Abstract
Head and neck squamous cell carcinoma (HNSCC) accounts for around 6 % of all cancers in the USA. Few of the greatest obstacles in HNSCC include development of secondary primary tumor, resistance and toxicity associated with the conventional treatments, together decreasing the overall 5-year survival rate in HNSCC patients to ≤50 %. Radiation and chemotherapy are the conventional treatment options available for HNSCC patients at both early and late stage of this cancer type malignancy. Unfortunately, patients response poorly to these therapies leading to relapsed cases, which further, emphasizes the need of additional strategies for the prevention/intervention of both primary and the secondary primary tumors post-HNSCC therapy. In recent years, growing interest has focused on the use of natural products or their analogs to reduce the incidence and mortality of cancer, leading to encouraging results. Resveratrol, a component from grape skin, is one of the well-studied agents with a potential role in cancer chemoprevention and other health benefits. As an anticancer agent, resveratrol suppresses metabolic activation of pro-carcinogens to carcinogens by modulating the metabolic enzymes responsible for their activation, and induces phase II enzymes, thus, further detoxifying the effect of pro-carcinogens. Resveratrol also inhibits cell growth and induces cell death in cancer cells by targeting cell survival and cell death regulatory pathways. Growing evidence also suggest that resveratrol directly binds to DNA and RNA, activates antioxidant enzymes, prevents inflammation, and stimulates DNA damage checkpoint kinases affecting genomic integrity more specifically in malignant cells.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
19.1 Introduction
This chapter aims to summarize recent development in the etiology and treatment of head and neck squamous cell carcinoma (HNSCC). Alcohol and its by-products have been reported to be strong possible carcinogens in different types of malignancies including HNSCC. In this perspective, chemopreventive agents are revealed to exert their chemopreventive efficacy either by blocking the activity of carcinogens or its metabolism or by targeting various cell survival pathways in tumor cells [69]. Further in-depth mechanistic studies revealed that nutraceutical resveratrol may inhibit carcinogenesis by affecting the molecular events in the initiation, promotion, and progression stages. Therefore, our goal in this chapter is to briefly describe the molecular mechanism involved in alcohol-induced oral cancer and to propose that these oral cancers can be prevented through the use of the nontoxic natural product resveratrol.
19.1.1 Head and Neck Squamous Cell Carcinoma
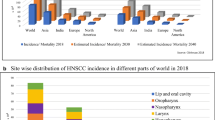
HNSCC is a devastating disease worldwide accounting for 650,000 new cases and 350,000 deaths every year [14]. According to the American Cancer Society, in the year 2013, approximately 53,640 new cases and 11,520 deaths are projected to occur, in the USA alone [59]. HNSCC is mostly curable with conventional treatment therapy when is diagnosed in early stage (I or II); unfortunately most of the HNSCC patients are diagnosed at advanced stage of the disease (III or IV), and survival rate is below 50 %. Epidemiological data suggest that several behavioral, environmental, viral, and genetic factors have been associated with the development of HNSCC. Tobacco and alcohol consumption accounts for ≥80 % of the risk factors associated with HNSCC [48, 56]. For individuals using both tobacco and alcohol, there is a synergistic effect, accelerating the risk of both oral and pharyngeal cancer by nearly 35-fold [65]. One cohort study with nearly 0.5 million participants focused on investigating the relationship between HNSCC risk and alcohol consumption, suggested that moderate drinkers (up to one drink a day) showed reduced risk of HNSCC compared to nondrinkers and heavy drinkers [17]. Reflecting this linearity, alcohol consumption is one of the major risk factors for nonsmoker. This was further supported by a population-based survey of 1,090 oral or pharyngeal cancer patients where the risk of secondary primary tumors (SPTs) was documented to be ≥50 % who continue with their drinking behavior after treatment [10]. Hence, considering concurrent risk of cancer development among alcoholics, understanding the relationship between alcohol consumption and cancer development, specifically HNSCC, is crucial for therapeutics and preventive purposes.
19.1.2 Major Molecular and Genetic Predispositions in HNSCC
Molecular and genetic analyses have revealed that multiple pathways are compromised in head and neck cancer [34]. Pathways that are critically altered in HNSCC include protein 53 (p53), retinoblastoma protein (Rb), epidermal growth factor receptor, signal transducer and activator of transcription, vascular endothelial growth factor, DNA repair regulators, and mammalian target of rapamycin; these pathways are thus also identified as potential therapeutic targets [18, 26]. Overexpression of dominant negative p53 and cyclin D1, together with increased telomerase activity (≥80 %), confer deregulated cell cycle and resistance to DNA damage stimulators in HNSCC [7]. Viral proteins E6 and E7 encoded by human papilloma virus (HPV) bind and inactivate p53 and Rb, respectively, disrupting the cell cycle regulation in HPV + tumors [29]. Most HPV + tumors are observed among young nonsmokers and nondrinkers, and are usually present at an advanced stage at the time of diagnosis [16, 22]. In addition, a clinical study with HNSCC patients (n = 37) and healthy individuals (n = 35) showed that tumor cells are more sensitive to irradiation-mediated DNA damage and display impaired DNA repair, indicating the crucial role of DNA repair mechanism in HNSCC treatment [8, 54]. Another study with archival human head and neck cancer tumor specimens revealed that Ku80, a DNA repair protein, was overexpressed and correlated with increased drug resistance, thus indicating this pathway as an attractive therapeutic target [8, 37, 41]. In relation to this linearity, patients with Fanconi Anemia (FA), a genetic syndrome with defective DNA repair mechanism, have been associated with an early lymph node metastases with poor clinical outcome [68]. DNA repair defects in Fanconi patients lead to pre-cancerous cells with increased levels of DNA damage and mutations. Although there is no evidence for genetic mutations in Fanc/Brca pathway in HNSCCs, loss or reduced expression of Fanc/Brca pathway genes has been reported in sporadic HNSCCs [36]. Likewise, amplification of several oncogenes [e.g., c-myc, Ras, EGFR, erbB2, nitric oxide synthetase, and cyclooxygenase 2 (COX2)] has been observed in HNSCC and has been associated with poor prognosis [28, 51]. The direct downstream target of tyrosine kinase receptors (EGFR, IGF-1R) and the PI3K/Akt signaling pathway is mammalian target of rapamycin (mTOR), which is found to be activated in 90–100 % of HNSCC [43]. Together, all these oncogenic pathways interlinked cellular pathways, deregulated in HNSCC, serve as potential therapeutic and preventive targets for HNSCC [5, 34, 45]. All these pathways directly or indirectly involved in cancer initiation, promotion, or progression are reported as possible targets of alcohol or its metabolites [12, 57]. Herein, identification of these cellular and molecular processes that are disrupted by exposure to alcohol is necessary to consider for the therapeutic and preventive intervention of cancer included HNSCC [26].
19.1.3 Alcohol: Carcinogen or Co-carcinogen in HNSCC
As mentioned earlier in this chapter, heavy alcohol consumption is directly associated with increased risk of cancer included HNSCC. In notion to this, International Agency for Cancer has classified alcohol as carcinogen to human, as it may influence cancer incidence by modulating different stages in cancer development [57]. In this chapter, we have briefly summarized cellular and molecular processes altered by alcohol.
19.1.3.1 Alcohol Metabolism and Metabolic Enzymes
The bacterial microfloras present in the oral cavity or esophagus convert ethanol to acetaldehyde with the help of alcohol dehydrogenase (ADHs), cytochrome P4502E1 (CYP2E1), and catalase [17]. Acetaldehyde so formed is further processed to acetate in the presence of aldehyde dehydrogenase (ALDH). Acetaldehyde binds covalently with DNA forming DNA adducts and interferes with DNA synthesis and repair, thereby initiating multistage carcinogenesis process after continuous exposure [57]. There are ample evidences showing that exposure to acetaldehyde produce mucosal lesions and adenocarcinomas in the nasal mucosa in rats [32, 70]. A study by Balbo and colleague have reported that N2-ethyl-2′-deoxyguanosine, a major acetaldehyde derived-DNA adduct was increased by several-fold from baseline after alcohol use in humans [2]. Genetic evidence suggests that individuals having fast metabolites alleles variants for ADHs [ADH1B*2, ADH1C*1] and the null allele for ALDH 2 [ALDH2*2] have increased acetaldehyde levels and inefficient alcohol metabolism, thereby increasing susceptibility to cancer after alcohol consumption [9, 57, 7]. Similarly, the activities of ADH and ALDH are shown to be significantly higher in cancerous than in healthy tissues [30], further suggesting the importance of these enzymes in alcohol metabolism and aggressive cancer. Furthermore, chronic alcohol consumption leads to induction of CYP2E1, which metabolizes alcohol to acetaldehyde, as well as generates reactive oxygen species (ROS) and reactive nitrogen species (RNS) as by-products [12]. These formed ROS and/or RNS can directly damage DNA, generate lipid peroxidation products, and increase inflammation. Moreover, prolonged ethanol exposure leads to decreased levels of endogenous antioxidants, thereby reducing cellular defense mechanisms [12]. Together, this supports the key role of alcohol metabolites in causing cancer including HNSCC in humans through different endogenous mechanisms.
19.1.3.2 Alcohol: DNA Damage and DNA Repair
Reactive oxygen- or nitrogen-containing molecules that are generated during alcohol metabolism can result in different types of DNA damage included single-base lesions, single-strand breaks (SSBs), and double-strand breaks (DSBs). To counteract the DNA damage, cells have elaborated DNA repair mechanisms, thus protecting genomic integrity [24]. SSBs and single-base lesions are repaired by base-excision repair (BER), nucleotide-excision repair (NER), and mismatch repair (MMR); and DSBs are repaired through non-homologous end joining (NHEJ) and homologous repair (HR) mechanisms. A prolonged consumption of alcohol results in higher levels of oxidative DNA damage, lipid peroxidation adducts, and acetaldehyde-DNA adducts, and thus overwhelming the relevant DNA repair mechanism and impairing genome function [12]. In recent years, polymorphisms in DNA repair have been directly linked with increased risk to DNA damaging agents with a likelihood of oncogenic transformation [19].
19.1.3.3 Alcohol Interacts with Oncogenes and Tumor Suppressor Pathways
Apart from mutagenic potential of alcohol metabolites through DNA adducts formation, alcohol is also shown to disrupt cellular and molecular pathways in the multistage carcinogenesis process. It has been suggested that acetaldehyde abrogates a cell’s ability to repair DNA damage [57]. Similarly, alcohol has been reported to either directly interacting with cell membrane proteins or modulating cellular function [57]. Long-term alcohol exposure preferentially causes K-ras mutation, impairs p16INK4A protein expression, and induces mutation in both retinoblastoma (Rb) and p53 proteins thereby, triggering cancer promotion [51]. Aberration of all these genes promote cell survival, evade apoptosis, and stimulate cell proliferation of cancer cells [49]. A recent study has reported that ethanol in cancer cells is ultimately converted to acetyl-CoA (a high-energy mitochondrial fuel) that can be used to synthesize ketone bodies, fueling tumor cell growth via oxidative mitochondrial metabolism (OXPHOS) [55]. Alcohol consumption has been associated with disruption of retinoid metabolism; retinoic acid (RA)-receptor signaling pathways involved in regulating cell proliferation, differentiation, lipid metabolism, and inflammation in many alcohol-associated malignancies [25]. Different natural products are shown to activate retinoid receptors expressed in cancer cell types initiating redifferentiation in cancer cells [27].
Recently, a connection between alcohol as a carcinogen and cancer has been made in Fanconi anemia (FA) patients, who are at risk for leukemia and HNSCC [20, 23]. Consistent with this, a very recent study in humans have suggested a compromised FA pathway which likely leads to an increased accumulation of aldehyde-induced DNA damage in hematopoietic stem cells, resulting in p53/p21 mediated cell death or senescence [23]. Earlier, a similar finding was observed in a preclinical model in which the hematopoietic stem cells in ALDH2/FANCD2 double knockout mice accumulate more DNA damage than hematopoietic stem cells in either of the single knockout mice [20]. In summary, loss of the ALDH2 isozyme in FA humans and knockout mice results in accumulation of acetaldehyde, which then acts as a carcinogen by producing DNA crosslinks that are not repaired due to the loss of the FA/BRCA DNA repair pathway. These studies may provide a rationale to explain why alcohol is a factor in the etiology of non-FA HNSCC. In this idea, continual exposure to alcohol may result in enough acetaldehyde being produced to cause an accumulation of mutations and increased risk for HNSCC.
19.1.3.4 Alcohol and Nutrition
Various studies have shown that chronic alcohol abuse may alter the way body processes nutrients, consequently changing its carcinogenic potential. This has been supported by the studies reporting that alcoholics have reduced levels of zinc, iron, vitamin E, and vitamin B [17, 57]. Once nutrients are absorbed, alcohol can prevent their utilization in the body by altering their transport, storage, and excretion [51].
19.1.4 Chemoprevention
19.1.4.1 Biologic Basis of Chemoprevention
Molecular and genetic analyses have revealed that various pathways are compromised in different malignancies included head and neck cancer [34], and that these pathways are being targeted by chemotherapeutic agents to improve life quality of patients, but have limited success [1]. It is, thus, inevitable that additional alternative strategies are required to significantly enhance the therapeutic index of conventional treatment modalities. In this regard, dietary components are reported to inhibit cancer development, progression, and metastasis by modulating different mechanisms of cancer development, under a modality known as “cancer chemoprevention.”
19.1.5 Resveratrol as Chemopreventive Agent
Resveratrol, a grape-derived stilbene, is one of the most widely investigated chemopreventive agents retaining a wide variety of health-beneficial activities, including anticancer properties [42]. It has been shown to decelerate carcinogenesis process via direct and indirect multiple targets, mechanisms involved in the survival of cancer cells, and accelerating cell death. As detailed review of chemopreventive potential of resveratrol is beyond the scope of this chapter, we will briefly summarize the underlying molecular mechanism involved in chemopreventive efficacy of resveratrol in multistage carcinogenesis process.
19.1.5.1 Resveratrol in Xenometabolism
Under continuous exposure to pro-carcinogenic agent, normal cells undergo DNA mutations leading to initiation of the carcinogenesis process. Generally, carcinogens such as 7,12-dimethylbenzo[a]anthracene, benzanthracene, benzopyrene [B(a)P], and 4-nitroquinolone-1-oxide are converted to active metabolites in the presence of Phase I metabolic enzymes. These metabolites interact with genomic DNA forming adducts that directly correlate with cancer initiation, promotion, and progression stages. Resveratrol is shown to be effective in suppressing cancer initiation process by inhibiting these metabolic enzymes that play an important role in activation of pro-carcinogen [21]. Resveratrol modulates the activities of CYP1A1, CYP1B1, CYP3A, glutathione-S-transferase, UDP-glucuronosyl transferase (UGT), aryl hydrocarbon receptor (AhR), O-acetyl transferase, and sulfotransferase in both preclinical and clinical studies, thereby changing the risk of carcinogen undergoing metabolism [21, 69]. Resveratrol also activates phase II enzymes gene expression through modulation of mitogen-activated protein kinase pathways [21]. Resveratrol is also shown to differentially induce NAD(P)H quinone reductase (NQO), glutathione (GSH), glutathione reductase, and hemoxygenase 1 (HO-1), subsequently inhibiting DNA damage [21]. In contrast, in some of the cancer cells, resveratrol exerts pro-oxidant effect in the presence of transition metals such as Cu (II) depending on its concentration and time of exposure, leaving normal cells unharmed [40].
19.1.5.2 Resveratrol: As Anti-inflammatory Agent
In general, excessive generation of ROS and nitrogen species plays a pivotal role during inflammation [35]. Other two important enzymes involved in triggering inflammatory responses include cyclooxygenase and lipoxygenase, promoting tumor growth, progression and metastasis [52]. Among cyclooxygenase enzymes, COX1 plays a key role in prostaglandin synthesis, and COX2 is involved during inflammation [52]. Both of these enzymes are known to promote DNA synthesis, cell proliferation, invasion, and metastasis [27]. In this context, resveratrol is known to inhibit de novo synthesis of iNOS and COX2 via inhibition of NF-kB pathway as well the upstream kinases activating this pathway [51]. Resveratrol also targets nitric oxide production and lipoxygenase-stimulated inflammatory responses [7]. In conclusion, resveratrol counteracts ROS- and/or RNS-associated DNA damage and inflammatory responses as a part of its potential cancer chemopreventive efficacy.
19.1.5.3 Resveratrol: Cell Growth and Death Regulatory Pathways
Resveratrol exerts anti-proliferative activity via induction of cell growth inhibition, and induces apoptosis by modulating the major survival pathways present in the cancer cells [20]. Phosphatidylinositol 3-kinase (PI3K)/AKT pathway is considered as one of the major regulators of cell survival. Resveratrol is reported to suppress the activation of mitogen-activated protein kinases (MAPKs), c-Jun N-terminal kinase (JNK), MEK/ERK/NF-kB, cyclins, and cyclin dependent kinases (CDKs) leading to cell cycle arrest at specific stage and reversal of epithelial-to-mesenchymal transition (EMT) [4]. For instance, resveratrol has been shown to inhibit cell growth of different cancer cells at G0/G1 phase by altering cyclin D1/CDK4; in addition, resveratrol also causes S and G2/M phase cell cycle arrest resulting in increased cyclin A and E levels [62, 66, 67]. Moreover, a study by Shi and colleagues has shown that resveratrol exerts synergistic effects, when given in combination with the cytotoxic agent tamoxifen, on inhibiting the growth of both MCF-7/TR cells and metastasis [4]. Regarding the apoptosis induction, it is reported that resveratrol activates TNF-related apoptosis ligand, modulates the expression of pro-(Bax) and anti-(Bcl2 and Bcl-xL) apoptotic proteins, disrupts mitochondrial membrane potential, and causes caspases 9, 3 and poly (ADP-ribose) polymerase (PARP) cleavage, thus facilitating apoptotic cell death both in culture and mouse xenograft models [6, 50, 53, 62, 66]. As an upstream trigger to this cellular function, resveratrol is also shown to stimulate DNA damage response molecules and their downstream targets facilitating DNA damage response, cell cycle arrest, and apoptosis in various cancer models including HNSCC [11, 66]. Collectively, detailed mechanistic studies in preclinical cancer models have revealed that resveratrol targets PI3K/Akt/mTOR, NF-kB, MAPKs and apoptotic pathways, cell cycle regulatory molecules, different cellular receptors, and angiogenic pathways, which attribute towards its cancer chemopreventive efficacy.
19.1.5.4 Resveratrol: An Antioxidant
Antioxidant property of resveratrol is considered one of the crucial mechanisms involved in its chemopreventive and anticancer efficacy. In support to this idea, resveratrol is shown to prevent the generation of ROS following exposure to oxidizing agents, e.g., chemical carcinogens generated from tobacco and alcohol, hydrogen peroxide, etc. [21]. Resveratrol strongly increases the activity of antioxidant response element (ARE)/Nrf-2, leading to enhanced expression of phase II-detoxifying enzymes and antioxidant enzymes including NAD(P)H: quinone oxidoreductase 1(NQO 1) and hemoxygenase 1(HO1) via modulation of p38/PI3K/Akt pathways [21, 60]. Resveratrol has also been shown to enhance histone/protein deacetylase SIRT1 and adenosine monophosphate-activated protein kinase (AMPK) leading to metabolic changes in the cancer cells [62]. Likewise, resveratrol exhibits protective effect against ROS-mediated lipid peroxidation and DNA damage in normal cells, versus toxic effect in malignant cells including head and neck cancer [66]. More recently, Bishayee and colleagues have reported that resveratrol suppresses 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK)- and benzo[a]pyrene (B[a]P)-mediated precancerous changes in the human epithelial breast cancer cell MCF10A [6, 30].
19.1.5.5 Resveratrol: Interaction with DNA Polymerase, Topoisomerase, and Telomerase
Various preclinical studies have revealed that resveratrol directly binds to DNA and RNA through H-bond and stabilizes the double-helical structure, and this might serve as a molecular basis for anti-mutagenic effect of resveratrol [21, 39]. Resveratrol also impedes DNA replication by specifically interacting with DNA polymerase α and δ, resulting in DNA damage [20]. DNA polymerases are the enzymes required for de novo synthesis of DNA, and are equally crucial in protecting cells against the effects of DNA damage, and for initiating DNA repair [47]. Resveratrol is also reported to result in DNA damage through pro-oxidant effect in the presence of transition metal [40]. This might raise doubts of its beneficial function in normal cells versus cancer cells in general. However, it has been reported that pro-oxidant effect of these phytochemicals are more specific to cancer cells, for the fact that cancer cells have higher levels of transition metals, produce more ROS, etc. [63]. Similarly, Topoisomerase activity is particularly higher by several folds in cancer cells including squamous cell carcinoma, and has been targeted by many anticancer drugs [15]. Topoisomerase is essential for DNA replication, facilitating chromosome tangling, condensation, and mitotic segregation [21]. Three different types of topoisomerases are described in mammalian cells (type IA, type IB, and type II). Among all these, molecular modeling has confirmed that resveratrol specially binds to topoisomerase II and stabilizes the cleavage complexes of DNA and topoisomerase compromising DNA topology in cancer cells [3]. Similarly, resveratrol is shown to inhibit telomerase, a cellular reverse transcriptase that catalyzes the synthesis and extension of telomeric DNA, further assisting the cells to proliferate and delay the development of cell senescence [33]. Recently, several studies have also shown that resveratrol downregulates telomerase activity as well as inhibits the nuclear localization of human telomerase reverse transcriptase (hTERT), a subunit of telomerase [21, 33]. As hTERT is regulated by upstream protein kinase C, NF-kB, MAP kinases, and effect of resveratrol on hTERT might be indirect due to inhibition of these upstream kinases as well.
19.1.5.6 Resveratrol: DNA Damage and DNA Damage Repair
As mentioned earlier in this chapter that chemopreventive and anticancer activities of resveratrol have been implicated to involve DSBs. After DSBs, DNA repair molecules, for instance Mre11, Rad50, and Nbs1 (MRN complex), are stimulated at the site of DSBs, and recruits PI3K-related kinases such as ataxia telangiectasia mutated (ATM)/ATR to the DNA break site. Once activated, ATM phosphorylates several key DSB repair and checkpoint control factors like H2AX, p53, Nbs1, BRCA1, SMC1, Chk2, and Chk1 [19]. H2A.X is critical for facilitating the assembly of specific DNA-repair complexes on damaged DNA site [44]. Resveratrol is reported to induce S-phase arrest through activation of an ATM/ATR–Chk1/Chk2–Cdc25C pathway [67]. A study by Galicia and colleagues have shown that resveratrol at higher concentrations also triggers the downregulation of several genes of MMR, DNA replication, homologous recombination (HR), and cell growth inhibition [36]. Similarly, resveratrol modulates another set of genes up-regulated in different cancers, namely mini-chromosome maintenance [46] genes family, that are recruited to sites of DNA replication and facilitate DNA replication via helicase activity [38, 39]. In one recent study, resveratrol was shown to possess an anti-MCM effect by inducing a significant decrease in MCM2–MCM7 and MCM10 gene expression [36]. Interestingly, in the same study, the authors have found that resveratrol downregulated the expression of Rad51, BRCA1, and BRCA2 genes in MCF-7 breast cancer cells [36]. In contrast to this finding, study from our group has shown that resveratrol at lower concentrations (5–50 μmol/L) induces DNA damage in HNSCC cells but not in normal human epidermal keratinocytes, and causes S-phase arrest together with induction of Brca1 and gamma-H2AX foci in both in vitro and in vivo models [66]. This discrepancy may be due to the fact that effect of resveratrol in different systems depends upon the phenotype of cancer cells. It should be noted that BRCA1 plays an important role in the maintenance of genome stability, specifically through the HR pathway for double-strand DNA repair [61]. The results from a study suggest that resveratrol reduces the expression of these targets, blocks DNA repair mechanisms, which in turn leads to cell death [36].
19.1.5.7 Resveratrol: Clinical Studies
According to the US National Institute of Health, at present, several clinical trials are being conducted assessing the potential effects of resveratrol alone or in combination with other agents on human diseases, including cancer (http://clinicaltrials.gov). Most of these clinical studies are designed to assess the therapeutic efficacy of resveratrol as an antioxidant, anti-hypertensive, anti-diabetic, anti-inflammatory, cardiac problems, anti-erythema, metabolic syndrome, and anticancer agent [62]. Red wine rich in resveratrol, has long been thought to be beneficial in preventing heart disease by increasing the levels of “good” cholesterol and protecting against artery damage. In one of the randomized double blinded placebo controlled studies, 50 healthy adult smokers were given 500 mg−1 resveratrol or placebo for 30 days, followed by a wash-out period of 4 weeks to determine the effect of resveratrol on endothelial function. The investigators have reported that 4 weeks of resveratrol treatment, significantly reduced triglyceride concentration and increased antioxidant status [4]. In another study resveratrol was evaluated against systemic oxidative stress, which revealed that it significantly increases antioxidant properties [6]. Similarly, high level of resveratrol is shown to inhibit CYPs and interact with transporters which modify the CYPs-mediated metabolism [72]. In another randomized control trial by De Groote et al., the investigator evaluated the change in the gene expression after resveratrol (150 mg/day for 28 days) ingestion. The results from this study have demonstrated that genes affected include antioxidants, inflammatory, stress-response and those regulating cell growth [11]. Another published study with colon cancer patients receiving either 500 or 1,000 mg of resveratrol has shown that it decreases the expression of Ki-67 proliferation marker. In contrary, another study with same dose of resveratrol did not exhibit any significant difference [62]. In a study by Howells et al., hepatic cancer patients (n = 3 receiving 5 g/day for 10–21 days) receiving resveratrol prior to surgery, have shown that apoptosis marker (cleaved caspase 3) was significantly increased in malignant hepatic tissues; however, there was no effect in the hepatic tissue levels of IGF-1, Ki-67, phospho-Akt, phospho-GSK, GSK3, phospho-ERK, ERK, β-catenin, survivin, Bcl-1, Bax, or PARP [27]. There are many mechanisms and pathways which are proven to be regulated by resveratrol in both preclinical and clinical studies, and to summarize all of these studies is beyond the scope of this chapter.
19.1.6 Conclusions and Prospect of Resveratrol in HNSCC
In HNSCC, the acute toxicity associated with conventional therapies is observed in 30–40 % of cases, thereby preventing from timely completion of therapy, affecting overall survival rates of the patients [64]. The results from different studies have revealed that only 10–20 % of patients are benefited from single targeted therapies, and remaining exhibit intrinsic resistance, thereby, limiting their clinical use [13, 31, 58]. Furthermore, >50 % of the head and neck patients undergoing surgical resection of primary tumors develop loco-regional recurrence, and the molecular genesis driving this phenomenon of secondary tumor development is largely unknown. Hence, from translational viewpoint, natural agents like resveratrol have demonstrated promising anti-tumor and cancer chemopreventive efficacy against different malignancies included head and neck cancer, by exerting pleiotropic effects on different signaling pathways as summarized in Fig. 19.1. Similarly, resveratrol is also shown to bind to DNA, inhibit DNA polymerase α/δ, modulate topoisomerase and telomerase activity, induce DNA damage, and alter DNA repair pathways (schematically shown in Fig. 19.1). Considering the importance of DNA repair mechanism in developing resistance to DNA damaging agents, often limiting the therapeutic efficacy of chemotherapy agents, it is suggestive that resveratrol might help to overcome drug resistance, reduce drug toxicity, and enhance efficacy when used in combination with other therapeutic agents. Furthermore, considering the selective toxicity to cancer cells, resveratrol might be a promising chemopreventive agent in a wide-range of HNSCC patients including smokers, alcoholics and FA patients; however, this assumption needs rigorous pre-clinical followed by clinical studies before resveratrol could “really” be beneficial to the identified cancer patient population.
Abbreviations
- 4NQO:
-
4-Nitroquinoline 1-oxide
- ADH:
-
Alcohol dehydrogenase
- ALDH:
-
Aldehyde dehydrogenase
- AP-1:
-
Activator protein 1
- ARE:
-
Antioxidant response element
- ATM:
-
Ataxia telangiectasia mutated
- ATR:
-
Ataxia telangiectasia-Rad3-related
- B[A]P:
-
Benzo[a]pyrene
- BER:
-
Base excision repair
- Brca1:
-
Breast cancer gene 1
- Cdc25C:
-
Cell division cycle 25C
- CDKs:
-
Cyclin dependent kinases
- Chk1/2:
-
Checkpoint kinase 1/2
- COX2:
-
Cyclooxygenase 2
- CYP450:
-
Cytochrome P450s
- DMBA:
-
7,12-Dimethylbenz[α]anthracene
- DSBs:
-
Double strand break
- EGFR:
-
Epidermal growth factor receptor
- Egr 1:
-
Early growth response 1
- EMT:
-
Epithelial mesenchymal transition
- FA:
-
Fanconi anemia
- GSH:
-
Glutathione
- HNSCC:
-
Head and neck squamous cell carcinoma
- HPV:
-
Human papilloma virus
- HRR:
-
Homologous recombination repair
- IGFR:
-
Insulin-like growth factor receptor
- iNOS:
-
Inducible nitric oxide synthetase
- JNK:
-
c-Jun N-terminal kinase
- MAPK:
-
Mitogen-activated protein kinases
- MCM:
-
Minichromosome maintenance
- MMPs:
-
Metalloproteinases
- MMR:
-
Mismatch repair
- mTOR:
-
Mammalian target of rapamycin
- NER:
-
Nucleotide excision repair
- NF-kB:
-
Nuclear factor kappa B
- NHEJ:
-
Non-homologous end joining
- NNK:
-
4-Methylnitrosamine-1-(3-pyridyl)-1-butanone
- P53:
-
Protein 53
- PARP:
-
Poly (ADP-ribose) polymerases
- PCNA:
-
Proliferating cell nuclear antigen
- RA:
-
Retinoic acid
- Rb:
-
Retinoblastoma protein
- Res:
-
Resveratrol
- ROS/RNS:
-
Reactive oxygen species/reactive nitrogen species
- SPT:
-
Secondary primary tumor
- SSBs:
-
Single strand break
- STAT3:
-
Signal transducer and activator of transcription 3
References
Aggarwal BB, Shishodia S (2006) Molecular targets of dietary agents for prevention and therapy of cancer. Biochem Pharmacol 71(10):1397–1421
Balbo S, Meng L et al (2012) Kinetics of DNA adduct formation in the oral cavity after drinking alcohol. Cancer Epidemiol Biomarkers Prev 21(4):601–608
Basso E, Fiore M et al (2013) Effects of resveratrol on topoisomerase II-alpha activity: induction of micronuclei and inhibition of chromosome segregation in CHO-K1 cells. Mutagenesis 28(3):243–248
Bo S, Ciccone G et al (2013) Anti-inflammatory and antioxidant effects of resveratrol in healthy smokers a randomized, double-blind, placebo-controlled, cross-over trial. Curr Med Chem 20(10):1323–1331
Brown GC, Borutaite V (2011) There is no evidence that mitochondria are the main source of reactive oxygen species in mammalian cells. Mitochondrion 12(1):1–4
Buonocore D, Lazzeretti A et al (2012) Resveratrol-procyanidin blend: nutraceutical and antiaging efficacy evaluated in a placebocontrolled, double-blind study. Clin Cosmet Investig Dermatol 5:159–165
Choi S, Myers JN (2008) Molecular pathogenesis of oral squamous cell carcinoma: implications for therapy. J Dent Res 87(1):14–32
Connell PP, Jayathilaka K et al (2006) Pilot study examining tumor expression of RAD51 and clinical outcomes in human head cancers. Int J Oncol 28(5):1113–1119
Cui R, Kamatani Y et al (2009) Functional variants in ADH1B and ALDH2 coupled with alcohol and smoking synergistically enhance esophageal cancer risk. Gastroenterology 137(5):1768–1775
Day GL, Blot WJ et al (1994) Second cancers following oral and pharyngeal cancers: role of tobacco and alcohol. J Natl Cancer Inst 86(2):131–137
De Groote D, Van Belleghem K et al (2012) Effect of the intake of resveratrol, resveratrol phosphate, and catechin-rich grape seed extract on markers of oxidative stress and gene expression in adult obese subjects. Ann Nutr Metab 61(1):15–24
Derry MM, Raina K et al (2013) Identifying molecular targets of lifestyle modifications in colon cancer prevention. Front Oncol 3:119
Dudek AZ, Lesniewski-Kmak K et al (2009) Phase I study of bortezomib and cetuximab in patients with solid tumours expressing epidermal growth factor receptor. Br J Cancer 100(9):1379–1384
Ferlay J, Shin HR et al (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127(12):2893–2917
Fortune JM, Osheroff N (2000) Topoisomerase II as a target for anticancer drugs: when enzymes stop being nice. Prog Nucleic Acid Res Mol Biol 64:221–253
Fouret P, Monceaux G et al (1997) Human papillomavirus in head and neck squamous cell carcinomas in nonsmokers. Arch Otolaryngol Head Neck Surg 123(5):513–516
Freedman ND, Schatzkin A et al (2007) Alcohol and head and neck cancer risk in a prospective study. Br J Cancer 96(9):1469–1474
Freudlsperger C, Burnett JR et al (2010) EGFR-PI3K-AKT-mTOR signaling in head and neck squamous cell carcinomas: attractive targets for molecular-oriented therapy. Expert Opin Ther Targets 15(1):63–74
Furgason JM, Bahassi M et al (2012) Targeting DNA repair mechanisms in cancer. Pharmacol Ther 137(3):298–308
Garaycoechea JI, Crossan GP et al (2012) Genotoxic consequences of endogenous aldehydes on mouse haematopoietic stem cell function. Nature 489(7417):571–575
Gatz SA, Wiesmuller L (2008) Take a break—resveratrol in action on DNA. Carcinogenesis 29(2):321–332
Gillison ML, Koch WM et al (2000) Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst 92(9):709–720
Hira A, Yabe H et al (2013) Variant ALDH2 is associated with accelerated progression of bone marrow failure in Japanese Fanconi anemia patients. Blood 122(18):3206–3209
Hoeijmakers JH (2001) Genome maintenance mechanisms for preventing cancer. Nature 411(6835):366–374
Hong WK, Endicott J et al (1986) 13-cis-retinoic acid in the treatment of oral leukoplakia. N Engl J Med 315(24):1501–1505
Howard JD, Lu B et al (2012) Therapeutic targets in head and neck squamous cell carcinoma: identification, evaluation, and clinical translation. Oral Oncol 48(1):10–17
Howells LM, Berry DP et al (2011) Phase I randomized, double-blind pilot study of micronized resveratrol (SRT501) in patients with hepatic metastases–safety, pharmacokinetics, and pharmacodynamics. Cancer Prev Res (Phila) 4(9):1419–1425
Irish JC, Bernstein A (1993) Oncogenes in head and neck cancer. Laryngoscope 103(1 Pt 1):42–52
Ishiji T (2000) Molecular mechanism of carcinogenesis by human papillomavirus-16. J Dermatol 27(2):73–86
Jelski W, Kutylowska E et al (2011) Alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) as candidates for tumor markers in patients with pancreatic cancer. J Gastrointestin Liver Dis 20(3):255–259
Kundu SK, Nestor M (2012) Targeted therapy in head and neck cancer. Tumour Biol 33(3):707–721
Lachenmeier DW, Monakhova YB (2011) Short-term salivary acetaldehyde increase due to direct exposure to alcoholic beverages as an additional cancer risk factor beyond ethanol metabolism. J Exp Clin Cancer Res 30:3
Lanzilli G, Fuggetta MP et al (2006) Resveratrol down-regulates the growth and telomerase activity of breast cancer cells in vitro. Int J Oncol 28(3):641–648
Leemans CR, Braakhuis BJ et al (2011) The molecular biology of head and neck cancer. Nat Rev Cancer 11(1):9–22
Lenaz G (2001) The mitochondrial production of reactive oxygen species: mechanisms and implications in human pathology. IUBMB Life 52(3–5):159–164
Leon-Galicia I, Diaz-Chavez J et al (2013) Resveratrol induces downregulation of DNA repair genes in MCF-7 human breast cancer cells. Eur J Cancer Prev 22(1):11–20
Maacke H, Opitz S et al (2000) Over-expression of wild-type Rad51 correlates with histological grading of invasive ductal breast cancer. Int J Cancer 88(6):907–913
Maiorano D, Lutzmann M et al (2006) MCM proteins and DNA replication. Curr Opin Cell Biol 18(2):130–136
Markus MA, Marques FZ et al (2011) Resveratrol, by modulating RNA processing factor levels, can influence the alternative splicing of pre-mRNAs. PLoS One 6(12):e28926
Martins LA, Coelho BP et al (2014) Resveratrol induces pro-oxidant effects and time-dependent resistance to cytotoxicity in activated hepatic stellate cells. Cell Biochem Biophys 68(2):247–257
Mitra A, Jameson C et al (2009) Overexpression of RAD51 occurs in aggressive prostatic cancer. Histopathology 55(6):696–704
Nassiri-Asl M, Hosseinzadeh H (2009) Review of the pharmacological effects of Vitis vinifera (Grape) and its bioactive compounds. Phytother Res 23(9):1197–1204
Nguyen SA, Walker D et al (2012) mTOR inhibitors and its role in the treatment of head and neck squamous cell carcinoma. Curr Treat Options Oncol 13(1):71–81
O’Neil N, Rose A (2006) DNA repair. WormBook, pp 1–12
Ohba S, Fujii H et al (2009) Overexpression of GLUT-1 in the invasion front is associated with depth of oral squamous cell carcinoma and prognosis. J Oral Pathol Med 39(1):74–78
Paglin S, Hollister T et al (2001) A novel response of cancer cells to radiation involves autophagy and formation of acidic vesicles. Cancer Res 61(2):439–444
Pavlov YI, Shcherbakova PV et al (2006) Roles of DNA polymerases in replication, repair, and recombination in eukaryotes. Int Rev Cytol 255:41–132
Petti S (2009) Lifestyle risk factors for oral cancer. Oral Oncol 45(4–5):340–350
Poeta ML, Manola J et al (2007) TP53 mutations and survival in squamous-cell carcinoma of the head and neck. N Engl J Med 357(25):2552–2561
Radhakrishnan S, Reddivari L et al (2011) Resveratrol potentiates grape seed extract induced human colon cancer cell apoptosis. Front Biosci (Elite Ed) 3:1509–1523
Radojicic J, Zaravinos A et al (2012) HPV, KRAS mutations, alcohol consumption and tobacco smoking effects on esophageal squamous-cell carcinoma carcinogenesis. Int J Biol Markers 27(1):1–12
Rakoff-Nahoum S (2006) Why cancer and inflammation? Yale J Biol Med 79(3–4):123–130
Roy S, Kaur M et al (2007) p21 and p27 induction by silibinin is essential for its cell cycle arrest effect in prostate carcinoma cells. Mol Cancer Ther 6(10):2696–2707
Rusin P, Olszewski J et al (2009) Comparative study of DNA damage and repair in head and neck cancer after radiation treatment. Cell Biol Int 33(3):357–363
Sanchez-Alvarez R, Martinez-Outschoorn UE et al (2013) Ethanol exposure induces the cancer-associated fibroblast phenotype and lethal tumor metabolism: implications for breast cancer prevention. Cell Cycle 12(2):289–301
Sankaranarayanan R, Masuyer E et al (1998) Head and neck cancer: a global perspective on epidemiology and prognosis. Anticancer Res 18(6B):4779–4786
Seitz HK, Stickel F (2007) Molecular mechanisms of alcohol-mediated carcinogenesis. Nat Rev Cancer 7(8):599–612
Sharafinski ME, Ferris RL et al (2010) Epidermal growth factor receptor targeted therapy of squamous cell carcinoma of the head and neck. Head Neck 32(10):1412–1421
Siegel R, Naishadham D et al (2013) Cancer statistics, 2013. CA Cancer J Clin 63(1):11–30
Signorelli P, Ghidoni R (2005) Resveratrol as an anticancer nutrient: molecular basis, open questions and promises. J Nutr Biochem 16(8):449–466
Smith J, Tho LM et al (2010) The ATM-Chk2 and ATR-Chk1 pathways in DNA damage signaling and cancer. Adv Cancer Res 108:73–112
Tome-Carneiro J, Larrosa M et al (2013) Resveratrol and clinical trials: the crossroad from in vitro studies to human evidence. Curr Pharm Des 19(34):6064–6093
Trachootham D, Alexandre J et al (2009) Targeting cancer cells by ROS-mediated mechanisms: a radical therapeutic approach? Nat Rev Drug Discov 8(7):579–591
Tsao AS, Garden AS et al (2006) Phase I/II study of docetaxel, cisplatin, and concomitant boost radiation for locally advanced squamous cell cancer of the head and neck. J Clin Oncol 24(25):4163–4169
Turati F, Garavello W et al (2010) A meta-analysis of alcohol drinking and oral and pharyngeal cancers. Part 2: results by subsites. Oral Oncol 46(10):720–726
Tyagi A, Gu M et al (2011) Resveratrol selectively induces DNA damage, independent of Smad4 expression, in its efficacy against human head and neck squamous cell carcinoma. Clin Cancer Res 17(16):5402–5411
Tyagi A, Singh RP et al (2005) Resveratrol causes Cdc2-tyr15 phosphorylation via ATM/ATR-Chk1/2-Cdc25C pathway as a central mechanism for S phase arrest in human ovarian carcinoma Ovcar-3 cells. Carcinogenesis 26(11):1978–1987
Wang M, Chu H et al (2013) Molecular epidemiology of DNA repair gene polymorphisms and head and neck cancer. J Biomed Res 27(3):179–192
Weng CJ, Yen GC (2012) Chemopreventive effects of dietary phytochemicals against cancer invasion and metastasis: phenolic acids, monophenol, polyphenol, and their derivatives. Cancer Treat Rev 38(1):76–87
Woutersen RA, Appelman LM et al (1986) Inhalation toxicity of acetaldehyde in rats. III. Carcinogenicity study. Toxicology 41(2):213–231
Yokoyama A, Muramatsu T et al (1998) Alcohol-related cancers and aldehyde dehydrogenase-2 in Japanese alcoholics. Carcinogenesis 19(8):1383–1387
Chow, H. H., L. L. Garland, et al. (2010). “Resveratrol modulates drug- and carcinogen-metabolizing enzymes in a healthy volunteer study.” Cancer Prev Res (Phila) 3(9): 1168–1175
Grant Support:
Supported by grants to R. Sclafani from the Fanconi Anemia Research Foundation and the University of Colorado Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this paper
Cite this paper
Shrotriya, S., Agarwal, R., Sclafani, R.A. (2015). A Perspective on Chemoprevention by Resveratrol in Head and Neck Squamous Cell Carcinoma. In: Vasiliou, V., Zakhari, S., Seitz, H., Hoek, J. (eds) Biological Basis of Alcohol-Induced Cancer. Advances in Experimental Medicine and Biology, vol 815. Springer, Cham. https://doi.org/10.1007/978-3-319-09614-8_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-09614-8_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-09613-1
Online ISBN: 978-3-319-09614-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)