Abstract
Anxiety is a prominent associated feature in autism spectrum disorder (ASD); however, determining the presence of anxiety in this population can be especially challenging for several reasons. Overlapping features between anxiety and ASD (e.g., social avoidance and repetitive and compulsive-like behavior) can make it difficult to determine if these behaviors are due to anxiety or a component of the autism. In addition, persons with ASD have limited communication skills and social impairments that limit self-report; and are at increased risk for engaging in problem behavior (e.g., aggression, self-injury, and property destruction)—some of which is known to occur to avoid or escape certain situations. Caution should be taken to not assume the presence of anxiety (or dismiss it) based on how the presenting complaint is labeled by care providers (or even by the individual him or herself). Rather, multimodal, multi-informant behavioral assessment should be initiated upon encountering individuals with avoidant and seemingly anxious behavior. Review of the existing literature suggests that many of the behavioral assessment strategies traditionally employed with non-ASD populations are applicable to individuals with ASD. Treatment should be individualized based on the characteristics and functioning level of the individual. The core components of behavioral treatment procedures include graduated exposure and reinforcement, but these are often supplemented with other components. Despite significant gaps in the literature, the existing research is sufficient to guide clinicians on how to proceed with assessment and treatment of anxiety in individuals with ASD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Anxiety has been described as a constellation of responses to a potential threat that includes behaviors from multiple response domains—specifically, behavioral, physiological, verbal/cognitive, and subjective (Davis and Ollendick 2005). In contrast to adaptive anxiety, where a potentially harmful stimulus is avoided, an anxiety disorder is said to exist when the avoided stimulus poses little actual risk, or when the avoidance generalizes to a broader class of stimuli to the extent that the individual’s functioning is impaired. Traditional two-factor learning models of anxiety posit that anxiety disorders are established and maintained though a conditioning process involving Pavlovian and operant conditioning (Mowrer 1960). This process involves the pairing of a neutral stimulus with an aversive event (via Pavlovian conditioning); and then escape and avoidance of the conditioned aversive stimulus is maintained through negative reinforcement. Among higher functioning individuals, conditioning or associations between aversive events and neutral stimuli do not need be directly experienced but may emerge via transfer of function (Friman et al. 1998) or higher-order conditioning. The extent to which the individual’s functioning is impaired due to avoidance depends on several factors, including how ubiquitous the avoided stimulus is in everyday life, the negative consequences or “costs” of avoiding it, and subjective distress associated with the experience (though this latter factor may not be difficult to determine in some individuals).
Special Considerations for ASD
Autism spectrum disorder (ASD) represents a heterogeneous diagnostic category in terms of intellectual functioning , communication skills, repetitive behavior , and psychiatric comorbidities (Myers and Johnson 2007). Limited communication skills and social impairments commonly present in ASD limit the extent to which the individual can self-report thoughts, affective states, and physiological sensations—making it more challenging to identify the subjective experiences of fear and anxiety. Therefore, it is important to have a working definition of anxiety that is applicable across the ASD continuum. We define anxiety here as a constellation of responses (including avoidant behavior, facial expressions indicative of fear and distress, and increased physiological arousal) that are occasioned by stimuli that signal potential punishment, and maintained by escape or avoidance of those stimuli. For persons with ASD who are able to verbally describe internal events (thoughts, feelings, physiological responses), these would be self-characterized as being aversive themselves and self-labeled using terms such as fear, anxiety, panic, etc.
Another challenge to determining the presence of anxiety in a person with ASD arises from the fact that anxiety and ASD share some common features, making it difficult to determine if behaviors typically thought of as symptomatic of anxiety (e.g., avoidance of certain situations) are actually secondary to ASD itself or indicative of the presence of anxiety (see Chaps. 7,8,9, and 10 for a detailed discussion of these issues). For example, avoidance of social interaction and other specific situations are the primary features of certain anxiety disorders (e.g., social phobia and specific phobia)—yet these behaviors are commonly seen in many individuals with ASD, including those who are not suspected of being anxious (Kuusikko et al. 2008). Similarly, repetitive and ritualistic behaviors that are the hallmarks of obsessive–compulsive disorder (OCD) are also commonly observed in many persons with ASD (McDougle et al. 1995; Zandt et al. 2007)—including those individuals that are not suspected of being anxious.
Another issue that complicates the assessment of anxiety in persons with ASD is that individuals with ASD are at increased risk for engaging in problem behavior (e.g., aggression, self-injury, and property destruction)—often to avoid or escape situations. This occurs in approximately 25 % of cases (Hagopian et al. 2013; Hanley et al. 2003), and can be associated with emotional distress—which can raise questions about whether anxiety may be present. Determining whether this is indicative of anxiety or simply the avoidance of nonpreferred or mildly aversive situations, such as academic tasks, can sometimes be challenging. We use the term simple avoidance to refer to avoidance of nonpreferred stimuli or situations (e.g., wearing shoes, participating in certain instructional tasks) that is not associated with seemingly anxious or fearful behavior—based on observation of facial expressions, affect, and physiological arousal traditionally associated with anxiety (and the absence of self-report indicative of anxiety in those who are able to communicate this). In contrast, we use the term anxious avoidance to refer to avoidant behavior that is associated with traditional indicators of anxiety (including facial expressions indicative of fear, increased physiological arousal, and self-reported anxiety in those who are able to report). Thus, the distinction between these two types of avoidant behavior is based on the presence or absence of some indicator of emotional distress and subjective states characteristic of anxiety. When anxious avoidance markedly interferes with functioning, then this would constitute an anxiety disorder (which particular diagnosis obviously depends on the nature of the feared stimulus and the response). This most often occurs when the avoided stimulus is encountered frequently (e.g., riding in a car, going into a restroom), and/or when avoidance comes at a high cost (e.g., avoiding examinations by a physician, getting a medically indicated injection). Thus, we argue that not all avoidant behavior in ASD is associated with anxiety, and not all anxiety in ASD would constitute an anxiety disorder per se.
Behavioral Assessment
The overarching goal of behavioral assessment is to formulate hypotheses regarding the controlling antecedent and consequent variables. Obviously, this must be done within the broader social and developmental context. The issues previously noted suggest one must consider the following: (1) social avoidance and ritualistic behaviors indicative of anxiety disorders in typically developing persons are routinely observed in ASD, including among those not suspected of being anxious; and (2) individuals with ASD (and intellectual disabilities; ID) often engage in avoidant behavior that may not necessarily be associated with anxiety. Another consideration is that both children and adults with ASD are more dependent on care providers (Shattuck et al. 2012) than typically developing peers—so behavioral assessment must include an analysis of the interactions between the individual with ASD and care providers .
In light of the unique challenges to the assessment of anxiety in ASD, the clinician’s first goal upon encountering a person with ASD referred for treatment of possible anxiety should be to ascertain whether the presenting problems are indeed due to anxiety (i.e., anxious avoidance), or represent simple avoidance. Caution should be taken to not assume the presence of anxiety (or dismiss it) based on how the presenting complaint is labeled by care providers (or even by the individual himself or herself). Rather, multimodal, multi-informant behavioral assessment should be initiated to determine this. Multimodal assessment includes a range of assessment modalities, including direct observation of behavior, observation of affect, and measurement of physiological responding, as well as self-reported cognitions and affective states. (King et al. 1997; MacNeil et al. 2009; Velting et al. 2004)
For individuals with ASD (or other developmental disorders), one must also consider this information in the context of the individual’s skills and skills deficits related to ASD (as well as the level of intellectual functioning) . In the case of ASD in particular, core skills deficits may contribute to the development of both simple avoidance and anxious avoidance. For example, communication deficits that limit one’s ability to ask for assistance with work or to request a break from work can lead to the establishment of escape-maintained problem behavior (i.e., simple avoidance). Deficits in social skills may result in embarrassing social interactions for higher functioning individuals with ASD, which then may result in social anxiety (White et al. 2010; see Chap. 9). Sensory stimulation may be experienced differently by people who have ASD, to the extent that stimuli that would be neutral or benign to most individuals (e.g., certain noises, the touch of water) appear to be highly aversive to some with ASD .
For many parents, observing one’s child in an anxious or upset state is often unpleasant and anxiety inducing itself. A parent reacting to an anxious child in a way that reduces child anxiety (e.g., by permitting the child to avoid the feared situation) may also reduce the parent’s anxiety and thus reinforce those parent behaviors that inadvertently reinforced the child’s avoidant behavior—resulting in a maladaptive self-sustaining parent–child interaction. Although avoidant behavior is, by definition, maintained by negative reinforcement, behavioral assessment must also attempt to determine what, if any, other reinforcing consequences may be obtained . Understanding these parent–child interactions is important for understanding the broader context in which anxiety occurs, and has important implications for designing treatment in a way that will increase the probability of parental adherence to recommendations. That is, it might be necessary to include treatment components aimed at minimizing and managing parental anxiety during the child’s treatment in cases where a parent has a very low tolerance for his/her child becoming anxious. An understanding of the antecedents, behavioral skills and deficits, and controlling consequences—including interactions with care providers—is important not only for guiding the development of an individualized treatment plan but also for adherence to recommendations (Reaven & Hepburn 2006). Behavioral assessment methods described below include screening and diagnostic instruments, behavioral interviews, direct observation of behavior, and physiological measures .
Behavioral Interviews
Interviews should be conducted with individuals with ASD to the extent possible with consideration of the individual’s cognitive and language capabilities (Blakeley-Smith et al. 2012). For some individuals with ASD, cognitive and communication deficits and difficulties identifying emotions may make the assessment of cognitions, and affective and physiological states through self-report very challenging, and in some cases not possible at all (Baron-Cohen 2002; Ollendick et al. 1993). Consequently, when assessing possible anxiety in ASD, interviews may rely mostly, or completely, on the report of other informants (typically, parents and other care providers). Information should be gathered on the nature of the anxiety response, collateral behaviors (including other problem behaviors such as aggression and self-injury), the relevant antecedents that occasion anxiety, as well as the consequences the behavior produces. Information provided by respondents regarding the individual’s affective states can help determine whether the behavior of concern is simple avoidance or anxious avoidance .
When interviewing care providers, it is important to distinguish between the respondent’s observation of events versus his or her interpretation of what the individual with ASD may be experiencing and why. In light of limited communication skills and overlapping features of ASD and anxiety, care providers are subject to the same challenges as clinicians in making attributions about behavior. For example, a parent may characterize a child as having “OCD” based on observations of repetitive, ritualistic behavior. While care providers’ own hypotheses about the individual’s anxiety may be useful, the clinician must also gather descriptive information and form his or her own hypotheses. In particular, it is important to identify what situations or stimuli the child avoids, elicit escape, and occasion negative emotional states suggesting anxiety (e.g., fearful facial expressions, crying, shaking, and panic-like states). For individuals who are unable to verbally express fear or a desire to avoid a situation, avoidance sometimes occurs in the form of dropping or running off, and may co-occur with problem behavior such as aggression, property destruction, and self-injury—particularly when initial attempts to avoid or escape are ineffective (Hagopian et al. 2001; Ricciardi et al. 2006). Although avoidant and escape responses are generally maintained by negative reinforcement, it is important to also determine how care providers respond. Reactions on the part of care providers, including attention (in the form of consoling the individual or talking about his/her anxiety), as well as providing access to preferred activities, can further reinforce these behaviors. Thus, in some cases, avoidant behaviors may be maintained by negative reinforcement in the form of escape/avoidance of the feared stimulus and by positive reinforcement in the form of attention or access preferred activities. The interview can also provide information about how the individual’s anxiety affects the care provider and how he/she might respond .
Screening and Diagnostic Instruments
In general, screening and diagnostic instruments can be important tools to use in order to assess whether the individual meets formal diagnostic criteria for an anxiety disorder. However, there are multiple issues to consider when using these measures with individuals with ASD as well as limited guidance from the literature to date (White and Roberson-Nay 2009). Currently, there are two categories of instruments available for the assessment of anxiety in individuals with ASD. These include (1) instruments designed to assess a broad range of psychopathology, including anxiety disorders, in individuals with ASD and (2) instruments originally designed to assess anxiety in typically developing individuals, which have been extended to individuals with ASD.
Instruments Designed to Assess a Broad Spectrum of Psychopathology in Individuals with ASD
There are only a few instruments that have been developed specifically for the ASD population. These involve both semi-structured interviews and rating scales. All of these instruments are in their infancy and require additional study of their psychometric properties.
The Autism Comorbidity Interview—Present and Lifetime Version (ACI-PL; Leyfer et al. 2006) is a semi-structured diagnostic interview based on the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS; Ambrosini 2000). It was modified to make it appropriate for use with individuals having ASD; and has been designed to distinguish whether impairment is due to a comorbid psychiatric disorder or due to the core features of ASD. Some of the modifications include questions to establish the child’s emotions and behaviors at his/her best in order to obtain a baseline, as well as additional screening questions about common observable features and presenting concerns of parents of children with ASD to determine whether the potential comorbid disorder is applicable. Thus far, the ACI-PL has been found to be reliable and valid only for certain psychiatric disorders, with OCD as the only anxiety disorder (Leyfer et al. 2006). However, in relation to other commonly used scales to assess for psychiatric comorbities in ASD, the ACI-PL yielded the fewest false positives (Mazefsky et al. 2011).
The Autism Spectrum Disorders—Comorbidity for Children (ASD-CC; Matson and Wilkins 2008) and the Baby and Infant Screen for Children with Autism Traits (BISCUIT—Part 2; Matson et al. 2009b) are informant-based rating scales used to examine comorbid psychopathology, including anxiety in children with ASD. Both scales were designed to be part of a comprehensive assessment battery for diagnosing ASD, comorbid psychopathology, and challenging behavior in children and adolescents. Parents or other caregivers are asked to endorse items on a 3-point Likert scale. The ASD-CC was designed for children with ASD aged 3–17, and the BISCUIT was designed for toddlers with ASD aged 17–37 months. Factor analyses of each scale have yielded factors specifically related to anxiety and avoidance behaviors (Matson et al. 2009a; Matson et al. 2011). Both scales have good reliability (Matson and Wilkins 2008; Matson et al. 2009b) and the ASD-CC has good validity (Matson et al. 2009a).
Instruments Designed for Typically Developing Children and Extended to Individuals with ASD
There are several well-established instruments developed to assess anxiety in typically developing children. Although many of these instruments have been extended to individuals with ASD, few have been tested for reliability or validity in this population. One possible limitation in using these instruments is the presence of overlapping symptoms between ASD and anxiety disorders. A couple of studies have looked at whether a clinical diagnosis of an anxiety disorder can be identified after eliminating the items targeted the overlapping symptoms or making other modifications (e.g., Kuusikko et al. 2008; Sukhodolsky et al. 2008) and have yielded improved validity. However, this research is still in its infancy and great caution still needs to be taken when using these tools (Davis 2012). Further, as with typically developing children, they should never be used in isolation to make a diagnosis of an anxiety disorder.
The most common instruments in this category involve semi-structured interviews, self-report measures, and informant-based rating scales. The Anxiety Disorders Interview Schedule Child and Parent Version (ADIS-C/P; Silverman and Albano 1996) is a commonly utilized semi-structured interview based on DSM-IV (APA 2000) criteria. Its reliability and validity are well established with typically developing children (Silverman et al. 2001; Wood et al. 2002) but not with children with ASD. Aside from this interview, there are many rating scales available for the assessment of anxiety in typically developing children, but the ones most widely adapted to this population include the Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds and Richmond 1985), the Multidimensional Anxiety Scale for Children (MASC; March 1997), the Spence Children’s Anxiety Scale (SCAS; Spence 1997), and the Screen for Child Anxiety and Related Emotional Disorders (SCARED; Birmaher et al. 1999). The latter three scales also have parent versions available.
Although the self-report versions of these scales generally have good psychometric properties for typically developing children (Silverman and Ollendick 2005), they should be used with caution with individuals with ASD who have cognitive challenges (White and Roberson-Nay 2009), as well as difficulties with emotion recognition (Baron-Cohen 2002). Very little research has been conducted on the accuracy of self-report in this population and the research that does exist has mixed results (Farrugia and Hudson 2006; Russell and Sofronoff 2005). A recent study suggested that there may be better agreement between child and parent report on some anxiety symptoms in more verbal individuals with ASD (Blakeley-Smith et al. 2012). However, questions still remain about agreement between parent and child report about anxiety symptoms, as well as whose report is the most accurate (Davis 2012). Until more research has been conducted to determine the validity of self-report in individuals with ASD, caution should be exercised (Mazefsky et al. 2011). Nevertheless, since these instruments are designed to obtain self-report of subjective states, the information they provide could help distinguish between simple and anxious avoidance.
Direct Observation of Behavior
Though more effortful and time consuming than other methods of assessment, direct observation of the apparently anxious or avoidant behavior is essential. Findings from the interviews with the individual and care providers and from self- and other-report measures will help one determine the appropriate methods for conducting direct observation. Once the stimuli that occasion avoidant behavior have been identified, it will be necessary to distinguish between those that can be presented in a controlled manner from those that cannot. For example, some studies have described cases in which anxiety was elicited by specific stimuli such as water, needles, or dental care (Conyers et al. 2004; Rapp et al. 2005; Shabani and Fisher 2006) . Certain anxiety disorders, such as specific phobias , social phobia , and separation anxiety disorder, and OCD are characterized by anxiety that is elicited by a specific stimulus or classes of stimuli (APA 2013). In these cases, presentation of the avoided stimulus in a controlled fashion may be possible. In other cases, however, the stimuli that occasion avoidance may be difficult to identify or control. For example, individuals with generalized anxiety disorder may not be able to identify specific stimuli that reliably elicit fear. Some stimuli may be identifiable but difficult to present and terminate with the level of control required in treatment—such as the behavior of peers and certain internal stimuli (e.g., physiological sensations). Another consideration, which may be more relevant for higher functioning individuals with ASD, is whether the individual may be reactive to contrived presentation conditions .
Behavioral Monitoring
In cases where the avoided stimulus cannot be readily presented in a controlled manner (or in cases where the individual may behave differently when being observed), enlisting care providers to conduct behavioral monitoring in the natural setting can be highly effective. In contrast to self- and other-report measures, which involve standard questions and the retrospective reporting of behavioral patterns or tendencies, behavioral monitoring involves the observation and recording of behaviors targeted for that particular individual—ideally, in real time. For example, behavioral monitoring may involve a care provider recording each time the individual engages in an avoidant or apparently anxious behavior that has been operationally defined a priori (e.g., dropping to the floor and crying) . The monitoring form would allow the care provider to record observable antecedents and consequences for this behavior; describe the behavior itself; provide some rating of the apparent level of distress based on observable indices of affect such as crying, trembling, or facial expressions (which is important to determining the presence of anxious avoidance); and record the date and time of the event. In addition to helping to identify antecedents and consequences during the assessment phase, data obtained using behavioral monitoring during the assessment phase can be used to establish a pretreatment baseline for the purpose of evaluate treatment outcomes. Parental monitoring of anxiety in children without ASD has been reported in several studies (Chorpita et al. 1996; Hagopian and Slifer 1993; Hagopian et al. 1990). Although all of these examples involved children without ASD, a similar type of monitoring can also be used with children with ASD, and in cases where the avoided stimulus cannot be readily controlled (or the individual may be reactive to contrived in-clinic sessions) may be the only source of direct behavioral observation data .
Behavioral Avoidance Test
In cases where the avoided stimulus is identifiable and can be presented in a controlled fashion (e.g., insects), it may be possible to arrange conditions to directly observe the response in vivo. This could involve creating a behavioral avoidance test (BAT; Dadds et al. 1994) which is a highly structured method of assessing avoidant behavior associated with the avoided stimulus. Generally, this procedure involves progressively exposing the individual to the stimulus along some dimension (e.g., physical distance between person and stimulus, time person can remain near the stimulus), and recording the point at which the avoidant response is displayed, and/or anxiety is reported. BATs can be highly individualized based on the specific stimuli that elicit avoidance in the person being observed. In addition to the benefit of observing the individual’s responses (including avoidance/escape, facial expressions, physiological arousal, and self-report that would suggest anxious avoidance) directly and in a controlled manner, one can use the same method of stimulus presentation during graduated exposure treatment (see the following section on treatment). For individuals with ASD who are unable to self-report, some form of BAT is essential during assessment and in treatment evaluation. Many of the available clinical case studies that report on the assessment and treatment of anxiety in this population describe the use of a BAT (Davis et al. 2007; Erfanian and Miltenberger 1990; Matson 1981) .
Assessment of Skills and Skills Deficits
In light of the social impairments that define ASD, assessment of social skills and skills deficits must be undertaken when anxiety related to social interactions is suspected. As previously noted, relative to their more intellectually disabled peers, higher functioning individuals with ASD may be more aware of skills deficits and more sensitive to embarrassing social interactions. This can establish social interaction as a conditioned aversive stimulus that induces anxiety, which in turn, can further impair social performance (White et al. 2010). The reader is referred to Chap. 9 for a more detailed discussion-related assessment and treatment of social skills deficits concurrently with social anxiety. In addition to addressing social skills deficits, it is also important to consider other adaptive skills deficits when assessing and treating anxiety in persons with ASD. This includes communication deficits, leisure skills deficits, the presence of restricted and stereotyped patterns of behavior, stimulus overselectivity, and deficits in varying behavior in the context of changing situations—all of which are commonly observed in ASD. Indeed, deficits in adaptive behavior and the severity of autism have been shown to be correlated with the presence of problem behavior such as aggression and self-injury (McClintock et al. 2003). Although those findings are correlational, it is possible that deficits in adaptive behavior may establish otherwise neutral or simply nonpreferred situations as aversive to the extent that they can lead to the emergence of escape-maintained problem behavior (i.e., simple avoidance). In some cases, this same process could lead to the emergence of anxious avoidance and ultimately an anxiety disorder. As noted at the outset, understanding the broader context of the individual’s skills and skills deficits is important to developing a treatment that addresses both the presenting problem and the deficits that may have predisposed its emergence .
Physiological Measures
The use of psychophysiological measurement for the assessment of anxiety is commonly recommended by researchers (King et al. 1997; Silverman and Lopez 2004) but rarely used in practice. The studies (Chok et al. 2010; Jennett et al. 2011) that have included physiological measures for assessment of anxiety in individuals with ASD have provided some support for the feasibility and utility of using heart rate monitors with this population. However, knowledge is still limited with regard to the selection of measures, appropriate conditions under which to measure physiological responding, and the validity of this measure (Turpin 1991). Moreover, for some individuals with ASD, physiological measurement may be even more challenging because they may have difficulty tolerating the equipment and procedures. Despite these limitations, the potential use of physiological measures should continue to be explored as these could provide additional information regarding the situations that cause increased arousal in individuals with ASD, especially for those individuals who are unable to reliably verbalize or report on internal sensations not readily observable. In combination with more subjective sources of data suggesting distress, the objective measurement of increased physiological arousal associated with exposure to the avoided stimulus would make a more compelling case in favor of anxious avoidance over simple avoidance.
Behavioral Treatment
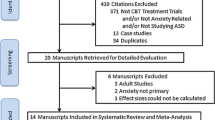
Although the literature on the treatment of anxiety in persons with ASD is quite limited, the available findings suggest that behavioral treatments demonstrated to be effective with other populations appear applicable to persons with ASD—though with some modifications (it should be noted that the focus of the current chapter is on behavioral treatment for anxiety in ASD; cognitive-behavioral treatment (CBT) , which has been utilized for a wide variety of anxiety diagnoses for higher functioning individuals with ASD, is discussed in detail in Chap. 12 see also Reaven & Hepburn 2006). Behavioral interventions used for treatment of escape-maintained problem behavior that could be described as simple avoidance provide indirect support for these types of interventions. A review by Jennett and Hagopian (2008) identified behavioral treatment as an evidence-based treatment for “phobic avoidance” in individuals with ID. The term phobic avoidance was used in that review because few studies reported on formal diagnoses (only Ricciardi et al. 2006 reported a diagnosis of Specific Phobia), but did report avoidant behavior of a particular stimulus that was associated with phobic-like emotional responses (characteristic of specific phobia). The authors identified 38 studies published over a 35-year period which included case reports, single-case experimental designs, and a few uncontrolled group studies. Among the studies were 12 well-designed, single-case, experimental studies. Four of these studies included five participants who were reported to have an ASD diagnosis, and ranged from having mild to profound ID (Love et al. 1990; Rapp et al. 2005; Ricciardi et al. 2006; Shabani and Fisher 2006). The main components of behavioral treatment for anxiety included graduated exposure and reinforcement for approach behavior. The review revealed that behavioral treatment, involving the use of graduated exposure and reinforcement, has been sufficiently researched to characterize this class of interventions as a “well-established” evidence-based treatment for individuals with ID based on APA Division 12 and 16 criteria for empirically supported treatments (Chambless and Hollon 1998; Chambless et al. 1998; Krotochwill and Stoiber 2002). Since this chapter, an additional two high-quality studies have been published that used single-case experimental studies to evaluate treatments for avoidance of a particular stimulus (i.e., “phobic avoidance”) in individuals with ASD (Chok et al. 2010; Schmidt et al. 2013; only Chok et al. 2010 reported a diagnosis of Specific Phobia). To date, there are a total of six studies utilizing good single-case design and showing an effect of graduated exposure plus reinforcement in individuals with ASD (see Table 11.1). Thus, this treatment can also be characterized as a “probably efficacious” treatment for individuals with autism according to the same guidelines.
Graduated Exposure
Graduated exposure is most appropriate for anxiety disorders in which there is an identifiable and controllable stimulus that is avoided (and therefore is most applicable to disorders such as specific phobia, social phobia, and OCD) . Graduated exposure involves presenting the avoided stimulus in progressively more intense forms along one or more physical dimensions—such as size, proximity, mode of presentation (pictorial to actual); ideally, while maintaining low levels of anxiety. This technique aims to extinguish any associations between the avoided stimulus and aversive events (such as intense physiological arousal) by presenting the avoided stimulus in the absence of those aversive events (i.e., Pavlovian extinction); and to extinguish negative reinforcement associated with escape or avoidance (i.e., operant extinction). For exposure to be therapeutic, it is critical that the avoided stimulus is not paired with any aversive events (including extreme anxiety), and that encountering the stimulus not result in anxious escape/avoidance from the stimulus in a manner that could strengthen avoidance and produce counter-therapeutic effects. The intensity of exposure is arranged in a graduated fashion to maximize the likelihood that the participant will not become too anxious and eventually habituate to the stimulus.
For individuals with ASD who may not be able to generate a hierarchy of stimuli based on verbal report, the hierarchy may be developed based on interviews with care providers, or the results of a BAT. It is advisable to consider a range of stimulus variations by altering the avoided stimulus along a physical dimension, such as its distance from the individual, the duration of contact, or size of the stimulus. Regardless of how the hierarchy is developed, graduated exposure involves systematically exposing the participant to variations of the avoided stimulus that progress to closer approximations of the actual stimulus. Progression along the hierarchy is based on the participant successfully completing the previous step, ideally with minimal anxiety. Based on the participant’s progress, the hierarchy can be changed by including intermediate stimulus variations.
Supplementing Graduated Exposure
Obviously, the primary maintaining consequence for anxious avoidance is negative reinforcement in the form or either avoidance or escape from the feared situation. Therefore, it is important to impose reinforcement procedures targeting approach responses that are strong enough to counter or compete with the negative reinforcement produced by escape or avoidance. Although typically developing individuals may be able to identify and verbalize powerful reinforcers, for lower functioning individuals with ASD, a systematic preference assessment to identify potential reinforces should be conducted to identify preferred items that may potentially serve as reinforcers (see Hagopian et al. 2004 for a comprehensive summary of preference assessment procedures for individuals with ASD and other developmental disabilities).
For nonverbal individuals who might not understand instructions, it may be necessary to program learning trials without using the avoided stimulus to establish compliance with the general procedures. That is, one could initiate exposure sessions using a neutral stimulus (instead of the feared stimulus) for the purpose of ensuring the individual contacts the programmed reinforcement contingencies for cooperation. For lower functioning individuals, numerous simulated exposure sessions may be necessary before initiating graduated exposure. For individuals who can understand verbal instructions, however, much time can be saved through informing the individual about the procedures, including the contingencies for approach behavior and appropriate ways to request termination of exposure.
Other Treatment Components
Prompting may be needed to assist the individual to comply with the steps of the exposure hierarchy and come into contact with the reinforcement contingencies in place; however, caution should be taken to not “force” compliance. This may be especially important when the individual appears to exhibiting signs of distress. For individuals who can understand verbal prompts, it may be helpful to prompt the individual how to approach the avoided stimulus—and how to appropriately request pausing at the current hierarchy step (Runyan et al. 1985). Modeling approach behavior and reinforcement consumption may facilitate learning the contingencies, and demonstrate successful approach behaviors (Erfanian and Miltertenberger 1990; Love et al. 1990). Video modeling may be appropriate for some individuals with ASD who prefer watching videos to observing live models. Response prevention is another component that has been reported (Rapp et al. 2005), but most studies published to date that describe the behavioral treatment of anxiety in individuals with ASD do not include response prevention or escape extinction. Finally, use of distracting stimuli, particularly free access to preferred activities and reinforcers may be used in conjunction with graduated exposure and contingent reinforcement (Luscre and Center 1996). The use of distracting stimuli might be helpful for several possible reasons including to help focus attention away from the feared stimulus, to increase the overall level of reinforcement in the context of exposure, and to pair otherwise anxiety-provoking exposure with a preferred stimulus. However, some caution should also be taken when providing free access to reinforcers, especially when using contingent reinforcement, because this has the potential to weaken programmed reinforcement for successful approach behavior. The combination of the specific treatment components listed above can be highly individualized based on the functioning level and needs of the individual. For higher functioning individuals, cognitive-behavioral treatment components may be used as well (see Chap. 12).
Caregiver Involvement
For individuals with ASD who are often supported by care providers (e.g., parents, aides), their involvement in treatment is essential. The more the individual is dependent on care providers, the more the care provider can support or degrade behavioral treatment. As noted previously, parent–child interactions can establish and maintain both simple and anxious avoidance. Therefore, it is essential to include an analysis of parent–child interactions that may reinforce anxiety and avoidant behavior, as well as evaluate parental anxiety. When developing interventions, one should provide parents with information regarding the nature of anxiety, how their interactions may inadvertently reinforce anxious and avoidant behavior, and how behavioral treatment will progress in a graduated fashion for the purpose of extinguishing avoidant behaviors. In many cases, it will be important to have parents conduct exposure exercises outside of therapy sessions to enhance generalization of the skills learned in session.
Skills Training
Skills training involves a focus on deficits specific to children with ASD that may impact the efficacy of treatment. Skills training is an explicit part of some CBT treatment packages (e.g., White et al. 2010; White and Roberson-Nay 2009; Wood et al. 2009), but it can also be an important component of behavioral treatment. For example, White and Roberson-Nay (2009) and White et al. (2010) have hypothesized that social deficits in individuals with high functioning autism (HFA) may contribute to the promotion of social anxiety in this population. Adolescents with HFA may develop and maintain social anxiety because of their awareness of their own social difficulties. As a result, they may avoid social situations, and therefore, have few opportunities to practice appropriate social skills. Thus, White and her colleagues have developed a comprehensive treatment package that contains the components described above plus the use of social skills training through the use of modeling, feedback, and reinforcement. Targeted social skills may include initiating interaction with peers, conversational skills, flexibility, recognizing the cues of others, and handling rejection. In another example, Wood et al. (2009), have included skills training on areas such as self-help skills and increasing interest in areas as an adjunct to the traditional components of treatment. These researchers hypothesize that skill deficits in such areas may make the completion of graduated exposure exercises more difficult and lead to diminished efficacy of treatment. White and Roberson-Nay (2009), White et al. (2010) and Wood et al. (2009) have shown promising results with their treatment packages for children with HFA. Although skills training has not been included as a primary component of the behavior treatment packages described in this chapter, there are decades of research showing that behavioral treatments are effective for skills training across all functioning levels on the autism spectrum (e.g., Carr and Durand 1985; Horner and Keilitz 1975; Lovaas 1987). Thus, the addition of skills training, such as functional communication training, social skills training, and self-help skills, should be considered as an adjunctive behavioral treatment whenever necessary.
Conclusions
Anxiety is a prominent associated feature in ASD; however, determining the presence of anxiety in this population can be especially challenging for several reasons. Overlapping features between anxiety and ASD (e.g., social avoidance and repetitive, seemly compulsive behavior) can make it difficult to determine if seemly anxious and avoidant behaviors are due to anxiety or a component of the autism . In addition, limited communication skills and social impairments common to ASD may limit the extent to which the individual can self-report, making it more challenging to identify the subjective experiences of fear and anxiety. Another issue that complicates the assessment of anxiety in persons with ASD is that these individuals are at increased risk for engaging in problem behavior (e.g., aggression, self-injury, and property destruction), some of which occurs to avoid or escape certain situations. We use the term simple avoidance to refer to avoidance of nonpreferred stimuli or situations (e.g., wearing shoes, participating in certain instructional tasks), and the term anxious avoidance to refer to avoidant behavior that is associated with traditional indicators of anxiety (including facial expressions indicative of fear, increased physiological arousal, and self-reported anxiety in those who are able). When the anxious avoidance markedly interferes with functioning, then this would constitute an anxiety disorder (which particular disorder obviously depends on the nature of the feared stimulus and the response). Caution should be taken to not assume the presence of anxiety (or dismiss it) based on how the presenting complaint is labeled by care providers (or even by the individual him or herself). Rather, multimodal, multi-informant behavioral assessment should be initiated.
Review of the existing literature suggests that many of the behavioral assessment strategies traditionally employed with non-ASD populations may be applicable to individuals with ASD, despite the communication deficits that may limit or prevent self-report. Interviews and direct behavioral observation via behavioral avoidance tests and behavioral monitoring in natural settings may be the primary sources of information during both the assessment and treatment evaluation phases. Treatment should be individualized based on the characteristics and functioning level of the individual. The core components of behavioral treatment procedures include graduated exposure and reinforcement, but these are often supplemented with other components. Despite significant gaps in the literature, research conducted thus far is sufficient to guide clinicians on how to proceed clinically with assessment and treatment of anxiety in individuals with ASD. Nevertheless, additional research designed to examine the presence of other types of anxiety disorders, to develop additional assessment strategies, and to further examine treatment efficacy for anxiety in individuals with ASD is needed.
References
American Psychiatric Association. (2000).Diagnostic and statistical manual of mental disorders (4th ed.). Washington, D.C.: Author.
American Psychiatric Association. (2013).Diagnostic and statistical manual of mental disorders (5th ed.). Washington, D.C.: Author.
Ambrosini, P. J. (2000). Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS).Journal of the American Academy of Child and Adolescent Psychiatry, 39, 49–58.
Baron-Cohen, S. (2002). The extreme male brain theory of autism.Trends in Cognitive Sciences, 6, 248–254,
Birmaher, B., Brent, D. A., Chiappetta, L., Bridge, J., Monga, S, & Baugher, M. (1999). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study.Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1230–1236.
Blakeley-Smith, A., Reaven, J., Ridge, K., & Hepburn, S. (2012). Parent-child agreement of anxiety symptoms in youth with autism spectrum disorders.Research in Autism Spectrum Disorders, 6(2), 707–716.
Carr, E. G., & Durand, V. M. (1985). Reducing behavior problems through functional communication training.Journal of Applied Behavior Analysis, 18, 111–126.
Chambless, D. L., & Hollon, S. D. (1998). Defining empirically supported therapies.Journal of Consulting and Clinical Psychology, 66, 7–18.
Chambless, D. L., Baker, M. J., Baucom, D. H., Beutler, L. E., Calhoun, K. S., Crits-Christoph, P., et al. (1998). Update on empirically validated therapies, II.The Clinical Psychologist, 51, 3–16.
Chok, J. T., Demanche, J., Kennedy, A., & Studer, L. (2010). Utilizing physiological measures to facilitate phobia treatment with individuals with autism and intellectual disability: A case study.Behavioral Interventions, 11, 325–337.
Chorpita, B. F., Albano, A. M., Heimberg, R. G., & Barlow, D. H. (1996). A systematic replication of the prescriptive treatment of school refusal behavior in a single subject.Journal of Behavior Therapy and Experimental Psychiatry, 27, 281–290.
Conyers, C., Miltenberger, R. G., Peterson, B., Gubin, A., Jurgens, M., Selders, A., et al. (2004). An evaluation of in vivo desensitization and video modeling to increase compliance with dental procedures in persons with mental retardation.Journal of Applied Behavior Analysis, 37, 233–238.
Dadds, M., Rapee, R., & Barrett, P. (1994). Behavioral Observation. In T. Ollendick, N. King, & W. Yule (Eds.),International handbook of phobic and anxiety disorders in children and adolescents (pp. 349–364). New York: Plenum.
Davis III, T. E. (2012). Where to from here for ASD and anxiety? Lessons learned from child anxiety and the issue of DSM-5.Clinical Psychology: Science and Practice, 19, 358–363. doi:10.1111/cpsp.12014.
Davis, T. E., & Ollendick, T. H. (2005). Empirically supported treatments for specific phobia in children: Do efficacious treatments address the components of a phobic response?Clinical Psychology: Science and Practice, 12, 144–160.
Davis III, T. E., Kurtz, P., Gardner, A., & Carman, N. (2007). Cognitive-behavioral treatment for specific phobias with a child demonstrating severe problem behavior and developmental delays.Research in Developmental Disabilities, 28, 546–558. doi:10.1016/j.ridd.2006.07.003.
Erfanian, N., & Miltenberger, R. G. (1990). Contact desensitization in the treatment of dog phobias in persons who have mental retardation.Behavioral Interventions, 5, 55–60.
Farrugia, S., & Hudson, J. (2006). Anxiety in adolescents with Asperger Syndrome: Negative thoughts, behavioral problems, and life interference.Focus on Autism and Other Developmental Disabilities, 21, 25–35.
Friman, P. C., Hayes, S. C., & Wilson, K. G. (1998). Why behavior analysts should study emotion: The example for anxiety.Journal of Applied Behavior Analysis, 31, 137–156.
Hagopian, L. P., & Slifer, K. J. (1993). Treatment of separation anxiety disorder with graduated exposure and reinforcement targeting school attendance: A controlled case study.Journal of Anxiety Disorders, 7, 271–280.
Hagopian, L. P., Weist, M. D., & Ollendick, T. H. (1990). Cognitive-behavior therapy with an 11- year-old girl fearful of AIDS infection, other diseases, and poisoning: A case study.Journal of Anxiety Disorders, 4, 257–265.
Hagopian, L. P., Crockett, J. L., & Keeney, K. M. (2001). Multicomponent treatment for blood- injury-injection phobia in a young man with mental retardation.Research in Developmental Disabilities, 22, 141–149.
Hagopian, L. P., Long, E. S., & Rush, K. S. (2004). Preference assessment procedures for individuals with developmental disabilities.Behavior Modification, 28, 668–677.
Hagopian, L. P., Rooker, G. W., Jessel, J., & Deleon, I. G. (2013). Initial functional analysis outcomes and modifications in pursuit of differentiation: A summary of 176 inpatient cases.Journal of Applied Behavior Analysis, 46, 88–100.
Hanley, G. P., Iwata, B. A., & McCord, B. E. (2003). Functional analysis of problem behavior: A review.Journal of Applied Behavior Analysis, 36, 147–185.
Horner, R. D., & Keilitz, I. (1975). Training mentally retarded adolescents to brush their teeth.Journal of Applied Behavior Analysis, 8, 301–309.
Jennett, H. K., & Hagopian, L. P. (2008). Identifying empirically supported treatments for phobic avoidance in individuals with intellectual disabilities.Behavior Therapy, 39, 151–161.
Jennett, H., Hagopian, L. P., & Beaulieu, L. (2011). Analysis of heart rate and self-injury with and without restraint in an individual with autism.Research in Autism Spectrum Disorders, 5, 1110–1118.
King, N. J., Ollendick, T. H., & Murphy, G. C. (1997). Assessment of childhood phobias.Clinical Psychology Review, 17, 667–687.
Krotochwill, T. R., & Stoiber, K. C. (2002). Evidence-based interventions in school psychology: conceptual foundations of the procedural and coding manual of division 16 and the society for the study of school psychology task force.School Psychology Quarterly, 17, 341–389.
Kuusikko, S., Pollock-Wurman, R., Jussila, K., Carter, A. S., Mattila, M. L., Ebeling, H., et al. (2008). Social anxiety in high-functioning children and adolescents with Autism and Asperger syndrome.Journal of Autism and Developmental Disorders, 8, 1697–1709.
Leyfer, O. T., Folstein, S. E., Bacalman, S., Davis, N. O., Dinh, E., Morgan, J., et al. (2006). Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders.Journal of Autism and Developmental Disorders, 36, 849–861.
Lovaas, O. I., (1987). Behavioral treatment and normal educational and intellectual functioning in young autistic children.Journal of Consulting and Clinical Psychology, 55, 3–9.
Love, S. R., Matson, J. L., & West, D. (1990). Mothers as effective therapists for autistic children’s phobias.Journal of Applied Behavior Analysis, 23, 379–385.
Luscre, D. M., & Center, D. B. (1996). Procedures for reducing dental fear in children with autism.Journal of Autism and Developmental Disorders, 26, 547–556.
MacNeil, B. M., Lopes, V. A., & Minnes, P. M. (2009). Anxiety in children and adolescents with autism spectrum disorders.Research in Autism Spectrum Disorders, 3, 1–21.
March, J. S. (1997).Multidimensional Anxiety Scale for Children (MASC). Toronto: Multi-Health Systems.
Matson, J. L. (1981). Assessment and treatment of clinical fears in mentally retarded children. Journal of Applied Behavior Analysis, 14, 287–294.
Matson, J., & Wilkins, J. (2008). Reliability of the autism spectrum disorders-comorbid for children (ASD-CC).Journal of Developmental & Physical Disabilities, 20, 327–336.
Matson, J. L., LoVullo, S. V., Rivet, T. T., & Boisjoli, J. A. (2009a). Validity of the autism spectrum disorder-comorbid for children (ASD-CC).Research in Autism Spectrum Disorders, 3, 345–357.
Matson, J. L., Wilkins, J., Sevin, J. A., Knight, C., Boisjoli, J. A., & Sharp, B. (2009b). Reliability and item content of the baby and infant screen for children with autism traits (BISCUIT): Parts 1–3.Research in Autism Spectrum Disorders, 3, 336–344.
Matson, J. L., Boisjoli, J. A., Hess, J. A., & Wilkins, J. (2011). Cormorbid psychopathology factor structure on the baby and infant screen for children with autism traits-Part 2 (BISCUIT-Part 2).Research in Autism Spectrum Disorder, 5, 426–432.
Mazefsky, C. A., Kao, J., & Oswald, D. P. (2011). Preliminary evidence suggesting caution in the use of psychiatric self-report measures with adolescents with high-functioning autism spectrum disorders.Research in Autism Spectrum Disorders, 5, 164–174.
McClintock, K., Hall, S., & Oliver, C. (2003). Risk markers associated with challenging behaviours in people with intellectual disabilities: A meta-analytic study.Journal of Intellectual Disability Research, 47, 405–416.
McDougle, C. J., Kresch, L. E., Goodman, W. K., Naylor, S. T., Volkmar, F. R., Cohen, D. J., & Price, L. H. (1995). A case-controlled study of repetitive thoughts and behavior in adults with autistic disorder and obsessive-compulsive disorder.American Journal of Psychiatry, 152, 772–777.
Mowrer, O. H. (1960).Learning theory and behavior. New York: Wiley.
Myers, S. M., & Johnson, C. P. (2007). American Academy of Pediatrics Council on Children with Disabilities. Management of children with Autism Spectrum Disorders.Pediatrics, 120, 1162–1182.
Ollendick, T. H., Oswald, D. P., & Ollendick, D. G. (1993). Anxiety disorders in mentally retarded persons. In J. L. Matson & R. P. Barrett (Eds.),Psychopathology in the mentally retarded (pp. 41–85). Needham Heights: Allyn & Bacon.
Reaven, J. (2011). The treatment of anxiety symptoms in youth with high-functioning autism spectrum disorders: Developmental considerations for parents.Brain research, 1380, 255–263.
Reaven, J., & Hepburn, S. (2006). The Parent’s Role in the Treatment of Anxiety Symptoms In Children With High-Functioning Autism Spectrum Disorders.Mental Health Aspects of Developmental Disabilities.
Rapp, J. T., Vollmer, T. R., & Hovanetz, A. N. (2005). Evaluation and treatment of swimming pool avoidance exhibited by an adolescent girl with autism. Behavior Therapy, 36, 101–105.
Reynolds, C. R., & Richmond, B. O. (1985).Revised Children’s Manifest Anxiety Scale: RCMAS Manual. Los Angeles: Western Psychological Services.
Ricciardi, J. N., Luiselli, J. K., & Camare, M. (2006). Shaping approach responses as intervention for specific phobia in a child with autism.Journal of Applied Behavior Analysis, 39, 445–448.
Runyan, M. C., Stevens, D. H., & Reeves, R. (1985). Reduction of avoidance behavior of institutionalized mentally retarded adults through contact desensitization.American Journal of Mental Deficiency, 90, 222–225.
Russell, E., & Sofronoff, K. (2005). Anxiety and social worries in children with Asperger syndrome.Australian and New Zealand Journal of Psychiatry, 39, 633–638.
Shabani, D. B., & Fisher, W. W. (2006). Stimulus fading and differential reinforcement for the treatment of needle phobia in a youth with autism.Journal of Applied Behavior Analysis, 39, 449–452.
Schmidt, J. D., Luiselli, J. K., Rue, H., & Whalley, K. (2013). Graduated exposure and positive reinforcement to overcome setting and activity avoidance in an adolescent with autism.Behavior Modification, 37, 128–142.
Shattuck, P. T., Roux, A. M., Hudson, L. E., Taylor, J. L., Maenner, M. J., & Trani, J. F. (2012). Services for adults with an autism spectrum disorder.Canadian Journal of Psychiatry, 57, 284–291.
Silverman, W., & Albano, A. (1996).Anxiety disorders interview schedule for children for DSM-IV: (Child and Parent Versions). San Antonio: Psychological Corporation/Graywind.
Silverman, W., & Lopez, B. (2004). Anxiety disorders. In M. Hersen (Ed.),Psychological assessment in clinical practice: A pragmatic guide (pp. 269–296). New York: Psychology.
Silverman, W. K., & Ollendick, T. H. (2005). Evidence-based assessment of anxiety and its disorders in children and adolescents.Journal of Clinical Child and Adolescent Psychology, 34, 380–411.
Silverman, W. K., Saavedra, L. M., & Pina, A. A. (2001). Test-retest reliability of anxiety symptoms and diagnoses with the anxiety disorders interview schedule for DSM-IV: Child and parent versions.Journal of the American Academy of Child and Adolescent Psychiatry, 40, 937–944.
Spence, S. H. (1997). Structure of anxiety symptoms among children: A confirmatory factor-analytic study.Journal of Abnormal Psychology, 106, 280–297.
Sukhodolsky, D. G., Scahill, L., Gadow, K. D., Arnold, L. E., Aman, M. G., McDougle, C. J., et al. (2008). Parent-rated anxiety symptoms in children with Pervasive Developmental Disorders: Frequency and association with core autism symptoms and cognitive functioning.Journal of Abnormal Child Psychology, 36, 117–128.
Turpin, G. (1991). The psychophysiological assessment of anxiety disorders: Three-systems measurement and beyond.Psychological Assessment: A Journal of Consulting and Clinical Psychology, 3, 366–375.
Velting, O. N., Setzer, N. J., & Albano, A. M. (2004). Update on and advances in assessment and cognitive-behavioral treatment of anxiety disorders in children and adolescents.Professional Psychology: Research and Practice, 35, 42–54.
White, S. W., & Roberson-Nay, R. (2009). Anxiety, social deficits, and loneliness in youth with autism spectrum disorders.Journal of Autism and Developmental Disorders, 39, 1006–1013.
White, S. W., Albano, A. M., Johnson, C. R., Kasari, C., Ollendick, T., Klin, A., et al. (2010). Development of a cognitive-behavioral intervention program to treat anxiety and social deficits in teens with high-functioning autism.Clinical Child and Family Psychology Review, 13, 77–90.
Wood, J. J., Piacentini, J. C., Bergman, R. L., McCracken, J., & Barrios, V. (2002). Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions.Journal of Clinical Child and Adolescent Psychology, 31, 335–342.
Wood, J. J., Drahota, A., Sze, K., Har, K., Chiu, A., & Langer, D. A. (2009). Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: A randomized, controlled trial.Journal of Child Psychology and Psychiatry, 50, 224–234.
Zandt, F., Prior, M., & Kyrios, M. (2007). Repetitive behaviour in children with high functioning autism and obsessive compulsive disorder.Journal of Autism and Developmental Disorders, 37, 251–259.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Hagopian, L., Jennett, H. (2014). Behavioral Assessment and Treatment for Anxiety for Those with Autism Spectrum Disorder. In: Davis III, T., White, S., Ollendick, T. (eds) Handbook of Autism and Anxiety. Autism and Child Psychopathology Series. Springer, Cham. https://doi.org/10.1007/978-3-319-06796-4_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-06796-4_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-06795-7
Online ISBN: 978-3-319-06796-4
eBook Packages: Behavioral ScienceBehavioral Science and Psychology (R0)