resting orthosis is realized and kept 15 days, and then other X-rays are realized to confirm the presence/absence of fracture.
However, we must keep in mind that the decalcification process around the fracture line that allows detecting a fracture after 15 days isn’t systematic, especially in proximal fractures. When in doubt, we use MRI and scintigraphy.
Echography also has a certain interest in the diagnosis, but its efficiency is operator dependent.
3 Therapeutical Process and Surgical Treatment [4–7]
The treatment depends on the location of the fracture line, whether the fracture is displaced or not, and the patient’s socioeconomical and sports context. This treatment can be orthopedic or surgical with conventional screwing, percutaneous technique, or simple pin.
3.1 Orthopedic Treatment [10]
The orthopedic treatment by prolonged immobilization stays the first-line indication to treat undisplaced fractures of the scaphoid, but the development of percutaneous osteosynthesis tends to progressively prevail over the cast. Several studies agree that there’s a high rate of consolidation (more than 90 %); however, opinions differ more widely as regards the type of immobilization, the wrist position, and the duration of immobilization.
3.1.1 Immobilize the Elbow and the Thumb?
The SOFCOT’s round table in 1988 gathers a series of 209 recent undisplaced fractures of the scaphoid treated with brachio-palmar immobilization in 41 % of the cases and antebrachio-palmar immobilization in 33 % of the cases. The 26 % left were treated with a combination of the 2 previous techniques (first brachio-palmar, then antebrachio-palmar). The conclusion of this study doesn’t bring formal statistical elements to confirm the superiority of one treatment or the other.
In 1990, a study shows on 10 subjects that pronosupination doesn’t put constraint on the scaphoid, unlike the flexion/extension and the radial and ulnar inclinations. Only two studies analyze the consolidation rate depending on whether the elbow is in the cast or not; they both conclude that the consolidation isn’t improved when the elbow is immobilized.
The fact that the elbow must be immobilized in fractures of the scaphoid is strongly anchored in people’s minds. In 1943 Watson-Jones recommends blocking the thumb’s metacarpophalangeal joint, and we have to wait until 1991 for a randomized prospective study to obtain results identical between the group of patients immobilized until the interphalangeal and those with the thumb free.
3.1.2 Wrist Position
The most common method is the immobilization in a neutral position in the sagittal and frontal planes, with a slight radial inclination to avoid distraction in the fracture site.
3.1.3 Immobilization Duration
Several studies have evaluated the consolidation duration between 12 and 15 weeks. Some authors recommend only 2 months of immobilization for distal fractures as the distal part is more vascularized, but no clinical study confirms this.
In theory, only a proof of consolidation should allow us to stop the immobilization, but in practice this consolidation is hard to confirm and immobilizing during 3 months seems to be the most scientifically established and the most prudent approach.
3.1.4 Immobilization Type
The cast still seems to be the most used technique. However, the resins have several advantages: They’re half as heavy as casts and they’re more solid and resist to water. But they also have disadvantages: poor plasticity making compressions more frequent and hardness of the material that can irritate the skin.
Thermoformed custom-made orthosis provides more comfort in the patients’ daily life and can be readjusted when the edema disappears.
In conclusion, 2–3 months of immobilization depending on the location of the fracture line, with the wrist in a neutral position and the thumb free in a thermoformed orthosis, is the first-line indication in undisplaced fractures of the scaphoid.
3.2 Surgery
Displaced fractures of the scaphoid and delayed bone healing are indications for surgery [11].
In 1968 the screwing with a spongy 4 mm screw has been described in the AO’s osteosynthesis manual, but subsequent studies have shown technique difficulties due to the particular anatomy of this bone [12] and the equipment load. Since the beginning of the 1980s and the apparition of Herbert’s headless screw, several screws have been developed to favor the compression and make the placement easier. In this chapter, we’ll develop the main osteosynthesis techniques with traditional screws, percutaneous screws, and percutaneous pins.
3.2.1 Traditional Screws
Screwing can be realized in a retrograde way with an anterior approach or from proximal to distal with a posterior approach in proximal fractures.
We use an AO stainless steel screw with a 2 mm diameter with a long thread length to allow a good compression (Fig. 3.4). Perforated screws avoid multiple drilling, but have a wider diameter.
In anterograde screwing from proximal to distal, we prefer screws with a smaller diameter considering the small size of the proximal fragment (Fig. 3.5).
The surgical follow-ups depend on the surgeon and go from no immobilization to a resin cuff during a month.
Consolidation rates vary between 90 and 100 %.
3.2.2 Percutaneous Screws [13]
Since a few years, little invasive surgical techniques have been developed to reduce morbidity and preserve the scaphoid’s vascularization as well as the ligaments surrounding it.
The approach can be palmar (Fig. 3.6) or dorsal, and the reduction is controlled with radioscopy or coupled with arthroscopy. This technique uses perforated screws guided by a pin. The diameter of the screw varies from 2 to 3 mm.
Instable and displaced fractures are formal indications for osteosynthesis [11]. The percutaneous technique is reserved to fractures that are little displaced and is more and more used in undisplaced fractures based on economic, social, professional, and sports factors, as it reduces the duration of immobilization (0–30 days).
3.2.3 Percutaneous Pins [14, 15]
The pins seem to be the best osteosynthesis technique for the scaphoid, putting compression on the fracture site. However, some authors are now wondering if compression is necessary for the scaphoid. The natural tendency in median fractures is towards flexion, so we’ll have to install a wiring during the synthesis. The pins allow a stable osteosynthesis without shortening of the scaphoid and avoid rotation disorders if we place at least 3 pins with a diameter between 14 and 16.
In conclusion, the surgical treatment is justified in undisplaced fractures when:
-
The fracture concerns the proximal part.
-
There’s an associated injury requiring surgery.
-
The fracture is open or unstable.
-
The patient is a sportsman or motivated worker who wants to quickly go back to his activities.
4 Rehabilitation and Orthotic Treatment [4–7]
Rehabilitation can follow surgery or a longer immobilization in case of orthopedic treatment.
The different protocol stages can be modified depending on the bone healing, regularly controlled with X-rays.
In any case, the priorities are regaining physiological amplitudes and strength to restore optimal function.
There are many similar points between this protocol and the one for the fractures of the inferior extremity of the radius, but the concerned patients are usually very different.
The patients with a fracture of the inferior extremity of the radius are usually woman of more than 60 years old with osteoporosis, whereas the patients with a fracture of the scaphoid are usually young men who have suffered a high kinetic energy trauma.
Therefore, the rehabilitation goals for these two pathologies are often different, as they’re related to the patient’s anterior capacities and functional imperatives. The exercises are usually more intense in fractures of the scaphoid, especially in muscular reinforcement and proprioception exercises.
4.1 Rehabilitation Protocol (Fig. 3.7)
4.1.1 Immobilization Phase (D0 to D15/45 with Surgery or D0 to D60/90 Without Surgery)
The duration of immobilization after surgery depends on the surgical technique and varies from 15 (percutaneous screws) to 45 days (pins).
During all this phase, rehabilitation isn’t essential and self-rehabilitation advices are given to the patient.
The treatment is based on the protocol PRICE that fights against trophic disorders resulting from the trauma and surgery:
-
P for protection of the fracture line during the whole phase, realized immobilizing the wrist and informing the patient about the tissue fragility in this phase.
-
R for rest of the damaged area that mustn’t be solicited during the immobilization phase, aside from self-rehabilitation exercises explained by the therapist. These exercises are described in the Chap. 5, Fig. 5.20.
-
I for ice, putting cold packs several times a day on the fracture zone. If there’s a cast it’s impossible, but if there is no wound, we immobilize the patient with a thermoformed orthosis, which allows cold bath against edema.
-
C for compression that can be realized in the fingers if they’re swollen.
-
E for elevation of the wrist to avoid edema.
These exercises are combined with sensorimotor stimulations to maintain the body mapping and cutaneous receptors and with simple active mobilizations of the free joint (the metacarpophalangeals in the long fingers tend to get easily stiff). We stop these exercises if pain appears.
4.1.2 Pre-consolidation Phase (D15/45 to D90 with Surgery or D60/90 to D120 Without Surgery)
In this phase we start putting load on the scaphoid, and the patient progressively goes back to his daily activities. We fight against pain and trophic disorders if they are still present, try to regain functional amplitudes, and start the muscular awakening and reinforcement.
4.1.2.1 Fight Against Trophic Disorders and Pain
It’s essential to start with the rest of the rehabilitation.
We use the similar techniques than in fractures of the inferior extremity of the radius:
-
Draining massages without slackening the scar in case of surgery. Decontracting massages for the forearm if we observe hypertonia in the extrinsic musculature, which is frequent (Fig. 3.8).
-
Analgesic electrotherapy can be used.
-
Pressotherapy from distal to proximal helps draining the wrist. In this phase, this technique can be badly tolerated by the patient; we’ll then delay its use.
-
Transcutaneous vibratory stimulations and infrasounds are used for their analgesic and vasomotor effect. Vibrations with more than 1 mm amplitude are realized far from the fracture site in order not to disturb the healing process.
4.1.2.2 Regaining Functional Amplitudes
It requires a good knowledge of the constraints transmitted to the scaphoid depending on the joint sector [16].
In flexion-extension, the ligaments are relaxed and the joint pressure minimal until 20°, to become significant at 40°. After that, the pressures increase to reach their maximal value around 80°. After 80°, they become pathogenic [6] (Fig. 3.9).
The normal amplitude in radial inclination is 15°. It induces compressive constraints on the scaphoid that tilts in flexion, which can encourage the formation of a vicious callus [17], closing the intrascaphoidal sagittal angle.
The normal amplitude in ulnar inclination is 45°. It creates traction constraints on the scaphoid that tilts in extension. The formation of a vicious callus [17] when the intrascaphoidal sagittal angle is open is rarer, but can happen.
Like for the fractures of the inferior extremity of the radius, these elements allow defining “risky” areas in which the exercises to regain amplitude will have to be realized very cautiously, without any force.
These areas are after 20° in flexion/extension and ulnar inclination and from 5° in radial inclination.
Trying to regain total amplitudes at all costs is, in this phase, useless and dangerous.
We use the same techniques than in fractures of the inferior extremity of the radius:
-
Fluidotherapy to relax the muscles and tissues. We use it at the beginning of the session to warm up the wrist.
-
Passive manual mobilizations are basic exercises to regain joint amplitude. They’re soft and pain-free and can be realized increasing the joint spaces a little. We work in all the authorized sectors, being particularly careful in extension and radial inclination where the constraints on the scaphoid are more important.
-
Active mobilizations are realized after the passive ones, in various finger positions to improve tendinous glidings at the level of the wrist (Fig. 3.10).
-
Active-assisted mobilizations can be assisted by an arthromotor. We ask the patient to participate actively in the movements applied by the device. This exercise is realized in amplitudes previously regained by the therapist in passive. It has an interest at the joint level, but also in draining the edema. It can be combined with icing (Fig. 3.11 and 3.11′).
-
Electrostimulation, combined with an active movement (winding the fingers), can help regaining the last degrees of mobility in finger flexion if necessary (Fig. 3.12). The patient mustn’t clutch his fingers as it would put important constraints on the scaphoid.
4.1.2.3 Muscular Awakening and Reinforcement for the Stabilizing Muscles
Muscular awakening is realized with exercises with energy overload, which can be used at first to progressively stimulate atrophic muscles.
“Trigger” muscles are part of the intrinsic musculature to avoid increasing the longitudinal constraints of the carpus on the forearm [16]:
-
Abductor pollicis brevis – pronator quadratus (Fig. 3.13)
-
Flexor digiti minimi – flexor carpi ulnaris (Fig. 3.14)
-
Thenar and hypothenar muscles – flexor carpi radialis (Fig. 3.15)
-
Abductor digiti minimi and thumb extensors – ulnar and radial carpal stabilizers (Fig. 3.16) [18]
The reinforcement protocol itself starts when the previous exercises are easily realized by the patient.
All the exercises are realized with the fingers in extension, the limit the axial constraints increased by the contraction of the finger flexors when clamping (Fig. 3.17).
The first solicited energy system is the aerobic one as it’s the least constraining at the muscular and articular level.
“Pure” aerobic exercises can’t be realized in this phase as the patient would be asked to realize long contraction (10–15 min), which in this phase would lead to tendinous and muscular disorders, as well as important pain. Therefore, we use static intermittent exercises adapted to the wrist’s functional biomechanics, the relative fragility of the callus, and the wrist muscles’ physiology.
At the beginning of the phase, we ask for low-intensity static contractions with series of 30 repetitions, held 6 s, and with 6 s of rest between the repetitions. The ideal contraction intensity is 20–30 % of the maximal strength, but as it can’t be assessed in this phase, it’s controlled by the therapist or the device.
We can’t use the contralateral side to determine the usual strength of the injured side as there are often important differences between the 2 sides of a patient.
The parameters (number of repetitions, contraction duration, and modalities) evolve during the treatment, adapting to the patient’s capacity and osseous consolidation.
A contraction with maximal resistance or clamping is never asked.
Dynamic contractions with wide amplitudes aren’t in relation with the physiological role of the wrist orient and stabilize the hand during prehensions). Therefore, they’re not included in the reinforcement protocol (except if there’s a particular indication).
We realize a static reinforcement of the 4 sides of the wrist, with the wrist in a neutral position and the fingers in extension.
4.1.2.3.1 Wrist Flexors
The flexor carpi radialis passes in front of the radial epiphysis and the scaphoid. It forms the most powerful active complex stabilizing the radial column, along with the radial extensors (Fig. 3.18).
The flexor carpi ulnaris passes in front of the ulnar head and ends on the pisiform. It produces expansions towards the anterior retinacular ligament, the hamate, and the 4th and 5th metacarpals. It’s prolonged along the internal column by the adductor digiti minimi. It forms the most powerful active complex stabilizing the ulnar column, along with the extensor carpi ulnaris (Fig. 3.19).
During these exercises, the flexor carpi radialis and ulnaris work in synergy, and the action of the finger flexors is limited as we place the fingers in extension.
We work with the espalier, with a contraction against an elastic band (moderate resistance). At the beginning of this rehabilitation phase, the patient brings the elastic band in the working position with his contralateral hand, to realize a pure static exercise.
The exercise is then realized only with the damaged side to alternate stato-concentric, static, and stato-eccentric contractions against a controlled resistance.
A visual feedback allows the patient to control the contraction and rest phases (Fig. 3.20).
Manually, the resistance is placed at the level of the palmar side of the metacarpal diaphyses, stabilizing the forearm with the contralateral hand. This grip allows us in controlling the osseous callus and limits the compression and shearing constraints imposed on it.
A digital grip with the fingers in extension is also possible (Fig. 3.21).
An ulnar or radial inclination can be asked to work with the flexor carpi ulnaris or radialis.
4.1.2.3.2 Wrist Extensors
The extensor carpi radialis longus and brevis pass on the posterior side of the radial styloid process and in the anatomical snuffbox, before ending, respectively, on the posterior side of the 2nd and 3rd metacarpals. They participate in stabilizing the radial column, along with the flexor carpi radialis (Fig. 3.22).
The extensor carpi ulnaris passes with the extensors between the styloid process and the ulnar head before ending on the 5th metacarpal’s posterointernal tubercle. It participates in stabilizing the ulnar column, along with the flexor carpi ulnaris.
The abductor pollicis longus and extensor pollicis brevis stabilize the radial column, but their analytical contraction is moderate in this phase as there are important risks of tendinopathy.
We use the espalier with an elastic band, according to the same modalities than for the wrist flexors, and always with visual feedback (Fig. 3.23).
Manually, the resistance is placed at the level of the dorsal side of the metacarpal diaphyses, stabilizing the ulnar side of the wrist with the contralateral hand (Fig. 3.24).
As for the reinforcement of the wrist flexors, we can associate a radial or ulnar inclination to work with the extensor carpi radialis or ulnaris.
4.1.2.3.3 Ulnar Stabilizers
The extensor and flexor carpi ulnaris can work in synergy in an exercise with the espalier (Fig. 3.25).
Manually, we can ask for a direct contraction against resistance at the level of the ulnar side of the carpus (triquetrum, hamate, and 5th metacarpal), stabilizing the scaphoid with the contralateral hand (Fig. 3.26).
Another exercise consists in working with the abductor digiti minimi brevis as it’s in continuity with the flexor carpi ulnaris.
4.1.2.3.4 Radial Stabilizers
The opposite exercise is proposed to solicit preferentially the wrist radial stabilizers. Resistances are placed on the radial side of the 2nd metacarpal to reduce the contraction of the thumb muscles.
This exercise is realized very carefully, and the patient is forbidden to mobilize his wrist in radial inclination during the contraction (Fig. 3.27).
4.1.2.3.5 Intrinsic Muscles
The contraction of the intrinsic muscles doesn’t produce important axial constraints, unlike the contraction of the extrinsic muscles (Fig. 3.28).
We’ll reinforce preferentially the interossei, the flexor pollicis brevis, and the adductor pollicis.
We ask the patient to realize a “vise” pinch against resistance, with visual feedback to manage the duration of contraction and rest (Fig. 3.29).
The same exercise can be realized manually.
The opposition arch between the thumb and the 5th finger can also be solicited manually (Fig. 3.30).
4.1.2.3.6 Electrostimulation
Combined with an active contraction of the stimulated muscles, it improves motor recruitment and maintains body mapping, thus participating in the active wrist stabilization.
It can concern intrinsic or extrinsic muscles (Fig. 3.31).
Note: even if these techniques are the same as in fractures of the inferior extremity of the radius, there are some variations. We’ll particularly insist on regaining strength in the radial muscles (flexor carpi radialis and radial extensors) that are important stabilizers of the scaphoid.
4.1.2.4 Prehensions
We work on prehensions to improve coordination and dexterity and therefore improve functional capacities in daily activities.
These exercises are realized without clamping or putting excessive constraints on the scaphoid.
For example, clamping a ball is forbidden (Fig. 3.32).
4.1.2.5 Proprioception
In this phase, these exercises are only realized if there is no pain or trophic disorders. They improve the patient’s proprioception without risk for the callus healing.
4.1.2.5.1 Table Tennis Racket
We ask the patient to maintain the ball on the racket, which implies a good sensorial analysis and a contraction adapted to the received informations.
Progressively, we ask the patient to throw the ball and receive it “softly” on the racket.
4.1.2.5.2 Exercises with a Plastic Ball
We use a light plastic ball and ask the patient to pass it from one hand to the other, to throw and catch it.
4.1.3 Consolidation (After D90 with Surgery, After D120 Without Surgery)
When the scaphoid is solid, we can start more intensive techniques (never aggressive).
In this phase, we aim to regain strength and wrist amplitudes. Rebalancing force ratios between the different muscular groups limits the risks of secondary tendinopathy.
Prehension and proprioception exercises help the patient in regaining the functionality he’ll need in his work and sports activities.
4.1.3.1 Regaining Wrist Amplitudes
We keep realizing techniques from the previous phase and intensify them if necessary (pain-free) to completely regain the wrist amplitudes.
We use specific peri-scaphoidal mobilization techniques.
4.1.3.1.1 Specific Mobilizations
They require a good knowledge of the morpho-palpatory anatomy [12] and the radio-carpal and intracarpal biomechanics [12, 18]. Tractions glidings are realized between the radius and the 1st carpal row, between the 1st and 2nd carpal row, and between the scaphoid and the adjacent bones, insisting on the lunate with which it forms a pair essential in the good functioning of the wrist (cf. Chap. 4).
We realize mobilizations between the radius and the carpus and between the 2 carpal rows (described in the Chap. 5), to which we add analytical mobilizations between the scaphoid and the adjacent bones:
4.1.3.1.2 Mobilization Scaphoid/Radius
The patient keeps the wrist in a neutral position to avoid limiting mobility with the reduction of the space between the trapezo-trapezoidal joint and the radius during radial inclination or the tension in radial ligaments during ulnar inclination.
The scaphoid is maintained between the therapist’s thumb and index, with the thumb on the scaphoid’s tubercle and the index on the posterior side of the proximal part.
The other hand maintains the radius, and we apply anteroposterior glidings on the scaphoid (Fig. 3.33).
4.1.3.1.3 Mobilization Scaphoid/Lunate
The wrist is still in a neutral position; the patient places his forearm in pronation.
The scaphoid is maintained by the radial hand between the thumb (dorsal side of the proximal part) and the index (tubercle). The lunate is maintained by the ulnar hand between the thumb (dorsal side) and the pulp of the other fingers (palmar side). Each hand applies an opposite gliding to obtain maximal movement (Fig. 3.34).
4.1.3.1.4 Mobilization Scaphoid/Trapezium
In the same position than for the mobilization scaphoid/lunate, the scaphoid is maintained the same way and the trapezium is between the thumb (dorsal side) and the index (palmar side). We apply a differential gliding on each bone in a direction oblique backward and outward or frontward and inward, with the scaphoid oriented frontward and outward.
4.1.3.2 Muscular Reinforcement
The scaphoid is healed so the muscular reinforcement can be realized with no other limit than the pain threshold and the progression of the techniques.
We use the same techniques as in the previous phase with more important loads, to regain strength comparable to the same side.
Chain work is realized according to the patient’s functional needs (Fig. 3.35 and 3.35′). The assessment of the muscular ratios is essential, and we often observe weakness in the radial and extrinsic elements in relation with the ulnar and intrinsic ones. This difference is probably related to the limits imposed in the other phases to protect the scaphoid:
-
Using a load cell and visual feedback allows accurately targeting the solicited energy system, modifying the load and duration of contraction and rest. The reinforcement is realized in flexion-supination and extension-pronation to improve muscular capacities and regain muscular balance, comparable to the same side (Fig. 3.36). If a comparison with the same side can’t be done, our experience has determined that strength in flexion-supination is 1.8 times more important than strength in extension-pronation in men and 2.6 times in women.
-
Using a dynamometer combined with a device allows regulating the duration of contraction and rest, with visual feedback to target the solicited energy system, reinforce and rebalance the pronators and supinators (Fig. 3.37). The same kind of device is used for the radial and ulnar stabilizers (Fig. 3.37′).
Fig. 3.37 -
Global exercises for the superior limb can be done too, realizing a controlled contraction with visual feedback of the ulnar (Fig. 3.38) or radial stabilizers, and the wrist flexors (Fig. 3.39) and extensors.
-
Using weights solicits flexors/extensors in half-open chain (Figs. 3.40 and 3.40′). It allows alternating concentric, static, and eccentric contractions whose parameters evolve depending on the patient’s functional needs.
-
Using a hammer solicits pronators/supinators in half-open chain (Fig. 3.41). Like with weights, we can alternate different contractile modes and the parameters evolve depending on the patient’s functional needs and progress.
-
Using a minibike in active mode improves the wrist flexors and extensors’ endurance. The resistance and exercise duration evolve, adapting to the patient’s needs and capacities (Fig. 3.42).
-
Support exercises to work in closed chain (Fig. 3.43).
-
Techniques using digito-antebrachial chains can be realized manually or instrumentally (Fig. 3.44).
-
Electrostimulation can be associated with every exercise previously described, adapting the program to the energy system we want to work with.
4.1.3.3 Proprioception and Feedforward
It’s essential in the functional recovery for the wrist and can be realized manually or with instrumental techniques.
We use exercises with oscillating poles, medicine balls, and rhythmical stabilization:
-
Multidirectional proprioception and feedforward pressing on a plastic ball first poorly inflated and then progressively more inflated (Fig. 3.45).
-
Rhythmical stabilization with an oscillating pole (Fig. 3.46).
-
Exercises passing a weighted ball from one hand to the other, throwing and receiving it. We progressively increase the weight (Fig. 3.47).
4.1.3.4 Prehensions
We realize exercises to improve the types of prehensions the patient will need in his daily activities, work, and sports.
4.2 Orthotic Treatment
The orthotic treatment evolves in parallel in relation with the rehabilitation protocol:
4.2.1 Immobilization
It can be a cast or made of resin, but we prefer using perforated thermoformable plastic (2,4mm thick) to realize a non-removable orthosis.
We obtain a precise immobilization, 8 times lighter than with resin, that can go in water (if there is no wound), radiolucent, and with perforations that allow the skin to “breathe.”
As described in the chapter about immobilization, recent studies tend to demonstrate that letting the thumb free doesn’t affect the healing process, so we realize orthosis leaving the thumb free (Fig. 3.48).
4.2.2 Pre-consolidation
It’s not realized all the time, but a resting orthosis can be useful in case of nocturnal pain or in daily activities.
However, we make sure the patient gets progressively rid of the orthosis without impeding his functional evolution.
The orthosis lets the thumb free and maintains the wrist in a neutral position. The plastic is perforated and its thickness depends on the patient’s morphology (Fig. 3.49).
4.2.3 Consolidation
A neoprene orthosis can be realized to go back to professional or sports activities. It protects the wrist from shocks and has an interesting contention effect, useful at a proprioceptive level and in the patient’s apprehension. It is most of the times a wrapped on cuff and thermoformed plastic reinforcements can be added depending on the indications (Fig. 3.50).
5 Complications
Other than the usual complications related to surgery and immobilization, pseudoarthrosis is the main complication in fractures of the scaphoid [19].
They are more frequent in case of insufficient initial treatment, displaced fractures, or fractures localized in the proximal part, which vascularization is precarious.
The treatment for pseudoarthrosis is surgical, most often realizing a bone graft from the hip bone or the radial epiphysis. The goal is to avoid the evolution towards an SNAC wrist. The rehabilitation after a graft uses the same principles as in simple fractures, modifying the durations depending on the case and the surgeon’s indications.
Remember
-
The scaphoid is a bone whose healing can be difficult as it is poorly vascularized, with important risks of pseudoarthrosis (proximal part).
-
Compressive constraints must be avoided during the whole healing phase.
-
The protocol is a lot like the one for fractures of the inferior extremity of the radius, but it’s often more intense and centered around reinforcement and proprioception.
Bibliography
Schernberg F (2005) Fractures récentes du scaphoïde (moins de 3 semaines). Chir Main 24:117–130
Berger RA (2001) The anatomy of the scaphoid. Hand Clin 17(4):525–532
Nakamura R (2000) Scaphoid mal-union — current concept and perspectives. Hand Surg 5(2):155–160
Herbert T (1990) The fractured scaphoid. Quality medical publishing Inc, St-Louis
Merle M (ed) (2009) La main traumatique, vol 2. Elsevier Masson, Issy-les-Moulineaux, p 379
Schernberg F, Harisboure A, Gaston E (2000) Fractures des os du carpe. In: Masson E (ed) EMC appareil locomoteur, Elsevier, Paris pp 14-046-B-10
Schubert HE (2000) Scaphoid fracture. Can Fam Physician 46:1825–1832
Weber E (1980) Biomechanical implications of scaphoid waist fractures. Clin Orthop 149:83–89
Herzberg G, Foissier D, Falaise C (2003) Coronal fractures of the proximal scaphoid: the proximal ring sign. J Hand Surg 28B:500–503
Dickson R, Leslie IJ (1982) Traitement orthopédique des fractures du scaphoïde carpien. Monographie du GEM. Le poignet. Ed.Expansion scientifique Française - Paris. pp 82–95
Toh S, Nagao A, Harata S (2000) Severely displaced scaphoid fracture treated by arthroscopic assisted reduction and osteosynthesis. J Orthop Trauma 14:299–302
Tubiana R, Thomine J-M (1990) La main anatomie fonctionnelle et examen clinique, Masson
Holley B (2009) Intérêt de l’arthroscopie dans le traitement par vissage percutané des fractures du scaphoïde carpien, analyse retrospective de 31 cas
Schadel-Hopfner M, Bohringer G, Gotzen L (2000) Percutaneous osteosynthesis of scaphoid fracture with the Herbert-Whipple screw-technique and results. Handchir Mikrochir Plast Chir 32:271–276
Brutus JP, Baeten Y, Kinnen L, Moermans JP, Ledoux P (2002) Ostéosyn- thèse percutanée des fractures du scaphoïde par la vis de Herbert: revue de 30 cas. Chir Main 21:350–354
Horii E, Garcia-Elias M, Bishop AT et al (1990) Effect on force transmission accross the carpus in procedures used to treat Kienboock’s disease. J Hand Surg 15A:393–400
Saffar P (2008) Cal vicieux du scaphoïde. Chir Main 27(2–3):65–75
Kuhlmann JN (2002) La stabilité et les instabilités radio- et médio-carpiennes. Sauramps médical, Montpellier
Herzberg G (ed) (2006) Arthrose péri-scaphoïdienne. Sauramps medical, Montpellier, p 340
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Mesplié, G., Grelet, V. (2015). Recent Fractures of the Scaphoid Bone. In: Hand and Wrist Rehabilitation. Springer, Cham. https://doi.org/10.1007/978-3-319-16318-5_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-16318-5_3
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16317-8
Online ISBN: 978-3-319-16318-5
eBook Packages: MedicineMedicine (R0)