Abstract
Early unfavorable or intermediate-stage Hodgkin lymphoma usually includes patients in stages I and IIA with clinical risk factors such as large mediastinal mass, extranodal disease, high ESR, or more than three or four nodal areas involved. In addition, selected stage IIB patients are also included in this risk group. The current treatment for these patients is based on four cycles of ABVD chemotherapy followed by involved-field radiotherapy. A more aggressive approach with two cycles of BEACOPP escalated followed by two cycles of ABVD has recently shown better tumor control but no advantage in overall survival yet. More cycles of chemotherapy have not resulted in better outcome in early unfavorable patients. One of the major current controversies in this risk group is the use of PET to guide treatment intensity or the use of additional radiotherapy in PET-negative patients. This chapter will give you an overview on the past and current treatment approaches and will highlight the discussion on PET-guided treatment in these patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Combine Modality
- Combine Modality Treatment
- German Hodgkin Study Group
- Combine Modality Approach
- Stanford Versus
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Early unfavorable or intermediate-stage Hodgkin lymphoma usually includes patients in stages I and IIA with clinical risk factors such as large mediastinal mass, extranodal disease, high ESR, or more than three or four nodal areas involved. In addition, selected stage IIB patients are also included in this risk group. The current treatment for these patients is based on four cycles of ABVD chemotherapy followed by involved-field radiotherapy. A more aggressive approach with two cycles of BEACOPP escalated followed by two cycles of ABVD has recently shown better tumor control but no advantage in overall survival yet. More cycles of chemotherapy have not resulted in better outcome in early unfavorable patients. One of the major current controversies in this risk group is the use of PET to guide treatment intensity or the use of additional radiotherapy in PET-negative patients. This chapter will give you an overview on the past and current treatment approaches and will highlight the discussion on PET-guided treatment in these patients.
2 Why Early Unfavorable?
The Ann Arbor staging system with the 1989 Cotswolds modifications [1] is still being used worldwide in the staging of patients with HL. Modern staging procedures recommend the routine use of FDG-PET/CT scanning at diagnosis [2]. Through the introduction of FDG-PET/CT scanning at diagnosis, patients will be upstaged in up to 30 % mainly from early to advanced stages. In addition, the extent of radiation fields in CS I/II disease can be influenced by identifying additional lesions by FDG-PET scanning [2, 3]. In the past, patients with limited-stage I/II disease were treated with extended-field radiotherapy (RT), whereas those with more advanced stage III or IV received multi-agent chemotherapy. Up to the 1990s of the twentieth century, staging laparotomy was performed to more reliably identify patients with disease truly limited to one side of the diaphragm. The successful introduction of chemotherapy in advanced stages and its potential to eradicate occult disease, the relapse rates of up to 30 % after extended-field RT alone, and the increasing awareness of serious long-term toxicity after extended-field RT promoted the development of combined modality treatment approaches. Combined modality has the evident advantage of combining two efficacious treatment modalities. It is given as combination of a fixed number of chemotherapy cycles followed by a certain dose and extent of RT. As a result, the extent of both RT and chemotherapy could be reduced in the combined treatment design as compared to administering single-treatment modalities. However, even in stage I/II, the extent of disease varies substantially requiring a risk-adapted treatment. In many early-stage patients, mediastinal bulky disease is present, which has been demonstrated as prognostically unfavorable. Other poor prognostic clinical factors include higher age, increased number of involved nodes, and elevated erythrocyte sedimentation rate (ESR), accompanied by B symptoms. Though slight differences in definition exist between major cooperative groups, CS I/II HL patients in Europe are generally divided into an early favorable and an early unfavorable (intermediate) subgroup. In contrast, patients in North America presenting with adverse factors (mainly the presence of bulky disease) are treated like stage III–IV disease and are not included in clinical trials for CS I/II disease. At present, progression-free survival rates of 85–90 % are common for patients with unfavorable CS I/II disease treated with a combined modality approach.
3 Prognostic Factors
The factors used by the European Organisation for Research and Treatment of Cancer (EORTC) Lymphoma Group, the German Hodgkin Study Group (GHSG), the National Cancer Institute of Canada (NCIC), and the Eastern Cooperative Oncology Group (ECOG) are shown in Table 12.1 [1, 4]. We have to bear in mind that these risk factors and the resulting prognostic groups were originally defined in the context of treatment with extended-field RT. In a combined modality setting, the differences in prognosis between favorable and unfavorable disease are likely to be smaller. Moreover, in more recent series, the treatment had already been tailored according to the prognostic groups. Thus, one would have anticipated that these prognostic factors today have less independent prognostic significance. However, a large randomized trial included a joint experimental treatment arm for both favorable and unfavorable subgroups, thus possibly addressing the current impact of predictive factors. In this trial, EORTC H7 [5], the unfavorable subset of patients was randomized between six cycles of EBVP (epirubicin, bleomycin, vinblastine, prednisone), a combination presumed to be less toxic and equally effective to ABVD [6], and six cycles of MOPP/ABV (mechlorethamine, vincristine, procarbazine, prednisone, Adriamycin, bleomycin, vinblastine, and dacarbazine), both followed by 30–36 Gy involved-field RT (IF-RT). After a median follow-up of 9 years, patients treated with EBVP had a significantly higher rate of tumor progression and relapse than those treated with MOPP/ABV resulting in a significantly inferior 10-year event-free survival (EFS) of 68 vs. 88 % (p < 0.001) (Fig. 12.1, upper chart). The favorable subset of patients was randomized between six cycles of EBVP followed by IF-RT and subtotal nodal irradiation (STNI), considered standard treatment at the time of initiation of the trial. Those treated with EBVP had a superior 10-year EFS compared to patients treated with STNI alone: 88 vs. 78 % (p = 0.01) (Fig. 12.1 lower chart). While the less toxic EBVP regimen produced superior results in the favorable subset of patients, the poor results in the unfavorable patients reflect the necessity for a more potent and intense treatment for this subgroup. Thus, the clinical relevance of the prognostic factors appeared to be maintained. Indirect evidence for the impact of discriminating between favorable and unfavorable early stages can be found in two other trials including patients with adverse prognostic factors, though differently defined. In a trial performed by the Grupo Argentino de Tratamiento de la Leucemia Aguda (GATLA), the less intense AOPE (Adriamycin, vincristine, prednisone, and etoposide) proved inferior to CVPP (cyclophosphamide, vincristine, procarbazine, prednisone) [7]. The Southwestern Oncology Group trial 9051 tested a less toxic combination of etoposide, vinblastine, and Adriamycin (EVA) followed by STNI and found an unacceptably high relapse rate mainly in non-irradiated areas indicating the inferiority of the chemotherapy [8]. Klimm et al. analyzed the impact of the three different staging and prognostic subgroup definitions on the outcome of 1,173 early-stage patients treated homogeneously in the HD10 and HD11 trials of the GHSG [9]. Figure 12.2 shows the PFS of these patients related to the GHSG, EORTC, and NCCN prognostic risk factors score, respectively: all three staging systems identified the unfavorable risk group. Especially tumor-specific (rather than patient-specific) risk factors such as mediastinal bulk and high tumor activity were predictive for poor outcome. For overall survival, the scores reflected the unfavorable risk profile as well (figures not shown). These data underline the continued usefulness of identifying a poor-risk group within the group of stage I/II disease though new risk factors with a higher specificity are needed.
In the upper chart, the estimated progression-free (PFS) (a) and overall survival (OS) (b) of the European Organisation for Research and Treatment of Cancer (EORTC) H7 randomized trial: MOPP/ABV vs. EBVP + involved-field radiotherapy in the unfavorable risk group are given; for comparison in the lower chart, the PFS (c) and OS (d) of the favorable risk groups are given for the EBVP + involved-field radiotherapy treatment arm vs. extended-field radiotherapy alone treatment arm [5]
Estimated progression-free survival using staging definitions of the German Hodgkin Study Group, the European Organisation for Research and Treatment of Cancer (EORTC), or National Comprehensive Cancer Network (NCCN) [9]
4 Chemotherapy Regimens
After the initial Bonadonna report on ABVD [10] and the randomized trial on ABVD vs. MOPP vs. MOPP/ABVD in advanced disease [11], the NCIC/ECOG intergroup trial on ABVD vs. MOPP/ABV hybrid set the stage for ABVD as standard chemotherapy due to equal efficacy but less toxicity as compared with MOPP/ABV [12]. In an attempt to reduce toxicity even further, the GOELAMS (Groupe Ouest-Est d’Étude des Leucémies et Autres Maladies du Sang) included both early favorable and unfavorable patients in their H90-NM study [13]. A total of 386 patients were randomized between ABVDm (ABVD plus methylprednisolone) and the potentially less toxic EBVMm, followed by extended-field RT in responding patients. The ABVDm arm proved to be superior to the EBVMm treatment in terms of complete remission rates and FFS. Very similar to the conclusions of the EORTC H7 trial, these results highlight the need for sufficiently effective chemotherapy. Notwithstanding concerns on toxicity of chemotherapy and a reluctance to apply more intense treatment in CS I/II disease, one could argue that a 10–15 % failure rate in the unfavorable subset of patients is too high and warrants improvement. In this respect, the trials summarized in Table 12.2 are important. Both the EORTC H9U and the GHSG HD11 studies failed to show a significant PFS advantage for more intensive treatment comparing four cycles of BEACOPP baseline with four cycles of conventional ABVD [14, 15]. The GHSG follow-up trial for early unfavorable patients, HD14, compared four cycles of ABVD with two cycles of BEACOPP escalated followed by two cycles of ABVD (“2 + 2”). The decision for this combination was in part based on the higher effective dose (ED) model calculations [8, 19]. Here, four cycles of ABVD given over 16 weeks have an ED of 15 as compared with 15.2 for four cycles of BEACOPP baseline given over 12 weeks. In contrast, the “2 + 2” variant has an ED of 17.3. In both treatment arms of the HD14 study, additional IF-RT with 30 Gy was given. The final analysis demonstrated a significantly better PFS for the more intensive “2 + 2” arm: PFS at 5 years was 95.4 % with “2 + 2” treatment compared with 89.1 % after ABVD (p < 0.001) [20]. While an absolute improvement in PFS of 6 % appears rather modest at first glance and one can argue about clinical relevance, the results show that even an up-front intensification with only two cycles of BEACOPP escalated indeed improves outcome in this group of patients. It corroborates the claim for a start of treatment with the most effective regimen to prevent the development of early chemoresistance, but it remains to be seen whether this gain in PFS outbalances the putative increased toxicity, for example, infertility and secondary malignancies. Whether the 12-week intense chemotherapy regimen Stanford V, with its mainly alkylating-agent-induced toxicity, could improve treatment outcome as compared with ABVD was addressed in the US intergroup study [16]. In this trial only 30 % of patients had stage I/II disease; the remaining were in stage III/IV. No benefit for the Stanford V over ABVD was observed. Intensification from ABVD to BEACOPP escalated dependent of persistent FDG-PET scan positivity after two cycles of ABVD is being addressed in EORTC/LYSA/FIL randomized H10 trial. Final results are not yet available (vide infra). So, the more intense BEACOPP escalated based “2 × 2” design reports a superior PFS suggesting that it is indeed possible to improve efficacy in this group of patients albeit at the cost of increased toxicity.
5 Number of Cycles of Chemotherapy
Only a few randomized trials have addressed the issue of number of cycles required. These studies show that four cycles of conventional chemotherapy are sufficient in a combined modality setting. In the EORTC/GELA H8U study, MOPP/ABV hybrid was used as standard chemotherapy regimen; four or six cycles followed by IF-RT were compared [21]. The EFS at 7 years did not differ significantly with rates of 86 and 84 %, respectively (Fig. 12.3). In the EORTC/GELA H9U trial, 533 patients were randomized between four and six cycles of ABVD followed by IF-RT [14]. The interim analysis showed an EFS of 87 and 91 % at 4 years, which was not significantly different. While some cooperative groups consider early unfavorable CS I/II disease as advanced stage and treat accordingly with six cycles of chemotherapy, a number of four cycles in a combined modality setting are currently considered standard treatment.
Estimated event-free (a) and overall survival (b) of the unfavorable cohort of patients enrolled in the European Organisation for Research and Treatment of Cancer (EORTC) and Groupe d’Etude des Lymphomes de l’Adulte (GELA) randomized H8 trial comparing different numbers of cycles of chemotherapy combined with different radiation fields [21]
6 Extent and Dose of RT
A number of randomized trials focused on the comparison of extended- and IF-RT in combined modality approaches (Table 12.3) [22, 24]. The important general conclusion from these trials was that extended-field RT was not needed in combined modality treatment and was associated with more long-term adverse effects. Thus, IF-RT became the standard of care in this setting. Meanwhile, the concept of involved-node irradiation (IN-RT) was introduced by the EORTC as part of the combined modality approach. The irradiated volume is further reduced to involved nodes instead of a complete lymphoid region and consequently less late adverse effects are anticipated [18]. The concept has been applied already in the EORTC/LYSA/FIL H10 trial (vide infra), but it has not yet been tested in a randomized trial.
In the era of extended-field RT as single modality, the standard dose of RT was 36 Gy, often followed by a boost of 4–6 Gy to residual disease and/or initial bulky sites. When combined with chemotherapy, both the field size and the RT dose could be reduced. In the GHSG HD11 trial, four cycles of ABVD or four cycles of BEACOPP baseline were followed by IF-RT, either 30 or 20 Gy dose. The final analysis showed no significant difference in PFS between the 30 and 20 Gy treatment arms for those patients receiving BEACOPP baseline. In contrast, those treated with four cycles of ABVD and 20 Gy IF-RT had a poorer tumor control as compared to those receiving 30 Gy IF-RT (p = 0.048) [15]. In the EORTC/GELA H9F trial randomizing between a dose of 36 and 20 Gy of IF-RT after EBVP chemotherapy, no differences in PFS were seen in the interim analysis, but this trial included only favorable stage I/II disease [14]. Thus, the dose of IF-RT needed in the combined modality treatment of early unfavorable HL depends on the efficacy of the preceding chemotherapy. To conclude, the extent and dose of RT can be reduced only in the appropriate combined modality treatment setting: adequate chemotherapy is the first prerequisite, then IF-RT can be given at a reduced dose of 20 Gy, or alternatively IN-RT can be preferred but—at least for the moment—at the higher dose of 30–36 Gy.
7 Chemotherapy Alone
Several randomized trials performed in patients with advanced stages indicated that RT can be omitted without compromising outcome, providing a robust CR was achieved with six to eight cycles of chemotherapy such as MOP/BAP, MOPP/ABV hybrid, or BEACOPP escalated [25, 26]. Positron emission tomography (PET) holds the promise of predicting more accurately which remission is robust and if residual masses will benefit from additional RT [27]. Conflicting data came out of a study from India [28]. Here, six cycles of ABVD were followed for patients in CR by IF-RT or no RT in a randomized fashion. Though patients who received RT had a significantly better PFS than those who did not, this study included many early stages, pediatric patients, and used suboptimal imaging methods. These data suggest that after an adequate number of cycles of effective chemotherapy and good response, additional RT will not further improve the outcome in patients with advanced-stage disease. The question therefore arose whether RT can also be omitted in unfavorable early stages. Table 12.4 summarizes the results of the most relevant trials, all having their limitations. In the GATLA study [29], a nonstandard chemotherapy was used; other studies included pediatric patients or all stages of disease, used divergent definitions of unfavorable prognostic features, or had not enough statistical power to detect clinically significant differences in PFS between RT and no-RT arms. The NCIC/ECOG study on early stages had 12-year overall survival as primary endpoint; patients with bulky disease were excluded from entry. This study showed a significant 11 % survival benefit for treatment with ABVD alone as compared to ABVD+STNI, notwithstanding a significant 8 % advantage in PFS for those who received combined modality approach [33]. The remarkable conversion of an inferior PFS to a superior long-term OS for the ABVD alone treatment arm was mainly due to an excess of late toxic deaths in the combined modality treatment: 23 vs. 11 in the former. These deaths were mainly due to second cancers. Admittedly, STNI is outdated now, but the results corroborate the difficulties in interpreting different treatment approaches with divergent short-term (control of disease) and long-term (toxicity) effects.
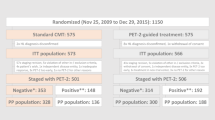
This dilemma was also encountered in the EORTC/LYSA/FIL randomized H10 trial. Based on the prognostic significance of an early FDG-PET scan, investigators hypothesized that patients who attain a negative FDG-PET scan after two cycles of ABVD would not need additional RT. Therefore, patients in the standard arm received standard combined modality treatment (ABVDx4+IN-RT) irrespective of the result of the early FDG-PET scan, whereas those in the experimental arm in case of a negative early FDG-PET scan had no IN-RT but instead a total of six cycles of ABVD. In this non-inferiority trial, a decrease of maximally 10 % in 3-year EFS was accepted as non-inferiority margin in an attempt to compensate for the presumed long-term benefit of omitting RT. The preplanned interim analysis after 22 events revealed a 74 % rate of early FDG-PET scan negativity [35]. The median follow-up at the time of analysis was 1.1 years. In the standard arm, less events occurred than in the experimental no-RT arm: 7 events out of 251 patients in the standard arm against 16 out of 268 in the no-RT arm (p = 0.026). Based on these results, it was unlikely that the trial would show non-inferiority for the experimental arm when continuing accrual to the originally planned total numbers and randomization was stopped. Thus, although overall outcome was excellent in both arms, omitting radiotherapy in early FDG-PET-negative patients with unfavorable stage I/II disease resulted in more early progressions than combined modality treatment. An individual patient-data comparison of combined modality and ABVD alone, including also early favorable stages, performed on the GHSG HD10 and HD11 and the NCIC HD trial confirmed the better short-term disease control for combined modality treatment over chemotherapy alone [36]. Until there is generally accepted evidence that RT can really be omitted in—subsets of identifiable—unfavorable stage I/II patients without jeopardizing the long-term outcome, combined modality treatment remains the preferred treatment approach.
8 Special Situations
8.1 Bulky Mediastinal Tumor
The presence of a bulky mediastinal tumor, defined as a mediastinum/thorax ratio of ≥0.35, is one of the most prominent negative prognostic factors in HL patients with CS I/II disease. Some groups treat these patients according to protocols for advanced disease. Upon treatment, the nodular sclerosing histology is associated with inherent slow regression particularly of bulky mediastinal tumors. When evaluated by conventional CT scans, a reliable and reproducible interpretation of response after chemotherapy is often difficult. In case of post-chemotherapy residual masses with uncertain dignity, investigators may easily conclude a partial remission and advocate additional RT. That would possibly not be wrong from a tumor control point of view; however, mediastinal radiation fields are typically associated with severe adverse long-term effects such as secondary malignancies (e.g., breast and bronchus carcinoma) and early cardiovascular events (see Chaps. 22 and 23 for more details). There are no randomized data specifically addressing the need for RT in patients with bulky mediastinal disease based on modern imaging techniques. Although being a single-arm study on a fixed combined modality approach, the experience with Stanford V chemotherapy followed by IF-RT provides the most appropriate data in this respect, including response evaluation with FDG-PET [37]. Patients with a persistent positive FDG-PET scan after Stanford V had a significantly higher relapse rate even after additional IF-RT when compared to those patients with a negative FDG-PET scan post-chemotherapy who also received RT as planned.
In future studies, patients who really need additional RT and those who will not benefit might be better identified by FDG-PET-based response evaluation. This would hopefully secure optimal tumor control and spare subgroups of patients already cured by chemotherapy alone from long-term RT-induced toxicity. For the time being, however, combined modality treatment remains the standard treatment for patients with CS I/II disease with bulky mediastinal disease.
8.2 Concomitant Disease
For patients who cannot tolerate chemotherapy or for whom chemotherapy is contraindicated due to concomitant disease, large-field RT at doses of 36–40 Gy is still an alternative treatment option. However, patients with unfavorable CS I/II disease have a relapse rate of more than 40 % after RT alone and will probably also experience considerable toxicity from large-field RT. Thus, a balance on an individual basis between tumor control and avoidance of serious toxicity has to be found.
9 Future
The most important challenge is the identification of patients who are adequately treated with ABVD alone, those who need combined modality treatment, and those who need intensified chemotherapy such as BEACOPP escalated. The results from the GHSG HD14 study show that more intense chemotherapy significantly improves tumor control. On the other hand, in these patients with localized disease, we also aim at minimizing early and late toxicity of treatment. New clinical prognostic factors are unlikely to allow for selecting patients needing more or less intensive treatment. Biomarkers could become useful, but at present no individual marker or set of markers has been sufficiently reliable. New functional imaging techniques will very likely become valid tools to identify subsets of patients requiring different treatment approaches early in the course of treatment (see Chap. 7). The EORTC/LYSA/FIL H10 trial on early treatment adaptation in early FDG-PET scan-negative patients was prematurely closed because of more events in the no-RT arm as compared to the combined modality approach [35].
In the meantime, new RT techniques will further evolve, and especially the reduction of the involved-field to the involved-node principle in the combined modality treatment setting will reduce toxicity while—probably—maintaining the high efficacy [18] (see Chap. 9). It remains to be seen whether refinement in the use of FDG-PET scanning, for example, by incorporating SUV values, will increase its predictive power for early treatment optimization. Ultimately, an individualized approach taking into account the risk factors and perspectives of the individual patient will define the most appropriate treatment out of a choice of treatments [38, 39].
References
Lister TA, Crowther D, Sutcliffe SB, Glatstein E, Canellos GP, Young RC et al (1989) Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin’s disease: cotswolds meeting. J Clin Oncol 7(11):1630–1636
Kostakoglu L, Cheson BD (2014) Current role of FDG PET/CT in lymphoma. Eur J Nucl Med Mol Imaging 41:1004–1027
Stevens WB, van Krieken JH, Mus RD, Arens AI, Mattijssen V, Oosterveld M et al (2012) Centralised multidisciplinary re-evaluation of diagnostic procedures in patients with newly diagnosed Hodgkin lymphoma. Ann Oncol 23(10):2676–2681
Specht L, Raemaekers J (2007) Do we need an early unfavorable (intermediate) stage of Hodgkin’s lymphoma? Hematol Oncol Clin N Am 21(5):881–896
Noordijk EM, Carde P, Dupouy N (2006) Combined-modality therapy for clinical stage I or II Hodgkin’s lymphoma: long-term results of the European Organisation for Research and Treatment of Cancer H7 randomized controlled trials. J Clin Oncol 24:3128–3135
Hoerni B, Orgerie MB, Eghbali H, Blanc CM, David B, Rojouan J et al (1988) New combination of epirubicin, bleomycin, vinblastine and prednisone (EBVP II) before radiotherapy in localized stages of Hodgkin’s disease. Phase II trial in 50 patients. Bull Cancer 75(8):789–794
Pavlovsky S, Schvartzman E, Lastiri F (1997) Randomized trial of CVPP for three versus six cycles in favorable- prognosis and CVPP versus AOPE plus radiotherapy in intermediate-prognosis untreated Hodgkin’s disease. J Clin Oncol 15:2652–2658
Wasserman TH, Petroni GR, Millard F (1999) Sequential chemotherapy (etoposide, vinblastine, and doxorubicin) and subtotal lymph node radiation for patients with localized stages of Hodgkin’s disease and unfavorable prognostic features: a phase II cancer and leukemia group B study. Cancer J 86:1590–1595
Klimm B, Goergen H, Fuchs M, von Tresckow B, Boll B, Meissner J et al (2013) Impact of risk factors on outcomes in early-stage Hodgkin’s lymphoma: an analysis of international staging definitions. Ann Oncol 24(12):3070–3076
Bonadonna G, Zucali R, Monfardini S, De Lena M, Uslenghi C (1975) Combination chemotherapy of Hodgkin’s disease with adriamycin, bleomycin, vinblastine, and imidazole carboxamide versus MOPP. Cancer 36(1):252–259
Canellos GP, Niedzwiecki D (2002) Long-term follow-up of Hodgkin’s disease trial. N Engl J Med 346(18):1417–1418
Duggan DB, Petroni GR, Johnson JL, Glick JH, Fisher RI, Connors JM et al (2003) Randomized comparison of ABVD and MOPP/ABV hybrid for the treatment of advanced Hodgkin’s disease: report of an intergroup trial. J Clin Oncol 21(4):607–614
Le Maignan C, Desablens B, Delwail V (2004) Three cycles of adriamycin, bleomycin, vinblastine, and dacarbazine (ABVD) or epirubicin, bleomycin, vinblastine, and methotrexate (EBVM) plus extended field radiation therapy in early and intermediate Hodgkin disease: 10-year results of a randomized trial. Blood 103:58–66
Thomas J, Ferme C, Noordijk E (2007) Results of the EORTC-GELA H9 randomized trials: the H9-F trial (comparing 3 radiation dose levels) and H9-U trial comparing 3 chemotherapy schemes) in patients with favorable or unfavorable early stage Hodgkin’s lymphoma. Haematologica 92(ABS):27
Borchmann P, Diehl V, Goergen H (2009) Combined modality treatment with intensified chemotherapy and dose-reduced involved field radiotherapy in patients with early unfavourable Hodgkin lymphoma (HL): final analysis of the German Hodgkin Study Group (GHSG) HD11 trial. Blood 114(abs):299–300
Gordon LI, Hong F, Fisher RI, Bartlett NL, Connors JM, Gascoyne RD et al (2013) Randomized phase III trial of ABVD versus Stanford V with or without radiation therapy in locally extensive and advanced-stage Hodgkin lymphoma: an intergroup study coordinated by the Eastern Cooperative Oncology Group (E2496). J Clin Oncol 31(6):684–691
Engert A, Borchmann P, Plütschow A, Fuchs M, Markova J, Lohri A et al (2009) Treatment with 2 cycles of BEACOPPesc followed by 2 cycles of ABVD and IF-RT is superior to 4 cycles of ABVD and IF-RT in patients with early unfavourable Hodgkin lymphoma (HL): an analysis of the German Hodgkin Study Group (GHSG) HD14 trial. Onkologie 32(Suppl 4):1–254
Girinsky T, van der Maazen R, Specht L, Aleman B, Poortmans P, Lievens Y et al (2006) Involved-node radiotherapy (INRT) in patients with early Hodgkin lymphoma: concepts and guidelines. Radiother Oncol 79(3):270–277
Hasenclever D, Loeffler M, Diehl V (1996) Rationale for dose escalation of first line conventional chemotherapy in advanced Hodgkin’s disease. German Hodgkin’s Lymphoma Study Group. Ann Oncol 7:95–98
von Tresckow B, Plutschow A, Fuchs M, Klimm B, Markova J, Lohri A et al (2012) Dose-intensification in early unfavorable Hodgkin’s lymphoma: final analysis of the German Hodgkin Study Group HD14 trial. J Clin Oncol 30(9):907–913
Ferme C, Eghbali H, Meerwaldt JH, Rieux C, Bosq J, Berger F et al (2007) Chemotherapy plus involved-field radiation in early-stage Hodgkin’s disease. N Engl J Med 357(19):1916–1927
Engert A, Schiller P, Josting A, Herrmann R, Koch P, Sieber M et al (2003) Involved-field radiotherapy is equally effective and less toxic compared with extended-field radiotherapy after four cycles of chemotherapy in patients with early-stage unfavorable Hodgkin’s lymphoma: results of the HD8 trial of the German Hodgkin’s Lymphoma Study Group. J Clin Oncol 21(19):3601–3608
Bonadonna G, Bonfante V, Viviani S, Di Russo A, Villani F, Valagussa P (2004) ABVD plus subtotal nodal versus involved-field radiotherapy in early-stage Hodgkin’s disease: long-term results. J Clin Oncol 22(14):2835–2841
Anselmo AP, Cavalieri E, Osti FM, Cantonetti M, De Sanctis V, Alfo M et al (2004) Intermediate stage Hodgkin’s disease: preliminary results on 210 patients treated with four ABVD chemotherapy cycles plus extended versus involved field radiotherapy. Anticancer Res 24(6):4045–4050
Aleman BM, Raemaekers JM, Tirelli U, Bortolus R, van ’t Veer MB, Lybeert ML et al (2003) Involved-field radiotherapy for advanced Hodgkin’s lymphoma. N Engl J Med 348(24):2396–2406
Diehl V, Franklin J, Pfreundschuh M, Lathan B, Paulus U, Hasenclever D et al (2003) Standard and increased-dose BEACOPP chemotherapy compared with COPP-ABVD for advanced Hodgkin’s disease. N Engl J Med 348(24):2386–2395
Kobe C, Dietlein M, Franklin J, Markova J, Lohri A, Amthauer H et al (2008) Positron emission tomography has a high negative predictive value for progression or early relapse for patients with residual disease after first-line chemotherapy in advanced-stage Hodgkin lymphoma. Blood 112(10):3989–3994
Laskar S, Gupta T, Vimal S, Muckaden MA, Saikia TK, Pai SK et al (2004) Consolidation radiation after complete remission in Hodgkin’s disease following six cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine chemotherapy: is there a need? J Clin Oncol 22(1):62–68
Pavlovsky S, Maschio M, Santarelli MT (1988) Randomized trial of chemotherapy versus chemotherapy plus radiotherapy for stage I-II Hodgkin’s disease. J Natl Cancer Inst 80:1466–1473
Aviles A, Delgado S (1998) A prospective clinical trial comparing chemotherapy, radiotherapy and combined therapy in the treatment of early stage Hodgkin’s disease with bulky disease. Clin Lab Haematol 20(2):95–99
Nachman JB, Sposto R, Herzog P, Gilchrist GS, Wolden SL, Thomson J et al (2002) Randomized comparison of low-dose involved-field radiotherapy and no radiotherapy for children with Hodgkin’s disease who achieve a complete response to chemotherapy. J Clin Oncol 20(18):3765–3771
Straus DJ, Portlock CS, Qin J, Myers J, Zelenetz AD, Moskowitz C et al (2004) Results of a prospective randomized clinical trial of doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) followed by radiation therapy (RT) versus ABVD alone for stages I, II, and IIIA nonbulky Hodgkin disease. Blood 104(12):3483–3489
Meyer RM, Gospodarowicz MK, Connors JM, Pearcey RG, Wells WA, Winter JN et al (2012) ABVD alone versus radiation-based therapy in limited-stage Hodgkin’s lymphoma. N Engl J Med 366(5):399–408
Meyer RM, Gospodarowicz MK, Connors JM, Pearcey RG, Bezjak A, Wells WA et al (2005) Randomized comparison of ABVD chemotherapy with a strategy that includes radiation therapy in patients with limited-stage Hodgkin’s lymphoma: National Cancer Institute of Canada Clinical Trials Group and the Eastern Cooperative Oncology Group. J Clin Oncol 23(21):4634–4642
Raemaekers JM, Andre MP, Federico M, Girinsky T, Oumedaly R, Brusamolino E et al (2014) Omitting radiotherapy in early positron emission tomography-negative stage I/II Hodgkin lymphoma is associated with an increased risk of early relapse: clinical results of the preplanned interim analysis of the randomized EORTC/LYSA/FIL H10 trial. J Clin Oncol 32:1188–1194
Hay AE, Klimm B, Chen BE, Goergen H, Shepherd LE, Fuchs M et al (2013) An individual patient-data comparison of combined modality therapy and ABVD alone for patients with limited-stage Hodgkin lymphoma. Ann Oncol 24(12):3065–3069
Horning SJ, Hoppe RT, Breslin S, Bartlett NL, Brown BW, Rosenberg SA (2002) Stanford V and radiotherapy for locally extensive and advanced Hodgkin’s disease: mature results of a prospective clinical trial. J Clin Oncol 20(3):630–637
Meyer RM, Hoppe RT (2012) Point/counterpoint: early-stage Hodgkin lymphoma and the role of radiation therapy. Blood 120(23):4488–4495
Meyer RM (2014) Limited-stage Hodgkin lymphoma: managing uncertainty. J Clin Oncol 32:1180–1182
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing
About this chapter
Cite this chapter
Raemaekers, J.M.M., Engert, A. (2015). Treatment of Early Unfavorable HL. In: Engert, A., Younes, A. (eds) Hodgkin Lymphoma. Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-319-12505-3_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-12505-3_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-12504-6
Online ISBN: 978-3-319-12505-3
eBook Packages: MedicineMedicine (R0)