Abstract
Delayed parenthood is a central feature of the massive transformation of family and reproduction in rich countries. We analyse the shift of motherhood towards later reproductive ages during the last four decades and review its consequences for children and their mothers in low-fertility countries in Europe, North America, Oceania and East Asia. First we analyse the trends in birth rates at advanced reproductive ages (35+) and document the rapid rise in first and second birth rates at these ages. We show that a relatively high share of childless women and of women with one child aged 35-44 still plan to have a(nother) child in the future. Subsequently, we discuss the limited success rates of assisted reproduction at advanced reproductive ages. Next we outline the key drivers of delayed parenthood and its demographic consequences. Finally, we briefly review the consequences of delayed motherhood for pregnancy outcomes, maternal and child health and highlight selected positive consequences of later parenthood for mothers and children. We argue that economic and social rationales for late reproduction clash with the biological and health rationales for having children earlier in life.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Introduction
Delayed parenthood is one of the defining features of the massive transformation of family and reproduction in rich countries [1]. The “contraceptive revolution ” that started in the late 1960s, together with relatively easy access to abortion in most countries, have given women and couples an effective control over their pregnancies and contributed to changing family and partnership relations [2]. Young people in Western Europe today are sexually active for more than a decade before becoming parents. Policy concerns about high rates of teenage pregnancies , common in many Western countries a few decades ago [3], have gradually given way to heated debates about late motherhood and ticking biological clock [4, 5]. In the United Kingdom, The Royal College of Obstetricians and Gynaecologists [6] declared later maternal age as an “emerging public health issue” that needs to be thoroughly studied.
Scientific and media debates on delayed motherhood take different angles, reflecting upon the advantages as well as drawbacks of this phenomenon. Some view late parenthood as an opportunity and a positive experience [7]. Older parents may offer children higher living standards and more stable family arrangements, improving their future life chances [8]. Often, delayed parenthood is portrayed as risky, potentially endangering mother’s and children’s health or leading to involuntary childlessness and demographic decline [9, 10]. Discussions in popular press often blame women (and occasionally men) who wait for “too long,” presenting them as selfish, career-oriented, irresponsible, and breaking the “natural order” [11, 12]. Some of these concerns are justified. It has been repeatedly shown that even well educated women are often poorly informed about female reproductive aging, infertility and the increased risk of pregnancy complications, and they often overestimate the chances of becoming pregnant at higher reproductive ages [12,13,14,16].
In this chapter we analyse the shift to later parenthood and review its consequences for children and parents, especially mothers. First we analyse the trends in birth rates at advanced reproductive ages (35+), including trends at very high reproductive ages (50+), which were characterised by a rapid rise in first and second birth rates. We show that a relatively high share of childless women and women with one child aged 35–44 still plan to have a child in the future. Subsequently, we analyse success rates of assisted reproduction at advanced reproductive ages and its role in fuelling the trend towards delayed motherhood. Next we discuss the key drivers of delayed parenthood and its demographic consequences. Finally, we briefly review the consequences of delayed motherhood for pregnancy outcomes, maternal and child health and highlight selected positive consequences of later parenthood for mothers and children, which provide economic and social rationale for late reproduction. Our main focus is on developed countries in Europe, North America, Oceania and East Asia which have experienced a continuing shift to delayed reproduction in the last four decades.
Shifting Childbearing to Advanced Reproductive Ages
The Long-Term Trend Towards Late Motherhood
The trend to later motherhood first started in Western and Northern Europe, the United States, Canada, Australia and Japan in the early 1970s, thus reversing the shift towards earlier first births observed during the post-war baby boom era [17]. Other developed countries and regions followed during the 1980s and 1990s. Recently, the mean age at first birth among women has surpassed 30 in several European countries including Italy and Spain, and in South Korea where it reached 31.1 in 2014, the record-high among rich countries (Fig. 2.1). In the most developed countries the age at starting a family among women has shifted from 22–25 in 1970 to 26–30 in 2014, without showing signs of stabilising or reversing.
In most other world regions women still become mothers early in life, but even many of the less developed countries with high fertility have seen postponement of first marriage and first birth and a decline in adolescent births in the last two decades ([21]: 38). A gradual trend towards delayed motherhood has been reported for many middle-income countries with relatively low fertility, including China, Iran, and the countries of Northern Africa, and Latin America (including Chile, Fig. 2.1) [22, 23].
More Frequent Late First and Second Births
Childbearing at higher reproductive ages is not a new phenomenon. Late births had been historically much more common than today, owing to many women having a large family and continuing reproducing until experiencing sterility. In the era of large families until the early twentieth century, childbearing was common even among women past age 40.
With the decline in family size, and a virtual disappearance of large families with more than four children, the historical pattern of having a fourth, fifth or sixth birth at late reproductive ages has been replaced with a new pattern of having a first or a second child later in life. This is especially the case in countries characterized by low fertility rates and a rapid shift to late motherhood, including Italy and Spain. Across the rich low-fertility countries the share of births to women aged 35 and older has risen quickly since 1980 and this increase has been particularly steep for first and second births and at ages 40+ (Table 2.1). For instance, in Japan, the share of first birth rates that took place among women aged 35 and over jumped from 2% in 1980 to 17% in 2014 and the share of second birth rates at these ages jumped from 4 to 26%. At the same time the contribution of women aged 40 and over to total fertility in Japan went up from a low of 0.5 to 3.8% (Table 2.1).
Despite these dramatic shifts, childbearing at ages 40 and higher still remains rather infrequent. In Spain and Sweden, where the shift to late motherhood is well advanced, women gave birth to 0.08 children on average after age 40 in 2014. This amounts to less than 6% of their theoretical reproductive capacity above age 40 estimated at 1.43 children per woman [24]. Late births are even less common in most other rich countries [18].
Childbearing at Very High Reproductive Ages
Advances in assisted reproductive technology (ART) , especially oocyte cryopreservation , have partly eroded the conventional boundaries of female reproductive lifespan marked by follicular depletion and menopause (see Kat and Broekmans in Chap. 1). In the United States, the number of births to women aged 50+ tripled from 255 in 2000 to 743 in 2014 [25, 26]. In the European Union countries (including the United Kingdom) the number of births to women aged 50+ in 2002–2014 jumped from 287 to 1019 ([27], own computations). Wikipedia [28] provides an extensive list of women who gave birth at age 50 or older, with the three oldest mothers reportedly being all from India and giving birth at age 70 between 2008 and 2016. The oldest mother with fully verified age is Maria del Carmen Bousada from Spain who gave birth to twin boys shortly before her 67th birthday, after receiving ART using donor oocytes in the United States.
Childbearing Intentions and Their Realisation at Higher Reproductive Ages
High Share of Childless Women Aged 35+ Intends to Have a Child
The Generations and Gender Surveys (GGS) for six European countries that took place in the 2000s reveal that many women still plan to have a child at an age when their reproductive capacity is declining [29]. This is especially the case in Austria, France, Italy, and Russia where 28–32% of women aged 35–39 intended having a(nother) child (Fig. 2.2). Perhaps more surprising is that more than one in ten women aged 40–44 in Austria, Italy and Russia intended having a(nother) child. These shares were much lower in Czechia and Poland, two post-communist countries where reproduction took place at relatively young ages until the 1990s. However, women at older reproductive ages also express uncertainty about their plans: in each analysed country the share of women responding they “probably” intend to have a child outnumbers the share responding they are “certain” about their intention.
(a) Share of women aged 35–39 and 40–44 stating they intend to have a(nother) child in the future; six European countries, surveys organized in 2000s. (b) Share of women aged 35–39 stating they intend to have a(nother) child in the future by the number of children they already have; six European countries. The graph combines “probably yes” and “certainly yes” answers. Source: Own computations from the Generations and Gender Survey (GGS) data for Austria 2008–2009, Czechia 2004–2005, France 2005, Italy 2003–2004, Poland 2010–2011, Russia 2004 (see [29] for questions asked and for more details about the data)
Another consistent finding is a strong family size gradient in reproductive intentions: the plan to have a child later in life is very common among childless women aged 35–39, with a majority of these women intending to become mothers. Also many women with one child still planned to have a second child in the future. In contrast, only a few women having two or more children intended to have another child at later ages (Fig. 2.2b). Very similar gradient is found also for women aged 40–44 and for men at advanced reproductive ages (not shown here; see [30]).
Actual Fertility at Higher Reproductive Ages Matches More Closely the Earlier Reproductive Intentions Among Mothers Than Those Among the Childless
How are intentions to have children later in life related to the actual fertility rates at higher reproductive ages? For three European countries, Austria, Italy, and the Netherlands, we compared survey data on reproductive intentions with the aggregate data on childbearing probabilities by age and parity included in the Human Fertility Database [18] and Human Fertility Collection [19]. We did not follow up the women interviewed at the time of the survey, but we compared their plans with population-wide data on the likelihood of having a child by the end of their reproductive life among all women who were of the same age and had the same number of children in the year intention estimates were calculated.
Table 2.2 illustrates this correspondence for Italy, where 37% of women aged 35–39 intended to have a child in the future (including those saying “probably yes”) according to the 2009 Multiscopo survey . This compares with the aggregate data showing that 22% of women of that age gave birth in the years following the survey. A similar correspondence is found for Austria (24% intended to have a child vs. 15% have had a child; see [30], Table 2.2a) and yet closer relationship is found for the Netherlands (20% vs. 16%) (results for Austria and the Netherlands not shown here). These comparisons indicate that women aged 35–39 wishing to have a child in the future still have a relatively good chance of achieving their goal, even when taking into account that those giving birth to a child are not always those who intended to have one.
The gap between reproductive intentions and actual pregnancies becomes much wider at later ages, 40–44, when many women are infertile and the potential mothers often widely overestimate their chances of becoming pregnant (see data for Italy in Table 2.2). In addition, childless women aged 35+ consistently show a larger gap between their reproductive intentions and subsequent childbearing. This gap is partly related to considerable uncertainty about the reproductive plans reported by these women, but it is also due to their unrealistic expectations and adverse life circumstances (which often include not having a partner). Selectivity plays a role as well, with more frequent health problems and higher infertility among the childless.
Assisted Reproduction and Delayed Childbearing
Rising ART Use and Declining ART Success Rates at Higher Reproductive Ages
Many women planning to have a child in their late 30s and early 40s are likely to face infertility and turn to ART treatment. This trend is partly fuelled by widespread misperceptions about the ability of ART to compensate for infertility at later reproductive ages [31], giving women an illusion of fertility control at higher reproductive ages [32, 33]. Despite many rich countries not subsidizing ART for women after a certain age threshold, the number of ART cycles is rising fastest at age 40 and higher. In the United States , 21% of all ART cycles in 2013 (i.e., 34 thousand cycles) were initiated by women aged 41+ (own computations from the Centers for Disease Control and Prevention data [34]).
In Europe , the incomplete data show that the number of registered ART cycles at ages 40+ increased much faster in 2002–2012, by a factor of 3.1, than the number of cycles initiated by younger women, which increased by a factor of 1.8 (computations based on [35, 36]). Especially steep rise was reported for ART using donor oocytes , which quadrupled in the same period. Overall, the share of ART cycles initiated by women aged 40+ jumped from 12 to 19% in 2002–2012, contributing about 7% of all children born to women over age 40.
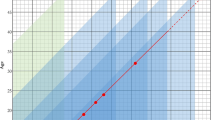
Success rates of non-donor assisted reproduction, measured especially by the percentage of ART cycles that result in pregnancies and live births or single-infant live births, decline rapidly with age among women past age 32 ([34], Fig. 14). Figure 2.3 illustrates this pattern using the data for the United States. Among women undergoing non-donor ART in 2013, pregnancy rates per cycle reached 46% at ages below 35, 25% at age 40 and only 4% at ages 45+. Because of high rates of miscarriage at higher ages, the fall in the likelihood of live birth following ART cycle is even steeper with age: 40% of non-donor ART cycles initiated at ages <35 resulted in live birth in 2013, compared with 17% of the cycles initiated at age 40 and 2% at ages 45+ (Fig. 2.3). The likelihood of live birth has improved only gradually among women past age 40. A majority of women do not achieve pregnancy leading to live birth after age 40 even after six or more ART cycles [37, 38].
Success rates of ART cycles with non-donor oocytes or embryos by age in the United States : Percentage of cycles resulting in pregnancies and live birth, 1998 and 2013. Source: [34] (Figs. 15 and 17) and 2000 (Figs. 10 and 12). Note: Data for single years of age published only for ages 40–44
Conventional ART using non-donor oocytes therefore cannot offset age-related fertility decline and for many women it does not provide a realistic chance of having a child after age 40 [31, 39, 40]. Also the cost of ART treatments per live birth delivery rises steeply after age 40, making conventional non-donor ART use problematic, especially after age 45 [41].
In contrast, ART with donor oocytes shows remarkably stable success rate with age of women treated, with the percentage of ART cycles resulting in live births staying over 50% even for women in their 40s according to the US data for 2013 ([34]: Fig. 40) (for more details on treatment options see Drakopoulos and Polyzos in Chap. 3). Therefore, despite higher costs and despite the fact that in case of successful treatment the child will not be genetically related to the mother, the use of donor oocytes increases rapidly. In the United States , donor oocytes accounted for 37% of ART cycles among women aged 41+ and for around 78% of live births among ART users of that age; for Europe the corresponding estimates were 17% and 41%, respectively (own computations from [34] data and [35] data). In addition, the cryopreservation of oocytes has rapidly evolved and reached the stage when it has become widely available ([42]; see also Chap. 8 and other chapters in this volume). In the US, the number of oocyte or embryo banking cycles rose dramatically from around a thousand in 2006 to over 27 thousand in 2013 [34]. Surprisingly many of these freezing cycles, 30%, are taking place at ages 41+, i.e., at ages when the quality of oocytes deteriorates rapidly, implying lower chances of successful pregnancy and delivery later in life.
Main Factors Contributing to Later Parenthood
A review by Mills et al. [43] identified the following key drivers of the shift towards later parenthood: expanding education, increased employment among women, economic uncertainty and precarious forms of employment, low availability and high costs of housing, delayed and more unstable partnerships, more individualized values including higher acceptance of childlessness, and lower levels of gender equality. These factors often reinforce each other and their importance differs by country and time period [17]. The shift towards later parenthood was supported by widely available efficient contraception, especially the pill [44, 45] and, more recently, by the spread of “emergency contraception” that is used especially among young adult women [46].
Being in education is commonly perceived as incompatible with parenthood [47]. The continuing expansion of higher education in the rich countries during the last four decades has been repeatedly identified as a central driver of delayed parenthood [48, 49]. However, in many countries including the United States, United Kingdom and Norway, highly educated women increasingly shifted childbearing well beyond the time of completing their education, often towards their mid- or late-30s [46,47,52]. This leads to rising contrasts (“polarization”) in first birth timing by social status, especially in Southern Europe and in English-speaking countries [53]. Unemployment and unstable economic conditions have been documented as important factors especially in Southern Europe, where policies supporting family formation are weak and many young adults face precarious labour market situation [54]. At an individual level, not having a suitable partner and, more generally, “not feeling ready” for motherhood are frequently cited as important reasons for delaying motherhood [55, 56].
Demographic Consequences of Delayed Childbearing
The shift to later motherhood has important population-level consequences. It negatively affects period birth rates as some women who would otherwise have had a child in any given year shifted their childbearing plans towards the future. As a result, period total fertility rates are depressed and often decline well below the corresponding indicators of cohort family size [57, 58]. Delayed childbearing implies wider age distance between generations, which in turn means that women and men having children later in life are less likely to survive to see their grandchildren when compared with younger parents or they might not remain in good health when becoming grandparents [59, 60]. The stretched intergenerational interval also implies a slower pace of population decline when fertility rates are below the replacement-level threshold of around 2.07 children per woman in low-mortality countries [61].
Later motherhood can also result in higher childlessness and reduced family size in the population. Leridon and Slama [62] simulated the impact of a postponement of the first pregnancy attempt by 30 and 69 months, initially starting at age 25 on average. The shift by 69 months would reduce the final number of children per woman by more than 10% (from 2.00 to 1.77) and would increase the share of childless couples from 11.7 to 17.7%. Te Velde et al. [63] used similar micro-simulation models, estimating that first birth postponement in six European countries between 1970 and 2007 led to an increase in permanent childlessness in the range of 4% in Czechia to 7% in Spain.
Delayed childbearing is closely associated with higher frequency of multiple births. Their increase with age of the mother is attributable to higher multiple follicle growth with age [64] and to high rates of multiple births following ART. In the highly developed countries the frequency of twin deliveries increased rapidly between 1970 and 2013, typically doubling, but in some cases (Greece, Hong Kong) tripling during that period [65]. In the United States, the number of twin live births per thousand live births went up from 18.9 in 1980 to 33.9 in 2014 ([25], Table 27). The analysis of data for 32 countries by Pison et al. [65] shows that ART use was the main reason for the rising frequency of twin births, contributing on average to three quarters of their observed rise between 1970 and 2005. As single embryo transfers are increasingly preferred by health professionals, the guidelines regulating ART use are being revised. Consequently, the frequency of twin and triplet deliveries peaked in 13 countries including Nordic countries, Australia, Japan, the Netherlands and Japan between 1998 and 2010 and then started declining [61,62,63,64,69].
Consequences of Delayed Motherhood for Pregnancy Outcomes, Maternal and Child Health
Extensive medical literature documents the effects of pregnancy and childbearing at advanced reproductive ages on pregnancy outcomes, foetal development, and maternal and child health (e.g., [60, 66,67,68,69,74]). Many risks are related to “natural pregnancies”, but some including multiple deliveries are more typical for ART use. We give only brief highlights of the most important findings; more details are discussed elsewhere in this volume.
Pregnancy complications and foetal loss are more frequent at higher maternal ages. The frequency of miscarriages (spontaneous abortions), ectopic pregnancies as well as stillbirths increases rapidly with age among women in their late 30s and older [60, 75]. Danish register-based study found that at age 42 and older, more than half of pregnancies intended to be carried to term (i.e. excluding induced abortions) resulted in foetal loss, compared with 13.5% of pregnancies across all ages [75]. Male partner’s age was also found to be an independent risk factor for miscarriage [76]. Interestingly, women using donor oocytes do not show an increase rise in pregnancy loss with age [77, 78], which again suggests that the age and quality of oocytes are the main factors determining reproductive success (see also Kat and Broekmans in Chap. 1). A combination of rising infertility and more frequent pregnancy losses with age implies that women who have a strong childbearing desire and a preference for larger family should aim to have children relatively early in life. Habbema et al. [79] showed that women planning only one child and willing to take a 50% risk that they do not succeed can start their pregnancy attempt at age 41 (or 42 if they are willing to use ART). Those planning three kids and wanting to have a 90% chance they succeed should start as early as at age 23.
Advanced maternal age is also a risk factor in preterm births [80, 81] and complications during pregnancy and delivery, including high rate of Caesarean delivery, excessive labour bleeding, and higher frequency of diabetes and chronic and pregnancy-induced hypertension among mothers [71, 73, 74]. Older mothers are more likely to suffer from obesity, take medication or experience morbidity (see [82] for obesity). Multiple births , more common at later childbearing ages, constitute an additional risk factor associated with low birth weight of infants, pregnancy complications, maternal risks, and higher long-term morbidity [83, 84]. Among children, advanced maternal age is often linked to higher incidence of congenital anomalies and chromosomal aberrations, as discussed in Chap. 1 by Kat and Broekmans.
Positive Consequences of Parenthood at Later Ages for Parents and Children
The Economic Rationale of Parenthood at Later Ages
Among higher educated women with better-paid jobs and good career prospects there is a strong economic rationale for delaying parenthood well beyond the period of completing education. It is based on a need for couples to accumulate resources before family formation, to have enough resources to rear their children and support their education as they grow up, to qualify for paid maternity and parental leaves, and to minimize the income loss linked to childcare-related career break.
Achieving financial security is often cited by couples as one of the most important factors in their parenthood decisions [16]. In many countries, especially in Southern and Eastern Europe, rental housing is scarce or too costly. Young couples may need to accumulate considerable savings and achieve a stable income before purchasing their own flat or a house—which is often seen as a precondition to having children [85, 86]. Married couples living in US cities with highest rents and housing sales prices were having their first child by 3–4 years later than the couples living in metropolitan areas with cheap housing [87]. In addition, raising children is costly, especially in countries where costs of childcare, healthcare and education shouldered by parents are high. In the US, the cost of raising a child from childbirth up to age 18 was estimated at 245,000 US Dollars for middle-income families, based on the 2013 computations by US Department of Agriculture [88]. This again motivates couples to put off childbearing until both partners achieve stable employment and steady income.
In countries which provide paid maternity and parental leave, including Nordic countries, their level is often linked to pre-leave income and a minimum period of uninterrupted employment before the leave. As this policy is focused on compensating parents their foregone earnings, it motivates prospective parents to get established on the labour market and achieve a stable full-time position before having a child, potentially delaying their parenthood [89]. Finally, among mothers with higher socio-economic position, earning losses due to childcare leave are substantially lower at higher childbearing ages when they are more advanced in their careers, have more secure employment, and experience lower skill depreciation [86,87,92]. The US data analysed by Herr [93] show that fertility delays are paying off especially for college graduates: for them, each year of delaying motherhood after their labour market entry implies a 2.9% increase in their wage after a 20-year period, accounting for 5.5% of their total wage growth.
Non-economic Positive Consequences of Delayed Parenthood
The positive consequences of delayed parenthood extend beyond resource accumulation, more stable careers and lower income losses. However, the research in this area is relatively limited and the evidence so far is often based on small datasets or data pertaining to one country. Many papers do not address selection effects—the fact that older mothers are also, on average, better educated and healthier, and therefore the possible effects of late motherhood reported below might be more closely associated with their education and health rather than age [94, 95]. Therefore, these findings do not imply causality and have to be interpreted with caution.
Later parenthood is linked with a lower likelihood for children to be born to a mother living without a partner [60] and a lower percentage of unintended pregnancies and births [96, 97]. Children born to older parents experience less frequent parental separation [98] and therefore they also experience living with a single mother or with stepparents less often than the children born earlier in life. The research on three indicators of child’s cognitive and behavioural outcomes at the age of three summarised by Hansen et al. [99] showed these outcomes peaking among children born to mothers in their 30s. While much of this developmental advantage was attributable to their mothers’ higher education, the positive effect of later motherhood persisted even when mothers’ education, return to employment and childcare use were controlled for. Myrskylä and Margolis [100] found that parents at older ages (35+) show more positive happiness trajectory after the childbirth than the younger parents.
Barclay and Myrskylä [101], working with Swedish data, demonstrated additional benefit of late motherhood for children. Children born to older mothers are also born in a later time period, reaping the benefits of improving social conditions over time. They are taller, more likely to attend university and perform better at standardised tests than their siblings born when their mothers were younger. Among mothers, late age at childbearing is associated with better health and longevity [102, 103]. These findings again suggest that some of the benefits of later motherhood might be explained by selectivity of mothers who are fertile (and presumably healthyier) at later ages.
Discussion: The Contrasting Biological and Social Rationales for and Against Late Parenthood
As longevity continues rising, life courses of men and women stretch and they experience many important transitions later in life [104]. They complete their education, move from parental home, enter the labour market, or retire at ever higher ages. The fast increase in the number of women who are childless past age 35 and plan to have a child in the future appears perfectly in line with this trend. With some simplification, children born to older parents are also born to more stable, happier and wealthier families. Many social and economic rationales speak for having children late in life. However, these rationales clash with “inconvenient biology” [105] as there is also a clear biological and health rationale for having children much earlier in life [9, 106]. The steep rise in the number of ART cycles at later reproductive ages illustrates the scale of infertility and unfulfilled pregnancy desires among women who arguably postponed parenthood for too long.
The rise of ART with donor oocytes and the advances in “social egg freezing” have gradually eroded the biological limits to fertility marked by follicular depletion and menopause. The number of post-menopausal women getting pregnant is increasing fast, although from very low numbers. At the same time, a vast majority of women still plan to get pregnant without the help of medically assisted reproduction. They are often caught between the conflicting motivations for and against having children and struggling with the ever more pertinent question of “How long can you wait to have a baby?” [4, 5, 107]. As Habbema et al. [79] demonstrate, the answer depends on family size preferences and the strength of these preferences.
Key Messages
-
1.
A sharp increase in the number of women having their first or second birth after age 35 has taken place across the highly developed countries. Also the frequency of motherhood among post-menopausal women past age 50 is rising fast, but from extremely low levels.
-
2.
Childbearing intentions past age 35 are especially common among the childless women, many of whom will face infertility when trying to realise these plans.
-
3.
Assisted reproduction use has been rising faster among women past age 40 than among the younger age groups. However, success rates of ART using fresh non-donor oocytes remain low at ages 41+, with ART using donor oocytes or women’s own cryopreserved oocytes being much more effective and rapidly expanding alternatives.
-
4.
The massive expansion of university education is the main factor behind the shift to later motherhood, followed by unstable labour market and deteriorating economic position of young adults as well as rapid changes in partnership behaviour and the availability of highly efficient contraception.
-
5.
Prospective parents face conflicting rationales for having children earlier or later in life. Biological and health rationales for early childbearing clash with economic and well-being rationales for later reproduction, which include higher family stability and higher happiness among older parents.
References
Lesthaeghe R. The unfolding story of the Second Demographic Transition. Popul Dev Rev. 2010;36(2):211–51.
van de Kaa DJ. On the societal impact of modern contraception. In: Beets G, Schippers J, te Velde E, editors. The future of motherhood in western societies. Dordrecht: Springer; 2011. p. 49–60.
Jones EF, Forrest JD, Goldman N, Henshaw SK, Lincoln R, Rosoff JI, Westoff CF, Wulf D. Teenage pregnancy in developed countries: determinants and policy implications. Fam Plan Perspect. 1985;17(2):53–63.
Heffner LJ. Advanced maternal age—how old is too old? N Engl J Med. 2004;351(19):1927–9.
Twenge J. How long can you wait to have a baby? The Atlantic July/August 2013 Issue. http://www.theatlantic.com/magazine/archive/2013/07/how-long-can-you-wait-to-have-a-baby/309374/
Royal College of Obstetricians and Gynaecologists. RCOG statement on later maternal age. 2009. http://www.rcog.org.uk/what-we-do/campaigning-and-opinions/statement/rcog-statement-latermaternal-age
La Liberte A. Why have a child after 40? Blog Post. 2012. http://achildafter40.com/about-a-child-after-40/. Accessed Oct 2016.
McLanahan S. Diverging destinies: How children are faring under the second demographic transition? Demography. 2004;41(4):607–27.
Bewley S, Davies M, Braude P. Which career first? BMJ. 2005;331:588–9.
Selvaratnam T. The big lie: motherhood, feminism, and the reality of the biological clock. Amherst, NY: Prometheus Books; 2014.
Budds K, Locke A, Burr V. Risky business: constructing the ‘choice’ to ‘delay’ motherhood in the British press. Fem Med Stud. 2013;13(1):132–47.
Shaw RL, Giles DC. Motherhood on ice? A media framing analysis of older mothers in the UK news. Psychol Health. 2009;24(2):221–36.
Bretherick KL, Fairbrother N, Avila L, Harbord SH, Robinson WP. Fertility and aging: do reproductive-aged Canadian women know what they need to know? Fertil Steril. 2010;93(7):2162–8.
Daniluk JC, Koert E, Cheung A. Childless women’s knowledge of fertility and assisted human reproduction: identifying the gaps. Fertil Steril. 2012;97(2):420–6.
Lampic C, Svanberg AS, Karlström P, Tydén T. Fertility awareness, intentions concerning childbearing, and attitudes towards parenthood among female and male academics. Hum Reprod. 2006;21(2):558–64.
Tough S, Benzies K, Fraser-Lee N, Newburn-Cook C. Factors influencing childbearing decisions and knowledge of perinatal risks among Canadian men and women. Matern Child Health J. 2007;11(2):189–98.
Sobotka T. Postponement of childbearing and low fertility in Europe. Ph.D. Thesis, University of Groningen. Amsterdam: Dutch University Press; 2004.
Human Fertility Database. Period and cohort fertility rates by age and birth order; data on mean age at first birth accessed at www.humanfertility.org (data downloaded 5 October 2016). Max Planck Institute for Demographic Research (Germany) and Vienna Institute of Demography (Austria). 2016.
Human Fertility Collection. Period age-specific fertility rates accessed at www.fertilitydata.org (data downloaded 5 October 2016). Max Planck Institute for Demographic Research (Germany) and Vienna Institute of Demography (Austria). 2016.
Yoo SH, Sobotka T. The role of tempo effect in the ultra-low fertility in South Korea. Paper presented at the 2016 annual meeting of the Population Association of America, Washington, D.C., 1 April 2016, 2016.
United Nations. World fertility report 2013: fertility at the extremes. New York: United Nations, Department of Economic and Social Affairs, Population Division; 2013.
Rosero-Bixby L, Castro-Martín T, Martín-García T. Is Latin America starting to retreat from early and universal childbearing? Demogr Res. 2009;20(9):169–94.
Sobotka T. Post-transitional fertility: the role of childbearing postponement in fuelling the shift to low and unstable fertility levels. J Biosoc Sci. 2017. Forthcoming.
Sheps MC. An analysis of reproductive patterns in an American isolate. Popul Stud. 1965;19(1):65–80.
Hamilton BE, Martin JA, Osterman MJK et al.. Births: final data for 2014. National vital statistics reports, vol. 64, No. 12. Hyattsville, MD: National Center for Health Statistics; 2015.
Martin JA, Hamilton BE, Ventura SJ, Menacker F, Park MM. Births: final data for 2000 national vital statistics reports, vol. 50, No. 5. Hyattsville, MD: National Center for Health Statistics; 2002.
Eurostat. Data on births by age of mother and birth order in 2000–2014. Eurostat online database, theme “Population and Social Conditions”. 2016. http://ec.europa.eu/eurostat/data/database. Accessed Oct 2016.
Wikipedia. Pregnancy over age 50. 2016. https://en.wikipedia.org/wiki/Pregnancy_over_age_50. Accessed 10 Oct 2016.
Beaujouan É. Counting how many children people want: The influence of question filters and pre-codes. Demográfia. 2014;56(5):35–61. English edition 2013
Beaujouan É, Sobotka T. Late motherhood in low-fertility countries: reproductive intentions, trends and consequences. In: Vienna Institute of Demography Working Papers and Human Fertility Database Research Report VID WP 02/2017 and HFD RR-2017-002; 2017.
Wyndham N, Figueira PGM, Patrizio P. A persistent misperception: assisted reproductive technology can reverse the “aged biological clock”. Fertil Steril. 2012;97(5):1044–7.
Mac Dougall K, Beyene Y, Nachtigall RD. Age shock: misperceptions of the impact of age on fertility before and after IVF in women who conceived after age 40. Hum Reprod. 2012;28(2):350–6.
Szewczuk E. Age-related infertility: a tale of two technologies. Sociol Health Illn. 2012;34(3):429–43.
CDC. Assisted reproductive technology national summary report 2013. Atlanta (GA): Centers for Disease Control and Prevention, American Society for Reproductive Medicine, Society for Assisted Reproductive Technology, US Dept of Health and Human Services; 2015.
Calhaz-Jorge C, De Geyter C, Kupka MS, De Mouzon J, Erb K, Mocanu E, Motrenko T, Scaravelli G, Wyns C, Goossens V, Gliozheni O. Assisted reproductive technology in Europe, 2012: results generated from European registers by ESHRE. Hum Reprod. 2016;31(8):1638–52.
Nyboe Andersen A, Gianaroli L, Felberbaum R, de Mouzon J, Nygren KG. Assisted reproductive technology in Europe, 2002. Results generated from European registers by ESHRE. Hum Reprod. 2006;21(7):1680–97.
Gnoth C, Maxrath B, Skonieczny T, Friol K, Godehardt E, Tigges J. Final ART success rates: a 10 years survey. Hum Reprod. 2011;26(8):2239–46.
Malizia BA, Hacker MR, Penzias AS. Cumulative live-birth rates after in vitro fertilization. N Engl J Med. 2009;360(3):236–43.
Leridon H. Can assisted reproduction technology compensate for the natural decline in fertility with age? A model assessment. Hum Reprod. 2004;19(7):1549–54.
Ng EHY, Ho PC. Ageing and ART: a waste of time and money? Best Pract Res Clin Obstet Gynaecol. 2007;21(1):5–20.
Sullivan E, Wang Y, Chapman M, Chambers G. Success rates and cost of a live birth following fresh assisted reproduction treatment in women aged 45 years and older, Australia 2002–2004. Hum Reprod. 2008;23(7):1639–43.
Stoop D, Cobo A, Silber S. Fertility preservation for age-related fertility decline. Lancet. 2014;384(9950):1311–9.
Mills M, Rindfuss RR, McDonald P, te Velde E. Why do people postpone parenthood? Reasons and social policy incentives. Hum Reprod Update. 2011;17(6):848–60.
Goldin C, Katz LF. The power of the pill: Oral contraceptives and women’s career and marriage decisions. J Polit Econ. 2002;110(4):730–70.
Bailey MJ. Reexamining the impact of family planning programs on US fertility: Evidence from the War on Poverty and the early years of Title X. Am Econ J Appl Econ. 2012;4(2):62–97.
Daniels K, Jones J, Abma J. Use of emergency contraception among women aged 15–44: United States, 2006–2010. NCHS data brief no 112. 2013. Hyattsville, MD: National Center for Health Statistics.
Blossfeld H-P, Huinink J. Human capital investments or norms of role transition? How women’s schooling and career affect the process of family formation. Am J Sociol. 1991;97(1):143–68.
Kalwij A, Gustafsson S, editors. Education and postponement of maternity: economic analyses for industrialized countries. Dordrecht: Kluwer/Springer; 2006.
Ní Bhrolcháin M, Beaujouan É. Fertility postponement is largely due to rising educational enrolment. Popul Stud. 2012;66(3):311–27.
Berrington A, Stone J, Beaujouan É. Educational differences in timing and quantum of childbearing in Britain: a study of cohorts born 1940–1969. Demogr Res. 2015;33(Article 26):733–64.
Lappegård T, Rønsen M. The multifaceted impact of education on entry into motherhood. Eur J Popul. 2005;21(1):31–49.
Rindfuss RR, Morgan SP, Offut K. Education and the changing age pattern of American fertility. Demography. 1996;33(3):277–90.
Rendall M, Aracil E, Bagavos C, Couet C, DeRose A, DiGiulio P, Lappegård T, Robert-Bobée I, Rønsen M, Smallwood S, Verropoulou G. Increasingly heterogeneous ages at first birth by education in southern European and Anglo-American family-policy regimes: a seven-country comparison by birth cohort. Popul Stud. 2010;64(3):209–27.
Adsera A. Vanishing children: from high unemployment to low fertility in developed countries. Am Econ Rev Pap Proc. 2005;95(2):189–93.
Cooke A, Mills TA, Lavender T. ‘Informed and uninformed decision making’—Women’s reasoning, experiences and perceptions with regard to advanced maternal age and delayed childbearing: a meta-synthesis. Int J Nurs Stud. 2010;47(10):1317–29.
Gregory E. Ready: why women are embracing the new later motherhood. New York: Basic Books; 2007.
Bongaarts J, Sobotka T. A demographic explanation for the recent rise in European fertility. Popul Dev Rev. 2012;38(1):83–120.
VID. European Demographic Data Sheet 2016. Vienna Institute of Demography and IIASA/Wittgenstein Centre for Demography and Global Human Capital. 2016. Accessed www.populationeurope.org
Leopold T, Skopek J. The delay of grandparenthood: a cohort comparison in East and West Germany. J Marriage Fam. 2015;77(2):441–60.
Schmidt L, Sobotka T, Bentzen JG, Nyboe Andersen A. Demographic and medical consequences of the postponement of parenthood. Hum Reprod Update. 2012;18(1):29–43.
Goldstein J, Lutz W, Scherbov S. Long-term population decline in Europe: The relative importance of tempo-effects and generational length. Popul Dev Rev. 2003;29(4):699–707.
Leridon H, Slama R. The impact of a decline in fecundity and of pregnancy postponement on final number of children and demand for assisted reproduction technology. Hum Reprod. 2008;23(6):1312–9.
Te Velde E, Habbema D, Leridon H, Eijkemans M. The effect of postponement of first motherhood on permanent involuntary childlessness and total fertility rate in six European countries since the 1970s. Hum Reprod. 2012;27(4):1179–83.
Beemsterboer SN, Homburg R, Gorter NA, Schats R, Hompes PGA, Lambalk CB. The paradox of declining fertility but increasing twinning rates with advancing maternal age. Hum Reprod. 2006;21(6):1531–2.
Pison G, Monden C, Smits J. Twinning rates in developed countries: trends and explanations. Popul Dev Rev. 2015;41(4):629–49.
Black M, Bhattacharya S. Epidemiology of multiple pregnancy and the effect of assisted conception. Semin Fetal Neonatal Med. 2010;15(6):306–12.
Cook JL, Collins J, Buckett W, Racowsky C, Hughes E, Jarvi K. Assisted reproductive technology-related multiple births: Canada in an international context. J Obstet Gynaecol Can. 2011;33(2):159–67.
Källén B, Finnström O, Lindam A, Nilsson E, Nygren KG, Olausson PO. Trends in delivery and neonatal outcome after in vitro fertilization in Sweden: data for 25 years. Hum Reprod. 2010;25(4):1026–34.
Umstad MP, Hale L, Wang YA, Sullivan EA. Multiple deliveries: The reduced impact of in vitro fertilisation in Australia. Aust N Z J Obstet Gynaecol. 2013;53(2):158–64.
Balasch J, Gratacós E. Delayed childbearing: effects on fertility and the outcome of pregnancy. Curr Opin Obstet Gynecol. 2012;24(3):187–93.
Bianco A, Stone J, Lynch L, Lapinski R, Berkowitz G, Berkowitz RL. Pregnancy outcome at age 40 and older. Obstet Gynecol. 1996;87(6):917–22.
Delbaere I, Verstraelen H, Goetgeluk S, Martens G, De Backer G, Temmerman M. Pregnancy outcome in primiparae of advanced maternal age. Eur J Obstet Gynecol Reprod Biol. 2007;135(1):41–6.
Jacobsson B, Ladfors L, Milsom I. Advanced maternal age and adverse perinatal outcome. Obstet Gynecol. 2004;104(4):727–33.
Luke B, Brown MB. Contemporary risks of maternal morbidity and adverse outcomes with increasing maternal age and plurality. Fertil Steril. 2007;88(2):283–93.
Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M. Maternal age and fetal loss: population based register linkage study. BMJ. 2000;320(7251):1708–12.
de La Rochebrochard E, Thonneau P. Paternal age and maternal age are risk factors for miscarriage; results of a multicentre European study. Hum Reprod. 2002;17(6):1649–56.
Abdalla HI, Burton G, Kirkland A, Johnson MR, Leonard T, Brooks AA, Studd JW. Pregnancy: age, pregnancy and miscarriage: uterine versus ovarian factors. Hum Reprod. 1993;8(9):1512–7.
Schieve LA, Tatham L, Peterson HB, Toner J, Jeng G. Spontaneous abortion among pregnancies conceived using assisted reproductive technology in the United States. Obstet Gynecol. 2003;101(5, Part 1):959–67.
Habbema JDF, Eijkemans MJ, Leridon H, te Velde ER. Realizing a desired family size: when should couples start? Hum Reprod. 2015;30(9):2215–21.
Joseph KS, Allen AC, Dodds L, Turner LA, Scott H, Liston R. The perinatal effects of delayed childbearing. Obstet Gynecol. 2005;105(6):1410–8.
Voigt M, Briese V, Carstensen M, Wolterdorf F, Hallier E, Straube S. Age-specific preterm birth rates after exclusion of risk factors—an analysis of the German Perinatal Survey. Z Geburtshilfe Neonatol. 2010;214(4):161–6.
Heslehurst N, Ells LJ, Simpson H, Batterham A, Wilkinson J, Summerbell CD. Trends in maternal obesity incidence rates, demographic predictors, and health inequalities in 36 821 women over a 15-year period. BJOG Int J Obstet Gynaecol. 2007;114(2):187–94.
Luke B, Brown MB, Nugent C, Gonzalez-Quintero VH, Witter FR, Newman RB. Risk factors for adverse outcomes in spontaneous versus assisted conception twin pregnancies. Fertil Steril. 2004;81(2):315–9.
Pinborg A. IVF/ICSI twin pregnancies: risks and prevention. Hum Reprod Update. 2005;11:575–93.
Mulder CH. Home-ownership and family formation. J Housing Built Environ. 2006;21(3):281–98.
Mulder CH, Billari FC. Homeownership regimes and low fertility. Hous Stud. 2010;25(4):527–41.
Clark WA. Do women delay family formation in expensive housing markets? Demogr Res. 2012;27(1):1–24.
Lino M. Expenditures on children by families, 2013. U.S. Department of Agriculture; 2014. https://www.cnpp.usda.gov/sites/default/files/expenditures_on_children_by_families/crc2013.pdf
Björklund A. Does family policy affect fertility? J Popul Econ. 2006;19(1):3–24.
Joshi H. Production, reproduction and education: Women, children and work in a British perspective. Popul Dev Rev. 2002;28(3):445–74.
Miller AR. The effects of motherhood timing on career path. J Popul Econ. 2011;24(3):1071–100.
Taniguchi H. The timing of childbearing and women’s wages. J Marriage Fam. 1999;61(6):1008–19.
Herr JL. Measuring the effect of the timing of first birth on wages. J Popul Econ. 2016;29(1):39–72.
Engelhardt H, Schreyer J. Timing of first birth and well-being in later life. J Fam Res (Zeitschrift für Familienforschung). 2014;26(3):331–46.
Goisis A, Sigle-Rushton W. Childbearing postponement and child well-being: a complex and varied relationship? Demography. 2014;51(5):1821–41.
Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2012;84(5):478–85.
Mosher WD, Jones J, Abma JC. Intended and unintended births in the United States: 1982–2010. National health statistics reports 55, July 2012; 2012.
Musick K, Michelmore K. Change in the stability of marital and cohabiting unions following the birth of a child. Demography. 2015;52(5):1463–85.
Hansen K, Hawkes D, Joshi H. The timing of motherhood, mothers’ employment and child outcomes. In: Stillwell J, Coast E, Kneale D, editors. Fertility, living arrangements, care and mobility. New York: Springer; 2009. p. 59–70. Chapter 4.
Myrskylä M, Margolis R. Happiness: before and after the kids. Demography. 2014;51(5):1843–66.
Barclay K, Myrskylä M. Advanced maternal age and offspring outcomes: reproductive aging and counterbalancing period trends. Popul Dev Rev. 2016;42(1):69–94.
Grundy E, Kravdal Ø. Reproductive history and mortality in late middle age among Norwegian men and women. Am J Epidemiol. 2008;167(3):271–9.
Jaffe D, Kogan L, Manor O, Gielchinsky Y, Dior U, Laufer N. Influence of late-age births on maternal longevity. Ann Epidemiol. 2015;25(6):387–91.
Lee RD, Goldstein JR. Rescaling the life cycle. Longevity and proportionality. In: Carey JR, Tuljapurkar S, editors. Life span. Evolutionary, ecological and demographic perspectives. Supplement to Popul Dev Rev. 2003;29:183–207.
Mac Dougall K, Beyene Y, Nachtigall RD. ‘Inconvenient biology:’ advantages and disadvantages of first-time parenting after age 40 using in vitro fertilization. Hum Reprod. 2012;27(4):1058–65.
Daly I, Bewley S. Reproductive ageing and conflicting clocks: King Midas’ touch. Reprod Biomed Online. 2013;27(6):722–32.
Menken J. Age and fertility. How late can you wait? Demography. 1985;22(4):469–83.
Acknowledgments
The research by T. Sobotka was funded by the European Research Council under the European Union’s Seventh Framework Programme (FP7/2007-2013)/ERC Grant agreement no 284238 (EURREP project). E. Beaujouan’s contribution was funded by the Austrian Science Fund (FWF), project FWF P28071-G22 (“Running Against the Clock? Realising Family Plans Over the Life-course”). The earlier more extensive draft of this chapter is available as a working paper [30].
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sobotka, T., Beaujouan, É. (2018). Late Motherhood in Low-Fertility Countries: Reproductive Intentions, Trends and Consequences. In: Stoop, D. (eds) Preventing Age Related Fertility Loss. Springer, Cham. https://doi.org/10.1007/978-3-319-14857-1_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-14857-1_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-14856-4
Online ISBN: 978-3-319-14857-1
eBook Packages: MedicineMedicine (R0)