Abstract
Social anxiety disorder (SAD) is characterized by a marked and persistent fear of being scrutinized by others in social situations. It is highly prevalent and follows a chronic course for many affected if untreated. Treatment with cognitive behavior therapy (CBT) has been shown to be highly effective for SAD with responder rates of 50–75 %. For more than a decade, Internet-based CBT (ICBT) has been researched and evidence has been provided by four independent research groups. In essence, most forms of ICBT for SAD can generally be described as therapist-guided Internet-based self-help CBT where a named therapist guides the client through the treatment. The treatments are manualized and highly structured comprising 5–15 modules or lessons, which are the equivalent of sessions in face-to-face CBT. The existing treatments for SAD all have vital features in common including that they are based in CBT, comprise the same interventions as have been shown to be effective in face-to-face CBT, have large amount of psychoeducational material, and use asynchronous text messages as the main communication between patient and therapist. ICBT for SAD has been proven to be effective in at least 16 randomized trials and found to be non-inferior to face-to-face CBT. A few studies suggest that ICBT is a cost-effective treatment. Since SAD is known to appear at an early age in most cases, one central future challenge is to increase the body of knowledge on ICBT for children and adolescents. For adults, ICBT for SAD is clearly an effective treatment and a promising option for increasing accessibility to evidence-based psychological treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Definition and Epidemiology
According to the DSM-IV, the main diagnostic feature of social anxiety disorder (SAD) is “a marked and persistent fear of one or more social or performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others (American Psychiatric Association 1994). The individual fears that he or she will act in a way (or show anxiety symptoms) that will be humiliating or embarrassing”. SAD is thus characterized by a fear of being negatively evaluated by others and the most commonly feared situation among persons with SAD is public speaking. A vast majority of affected individuals fear not just one but several social situations (Furmark et al. 1999; Ruscio et al. 2008). SAD was first viewed as a simple phobia, but several aspects of the disorder make it different compared to, for example, animal phobias. The individual with SAD not only experiences fear when in social situations but often also has high levels of anticipatory worry before entering these situations, which could increase the probability that the person avoids the social event all together or engages in safety behaviors (Clark and Wells 1995). These can be described as subtle avoidance behaviors, e.g., using anxiolytics or avoiding eye contact. After the social event, the individual with SAD often engages in postmortem processing, which means scrutinizing one’s own performance and paying close attention to actions that could have been negatively perceived by others (Clark and Wells 1995). As a way of recognizing the profound impact of SAD in terms of symptom presentation and aversive consequences, the term SAD – as a complement to social phobia – was introduced in DSM-III-R (Liebowitz et al. 2000). The diagnostic criteria for SAD have remained largely the same in DSM-5 (American Psychiatric Association 2013).
SAD is one of the most common anxiety disorders with 12-month prevalence estimates of 7–8 % in large-scale community-based studies (Kessler et al. 1994; Magee et al. 1996). A stable finding from epidemiological studies on SAD is that women have a higher risk of developing the disorder (Furmark 2002). Considering sample size and methodological strengths, it is likely that the best estimate is around 1.5:1 (Furmark 2002). SAD has an early onset, usually between 11 and 13 years of age, and it is uncommon to develop the disorder in adulthood (Wittchen and Fehm 2003; Beesdo et al. 2007). More than half of persons with SAD suffer from a comorbid psychiatric disorder, often an anxiety disorder, depression, or substance abuse (Chartier et al. 2003; Ruscio et al. 2008). As the debut of SAD often precedes that of the comorbid disorders, it has been suggested that SAD may play a causal role in the development of the latter disorders. SAD is associated with functional impairment in several life domains (Fehm et al. 2005). It leads to an increased risk of unemployment (Wittchen et al. 2000; Lampe et al. 2003; Bruch et al. 2003), lower academic attainment (Furmark et al. 1999; Davidson et al. 1993), reduced quality of life (Wittchen et al. 2000; Olatunji et al. 2007), and poorer somatic health (Dahl and Dahl 2010). In clinical samples, SAD rarely remits spontaneously but is chronic for a majority of patients if untreated (Yonkers et al. 2001).
Treatment of SAD
Among psychological treatments, cognitive behavior therapy (CBT) has the most empirical support. The two most well-researched treatments are cognitive behavior group therapy (CBGT) developed by Heimberg and coworkers (2002) and individual cognitive therapy (ICT) developed by Clark and coworkers (2003). These two treatments are relatively brief (about 12–16 weeks), based on similar CBT models of social anxiety and are aimed at breaking the vicious cycle between anxiety symptoms, catastrophic interpretations, attention to internal and external threat, safety behaviors, and avoidance behaviors. Common to both CBGT and ICT is the formulation of an individual conceptualization of the patient’s problem based on the CBT model. In addition, both treatments put a strong emphasis on weekly homework assignments and include exercises where exposure to social stimuli and cognitive restructuring are integrated, and finally, both entail relapse prevention. Of course, this means that both treatments are challenging for the patient as they require the patient to confront what he or she fears the most. There are however some differences between the treatments. In Heimberg’s CBGT, the main component is in-session exposure to feared social situations in combination with verbal cognitive restructuring where exposure is conducted within a largely habituational framework (Heimberg and Becker 2002). In ICT, reduction of social anxiety is promoted by getting patients to make predictions and test the predictions in behavior experiments in which safety behaviors are dropped and/or feared catastrophes are intentionally enacted. The treatment also includes exercises to demonstrate the adverse effects of self-focused attention and safety behaviors, training in externally focused attention, and video feedback to correct negative self-imagery (Clark et al. 2003). The empirical evidence for these two treatments is strong as they have been tested in at least 17 randomized controlled trials and have been shown to be superior to other psychological treatments and pill placebo (Ponniah and Hollon 2008). The magnitude of effects is generally large for these two treatments. There is some empirical data suggesting that ICT may be more effective than CBGT, which could perhaps be attributable to the slightly more complex procedures per se or that the individual format allows for a more tailored treatment. Approximately two out of three patients achieve clinically significant improvement, and long-term follow-up studies have demonstrated that these two treatments yield improvements that are sustained for at least 5 years (Heimberg et al. 1993; Mörtberg et al. 2011). One study showed that a combination of pharmacological treatment (phenelzine) and CBGT produced larger improvements than CBGT alone (Blanco et al. 2010). However, the small number of studies in this field does not allow any firm conclusions that combinatorial treatment is superior to monotherapy in the treatment of SAD (Hofmann et al. 2009).
Internet-Based Treatments for SAD
SAD is one of the clinical domains where research on Internet-based treatments has been most extensive during the last decade and is likely that SAD is the disorder for which this type of treatment has the strongest empirical support. Five independent research groups in Sweden, Switzerland, Spain, Australia, and the UK have developed and tested Internet-based cognitive behavior therapy (ICBT) for SAD. In essence, most forms of ICBT for SAD can generally be described as therapist-guided Internet-based self-help CBT where a named therapist guides the client through the treatment. Common to ICBT for many other disorders, the treatments are manualized and highly structured comprising 5–15 modules or lessons, which are the equivalent of sessions in face-to-face CBT. The existing treatments for SAD all have vital features in common including that they:
-
Are based on cognitive behavior therapy
-
Entail treatment components that have been shown to be effective in a face-to-face format, such as exposure
-
Have large amounts of psychoeducational material
-
Are 8–15 weeks long
-
Most often use asynchronous written text messages as the main communication form between therapist and patient
-
Have integrated worksheet and assessment systems in the Internet-based treatment platform
To some extent, it could be that ICBT is especially suitable for this patient group, and it has been suggested that the absence of face-to-face contact, which can be fear provoking for persons with SAD, might actually improve learning of the psychoeducational parts of the treatment (Hedman et al. 2014a). That is, learning the relatively complex treatment models and principles underlying the treatment may be easier if not done in a social context where the patient may feel that he or she is being evaluated by the therapist. In the following, a brief description of the five different ICBT treatments is presented.
The Swedish ICBT for SAD
One of the first therapist-guided ICBT treatments was developed by Andersson and coworkers (2006). This treatment is primarily based on Clark et al.’s individual cognitive treatment for SAD and thus comprises components such as behavior experiments, manipulation of safety behaviors, and attention training. It also entails exposure exercises and social skills training. The treatment is structurally based on 9–15 so-called modules, which are text chapters that correspond to therapy sessions and are designed to provide the patient with the same knowledge and tools as he or she would obtain in face-to-face CBT. Table 4.1 displays an example of the contents of modules in ICBT for SAD. To each module belongs a set of homework exercises and the patient is granted gradual access to the modules contingent on completion of homework exercises. The patient has access to an identified and personal therapist throughout the treatment and the contact is almost exclusively through written text messages. The patient also has access to a discussion forum where he or she anonymously can post messages to other patients that receive treatment. Generally, this treatment has few complex technical features, is heavily text based, and could essentially be described therapist-guided online bibliotherapy. Although most conducted studies have used on beforehand fixed modules, i.e., all participants regardless of symptom profiles have been exposed to the same modules, a more recent development has been to tailor the treatment content to the patient’s characteristics (e.g., Carlbring 2011a). This could, for example, be that a patient with SAD who has comorbid sleep difficulties is granted access to additional insomnia modules containing information about how to improve sleep.
The Swiss ICBT for SAD
The Swiss treatment, developed by Berger and coworkers (2009), is also explicitly based on individual cognitive therapy and therefore shares many basic components with the Swedish treatment program. The treatment is 10 weeks long and comprises five lessons, and the patient has access to a named therapist as well as to a discussion forum. In contrast to the Swedish program, this treatment includes more interactive features and is less like a self-help book. For instance, participants are asked to use online diaries or to make an exposure hierarchy online. In addition, it uses the video format as a phobic stimulus in the sense that patients are encouraged to conduct exposure exercises and behavior experiments in front of, e.g., a virtual video audience. The program does not only include a discussion forum but also other collaborative online group elements such as the possibility to anonymously share work sheets and diaries with other participants. The program can be used in an unguided and guided format (Berger et al. 2011) and in a tailored approach in which the self-help guide is individually tailored to comorbid other anxiety disorders (panic disorder with or without agoraphobia, generalized anxiety disorder) (Berger et al. 2014).
The Spanish ICBT for SAD
Botella and coworkers developed the first ICBT for SAD (Botella et al. 2000, 2004). This ICBT includes several components: psychoeducation, cognitive restructuring, attention training, and exposure. Figure 4.1 presents the structure and contents of the different modules of this ICBT. To each module belongs a set of homework exercises and the patient is granted gradual access to the module contingent on completion of homework exercises. The treatment can be fully automated; this means that potential patients go through an online self-report assessment and are granted access to treatment if predefined criteria for eligibility are met. In this case, the patient has no therapist contact but is asked to complete questions and is not allowed to go through the program if the answers indicate that he or she has not understood the main aspects of the treatment and/or if the level of anxiety confronting the feared situation has not decreased. In these cases, the patient is asked to look over the treatment material once more. It is possible also to deliver the program in a blended form, that is, the online program can be combined with therapist’s contact (by phone or face to face). The main component of the treatment is virtual exposure, and the program entails six different typical scenarios that evoke social anxiety in persons with SAD, e.g., “The class” or “The job interview.” For each scenario there is a set of video films that constitute the phobic stimulus and the patient is asked to conduct oral presentations in front of these video audiences. The program organizes a hierarchy created during the initial assessment, and the specific scenarios are presented based on levels of fear, progressing from those less feared to those more feared. The program provides different advice to users depending on their level of fear upon finishing the exposure, encourages the users to continue working, and congratulates them for their effort. The program also recommends completing daily homework assignments.
The Australian ICBT for SAD
Titov, Andrews, and coworkers have developed and tested an Internet-based treatment for SAD often referred to as The Shyness Program (Titov et al. 2008a). This ICBT for SAD is based on the previously developed CLIMATEGP online lessons for SAD. This treatment comprises six lessons over 10 weeks where the main components are psychoeducation about CBT and social anxiety, exposure exercises, and cognitive restructuring. The main message of each lesson is illustrated in part through a treatment story where a fictive person with SAD learns to overcome social anxiety through CBT. Structurally, the treatment is similar to the Swedish and Swiss treatments meaning that patients have access to an identified therapist who provide asynchronous written feedback on homework exercises. Integrated in the treatment is also an online discussion forum where patients can share experiences and provide support to each other anonymously.
The British ICBT for SAD
This type of ICBT for SAD (Stott et al. 2013) is fully based on the individual cognitive therapy developed by Clark and coworkers. It is designed to incorporate all central components of individual cognitive therapy while using less therapist time and has largely the same structure as the Swedish, Swiss, and Australian treatments. That is, the patient has email-like contact with a named therapist, the treatment is comprised of several Internet-based modules, and patients spend about the same time in treatment as in face-to-face treatment. Nine core modules are obligatory for all patients, but if the therapist judges it to be helpful, he or she can assign additional modules to the patient that address common obstacles in treatment or problem-specific aspects that may not be applicable for all persons with SAD. This treatment is relatively advanced from a technical view; it entails several psychoeducational video clips and uses web-cam linked communication. Recordings from webcam interactions are also used in video-feedback exercises where patients can learn to discriminate between self-perceptions and actual social performance. An instruction video describing the treatment is available on the following URL: http://youtu.be/rXXOOSkA0qg.
Studies on Internet-Based CBT for SAD
Independent researchers in different countries (Australia, Sweden, Switzerland, Spain, and United Kingdom) have tested several ICBT programs for SAD. The existing empirical evidence is quite strong with at least 16 conducted RCTs demonstrating the treatment’s efficacy. Data from a meta-analysis (Andrews et al. 2010) showed that the overall effect size of ICBT for SAD compared to control group was large (g = 0.92, 95 % CI 0.74–1.09), and the results indicate both short- and long-term improvements. Furthermore, the findings showed that treatment adherence was good and that patients were satisfied with the treatment despite the relatively limited therapist contact. ICBT appears to be a promising way to overcome treatment barriers for persons suffering from SAD. Here we present the most relevant research conducted in the field of ICBT for SAD.
Efficacy and Long-Term Outcomes
In a case study using an ICBT program for SAD, Botella and coworkers in Spain found initial empirical support for the treatment efficacy (Botella et al. 2004). This same program was further tested in a series of case studies (Botella et al. 2007) presenting efficacy data from 12 social phobia patients with good results. The Swedish team (Carlbring et al. 2006) published an open trial in which 26 participants were treated with an ICBT program plus weekly therapist contact via email. The results showed that the participants improved significantly on all outcomes and the treatment gains were maintained or improved at the 6-month follow-up. All these studies provided preliminary evidence supporting the use of ICBT programs for people diagnosed with SAD.
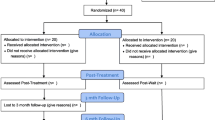
Table 4.2 presents an overview of randomized clinical trials investigating the effect of Internet-based CBT. Andersson and coworkers published the first RCT (Andersson et al. 2006) on the efficacy of ICBT for SAD which was then followed by several trials with the same ICBT program (see below). In this first RCT, 64 participants were randomly assigned to the ICBT program supported by email contact of a named therapist plus two in vivo exposure sessions in a group format, or a waiting list control condition. The results revealed that the ICBT condition was significantly more efficacious than the control condition with treatment gains maintained at 1-year follow-up. The authors also published results on long-term outcome (30-month follow-up) which suggested that the long-term effects seen in previous live treatment CBT for SAD trials also occur in Internet-delivered treatment (Carlbring et al. 2009). Using largely the same treatment but without in vivo exposure sessions, Hedman and coworkers found that treatment gains were sustained 5 years after treatment (Hedman et al. 2011a). The efficacy of ICBT for SAD has also been demonstrated in several trials conducted in Australia. Titov and colleagues (2008b) carried out an RCT in which 105 participants with SAD were randomly assigned to an ICBT program or to a waiting list control group. The results showed significant differences between treatment and waiting list participants. As in the trials conducted in Sweden, effects were comparable with those obtained in face-to-face treatment. In Switzerland, Berger and coworkers conducted an RCT (Berger et al. 2009) including 52 individuals with SAD who were randomly assigned either to an ICBT program with minimal therapist contact via email or to a waiting list control group. Significant differences between the two groups were found at posttreatment on all primary outcome measures. The results provided additional support to the hypothesis that ICBT interventions with minimal therapist contact are a promising treatment for SAD. Gallego, Emmelkamp, van der Kooj, and Mees (2011) presented an RCT in which the effects of a Dutch version of the Spanish ICBT for SAD were investigated. Forty-one participants suffering from SAD were randomly assigned to either the ICBT program combined with minimal therapist contact via email or a waiting list control group. The group treated with ICBT was significantly improved from pretest to posttest on all SAD measures, and this condition was significantly more effective than the control group. This study as well as a pilot study of the British team (Stott et al. 2013) provides additional evidence for the efficacy of ICBT for SAD and shows that an ICBT program can be adapted and used with maintained effects in different cultural frameworks.
ICBT Compared to Face-to-Face CBT
ICBT has also been compared to traditional face-to-face CBT for SAD. Hedman et al. (2011b) carried out an RCT to investigate whether ICBT was at least as effective as traditional CBT group therapy when treatments are delivered in a psychiatric setting. One hundred and twenty-six individuals with SAD were randomly assigned to one of these two treatment conditions. The results revealed that both conditions made large and similar improvements and it was concluded that ICBT can be as effective as traditional CBT group therapy in the treatment of SAD. Botella and coworkers (2010) conducted an RCT in which 127 participants with a diagnosis of SAD were randomly assigned to three experimental conditions: an ICBT self-administered program, the same CBT treatment applied by a therapist, and a waiting list control group. The data showed that both treatment formats (self-administered and therapist administered) were equally efficacious and superior to the waiting list condition. The treatment gains were maintained at 1-year follow-up. In a study conducted in Australia, Titov et al. (Andrews et al. 2011b) also compared the effectiveness of ICBT with face-to-face CBT group therapy for SAD in an RCT including 75 participants. Both treatment formats yielded significant improvements and there were no significant differences between them. All these results provide evidence showing that both forms of delivering the treatment (face-to-face CBT and ICBT) can be equally effective while the difference in therapist time required is substantial. The results are also consistent with previous findings obtained in ICBT for panic disorder (e.g., Carlbring et al. 2005).
Studies Investigating Therapist Support
An important line of research has focused on studying the degree of support and guidance needed during the treatment. Tillfors and coworkers (Tillfors et al. 2008) carried out an RCT specifically targeting university students and investigating whether the ICBT self-help program would be more effective if five live group exposure sessions were added. Thirty-eight participants meeting the diagnostic of SAD were randomized into two different treatment groups: ICBT combined with five group exposure sessions or the same ICBT program alone. Both treatment conditions showed significant improvements from pre- to posttest and from pretest to 1-year follow-up on all measured SAD dimensions. The results suggest that adding group exposure sessions did not improve the outcome significantly.
Berger and coworkers (Berger et al. 2011) studied the role and necessity of therapist guidance in an RCT comparing the benefits of a 10-week unguided treatment, with the same intervention complemented with minimal weekly therapist support via email. The study included a third condition, in which the level of support was flexibly stepped up from no support to email or telephone support on demand of the participants. Eighty-one individuals with SAD were randomly assigned to one of the three conditions. Results showed significant improvements in all three treatment groups and no differences between the conditions regarding clinical outcomes, dropout rates, and adherence to treatment. These results provided additional evidence showing that ICBT for SAD is an effective treatment option when therapist guidance is provided but also when no support is provided.
The Australian team also contributed to this line of research carrying out several RCTs. For instance, in a trial by Titov and coworkers (2008c), 98 participants suffering from SAD were randomly assigned to a clinician-assisted ICBT program (email contact with a therapist and participation in an online discussion forum), the same ICBT program but without contact with a clinician, or to a wait list control group. The therapist-guided condition was superior to the self-guided condition, but a subgroup of participants who completed the program benefited considerably from the latter. In a subsequent study, Titov and colleagues (2009a) compared the self-guided treatment with a self-guided plus weekly telephone reminder condition in which participants were called once a week by a research assistant. Results showed that adherence and outcome were better in the condition that included reminders.
Overall, results on unguided treatments for SAD are still inconclusive. However, it is quite surprising that some studies (Berger et al. 2011), including a trial by Furmark and coworkers (Furmark et al. 2009b) in which an unguided treatment for SAD delivered in the form of bibliotherapy with no therapist support was as efficacious as guided ICBT, found no difference between unguided and guided treatments. Data from meta-analyses on ICBT for several disorders indicate better results of guided versus unguided treatments regarding improvements and dropout rates (Richards and Richardson 2012; Spek et al. 2007). It may be that guidance is less important in ICBT for SAD than for other disorders such as depression. However, it may also be that unguided treatments only achieve good therapeutic outcome under specific conditions. In the two studies mentioned above, a proper diagnosis was established and there was a contact with a clinician or the study team during the diagnostic phase. In one uncontrolled study in which there was no contact at all with the researchers, dropout was substantial (Klein et al. 2011). In another study in which the effects of clinician contact in the diagnostic phase was evaluated in an unguided treatment, participation in the structured diagnostic interview did not influence primary outcome but had a beneficial effect on adherence and secondary outcomes (Boettcher et al. 2012a). Clearly, more research is needed with regard to the role of support and contact before and during ICBT for SAD.
Another line of research that addresses questions on the role of support is related to therapists in guided ICBT. Does it matter who provides the support? Titov and coworkers (2009b) found that ICBT for SAD with guidance given by non-clinicians resulted in good outcomes. Andersson and coworkers (Andersson et al. 2012) evaluated the role of therapist experience and found no differences between experienced therapists and therapists with no previous experience in ICBT. However, inexperienced therapists needed more time to provide guidance than experienced therapists. Overall, the findings suggest that ICBT does not require experienced therapists to be effective which is plausible given that (a) the treatment is highly structured and (b) the main component is a self-help program which also incorporates clinical expertise. In addition, it is important to note that non-clinicians and inexperienced therapists were under careful clinical supervision in all studies that included support by inexperienced therapists/coaches.
Another issue that has been examined is the possible role of including additional strategies for enhancing clinical results. For instance, Titov and coworkers (2010a) added motivational enhancement strategies to their ICBT program (understanding and exploring ambivalence about change, enhancing self-efficacy, etc.). Results of an RCT showed that ICBT with or without this additional component was efficacious. Although more participants in the motivational treatment condition completed the treatment lessons (75 % versus 56 %, respectively), no differences between the two conditions were found at posttreatment and at 3-month follow-up.
It is also possible that adding collaborative online group elements such as discussion groups could enhance treatment effects. There is at least indirect evidence that integrating collaborative elements into ICBT could be beneficial. Titov and colleagues could improve small within-group effect sizes for unguided ICBT for SAD (Titov et al. 2008c) by adding a clinician-moderated online discussion forum in a subsequent study. As mentioned previously, in the study by Furmark and coworkers (2009a), an intervention consisting of a self-help guide delivered in the form of bibliotherapy with no therapist support but with access to an online discussion forum was as effective as guided ICBT. Moreover, qualitative analyses of the content of discussions in integrated forums showed that therapeutic mechanisms of change may come into play that are known from research on group psychotherapies (e.g., normalization, altruism, instillation of hope, development of socializing techniques, imitative behavior, cohesiveness (Berger 2011)). However, since to the best of our knowledge there are no studies directly comparing the same internet-based treatment with and without collaborative elements, it is not possible to draw firm conclusions on the effects of integrated online discussion boards.
Addressing Comorbidity in ICBT for SAD
Still another arena of research explores whether addressing the high comorbidity rates in patients with SAD is beneficial. This was done with unified transdiagnostic treatments (Titov et al. 2010b, 2011; Johnston et al. 2011) and tailored approaches in which the self-help guide is individually tailored to the symptom profile of a patient by providing modules on comorbid problems and disorders such as mood disorders, other anxiety disorders, or insomnia (Berger et al. 2014; Carlbring et al. 2011b; Andersson et al. 2011). Both approaches seem to be effective, but it is not clear whether patients with SAD would benefit more from a transdiagnostic or tailored approach than from a treatment that targets SAD only. There is one study directly comparing a tailored versus standardized disorder-specific approach finding no differences between the two approaches, but this trial included patients with various anxiety disorders and levels of comorbidity (Berger et al. 2014). It is possible that a tailored approach is especially beneficial for subgroups of SAD patients such as individuals with high levels of comorbidity. This could not be tested in the trial mentioned above as the subgroup of SAD patients with high comorbidity rates was too small for appropriate subgroup analyses (Berger et al. 2014). Indeed, in a controlled trial comparing standard ICBT versus a tailored intervention in depression with comorbid problems, it was found that the tailored treatment was better suited to handle more severe disorders (Johansson et al. 2012).
Predictors and Mediators
As shown before, guided and unguided ICBT have shown to be effective treatments and may increase access to evidence-based psychological treatment for SAD. However, as at least a third of patients do not respond sufficiently to treatment, it is important to identify specific predictors and mediators that can guide the clinician in making treatment decisions. Knowledge on predictors and mediators can lead to more effective implementation of ICBT and ultimately to a larger proportion of patients that respond to treatment (Kraemer et al. 2002).
In their RCT comparing ICBT with group therapy, Hedman et al. (2012a) investigated possible clinical and genetic predictors and moderators of outcome. The results showed that the most stable predictors of better treatment outcomes were working full time, having children, suffering from less depressive symptoms, treatment expectancy and credibility, and better adherence to treatment. There were no significant results regarding gene polymorphisms that have also been tested. As for moderators, it was found that lower levels of comorbid anxiety and depression were associated with a better treatment response in the ICBT condition but not in the face-to-face CBT group therapy. Nordgreen et al. (2012) evaluated a series of pretreatment symptoms (including baseline SAD symptoms and comorbid depressive symptoms) and program factors (e.g., credibility and adherence) as potential predictors of treatment adherence and outcome in the context of guided and unguided self-help for SAD. The study included 245 patients who received either guided or unguided self-help for SAD. The results were in the same line than those obtained in the face-to-face CBT literature treatment for SAD (Eskildsen et al. 2010), namely, the intensity of SAD symptoms before treatment predicted treatment outcomes in both unguided and guided ICBT conditions, and the results were similar, regardless of whether participants had a diagnosis of generalized or specific SAD. The findings partly contrasted to those in the study by Hedman et al. (2012a) as treatment expectancy and credibility was unrelated to outcome. Nordgreen et al. (2012) also investigated predictors of adherence and found that in the guided ICBT condition, neither pretreatment symptoms nor credibility predicted treatment adherence. For the unguided ICBT group, higher credibility ratings of the treatment program were associated with increased treatment adherence with no group differences in credibility ratings between guided and unguided ICBT. That is, patients in the unguided intervention who perceived the program as a highly credible treatment, showing high expectations, had similar adherence rates as patients in the guided ICBT. Taking into account their findings, Nordgreen and coworkers (2012) recommended to provide the patients information about the potential effects of guided and unguided ICBT for SAD in order to promote positive expectations. In this same line, Boettcher and colleagues (2013a) hypothesized the relevance of patient expectations as an important mechanism to explain the change. They conducted a study including 109 participants that went through an unguided ICBT program for SAD. The results confirmed that positive outcome expectations were a significant predictor of change and treatment adherence, and this effect was mediated by early symptom change. These authors concluded that patient expectations could be a useful factor for guiding clinical decisions about possible treatments for SAD.
Globally, the results of all these studies highlight the importance of conducting further research to examine the predictors and mediators of outcomes in various clinical settings and populations to guide future dissemination efforts in ICBT for SAD.
Case Description
Hanna, 32 years old, suffers from social fears since childhood. She has become aware of the Internet-based guided self-help treatment, which is provided by the University of Bern in Switzerland, through a newspaper article. Hanna gets in touch by email and is then asked to answer different online questionnaires about anxiety, depression, well-being, and other aspects. From the answers, it becomes apparent that Hanna lives alone, has no children, has never been in psychotherapy, is not suicidal, and exceeds the cutoff criteria for SAD on various social phobia questionnaires. In a following diagnostic interview by phone, the diagnosis of SAD is confirmed. During the phone call, Hanna says that she is a teacher and lives in a village in the Swiss mountains where no psychotherapeutic treatment is available. She has decided to take advantage of the Internet-based approach because she does not want to drive to the next town for traditional therapy and is also afraid that someone in the small village would find out that she – the small village teacher – is in psychotherapy.
Hanna receives access to the first session of the Internet-based password-protected program, and she is told that a psychologist named Simon Weber will support her during her work with the program by a secure integrated email system. The psychologist will write her a feedback on her progress once a week and will be at her disposal if there are any questions. In a therapist cockpit, in which therapists/coaches can track participants’ program use and symptomatic progress, Simon Weber observes that Hanna is working through the first self-help session, which contains many psychoeducational elements and an online anxiety diary. In his first weekly feedback, he writes in the integrated email system: “Dear Hanna, I see that you have worked through the first session. That’s great! Your entries in the anxiety diary are very understandable. You describe a teacher’s meeting in which you sat quietly in the corner and had thoughts like ‘I won’t be able to say anything because I’m so nervous’. These are behaviours and thoughts which are very typical for people suffering from social anxiety. We can assume that this program fits very well to your needs. In the course of the program we will work towards changing the behaviours and thoughts you have noted. You may start with the second session now.”
Hanna instantly writes back that she has read the first session with great interest and is now very motivated to start with the second session. In this second session, she is asked to develop an individual explanatory model of her social anxieties on the basis of the cognitive-behavior model. Hanna writes that she was teased in primary school because she could not pronounce the letter R properly. Later her teachers made a fool of her in front of the class. Furthermore, she recognizes several of the described safety behaviors. Before parent-teacher conferences, she always takes a sedative tablet and practices her statements with great care. In these situations, she also focuses her attention very strongly toward herself in hopes of controlling bodily symptoms such as blushing. Now she understands that this behavior only reinforces and preserves her fears.
After a short and motivating feedback from the psychologist, Hanna begins with the third session. She is instructed to question her negative thoughts that she has noted in the anxiety diary and to find more realistic thoughts. Hanna seems to succeed in this task. However, in a message to the psychologist, she writes that her realistic thoughts collapse like a house of cards and the negative thoughts take over in real-life situations. The psychologist reassures her that she has already done a great job by not avoiding the situation and that it needs time and effort to change the negative thought patterns she has developed over the years.
In the fourth session, Hanna is instructed to conduct various exercises on self-focused attention in which she learns to focus her attention toward the task and the environment and not toward herself. In a message to the psychologist, Hanna writes that the exercises have helped her a lot because she could apply all that she has learned in a social small-talk situation in which she succeeded to focus on the environment and not on herself. She writes that the exercise had broadened her horizon and that she had not felt so helpless toward her fears anymore.
In session five, the exposure rationale and a diary are introduced in which fear-evoking situations are noted. Hanna is told that it is especially important that she write down situations that are important to her in a sense that they hinder her from living the life she wants and also that it should be likely to expose to the situations within a few weeks. The expected level of anxiety and safety behavior, which should be reduced, are noted in the diary. During the 10-week intervention, Hanna notes a total of 30 situations of which she finally exposes herself to 24. In most cases after experiencing the situation, she reports that the actual fear was much less than anticipated. From the entries, it becomes evident that with time she finds it easier to seek social situations and to refrain from safety behaviors.
After 10 weeks, Hanna does not fulfill the criteria of SAD anymore which becomes clear in a final diagnostic interview. The same pattern of improvement emerges in different disorder-specific questionnaires. Hanna writes a concluding message to her therapist: “I can only say that I am doing well. The social anxiety symptoms bother me considerably less and I hope that it will stay that way. I have started the school year probably just as motivated as my new first graders and I also enjoy my free time. I reread all the messages we sent each other and you deserve a huge compliment on your work! You and the program have accompanied me competently on a piece of my journey. During that time I always felt as though I was in good hands. I could venture on things that I had remained silent for years. Thank you so much.” In a 6-month follow-up, it becomes apparent that the positive change has been maintained.
Cost-Effectiveness
SAD is associated with a great individual burden (Stein and Stein 2008; Kessler et al. 2012) and the majority of patients with SAD also suffer from other comorbid mental disorders (e.g., depression, other anxiety disorders, or substance abuse) (Fehm et al. 2005; Lipsitz and Schneier 2000). Besides the suffering of the affected individuals, SAD is associated with an important economic burden for the society in terms of direct and indirect costs (Stuhldreher et al. 2014). Also, this condition is characterized by an increased risk of unemployment and disability; the annual societal costs of SAD have been estimated to more than $350 million per 1 million inhabitants (Hedman et al. 2014b). However, while costs incurred by healthcare utilization of patients suffering SAD (direct costs) are rather low, the societal burden resulting from lost productivity (indirect costs) is considerable. This might indicate that most patients had not sought for sufficient treatment yet (Stuhldreher et al. 2014).
As noted above, guided ICBT has shown to be a promising treatment for SAD. In addition, ICBT has the potential to dramatically increase availability of traditional face-to-face CBT for SAD (Hedman et al. 2012b). However, a key question before the dissemination of ICBT programs can be massively recommended is to know more about their health economic effects. Studies on the cost-effectiveness of SAD treatment are scarce. In fact, Lewis, Pearce, and Bisson (2012) carried out a systematic review to determine the efficacy and cost-effectiveness of self-help interventions for anxiety disorders. The results showed that self-help interventions appear to be an effective treatment for individuals diagnosed with SAD, but it was not possible to conclude anything about cost-effectiveness because none of the studies included in the review conducted a concurrent economic evaluation of the self-help intervention. Here we will try to summarize the most important contributions on cost-effectiveness of ICBT for SAD.
Titov and coworkers (2009d) carried out a study trying to determine cost-effectiveness of an ICBT program for SAD. One hundred and ninety-three participants were randomly assigned to an ICBT program or a waiting list condition. Cost-effectiveness was calculated to determine the cost per year gained living with disability (YLD). The results showed better results in the ICBT group treatment. The authors concluded that the ICBT program appears to be cost-effective. However, an important limitation of this study was that the effect sizes and estimates of staff time were derived from published results of a benchmarking study of face-to-face group treatment for SAD (McEvoy 2007).
In their RCT comparing ICBT with face-to-face group CBT, Hedman et al. (2011c) conducted the first prospective RCT investigating the cost-effectiveness of ICBT from a societal perspective; that is, both direct and indirect costs were analyzed. Results revealed that the total costs were significantly reduced in both treatment conditions. Furthermore, both treatments were equivalent in reducing SAD symptoms and gross total costs. The authors concluded that both treatments are useful in reducing societal costs for SAD, but ICBT can be considered more cost-effective than CBGT due to lower intervention costs regarding therapist time required. On average, in ICBT, the therapist spent 5.5 min weekly per patient; in CBGT, the corresponding estimate was 50 min (2.5 h sessions with two therapists and six patients). Recently, the same group presented the 4-year follow-up data (Hedman et al. 2014b). Results revealed that, at long term, ICBT for SAD is as effective as CBGT and that the interventions have similar longer-term health economic effects.
Hedman and coworkers (2012b) also conducted a systematic review on the efficacy and cost-effectiveness of ICBT. The results showed large effects for ICBT, and combining this data with the limited therapist time required by ICBT, the authors suggested that this kind of intervention may be highly cost-effective. However, it is important to underscore that of the 108 studies included in the review, only eight provided data regarding cost-effectiveness, and only two of these studies were focused on SAD.
Finally, Nordgreen et al. (2014) conducted an RCT to investigate the effectiveness and cost-effectiveness of ICBT when tailoring the treatment to address comorbidities and preferences for primary-care patients with a principal diagnosis of anxiety disorder. The authors were interested in studying whether treatment could lower direct and indirect societal costs in this population. The trial included one hundred participants that were recruited through their primary-care contact and randomized to an ICBT condition with scheduled guidance (7–10 weekly individually assigned modules guided by online therapists) or an active waiting list control group (“attention control”). Thirty-two percent of participants in both groups had a primary diagnosis of SAD. Costs were assessed at pretreatment, posttreatment, and at 12-month follow-up. The control condition was crossed over to treatment after posttreatment, then between-group comparisons were made only for the posttreatment data. The cost analysis results showed significant reduction of total costs for the tailored ICBT group. The results were maintained at 1-year follow-up, and the incremental cost-effectiveness ratio favored tailored ICBT compared to the control group. That is, from a societal perspective, the treatment constitutes a win-win situation as patients make large improvements while society makes a substantial net reduction of costs. This study provides evidence of cost savings without compromising clinical effectiveness. Given that evidence-based psychological treatments often are lacking in primary care, this kind of intervention may be an excellent treatment alternative.
In summary, it is possible to conclude that although the studies on cost-effectiveness of SAD are scarce, the results are quite encouraging. The available data show that ICBT is a cost-effective and well-established alternative to traditional CBT for SAD. However, research is needed to further evaluate the long-term cost-effectiveness of SAD treatment.
Clinical Implementation and Dissemination
Most of the studies mentioned above are efficacy trials conducted under controlled conditions with participants recruited via advertisement. There are, however, at least three studies examining the effectiveness of ICBT for SAD delivered in regular clinical services: one larger study conducted in a regular clinic in Stockholm, in which ICBT is delivered regularly to patients from the Stockholm county region (Hedman et al. 2011c), and two smaller studies conducted with patients referred to an anxiety disorder clinic in Australia (Andrews et al. 2011b; Aydos et al. 2009). The results of these studies, but also clinical experience and unpublished findings from the clinics mentioned above, show that the promising effects found in efficacy trials can be replicated in routine clinical practice.
However, the small number of studies and involved clinics also illustrates that ICBT for SAD is not yet implemented into clinical services on a larger scale. This may change in the future since data on aspects that are important to consider in the dissemination of a treatment such as patient preferences and cost-effectiveness may support efforts for the sustained implementation: Hedman and colleagues (2011c) as well as Andrews and colleagues (2011b) report that about half of the patients treated in a regular clinical setting prefer ICBT over face-to-face therapy. Moreover, and as described above, ICBT for SAD has been shown to be more cost-effective when compared with a cognitive behavior group therapy, mainly because ICBT was associated with less treatment costs (Hedman et al. 2011c). Of course, one of the strongest arguments for implementation on a larger scale is that the body of knowledge indicates that ICBT increases accessibility by a factor of four while producing large improvement in social anxiety.
As in ICBT for other conditions, the clinical implementation may be hindered by negative clinician attitudes toward Internet-based interventions (Mohr et al. 2010). Regarding ICBT for SAD, it may be especially important to inform and educate clinicians about these interventions because it is not obvious that ICBT should work for patients with social phobia. Indeed, it has been found that persons with social phobia do use the Internet extensively (Erwin et al. 2004), and it could be argued that ICBT reinforces their avoidance of contact with people. It is important to understand that Internet interventions do not direct patients to stay at home in front of their computer, but encourage participants to conduct real-life exposures. Our experience is that many patients manage to seek outside exposure with the guidance of a self-help program and the limited support of a clinician.
Finally, it is important to note that the implementation into routine clinical practice is only one pathway through which ICBT can and should be disseminated. Given that treatment rates among individuals suffering from SAD are particularly low (Kessler 2003), presumably also because of the increased fear and embarrassment in social situations, the development of low-threshold services providing direct online access to evidence-based ICBT for SAD should also be considered. However, such services should also include good referral methods to traditional treatments when ICBT does not result in sufficient improvement.
Discussion and Future Challenges
SAD is one of the most researched disorders in field of ICBT. More than 20 studies have consistently produced outcomes that are in line with results found in studies on face-to-face CBT, making ICBT one of the most evidence-based treatments for SAD. Effects tend to be stable over long-term follow-up, and there are indications that ICBT also works under clinically representative conditions.
On the basis of this extensive evidence, research on ICBT for SAD has already moved beyond a legitimation phase, i.e., research that basically addresses the question whether a treatment works. There is already a considerable amount of research on questions such as “What works better?,” though results are not always conclusive. For example, the available evidence does not clearly answer important questions regarding the role of therapist support. More research is needed to establish the type and amount of support that is optimal in ICBT for SAD, and it should be underscored that power has been rather limited in the studies investigating the role of the therapist.
Further research regarding “What works better in IBCT for SAD” is important since a considerable number of patients do not benefit or recover fully from traditional or Internet-based treatments for SAD (Heimberg et al. 1993; Boettcher et al. 2013b). Because studies on Internet interventions can be conducted faster and more efficiently than trials on face-to-face treatments, it is likely that research on ICBT for SAD will also contribute to the overall development of new or optimized interventions for SAD in the future.
Another way of optimizing treatments for SAD is to understand better for whom and how treatments work. As outlined above, research on predictors of ICBT for SAD is still rather scarce and few findings are stable across studies. The only finding that seems to be relatively consistent is that baseline social anxiety levels and patient expectations are related to outcome. Future directions in this line of research should also be to take advantage of the fact that ICBT confers the possibility to easily monitor patients’ behavior. Assessing early process predictors, such as program usage, could be used to inform therapeutic decisions on an ongoing basis.
More research is also necessary regarding moderators of outcome in face-to-face therapy versus ICBT because it is likely that patients may be more or less suitable for either format. As described above, it may be that patients with comorbid general anxiety and depression are somewhat more suitable for face-to-face CBT, but results need to be replicated before any strong clinical recommendations can be made concerning when a patient should receive ICBT and when face-to-face CBT is preferable.
When it comes to treatment mechanisms, it is likely that ICBT partly achieve its effects through the same mechanisms as face-to-face CBT. But there may also be working mechanisms of change that are unique or realized to a larger extent in Internet interventions. For instance, there are indications that in comparison with usual care, web-based interventions may have a positive effect on patient empowerment, self-efficacy, and mastery (Samoocha et al. 2010). This is plausible since ICBT aims at improving self-management and self-help capabilities. Another aspect previously mentioned is that especially SAD patients may be more relaxed when learning about their condition at home in a “safe” environment. Thus, the increase of knowledge about SAD through psychoeducation may be larger in Internet-based than face-to-face treatments and may play a more important role in ICBT. While there is no data to support this notion, there is at least one study showing that knowledge about SAD increased during ICBT, and that knowledge gain was significantly, although modestly, associated with outcome (Andersson et al. 2012).
Overall, ICBT for SAD is clearly an effective treatment and a promising treatment option for increasing accessibility to evidence-based psychological treatment. Since SAD is known to appear at an early age in most cases, one central future challenge is to increase the body of knowledge on ICBT for children and adolescents. Blended treatments combining face-to-face sessions with internet-based interventions should also be considered and researched in the future. And finally, more research is needed on how Internet-based treatments work and for whom they are indicated.
References
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders: DSM-IV, 4th edn. American Psychiatric Association, Washington
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Arlington
Andersson G, Carlbring P, Holmström A, Sparthan E, Furmark T, Nilsson-Ihrfelt E, Buhrman M, Ekselius L (2006) Internet-based self-help with therapist feedback and in vivo group exposure for social phobia: a randomized controlled trial. J Consult Clin Psychol 74:677–686
Andersson G, Estling F, Jakobsson E, Cuijpers P, Carlbring P (2011) Can the patient decide which modules to endorse? An open trial of tailored internet treatment of anxiety disorders. Cogn Behav Ther [Research Support, Non-U.S. Gov’t] 40:57–64
Andersson G, Carlbring P, Furmark T, Group SOFIER (2012) Therapist experience and knowledge acquisition in internet-delivered CBT for social anxiety disorder: a randomized controlled trial. PLoS One [Randomized Controlled Trial Research Support, Non-U.S. Gov’t] 7:e37411
Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N (2010) Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One 5, e13196
Andrews G, Davies M, Titov N (2011b) Effectiveness randomized controlled trial of face to face versus internet cognitive behaviour therapy for social phobia. Aust N Z J Psychiatry [Randomized Controlled Trial] 45:337–340
Aydos L, Titov N, Andrews G (2009) Shyness 5: the clinical effectiveness of internet-based clinician-assisted treatment of social phobia. Australas Psychiatry 17:488–492
Beesdo K, Bittner A, Pine DS, Stein MB, Hofler M, Lieb R, Wittchen HU (2007) Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Arch Gen Psychiatry 64:903–912
Berger T (2011) Web 2.0 – soziale netzwerke und psychotherapie. Psychother Dialog 12:118–122
Berger T, Hohl E, Caspar F (2009) Internet-based treatment for social phobia: a randomized controlled trial. J Clin Psychol 65:1021–1035
Berger T, Caspar F, Richardson R, Kneubuhler B, Sutter D, Andersson G (2011) Internet-based treatment of social phobia: a randomized controlled trial comparing unguided with two types of guided self-help. Behav Res Ther 49:158–169
Berger T, Boettcher J, Caspar F (2014) Internet-based guided self-help for several anxiety disorders: a randomized controlled trial comparing a tailored with a standardized disorder-specific approach. Psychotherapy [Research Support, Non-U.S. Gov’t] 51:207–219
Blanco C, Heimberg RG, Schneier FR, Fresco DM, Chen H, Turk CL, Vermes D, Erwin BA, Schmidt AB, Juster HR, Campeas R, Liebowitz MR (2010) A placebo-controlled trial of phenelzine, cognitive behavioral group therapy, and their combination for social anxiety disorder. Arch Gen Psychiatry 67:286–295
Boettcher J, Berger T, Renneberg B (2012a) Does a pre-treatment diagnostic interview affect the outcome of internet-based self-help for social anxiety disorder? A randomized controlled trial. Behav Cogn Psychother 40:513–528
Boettcher J, Berger T, Renneberg B (2012b) Does a pre-treatment diagnostic interview affect the outcome of internet-based self-help for social anxiety disorder? A randomized controlled trial. Behav Cogn Psychother [Randomized Controlled Trial] 40:513–528
Boettcher J, Renneberg B, Berger T (2013a) Patient expectations in internet-based self-help for social anxiety. Cogn Behav Ther 42:203–214
Boettcher J, Carlbring P, Renneberg B, Berger T (2013b) Internet-based interventions for social anxiety disorder – an overview. Verhaltenstherapie 23:160–168
Botella C, Banos RM, Guillén V, Perpina C, Alcaniz M, Pons A (2000) Telepsychology: public speaking fear treatment on the internet. Cyber Psychol Behav 3:959–968
Botella C, Hofmann S, Moscovitz D (2004) A self-applied internet-based intervention for fear of public speaking. J Clin Psychol 60:1–10
Botella C, Guillen V, Banos RM, García-Palacios A, Gallego MJ, Alcaniz M (2007) Telepsychology and self-help: the treatment of fear of public speaking. Cogn Behav Pract 14:46–57
Botella C, Gallego MJ, Garcia-Palacios A, Guillen V, Banos RM, Quero S, Alcaniz M (2010) An internet-based self-help treatment for fear of public speaking: a controlled trial. Cyberpsychol Behav Soc Netw 13:407–421
Bruch MA, Fallon M, Heimberg RG (2003) Social phobia and difficulties in occupational adjustment. J Counc Psychol 50:109–117
Carlbring P, Furmark T, Steczko J, Ekselius L, Andersson G (2006) An open study of internet-based bibliotherapy with minimal therapist contact via email for social phobia. Clin Psychol 10:30–38
Carlbring P, Gunnarsdottir M, Hedensjo L, Andersson G, Ekselius L, Furmark T (2007) Treatment of social phobia: randomised trial of internet-delivered cognitive-behavioural therapy with telephone support. Br J Psychiatry 190:123–128
Carlbring P, Bergman Nordgren L, Furmark T, Andersson G (2009) Long-term outcome of internet-delivered cognitive-behavioural therapy for social phobia: a 30-month follow-up. Behav Res Ther 47:848–850
Carlbring P, Maurin L, Torngren C, Linna E, Eriksson T, Sparthan E, Straat M, Marquez von Hage C, Bergman-Nordgren L, Andersson G (2011a) Individually-tailored, internet-based treatment for anxiety disorders: a randomized controlled trial. Behav Res Ther 49:18–24
Carlbring P, Maurin L, Torngren C, Linna E, Eriksson T, Sparthan E, Straat M, Marquez von Hage C, Bergman-Nordgren L, Andersson G (2011b) Individually-tailored, internet-based treatment for anxiety disorders: a randomized controlled trial. Behav Res Ther [Randomized Controlled Trial Research Support, Non-U.S. Gov’t] 49:18–24
Chartier MJ, Walker JR, Stein MB (2003) Considering comorbidity in social phobia. Soc Psychiatry Psychiatr Epidemiol 38:728–734
Clark DM, Wells A (1995) A cognitive model of social phobia. In: Heimberg RG, Leibowitz M, Hope DA, Schneider FR (eds) Social phobia: diagnosis, assessment and treatment. Guilford press, New York
Clark DM, Ehlers A, McManus F, Hackmann A, Fennell M, Campbell H, Flower T, Davenport C, Louis B (2003) Cognitive therapy versus fluoxetine in generalized social phobia: a randomized placebo-controlled trial. J Consult Clin Psychol 71:1058–1067
Dahl AA, Dahl CF (2010) Are there gender differences in impairment associated with high social anxiety? A community-based study. J Anxiety Disord 24:487–493
Davidson JR, Hughes DL, George LK, Blazer DG (1993) The epidemiology of social phobia: findings from the duke epidemiological catchment area study. Psychol Med 23:709–718
Erwin BA, Turk CL, Heimberg RG, Fresco DM, Hantula DA (2004) The internet: home to a severe population of individuals with social anxiety disorder? J Anxiety Disord 18:629–646
Eskildsen A, Hougaard E, Rosenberg NK (2010) Pre-treatment patient variables as predictors of drop-out and treatment outcome in cognitive behavioural therapy for social phobia: a systematic review. Nord J Psychiatry 64:94–105
Fehm L, Pelissolo A, Furmark T, Wittchen H-U (2005) Size and burden of social phobia in europe. Eur Neuropsychopharmacol 15:453–462
Furmark T (2002) Social phobia: overview of community surveys. Acta Psychiatr Scand 105:84–93
Furmark T, Tillfors M, Everz P, Marteinsdottir I, Gefvert O, Fredrikson M (1999) Social phobia in the general population: prevalence and sociodemographic profile. Soc Psychiatry Psychiatr Epidemiol 34:416–424
Furmark T, Carlbring P, Hedman E, Sonnenstein A, Clevberger P, Bohman B, Eriksson A, Hallen A, Frykman M, Holmstrom A, Sparthan E, Tillfors M, Ihrfelt EN, Spak M, Ekselius L, Andersson G (2009a) Guided and unguided self-help for social anxiety disorder: randomised controlled trial. Br J Psychiatry J Ment Sci [Randomized Controlled Trial Research Support, Non-US Gov’t] 195:440–447
Furmark T, Carlbring P, Hedman E, Sonnenstein A, Clevberger P, Bohman B, Eriksson A, Hallen A, Frykman M, Holmstrom A, Sparthan E, Tillfors M, Ihrfelt EN, Spak M, Eriksson A, Ekselius L, Andersson G (2009b) Guided and unguided self-help for social anxiety disorder: randomised controlled trial. Br J Psychiatry J Ment Sci [Randomized Controlled Trial Research Support, Non-U.S. Gov’t] 195:440–447
Gallego M, Emmelkamp P, van der Kooj M, Mees H (2011) The effects of a Dutch version of an internet based treatment program for fear of public speaking: a controlled study. Int J Clin Health Psychol 11:459–472
Hedman E, Furmark T, Carlbring P, Ljotsson B, Ruck C, Lindefors N, Andersson G (2011a) A 5-year follow-up of internet-based cognitive behavior therapy for social anxiety disorder. J Med Internet Res 13, e39
Hedman E, Andersson G, Ljótsson B, Andersson E, Rück C, Mörtberg E, Lindefors N (2011b) Internet-based cognitive behavior therapy vs cognitive behavioral group therapy for social anxiety disorder: a randomized controlled non-inferiority trial. PLoS ONE 6, e18001
Hedman E, Andersson E, Ljotsson B, Andersson G, Ruck C, Lindefors N (2011c) Cost-effectiveness of internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: results from a randomized controlled trial. Behav Res Ther 49:729–736
Hedman E, Andersson E, Ljótsson B, Andersson G, Andersson E, Schalling M, Lindefors N, Ruck C (2012a) Clinical and genetic outcome determinants of internet- and group-based cognitive behavior therapy for social anxiety disorder. Acta Psychiatr Scand 126:126–136
Hedman E, Ljótsson B, Lindefors N (2012b) Cognitive behavior therapy via the internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev Pharmacoecon Outcomes Res 12:745–764
Hedman E, Carlbring P, Ljótsson B, Andersson G (2014a) Internetbaserad psykologisk behandling: evidens, indikation och praktiskt genomförande. Natur & Kultur, Stockholm
Hedman E, El Alaoui S, Lindefors N, Andersson E, Ruck C, Ghaderi A, Kaldo V, Lekander M, Andersson G, Ljotsson B (2014b) Clinical effectiveness and cost-effectiveness of internet- vs. group-based cognitive behavior therapy for social anxiety disorder: 4-year follow-up of a randomized trial. Behav Res Ther 59:20–29
Heimberg RG, Becker RE (2002) Cognitive-behavioral group therapy for social phobia. Basic mechanisms and clinical strategies. Guilford Press, New York
Heimberg RG, Salzman DG, Holt CS, Blendell KA (1993) Cognitive-behavioral group treatment for social phobia: effectiveness at five-year follow up. Cogn Ther Res 17:325–339
Hofmann SG, Sawyer AT, Korte KJ, Smits JA (2009) Is it beneficial to add pharmacotherapy to cognitive-behavioral therapy when treating anxiety disorders? A meta-analytic review. Int J Cogn Ther 2:160–175
Johansson R, Sjoberg E, Sjogren M, Johnsson E, Carlbring P, Andersson T, Rousseau A, Andersson G (2012) Tailored vs. standardized internet-based cognitive behavior therapy for depression and comorbid symptoms: a randomized controlled trial. PLoS One [Clinical Trial Randomized Controlled Trial Research Support, Non-U.S. Gov’t] 7:e36905
Johnston L, Titov N, Andrews G, Spence J, Dear BF (2011) A RCT of a transdiagnostic internet-delivered treatment for three anxiety disorders: examination of support roles and disorder-specific outcomes. PLoS One 6, e28079
Kessler RC. The impairments caused by social phobia in the general population: implications for intervention. Acta Psychiatr Scand Suppl [Research Support, Non-U.S. Gov’t Review] 2003:19–27
Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS (1994) Lifetime and 12-month prevalence of dsm-iii-r psychiatric disorders in the United States. Results from the national comorbidity survey. Arch Gen Psychiatry 51:8–19
Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU (2012) Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res 21:169–184
Klein B, Meyer D, Austin DW, Kyrios M (2011) Anxiety online: a virtual clinic: preliminary outcomes following completion of five fully automated treatment programs for anxiety disorders and symptoms. J Med Internet Res [Clinical Trial Research Support, Non-U.S. Gov’t]. 13:e89
Kraemer HC, Wilson GT, Fairburn CG, Agras WS (2002) Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry 59:877–883
Lampe L, Slade T, Issakidis C, Andrews G (2003) Social phobia in the Australian national survey of mental health and well-being (NSMHWB). Psychol Med 33:637–646
Lewis C, Pearce J, Bisson JI (2012) Efficacy, cost-effectiveness and acceptability of self-help interventions for anxiety disorders: systematic review. Br J Psychiatry 200:15–21
Liebowitz MR, Heimberg RG, Fresco DM, Travers J, Stein MB (2000) Social phobia or social anxiety disorder: what’s in a name? Arch Gen Psychiatry 57:191–192
Lipsitz JD, Schneier FR (2000) Social phobia. Epidemiology and cost of illness. Pharmacoeconomics 18:23–32
Magee WJ, Eaton WW, Wittchen HU, McGonagle KA, Kessler RC (1996) Agoraphobia, simple phobia, and social phobia in the national comorbidity survey. Arch Gen Psychiatry 53:159–168
McEvoy PM (2007) Effectiveness of cognitive behavioural group therapy for social phobia in a community clinic: a benchmarking study. Behav Res Ther 45:3030–3040
Mohr DC, Siddique J, Ho J, Duffecy J, Jin L, Fokuo JK (2010) Interest in behavioral and psychological treatments delivered face-to-face, by telephone, and by internet. Ann Behav Med Publ Soc Behav Med [Comparative Study Research Support, N.I.H., Extramural] 40:89–98
Mörtberg E, Clark DM, Bejerot S (2011) Intensive group cognitive therapy and individual cognitive therapy for social phobia: sustained improvement at 5-year follow-up. J Anxiety Disord 25:994–1000
Nordgreen T, Havik OE, Ost LG, Furmark T, Carlbring P, Andersson G (2012) Outcome predictors in guided and unguided self-help for social anxiety disorder. Behav Res Ther 50:13–21
Nordgren LB, Hedman E, Etienne J, Bodin J, Kadowaki A, Eriksson S, Lindkvist E, Andersson G, Carlbring P (2014) Effectiveness and cost-effectiveness of individually tailored internet-delivered cognitive behavior therapy for anxiety disorders in a primary care population: a randomized controlled trial. Behav Res Ther 59:1–11
Olatunji BO, Cisler JM, Tolin DF (2007) Quality of life in the anxiety disorders: a meta-analytic review. Clin Psychol Rev 27:572–581
Ponniah K, Hollon SD (2008) Empirically supported psychological interventions for social phobia in adults: a qualitative review of randomized controlled trials. Psychol Med 38:3–14
Richards D, Richardson T (2012) Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev [Meta-Analysis] 32:329–342
Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC (2008) Social fears and social phobia in the USA: results from the national comorbidity survey replication. Psychol Med 38:15–28
Samoocha D, Bruinvels DJ, Elbers NA, Anema JR, van der Beek AJ (2010) Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. J Med Internet Res [Meta-Analysis Review] 12:e23
Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V (2007) Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med [Comparative Study Meta-Analysis Research Support, Non-U.S. Gov’t] 37:319–328
Stein MB, Stein DJ (2008) Social anxiety disorder. Lancet 371:1115–1125
Stott R, Wild J, Grey N, Liness S, Warnock-Parkes E, Commins S, Readings J, Bremner G, Woodward E, Ehlers A, Clark DM (2013) Internet-delivered cognitive therapy for social anxiety disorder: a development pilot series. Behav Cogn Psychother 41:383–397
Stuhldreher N, Leibing E, Leichsenring F, Beutel ME, Herpertz S, Hoyer J, Konnopka A, Salzer S, Strauss B, Wiltink J, Konig HH (2014) The costs of social anxiety disorder: the role of symptom severity and comorbidities. J Affect Disord 165:87–94
Tillfors M, Carlbring P, Furmark T, Lewenhaupt S, Spak M, Eriksson A, Westling BE, Andersson G (2008) Treating university students with social phobia and public speaking fears: internet delivered self-help with or without live group exposure sessions. Depress Anxiety 25:708–717
Titov N, Andrews G, Schwencke G, Drobny J, Einstein D (2008a) Shyness 1: distance treatment of social phobia over the internet. Aust N Z J Psychiatry 42:585–594
Titov N, Andrews G, Schwencke G (2008b) Shyness 2: treating social phobia online: replication and extension. Aust N Z J Psychiatry 42:595–605
Titov N, Andrews G, Choi I, Schwencke G, Mahoney A (2008c) Shyness 3: randomized controlled trial of guided versus unguided internet-based CBT for social phobia. Aust N Z J Psychiatry 42:1030–1040
Titov N, Andrews G, Choi I, Schwencke G, Johnston L (2009a) Randomized controlled trial of web-based treatment of social phobia without clinician guidance. Aust N Z J Psychiatry 43:913–919
Titov N, Andrews G, Schwencke G, Solley K, Johnston L, Robinson E (2009b) An RCT comparing effect of two types of support on severity of symptoms for people completing internet-based cognitive behaviour therapy for social phobia. Aust N Z J Psychiatry 43:920–926
Titov N, Andrews G, Johnston L, Schwencke G, Choi I (2009c) Shyness programme: longer term benefits, cost-effectiveness, and acceptability. Aust N Z J Psychiatry 43:36–44
Titov N, Andrews G, Schwencke G, Robinson E, Peters L, Spence J (2010a) Randomized controlled trial of internet cognitive behavioural treatment for social phobia with and without motivational enhancement strategies. Aust N Z J Psychiatry 44:938–945
Titov N, Andrews G, Johnston L, Robinson E, Spence J (2010b) Transdiagnostic internet treatment for anxiety disorders: a randomized controlled trial. Behav Res Ther [Randomized Controlled Trial Research Support, Non-U.S. Gov’t] 48:890–899
Titov N, Dear BF, Schwencke G, Andrews G, Johnston L, Craske MG, McEvoy P (2011) Transdiagnostic internet treatment for anxiety and depression: a randomised controlled trial. Behav Res Ther [Randomized Controlled Trial Research Support, Non-U.S. Gov’t] 49:441–452
Wittchen HU, Fehm L (2003) Epidemiology and natural course of social fears and social phobia. Acta Psychiatr Scand Suppl 4–18
Wittchen HU, Fuetsch M, Sonntag H, Müller N, Liebowitz M (2000) Disability and quality of life in pure and comorbid social phobia. Findings from a controlled study. Eur Psychiatry 15:46–58
Yonkers KA, Dyck IR, Keller MB (2001) An eight-year longitudinal comparison of clinical course and characteristics of social phobia among men and women. Psychiatr Serv 52:637–643
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Hedman, E., Botella, C., Berger, T. (2016). Internet-Based Cognitive Behavior Therapy for Social Anxiety Disorder. In: Lindefors, N., Andersson, G. (eds) Guided Internet-Based Treatments in Psychiatry. Springer, Cham. https://doi.org/10.1007/978-3-319-06083-5_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-06083-5_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-06082-8
Online ISBN: 978-3-319-06083-5
eBook Packages: MedicineMedicine (R0)