Abstract
Atopic dermatitis (AD) is a chronic relapsing inflammatory skin disease characterized by pruritic and eczematous skin lesions. AD is thought to be caused by multiple pathogenic factors, such as genetic susceptibility, environmental triggers, cutaneous barrier dysfunction, bacterial infection, and/or immune dysregulation. About 20 % of Caucasian children as well as 2–10 % of adults are affected by AD. One of the biggest discoveries in recent studies of AD was an apparent loss-of-function that genetic variants in the gene encoding filaggrin demonstrated; those are a strong predisposing factor for the development of AD with very-high significance. Up to 60 % of European AD patients have loss-of-function mutations in the filaggrin gene.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Core Messages-
The stratum corneum (SC) of atopic dermatitis (AD) skin contains unusual lipids, particularly with respect to ceramides (CER).
-
Abnormalities in the lipid bilayer at intercellular spaces of the SC cause an impaired barrier function as seen in higher values of transepidermal water loss.
-
The mechanism underlying these lipid abnormalities could be altered enzymatic activities relevant to the de novo synthesis of CER in the epidermis of AD skin.
-
Whether the abnormalities are primary or secondary to AD has not been fully elucidated although the outside–inside view has become more probable.
Introduction
Atopic dermatitis (AD) is a chronic relapsing inflammatory skin disease characterized by pruritic and eczematous skin lesions. AD is thought to be caused by multiple pathogenic factors, such as genetic susceptibility, environmental triggers, cutaneous barrier dysfunction, bacterial infection, and/or immune dysregulation. About 20 % of Caucasian children as well as 2–10 % of adults are affected by AD (Alanne et al. 2011; Slattery et al. 2011). One of the biggest discoveries in recent studies of AD was an apparent loss-of-function that genetic variants in the gene encoding filaggrin demonstrated; those are a strong predisposing factor for the development of AD with very-high significance (Palmer et al. 2006). Up to 60 % of European AD patients have loss-of-function mutations in the filaggrin gene (Elias and Wakefield 2011).
The relationship between AD and skin lipids was first reported by Melnik et al. 1988; Imokawa et al. 1991 then published an epoch-making article reporting lipid abnormalities with special reference to ceramides (CER) in the stratum corneum (SC) of AD skin. Since then, great attention has been paid to CER in the SC of patients with AD as well as their abnormal immune system. Until the beginning of the twenty-first century, thin-layer chromatography (TLC) was the only tool available to analyze CER in the SC, but the appearance of a new powerful technique, liquid chromatography-mass spectrometry (LC-MS), shifted the paradigm of dermatological studies regarding CER (Vietzke et al. 2001; Farwanah et al. 2005a). Progress worthy of special mention was that LC-MS analysis of CER in the SC of human skin revealed as many as 350 species that were structurally characterized (Masukawa et al. 2008), and that each of those diverse species could be quantified precisely and comprehensively using a newly developed LC-MS method (Masukawa et al. 2009). This method allowed the detailed features of the CER composition of the SC to be delineated.
The aim of this chapter is to clarify what has been known and unknown about the relationship between AD and skin lipids by answering the following four questions: (1) Are SC lipids in AD skin different from the lipids found in normal skin? (2) Do the lipid abnormalities affect the structures and/or properties of AD skin? (3) Is the mechanism underlying the lipid abnormalities known? (4) Are the lipid abnormalities primary or secondary to the development of AD? This chapter focuses on the relationships with skin lipids and not on relationships with skin proteins, such as filaggrin and cornified envelopes, except for those relevant to skin lipids. Readers who are interested in relationships between AD and skin proteins should consult other reviews (Proksch et al. 2008; Kypriotou et al. 2012; Nishifuji and Yoon 2013).
Are SC Lipids in AD Skin Different from the Lipids Found in Normal Skin?
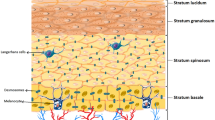
Skin barrier function strongly relies on the SC (outermost layers of the skin), which consists of stacked layers of corneocytes (enriched proteins) “bricks” embedded in an intercellular lipid mixture “mortar” (Michaels et al. 1975). CER, cholesterol and free fatty acids (FFA) are the three abundant lipid classes in the free intercellular lipids of the SC of human skin and CER accounts for 40–50 % of the total lipid mass (Wertz 1992). There are 12 CER subclasses (Robson et al. 1994; Ponec et al. 2003; Masukawa et al. 2008; Van Smeden et al. 2011), which can be expressed based on previous terminology (Motta et al. 1993; Robson et al. 1994) as depicted in Fig. 24.1; CER[ADS] consisting of α-hydroxy fatty acids and dihydrosphingosines (corresponding to CER 5 in the TLC analysis); CER[AH] consisting of α-hydroxy fatty acids and 6-hydroxysphingosines (CER 6II); CER[AP] consisting of α-hydroxy fatty acids and phytosphingosines (CER 6I); CER[AS] consisting of α-hydroxy fatty acids and sphingosines (CER 5); CER[EODS] consisting of ester-linked ω-hydroxy fatty acids and dihydrosphingosines (CER 1); CER[EOH] consisting of ester-linked ω-hydroxy fatty acids and 6-hydroxysphingosines (CER 4); CER[EOP] consisting of ester-linked ω-hydroxy fatty acids and phytosphingosines (CER 2); CER[EOS] consisting of ester-linked ω-hydroxy fatty acids and sphingosines (CER 1); CER[NDS] consisting of nonhydroxy fatty acids and dihydrosphingosines (CER 2); CER[NH] consisting of nonhydroxy fatty acids and 6-hydroxysphingosines (CER 6I); CER[NP] consisting of nonhydroxy fatty acids and phytosphingosines (CER 3); and CER[NS] consisting of nonhydroxy fatty acids and sphingosines (CER 2). In addition to the 12 free CER subclasses, two subclasses of protein-bound CER are found in the SC, CER[OH] consisting of ω-hydroxy fatty acids and 6-hydroxysphingosines and CER[OS] consisting of ω-hydroxy fatty acids and sphingosines (Robson et al. 1994).
Structures and nomenclature of ceramides (CER) in human stratum corneum (SC). (Note: this research was originally published in J. Lipid Res. (Masukawa et al. 2008). © the American Society for Biochemistry and Molecular Biology)
Table 24.1 shows a summary of intercellular lipids reported in the SC of AD lesional, AD nonlesional and controlled healthy nonlesional skin. Although numerous studies have emphasized diverse results due to the different subjects tested and the different methods used, there are common features for AD lesional skin as follows: (1) the level and/or wt. % of total CER is lower; (2) the CER composition is altered; and (3) the chain length of CER species is shortened. The first feature was confirmed by analyses done by Imokawa et al. 1991; Matsumoto et al. 1999; and Ishikawa et al. 2010. The second feature, i.e., that the balance of CER[EOS], other EO-containing CER subclasses and CER[NP] is commonly altered, was reported by Imokawa et al. (1991); Di Nordo et al. (1998); Matsumoto et al. (1999); Ishikawa et al. (2010); and Angelova-Fischer et al. (2011). The third feature, most recently unveiled, comes from the significantly higher levels of CER[NS], CER[NDS], and CER[AS] with shorter chain lengths, as represented in C34-CER[NS] (Ishikawa et al. 2010). The validity of the third feature is corroborated by the fact that there were significantly lower levels of CER[NS], CER[NDS], CER[NH], CER[AS], and CER[AH] with longer chain lengths in the AD lesions (Ishikawa et al. 2010), the fact that a CER[AS] species with a shorter chain length was detected in AD nonlesional skin but not in healthy skin (Bleck et al. 1999), and the fact that significantly higher wt. % of C34-CER[NS], C-34CER[NH], C34-CER[AS], and C-34CER[AH] were found in AD nonlesional skin (Janssens et al. 2012). Macheleidt et al. (2002) found a lower wt. % of very-long-chain FFA in the SC of AD lesional skin although this is not for CER.
Compared with the lipid abnormalities in AD lesional skin, AD nonlesional skin looks somewhat indefinite in terms of the levels and composition of CER. As shown in Table 24.1, the intermediate features of AD nonlesional skin between AD lesional skin and healthy skin were described in some articles (Di Nardo et al. 1998; Ishikawa et al. 2010) and characteristics in the lipid abnormalities similar to AD lesions were shown in AD nonlesional skin by others (Bleck et al. 1999; Janssens et al. 2011, 2012). On the other hand, Matsumoto et al. (1999) and Farwanah et al. (2005b) reported no differences between AD nonlesional skin and healthy skin. Those inconsistencies in results obtained for nonlesional SC of AD skin would be due to the varieties of subjects tested (severity, progress, and degree of nonlesions), sampling sites/procedures and analytical methods used. Filaggrin gene mutations do not appear to directly influence the lipid abnormalities for the nonlesional SC of AD skin. No significant differences at the nonlesional sites were found between individuals carrying and not carrying the mutations (Jungersted et al. 2010). In another study undertaken by Janssens et al. (2012), the nonlesional SC of AD subjects carrying filaggrin mutations did not have any differences in lipids with those not carrying the mutations. However, the lower level of CER[EOH] in the lesional SC of AD patients carrying the mutations than those not carrying them was pointed out (Angelova-Fischer et al. 2011). To define characteristics of the lipids in AD nonlesional skin and the impact of filaggrin gene mutations on the lipids in the SC of AD skin, much larger-scaled studies are needed.
Collectively, the answer for the question “are SC lipids in AD skin different from the lipids found in normal skin?” is likely “yes” for the SC of AD lesional skin, as indicated by the lower level of total CER, the altered CER composition and the CER species with shorter chain lengths. For AD nonlesional skin, the abnormalities may be present with slight but similar characteristics to AD lesional skin, but further studies are required in a way that the subjects tested are standardized in terms of severity, progress, and degree of nonlesional skin. The filaggrin gene mutations do not seem to directly affect the lipid abnormalities, at least for the nonlesional SC of AD skin but this also remains to be defined.
Do the Lipid Abnormalities Affect the Structures and/or Properties of Skin?
No studies have been reported that characterized structures of the lipid bilayer at intercellular spaces in the SC of AD lesional skin, and only structures in nonlesional SC have been investigated. The long-periodicity phase in the lipid bilayer in the nonlesional SC was found to be slightly but significantly reduced in the repeat distance or repeat quantity compared to healthy SC (Janssens et al. 2012). Regarding the lateral lipid packing, it was found that the nonlesional SC of AD patients has an increased percentage of hexagonal lattice, gel phase, compared to healthy skin which is characterized by a larger presence of orthorhombic packing, crystalline phase (Pilgram et al. 2001; Janssens et al. 2012, 2013). These differences could be interpreted as originating from the lipid abnormalities, such as a lower level of total CER, an altered CER composition, and/or CER species with shorter chain lengths.
The diminished level of total CER in the SC of AD skin had a negative correlation with transepidermal water loss (TEWL), which is an index of impaired barrier function (Ishikawa et al. 2010). Also, there was a significantly negative correlation of the TEWL value versus the level of each CER subclass other than CER[AS] and CER[NS]. The subclass of CER[AS] had a significantly positive correlation with TEWL (Ishikawa et al. 2010). Only the subclass CER[AS] seems to have a different nature in terms of the involvement with the barrier function in AD skin. An effect of chain lengths of CER species on the TEWL has also been revealed. Thus, the more abundant the CER species with shorter chain lengths are, the higher the TEWL values (Ishikawa et al. 2010; Joo et al. 2010; Janssens et al. 2012). Since the level of C34 CER species sounds strongly correlated with TEWL (Ishikawa et al. 2010; Janssens et al. 2012), it may be a characteristic marker for the diagnosis of AD. Janssens et al. (2013) showed that the change in tendency in the lateral packing is correlated with the TEWL value. That correlation could be interpreted by the physicochemical nature that the hexagonal lattice is a less-packed structure in the lateral direction, where water can be less disturbed through the lipid bilayer.
The structure of the lipid bilayer in the SC of AD skin is likely to be changed into a bilayer with the reduced repeat distance or repeat quantity in the long-periodicity phase and with an increase in the hexagonal lattice, which may be due to the lipid abnormalities. This change in structure would cause a higher TEWL value corresponding to the impaired barrier function of AD skin.
Is the Mechanism Underlying the Lipid Abnormalities Known?
An ultrastructural study of AD skin versus healthy skin indicated the immature formation of lipid lamellae at the border between the stratum granulosum and the SC of AD skin (Fartasch et al. 1992). Thus, in AD skin, lamellar body-discs remained undelivered and were found even within the horny cells, in contrast to healthy skin where the body-discs completely disappeared. This suggested an abnormal keratinization coming from the unusual lipid metabolism in AD skin. The deficiency of CER in the SC of patients with AD can be explained by the extraordinary upregulation of glucosylceramide sphingomyelin deacylase (GSDase), which hydrolyzes glucosylceramide (GlcCER) or sphingomyelin (SM) at an acyl site to yield sphingosylphosphorylcholine (SPC) or glucosylsphingosine (GSP), respectively, instead of CER (Imokawa 2009), as illustrated in Reaction 1 of Fig. 24.2. The substantiality of the enzyme is supposed to be the β-subunit of acid ceramidase (CDase) based on a study using rat skin (Nogami-Itoh et al. 2010). At first, it was found that in the skin of patients with AD, the activities of three sphingolipid hydrolysis enzymes, β-glucocerebrosidase, sphingomyelinase (SMase), and CDase were not changed (Jin et al. 1994; Murata et al. 1996) whereas SM hydrolysis was increased with the occurrence of SPC as a reaction product and this hitherto undiscovered enzyme was tentatively termed SM deacylase (Murata et al. 1996; Hara et al. 2000). In a subsequent study, this enzyme was then termed GSDase because it hydrolyzes not only SM but also GlcCER in AD skin (Higuchi et al. 2000). The fact that the levels of SPC and GSP were both significantly higher in the epidermis of AD patients (Okamoto et al. 2003; Ishibashi et al. 2003), as listed in Table 24.1, corroborates the mechanism that the upregulation of GSDase generates the CER deficiency.
Other possible mechanisms underlying the diminished level of CER were proposed regarding reduced SMase activity (Reaction 2 of Fig. 24.2) and the involvement of bacterial CDase (Reaction 3 of Fig. 24.2). Acid SMase as well as neutral SMase, which produce CER from SM in the epidermis, were decreased both in the lesional and nonlesional skin from AD patients compared to control healthy skin (Jensen et al 2014). The involvement of bacteria secreting CDase by which CER would be decomposed in the SC of AD skin was proposed (Ohnishi et al. 1999). Those mechanisms might be responsible in part for the diminished level of total CER. However, the altered CER composition cannot be explained only by the SMase activity or bacterial CDase because CER[NS] and CER[AS] are derived in part from the corresponding SM precursors while other subclasses such as EO-containing CER are derived only from GlcCER (Uchida et al. 2000; Hamanaka et al. 2002). Those mechanisms are not enough to explain the altered CER composition in the selective changes in the balances of CER[EOS], other EO-containing CER subclasses, and CER[NP].
Macheleidt et al. (2002) compared the de novo synthesis of GlcCER and CER in lesional AD skin with healthy skin using a metabolic labeling technique, which revealed remarkable decreases of newly biosynthesized ClcCER and CER in lesional AD skin. An experimental system using a reconstructed human epidermal keratinization model suggested that the Th2 type of inflammation evoked in AD skin may be one factor involved in the downregulated biosynthesis of CER, which results in the reduced levels of CER in the SC (Sawada et al. 2012). Therefore, the deficiency of CER in the SC of AD skin is likely to be caused not only by the abnormal pathway from GlcCER and SM to CER, such as the upregulation of GSDase (Reaction 1 of Fig. 24.2), but also reduced the de novo synthesis of CER skeletons themselves (Reaction 4 of Fig. 24.2). As for the chain length, elongases in the epidermis seem to be involved. Although the results were obtained in an experimental system using mice but not humans, some elongases that synthesize very-long-chain FFA were downregulated in a hapten-induced AD model (Park et al. 2012). It could be assumed that the downregulated elongases resulted in the decreased levels of CER species with longer -chain lengths (Bleck et al. 1999; Ishikawa al. 2010; Janssens et al. 2012)very-long-chain FFA (Macheleidt et al. 2002).
Based on evidence accumulated to date, the mechanism underlying the lipid abnormalities for the SC in AD skin can most probably be explained by a combination of events, as follows: (1) the lower level of total CER would be caused by both the upregulation of GSDase and the reduced de novo synthesis of CER in the epidermis of AD skin, (2) the altered CER composition might be ascribed to changes in activities of enzymes relevant to the production of CER in the SC although this remains to be clarified, and (3) CER species with shorter chain lengths might originate from downregulated elongases although that also remains to be elucidated.
Are the Lipid Abnormalities Primary or Secondary to the Development of AD?
Traditionally, it was thought that the primary cause of AD was an immunological abnormality that led to the secondary barrier dysfunction (inside–outside view of AD pathogenesis). Many reports on the pathogenesis of AD focused on the primary role of abnormalities in the immune system, as reviewed by Leung (2006) and Ong and Leund (2006). In fact, therapy for AD was largely directed toward ameliorating Th2-mediated inflammation and/or pruritus using steroids or immunomodulators in spite of concerns about their side effects. A new paradigm of the outside–inside view (or outside–inside–outside), however has proposed that the primary inherited and acquired barrier abnormalities are followed by immune system activation, which further exacerbates the barrier function with a vicious cycle (Elias 2008; Cork et al. 2009; Elias and Schmuth 2009; Elias and Wakefield 2011).
Elias and Schmuth (2009) insist on the probability of the outside–-inside view because specific replacement therapy, which targets the prominent lipid abnormalities that account for the barrier abnormality in AD, corrects not only the barrier impairment but also comprises an effective anti-inflammatory therapy for AD. Topical application of a CER or pseudoceramide-dominant physiological lipid-base barrier repair emulsion has demonstrated clinical efficacies to improve the impaired barrier function in AD skin as well as to ameliorate AD symptoms (Mao-Qiang et al. 1996; Berardesca et al. 2001; Chamlin et al. 2002; Jensen and Elias 2006; Madaan 2008; Bikowski 2009; Park et al. 2010; Kircik et al. 2011). The availabilities of skin care products containing lipids/oils for AD skin have also been evidenced in other cases. Topical application of emollients, moisturizers, or creams containing lipids/oils, such as CER (Hon et al. 2013), pseudoceramide (Hon et al. 2011), petrolatum (Matsumoto et al. 2007), and paraffin oil and vegetable oil (Patzelt et al. 2012), efficiently improved the impaired skin conditions. Those clinical efficacies could be considered in part to be caused by the lipids/oils which provide an exogenous barrier to water loss from the inside and to the penetration of foreign material from the outside. This corroborates the validity of the outside–inside view as well as the important role of CER. However, the outside–inside view and the role of CER are still speculative. Before getting a true answer for the question, the further detailed studies are required.
The current conclusion to answer the question “are the lipid abnormalities primary or secondary to the development of AD?” is that it has not been fully elucidated whether the impaired barrier function due to the lipid abnormalities is primary or secondary to AD. Recent studies showing the availabilities of lipids/oils therapy to treat AD skin certainly suggest that the outside–inside view might be more likely and that CER might be a key. However, no technologies seem to have reached a scientifically convincing proof from the viewpoint of the mechanism underlying the clinical efficacies to AD skin, although there have been some reports of technologies that can upregulate levels of endogenous CER in in vivo and in vitro studies (Rawlings et al. 1996; Tanno et al. 2000; Ishikawa et al. 2012). We need to wait some time to get a true answer which would be obtained from our future studies.
Summary
It is well known that lipid abnormalities occur in the SC of lesional AD skin, as seen in the lower level of total CER, the altered CER composition and the CER species with shorter chain lengths compared to control healthy skin. It is also known that the lipid abnormalities cause an altered structure of the lipid bilayer, which further causes the impaired barrier function of AD skin, as seen in the higher values of TEWL. The reason for the lower level of total CER is likely to involve a mechanism where GSDase is upregulated and the de novo synthesis of CER is deactivated in the epidermis of AD skin. Based on accumulated evidence showing the clinical efficacies of lipids/oils therapy for patients with AD, the outside–inside view seems more likely than the traditional inside–outside view. On the other hand, there are still several unknown factors as follows; the lipid abnormalities for the nonlesional SC of AD, the reasons why the composition of CER subclasses is altered and why the chain lengths of CER species become shorter in AD lesions, the mechanism underlying the development of AD, and its relationship to the lipid abnormalities, that is, whether the lipid abnormalities are primary or secondary for AD. Those unknown factors will be clarified by our future work, which should help improve the quality of life for patients who suffer from AD symptoms.
References
Alanne S, Nermes M, Soderlund R, Laitinen K. Quality of life in infants with atopic dermatitis and healthy infants: a follow-up from birth to 24 months. Acta Paediatr. 2011;100:e65–70.
Angelova-Fischer I, Mannheimer AC, Hinder A, Ruether A, Franke A, Neubert RH, Fischer TW, Zillikens D. Distinct barrier integrity phenotypes in filaggrin-related atopic eczema following sequential tape stripping and lipid profiling. Exp Dermatol. 2011;20:351–6
Arikawa J, Ishibashi M, Kawashima M, Takagi Y, Ichikawa Y, Imokawa G. Decreased levels of sphingosine, a natural antimicrobial agent, may be associated with vulnerability of the stratum corneum from patients with atopic dermatitis to colonization by Staphylococcus aureus. J Invest Dermatol. 2002;119:433–9.
Berardesca E, Barbareschi M, Veraldi S, Pimpinelli N. Evaluation of efficacy of a skin lipid mixture in patients with irritant contact dermatitis, allergic contact dermatitis or atopic dermatitis: a multicenter study. Contact Dermatitis. 2001;45:280–5.
Bikowski J. Case studies assessing a new skin barrier repair cream for the treatment of atopic dermatitis. J Drugs Dermatol. 2009;8:1037–41.
Bleck O, Abeck D, Ring J, Hoppe U, Vietzke JP, Wolber R, Brandt O, Schreiner V. Two ceramide subfractions detectable in Cer(AS) position by HPTLC in skin surface lipids of non-lesional skin of atopic eczema. J Invest Dermatol. 1999;113:894–900.
Chamlin SL, Kao J, Frieden IJ, Sheu MY, Fowler AJ, Fluhr JW, Williams ML, Elias PM. Ceramide-dominant barrier repair lipids alleviate childhood atopic dermatitis: changes in barrier function provide a sensitive indicator of disease activity. J Am Acad Dermatol. 2002;47:198–208.
Cork MJ, Danby SG, Vasilopoulos Y, Hadgraft J, Lane ME, Moustafa M, Guy RH, Macgowan AL, Tazi-Ahnini R, Ward SJ. Epidermal barrier dysfunction in atopic dermatitis. J Invest Dermatol. 2009;129:1892–908.
Di Nardo A, Wertz P, Giannetti A, Seidenari S. Ceramide and cholesterol composition of the skin of patients with atopic dermatitis. Acta Derm Venereol. 1998;78:27–30.
Elias PM. Barrier repair trumps immunology in the pathogenesis and therapy of atopic dermatitis. Drug Discov Today Dis Mech. 2008;5:e33–8.
Elias PM, Schmuth M. Abnormal skin barrier in the etiopathogenesis of atopic dermatitis. Curr Opin Allergy Clin Immunol. 2009;9:437–46.
Elias PM, Wakefield JS. Therapeutic implications of a barrier-based pathogenesis of atopic dermatitis. Clin Rev Allergy Immunol. 2011;41:282–95.
Fartasch M, Bassukas ID, Diepgen TL. Disturbed extruding mechanism of lamellar bodies in dry non-eczematous skin of atopics. Br J Dermatol. 1992;127:221–7.
Farwanah H, Wohlrab J, Neubert RH, Raith K. Profiling of human stratum corneum ceramides by means of normal phase LC/APCI-MS. Anal Bioanal Chem. 2005a;383:632–7.
Farwanah H, Raith K, Neubert RH, Wohlrab J. Ceramide profiles of the uninvolved skin in atopic dermatitis and psoriasis are comparable to those of healthy skin. Arch Dermatol Res. 2005b;296:514–21.
Hamanaka S, Hara M, Nishio H, Otsuka F, Suzuki A, Uchida Y. Human epidermal glucosylceramides are major precursors of stratum corneum ceramides. J Invest Dermatol. 2002;119:416–23.
Hara J, Higuchi K, Okamoto R, Kawashima M, Imokawa G. High-expression of sphingomyelin deacylase is an important determinant of ceramide deficiency leading to barrier disruption in atopic dermatitis. J Invest Dermatol. 2000;115:406–13.
Higuchi K, Hara J, Okamoto R, Kawashima M, Imokawa G. The skin of atopic dermatitis patients contains a novel enzyme, glucosylceramide sphingomyelin deacylase, which cleaves the N-acyl linkage of sphingomyelin and glucosylceramide. Biochem J. 2000;350:747–56.
Hon KL, Wang SS, Lau Z, Lee HC, Lee KK, Leung TF, Luk NM. Pseudoceramide for childhood eczema: does it work? Hong Kong Med J. 2011;17:132–6.
Hon KL, Pong NH, Wang SS, Lee VW, Luk NM, Leung TF. Acceptability and efficacy of an emollient containing ceramide-precursor lipids and moisturizing factors for atopic dermatitis in pediatric patients. Drugs R D. 2013;13:37–42.
Imokawa G. A possible mechanism underlying the ceramide deficiency in atopic dermatitis: expression of a deacylase enzyme that cleaves the N-acyl linkage of sphingomyelin and glucosylceramide. J Dermatol Sci. 2009;55:1–9.
Imokawa G, Abe A, Jin K, Higaki Y, Kawashima M, Hidano A. Decreased level of ceramides in stratum corneum of atopic dermatitis: an etiologic factor in atopic dry skin? J Invest Dermatol. 1991;96:523–6.
Ishibashi M, Arikawa J, Okamoto R, Kawashima M, Takagi Y, Ohguchi K, Imokawa G. Abnormal expression of the novel epidermal enzyme, glucosylceramide deacylase, and the accumulation of its enzymatic reaction product, glucosylsphingosine, in the skin of patients with atopic dermatitis. Lab Invest. 2003;83:397–408.
Ishikawa J, Narita H, Kondo N, Hotta M, Takagi Y, Masukawa Y, Kitahara T, Takema Y, Koyano S, Yamazaki S, Hatamochi A. Changes in the ceramide profile of atopic dermatitis patients. J Invest Dermatol. 2010;130:2511–4.
Ishikawa J, Shimotoyodome Y, Chen S, Ohkubo K, Takagi Y, Fujimura T, Kitahara T, Takema Y. Eucalyptus increases ceramide levels in keratinocytes and improves stratum corneum function. Int J Cosmet Sci. 2012;34:17–22.
Janssens M, van Smeden J, Gooris GS, Bras W, Portale G, Caspers PJ, Vreeken RJ, Kezic S, Lavrijsen AP, Bouwstra JA. Lamellar lipid organization and ceramide composition in the stratum corneum of patients with atopic eczema. J Invest Dermatol. 2011;131:2136–8.
Janssens M, van Smeden J, Gooris GS, Bras W, Portale G, Caspers PJ, Vreeken RJ, Hankemeier T, Kezic S, Wolterbeek R, Lavrijsen AP, Bouwstra JA. Increase in short-chain ceramides correlates with an altered lipid organization and decreased barrier function in atopic eczema patients. J Lipid Res. 2012;53:2755–66.
Janssens M, Mulder AA, van Smeden J, Pilgram GS, Wolterbeek R, Lavrijsen AP, Koning RI, Koster AJ, Bouwstra JA. Electron diffraction study of lipids in non-lesional stratum corneum of atopic eczema patients. Biochim Biophys Acta. 2013;1828:1814–21.
Jensen JM, Elias PM. The stratum corneum of the epidermis in atopic dermatitis. In: Elias PM, Feingold KR, editors. Skin barrier. New York: Taylor and Francis; 2006. pp. 569–89.
Jensen JM, Fölster-Holst R, Baranowsky A, Schunck M, Winoto-Morbach S, Neumann C, Schütze S, Proksch E. Impaired sphingomyelinase activity and epidermal differentiation in atopic dermatitis. J Invest Dermatol. 2014;122:1423–31.
Jin K, Higaki Y, Takagi Y, Higuchi K, Yada Y, Kawashima M, Imokawa G. Analysis of b-glucocerebrosidase and ceramidase actibities in atopic and aged dry skin. Acta Derm Venereol (Stockh). 1994;74:337–40.
Joo KM, Jeong HJ, Lee SY. Relationship between cutaneous barrier function and ceramide species in human stratum corneum. J Dermatol Sci. 2010;60:47–50.
Jungersted JM, Scheer H, Mempel M, Baurecht H, Cifuentes L, Høgh JK, Hellgren LI, Jemec GB, Agner T, Weidinger S. Stratum corneum lipids, skin barrier function and filaggrin mutations in patients with atopic eczema. Allergy. 2010;65:911–8.
Kircik LH, Del Rosso JQ, Aversa D. Evaluating clinical use of a ceramide-dominant, physiologic lipid-based topical emulsion for atopic dermatitis. J Clin Aesthet Dermatol. 2011;4:34–40.
Kypriotou M, Huber M, Hohl D. The human epidermal differentiation complex: cornified envelope precursors, S100 proteins and the ‘fused genesʼ family. Exp Dermatol. 2012;21:643–9.
Leung DY. New insights into the complex gene-environment interactions evolving into atopic dermatitis. J Allergy Clin Immunol. 2006;118:37–45.
Macheleidt O, Kaiser HW, Sandhoff K. Deficiency of epidermal protein-bound omega-hydroxyceramides in atopic dermatitis. J Invest Dermatol. 2002;119:166–73.
Madaan A. Epiceram for the treatment of atopic dermatitis. Drugs Today (Barc). 2008;44:751–5.
Mao-Qiang M, Feingold KR, Thornfeldt CR, Elias PM. Optimization of physiological lipid mixtures for barrier repair. J Invest Dermatol. 1996;106:1096–101.
Masukawa Y, Narita H, Shimizu E, Kondo N, Sugai Y, Oba T, Homma R, Ishikawa J, Takagi T, Kitahara T, Takema Y, Kita K. Characterization of overall ceramide species in human stratum corneum. J Lipid Res. 2008;49:1466–76.
Masukawa Y, Narita H, Sato H, Naoe A, Kondo N, Sugai Y, Oba T, Homma R, Ishikawa J, Takagi Y, Kitahara T. Comprehensive quantification of ceramide species in human stratum corneum. J Lipid Res. 2009;50:1708–19.
Matsumoto M, Umemoto N, Sugiura H, Uehara M. Difference in ceramide composition between “dry” and “normal” skin in patients with atopic dermatitis. Acta Derm Venereol. 1999;79:246–7.
Matsumoto T, Yuasa H, Kai R, Ueda H, Ogura S, Honda Y. Skin capacitance in normal and atopic infants, and effects of moisturizers on atopic skin. J Dermatol. 2007;34:447–50.
Melnik B, Hollmann J, Plewig G. Decreased stratum corneum ceramides in atopic individuals—a pathobiochemical factor in xerosis? Br J Dermatol. 1988;119:547–9.
Michaels AS, Chandrasekaran SK, Shaw JE. Drug penetration through human skin. Theory and in vitro experimental measurements. AIChE J. 1975;21:985–96.
Motta S, Monti M, Sesana S, Caputo R, Carelli S, Ghidoni R. Ceramide composition of the psoriatic scale. Biochim Biophys Acta. 1993;1182:147–51.
Murata Y, Ogata J, Higaki Y, Kawashima M, Yada Y, Higuchi K, Tsuchiya T, Kawainami S, Imokawa G. Abnormal expression of sphingomyelin acylase in atopic dermatitis: an etiologic factor for ceramide deficiency? J Invest Dermatol. 1996;106:1242–9.
Nishifuji K, Yoon JS. The stratum corneum: the rampart of the mammalian body. Vet Dermatol. 2013;24:60–72.
Nogami-Itoh M, Teranishi Y, Kuwahara H, Kusumoto M, Nakamura K, Matsumoto M, Sakai J, Kimura T, Kawashima M. Purification and identification of sphingomyelin deacylase from rat skin. J Invest Dermatol. 2010;130(suppl 2):s24.
Ohnishi Y, Okino N, Ito M, Imayama S. Ceramidase activity in bacterial skin flora as a possible cause of ceramide deficiency in atopic dermatitis. Clin Diagn Lab Immunol. 1999;6:101–4.
Okamoto R, Arikawa J, Ishibashi M, Kawashima M, Takagi Y, Imokawa G. Sphingosylphosphorylcholine is upregulated in the stratum corneum of patients with atopic dermatitis. J Lipid Res. 2003;44:93–102.
Ong PY, Leung DY. Immuno desregulation in atopic dermatitis. Curr Allergy Asthema Rep. 2006;6:384–9.
Palmer CN, Irvine AD, Terron-Kwiatkowski A, Zhao Y, Liao H, Lee SP, Goudie DR, Sandilands A, Campbell LE, Smith FJ, O’Regan GM, Watson RM, Cecil JE, Bale SJ, Compton JG, DiGiovanna JJ, Fleckman P, Lewis-Jones S, Arseculeratne G, Sergeant A, Munro CS, Houate BE, McElreavey K, Halkjaer LB, Bisgaard H, Mukhopadhyay S, McLean WI. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet. 2006;38:441–6.
Park KY, Kim DH, Jeong MS, Li K, Seo SJ. Changes of antimicrobial peptides and transepidermal water loss after topical application of tacrolimus and ceramide-dominant emollient in patients with atopic dermatitis. Prevention of AD with emollient. J Korean Med Sci. 2010;25:766–71.
Park YH, Jang WH, Seo JA, Park M, Lee TR, Park YH, Kim DK, Lim KM. Decrease of ceramides with very long-chain fatty acids and downregulation of elongases in a murine atopic dermatitis model. J Invest Dermatol. 2012;132:476–9.
Patzelt A, Lademann J, Richter H, Darvin ME, Schanzer S, Thiede G, Sterry W, Vergou T, Hauser M. In vivo investigations on the penetration of various oils and their influence on the skin barrier. Skin Res Technol. 2012;18:364–9.
Pilgram GS, Vissers DC, van der Meulen H, Pavel S, Lavrijsen SP, Bouwstra JA, Koerten HK. Aberrant lipid organization in stratum corneum of patients with atopic dermatitis and lamellar ichthyosis. J Invest Dermatol. 2001;117:710–7.
Ponec M, Weerheim A, Lankhorst P, Wertz PW. New acylceramide in native and reconstructed epidermis. J Invest Dermatol. 2003;120:581–8.
Proksch E, Brandner JM, Jensen JM. The skin: an indispensable barrier. Exp Dermatol. 2008;17:1063–72.
Rawlings AV, Davies A, Carlomusto M, Pillai S, Zhang K, Kosturko R, Verdejo P, Feinberg C, Nguyen L, Chander P. Effect of lactic acid isomers on keratinocyte ceramide synthesis, stratum corneum lipid levels and stratum corneum barrier function. Arch Dermatol Res. 1996;288:383–90.
Robson KJ, Stewart ME, Michelsen S, Lazo ND, Downing DT. 6-hydroxy-4-sphingenine in human epidermal ceramides. J Lipid Res. 1994;35:2060–8.
Sawada E, Yoshida N, Sugiura A, Imokawa G. Th1 cytokines accentuate but Th2 cytokines attenuate ceramide production in the stratum corneum of human epidermal equivalents: an implication for the disrupted barrier mechanism in atopic dermatitis. J Dermatol Sci. 2012;68:25–35.
Slattery MJ, Essex MJ, Paletz EM, Vanness ER, Infante M, Rogers GM, Gern JE. Depression, anxiety, and dermatologic quality of life in adolescents with atopic dermatitis. J Allergy Clin Immunol. 2011;128:668–71.
Tanno O, Ota Y, Kitamura N, Katsube T, Inoue S. Nicotinamide increases biosynthesis of ceramides as well as other stratum corneum lipids to improve the epidermal permeability barrier. Br J Dermatol. 2000;143:524–31.
Uchida Y, Hara M, Nishio H, Sidransky E, Inoue S, Otsuka F, Suzuki A, Elias PM, Holleran WM, Hamanaka S. Epidermal sphingomyelins are precursors for selected stratum corneum ceramides. J Lipid Res. 2000;41:2071–82.
Van Smeden J, Hoppel L, van der Heijden R, Hankemeier T, Vreeken RJ, Bouwstra JA. LC/MS analysis of stratum corneum lipids: ceramide profiling and discovery. J Lipid Res. 2011;52:1211–21.
Vietzke JP, Brandt O, Abeck D, Rapp C, Straßner M, Schreiner V, Hintze U. Comparative investigation of human stratum corneum ceramides. Lipids. 2001;36:299–304.
Wertz PW. Epidermal lipids. Semin Dermatol. 1992;11:106–13.
Yamamoto A, Serizawa S, Ito M, Sato Y. Stratum corneum lipid abnormalities in atopic dermatitis. Arch Dermatol Res. 1991;283:219–23.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Masukawa, Y. (2015). Atopic Dermatitis (AD) and Lipids. In: Pappas, A. (eds) Lipids and Skin Health. Springer, Cham. https://doi.org/10.1007/978-3-319-09943-9_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-09943-9_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-09942-2
Online ISBN: 978-3-319-09943-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)