Abstract
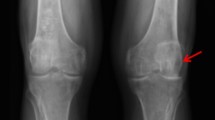
Alkaptonuria (AKU) is a rare inherited disease caused by defects of the enzyme homogentisic acid dioxygenase, resulting in the accumulation of homogentisic acid in the body and its excretion in the urine. Its polymer, a yellow-black ochronotic pigment, deposits in cartilage and connective tissue, especially in the skin, visceral organs, eyes and ears causing their pigmentation (ochronosis). From the clinical point of view, the most serious pigmentation is in joints, causing ochronotic arthropathy which usually results in severe disability. It is a degenerative process that primarily affects the spine (causing calcification of intervertebral discs) as well as large joints (Rovensky and Urbanek 2003).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Alkaptonuria (AKU) is a rare inherited disease caused by defects of the enzyme homogentisic acid dioxygenase, resulting in the accumulation of homogentisic acid in the body and its excretion in the urine. Its polymer, a yellow-black ochronotic pigment, deposits in cartilage and connective tissue, especially in the skin, visceral organs, eyes and ears causing their pigmentation (ochronosis). From the clinical point of view, the most serious pigmentation is in joints, causing ochronotic arthropathy which usually results in severe disability. It is a degenerative process that primarily affects the spine (causing calcification of intervertebral discs) as well as large joints (Rovenský and Urbánek 2003).
In the catalogue of inherited diseases “Mendelian Inheritance in Man” (MIM), the code for AKU is MIM 203 500 (www.ncbi.nlm.nih.gov/omim/). From the historical point of view, it was the first inherited disease in man, which Sir Archibald Garrod identified as following Mendelian inheritance determined by a simple recessive factor (Garrod 1902). He ranked it among those inherited metabolic disorders caused by the defect of a specific enzyme in spite of the fact that he did not know its molecular nature at that time. AKU is a monogenic disease with autosomal recessive inheritance, i.e. it is determined by one gene that is located on some of the homologous chromosomes of man – autosomes (chromosomes 1–22). In a classical case of this type of inheritance, both parents are usually healthy, but they are carriers of a pathological allele (healthy carriers – heterozygotes); the risk of children who are recessive homozygotes is 25 % and they will suffer from the disease. Fifty percent of children are healthy, but they are carriers of the pathological allele and 25 % of children are healthy and they are not carriers. In the case of a marriage between a patient with AKU and a healthy carrier, the risk of affected children increases to 50 %. The first mathematical-statistical proof of autosomal recessive inheritance of AKU was provided by Hogben et al. in 1932 (Hogben et al. 1932).
In 1958, La Du with his co-workers (La Du et al. 1958) found out that the biochemical principle of AKU is based on the absence of biological activity of the enzyme homogentisate 1,2-dioxygenase (HGD) in the liver, thus confirming the original assumption of Garrod that it is a metabolic disorder. HGD (MIM 607 474, older term HGO) is the enzyme that participates in the catabolism of phenylalanine and tyrosine (EC 1.13.11.5). Its molecular weight is 50 kDa and it consists of 445 amino acids. It is specific for homogentisic acid and it does not oxidize similar substances like gentisic acid or phenylacetic acid (Schmidt et al. 1997). The gene that codes for the enzyme HGD was cloned in 1996 (Granadino et al. 1997), starting the era of study of AKU molecular genetics. Currently we know that the HGD gene is a single-copy gene (Fernandez-Canon et al. 1996; Granadino et al. 1997). It consists of 14 exons (coding parts of the gene) and 13 introns (non-coding parts of the gene). The complete length of nucleotide sequence is 54,363 bp (base pairs), whilst the coding part of the gene represents only 3 % of its length (1,715 bp). The length of exons ranges from 35 to 360 bp (Genbank sequence NM 000187.2). Repetitive elements represent approximately 26 % of the gene sequence. HGD gene expression is tissue specific; it is found especially in the liver and kidney, with a much lower expression in the small and large intestine, prostate and brain (Fernandez-Canon et al. 1996). Increased activity in the liver and kidney is attributed to the metabolic activity of these organs. In the brain, HGD probably participates in the degradation of amino acids derived from neurotransmitters which often contain aromatic amino acids. In other studied tissues like blood, germinal epithelium, muscles and salivary glands, significant activity of the enzyme was not found (La Du 1989). In 1994, the HGD gene was localized on the long arm of chromosome 3 in man (3q). In the next years, its localization on chromosome 3 was specified more precisely to 3q13.33 using polymerase chain reaction (PCR) and fluorescence in situ hybridization (Fernandez-Canon et al. 1996).
Molecular genetic studies in AKU brought the surprising finding that the HGD enzyme defect is not caused by only one mutation as it was originally anticipated, but by several mutations that are localized in coding as well as in non-coding parts of HGD gene. The first proof that enzymatic loss in AKU is caused by a mutation within the HGD gene was presented by Fernandez-Canon et al. 1996 in a Spanish population. In 2000, in a set of more than 100 patients coming from several countries worldwide, more than 40 various mutations causing AKU were identified (Beltrán-Valero de Bernabé et al. 1999; Porfirio et al. 2000; Zat´ková et al. 2000a, b, c). More recently at least 116 mutations and 33 HGD polymorphisms have been encountered (Introne et al. 2009; Grasko et al. 2009; Abdulrazzaq et al. 2009; Oexle et al. 2008; Zat´ková et al. 2000a, b, c; Zat´ková 2011; Sakthivel et al. 2014). AKU-causing mutations are distributed throughout the entire HGD gene with a somewhat higher prevalence in exons 6, 8, 10 and 13 (Fig. 7.1). Missense mutations are the most numerous with 77/115 (66.37 %), followed by an equal number of small deletions and insertions causing frameshift and splicing mutations, each in 14/115 (12.2 %), and then nonsense mutations in 7/115 (6 %). The 23 most frequent mutations are present in 361 out of 496 (72.8 %) AKU chromosomes observed worldwide (Zat´ková 2011). There are about 30 AKU chromosomes reported in which no HGD mutation was identified (Aquaron et al. 2009; Beltrán-Valero de Bernabé et al. 1998; Ladjouze-Rezig et al. 2006; Mannoni et al. 2004; Muller et al. 1999; Phornphutkul et al. 2002; Vilboux et al. 2009). These chromosomes might carry deep intronic mutations affecting splicing that could not have been identified when only exons with short neighbouring intronic parts were analysed in the patients. They might carry mutations in the promotor region or in other cis regulatory sequences that also have not been captured using classic mutation detection methods. The most frequent mutation in Europe representing about 20 % of the mutations is Met368Val (replacement of methionine by valine at position 368), whilst in the Dominican Republic it is Cys120Trp and in Slovakia it is IVS2 + 1G → A. No typical pattern was found in the USA. It has to be noted that the majority of mutations are rare, and they are characteristic for a certain location or family (www.cib.csic.es/~akudb/index.htm). Beltrán-Valero de Bernabé et al. (1998) showed in 1998 that patients from different countries who shared the same mutations – M368V, V300G or P230S – also shared the same haplotype. Alternatively, haplotypes differed among these patients only in regions distal to the mutation position; thus, the differences could be explained by recombination events. The authors concluded these were most likely old mutations introduced to Europe with the founder populations, and they have spread throughout Western Europe along with different migrations. The “CCC” sequence motif and its inverted complement, “GGG”, are preferentially mutated (Beltrán-Valero de Bernabé et al. 1999). Subsequently, nucleotide c.342 + 1 G was also described as a mutational hot spot in HGD (Zat´ková et al. 2000a, b, c). Although most of the mutant enzymes showed a complete lack or very low levels of enzyme activity, five mutations led to specific activity that was 22–37 % of the wild type (E42A, Y62C, A122D, D153G and M368V). So far, no apparent correlation between the type of mutation and excretion of homogentisic acid in urine or severity of the disease has been found (Phornphutkul et al. 2002; Goicoechea et al. 2002; Uyguner et al. 2003; Ladjouze-Rezig et al. 2006; Zat´ková 2011). As a consequence of the large number of mutations, patients with AKU can have two different mutations on a given locus, i.e. he/she is a heterozygote. As both alleles are not functional, such a condition is called compound heterozygous. It means that a patient with AKU is not always a recessive homozygote as it is understood according to the original classical conception of the genetic determination of this disease.
Distribution of AKU mutations in the HGD gene (Zat´ková 2011). 1–14 exons, Kb kilobase. Variants IVS9-56G>A** and IVS9-17G>A** were published as mutations, but (Vilboux et al. 2009) reported that they are most likely benign variants. Mutations G115fs* and V157fs* are caused by genomic deletions which are predicted to cause exon 6 and 8 skipping, respectively, thus leading to frameshift and preliminary stop of translation (Zat´ková 2011)
In Slovakia, within the rather relatively small population of 5.5 million, 208 patients have been registered (Sršeň et al. 2002) and a total of 12 different HGD mutations have been established, revealing a remarkable allele heterogeneity of AKU in this country. An allelic association was performed for 11 HGD intragenic polymorphisms in a total of 69 AKU chromosomes from 32 Slovak pedigrees. These were then compared to the HGD haplotypes of all AKU chromosomes carrying identical mutations characterized thus far in non-Slovak patients in order to study the possible origin of these mutations (Zat´ková 2011). Based on the analysis and comparison of haplotypes, two groups of HGD mutations were observed in Slovakia. To the first group belong mutations P230S, V300G, S59fs (R58fs), M368V and IVS1-1 G > A, which account for 17.3 % of the Slovak AKU chromosomes and thus provide a marginal contribution to the AKU gene pool in this country. The most frequent European mutation, M368V, is present in one copy in only two unrelated Slovak families. Mutations of this group are shared by different populations and have most likely been introduced into Slovakia by the founder populations that spread throughout Europe (Zat´ková et al. 2000a, b, c). The second group consists of the remaining seven mutations established in 82.7 % of Slovak patients. These include the most prevalent G161R (44.2 %), D153fs (G152fs) (14.4 %), H371fs (P370fs) (11.5 %) and G270R (7.7 %), as well as IVS5 + 1 G > A present on three AKU chromosomes and the S47L and E178G mutations observed each in only one patient. It is likely that mutations from this second group originated in Slovakia. The distribution of the identified mutations within Slovak territory is also interesting. As previously reported, examination of the geographical origin of Slovak AKU mutations shows remarkable clustering in a small area in northwest Slovakia, with these mutations most likely originating in this area and spreading into other regions after the breakdown of genetic isolates in the 1950s (Zat´ková et al. 2000a, b, c). As the combined sequence and haplotype analysis shows, 7 of the 12 AKU mutations (58.3 %) that most likely originated in Slovakia are associated with hypermutated sequences in the HGD, whilst worldwide it is 40/115 (34.8 %). Therefore, it is possible that an increased mutation rate in the HGD gene in a small geographical region is responsible for the high genetic heterogeneity in Slovak AKU (Zat´ková et al. 2000a, b, c). However, it remains unclear which mechanism acted specifically on the HGD gene to increase its mutation rate, since similar targets are also present in other genes without evident elevated gene frequency in Slovakia (Sršeň et al. 2002; Zat´ková et al. 2000a, b, c). The increased number of mutations could also be the result of random accumulation of mutations in the region. It has been suggested that the Valachian colonization during the fourteenth to seventeenth centuries may also have played a role in the increased prevalence of AKU in Slovakia (Sršeň et al. 2002; Zat´ková et al. 2000a, b, c). The preservation of the most prevalent AKU variants, which either arose in Slovakia or were brought there, may be the result of a founder effect and genetic drift, due to the geographic isolation of villages in northwest Slovakia.
AKU belongs to rare diseases from the point of population genetics. Only slightly over 1,000 cases have been reported in the literature. The worldwide prevalence of AKU is not precisely known; it is estimated to be 1:250,000–1,000,000 (Beighton et al. 1993). However, it has got wide ethnic and geographic distribution. Its occurrence has been reported in various populations in Europe, America and Asia, i.e. this disease is not restricted to a certain race, but it affects individuals of various ethnic groups. It is interesting that AKU occurrence was not observed in the Gypsy ethnic group in Slovakia. Findings of typical ochronotic spondylosis in Egyptian mummies dated about 1500 B.C. suggest its occurrence in the ancient past (Beighton et al. 1993). The highest worldwide incidence of AKU is found in the Dominican Republic and Slovakia. For example, overall 149 patients were registered in Slovakia in the 1980s. A 6-year screening of the newborn population in Slovakia (417,122 newborns who survived the first 4 weeks of life) revealed about 1:19,000 incidence (Sršeň 1984). In certain regions of Slovakia, the disease incidence was up to ten times higher. These regions developed for a long time (until World War II) as genetic isolates, e.g. Kysuce, Orava and surroundings of Trenčín and Horehronie – the inbreeding coefficient (F) ranged from 0.003 to 0.029 (Sršeň 1984). The higher AKU incidence in these regions is probably a consequence of their long-term geographic isolation and endogamy, in addition to such genetic factors like genetic drift and founder effect. Break-up of isolates after World War II resulted in the gradual decrease of AKU incidence in Slovakia. On the basis of genetic population analyses, the frequency of gene/allele for AKU in Slovakia was estimated to be 0.7 % – q = 0.007 (Sršeň 1984). This value is relatively high, but in contrast to AKU frequency, it will not be significantly affected by break-up of isolates. On its basis, it is possible to perform certain genetic estimates that are not accurate with regard to several factors, which have to be taken into account in population analyses. However, they enable us to obtain several data of orientation value that can be useful from a practical point of view. On the basis of these estimates, there could be more than 250 patients with AKU in the whole current population of Slovakia (about 5.5 million citizens). The frequency of heterozygotes, i.e. healthy carriers of the pathological allele, would be approximately 14 persons per 1,000, and two matrimonies out of 10,000 would carry the risk of 25 % of two healthy heterozygotes having children with AKU. It has to be emphasized that in the case of consanguineous marriages or marriage of the people who come from the above-mentioned endogamous locations, the risk of AKU incidence in children is even higher. These data demonstrate that AKU problems and of course subsequent ochronosis and ochronotic arthropathy are topical in the Slovak population even nowadays and attention has to be paid to this disease.
With regard to the aforementioned frequent incidence of AKU in the Slovak population, it has been the subject of long-term research. Four institutions in Slovakia were devoted to its study – National Institute of Rheumatic Diseases in Piestany, Institute of Clinical Genetics of Jessenius Medical Faculty of Comenius University in Martin, Institute of Molecular Physiology and Genetics of Slovak Academy of Sciences in Bratislava and Faculty of Natural Sciences of Comenius University in Bratislava. The following years are important from the historical point of view:
-
1947 – The first reported case of AKU and ochronosis in Slovak population (Sit´aj 1947).
-
1956 – The first monograph on AKU in world literature was published in Slovakia (Sit´aj et al. 1956).
-
1950–1960 – There were 182 cases of AKU found in Slovak population (four million citizens). The patients came from 28 families. It was the largest group of patients worldwide (Červeňanský et al. 1959).
-
1966 – Hüttl et al. described inclusions of ochronotic pigment in the cytoplasm of synovial fluid cells (Hüttl et al. 1966).
-
1974–1984 – Large population studies were performed in Slovakia. Their results are summarized in the second monograph on AKU (Sršeň 1984).
-
1980–1981 – An analysis of 90 families with AKU occurrence confirmed an autosomal recessive type of inheritance in Slovak population (Kaprálik and Sršeň 1980).
-
1993–1994 – AKU gene was localized on the long arm of chromosome 3 in humans (3q). Slovak authors also contributed to this discovery (Janocha et al. 1994).
-
1994–2000 – Molecular characterization of mutations in HGD gene in Slovak population (Zat´ková et al. 1999, 2000a, b, c).
Advances in the field of AKU molecular genetics contributed not only to a better understanding of the disease etiopathogenesis, but they were also significant from a practical point of view as they enabled disease diagnostics at DNA (gene) level which gives a high-quality definitive diagnosis. DNA analysis can be used for identifying healthy carriers of the pathological allele (heterozygotes), which was not possible by biochemical methods. This knowledge can be used in genetic counselling. Knowledge of the molecular-genetic basis of AKU is very promising for the development of new approaches to the therapy of this disease which is currently aimed at symptomatic treatment of some complications and is not always effective. Two options of causal therapy are possibilities – substitute administration of HGD enzyme and gene therapy at the level of the somatic cell. Direct administration of the enzyme faces several problems, especially its localization in the liver, but also the route, the dose and the period and interval of administration. The most convenient option would be the application of the so-called recombinant enzyme. An example of such replacement enzymatic therapy is Gaucher’s disease. Somatic gene therapy currently moves from animal studies to clinical trials in humans, e.g. in phenylketonuria. The normal functional gene is given to the patients using a suitable vector. According to current knowledge and experience with gene therapy, it is sufficient to achieve 5 % expressivity of the gene in order to yield its curative effect. Such an approach is supported by the recent results of a liver transplantation in an AKU patient in whom the progression of clinical and radiological changes was stopped, because hepatocytes of the transplanted liver had a functional HGD gene (Kobak et al. 2005). Gene therapy is a great hope for AKU patients because we still cannot treat this disease, which often causes disability and considerable suffering. Several other treatment strategies have also been suggested for AKU including nitisinone, the triketone herbicide, which inhibits the 4-hydroxyphenylpyruvate dioxygenase enzyme that produces HGA (Suwannarat et al. 2005).
References
Abdulrazzaq, Y.M., Ibrahim, A., Al-Khayat, A.L., Nagelkerke, N., Ali, B.R.: R58fs mutation in the HGD gene in a family with alkaptonuria in the UAE. Ann. Hum. Genet. 73, 125–130 (2009)
Aquaron, R., Rodríguez de Córdoba, S., Penalva, M.A., Badens, C., Roux, H.: Alkaptonuria, ochronosis and ochronotic arthropathy in mainland France and the Reunion Island. A report of clinical and molecular findings. Curr. Rheumatol. Rev. 5, 111–125 (2009)
Beighton, P., Berman, P., Sršeň, Š.: Alkaptonuria. In: McKusick’s heritable disorders of connective tissue, 5th edn, pp. 315–334. Mosby, St. Louis (1993)
Beltrán-Valero de Bernabé, D., Granadino, B., Chiarelli, I., Porfirio, B., Mayatepek, E., Aquaron, R., Moore, M.M., Festen, J.J., Sanmartí, R., Penalva, M.A., de Córdoba, S.R.: Mutation and polymorphism analysis of the human homogentisate 1, 2-dioxygenase gene in alkaptonuria patients. Am. J. Hum. Genet. 62, 776–784 (1998)
Beltrán-Valero de Bernabé, D., Jimenez, F.J., Aquaron, R., Rodríguez de Cordoba, S.: Analysis of alkaptonuria mutations and polymorphisms reveals the CCC sequence motif is mutational hot spot in the homogentisate 1,2 dioxygenase gene. Am. J. Med. Genet. 64, 1316–1322 (1999)
Červeňanský, J., Sit´aj, Š., Urbánek, T.: Alkaptonuria and ochronosis. J Bone Joint Surg 41, 1169–1182 (1959)
Fernandez-Canon, J.M., Granadino, B., Beltrán-Valero de Bernabé, D., Renedo, M., Fernández-Ruiz, E., Penalva, M.A., Rodriguez de Cordoba, S.: The molecular basis of alkaptonuria. Nat. Genet. 14, 19–24 (1996)
Garrod, A.E.: The incidence of alkaptonuria: a study in chemical individuality. Lancet 2, 1616–1620 (1902)
Goicoechea de Jorge, E., Lorda, L., Gallardo, M.E., Pérez, B., Pérez de Ferrán, C., Mendoza, H., Rodriguez de Córdoba, S.: Alkaptonuria in the Dominican Republic: identification of the founder AKU mutation and further evidence of mutation hot spots in the HGO gene. J. Med. Genet. 39, E40 (2002)
Granadino, B., Beltrán-Valero de Bernabé, D., Fernández-Canón, J.M., Penalva, M.A., Rodriguez de Córdoba, S.: The human homogentisate 1,2-dioxygenase (HGO) gene. Genomics 43, 115–122 (1997)
Grasko, J.M., Hooper, A.J., Brown, J.W., McKnight, C.J., Burnett, J.R.: A novel missense HGD gene mutation, K57N, in a patient with alkaptonuria. Clin. Chim. Acta 403, 254–256 (2009)
Hogben, L., Worrall, R.L., Zieve, I.: The genetic basis of alkaptonuria. Proc. R. Soc. Edinb. 52, 264–295 (1932)
Hüttl, S., Markovic, O., Sit´aj, Š.: Hemarthrosis in ochronotic arthropathy. Z. Rheumaforsch. 25, 169–181 (1966)
Introne, W.J., Kayser, M.A., Gahl, W.A.: Gene Reviews at Gene Tests: Medical Genetics Information Resource. University of Washington; Seattle: Alkaptonuria. Database online (2009)
Janocha, S., Wolz, W., Sršeň, Š., Sršňová, K., Montagutelli, X., Guénet, J.L., Grimm, T., Kress, W., Müller, C.R.: The human gene for alkaptonuria (AKU) maps to chromosome 3q. Genomics 19, 5–8 (1994)
Kaprálik, I., Sršeň, Š.: Analysis of inheritance type in alkaptonuria (author’s transl). Bratisl. Lek. Listy. 73, 459–471 (1980)
Kobak, A.C., Oder, G., Kobak, S., Argin, M., Inal, V.J.: Ochronotic arthropathy: disappearance of alkaptonuria after liver transplantation for hepatitis B-related cirrhosis. Clin. Rheumatol. 11, 323–325 (2005)
La Du, B.N.: Alcaptonuria. In: Scriver, C.R., Beaudet, A.L., Sly, W.S., et al. (eds.) The metabolic bases of inherited diseases, pp. 775–790. Mc Graw-Hill, New York (1989)
La Du, B.N., Zannoni, V.G., Laster, L., Seegmiller, J.E.: The nature of the defect in tyrosine metabolism in alkaptonuria. J. Biol. Chem. 230, 251–260 (1958)
Ladjouze-Rezig, A., Rodriguez de Cordoba, S., Aquaron, R.: Ochronotic rheumatism in Algeria: clinical, radiological, biological and molecular studies a case study of 14 patients in 11 families. Joint Bone Spine 73, 284–292 (2006)
Mannoni, A., Selvi, E., Lorenzini, S., et al.: Alkaptonuria, ochronosis, and ochronotic arthropathy. Semin. Arthritis Rheum. 33, 239–248 (2004)
Muller, C.R., Fregin, A., Srsen, S., et al.: Allelic heterogeneity of alkaptonuria in Central Europe. Eur. J. Hum. Genet. 7, 645–651 (1999)
Oexle, K., Engel, K., Tinschert, S., Haas, D., Lee-Kirsch, M.A.: Three-generational alkaptonuria in a non-consanguineous family. J. Inherit. Metab. Dis. 31(Suppl 2), S425–S430 (2008)
Phornphutkul, C., Introne, W.J., Perry, M.B., Bernardini, I., Murphey, M.D., Fitzpatrick, D.L., Anderson, P.D., Huizing, M., Anikster, Y., Gerber, L.H., Gahl, W.A.: Natural history of alkaptonuria. N. Engl. J. Med. 26, 2111–2121 (2002)
Porfirio, B., Chiarelli, I., Graziano, C., Mannoni, A., Morrone, A., Zammarchi, E., De Bernabé, D.B., De Córdoba, S.R.: Alkaptonuria in Italy: polymorphic haplotype background, mutational profile, and description of four novel mutations in the homogentisate 1,2-dioxygenase gene. J. Med. Genet. 37, 309–312 (2000)
Rovenský, J., Urbánek, T.: Alkaptonurie a ochronoza. In: Hrncir, Z. (ed.) Klinická revmatologie, pp. 509–516. Galen, Praha (2003)
Sakthivel, S., Zatkova, A., Nemethova, M., Surovy, M., Kadasi, L., Saravanan, M.P.: Mutation screening of the HGD gene identifies a novel alkaptonuria mutation with significant founder effect and high prevalence. Ann. Hum. Genet. 78, 155–164 (2014)
Schmidt, S.R., Gehrig, A., Koehler, M.R., Schmid, M., Müller, C.R., Kress, W.: Cloning of the homogentisate-1,2-dioxygenase, the key enzyme of alkaptonuria in mouse. Mamm. Genome 8, 168–171 (1997)
Sit´aj, Š.: Artropatia alcaptonurica. Bratisl. Lek. Listy 27(4), 1–9 (1947)
Sit´aj, Š., Červeňanský, J., Urbanek, T.: Alkaptonuria and ochronosis, (in Slovak). SAV Publishing, Bratislava (1956), 156 p
Sršeň, Š.: Alkaptonuria. In: Sit´aj, Š., Hyanek, J. (eds.) Alkaptonuria, p. 48. Martin, Osveta (1984). 264 pp
Sršeň, S., Müller, C.R., Fregin, A., Sršňová, K.: Alkaptonuria in Slovakia: thirty-two years of research on phenotype and genotype. Mol. Genet. Metab. 75, 353–359 (2002)
Suwannarat, P., O’Brien, K., Perry, M.B., Sebring, N., Bernardini, I., Kaiser-Kupfer, M.I., Rubin, B.I., Tsilou, E., Gerber, L.H., Gahl, W.A.: Use of nitisinone in patients with alkaptonuria. Metabolism 54, 719–728 (2005)
Uyguner, O., Goicoechea de Jorge, E., Cefle, A., Baykal, T., Kayserili, H., Cefle, K., Demirkol, M., Yuksel-Apak, M., Rodriguez de Córdoba, S., Wollnik, B.: Molecular analyses of the HGO gene mutations in Turkish alkaptonuria patients suggest that the R58fs mutation originated from central Asia and was spread throughout Europe and Anatolia by human migrations. J. Inherit. Metab. Dis. 26, 17–23 (2003)
Vilboux, T., Kayser, M., Introne, W., Suwannarat, P., Bernardini, I., Fischer, R., O’Brien, K., Kleta, R., Huizing, M., Gahl, W.A.: Mutation spectrum of homogentisic acid oxidase (HGD) in alkaptonuria. Hum Mutat. 30, 1611–1619 (2009)
Zat´ková, A.: An update on molecular genetics of alkaptonuria. J. Inherit. Metab. Dis. 34, 1127–1136 (2011)
Zat´ková, A., Poláková, H., Mičutková, L., Zvarík, M., Feráková, E., Bošák, V., Kádasi, L.: Mutation heterogenity in Slovak alkaptonuria patients. Eur. J. Hum. Genet. 7(1), 127–518 (1999)
Zat´ková, A., de Bernabe, D.B., Poláková, H., Zvarík, M., Feráková, E., Bošák, V., Ferák, V., Kádasi, L., de Cordoba, S.R.: High frequency of alkaptonuria in Slovakia: evidence for the appearance of multiple mutations in HGO involving different mutational hot spots. Am. J. Hum. Genet. 67, 1333–1339 (2000a)
Zat´ková, A., de Bernabé, D.B., Poláková, H., Feráková, E., Bošák, V., Cisárik, F., Lukačovič, M., de Córdoba, S.R., Kádasi, L., Ferák, V.: Alelova heterogennost mutacii sposobujucich alkaptonuriu a mozne priciny vysokeho vyskytu tejto choroby na Slovensku. Lek. Obzor. 49, 347–352 (2000b)
Zat´ková, A., Poláková, H., Mičutková, L., Zvarík, M., Bošák, V., Feráková, E., Matušek, J., Ferák, V., Kádasi, L.: Novel mutations in the homogentisate-1,2-dioxygenase gene identified in Slovak patients with alkaptonuria. J. Med. Genet. 37, 539–542 (2000c)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Bošák, V. (2015). Genetics of Alkaptonuria. In: Rovenský, J., Urbánek, T., Oľga, B., Gallagher, J. (eds) Alkaptonuria and Ochronosis. Springer, Cham. https://doi.org/10.1007/978-3-319-15108-3_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-15108-3_7
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-15107-6
Online ISBN: 978-3-319-15108-3
eBook Packages: MedicineMedicine (R0)