Abstract
Diagnostic and prognostic biomarkers are used to predict the progress and outcome of several chronic diseases, including neoplastic and noncommunicable diseases. Recently, biomarker research has been exploited to accurately discriminate the severe forms of malaria, since no biological tests to confirm the diagnosis of severe malaria and its complications are available so far. In this context, human lysozyme appears as a good candidate. Since its discovery almost one century ago, several easy-to-handle and cost-effective methods to determine lysozyme activity in various samples (plasma, urine, and tissue sections) have been developed. Interestingly, results from two small prospective studies enrolling healthy volunteers and malaria patients from Sudan showed a significant correlation between disease severity and lysozyme plasma levels. These promising data encourage further studies employing larger cohorts of patients from different areas endemic for malaria. Intriguingly, an old molecule such as human lysozyme might reveal itself as a new and effective biomarker for malaria severity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Biomarkers are substances such as metabolites, enzymes, cytokines, and genetic markers that can be objectively measured in any biological fluids or specimens—including serum, plasma, urine, and cells—and used as indicators of physiological and pathological processes as well as responses to therapeutics. As such, biomarkers allow to support disease management and control by prosecuting different objectives: (1) to diagnose a disease; (2) to assess disease severity; (3) to provide a prognosis; (4) to provide some information relevant for the treatment and management of the disease; and (5) to identify the patients at risk for incurrence of the disease itself as well as long-term complications. Notably, the procedures required for biomarker evaluation must be simple, quantitative, and inexpensive therefore allowing for wide usage.
To date, biomarkers have been employed to diagnose and prognosticate the progress and outcome of several chronic and acute infectious, metabolic, and noncommunicable diseases, including cancer, diabetes, autoimmune diseases, and HIV/AIDS. However, the use of biomarkers in parasitic infectious diseases has been limited so far. As discussed in Chap. 1, the transition from mild malaria to the severe forms of malaria can be sudden and requires immediate intervention. Therefore, the use of biomarkers to risk-stratify severe malaria patients would greatly enhance patient care and assist in appropriate management of health care resources (Lucchi et al. 2011). In addition, biomarkers able to identify asymptomatic patients, who might have levels of parasitemia undetectable by light microscopy or other conventional testing methods (see Chap. 2), could play a key role in monitoring the elimination of malaria reservoirs from endemic populations (Ogutu et al. 2010). The use of early, diagnostic, and prognostic biomarkers during the clinical course of malaria (see Fig. 6.1) might significantly improve the results obtained by malaria control and management programs.
Intriguingly, little yet consistent evidence is currently available from in vitro experiments (Prato et al. 2009; Polimeni et al. 2012, 2013) as well as from clinical studies (Mohamed et al. 1996; Mohammed et al. 2003) showing that increased levels of human lysozyme are associated with malaria severity. As it will be discussed in the next paragraphs, lysozyme can be detected in human fluids and specimens through several simple, quantitative, and inexpensive techniques. Therefore, a potential role for this molecule as an affordable biomarker of malaria severity has been recently proposed (Prato 2012).
Of course, it should be noted that the employment of biomarkers in the clinical practice requires a thorough validation of their utility. Collectively, five phases of biomarker development can be pinpointed (Pepe et al. 2001; Coca and Parikh 2008). The initial phase involves preclinical exploration during which potential biomarkers are identified. At this phase, markers capable of discriminating the severity of the disease are identified. During the second phase, new clinical assays measuring the potential biomarkers are established. In the third phase, retrospective longitudinal studies are carried out to test the new biomarkers for their utility, sensitivity, and specificity. The fourth phase involves a prospective screening phase which entails the use of the identified biomarkers to screen large populations. Finally, during the fifth phase the impact of the biomarkers on disease control and management is determined. In this context, the data supporting a role for human lysozyme as a marker of malaria severity have been scaled up to the third phase so far.
2 Methods to Measure Lysozyme Levels in Human Specimens
Since the discovery of lysozyme (Fleming 1922), several authors have proposed different methods for determining the activity of various preparations containing this enzyme. Most of these methods were based upon the clearing of dense suspensions of a susceptible organism without concern for accurate quantitative results. In 1946, the isolation of highly purified crystalline lysozyme by Alderton and Fevold suggested the possibility of a method for assaying lysozyme (Alderton and Fevold 1946). Since then, several quantitative methods to measure lysozyme levels in human fluids (serum, blood, urine) and specimens (tissues and cells) have been developed and standardized. In these days, several simple, cheap, and sensitive approaches routinely employed in research and diagnostic laboratories are available, including: (1) photometric assay; (2) radioimmunoassay (RIA); (3) immunohistochemistry (IHC); and (4) enzyme-linked immunoadsorbent assay (ELISA).
2.1 Photometric Assay
Lysozyme photometric assays have been developed after the methods proposed by Smolelis and Hartsell (1949) and Litwack (1955). These procedures provide for the rapid and accurate microbiological assay of fluid materials that show lytic activity considered to be due to lysozyme, including urine, serum, saliva, mucus, and tears (Osserman and Lawlor 1966; Seal et al. 1980).
The method is based on a comparison of light transmissions of standard crystalline lysozyme dilutions with the values for the substance being tested, after the addition of susceptible cells and incubation. A purified hen egg lysozyme is generally used as the standard. The natural substrate for lysozyme is the high molecular weight, insoluble peptidoglycan polymer that generally reinforces the bacterial cell wall. As such, this molecule—employed in the form of dried cells of UV-inactivated Micrococcus lysodeikticus—represents the most widely used substrate for measuring lysozyme lytic action on the linkages between N-acetylmuramic acid and N-acetylglucosamine in the cell wall. The cell suspension from the dried cells and the dilutions of crystalline lysozyme from a stock solution are prepared in Sorenson’s phosphate buffer, pH 6.2. Rehydration is easily accomplished since lyophilized cells can be readily resuspended. Prior to the test the unknown should be checked for its activity to determine what dilutions are needed to give the same level of activity as the crystalline control. Before beginning the assay, a sufficient number of test tubes are matched so that all tubes will show the same light transmission value with distilled water as a reference. At measured intervals the lysozyme dilution is mixed with the cell suspension. The same procedure is used for the dilutions of the material being tested. All mixtures are made in duplicate.
After a 20-min incubation at room temperature, the light transmissions for the various mixtures are recorded and the concentration of the unknown is determined. With the transmission values for the crystalline lysozyme mixtures, a standard curve is prepared by plotting the transmission against concentration. A log scale is used on the abscissa of the standard curve. The transmission values for the unknown dilutions are located on the ordinate and projected to the standard curve. By projection to the abscissa from these points, the concentration of lysozyme in each dilution is determined. Multiplication by the dilution factor results in the concentration of lysozyme per mL of undiluted extract. The results obtained from this test are generally accurate and reliable.
2.2 Radioimmunoassay
The first studies to develop a RIA for human serum and urinary lysozyme date back to the late 1970s (Peeters et al. 1978; Thomas et al. 1981), as a consequence of the ongoing discussion concerning the diagnostic value of serum lysozyme determinations in gastrointestinal diseases, where differences in methodology were evoked as the cause of the observed discrepancies (Falchuk et al. 1975; Peeters et al. 1976).
Briefly, antiserum and labeled lysozyme are diluted in phosphate-buffered saline with 20 g/L of bovine serum albumin while standard dilutions are prepared from a stock lysozyme solution. Antiserum and labeled lysozyme are added to the standards and the diluted samples. The vials are incubated overnight at 4 °C, then the bound and free moieties are separated, vortex-mixed, and centrifuged. After aspirating the supernatant fluid, the radioactivity of the “free” fraction is counted. Samples of pooled sera at low, medium, and high lysozyme concentrations may serve as a quality control. Lysozyme results are interpolated from a curve, constructed by plotting the “free” count rate (in cpm) of standards versus the concentration of lysozyme.
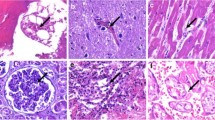
2.3 Immunohistochemistry
IHC has become an increasingly popular and effective tool in research and diagnostic laboratories. The manifest success of this method is due to technological improvements, increased availability of purified antigens, antisera, and other reagents, and the accumulation of practical experience in a variety of applications. IHC combines the advantages of the high specificity and affinity of antibodies in recognizing tissue antigens with the high topographical resolution of light and electron microscopy. It can thus provide information which would be difficult or impossible to obtain by other techniques (Linnoila and Petrusz 1984).
In the respiratory system, for example, IHC investigations have demonstrated the presence of lysozyme in a number of different cell types, including serous cells of bronchial glands, neutrophils, and alveolar macrophages, pointing to the role of the enzyme as an antibacterial agent and as a diagnostic biomarker for pneumonia (Ishii et al. 2010). Specific staining was obtained with rabbit anti-rat lysozyme or anti-human urinary lysozyme antibodies but not with antibodies against egg white lysozyme.
2.4 Enzyme-Linked Immunoadsorbent Assay
Several ELISA kits for research or diagnostic purposes are commercially available to quantitatively measure lysozyme levels in human plasma, serum, urine, saliva, tears, mucus, and cell culture supernatants (Tiwari et al. 2012; Lu et al. 2014). This assay employs a quantitative competitive enzyme immunoassay technique that measures lysozyme rather quickly (~3 h). In general, an antibody specific for lysozyme is precoated onto a 96-well microplate with removable strips. Lysozyme in standards and samples can be competed with a biotinylated lysozyme sandwiched by the immobilized antibody and streptavidin-peroxidase conjugate. All unbound material is then washed away and a peroxidase enzyme substrate is added. The color development is stopped and the intensity of the color is measured. Lysozyme levels in the samples are finally calculated based on the generated standard curve.
3 Plasma Levels of Human Lysozyme in Malaria Patients
Although no retrospective longitudinal studies are available so far, the results from two small prospective studies enrolling healthy volunteers and malaria patients from Sudan have intriguingly shown enhanced lysozyme plasma levels in malaria patients, with a significant correlation between disease severity and lysozyme levels.
The first study (Mohamed et al. 1996) enrolled 14 patients with severe malaria cases in the pediatric casualty ward of Khartoum Teaching Hospital, Sudan, displaying convulsions, coma, and fever as clinical features with thick blood film positive for P. falciparum. Blood samples were collected before the administration of quinine, the standard treatment in such conditions. Lysozyme was estimated by RIA. Mean plasma lysozyme levels in patients were ~2200 μg/L, an amount almost double with respect to the corresponding levels in the controls. The differences between the levels of lysozyme in the patients and the controls were significant.
Interestingly, there was also a strong correlation between the levels of lysozyme and those of myeloperoxidase, another enzyme secreted by leucocytes (Dunn et al. 1968). The authors suggested that such a correlation may mean that both molecules were produced by the same cell type, or that the signal that activates myeloperoxidase production is also responsible for macrophage activation. It should be noted that the products of neutrophil degranulation are toxic to host tissues. Therefore, they may be responsible for the induction of severe malaria. However, both myeloperoxidase and lysozyme are produced also by monocytes/macrophages. Additionally, the study did not compare uncomplicated and severe malaria.
For this reason, the role of neutrophil activation in severe malaria patients was investigated by the same group in a second Sudanese study (Mohammed et al. 2003). Mohammed and colleagues enrolled three groups: (1) healthy individuals (n = 18); (2) patients with uncomplicated malaria (n = 25); and (3) patients with severe malaria (n = 22). Moreover, they did not measure lysozyme and myeloperoxidase plasma levels only, but also human neutrophil lipocalin, a specific marker for neutrophil activation stored in neutrophil secondary granules (Xu et al. 1994). All malaria patients were P. falciparum infected, since patients infected with P. vivax or with mixed infections were excluded. Patients with mild, uncomplicated malaria received standard chloroquine, pyrimethamine/sulfadoxine, or quinine treatment.
Before starting the treatment, blood was collected from all individuals involved in the study. The plasma concentrations of lysozyme, lipocalin, and myeloperoxidase were measured by a double-antibody RIA. The severe malaria group showed significantly higher levels of all three proteins as compared with the mild malaria group or the group with no malaria. There were no significant differences between the mild malaria group and the group with no malaria. Interestingly, there was a highly significant correlation between the plasma levels of lipocalin and myeloperoxidase or lysozyme, respectively.
Notably, some studies have shown that the hemozoin-containing leucocyte count is a simple marker of disease severity in children with malaria (Amodu et al. 1997, 1998; Were et al. 2009). Consistently, as discussed in Chap. 5, the phagocytosis of hemozoin by human leucocytes has been associated with enhanced lysozyme secretion (Prato et al. 2009; Polimeni et al. 2012, 2013).
4 Conclusion
According to the results from two small prospective studies performed on Sudanese patients with malaria, human plasma lysozyme appears as a good candidate marker of disease severity. Therefore, future prospective as well as retrospective studies using larger cohorts of patients, possibly from different geographic areas, are certainly encouraged to assess the possible role of lysozyme as a biomarker for malaria.
References
Alderton G, Fevold HL (1946) Direct crystallization of lysozyme from egg white and some crystalline salts of lysozyme. J Biol Chem 164:1–5
Amodu OK, Adeyemo AA, Olumese PE et al (1997) Intraleucocyte malaria pigment in asymptomatic and uncomplicated malaria. East Afr Med J 74:714–716
Amodu OK, Adeyemo AA, Olumese PE et al (1998) Intraleucocytic malaria pigment and clinical severity of malaria in children. Trans R Soc Trop Med Hyg 92:54–56
Coca SG, Parikh CR (2008) Urinary biomarkers for acute kidney injury: perspectives on translation. Clin J Am Soc Nephrol 3:481–490
Dunn WB, Hardin JH, Spicer SS (1968) Ultrastructural localization of myeloperoxidase in human neutrophil and rabbit heterophil and eosinophil leucocytes. Blood 32:935–944
Falchuk KR, Perrotto JL, Isselbacher KJ (1975) Serum lysozyme in Crohn’s disease and ulcerative colitis. N Engl J Med 292:395–397
Fleming A (1922) On a remarkable bacteriolytic element found in tissues and secretions. Proc R Soc Lond Ser B Biol Sci 93:306–317
Ishii H, Iwata A, Oka H et al (2010) Elevated serum levels of lysozyme in desquamative interstitial pneumonia. Intern Med 49:847–851
Linnoila I, Petrusz P (1984) Immunohistochemical techniques and their applications in the histopathology of the respiratory system. Environ Health Perspect 56:131–148
Litwack G (1955) Photometric determination of lysozyme activity. Proc Soc Exp Biol Med 89:401–403
Lu D, Li Q, Wu Z et al (2014) High-level recombinant human lysozyme expressed in milk of transgenic pigs can inhibit the growth of Escherichia coli in the duodenum and influence intestinal morphology of sucking pigs. PLoS One 9:e89130
Lucchi NW, Jain V, Wilson NO et al (2011) Potential serological biomarkers of cerebral malaria. Dis Markers 31:327–335
Mohamed AO, Elbashir MI, Ibrahim G et al (1996) Neutrophil leucocyte activation in severe malaria. Trans R Soc Trop Med Hyg 90:277
Mohammed AO, Elghazali G, Mohammed HB et al (2003) Human neutrophil lipocalin: a specific marker for neutrophil activation in severe Plasmodium falciparum malaria. Acta Trop 87:279–285
Ogutu B, Tiono AB, Makanga M et al (2010) Treatment of asymptomatic carriers with artemether-lumefantrine: an opportunity to reduce the burden of malaria? Malar J 9:30
Osserman EF, Lawlor DP (1966) Serum and urinary lysozyme (muramidase) in monocytic and monomyelocytic leukemia. J Exp Med 124:921–952
Peeters TL, Vantrappen G, Geboes K (1976) Serum lysozyme levels in Crohn’s disease and ulcerative colitis. Gut 17:300–305
Peeters TL, Depraetere YR, Vantrappen GR (1978) Radioimmunoassay for urinary lysozyme in human serum from leukemic patients. Clin Chem 24:2155–2157
Pepe MS, Etzioni R, Feng Z et al (2001) Phases of biomarker development for early detection of cancer. J Natl Cancer Inst 93:1054–1061
Polimeni M, Valente E, Aldieri E et al (2012) Haemozoin induces early cytokine-mediated lysozyme release from human monocytes through p38 MAPK- and NF-kappaB-dependent mechanisms. PLoS One 7(6):e39497
Polimeni M, Valente E, Aldieri E et al (2013) Role of 15-hydroxyeicosatetraenoic acid in hemozoin-induced lysozyme release from human adherent monocytes. Biofactors 39(3):304–314
Prato M (2012) Human and mosquito lysozymes in malaria: old molecules for new approaches towards diagnosis, therapy and vector control. J Bacteriol Parasitol 3:e113
Prato M, Giribaldi G, Arese P (2009) Hemozoin triggers tumor necrosis factor alpha-mediated release of lysozyme by human adherent monocytes: new evidences on leucocyte degranulation in P. falciparum malaria. Asian Pac J Trop Med 2:35–40
Seal DV, Mackie IA, Coakes RL et al (1980) Quantitative tear lysozyme assay: a new technique for transporting specimens. Br J Ophthalmol 64:700–704
Smolelis AN, Hartsell SE (1949) The determination of lysozyme. J Bacteriol 58:731–736
Thomas MJ, Russo A, Craswell P et al (1981) Radioimmunoassay for serum and urinary lysozyme. Clin Chem 27:1223–1226
Tiwari S, Ali MJ, Balla MM et al (2012) Establishing human lacrimal gland cultures with secretory function. PLoS One 7:e29458
Were T, Davenport GC, Yamo EO et al (2009) Naturally acquired hemozoin by monocytes promotes suppression of RANTES in children with malarial anemia through an IL-10-dependent mechanism. Microbes Infect 11:811–819
Xu SY, Carlson M, Engström A et al (1994) Purification and characterization of a human neutrophil lipocalin (HNL) from the secondary granules of human neutrophils. Scand J Clin Lab Invest 54:365–376
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Prato, M., Polimeni, M., Tullio, V. (2015). Human Lysozyme in Malaria Patients: Possible Role as Biomarker for Disease Severity. In: Prato, M. (eds) Human and Mosquito Lysozymes. Springer, Cham. https://doi.org/10.1007/978-3-319-09432-8_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-09432-8_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-09431-1
Online ISBN: 978-3-319-09432-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)