Abstract
The treatment of disease with hematopoietic stem cell transplant is a very intense, multifaceted process that triggers various psychosocial responses and stresses patient’s coping strategies. The course of treatment and its recovery can span over months to years, stretching these patients’ and support persons’ psychosocial capabilities to their limits and beyond. The stages of this process have unique aspects that need understanding and attention. They span from the decision to have a transplant, preparation, treatment, early recovery, and long-term recovery. The psychological health of the caregiver and support system has been shown to be effected in varying degrees and has an impact on the patient as well as themselves. This chapter focuses on the psychosocial issues of the patient along the continuum, as well as the effect on the caregiver.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Hematopoietic stem cell transplant (HSCT) is a complex treatment that often results in high levels of psychological distress and social/financial strain for patients and their families. The procedure and the ensuing recovery can test even the most adaptive functional patient and support system. Indeed, it is the psychosocial issue that can be the most vexing for transplant teams.
HSCT patients and their support teams require information as well as physical and emotional resources in order to maximize the benefit of the procedure. Each patient brings their past medical, emotional, financial, and personal experiences which impact their ability to tolerate the ardors of transplant.
Five phases of the HSCT process have been described:
-
1.
The decision to undergo HSCT
-
2.
Pre-HSCT preparation
-
3.
HSCT hospitalization
-
4.
Hospital discharge and early recovery
-
5.
Long-term recovery
This chapter focuses on the psychosocial issues along this continuum.
Each patient has a unique diagnosis, staging, and comorbidities that affect his/her journey through transplant. Psychologically, an individual adjusts to each transition utilizing their adaptive to maladaptive coping mechanisms. An early study on “returning to normal” revealed that patients least likely to report return to normalcy were those with unrealistic expectations. While there will be patients who will remain unrealistic, a majority can be assisted by providing realistic information and support.
A patient-centered approach is at the forefront of new accreditation standards for hospital cancer programs released by the Commission on Cancer (CoC) of the American College of Surgeons (ACS). Four national cancer patient support/advocacy organizations worked closely with the CoC to develop patient-centered standards to better enable cancer patients to work with their interdisciplinary cancer treatment team: American Cancer Society, Cancer Support Community, National Coalition for Cancer Survivorship, and LIVESTRONG™. The CoC includes Distress Treatment Guidelines for Patients as a standard to be established for accreditation (http://www.facs.org/cancer/coc/whatis.html).
Distress in pre-HSCT patients was first described in 1995 as demonstrated by scores on the Profile of Mood States Scale. Study results showed that a decreased sense of control (intrapersonal mastery) and decreased sense of optimism were related to a higher level of distress. In a 2005 study, it was identified that pre-transplant distress is highly predictive of post-transplant distress, and there was a statistically significant association between self-reported distress and medication noncompliance. The distress thermometer (DT) with HSCT patients, when studied for validation in comparison to the Center for Epidemiological Studies-Depression Scale (CES-D) and the State–Trait Anxiety Inventory-State Version (STAI-S), showed that the single-item DT compares well with the longer measures to assess psychological distress. The DT cutoff score of four supports significant distress to warrant further assessment, and while the DT is being promoted as a screening tool by the National Comprehensive Cancer Network (NCCN), they suggest a cutoff of five or above for further assessment. Additional study is indicated in the HCST population.
Seven causes of distress in patients who undergo HCST have been identified:
-
1.
Uncertainty regarding treatment outcome, recurrence, and mortality
-
2.
Impact of the treatment on their family
-
3.
Changes in appearance and impact on sexuality
-
4.
Long-term burden of treatment such as reduced functional status
-
5.
Interaction with the medical system
-
6.
Communication with medical personnel and obtaining information
-
7.
Financial considerations, such as insurance coverage, the cost of treatment, and supporting self/family
Although no consensus guidelines regarding psychosocial eligibility for HSCT have been developed, there are data-identifying psychosocial factors associated with pre-HSCT vulnerability that influence outcomes. In a study of HSCT clinicians deciding whether to proceed with transplant given specific psychosocial risk factors, 75 % of responding physicians recommended not to proceed in cases of suicidal ideation, use of illicit drugs, and history of noncompliance. Additionally, 69 % recommended not to proceed in cases where no caregiver support was identified.
Psychosocial issues have been studied in the solid organ transplant population, as these patients require psychosocial evaluation prior to being added to the waiting list. In HSCT, autologous or allogeneic donors are used which also require appropriate psychosocial evaluation. Pretransplant screening for HSCT has borrowed from solid organ transplant in the format of the Psychosocial Assessment of Candidates for Transplant (PACT) and Transplant Evaluation Rating Scale (TERS) .
While transplant programs vary in size and funding, there is value in having a mental health professional assess a patient’s ability to withstand the psychological stresses of HSCT, including assessment of preexisting psychiatric morbidities. Individuals with anxiety and depression are at risk for poor health outcomes. Patients who experience overall mood, anxiety, or adjustment disorder have 8 % longer lengths of stay.
1 Psychosocial Evaluation and Assessment
The key aspects for assessment are the characteristics and needs of the patient, family, and caregiver(s), including financial status, employment/disability, insurance, past/current mental health, and/or substance abuse history, and details about their care plan: who, what, and where.
-
1.
Demographics:
-
a.
Marital status
-
b.
Family composition
-
c.
Current living situation
-
d.
Developmental stage
-
e.
Formal education
-
f.
Legal issues
-
g.
Children’s issues/preparation
-
a.
-
2.
Employment and financial information:
-
a.
Employment and/or disability status
-
b.
Source of income
-
c.
Primary wage earner
-
d.
Insurance status
-
e.
Out-of-pocket obligation
-
f.
Prescription coverage
-
g.
Ability to maintain insurance and income
-
h.
Other (alimony, outstanding debts, financial planning, power of attorney, etc.)
-
a.
-
3.
Cognitive/mental health/substance abuse:
-
a.
Cognitive deficits
-
b.
Literacy
-
c.
Learning ability
-
d.
Mental health history
-
e.
Psychiatric medications
-
f.
Counseling or hospitalization history
-
g.
Significant recent stressors (marriage, divorce, death, job loss, moves, etc.)
-
h.
Substance-abuse history
-
a.
-
4.
Coping skills:
-
a.
Strengths/weaknesses
-
b.
Coping approach
-
c.
Avoidance mechanism
-
d.
History of significant losses
-
e.
Use of alternative/complementary treatments
-
f.
Adaptation to illness
-
a.
-
5.
Relationships/support systems:
-
a.
Partner relationship (cohesion)
-
b.
Extended family support/availability
-
c.
Identification of caregivers
-
d.
Familial coping patterns
-
e.
Adaptation
-
f.
Spiritual/faith-based support
-
g.
Cultural traditions, informal, and community support
-
a.
-
6.
Medical concerns:
-
a.
Level of understanding of the HSCT process
-
b.
Decision-making issues (and agreement of support persons)
-
c.
Pain issues
-
d.
Expectations
-
e.
Optimism
-
f.
Ability to make post-HCST plans
-
g.
Advance care planning/directives
-
a.
2 Preparation and Planning
-
1.
Issues:
-
a.
Comprehension of the medical circumstance (e.g., remission vs. recurrence, intensity of therapy, prognosis)
-
b.
Mode of learning of the patient and caregiver (i.e., written or verbal? Are they literate? Is English their primary language?)
-
c.
Informed consent and decision making
-
d.
Anxiety/fear
-
e.
Practical arrangements (e.g., distance from transplant center, housing arrangements, caregiver support)
-
a.
-
2.
Interventions:
-
a.
Education about medical status and proposed treatment, as well as duties and duration of commitment of a caregiver
-
b.
Maximizing information delivery (e.g., repetition, multiple formats including written information, audiovisual aids, support groups, internet sites)
-
c.
Institution-specific expectations and requirements
-
d.
Preparative counseling
-
a.
-
3.
Referrals:
-
a.
Educational classes are a way to reinforce prior teaching and discussions with HSCT staff; orient the patient to the hospital campus, the inpatient unit, and outpatient clinic; begin discharge planning; review advance directives and patient/caregiver agreement forms; and provide a forum to share anxiety and distress .
-
b.
Connect with community resources, i.e., Leukemia & Lymphoma Society, Medicaid, counseling services, etc.
-
c.
HSCT assistance resources available on the internet (see Table 5.1).
-
a.
3 Active Treatment: Inpatient and Outpatient
-
1.
Issues:
-
a.
Patient/caregiver anxiety and uncertainty about the HSCT process and outcome
-
b.
Disruption of patient/family roles
-
c.
Fears of recurrence, infection , death
-
d.
Interpersonal stressors (e.g., poor coping strategies, mental health issues, etc.)
-
e.
Uncertainty about discharge plans
-
a.
-
2.
Interventions:
-
a.
Negotiate personal control
-
b.
Build on previous experiences/successes
-
c.
Ongoing self-assessment and training
-
d.
Educate about outpatient process (e.g., medications, expected appointments, availability of 24-h medical advice/support)
-
a.
4 Immediate Short Term
-
1.
Issues:
-
a.
Transition to outpatient setting post HSCT
-
b.
Increased stress on relationship between patient and caregiver
-
c.
Caregiver burden and feelings of incompetence
-
d.
Patient’s dependency and loss of control
-
e.
Graft-versus-host disease (GVHD) risk in allogeneic recipients
-
a.
-
2.
Interventions:
-
a.
Assess the meaning of uncertainty and stressors
-
b.
Evaluate burdensome tasks
-
c.
Assist patient/family to identify and mobilize available resources
-
d.
Assist in evaluating relationship enhancements
-
e.
Assure continuation of medical support/management in transitions to outpatient setting
-
a.
5 Long Term/Survivorship
-
1.
Issues:
-
a.
Transition back to home, work, and/or previous family roles
-
b.
Changes in patient’s emotional and physical functions due to complications and long-term effects of HSCT
-
c.
Fear of recurrence
-
d.
Feelings of “being different”
-
a.
-
2.
Interventions:
-
a.
Assess transitional needs and provide referrals to the Department of Vocational Rehabilitation, Social Security Disability, etc.
-
b.
Evaluate the effect of complications/late effects on relationships
-
c.
Problem-solve positive steps to build on strengths
-
d.
Assess and support survival techniques
-
e.
Provide support groups and reunions for survivors (NBMTlink webinars, Peer to Peer, BMTinfonet, etc.)
-
a.
6 End-of-Life Care
-
1.
Issues:
-
a.
Emotions including fear, sadness, failure
-
b.
Effects on the family, especially young children
-
c.
Physical changes, pain , comfort
-
d.
Spiritual needs
-
e.
Home versus hospital versus skilled facility
-
a.
-
2.
Intervention:
-
a.
Assess the source of expressed emotions
-
b.
Assess the impact on the family and assist with children, involve child life services when appropriate
-
c.
Foster hope
-
d.
Consider home hospice as an option for patient and family
-
e.
Advocate with provider team and family to meet patient’s wishes as possible
-
a.
-
3.
Special considerations:
-
a.
Patient questioning if they should have had the transplant? Did it matter?
-
b.
Related donor’s grief and feelings about transplant outcome. Are they responsible for the outcome?
-
a.
7 Palliative Care and Hematologic Malignancy
A U.S. retrospective study showed patients with a hematologic malignancy accessed palliative care less frequently than those with solid tumors (11 % vs. 89 % respectively; see Chap. 33). Research suggests that while hematology staff are aware of the needs for palliative care, the lack of access and integration to care has an adverse effect on families and caregivers. Qualitative analysis suggests family members were aware of patient dying, but were reluctant to speak to staff about it and felt inadequately assisted in preparing for the dying experience.
Barriers to integration of palliative care in the setting of hematologic malignancies include:
-
1.
The course of the illness
-
2.
Availability of community resources including hospice support with no reimbursement for palliative care or ongoing transfusion support
-
3.
Unpredictability of the illness
-
4.
Unclear goals of care
-
5.
Availability of early-phase clinical trials and the patient’s comprehension of the study objective
-
6.
Availability of ongoing supportive therapies
-
7.
Psychological dependency and the ongoing relationship between patient/family and providers
Provider skills needed for provision of palliative care:
-
1.
Assessment
-
2.
Information sharing
-
3.
Decision-making capacity
-
4.
Ability to determine patient’s capacity for decision making
-
5.
Ability to clearly define goals of care
-
6.
Capacity for objective discussion of withdrawal of therapy
-
7.
Openness to discussion of Death with Dignity where allowed
-
8.
Advance care planning and delivery
-
9.
Surrogate decision making
-
10.
Conflict resolution
-
11.
Affirmation of patient/family understanding, satisfaction, concerns
8 Caregiving Needs and Requirements
Individuals who undergo HSCT require caregiver support until otherwise told by their transplant provider team. Autologous HSCT recipients typically require a 24-hour caregiver for approximately 2–3 weeks after discharge from the hospital, while allogeneic HSCT recipients may require a caregiver anywhere from 2–6 months depending on complications that may arise.
Changes in health-care delivery systems and policy highlighting reduction of costs have moved much of the HSCT process from the inpatient to the outpatient setting, which may extend the caregiver’s commitment by weeks to months. These changes also add an additional layer of responsibility to the caregiver, as greater involvement during the earlier phases of HSCT is required. Payer contracts may not reimburse for post-HSCT caregiver support. Therefore, the responsibility lies with the patient’s natural supports, i.e., family members or friends. This incredible commitment requires even further time away from work and other personal responsibilities.
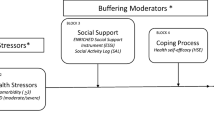
9 Psychosocial Impact of Caregiving and Protective Factors
While there has been a breadth of research that explores the psychosocial implications for the HSCT recipient, less is known about the experience of the caregiver . Research has shown that the psychosocial health of the caregiver has a direct impact on the health and well-being of the patient. Caregivers suffer from anxiety and depression , sleep deprivation and fatigue, sexual dysfunction, and greater vulnerability to illness, and may experience fear, frustration, and isolation. Adaptation of the caregiver is important not only for his/her own wellbeing but also in achieving optimal patient outcomes.
Studies have shown female caregivers tend to report higher levels of distress than male caregivers, because they are more likely to assume the role of primary caregiver while maintaining responsibility for the care of the rest of the family. Additionally, small studies suggest females to be more empathetic.
Control refers to the caregiver’s ability to maintain a sense of predictability and manageability within their life and the lives of their loved ones. Adaptation to the caregiving role, as indicated by lower levels of distress, was noted in caregivers who reported a higher sense of personal control and spiritual well-being. Providing caregivers with detailed information about a patient’s treatment course may offer more predictability. Caregivers who identified with a form of spiritual practice also showed increased adaptation to distress . Their faith allowed them to navigate the burdens of caregiving by applying meaning to their role and the role of illness in the life of their loved one.
Developing strategies and interventions to support caregivers can prove to be an important part of a patient’s care. Support groups, online resources, and web-based tools to assist caregivers in managing their role are emerging. These resources are likely to be more beneficial when provided early in the planning process, as coping patterns established early can prove to be an essential part of the overall effectiveness of stress management.
Bibliography
Andrykowski MA, Brady MJ, Greiner CB, Altmaier EM, Burish TG, Antin JH, et al. “Returning to Normal” following bone marrow transplantation: outcomes, expectations and informed consent. Bone Marrow Transplant. 1995;15:573–81.
Armoogum J, Richarson A, Armes J, A survey of the supportive care needs of informal caregivers of adult bone marrow transplant patients. Support Care Cancer. 2013;21:977–86.
Baker F, Marcellus D, Zabora J, Pollard A, Jodrey D. Psychological distress among adult patients being evaluated for bone marrow transplantation. Psychosomatics. 1997;38:10–9.
Chung HL, Lyckholm LJ, Smith TJ. Review palliative care in BMT. Bone Marrow Transplant. 2009;43:265–73.
Cohen MP, Jenkins D, Holston EC, Carlson ED. Understanding health literacy in patients receiving hematopoietic stem cell transplantation. Oncol Nurs Forum. 2013;40:508–515.
Cooke LG. Creating a palliative/educational session for HCT patients at relapse. Clin J Oncol Nurs. 2011;15:411–7.
Cooke L, Gemmill R, Kravits K, Grant M. Psychosocial issues of stem cell transplant. Semin Oncol Nurs. 2009;25:139–50.
Cooke L, Grant M, Eldredge D, Maziarz R, Nail L. Informal caregiving in HCT patients. Eur J Oncol Nurs. 2011;15(5):500–7.
Eldredge D, Nail L, Maziarz R, Hansen L, Ewing D, Archbold PG. Explaining family careiver role strain following autologous bleood and marrow transplantation. J Psychosocial Oncol. 2006;24:3
Epstein AG, Goldberg GR, Meier DE. Palliative care and hematologic oncology: the promise of collaboration. Blood Rev. 2012;doi:10.1016/j.blre.2012.07.001.
Fadul ND, Osta BE, Dalal S, Poulter VA, Bruera E. Comparison of symptom burden among patients referred to palliative care with hematologic malignancies versus those with solid tumors. J Palliat Med. 2008;3:422–7.
Ferris FD, Bruera E, Cherny N, Cummings C, Currow D, Dudgeon D, et al. Palliative cancer care a decade later: accomplishments, the need, next steps—from the American Society of Clinical Oncology. J Clin Oncol. 2009;27:3052–8.
Fife BL, Monahan PO, Abonour R, Wood LL, Stump TE. Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplant. 2009;43:959–6.
Foster LW, McLellan LJ, Rybicki LA, Dabney J, Welsh E, Bolwell BJ. Allogenic BMT and patient eligibility based on psychosocial criteria: a survey of BMT professionals. Bone Marrow Transplant. 2006;44:223–8.
Foster LW, McLellan LJ, Rybicki LA, Dabney J, Visnosky M, Bolwell BJ. Utility of the psychosocial assessment of the candidates for the transplantation (PACT) scale in allogeneic BMT. Bone Marrow Transplant. 2009;375–80.
Garcia CM, Mumby PB, Thiles S, Stiff PJ. Comparison of early qulaity of life outcomes in autologous and allogenic transplant patients. Bone Marrow Transplant. 2012; 1–6.
Goetzman L, Klaghofer R, Wagner-Huber R, Halter J, Boehler A, Muelhaupt B, et al. Psychosocial vulnerability predicts psychosocial outcome after an organ transplant: results of a prospective study with lung, liver and bone marrow transplant. J Psychosom Res. 2007;62:93–100.
Hill Q. Intensify, resuscitate or palliate: decision making in the critically ill patient with hematological malignancy. Blood Rev. 2010;24:17–25.
Hoodin FK. Factor analysis and validity of the transplant evaluation rating scale in a large bone marrow transplant sample. J Psychosom Res. 2003;54:465–73.
Hoodin HF, Harper FW, Posluszny DM. Allogenic stem cell transplantation, contemporary hematology. Chap. 35, Psychological Care of Adult Allogeneic Transplant. New York: Springer Science + Business Media, LLC; 2010.
Howell D, Shellens R, Roman E, Garry A, Patmore R, Howard M. Haematological malignancy: are patients appropriately referred for specialist palliative and hospice care? A systematic review and meta analysis of published data. Palliative Med. 2010;25(6):630–41.
Manitta VJ, Phillip JA, Cole-Sinclair MF. Palliative care and the hemato-oncological patient: can we live together? a review of the literature. J Palliative Med. 2010;13(8):1021–5.
McGrath P. Palliative care for patients with hematological malignancies-if not, why not? J Palliative Care. 1999;15:24–30.
McGrath P, Holewa H. Special considerations for haematology patients in relation to end of life care: Australian findings. Eur J Cancer Care. 2007;16:164–71.
Morishita S, Kaida K, Yamauchi S, Wakasugi T, Yoshihara S, Taniguchi K, et al. Gender difference in health-related quality of life, physical function and psychological status among patients in the early phase following allogenic haematopoietic stem cell transplantion. Psycho-Oncology. 2012;doi:10.1002/pon.312B.
Mosher CR, Redd WH, Rini CM, Burkhalter JE, DuHamel KN. Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psycho-Oncol. 2009;18:113–27.
Niederbacher ST, Tem C, Pinna A, Vittadello F, Mantovan F. Patient's quality of life after allogenic haematopoietic stem cell transplantation: mixed-methods study. Eur Cancer Care. 2012;21:548–59.
Presberg BM, Levenson JL, Olbrisch ME, Best AM. Rating scales for the psychosocial evaluation of organ transplant candidates. Psychosomatics. 1995;36:458–61.
Prieto JM, Atala J, Blanch J, Carreras E, Rovira M, Cierra E, et al. Role of depression as a predictor of mortality among cancer patients after stem cell transplantation. J Clin Oncol. 2005;23:6063–71.
Prieto JM, Atala J, Blanch J, Carreras E, Rovira M, Cierra E, et al. Stem cell transplantation: risk factors for psychiatric morbidity. Eur Cancer Care. 2006;42:514–20.
Ransom S, Jacobsen P, Booth-Jones M. Validation of the distress thermometer with bone marrow transplant patients. Psycho-Oncol. 2006;15:604–12.
Siegel S. Psychosocial considerations in Hematopoietic stem cell transplantation: implications for patient quality of life and post-transplant survival. Comm Oncol. 2008;5:407–8.
Twillman RP, Manetto C, Wellisch DK, Wolcott DL. The transplant evaluation rating scale: a revision of the psychosocial levels system for evaluating organ transplant candidates. Psychomatics. 1993;144–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Boyle, N., McCord, K. (2015). Social Work: Evaluation and Support. In: Maziarz, R., Slater, S. (eds) Blood and Marrow Transplant Handbook. Springer, Cham. https://doi.org/10.1007/978-3-319-13832-9_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-13832-9_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-13831-2
Online ISBN: 978-3-319-13832-9
eBook Packages: MedicineMedicine (R0)