Abstract
The potential for natural products to interact with drugs is considerable given the large number of constituents they contain. Possible interactions may occur during absorption, metabolism, distribution, excretion, transport across the cell membrane, and binding to the specific receptors of drugs. Some of the ingredients in natural products have been shown to significantly influence the pharmacokinetics and pharmacodynamics of drugs. Such interactions may be partly mediated through the significant inhibition or induction of drug-metabolizing enzymes and transporters in the small intestine, liver, kidney, and brain. It remains to be clarified whether the interactions of natural products with medicines are clinically harmful or beneficial to drug therapies. Further scientific and clinical evaluations are needed to establish the proper uses of natural products. This chapter focuses on the possible pharmacokinetic and pharmacodynamic interactions of ginkgo biloba extract, saw palmetto extract, Coleus forskohlii extract, grapefruit juice, and green tea with drugs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Grapefruit Juice
- Constitutive Androstane Receptor
- Ginkgo Biloba Extract
- Ginkgo Biloba Extract
- Hepatic CYPs
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
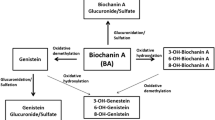
The popularity of dietary supplements and natural products is rapidly increasing in terms of the promotion of health and the prevention and treatment of diseases. Herbal ingredients have received a great deal of attention in complementary and alternative medicine and are used as dietary supplements or natural products in many countries. Herbal ingredients are perceived as safe because they are natural and have been used for centuries in Asian cultures. Elderly people frequently take dietary supplements and natural products with prescription drugs, and this will increase in the near future. A major concern is the adverse events caused by a large excess intake or the interactions of dietary supplements and natural products (including beverages such as fruit juices and green tea) with drugs. The potential for their interaction with drugs is considerable because a large number of constituents are contained in dietary supplements and natural products [43, 117]. Possible changes may occur in the pharmacokinetics and pharmacodynamics of drugs: absorption in the small intestine, metabolism in the intestine and liver, distribution to target organs, transport across the cell membrane, and binding to specific receptors (Fig. 10.1). The induction and inhibition of hepatic drug-metabolizing enzymes by herbal ingredients or dietary compounds have been investigated. For example, St. John’s wort, a herbal medicine used to treat mild depression, has been shown to decrease the blood concentrations of drugs by inducing hepatic cytochrome P450 (CYP) 3A4 activity and thereby attenuates the efficacy of drugs such as cyclosporin, indinavir, and digoxin [5, 27, 89] (Fig. 10.2). Furthermore, ginkgo biloba extract (GBE) and saw palmetto extract (SPE) are commonly prescribed in some European countries for the treatment of cerebral insufficiency and peripheral vascular diseases [51, 67] and reduce the symptoms of benign prostatic hyperplasia (BPH) [28], respectively. Coleus forskohlii extracts (CFE) contain the diterpene forskolin, an activator of adenylate cyclase, and are expected to have various therapeutic [7, 6] and weight loss effects [41, 35]. These herbs are used as dietary supplements and natural products in the USA and Japan. Common beverages such as fruit juice, green tea, and cranberry juice have been reported to affect the pharmacokinetics and pharmacodynamics of drugs [71, 81, 104, 115].
This chapter focuses on the possibility of the pharmacokinetic and pharmacodynamic interactions of GBE, SPE, CFE, grapefruit juice, and green tea with drugs.
2 Ginkgo Biloba Extract
2.1 Induction of CYP by GBE
GBE is one of the most popular herbal ingredients and is used to improve cognitive function and peripheral arterial disease [96]. Recent randomized control trials failed to confirm the effectiveness of GBE in reducing the incidence of dementia in elderly individuals with normal cognition or mild cognitive impairment [19, 97]. Nevertheless, GBE has remained popular among the elderly. As elderly people frequently take prescription drugs with dietary supplements [74], GBE–drug interactions may represent a major concern.
GBE is a natural plant product containing many chemicals. Most commercially available GBE products are standardized according to the amount of ginkgo flavonol glycosides (glycosidic derivatives of quercetin, kaempferol, and isorhamnetin) and terpenoids (ginkgolides A, B, C, and bilobalide), which comprise 22–27 % and approximately 5–7 % of GBE, respectively, and less than 5 ppm of ginkgolic acid [10]. GBE products also contain 0.5–1 % of organic acids, such as vanillic acid and p-hydroxybenzoic acid. The exact constituents of GBE may vary among products due to the time and place of harvest and the extraction methods used.
In pharmacokinetic studies with rats and mice, GBE induced the expression of hepatic drug-metabolizing enzymes, particularly CYP, in a dose- and time-dependent manner (Fig. 10.3) without causing hepatic damage [110, 111]. Significant increases in the concentrations and activities of CYP enzymes were detected on day 1 of feeding of a 0.5 % GBE diet and after the administration of 10 mg GBE/kg body weight for 5 days by intragastric gavage. The human equivalent dose, determined by the body surface normalization method [85], is 1.62 mg/kg body weight, which is approximately 100 mg GBE/60 kg body weight and within the recommended dose range (up to 240 mg) taken from dietary supplements. Among the CYP enzymes, the activity of pentoxyresorufin O-dealkylase, a CYP2B enzyme, was markedly increased, as confirmed by Western blot analysis and expression of mRNA. GBE also increased CYP2B1/2, CYP3A1, and CYP3A2 mRNA levels and related CYP activities in the rat liver [95, 110]. A similar induction of hepatic CYPs by GBE in rats was observed with EGb761, a standardized GBE extract [14, 127].
Dose-dependent changes in hepatic CYP activities in rats administered various doses of GBE. Rats were orally administered GBE at doses of 0, 1, 10, 100, and 1,000 mg/kg body weight for 5 days. Subtypes of CYP enzymes were determined by HPLC. Each column represents the mean ± S.E. *Significantly different from untreated controls, p < 0.05 (cited from Umegaki et al. Jpn J Pharmacol. 90: 345-351, 2002)
It is important to identify which substances in GBE are involved in the induction of CYPs. In vitro and in vivo studies revealed bilobalide to be a major substance inducing hepatic CYPs [13, 20, 91, 107, 111] (Fig. 10.4). Although the contribution of bilobalide is unclear, GBE activated mouse and human PXR, a nuclear receptor involved in the transcriptional regulation of drug-metabolizing enzymes and transporters [121]. The reported half-life of bilobalide in the blood is approximately 2 h in rats and humans [9, 66], indicating that it is eliminated easily from the blood. A single dose by gavage of bilobalide (30 mg/kg) in rats was found to produce a time-dependent induction of hepatic CYP activity and protein expression, and mRNA expression of CYP2B, which was maximal at 6 h and showed a similar response to that exhibited by plasma and liver bilobalide concentrations [106]. These findings suggested that bilobalide markedly induced CYPs; however, the induction was quickly turned off due to bilobalide’s rapid elimination from the liver. The rapid recovery of CYPs was confirmed in rats given excess GBE [100]; continuous and excess feeding of GBE (approximate dose: 500 mg GBE/kg and 21 mg bilobalide/kg) for 1 week to rats markedly induced hepatic CYPs, while discontinuation of the treatment led to normal levels of CYPs within 1 week. These findings suggest that interactions with drugs could be avoided by discounting the GBE treatment.
Content of hepatic CYPs in mice given bilobalide or GBE containing an equivalent amount of bilobalide. Mice were administered either bilobalide (10.5, 21, 42 mg/kg) or GBE (1,000 mg/k; 42 mg/kg as bilobalide) for 5 days. Each value is expressed as the mean ± S.D. for five mice. *Significantly different from untreated controls, p < 0.05. NS: Not significantly different from GBE (1,000 mg/kg) (cited from Umegaki et al. J Pharm Pharmacol. 59: 871-877, 2007)
2.2 CYP-Mediated Interactions
The induction of CYP by GBE suggested an interaction with various drugs. In rats, GBE at 0.5 % in the diet for 2 weeks increased hepatic CYPs and reduced the hypotensive effect of nicardipine, which is metabolized by CYP3A, with a decrease in the maximal nicardipine plasma concentration (C max) and 23-h area under the curve (AUC0–23) [53]. Similarly, 0.5 and 1.0 % GBE diets given to rats for 2 weeks shortened the sleeping time of phenobarbital, which is known to be metabolized by CYP2B, with a reduction in the maximal phenobarbital plasma concentration (C max) and 24-h area under the curve (AUC0–24) [54]. The interaction of GBE with tolbutamide, an oral antidiabetic agent, was also detected in young and aged rats, where a 5-day pretreatment with a 0.1 % GBE diet attenuated the hypoglycemic action of tolbutamide and corresponded well to the enhanced activity of (S)-warfarin 7-hydroxylase, which is a CYP2C subtype and a major isoform metabolizing tolbutamide [99] (Fig. 10.5). It is noteworthy that the interaction of GBE with tolbutamide was clearly observed in aged rats, which have a lower basal activity level of CYP subtypes in the liver, while induction by the GBE treatment was greater than that in young rats. The effects of GBE on the pharmacokinetics and pharmacodynamics of tolbutamide were significantly enhanced in rats maintained on a low-protein diet [105]. In mice, GBE interacted with (s)-warfarin through the induction of hepatic CYP2C by bilobalide, which resulted in increased warfarin metabolism, thereby decreasing the concentration of warfarin and its anticoagulant action [107] (Fig. 10.6).
Effects of a simultaneous treatment and 5-day pretreatment with GBE on the hypoglycemic effect of tolbutamide in young (a) and old (aged) (b) rats. Young rats (7 weeks old) or old rats (19 months old) were administered tolbutamide (40 mg/kg, p.o.) with or without GBE treatment. The GBE-pretreated group was given feed containing 0.1 % GBE for 5 days, and the simultaneous GBE-treated group was given a single dose of GBE (100 mg/kg, p.o.) with tolbutamide. After the administration of tolbutamide, blood was collected for the analysis of blood glucose concentrations. Each point represents the mean ± S.D. for six rats. Filled circles: control group; filled triangles: GBE-pretreated group; and open squares: GBE-simultaneous-treated group. Each point is expressed as the mean ± S.D. for five rats. *Significantly different from controls, p < 0.05 (cited from Sugiyama et al. Life Sci. 75: 1113-1122, 2004)
Effects of the GBE pretreatment on changes in anticoagulation parameters induced by (S)-warfarin or (R)-warfarin. Mice were orally administered GBE (100 mg/kg) for 5 days and (S)-warfarin or (R)-warfarin at a dose of 0.75 mg/kg for the last 3 days of the 5-day regimen. The coagulation parameters shown are prothrombin time (PT), activated partial thromboplastin time (APTT), and thrombotest (Owren) (TTO). Each column represents the mean ± S.E. for 5–6 mice (cited from Taki et al. Phytomed. 19: 177-182, 2012)
Species differences exist for drug-metabolizing enzymes; thus, it is important to investigate whether GBE has the potential to interact with drugs in humans at the current recommended doses. In contrast to studies with rats and mice, reports of GBE–drug interactions in clinical studies are inconsistent; some show interactions [87, 108], while others do not [26, 40, 45, 59, 125]. The intake of GBE (240 mg/day for 28 days) slightly decreased midazolam’s AUC0–infinity and C max in 14 healthy subjects, indicating the interaction of GBE with CYP3A4 drugs [87]. The intake of GBE at 360 mg/day for 28 days slightly lowered the area under the concentration versus time curve (AUC0–infinity) of tolbutamide and blood glucose-lowering effect of tolbutamide in healthy male volunteers [108]. On the other hand, GBE 400 mg/day for 13 days did not influence the elimination half-life of antipyrine in a human study [26]. The administration of GBE of 240 mg/day for 28 days to healthy subjects caused no alteration in the activities of CYP3A4, CYP1A2, CYP2E1, or CYP2D6 assessed using a cocktail of specific substrates for individual CYPs [40]. A 7-day pretreatment with the recommended doses of GBE did not influence the pharmacokinetics or the pharmacodynamics of warfarin in 12 healthy male subjects [45]. The intake of GBE of 240 mg/day for 12 days did not affect the pharmacokinetics of voriconazole, a substrate of CYP2C19, in Chinese volunteers genotyped as either CYP2C19 extensive or poor metabolizers [59]. No relevant effect of GBE for the major CYP enzymes (CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A) was observed following an 8-day pretreatment with GBE at 240 mg/day in 18 healthy men and women [125].
According to the above reports, the interaction of GBE with drugs appears to be slight. In a study of GBE–atorvastatin interactions, treatment with 360 mg of GBE daily for 14 days slightly decreased plasma atorvastatin concentrations, but had little significant effect on its cholesterol-lowering efficacy [38]. The different influences of GBE–drug interactions between humans and rats may be due to species differences in CYPs, the dose of and intake periods of GBE, and the amount of the active substance that induces CYPs.
One of the most concerning adverse events associated with GBE is bleeding, which has been reported in those simultaneously taking GBE and anticoagulant drugs such as aspirin and warfarin [109]. Although an in vitro study showed the PAF antagonistic action of ginkgolide B [18, 57], human studies failed to demonstrate enhanced bleeding by the intake of GBE [52, 55, 107]. In animal studies, GBE attenuated rather than promoted the anticoagulant action of warfarin through the induction of hepatic CYPs by bilobalide [107]. Nevertheless, careful observations for bleeding and hemorrhage and interaction with drugs related to GBE-containing products are needed in clinical practice because of individual differences in sensitivity.
3 Saw Palmetto Extract
The ripe berries of the American dwarf palm (Serenoa repens) have been traditionally used to treat genitourinary problems; to enhance sperm production, breast size, or libido; and as a mild diuretic [28]. SPE is almost exclusively used to treat BPH. Fujino et al. [32] showed that the repeated oral administration of SPE in rats had little significant influence on the content and activities of hepatic drug-metabolizing enzymes. Markowitz et al. [65] reported that SPE (320 mg/day for 14 days) for the treatment of lower urinary tract symptoms (LUTS) suggestive of BPH did not alter the plasma concentrations of probe drugs for CYP2D6 and CYP3A4 activities in normal volunteers (Fig.10.7). No effect of the repeated treatment with SPE (160 mg/day for 28 days) was shown using each probe drug for CYP1A2, CYP2D6, CYP2E1, and CYP3A4 [39]. Therefore, it is unlikely that SPE at generally recommended doses alters the disposition of co-administered drugs.
SPE has been shown to significantly improve urinary dysfunction possibly through the direct action of drug targets such as pharmacological α1-adrenoceptors and muscarinic cholinoceptors in the prostate and bladder [79, 101, 102]; and thus, the combination of SPE and medicines (α1-blockers or antimuscarinics) may be advantageous in terms of a reduction in the dosage, cost, and adverse effects of drugs with pharmacodynamic interactions.
4 Coleus forskohlii Extract
Coleus forskohlii is a member of the mint family and is native to India [8], where it has been used for centuries in Ayurvedic medicine to treat various diseases of the cardiovascular, respiratory, gastrointestinal, and central nervous systems [1]. Extracts of C. forskohlii (CFE) roots contain the diterpene forskolin, which increases cAMP concentrations via the activation of adenylate cyclase, resulting in various therapeutic effects against asthma and idiopathic congestive cardiomyopathy [6, 7]. Theoretically, an increase in cAMP induced by forskolin should enhance lipolysis, leading to elevated fat degradation and physiological fat utilization, thereby promoting fat and weight loss. CFE standardized with forskolin was shown to induce favorable effects on body fat in overweight women and obese men [35, 41]. Thus, CFE standardized with 10 % forskolin is a popular herbal ingredient for commercial weight-loss dietary supplements.
Feeding mice a diet containing CFE (standardized with 10 % forskolin) was clearly shown to dose and time dependently induce hepatic CYP enzymes such as CYP2B, CYP2C, and CYP3A [112]. Significant induction was observed at a CFE dose of 60 mg/kg body weight in mice, which corresponded to approximately 5 mg/kg body weight of a human equivalent dose when calculated using the body surface normalization method [85]. Furthermore, CFE also induced hepatic steatosis in mice, although the effective dose was ten times higher than the dose that induced CYPs [113]. CFE is composed of various substances; however, forskolin was not involved in CYP activation or hepatic steatosis [112, 113], indicating the contribution of unidentified substances. A study of the solvent fractionation of CFE revealed that the unidentified substances involved in CYP induction were mainly distributed in the diethyl ether fraction [122]. The route of CFE administration, by a diet or an intragastric gavage, did not influence the induction of CYPs as long as the CFE dose and feeding diet were the same. In addition, the level of hepatic CYP in CFE-treated groups was positively correlated with the level of starch in a semi-purified diet, which indicated that dietary starch enhanced CYP induction by CFE [124].
Activation of the nuclear receptors pregnane X receptor (PXR) and constitutive androstane receptor (CAR) was shown to regulate drug-metabolizing enzymes as well as glucose and lipid metabolism [34]. Ding and Staudinger clearly demonstrated that the constituents of CFE, namely, forskolin and 1,9-dideoxyforskoiln, induced CYP3A gene expression through the PXR in cultured hepatocytes [21]. Therefore, the activation of PXR and/or CAR may be involved in the mechanism of action of CFE-induced drug-metabolizing enzymes and steatosis.
The induction of hepatic CYPs by CFE suggests the interaction of CFE with prescribed drugs. Warfarin has a powerful anticoagulant action and is metabolized by the CYP2C subfamily of enzymes, which were induced by CFE [112]. As expected, CFE pretreatment attenuated the anticoagulant action of warfarin via the induction of hepatic CYP2C in mice in vivo [123] (Fig. 10.8). CFE also directly inhibited CYP2C activity in human and mouse microsomes to a similar extent in vitro. These findings suggest the interaction of CFE and warfarin and that the intake of warfarin together with dietary supplements containing CFE increases the risk of thrombus formation. As CFE also induced CYP3A, which catalyzes 50 % of prescribed drugs [86], the interaction of CFE and other prescribed drugs may also occur. Healthcare professionals should observe and communicate with patients who are receiving warfarin or other drugs metabolized by CYP2C and CYP3A while consuming dietary weight-loss supplements containing CFE.
Effects of the Coleus forskohlii extract (CFE) pretreatment and/or warfarin administration in mice on (S)-warfarin 7-hydroxylase activities in the liver and prothrombin time in blood. Mice were fed various doses of CFE standardized with 10 % forskolin for 1 week and were administered warfarin by gavage on the last 2 days of the treatment regimen (cited from Yokotani et al. J Pharm Pharmacol. 64: 1793-1801, 2012)
5 Grapefruit Juice
Grapefruit juice was shown to increase the bioavailability of drugs such as calcium channel blockers, benzodiazepines, and immunosuppressants [4, 3, 25, 31, 33, 56]. The main mechanism for this interaction is considered to be the irreversible inhibition of CYP3A, a major drug-metabolizing enzyme in the small intestine, by the furanocoumarins present in grapefruit juice [82]. Grapefruit juice inhibits not only metabolic enzymes but also drug transporters such as P-glycoprotein [23, 64, 104], which play important roles in the function of the intestinal barrier in a coordinated manner with CYP3A [103]. The inhibitory effect of grapefruit juice on the intestinal barrier may enhance the oral bioavailability of drugs, which has been associated with a higher incidence of side effects.
Morphine is the most commonly used opioid analgesic for the treatment of pain associated with cancer. The antinociceptive effect of morphine, a substrate of P-glycoprotein [92], was enhanced by the knockout of the P-glycoprotein gene in mice and the administration of a P-glycoprotein inhibitor in rats [60, 118, 129]. Furthermore, P-glycoprotein may be partly associated with morphine tolerance [2, 80], which limits the clinical use of morphine. We examined the effects of grapefruit juice on oral morphine antinociception and pharmacokinetics in morphine-tolerant rats [81]. Morphine tolerance was developed by the repeated oral administration of morphine for 5 days, and grapefruit juice significantly potentiated the antinociceptive effect. Morphine concentrations in blood and intrathecal cerebrospinal fluid (CSF) were gradually reduced by the repeated treatment with morphine. Grapefruit juice significantly increased the blood concentration of morphine in morphine-tolerant rats. These results suggest that grapefruit juice enhances antinociception by increasing the intestinal absorption of morphine. The inhibition of intestinal P-glycoprotein by grapefruit juice may partly overcome morphine tolerance. However, there is absence of clinical evidence demonstrating an enhancement in the effects of morphine by grapefruit juice. In humans, the absorption of morphine is regulated by the intestinal P-glycoprotein [48]. Thus, further clinical studies are needed to examine the clinical effects of grapefruit juice on intestinal P-glycoprotein activity.
6 Green Tea (Catechins)
Over recent decades, green tea has been recognized as a healthy beverage for the prevention of cancer, cardiovascular disorders, and infectious diseases [47, 119] and is consumed by a large proportion of the world’s population. Accordingly, it is anticipated that opportunities for the concomitant use of various drugs with green tea are increasing; thus, the evaluation of scientific evidence on possible drug interactions with green tea catechins is of importance to reduce the risks of unwanted side effects. Green tea catechin–drug interactions mediated by the inhibition or the induction of enzymes such as drug-metabolizing enzymes and drug transporters need to be considered.
Green tea (Camellia sinensis) is the most abundant source of catechins and consists of (-)-epigallocatechin-3-gallate (EGCG), (-)-epigallocatechin (EGC), (-)-epicatechin (EC), and (-)-epicatechin-3-gallate (ECG) [37], which accounts for 30–42 % of the dry weight of the solids in brewed green tea [47]. In general, a cup of infused green tea (150 mL) supplies 30–40 mg of EGCG [42]. After the ingestion of a green tea extract containing 375 mg of EGCG, the plasma concentration of EGCG reached approximately 4 μM [75].
6.1 Cytochrome P450 Enzymes
Many drug interactions are attributed to the inhibition or the induction of CYP enzymes [116]. The effects of green tea on the activity of CYP enzymes were first reported in rodents: drinking green tea significantly increased rat CYP1A1, 1A2, and 2B1 activities, but not CYP2E1 or 3A activities [98]. Park et al. recently demonstrated that repeated treatment with a green tea extract up-regulated CYP2B1 and downregulated CYP3A mRNA expression in the rat liver [83]. Pharmacokinetic interactions between green tea catechins and CYP substrate drugs including clozapine [44], diltiazem [61], midazolam [77], nicardipine [15], tamoxifen [94], and verapamil [17] have been studied in rats. The main findings are summarized in Table 10.1. These animal studies suggest that green tea catechins markedly inhibit CYP3A activity in the liver or the intestine and increase the plasma concentrations of its substrates. Regarding human CYP enzymes, Muto et al. reported that ECG and EGCG inhibited CYP1A1, 1A2, 2A6, 2C9, 2E1, and 3A4 activities in a concentration-dependent manner in a human CYP-expressing membrane fraction [72]. Contrary to its inhibitory effects, treatment with green tea extract for 6 h induced CYP1A1 and 1A2 expression and increased the mRNA levels of CYP2E1, 2D6, and 2C isoforms in human tongue cells [120]. In a clinical study, the chronic consumption of decaffeinated green tea extract did not alter either the pharmacokinetics of alprazolam, a CYP3A4 probe drug, or the metabolic ratio of dextromethorphan, an index of CYP2D6 activity, in healthy volunteers [22]. Chow and colleagues conducted a clinical trial to determine the effects of repeated green tea catechin administration on in vivo CYP activities using a drug cocktail containing caffeine (CYP1A2), dextromethorphan (CYP2D6), losartan (CYP2C19), and buspirone (CYP3A) [16]. Among the phenotypic indices investigated, only the area under the plasma concentration–time curve (AUC) of buspirone was significantly higher (by 1.2-fold) than the baseline value by green tea catechins, suggesting that green tea caused a small reduction in CYP3A activity but had no effects on CYP1A2, 2D6, or 2C19. More recently, Werba et al. showed that green tea intake doubled the AUC of simvastatin, a cholesterol-lowering agent, and led to intense leg muscle cramps and pain in a hypercholesterolemic patient [115] (Fig. 10.9). Because simvastatin is mainly metabolized by CYP3A [76], this interaction may be due to a reduction in CYP3A activity by green tea. Further studies are required to clarify whether these interactions stem from the modulation of CYP3A activity. Collectively, green tea catechins may have an inhibitory effect on CYP3A in humans. However, considering the low bioavailability of catechins [58], the pharmacokinetic interactions of green tea catechins with CYP3A substrate drugs may mainly occur in the gastrointestinal tract, similar to grapefruit juice [68]. It also cannot be excluded that green tea catechins have an inductive effect on some CYP subtypes, especially during the chronic consumption of green tea. Further investigations of the interactions between green tea catechins and CYP substrates including the underlying mechanisms will help toward optimal pharmacotherapy in patients who drink green tea.
6.2 Other Enzymes
Interactions mediated by other drug-metabolizing enzymes, such as phase II conjugating enzymes, have received less attention than CYP enzymes [49]. However, because many drugs and their metabolites undergo conjugation reactions, it is important to enhance our understanding of phase II enzyme-mediated drug interactions. Since green tea catechins undergo conjugate metabolism by UDP-glucuronosyltransferase (UGT), sulfotransferase (SULT), and catechol-O-methyltransferase (COMT) in rodents and humans [29], the coexistence of green tea catechins and their substrates may cause drug interactions through the inhibition of these enzymes. Zhu et al. reported that a green tea catechin mixture and EGCG inhibited the glucuronidation of estrone in a concentration-dependent manner with IC50 values of 12.5 and 10 μg/ml, respectively, in rat liver microsomes [128]. Moreover, recent studies revealed that UGT1A1 and UGT1A4 activities were markedly inhibited by EGCG with IC50 values of 7.8 and 34.4 μg/mL in human liver microsomes [69, 70]. EGCG showed weak inhibitory activities toward UGT1A6 and UGT1A9 [69]. On the other hand, EGCG was shown to have no effect on the mRNA expression of UGT1A1 [11]. To the best of our knowledge, there is currently no clinical evidence regarding UGT-mediated drug interactions with green tea catechins. As for the other phase II enzymes, EGCG has been reported to inhibit COMT activity with IC50 values ranging from 0.07 to 0.2 μM in human liver cytosol [63, 73]. In in vitro experiments using human recombinant SULT1A1 and SULT1A3, green tea catechins, particularly ECC and EGCG, inhibited SULT1A1 and SULT1A3 activities at around 10 μM [78]. In addition to the inhibition of phase II enzymes, Golden and colleagues reported that EGCG directly reacted with bortezomib, an anticancer drug, and blocked its antiproliferative function in preclinical in vitro and in vivo models [36]. This interaction may have arisen as a result of a physicochemical interaction leading to the formation of a covalent cyclic boronate between EGCG and bortezomib. In summary, the findings described above highlight the possibility of green tea catechin–drug interactions through the modulation of not only phase II enzymes but also the chemical structures of co-administered drugs.
6.3 Transporter-Mediated Interactions
Many findings from in vitro and in vivo studies suggest that drug transporter-mediated drug interactions are of clinical importance [24]. The recognition of drug interactions that lead to negative clinical outcomes, i.e., decreased effectiveness or tolerability, should support better medication and improve patient care. Several dietary flavonoids were found to modulate the efflux transporter, P-glycoprotein [12, 93]. Concerning green tea catechins, EGCG in green tea was shown to inhibit the efflux of drugs mediated by P-glycoprotein in vitro [46]. Qian et al. also demonstrated that EGCG modulated the function of P-glycoprotein and reversed P-glycoprotein-mediated multidrug resistance in human cancer cells [84]. To date, there is a lack of in vivo evidence to support the inhibitory effects of green tea catechins on P-glycoprotein. A recent study showed that the intravenous administration of EGCG (20 mg/kg) to rats inhibited the transport of irinotecan and its active metabolite, SN-38, into the biliary tract, and prolonged their half-lives in plasma, possibly by modulating P-glycoprotein activity [62]. BCRP is another efflux transporter involved in cross-resistance to chemotherapeutic agents [88]. Some flavonoids have been identified as potent inhibitors of BCRP; however, EGC and EGCG did not exhibit such inhibitory activity in vitro [126].
Uptake carriers such as OATP represent another class of drug transporters [50]. Although no data are available regarding the in vivo impact of green tea catechins on OATP activity, a few in vitro studies may facilitate further investigations of OATP-mediated drug interactions with green tea catechins. Using OATP1B1-expressing HeLa cells, Wang et al. found that EGCG, but not EGC, was a potential inhibitor of OATP1B1 with an IC50 of 14.1 μM [114]. As for OATP2B1, which is expressed on human intestinal epithelia, green tea itself and green tea catechins including EC, ECG, and EGCG, significantly inhibited the OATP2B1-mediated transport of estrone-3-sulfate in human embryonic kidney 293 cells at concentrations considered likely to be attainable in the human intestine [30]. Recently, Roth et al. showed that ECG and EGCG inhibited the uptake activities of OATP1A2, 1B1, and 2B1 in a concentration-dependent manner, while EC and EGC had minimal effects on OATPs [90]. Interestingly, EGCG was found to be a potent stimulator of OATP1B3-mediated uptake for one substrate examined, whereas EGCG behaved as an inhibitor of OATP1B3 for another substrate [90]. This study suggested that potential inhibitors should be examined using multiple and clinically relevant substrates when screening for OATP-mediated drug interactions. In summary, more in vivo evidence is needed for a better understanding of drug transporter-mediated drug interactions between green tea catechins and drugs. We also note that such interactions may have beneficial properties. For example, given that green tea catechins have potent inhibitory effects on efflux transporters such as P-glycoprotein in vivo, drinking green tea may be valuable for patients receiving cancer chemotherapy because P-glycoprotein inhibition by catechins could suppress multidrug resistance in cancer cells.
7 Conclusions
The oral intake of some natural products has been shown to significantly influence the pharmacokinetics and pharmacodynamics of co-administered drugs. Such interactions may be partly mediated through the significant inhibition or induction of drug-metabolizing enzymes and transporters in the small intestine, liver, kidney, and brain. Whether the interactions of natural products with medicines have clinically harmful or beneficial effects for drug therapies is needed to be clarified. Furthermore, some ingredients of natural products may directly affect the pharmacological targets of medicines, thereby causing a significant augmentation or deterioration in therapeutic effects. Further scientific and clinical evaluations of the pharmacokinetic and pharmacodynamic interactions of natural products with prescription drugs are prospectively encouraged to establish their proper uses in clinical settings. Finally, it should be kept in mind that combinations of natural products (including beverages) and medicines should be viewed cautiously in terms of potential adverse interactions in patients treated with drugs, such as warfarin, that have relatively narrow therapeutic windows.
References
Ammon HP, Muller AB (1985) Forskolin: from an ayurvedic remedy to a modern agent. Planta Med 51:473–477
Aquilante CL, Letrent SP, Pollack GM, Brouwer KL (2000) Increased brain P-glycoprotein in morphine tolerant rats. Life Sci 66:L47–L51
Bailey DG, Arnold JM, Strong HA, Munoz C, Spence JD (1993) Effect of grapefruit juice and naringin on nisoldipine pharmacokinetics. Clin Pharmacol Ther 54:589–594
Bailey DG, Spence JD, Munoz C, Arnold JM (1991) Interaction of citrus juices with felodipine and nifedipine. Lancet 337:268–269
Barone GW, Gurley BJ, Ketel BL, Lightfoot ML, Abul-Ezz SR (2000) Drug interaction between St. John's wort and cyclosporine. Ann Pharmacother 34:1013–1016
Bauer K, Dietersdorfer F, Sertl K, Kaik B, Kaik G (1993) Pharmacodynamic effects of inhaled dry powder formulations of fenoterol and colforsin in asthma. Clin Pharmacol Ther 53:76–83
Baumann G, Felix S, Sattelberger U, Klein G (1990) Cardiovascular effects of forskolin (HL 362) in patients with idiopathic congestive cardiomyopathy—a comparative study with dobutamine and sodium nitroprusside. J Cardiovasc Pharmacol 16:93–100
Bhat SV, Bajwa BS, Dornauer H, de Souza HJ (1977) Structures and stereochemistry of new labdane diterpenoids from Coleus forskohlii briq. Tetrahedron Lett 19:1669–1672
Biber A, Koch E (1999) Bioavailability of ginkgolides and bilobalide from extracts of ginkgo biloba using GC/MS. Planta Med 65:192–193
Blumenthal M (1998) The complete German commission e monographs—therapeutic guide to herbal medicines. The American Botanical Council, Austin, TX
Bothe H, Gassmann K, Gotz C, Fritsche E, Abel J, Haarmann-Stemmann T (2011) Epigallocatechin-3-gallate does not affect the activity of enzymes involved in metabolic activation and cellular excretion of benzo[a]pyrene in human colon carcinoma cells. Toxicol Lett 203:258–264
Castro AF, Altenberg GA (1997) Inhibition of drug transport by genistein in multidrug-resistant cells expressing P-glycoprotein. Biochem Pharmacol 53:89–93
Chang TK, Chen J, Teng XW (2006) Distinct role of bilobalide and ginkgolide A in the modulation of rat CYP2B1 and CYP3A23 gene expression by Ginkgo biloba extract in cultured hepatocytes. Drug Metab Dispos 34:234–242
Chatterjee SS, Doelman CJ, Noldner M, Biber A, Koch E (2005) Influence of the Ginkgo extract EGb 761 on rat liver cytochrome P450 and steroid metabolism and excretion in rats and man. J Pharm Pharmacol 57:641–650
Choi JS, Burm JP (2009) Effects of oral epigallocatechin gallate on the pharmacokinetics of nicardipine in rats. Arch Pharm Res 32:1721–1725
Chow HH, Hakim IA, Vining DR, Crowell JA, Cordova CA, Chew WM, Xu MJ, Hsu CH, Ranger-Moore J, Alberts DS (2006) Effects of repeated green tea catechin administration on human cytochrome P450 activity. Cancer Epideml Biomarkers Prev 15:2473–2476
Chung JH, Choi DH, Choi JS (2009) Effects of oral epigallocatechin gallate on the oral pharmacokinetics of verapamil in rats. Biopharm Drug Dispos 30:90–93
Chung KF, Dent G, Mccusker M, Guinot P, Page CP, Barnes PJ (1987) Effect of a ginkgolide mixture (BN 52063) in antagonising skin and platelet responses to platelet activating factor in man. Lancet 1:248–251
Dekosky ST, Williamson JD, Fitzpatrick AL, Kronmal RA, Ives DG, Saxton JA, Lopez OL, Burke G, Carlson MC, Fried LP, Kuller LH, Robbins JA, Tracy RP, Woolard NF, Dunn L, Snitz BE, Nahin RL, Furberg CD (2008) Ginkgo biloba for prevention of dementia: a randomized controlled trial. JAMA 300:2253–2262
Deng Y, Bi HC, Zhao LZ, Wang XD, Chen J, Ou ZM, Ding L, Xu LJ, Guan S, Chen X, Zhou SF, Huang M (2008) Induction of cytochrome P450 3A by the Ginkgo biloba extract and bilobalides in human and rat primary hepatocytes. Drug Metab Lett 2:60–66
Ding X, Staudinger JL (2005) Induction of drug metabolism by forskolin: the role of the pregnane X receptor and the protein kinase a signal transduction pathway. J Pharmacol Exp Ther 312:849–856
Donovan JL, Chavin KD, Devane CL, Taylor RM, Wang JS, Ruan Y, Markowitz JS (2004) Green tea (Camellia sinensis) extract does not alter cytochrome p450 3A4 or 2D6 activity in healthy volunteers. Drug Metab Dispos 32:906–908
Dresser GK, Bailey DG, Leake BF, Schwarz UI, Dawson PA, Freeman DJ, Kim RB (2002) Fruit juices inhibit organic anion transporting polypeptide-mediated drug uptake to decrease the oral availability of fexofenadine. Clin Pharmacol Ther 71:11–20
Dubuske LM (2005) The role of P-glycoprotein and organic anion-transporting polypeptides in drug interactions. Drug Saf 28:789–801
Ducharme MP, Warbasse LH, Edwards DJ (1995) Disposition of intravenous and oral cyclosporine after administration with grapefruit juice. Clin Pharmacol Ther 57:485–491
Duche JC, Barre J, Guinot P, Duchier J, Cournot A, Tillement JP (1989) Effect of Ginkgo biloba extract on microsomal enzyme induction. Int J Clin Pharmacol Res 9:165–168
Durr D, Stieger B, Kullak-Ublick GA, Rentsch KM, Steinert HC, Meier PJ, Fattinger K (2000) St John's Wort induces intestinal P-glycoprotein/MDR1 and intestinal and hepatic CYP3A4. Clin Pharmacol Ther 68:598–604
Ernst E (2002) The risk-benefit profile of commonly used herbal therapies: Ginkgo, St. John's Wort, Ginseng, Echinacea, Saw Palmetto, and Kava. Ann Intern Med 136:42–53
Feng WY (2006) Metabolism of green tea catechins: an overview. Curr Drug Metab 7:755–809
Fuchikami H, Satoh H, Tsujimoto M, Ohdo S, Ohtani H, Sawada Y (2006) Effects of herbal extracts on the function of human organic anion-transporting polypeptide OATP-B. Drug Metab Dispos 34:577–582
Fuhr U, Muller-Peltzer H, Kern R, Lopez-Rojas P, Junemann M, Harder S, Staib AH (2002) Effects of grapefruit juice and smoking on verapamil concentrations in steady state. Eur J Clin Pharmacol 58:45–53
Fujino (Oki) T, Suzuki M, Yamada S (2007) Effects of saw palmetto extract on urodynamic function and receptors in the lower urinary tract. Jap J Complem Alter Med 4:41–50
Fukatsu S, Fukudo M, Masuda S, Yano I, Katsura T, Ogura Y, Oike F, Takada Y, Inui K (2006) Delayed effect of grapefruit juice on pharmacokinetics and pharmacodynamics of tacrolimus in a living-donor liver transplant recipient. Drug Metab Pharmacokinet 21:122–125
Gao J, Xie W (2010) Pregnane X receptor and constitutive androstane receptor at the crossroads of drug metabolism and energy metabolism. Drug Metab Dispos 38:2091–2095
Godard MP, Johnson BA, Richmond SR (2005) Body composition and hormonal adaptations associated with forskolin consumption in overweight and obese men. Obes Res 13:1335–1343
Golden EB, Lam PY, Kardosh A, Gaffney KJ, Cadenas E, Louie SG, Petasis NA, Chen TC, Schonthal AH (2009) Green tea polyphenols block the anticancer effects of bortezomib and other boronic acid-based proteasome inhibitors. Blood 113:5927–5937
Graham HN (1992) Green tea composition, consumption, and polyphenol chemistry. Prev Med 21:334–350
Guo CX, Pei Q, Yin JY, Peng XD, Zhou BT, Zhao YC, Wu LX, Meng XG, Wang G, Li Q, Ouyang DS, Liu ZQ, Zhang W, Zhou HH (2012) Effects of Ginkgo biloba extracts on pharmacokinetics and efficacy of atorvastatin based on plasma indices. Xenobiotica 42(8):784–790
Gurley BJ, Gardner SF, Hubbard MA, Williams DK, Gentry WB, Carrier J, Khan IA, Edwards DJ, Shah A (2004) In vivo assessment of botanical supplementation on human cytochrome P450 phenotypes: citrus aurantium, Echinacea purpurea, milk thistle, and saw palmetto. Clin Pharmacol Ther 76:428–440
Gurley BJ, Gardner SF, Hubbard MA, Williams DK, Gentry WB, Cui Y, Ang CY (2002) Cytochrome P450 phenotypic ratios for predicting herb-drug interactions in humans. Clin Pharmacol Ther 72:276–287
Henderson S, Magu B, Rasmussen C, Lancaster S, Kerksick C, Smith P, Melton C, Cowan P, Greenwood M, Earnest C, Almada A, Milnor P, Magrans T, Bowden R, Ounpraseuth S, Thomas A, Kreider RB (2005) Effects of coleus forskohlii supplementation on body composition and hematological profiles in mildly overweight women. J Int Soc Sports Nutr 2:54–62
Imai K, Suga K, Nakachi K (1997) Cancer-preventive effects of drinking green tea among a Japanese population. Prev Med 26:769–775
Izzo AA, Ernst E (2001) Interactions between herbal medicines and prescribed drugs: a systematic review. Drugs 61:2163–2175
Jang EH, Choi JY, Park CS, Lee SK, Kim CE, Park HJ, Kang JS, Lee JW, Kang JH (2005) Effects of green tea extract administration on the pharmacokinetics of clozapine in rats. J Pharm Pharmacol 57:311–316
Jiang X, Williams KM, Liauw WS, Ammit AJ, Roufogalis BD, Duke CC, Day RO, Mclachlan AJ (2005) Effect of ginkgo and ginger on the pharmacokinetics and pharmacodynamics of warfarin in healthy subjects. Br J Clin Pharmacol 59:425–432
Jodoin J, Demeule M, Beliveau R (2002) Inhibition of the multidrug resistance P-glycoprotein activity by green tea polyphenols. Biochim Biophys Acta 1542:149–159
Khan N, Mukhtar H (2007) Tea polyphenols for health promotion. Life Sci 81:519–533
Kharasch ED, Hoffer C, Whittington D, Sheffels P (2003) Role of P-glycoprotein in the intestinal absorption and clinical effects of morphine. Clin Pharmacol Ther 74:543–554
Kiang TK, Ensom MH, Chang TK (2005) UDP-glucuronosyltransferases and clinical drug-drug interactions. Pharmacol Ther 106:97–132
Kim RB (2006) Transporters and drug discovery: why, when, and how. Mol Pharmacol 3:26–32
Kleijnen J, Knipschild P (1992) Ginkgo biloba. Lancet 340:1136–1139
Kohler S, Funk P, Kieser M (2004) Influence of a 7-day treatment with Ginkgo biloba special extract EGb 761 on bleeding time and coagulation: a randomized, placebo-controlled, double-blind study in healthy volunteers. Blood Coagul Fibrinolysis 15:303–309
Kubota Y, Kobayashi K, Tanaka N, Nakamura K, Kunitomo M, Umegaki K, Shinozuka K (2003) Interaction of Ginkgo biloba extract (GBE) with hypotensive agent, nicardipine, in rats. In Vivo 17:409–412
Kubota Y, Kobayashi K, Tanaka N, Nakamura K, Kunitomo M, Umegaki K, Shinozuka K (2004) Pretreatment with Ginkgo biloba extract weakens the hypnosis action of phenobarbital and its plasma concentration in rats. J Pharm Pharmacol 56:401–405
Kudolo GB, Dorsey S, Blodgett J (2002) Effect of the ingestion of Ginkgo biloba extract on platelet aggregation and urinary prostanoid excretion in healthy and Type 2 diabetic subjects. Thromb Res 108:151–160
Kupferschmidt HH, Ha HR, Ziegler WH, Meier PJ, Krahenbuhl S (1995) Interaction between grapefruit juice and midazolam in humans. Clin Pharmacol Ther 58:20–28
Lamant V, Mauco G, Braquet P, Chap H, Douste-Blazy L (1987) Inhibition of the metabolism of platelet activating factor (PAF-acether) by three specific antagonists from Ginkgo biloba. Biochem Pharmacol 36:2749–2752
Lee MJ, Maliakal P, Chen L, Meng X, Bondoc FY, Prabhu S, Lambert G, Mohr S, Yang CS (2002) Pharmacokinetics of tea catechins after ingestion of green tea and (-)-epigallocatechin-3-gallate by humans: formation of different metabolites and individual variability. Cancer Epidem Biomarkers Prev 11:1025–1032
Lei HP, Wang G, Wang LS, Ou-Yang DS, Chen H, Li Q, Zhang W, Tan ZR, Fan L, He YJ, Zhou HH (2009) Lack of effect of Ginkgo biloba on voriconazole pharmacokinetics in Chinese volunteers identified as CYP2C19 poor and extensive metabolizers. Ann Pharmacother 43:726–731
Letrent SP, Pollack GM, Brouwer KR, Brouwer KL (1999) Effects of a potent and specific P-glycoprotein inhibitor on the blood–brain barrier distribution and antinociceptive effect of morphine in the rat. Drug Metab Dispos 27:827–834
Li C, Choi JS (2008) Effects of epigallocatechin gallate on the bioavailability and pharmacokinetics of diltiazem in rats. Pharmazie 63:815–818
Lin LC, Wang MN, Tsai TH (2008) Food-drug interaction of (-)-epigallocatechin-3-gallate on the pharmacokinetics of irinotecan and the metabolite SN-38. Chem Biol Interact 174:177–182
Lu H, Meng X, Yang CS (2003) Enzymology of methylation of tea catechins and inhibition of catechol-O-methyltransferase by (-)-epigallocatechin gallate. Drug Metab Dispos 31:572–579
Marchetti S, Mazzanti R, Beijnen JH, Schellens JH (2007) Concise review: Clinical relevance of drug drug and herb drug interactions mediated by the ABC transporter ABCB1 (MDR1, P-glycoprotein). Oncologist 12:927–941
Markowitz JS, Donovan CL, Devane CL, Taylor RM, Ruan Y, Wang JS, Chavin KD (2003) Multiple doses of saw palmetto (Serenoa repens) did not alter cytochrome P450 2D5 and 3A4 activity in normal volunteers. Clin Pharmacol Ther 74:536–542
Mauri P, Simonetti P, Gardana C, Minoggio M, Morazzoni P, Bombardelli E, Pietta P (2001) Liquid chromatography/atmospheric pressure chemical ionization mass spectrometry of terpene lactones in plasma of volunteers dosed with Ginkgo biloba L. extracts. Rapid Commun Mass Spectrom 15:929–934
Mckenna DJ, Jones K, Hughes K (2001) Efficacy, safety, and use of ginkgo biloba in clinical and preclinical applications. Altern Ther Health Med 7(70–86):88–90
Mertens-Talcott SU, Zadezensky I, De Castro WV, Derendorf H, Butterweck V (2006) Grapefruit-drug interactions: can interactions with drugs be avoided? J Clin Pharmacol 46:1390–1416
Mohamed ME, Frye RF (2011) Inhibitory effects of commonly used herbal extracts on UDP-glucuronosyltransferase 1A4, 1A6, and 1A9 enzyme activities. Drug Metab Dispos 39:1522–1528
Mohamed MF, Tseng T, Frye RF (2010) Inhibitory effects of commonly used herbal extracts on UGT1A1 enzyme activity. Xenobiotica 40:663–669
Mohammed Abdul MI, Jiang X, Williams KM, Day RO, Roufogalis BD, Liauw WS, Xu H, Mclachlan AJ (2008) Pharmacodynamic interaction of warfarin with cranberry but not with garlic in healthy subjects. Br J Pharmacol 154:1691–1700
Muto S, Fujita K, Yamazaki Y, Kamataki T (2001) Inhibition by green tea catechins of metabolic activation of procarcinogens by human cytochrome P450. Mutat Res 479:197–206
Nagai M, Conney AH, Zhu BT (2004) Strong inhibitory effects of common tea catechins and bioflavonoids on the O-methylation of catechol estrogens catalyzed by human liver cytosolic catechol-O-methyltransferase. Drug Metab Dispos 32:497–504
Nahin RL, Pecha M, Welmerink DB, Sink K, Dekosky ST, Fitzpatrick AL (2009) Concomitant use of prescription drugs and dietary supplements in ambulatory elderly people. J Am Geriatr Soc 57:1197–1205
Nakagawa K, Okuda S, Miyazawa T (1997) Dose-dependent incorporation of tea catechins, (-)-epigallocatechin-3-gallate and (-)-epigallocatechin, into human plasma. Biosci Biotechnol Biochem 61:1981–1985
Neuvonen PJ, Niemi M, Backman JT (2006) Drug interactions with lipid-lowering drugs: mechanisms and clinical relevance. Clin Pharmacol Ther 80:565–581
Nishikawa M, Ariyoshi N, Kotani A, Ishii I, Nakamura H, Nakasa H, Ida M, Kimura N, Kimura M, Hasegawa A, Kusu F, Ohmori S, Nakazawa K, Kitada M (2004) Effects of continuous ingestion of green tea or grape seed extracts on the pharmacokinetics of midazolam. Drug Metab Pharmacokinet 19:280–289
Nishimuta H, Ohtani H, Tsujimoto M, Ogura K, Hiratsuka A, Sawada Y (2007) Inhibitory effects of various beverages on human recombinant sulfotransferase isoforms SULT1A1 and SULT1A3. Biopharm Drug Dispos 28:491–500
Oki T, Suzuki M, Nishioka Y, Yasuda A, Umegaki K, Yamada S (2005) Effects of saw palmetto extract on micturition reflex of rats and its autonomic receptor binding activity. J Urol 173:1395–1399
Okura T, Ozawa T, Ibe M, Taki Y, Kimura M, Kagawa Y, Kato Y, Yamada S (2009) Effects of repeated morphine treatment on the antinociceptive effects, intestinal absorption, and efflux from intestinal epithelial cells of morphine. Biol Pharm Bull 32:1571–1575
Okura T, Ozawa T, Ito Y, Kimura M, Kagawa Y, Yamada S (2008) Enhancement by grapefruit juice of morphine antinociception. Biol Pharm Bull 31:2338–2341
Paine MF, Widmer WW, Hart HL, Pusek SN, Beavers KL, Criss AB, Brown SS, Thomas BF, Watkins PB (2006) A furanocoumarin-free grapefruit juice establishes furanocoumarins as the mediators of the grapefruit juice-felodipine interaction. Am J Clin Nutr 83:1097–1105
Park D, Jeon JH, Shin S, Joo SS, Kang DH, Moon SH, Jang MJ, Cho YM, Kim JW, Ji HJ, Ahn B, Oh KW, Kim YB (2009) Green tea extract increases cyclophosphamide-induced teratogenesis by modulating the expression of cytochrome P-450 mRNA. Reprod Toxicol 27:79–84
Qian F, Wei D, Zhang Q, Yang S (2005) Modulation of P-glycoprotein function and reversal of multidrug resistance by (-)-epigallocatechin gallate in human cancer cells. Biomed Pharmacother 59:64–69
Reagan-Shaw S, Nihal M, Ahmad N (2008) Dose translation from animal to human studies revisited. FASEB J 22:659–661
Rendic S, Di Carlo FJ (1997) Human cytochrome P450 enzymes: a status report summarizing their reactions, substrates, inducers, and inhibitors. Drug Metab Rev 29:413–580
Robertson SM, Davey RT, Voell J, Formentini E, Alfaro RM, Penzak SR (2008) Effect of Ginkgo biloba extract on lopinavir, midazolam and fexofenadine pharmacokinetics in healthy subjects. Curr Med Res Opin 24:591–599
Robey RW, To KK, Polgar O, Dohse M, Fetsch P, Dean M, Bates SE (2009) ABCG2: a perspective. Adv Drug Deliv Rev 61:3–13
Roby CA, Anderson GD, Kantor E, Dryer DA, Burstein AH (2000) St John's Wort: effect on CYP3A4 activity. Clin Pharmacol Ther 67:451–457
Roth M, Timmermann BN, Hagenbuch B (2011) Interactions of green tea catechins with organic anion-transporting polypeptides. Drug Metab Dispos 39:920–926
Sasaki K, Wada K, Hatta S, Ohshika H, Haga M (1997) Bilobalide, a constituent of Ginkgo biloba L., potentiates drug-metabolizing enzyme activities in mice: possible mechanism for anticonvulsant activity against 4-O-methylpyridoxine-induced convulsions. Res Comm Mol Pathol Pharmacol 96:45–56
Schinkel AH, Wagenaar E, Van Deemter L, Mol CA, Borst P (1995) Absence of the mdr1a P-Glycoprotein in mice affects tissue distribution and pharmacokinetics of dexamethasone, digoxin, and cyclosporin A. J Clin Invest 96:1698–1705
Shapiro AB, Ling V (1997) Effect of quercetin on Hoechst 33342 transport by purified and reconstituted P-glycoprotein. Biochem Pharmacol 53:587–596
Shin SC, Choi JS (2009) Effects of epigallocatechin gallate on the oral bioavailability and pharmacokinetics of tamoxifen and its main metabolite, 4-hydroxytamoxifen, in rats. Anticancer Drugs 20:584–588
Shinozuka K, Umegaki K, Kubota Y, Tanaka N, Mizuno H, Yamauchi J, Nakamura K, Kunitomo M (2002) Feeding of Ginkgo biloba extract (GBE) enhances gene expression of hepatic cytochrome P-450 and attenuates the hypotensive effect of nicardipine in rats. Life Sci 70:2783–2792
Sierpina VS, Wollschlaeger B, Blumenthal M (2003) Ginkgo biloba. Am Fam Physician 68:923–926
Snitz BE, O'meara ES, Carlson MC, Arnold AM, Ives DG, Rapp SR, Saxton J, Lopez OL, Dunn LO, Sink KM, Dekosky ST (2009) Ginkgo biloba for preventing cognitive decline in older adults: a randomized trial. JAMA 302:2663–2670
Sohn OS, Surace A, Fiala ES, Richie JP Jr, Colosimo S, Zang E, Weisburger JH (1994) Effects of green and black tea on hepatic xenobiotic metabolizing systems in the male F344 rat. Xenobiotica 24:119–127
Sugiyama T, Kubota Y, Shinozuka K, Yamada S, Wu J, Umegaki K (2004) Ginkgo biloba extract modifies hypoglycemic action of tolbutamide via hepatic cytochrome P450 mediated mechanism in aged rats. Life Sci 75:1113–1122
Sugiyama T, Kubota Y, Shinozuka K, Yamada S, Yamada K, Umegaki K (2004) Induction and recovery of hepatic drug metabolizing enzymes in rats treated with Ginkgo biloba extract. Food Chem Toxicol 42:953–957
Suzuki M, Ito Y, Fujino T, Masayuki A, Umegaki K, Onoue S, Noguchi H, Yamada S (2009) Pharmacological effects of saw palmetto extract in the lower urinary tract. Acta Pharmacol Sin 30:271–281
Suzuki M, Oki T, Sugiyama T, Umegaki K, Uchida S, Yamada S (2007) Muscarinic and alpha-1-adrenergic receptor binding characteristics of saw palmetto extract in rat lower urinary tract. Urol 69:1216–1220
Synold TW, Dussault I, Forman BM (2001) The orphan nuclear receptor SXR coordinately regulates drug metabolism and efflux. Nat Med 7:584–590
Takanaga H, Ohnishi A, Matsuo H, Sawada Y (1998) Inhibition of vinblastine efflux mediated by P-glycoprotein by grapefruit juice components in caco-2 cells. Biol Pharm Bull 21:1062–1066
Taki Y, Hagiwara E, Hirose C, Shinozuka K, Umegaki K, Yamada S (2011) Effects of Ginkgo biloba extract on the pharmacokinetics and pharmacodynamics of tolbutamide in protein-restricted rats. J Pharm Pharmacol 63:1238–1243
Taki Y, Yamazaki Y, Shimura F, Yamada S, Umegaki K (2009) Time-dependent induction of hepatic cytochrome P450 enzyme activity and mRNA expression by bilobalide in rats. J Pharmacol Sci 109:459–462
Taki Y, Yokotani K, Yamada S, Shinozuka K, Kubota Y, Watanabe Y, Umegaki K (2012) Ginkgo biloba extract attenuates warfarin-mediated anticoagulation through induction of hepatic cytochrome P450 enzymes by bilobalide in mice. Phytomedicine 19:177–182
Uchida S, Yamada H, Li XD, Maruyama S, Ohmori Y, Oki T, Watanabe H, Umegaki K, Ohashi K, Yamada S (2006) Effects of ginkgo biloba extract on pharmacokinetics and pharmacodynamics of tolbutamide and midazolam in healthy volunteers. J Clin Pharmacol 46:1290–1298
Ulbricht C, Chao W, Costa D, Rusie-Seamon E, Weissner W, Woods J (2008) Clinical evidence of herb-drug interactions: a systematic review by the natural standard research collaboration. Curr Drug Metab 9:1063–1120
Umegaki K, Saito K, Kubota Y, Sanada H, Yamada K, Shinozuka K (2002) Ginkgo biloba extract markedly induces pentoxyresorufin O-dealkylase activity in rats. Jpn J Pharmacol 90:345–351
Umegaki K, Taki Y, Endoh K, Taku K, Tanabe H, Shinozuka K, Sugiyama T (2007) Bilobalide in Ginkgo biloba extract is a major substance inducing hepatic CYPs. J Pharm Pharmacol 59:871–877
Virgona N, Yokotani K, Yamazaki Y, Shimura F, Chiba T, Taki Y, Yamada S, Shinozuka K, Murata M, Umegaki K (2012) Coleus forskohlii extract induces hepatic cytochrome P450 enzymes in mice. Food Chem Toxicol 50:750–755
Virgona N, Taki Y, Yamada S, Umegaki K (2012) Dietary Coleus forskohlii extract generates dose-related hepatotoxicity in mice. J Appl Toxicol 33(9):924–932
Wang X, Wolkoff AW, Morris ME (2005) Flavonoids as a novel class of human organic anion-transporting polypeptide OATP1B1 (OATP-C) modulators. Drug Metab Dispos 33:1666–1672
Werba JP, Giroli M, Cavalca V, Nava MC, Tremoli E, Dal Bo L (2008) The effect of green tea on simvastatin tolerability. Ann Intern Med 149:286–287
Wilkinson GR (2005) Drug metabolism and variability among patients in drug response. N Engl J Med 352:2211–2221
Williamson EM (2001) Synergy and other interactions in phytomedicines. Phytomedicine 8:401–409
Xie R, Hammarlund-Udenaes M, De Boer AG, De Lange EC (1999) The role of P-glycoprotein in blood–brain barrier transport of morphine: transcortical microdialysis studies in mdr1a (−/−) and mdr1a (+/+) mice. Br J Pharmacol 128:563–568
Yang CS, Wang X, Lu G, Picinich SC (2009) Cancer prevention by tea: animal studies, molecular mechanisms and human relevance. Nat Rev Cancer 9:429–439
Yang SP, Raner GM (2005) Cytochrome P450 expression and activities in human tongue cells and their modulation by green tea extract. Toxicol Appl Pharmacol 202:140–150
Yeung EY, Sueyoshi T, Negishi M, Chang TK (2008) Identification of Ginkgo biloba as a novel activator of pregnane X receptor. Drug Metab Dispos 36:2270–2276
Yokotani K, Chiba T, Sato Y, Kubota Y, Watanabe Y, Murata M, Umegaki K (2012) Estimation of components which induce mice cytochrome P-450 in coleus forskohlii extract. Pharmacometrics 82:67–73
Yokotani K, Chiba T, Sato Y, Taki Y, Yamada S, Shinozuka K, Murata M, Umegaki K (2012) Hepatic cytochrome P450 mediates interaction between warfarin and Coleus forskohlii extract in vivo and in vitro. J Pharm Pharmacol 64:1793–1801
Yokotani K, Chiba T, Sato Y, Nakanishi T, Murata M, Umegaki K (2013) Influence of dietary macronutrients on induction of hepatic drug metabolizing enzymes by coleus forskohlii extract in mice. J Nutr Sci Vitaminol 59:37–44
Zadoyan G, Rokitta D, Klement S, Dienel A, Hoerr R, Gramatte T, Fuhr U (2012) Effect of Ginkgo biloba special extract EGb 761(R) on human cytochrome P450 activity: a cocktail interaction study in healthy volunteers. Eur J Clin Pharmacol 68:553–560
Zhang S, Yang X, Morris ME (2004) Flavonoids are inhibitors of breast cancer resistance protein (ABCG2)-mediated transport. Mol Pharmacol 65:1208–1216
Zhao LZ, Huang M, Chen J, Ee PL, Chan E, Duan W, Guan YY, Hong YH, Chen X, Zhou S (2006) Induction of propranolol metabolism by Ginkgo biloba extract EGb 761 in rats. Curr Drug Metab 7:577–587
Zhu BT, Taneja N, Loder DP, Balentine DA, Conney AH (1998) Effects of tea polyphenols and flavonoids on liver microsomal glucuronidation of estradiol and estrone. J Steroid Biochem Mol Biol 64:207–215
Zong J, Pollack GM (2000) Morphine antinociception is enhanced in mdr1a gene-deficient mice. Pharm Res 17:749–753
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 American Association of Pharmaceutical Scientists
About this chapter
Cite this chapter
Yamada, S., Misaka, S., Ito, Y., Watanabe, H., Umegaki, K. (2014). Effects of Natural Products on Pharmacokinetics and Pharmacodynamics of Drugs. In: Folkerts, G., Garssen, J. (eds) Pharma-Nutrition. AAPS Advances in the Pharmaceutical Sciences Series, vol 12. Springer, Cham. https://doi.org/10.1007/978-3-319-06151-1_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-06151-1_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-06150-4
Online ISBN: 978-3-319-06151-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)