Abstract
Kyphosis is a difficult topic of spinal surgery, and its management contains many controversies. Surgical management needs consideration of different aspects of the kyphotic deformity such as neurological status, the presence of spinal cord compression, angle of the kyphosis, the quality of bone, and accompanying diseases. In case of significant cord compression and neurological compromise, anterior surgery should have the priority. However, in smooth-angled kyphosis and ankylosing spondylitis patients, deformity can easily be reduced by a posterior-only approach. Since they have no neurological deficits, and large spinal canals, most suitable patients for pedicle subtraction osteotomy are the patients with ankylosing spondylitis.
In lumbar kyphosis one-level pedicle subtraction osteotomy (especially at L2 or L3 levels), in thoracic kyphosis multilevel osteotomies, and in cervicothoracic kyphosis an osteotomy at C7–T1 level should be preferred.
Pedicle subtraction osteotomy is a technically demanding procedure that requires surgeons to perform meticulous technique and consider biomechanical issues to achieve satisfactory results and avoid complications. An attempt to correct the rigid fixed spinal deformity is a difficult task and requires the capability of a highly experienced spine surgeon. Although the physical outcome and patient satisfaction of surgical treatment is quite good, risks and complications should always be considered by both the physician and patient.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Kyphosis
- Sagittal plane deformity
- Ankylosing spondylitis
- Pedicle subtraction osteotomy
- Deformity correction
Introduction
Kyphosis is a sagittal spine deformity that may cause significant disability, pain, and neurological deficits. Kyphosis may be due to trauma, infection such as tuberculosis, ankylosing spondylitis, Scheuermann disease, degenerative diseases, and osteoporotic compression and iatrogenic reasons usually after multilevel laminectomy.
This chapter aims to review the surgical techniques to correct thoracolumbar kyphosis and diminish the neurological deficits caused by compression of the kyphotic deformity. Cervical kyphosis will not be reviewed in this manuscript.
History
Surgery to correct the kyphosis was possibly first attempted in Pott’s disease. In 1945, vertebral osteotomy to correct spinal deformity in ankylosing spondylitis was first introduced by Smith-Peterson [27]. Smith-Peterson and coworkers [27] have reported their results in six patients by applying a single posterior osteotomy and hyperextension of lumbar spine. Postoperatively the patients were placed in plaster immobilization. The results were satisfactory, and patients could stand erect and were able to see ahead.
LaChapelle [16] have performed a two-stage osteotomy for thoracolumbar kyphosis under local anesthesia at L2–L3 level. After removal of posterior elements in first stage, he had performed an anterior osteotomy to place bone grafts into the disc space under general anesthesia 2 weeks later. He then placed the patient in a plaster jacket. Briggs and coworkers [4] and have used similar technique and again without internal fixation.
First articles reporting posterior osteotomy declared a significant incidence of major complications with mortality up to 10 % and paraplegia 30 % [4, 16, 27]. Rupture of the aorta, acute gastric dilation, and superior mesenteric artery thrombosis have also been reported.
Since anterior opening-wedge osteotomies pose a particular risk to rupture or obstruct the aorta [1, 18], Scudese and Calabro [24] have modified the Smith-Peterson osteotomy by removing the disc at the selected level together with the superior portion of the body. They claimed that aortic or inferior vena cava obstruction is less likely by shortening posterior part of the spine and not opening the disc space and anterior longitudinal ligament in front.
Simmons [25] has done osteotomy of the cervical and lumbar spine by using local anesthesia, which allows continuous intraoperative monitoring of neurologic status. However, with recent surgical techniques, the use of general anesthesia, and early mobilization by internal fixations, morbidity and mortality have markedly decreased [5, 11, 13, 19, 20, 23].
In 1985, Thomasen [30] first reported a transpedicular closing-wedge osteotomy in treating ankylosing spondylitic kyphosis. This technique has been widely used for correcting kyphosis of various kinds with good results.
Etiology
There are many causes of kyphosis which are summarized below:
-
(a)
Congenital: Congenital vertebral body and posterior element anomalies, fusion defects, and segmentation abnormalities may result in progressive flexion deformity. Without surgical intervention, the deformity is progressive.
The congenital kyphosis is radiographically classified as failure of formation (Type 1), failure of segmentation (Type 2), and mixed deformity (Type 3) [20, 36, 37].
-
(b)
Ankylosing spondylitis: Ankylosing spondylitis belongs to a group of seronegative spondyloarthropathies. The incidence of the ankylosing spondylitis is estimated 1.4 % of the general population [8]. It goes with remission and exacerbation periods and primarily affects the spine and hip joints causing progressive bone fusion resulting with ossification of the intervertebral disc, narrowing of joints, and osteoporosis and fusion of the spine. Spinal fusion starts from lumbar level and progresses cranially to the cervical spine. Whole spine is now like a long bone and susceptible to fractures. A progressive flexion deformity may result with a disabling kyphosis.
A severely disturbed sagittal contour, loss of horizontal gaze resulting to inability to see the front and especially the sky, and social and psychological isolation are results of severe kyphosis. Besides, respiratory restriction and a higher risk for trauma occur. Although not a strong indicator, HLA-B27 antigen is a test for searching ankylosing spondylitis. Besides, the attachment of sacroiliac joints is an important indicator of the disease. Kyphotic deformity can be measured by the Cobb method and the chin-brow technique.
Trauma in ankylosing spondylitis may also cause kyphosis. Although fractures occurring in ankylosing spondylitis patients are potentially very disabling, even lethal, they may sometimes be unrecognized and cause insidious kyphosis with mild pain. The majority occur in the lower cervical spine and often result in quadriplegia [2, 9, 22, 29, 31].
-
(c)
Trauma: Thoracolumbar fractures and dislocations may result with kyphotic deformity if not properly treated [5]. Kyphosis after trauma may be accepted as a long-term complication which can lead to further deterioration in function and quality of life.
-
(d)
Infection: The most frequent infection causing kyphosis is tuberculosis, or the so-called Pott’s disease. Besides, other infections, primary or iatrogenic spondylodiscitis, may also cause kyphosis in chronic forms.
-
(e)
Degenerative: Degenerative diseases, especially in the lumbar spine, may change the sagittal balance and cause the so-called flat back deformity and sometimes significant kyphosis [12].
-
(f)
Postlaminectomy: Postlaminectomy kyphosis is more frequent in cervical spine. However, especially in pediatric ages, multilevel laminectomies in thoracic and lumbar spine can also cause kyphotic deformity.
Clinical and Radiological Evaluation
From the physician’s point of view, there are mainly two types of kyphosis: (a) kyphosis without neurological deficits and (b) kyphosis with neurological deficits. For a good management planning, the bone density, angle of the kyphosis, age of the patient, associated disorders, and comorbidities should also be evaluated (Table 1).
The normal values of physiological thoracic kyphosis (T2–T12) vary between 30° and 50°. Lumbar lordosis varies between 45° and 70°. The sagittal vertical axis passes 2 cm of the posterior superior corner of S1.
The C7 plumb line is the line drawn perpendicular to the floor from the centrum of C7 body. It must cross from the posterior superior edge of S1 end plate. If the plumb line is anterior to the S1, it is called positive sagittal balance which indicates a hyperkyphosis. If the C7 plumb line is dorsal to the S1, it is called negative sagittal balance which indicates a hyperlordosis.
Spinal deformity can be clinically measured by the “chin-brow technique.” A line drawn from the brow to the chin intersecting the vertical axis would give approximate angle of kyphosis. It is a practical method to measure the angulation clinically without direct X-rays.
Radiologic assessment should include a whole-spine standing direct roentgenogram including hip joints. For evaluation of the fexibility, a flexion-extension view should also be obtained.
With assessment of radiographic images, the site of the primary deformity should be determined. This will be the site of major surgical correction. The amount of bone to be resected at each level can then be measured.
Magnetic resonance images will also be valuable to obtain information about bone density and edema and other abnormalities, such as congenital problems and tethered cord syndrome.
Treatment Planning
Surgical indications are summarized in Table 2. The indications are quite variable and more related with etiology of the kyphosis.
-
(a)
Cord compression: If it causes significant cord compression, the principle of the surgery must be to decompress the apex of the kyphotic deformity. At the same session, deformity correction may also be tried. Kyphosis due to trauma, Pott’s disease, and some congenital diseases are most frequent reasons for kyphosis with neurological deficits.
-
(b)
Pain may be the only symptom in traumatic, degenerative, osteoporotic kyphosis. In that instance, the aim of the surgery must be deformity correction together with fusion.
-
(c)
Respiratory problems are a late complication of severe kyphosis. Surgery should aim to prevent respiratory failure. However, in severe kyphotic cases with significant restriction of respiration, the surgery under general anesthesia will pose significant risk.
-
(d)
Deformity itself can cause significant disability and may be the primary aim of the surgery. Ankylosing spondylitis is a good example to that situation. If the angle of the kyphosis exceeds 75°, patients are not able to see the faces of the other persons when sitting and standing. They cannot walk easily. To correct their sagittal balance, they try to flex their knees and hips.
In general, an anterior surgery is necessary if kyphosis is with neurologic deficits and if the angle of kyphosis is more than 70°. Posterior techniques with osteotomy is necessary, if there is a long curvature kyphosis, if the short curvature thoracic kyphosis is between 30° and 70°, or if lumbar kyphosis is more than 20°.
Decision making in kyphosis management is not well defined, and there are many options for surgery. Table 3 gives a personal algorithm for surgical management.
General Precautions
Before surgery, specific problems that might result in intraoperative complications should be evaluated.
-
(a)
Respiratory function may be diminished by kyphotic deformity, especially in severe thoracic kyphosis. Besides, ankylosis of the ribs may restrict chest expansion. As a result, postoperative use of a ventilator may be necessary.
-
(b)
Intubation difficulty may pose an important problem especially in ankylosing spondylitis patients. Deformity in cervicothoracic junction and ankylosis of temporomandibular joints are the reasons for that. Fiber-optic intubation may be helpful. In some cases a tracheostomy may be necessary.
-
(c)
Nutritional status: Ankylosing spondylitis patients may have associated ileitis or colitis. The nutritional status of the patient may be worse.
-
(d)
Osteoporosis: Bone density is another condition that must be evaluated well. Geriatric patients and patients with ankylosing spondylitis are prone to diminished bone density. In case of significant osteopenia, special planning of fixation should be anticipated.
-
(e)
Hip joints: If hip joints are ankylosed and a flexion deformity is developed, correction of this problem, i.e., hip replacement, should proceed before kyphosis correction.
Surgical Techniques
In thoracolumbar kyphosis, anterior surgery is necessary mainly for decompression of the spinal cord. If there is no cord compression, posterior-only approaches may be used. However, both for correction purposes and stabilization of the vertebral column, posterior surgery is necessary. Table 4 summarizes the surgical techniques.
Van Royen and De Gast [34] have classified the posterior osteotomies as follows: (1) opening-wedge osteotomy, (2) polysegmental wedge osteotomies, and (3) closing-wedge osteotomy. There is no consensus on the literature of which technique is more suitable for surgery of kyphosis correction.
-
(a)
Rod reduction and fixation: This technique may be applied for more flexible kyphosis, and good candidates are patients with degenerative kyphosis and Scheuermann disease. Rods are first placed on the proximal screws, then the rods are pushed to the distal screws by reducing the hyperkyphosis and connected to the distal part of the construct [19] (Fig. 1).
Fig. 1 Rod reduction and fixation technique for flexible kyphosis. The upper and lower segments of the kyphosis are anchored whether by screws or hooks; after placing and tightening both rods on the upper vertebra, rods are pushed ventrally and placed on the lower screws by achieving some kyphosis correction
Kyphosis in Scheuermann disease can be managed by an anterior apical release and fusion before posterior rod compression instrumentation and closing-wedge lamina resection. A report by Johnston and coworkers [13] has examined the necessity of anterior spinal fusion and concluded that a posterior-only surgery with posterior compressive instrumentation with threaded rods is sufficient.
-
(b)
Smith-Peterson osteotomy: This an extension osteotomy and is originally described by Smith-Peterson in 1945. Osteotomies are done by removing the posterior elements completely at the disc level. Then, the spine is extended through the osteotomized segments and disc spaces. It causes approximately 10–15° of correction at each level (Figs. 2 and 3). The main risk of this technique as originally described is rupture of the ventral part of the disc and anterior longitudinal ligament, resulting to stretching of the abdominal viscera which may cause rupture or obstruction of the aorta. Some surgeons prefer to place anterior strut grafts after posterior instrumentation [16].
Fig. 2 -
(c)
Pedicle subtraction osteotomy: This is an approach resecting posterior elements, both pedicles and a part of the body in a wedge style (Fig. 4). The main advantage is that the whole procedure can be done by a posterior-only approach.
Fig. 4 Pedicle subtraction osteotomy. This technique is done by removing lamina, facet joints, pedicles, and transverse processes on both sides. Posterior part of the body removal is deepened till anterior longitudinal ligament by creating a wedge of the body. I push the hidden posterior cortex of the body ventrally to prevent retropulsion during reduction. This type of osteotomy does not distract the ventral disc or ligament and causes some shortening of the spine. Approximately 30° of kyphosis reduction may be provided in one level
Thirty to thirty-five degrees of lordosis can be achieved with this technique. If the surgeon expects more degrees of correction, osteotomies must be performed in multiple consecutive levels. For example, 100° of kyphosis may be corrected by three-level pedicle subtraction osteotomy.
The so-called egg-shell procedure is to enter the vertebral body via pedicles and remove spongious bone inside the body by leaving the cortex of the body like a shell of an egg. Then, compressive instrumentation would result in collapse of the body and result with lordosis. This procedure, however, poses a risk that the posterior part of the body may retropulse the spinal canal and cause spinal cord compression.
Pedicle subtraction osteotomy is performed by a careful resection of the posterior elements than decancellation of the body via a transpedicular route. I perform this procedure under operation microscope, remove transverse processes and lateral margins of the pedicle, enter the body using a high-speed drill, and go through till the anterior longitudinal ligament. At last, I push the posterior cortex of the body ventrally and excise the posterior longitudinal ligament. Afterwards, the entire spine is extended through the osteotomy site using deflection of the operating table and sometimes by additional compression of the adjacent pedicle screws on the rod. After closing the gap, the dura must be observed carefully, and any kinking or compression by lamina must be avoided to prevent neurological deficits.
If it is a whole-spine—thoracic and lumbar—kyphosis, correction may be achieved through lumbar osteotomy, and relordosation is accomplished. Thomasen has chosen the L2 vertebra for posterior osteotomy [30]. Although he has used plates and metallic wires posteriorly in some patients, he also has placed the patients in a plaster jacket for 3 months. Simmons [26] has used Harrington compression system for thoracic deformity. With the advent of new pedicle-based internal fixation techniques, plaster jackets have been abandoned today [3, 28, 34].
-
(d)
Combined anterior-posterior surgery: This is advocated in severe deformity with significant compromise to the spinal cord. If a combined anterior-posterior osteotomy is chosen, thoracotomy is performed from the convex site of the deformity. In both approaches a ventral cage with grafts should also be placed.
Anterior strut grafting has also been advocated after Smith-Peterson osteotomy to support anterior column [10, 16]. LaChapelle [16] has first performed a posterior laminectomy and osteotomy under local anesthesia and, 2–3 weeks later, an anterior surgery under general anesthesia and excised the intervertebral disc and applied autologous bone grafts inside the disc space. He then applied a plaster brace for 6 months.
-
(e)
Vertebral column resection: This is the procedure of choice in severe rigid deformities. Although a combined anterior-posterior osteotomy may be chosen in some instances, deformities 90° or more can easily be handled with a posterior-only approach, since the deformity facilitates it. Some surgeons prefer a circumferential decompression and instrumentation in the same stage [21].
Chen and coworkers [7] have claimed that in severe sharp-angled kyphosis, a shortening procedure will be too risky, and they advocated the resection of the apex of the kyphosis, corrected the segment with two rods, and placed a cage in the resected segment ventrally.
Operative Positioning and Anesthesia
Early reports on posterior kyphosis surgery have used local anesthesia [26]. Smith-Peterson and colleagues have used general anesthesia with the patient lying in the prone position. Adams [1] has performed the surgery with the patients lying on their side.
For cervical osteotomy, Simmons [26] and Law [17] have also used local anesthesia in sitting position on a dentist’s chair. Urist [32] has used general anesthesia for cervical osteotomy. Two reasons for local anesthesia are observing the neurological function and difficulty of intubation [26].
We always preferred general anesthesia and prone position with three-pin head holder. We seldom used sitting position. The surgeon must be prepared to change the position of the table and correct the deformity after completing the osteotomy (Fig. 5). Although it is advocated to use spinal cord monitoring, we did not use it in any of our cases.
Some surgeons recommend to place a nasogastric tube since the superior mesenteric artery may be stretched over duodenum resulting in gastric dilation [15].
Technical Considerations in Lumbar and Thoracolumbar Junction Kyphosis
Posterior-only surgeries in lumbar spine is easier than thoracic and cervical spine, because the retraction of the cauda equina is possible and reduction is not hard as is thoracic spine with rigidity provided by the ribs. In patients with ankylosing spondylitis, a patient will resume a more erect position, diaphragmatic ventilation will be possible, and compression to the abdominal structures by the edges of the ribs will be reduced.
In smooth-angled kyphosis at the thoracolumbar junction, an osteotomy at L2 level will be sufficient. In lumbar kyphosis, L3 may be the level of choice.
Technical Considerations in Thoracic Kyphosis
The previous reports have tried not to implement reduction of thoracic kyphosis with posterior-only approaches. Simmons [26] has recommended anterior and posterior combined approaches in severe thoracic kyphosis.
It is our intention also to be more cautious at the thoracic levels during correction by a posterior osteotomy. We believe that multilevel pedicle subtraction osteotomies by gaining a 30° reduction at each level and meticulous observation of the spinal cord to be sure that there is no kinking of the dura should be applied.
Simmons has advocated an osteotomy in the midlumbar spine, in case the dorsal kyphosis is associated with a loss of lumbar lordosis or if the thoracolumbar deformity is less than 40° [26]. We believe that in smooth-angled kyphosis involving both thoracic and lumbar levels, the midpoint of osteotomy should be L2.
Technical Considerations in Cervicothoracic Kyphosis
Cervicothoracic kyphosis is a more disabling problem than thoracolumbar kyphosis. The field of vision is severely restricted, and the patient cannot open his/her mouth. Because of excessive loads on craniocervical junction, atlantoaxial subluxation may develop. Dyspnea and dysphagia may happen because of compression of trachea and esophagus.
The first experience of cervical osteotomy is from the 1960s. Urist [32] is the first surgeon performing osteotomy of the cervical spine in 1958. In 1962 Law [17] made an extensive report of this technique. Law has performed osteotomy under general anesthesia at any level below the second cervical vertebra. Internal fixation was done with wire or plates, and then the patient was placed in a Minerva cast.
In 1972, Simmons has recommended cervical osteotomy under local anesthesia and in sitting position because of intubation difficulty [25]. One other advantage of surgery under local anesthesia is the patients report on paresthetic pain along the distribution of the cervical roots and prevent damage to the roots. Another difference from Law’s approach is the site of osteotomy which was at C7 or T1. The vertebral artery compromise is unlikely at that level since it enters the foramen at C6 level. Besides, C8 and T1 roots are less eloquent roots and can be mobilized easily. Simmons has not used internal fixation and placed the patient in a halo cast after surgery which was worn for 4 months (Fig. 6).
The technique we use for cervicothoracic kyphosis is a C7 osteotomy. I consider that kinking of the vertebral artery at upper levels may pose a great risk and stretching of C8 nerve roots is unlikely. We choose the prone position and use a Mayfield three-pin head holder. The most difficult part is the intubation of the patient. The difficulty comes not just from the deformity, but also the ankylosis of temporomandibular joints causes immobility. A fiber-optic intubation in an awake patient and using nasal route may be helpful in severely deformed patients. After removing C7 spinous process, both pedicles and posterior part of the vertebral body are removed using a high-speed drill. Both C8 roots were mobilized. Then, by holding the head with both hands, the Mayfield head holder is released and the head is extended carefully, and the gap between C6 and T1 lamina is closed. The dura and roots are observed again to be sure there is no kinking and impingement. A posterior screw system two levels up and two levels below is then applied in corrected position. The patient is let to walk the next day using a rigid collar.
Complications and Outcome
There are many reported complications in kyphosis correction:
-
(a)
Neurological worsening: Neurologic compromise could result from spinal cord compression as a result of inadequate decompression [33] or subluxation [10]. In Simmons’ series [26] using single-level wedge osteotomy in 90 patients, seven (8 %) developed L3 root or cauda equina compression.
-
(b)
Aorta rupture and death: This complication is reported in earlier series with posterior osteotomies causing rupture of the anterior longitudinal ligament that loads stretching forces to the aorta. The first report for aortic rupture in correction of ankylosing spondylitis is in 1956 by Lichtblau and Wilson [18]. Law [17] presented a large sample of kyphotic correction and reported a 10 % risk of death associated with surgical intervention. In patients with ankylosing spondylitis, inflammatory changes may cause the fibrosis of cardiac vessels and the aorta, and the aorta weakens and becomes prone to rupture from aneurysms. There are some other reports describing aortic rupture due to lumbar extension osteotomy during surgery or late after surgery [6, 14, 35].
Besides, by elongation of the anterior column, a stretch of the superior mesenteric artery over duodenum may cause gastric dilation and vomiting [26].
-
(c)
Respiratory problems: This is possible especially in patients with preoperative restriction of the lung capacity.
-
(d)
Infection is a common complication in long-lasting and instrumented spine surgeries.
-
(e)
Correction loss: Loss of correction may happen by many reasons such as inappropriate surgical planning, pseudarthrosis, osteopenia, and smoking.
In a report of 33 patients with lumbar pedicle subtraction osteotomy, Bridwell and coworkers [3] reported that 7 had pseudarthrosis, 2 had acute angular kyphosis, and 5 had transient neurologic deficits whose deficits resolved after central canal enlargement. Overall patient satisfaction was good, and they concluded that the clinical result with pedicle subtraction osteotomy is reduced with pseudarthrosis in the thoracic or lumbar spine and subsequent breakdown adjacent to the fusion. The results with a degenerative sagittal imbalance etiology were worse, and the complications were higher. They found that central canal enlargement is a critical issue in surgical management of thoracolumbar kyphosis.
Ikenaga and coworkers [11] have examined the rate of complications after pedicle subtraction osteotomy in a clinical series and reported 48 complications in 67 patients. There were 6 intraoperative, 4 perioperative (during first 2 weeks), and 38 late postoperative complications. Among late complications, there were adjacent-segment collapse, 8 (12 %); progression of kyphosis without collapse, 10 (15 %); infection, 2 (3 %); pseudarthrosis, 7 (10 %); and instrumentation failure, 3 (4 %). Additional surgery was necessary in 7 patients (10 %).
Personal Series
Between 1992 and 2011, 62 patients with thoracic and lumbar kyphosis were surgically treated. The mean age is 38 (between 6 and 70 years); male/female ratio is 32/30. Etiology of kyphosis were congenital (21), ankylosing spondylitis (13), degenerative diseases (7), trauma (7), infection (4), previous laminectomy (4), Scheuermann kyphosis (2), tuberculosis (2), myelomeningocele (1), and osteoporotic compression (1) (Table 5).
There were soft angle kyphosis in 15 patients (cervicothoracic 3, thoracic 3, thoracolumbar 9). Remaining 47 patients had a sharp-angle kyphosis in either cervicothoracic junction (T1, 1 case; T3–4, 4 cases), thoracic spine (T6, 1 case; T7–8 2 cases; T8–9, 1 case; T9, 1 case; T10, 1 case; T11–12, 2 cases; T12, 4 cases; T12–L1, 2 cases; L1, 10 cases), or lumbar spine (L1–2, 1 case; L2, 3 cases; L3, 4 cases; L3–4, 5 cases; L4, 2 cases; L4–5, 3 cases).
The type of surgery performed for this series was posterior osteotomy and reduction with pedicle fixation (36), posterior fixation with interbody fusion (11), anterior decompression and reduction with fixation (7), and combined anterior and posterior surgery (8) (Table 6).
Results: Significant reduction could be achieved in 57 cases. Neurological deficits did not worsen in patients with preoperative deficits. Complications of surgery were hardware failures (5 cases), loss of correction (8 cases), wound problems and local infection (12 cases), and CSF leakage (3 cases). There were no neurological complications. Figures 7, 8, 9, and 10 are some examples from our personal series.
A 21-year-old male with Scheuermann kyphosis (a, b). Smith-Peterson osteotomies were performed at T6–7, T7–8, T8–9, and T9–10 levels. T2–5 and T9–12 pedicle screw fixations were performed, and a compressive correction on rods was performed through a posterior-only approach (c, d). Postop direct radiograms (e–g) and posture (h) show the reduction of the kyphosis
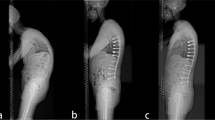
A 42-year-old male with severe thoracolumbar kyphosis. He suffers from ankylosing spondylitis for 20 years. He was not able to walk in erect position and look at the faces of other persons and also the sky when standing (a, b). The kyphosis was approximately 100° (c–f). A four-level pedicle subtraction osteotomy was performed (g–j), and an excellent reduction could be achieved (k–n). Note the degree of kyphosis on the operating table before (g) and after (j) surgery
A 34-year-old male with ankylosing spondylitis for more than 10 years. He had kyphosis more prominent on cervicothoracic junction in addition to some lumbar kyphosis (a–c). Intubation was not difficult; however, you can note the degree of deformity in supine position (d). After a Ct posterior osteotomy, both C8 nerve roots are visualized (e). The gap at the osteotomy site is closed using manual extension with the release of Mayfield head holder (f). C5 and C6 lateral mass and T1 and T2 pedicle screw fixations were performed (g). Postoperative photograph 2 days after surgery depicts the amount of correction and recovery of the forward gaze angle (h). Postoperatively he used a SOMI brace for 8 weeks
A 51-year-old female admitted with severe cervicothoracic kyphosis. She has been diagnosed with ankylosing spondylitis for 15 years. She was unable to look at the faces of other people when she was standing, and her chin was on her sternum with 1 cm distance between (a–c). She had difficulty of swallowing due to compression of the esophagus by manubrium sterni (d, e). Also she described abdominal pain due to xiphoid compression to the abdomen. We planned to perform a two-stage surgery with posterior osteotomies on 7 levels, cervical and thoracic (e). The first stage was performed in sitting position. The hardest part was intubation and could be performed with fiber-optic bronchoscopy (f). Pedicle subtraction osteotomies were performed at T4, T6, T8, and T11 levels (g), and pedicle screw fixation was performed (h). At the end of the first session, it was possible to place fingers under the mandible (i). Two weeks later, the second stage of surgery was performed with the patient on prone position (j) with osteotomies at C6–7, C7–T1, and T2–3 disc levels. The previous rods were removed, and new rods were inserted from C6 to L3 (k). Significant reduction was achieved by deflection of the head on Mayfield head holder (l). She stayed in intensive care unit for 1 month and recovered well with significant deformity correction (m–r). Block 1 (a– c, o, p, r) Pre- and postoperative photographs of the patient. Block 2 (d, e, m, n) Pre- and postoperative direct radiograms and sagittal MR. Block 3 (f–i) Stage 1 surgery, thoracic osteotomies. Block 4 (j–l) Stage 2 surgery, cervicothoracic osteotomies
Conclusion
Surgical management of kyphosis needs consideration of different aspects of the kyphotic deformity such as neurological status, the presence of spinal cord compression, angle of the kyphosis, the quality of bone, and accompanying diseases. In case of significant cord compression and neurological compromise, anterior should have the priority.
However, in smooth-angled kyphosis and ankylosing spondylitis patients, deformity can easily be reduced by a posterior-only approach. Since they have no neurological deficits, and large spinal canal, most suitable patients for pedicle subtraction osteotomy are the patients with ankylosing spondylitis.
In lumbar kyphosis one-level pedicle subtraction osteotomy (especially at L2 or L3 levels), in thoracic kyphosis multilevel osteotomies, and in cervicothoracic kyphosis an osteotomy at C7–T1 level should be preferred.
Pedicle subtraction osteotomy is a technically demanding procedure that requires surgeons to exercise caution to achieve satisfactory results while avoiding complications. An attempt to correct the rigid fixed spinal deformity in ankylosing spondylitis is not an easy task and requires the capability of a highly experienced spine surgeon. Although the physical outcome of surgical treatment is beneficial, risks and complications exist that demand awareness by both the physician and patient.
References
Adams JC (1952) Technique, dangers and safeguards in osteotomy. J Bone Joint Surg Am 34B:226
Amamilo SC (1989) Fractures of the cervical spine in patients with ankylosing spondylitis. Orthop Rev 18:339–344
Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A, Baldus C, Blanke K (2003) Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine 28:2093–2101
Briggs H, Keats S, Schlesinger PT (1947) Wedge osteotomy of the spine with bilateral intervertebral foraminotomy: correction of flexion deformity in five cases of ankylosing arthritis of the spine. J Bone Joint Surg Am 29:1075–1082
Buchowski JM, Kuhns CA, Bridwell KH, Lenke LG (2008) Surgical management of posttraumatic thoracolumbar kyphosis. Spine J 8:666–677
Camargo FP, Cordeiro EN, Napoli MMM (1986) Corrective osteotomy of the spine in ankylosing spondylitis: experience with 66 cases. Clin Orthop 208:157–167
Chen Z, Zeng Y, Li W, Guo Z, Qi Q, Sun C (2011) Apical segmental resection osteotomy with dual axial rotation corrective technique for severe focal kyphosis of the thoracolumbar spine. J Neurosurg Spine 14:106–113
Cruickshank B (1951) Histopathology of diathrodial joints in ankylosing spondylitis. Ann Rheum Dis 10:393–404
Graham B, Van Peteghem PK (1989) Fractures of the spine in ankylosing spondylitis. Diagnosis, treatment, and complications. Spine 14(8):803–807
Herbert JJ (1959) Vertebral osteotomy for kyphosis, especially in Marie–Strumpell arthritis. J Bone Joint Surg Am 41A(2):291–302
Ikenaga M, Shikata J, Takemoto M, Tanaka C (2007) Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine 6:330–336
Jang JS, Lee SH, Kim JM, Min JH, Han KM, Maeng DH (2009) Can patients with sagittally well-compensated lumbar degenerative kyphosis benefit from surgical treatment for intractable back pain? Neurosurgery 64:115–121
Johnston CE, Elerson E, Dagher G (2005) Correction of adolescent hyperkyphosis with posterior-only threaded rod compression instrumentation: is anterior spinal fusion still necessary? Spine 30:1528–1534
Klems VH, Friedebold G (1971) Ruptur der Aorta abdominalis nach Aufrichtungsoperation bei Spondylitis ankylopoetica. Z Orthop 108:554–563
Kostuik JP (1997) Ankylosing spondylitis: surgical treatment. In: Frymoyer JW (ed) The adult spine: principles and practice, 2nd edn. Lippincott-Raven, Philadelphia
LaChapelle EH (1946) Osteotomy of the lumbar spine for correction of kyphosis in a case of ankylosing spondylarthritis. J Bone Joint Surg Am 28:851–858
Law WA (1962) Osteotomy of the spine. J Bone Joint Surg Am 44:1199–1206
Lichtblau PO, Wilson PD (1956) Possible mechanism of aortic rupture in orthopedic correction of rheumatoid spondylitis. J Bone Joint Surg Am 38A:123–127
Lim M, Green DW, Billinghurst JE, Huang RC, Rawlins BA, Widmann RF, Burke SW, Adjei OB (2004) Scheuermann kyphosis: safe and effective surgical treatment using multisegmental instrumentation. Spine 29:1789–1794
McMaster MH, Singh H (1999) Natural history of congenital kyphosis, kyphoscoliosis. J Bone Joint Surg Am 81:1367–1383
Mirzanli C, Ozturk C, Karatoprak O, Aydogan M, Tezer M, Hamzaoglu A (2008) Double-segment total vertebrectomy for the surgical treatment of congenital kyphoscoliosis: a case report. Spine J 8:683–686
Podolsky SM, Hoffman JR, Pietrafesa CA (1983) Neurologic complications following immobilization of cervical spine fracture in a patient with ankylosing spondylitis. Ann Emerg Med 12:578–580
Roy-Camille R, Henry P, Saillant G, Doursounian L (1987) Chirurgie des grandes cyphoses vertebrales de la spondylarthrite ankylosante. Rev Rhum 54(3):261–267
Scudese YA, Calabro JJ (1963) Vertebral wedge osteotomy. Correction of rheumatoid (ankylosing) spondylitis. JAMA 186:627–631
Simmons EH (1972) The surgical correction of flexion deformity of the cervical spine in ankylosing spondylitis. Clin Orthop 86:132–143
Simmons EH (1977) Kyphotic deformity of the spine in ankylosing spondylitis. Clin Orthop 128:65–77
Smith-Peterson MN, Larson CB, Aufranc OE (1945) Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg Am 27:1–11
Suk SI, Chung EW, Lee SM, Lee JH, Kim SS, Kim JH (2005) Posterior vertebral column resection in fixed lumbosacral deformity. Spine 30:E703–E710
Surin YY (1980) Fractures of the cervical spine in patients with ankylosing spondylitis. Acta Orthop Scand 51:79–84
Thomasen E (1985) Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop 194:142–146
Thorngren KG, Liedberg E, Aspelin P (1981) Fractures of the thoracic and lumbar spine in ankylosing spondylitis. Arch Orthop Trauma Surg 98:101–107
Urist MR (1958) Osteotomy of the cervical spine: report of a case of ankylosing rheumatoid spondylitis. J Bone Joint Surg Am 40:833–843
van Royen B, Slot GH (1995) Closing-wedge posterior osteotomy for ankylosing spondylitis. J Bone Joint Surg Br 77:117–121
van Royen BJ, De Gast A (1999) Lumbar osteotomy for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. A structured review of three methods of treatment. Ann Rheum Dis 58:399–406
Weatherley C, Jaffray D, Terry A (1988) Vascular complications associated with osteotomy in ankylosing spondylitis: a report of two cases. Spine 13:43–46
Winter RB, Hall JE (1978) Kyphosis in childhood, adolescence. Spine 3:285–308
Winter RB, Moe JH, Lonstein JE (1985) The surgical treatment of congenital kyphosis: a review of 94 patients age 5 years or older, with 2 years or more follow-up in 77 patients. Spine 10:224–231
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Zileli, M. (2014). Surgery for Kyphosis. In: Schramm, J. (eds) Advances and Technical Standards in Neurosurgery. Advances and Technical Standards in Neurosurgery, vol 41. Springer, Cham. https://doi.org/10.1007/978-3-319-01830-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-01830-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-01829-4
Online ISBN: 978-3-319-01830-0
eBook Packages: MedicineMedicine (R0)