Abstract
In airway smooth muscle (ASM) cells, contractile tone is tightly coupled to the intracellular calcium (Ca2+) concentration, with Ca2+ release from intracellular stores, followed by influx through plasma membrane ion channels providing the signature Ca2+ signal leading to contraction. One such Ca2+ influx pathway, via store-operated calcium (SOC) channels, is particularly prominent in ASM cells. SOC entry not only supplies Ca2+ to replenish the depleted intracellular stores but also provides a sustained Ca2+ signal to maintain contraction and potentially initiate downstream cellular responses. The molecular determinants of store-operated Ca2+ entry were poorly defined until the relatively recent discovery of the central roles of the stromal interaction molecules and Orai proteins in this pathway. In this chapter, we describe the current understanding of the mechanism of SOC entry and its functional significance in ASM cells.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Airway smooth muscle (ASM) tone is the critical determinant of bronchial diameter and, thus, bronchial airflow. At rest, ASM is relatively quiescent, but activation of ASM cells by bronchoconstrictors (e.g. acetylcholine, histamine) can lead, in asthmatics, to marked airway constriction and bronchospasm. In asthma, bronchial hyperresponsiveness is a major cause of respiratory dysfunction, and many common asthma therapies target ASM to directly regulate airway tone and ameliorate these symptoms.
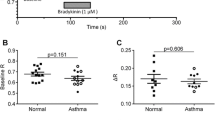
In ASM cells, contractile tone is predominantly determined by the intracellular calcium (Ca2+) concentration. Many bronchoconstrictors act through Gq protein-coupled receptors to elevate Ca2+ through phospholipase C (PLC) activation and inositol trisphosphate (IP3)-dependent Ca2+ release from intracellular stores [2]. The tight regulation of intracellular Ca2+ levels is critical for the regulation of myriad cellular functions and, ultimately, cell viability [43]. Accordingly, in ASM cells, Ca2+ modulates such key cellular events as contraction, proliferation, migration and cytokine synthesis. Dysfunction in one or a combination of these events may initiate, orchestrate and perpetuate the permanent structural changes to the airways observed in people with chronic asthma. The molecular components involved in regulating intracellular Ca2+ levels in ASM therefore constitute attractive therapeutic targets in the treatment of asthma (and other airway diseases) and, as such, have attracted considerable research efforts.
A variety of Ca2+-gating pathways, including voltage-dependent calcium channels (VDCCs), receptor-operated calcium channels (ROCs) and sodium/calcium exchangers, may be found in the plasma membrane of ASM. However, the dominant mechanism by which intracellular Ca2+ is modulated in ASM cells is via store-operated calcium (SOC) entry (SOCE), and it is this mechanism which primarily drives ASM contraction [61]. SOCE [formerly referred to as capacitative calcium entry (CCE)] was first postulated in 1986 by James Putney and is the process by which a decrease in endoplasmic reticulum (ER) Ca2+ content signals to induce an influx of extracellular Ca2+ via plasma membrane Ca2+ channels [51, 55]. The current mediating this Ca2+ entry was first identified by Hoth and Penner ([28]), who coined the term ICRAC (for calcium release-activated calcium current).
Experimentally, Sarcoplasmic reticulum (SR) Ca2+ stores may be depleted by a variety of manipulations, often in combination with the removal of extracellular Ca2+, including inhibition of the sarcoplasmic/endoplasmic reticulum (SR/ER) Ca2+-ATPase (SERCA) pump (e.g. with thapsigargin [46]); emptying of the SR by ryanodine or caffeine treatment [3, 4, 10]; exposure to the Ca2+ chelator ethylene glycol-bis(β-aminoethyl)-N,N,N′,N′-tetraacetic acid (EGTA); or the activation of G-protein-coupled receptors (GPCRs), predominantly in response to contractile agents and coupled to the Gq family of G proteins [8, 24]. In ASM cells, bradykinin and histamine (acting via the B2 and H1 Gq-protein-coupled receptors, respectively) are commonly used as ligands due to their pathophysiological and clinical relevance.
Upon extracellular exposure to a contractile agonist such as bradykinin or histamine, an initial rise in intracellular Ca2+ is observed, which is a direct result of Ca2+ being released from intracellular SR stores (via the IP3R) into the cytoplasm. This rise in intracellular Ca2+ causes the ASM cell to contract. The subsequent influx of Ca2+ from the extracellular milieu is largely via SOCE, and this process is central to the maintenance of contraction [61], although the contribution of L-type VDCC, ROC and reverse-mode Na+/Ca2+ exchange to Ca2+ homeostasis/contraction in ASM cells has also been demonstrated [15, 16]. SOCE is also crucial in enabling the cell to re-establish its levels of Ca2+ to those appropriate for each intracellular location and, hence, allows the cell to return to a basal state.
Refilling of intracellular stores is clearly a crucial stage of Ca2+ homeostasis, and in the past decade understanding of the molecules and mechanisms involved has advanced rapidly with the discovery of the STIM and Orai families of proteins and increased understanding of the roles of transient receptor potential (TRP) channels. In this chapter we will describe the current understanding of STIM, Orai and canonical TRP (TRPC) channels and how they orchestrate store refilling. We will also address some of the emerging evidence for the involvement of SOCE in ASM cell physiology and pathophysiology. Although some general concepts may be drawn from studies in non-ASM cells, where possible we will focus on what is known specifically in ASM cells.
2 ICRAC and ISOC
In the absence of a molecular definition of the mechanism of SOCE, considerable efforts went into biophysically characterizing the currents underlying Ca2+ entry, with the ICRAC current representing the best characterized SOCE current. ICRAC is defined as a small-conductance (0.02 pS), non-voltage-gated, inwardly rectifying and highly Ca2+-selective (approx. 1,000-fold selective for Ca2+ over Na+) current [44]. In ASM cells, a small, transient inward current, consistent with ICRAC (i.e. a positive reversal potential and limited outward rectification) was identified [46]. However, in common with many other cell types, including vascular smooth muscle [1], larger, less Ca2+-selective SOC currents (ISOC) have been observed in ASM cells. Indeed, store depletion with cyclopiazonic acid (CPA) has been shown to elicit a larger, more outwardly rectifying cation current in both bovine [25] and human [45, 46, 61] ASM cells. These findings highlight that ASM cells can utilize multiple pathways to gate Ca2+ in response to store depletion, adding further complexity to the task of dissecting the molecular determinants of SOCE.
3 STIM
Stromal interaction molecules (STIM) STIM1 and STIM2 were first reported in 1996 [42]; however, a role for STIM in Ca2+ signalling was not suggested until 2005, when two RNAi screens highlighted STIM as a modulator of Ca2+ [32, 52]. The field has since advanced rapidly, and STIM is now recognized as the key molecule alerting cells to increase the flow of Ca2+ across the plasma membrane following depletion of intracellular stores.
The domain architecture of STIM1 and STIM2 has been carefully researched and is shown in Fig. 1. Apart from a small proportion of STIM1 molecules which have been observed on the plasma membrane, STIMs consist of one transmembrane region with the N-terminus located in the lumen of the ER store and the soluble C-terminus projecting into the cytosol [59]. Systematic mutagenesis experiments have revealed the protein domains which are crucial for Ca2+ sensing, subcellular reorganization, punctae formation and facilitation of a CRAC current. The step-by-step role of STIM in the regulation of SOCE was recently reviewed by Michael Cahalan [11] and is summarized schematically in Fig. 2.
Schematic illustration of molecular domains of STIM1 and STIM2. Both proteins consist of a single transmembrane domain (TM), separating cytoplasmic and intraluminal portions of the proteins. The N-terminal signal peptides (S) are cleaved during translation. The intraluminal domains contain canonical Ca2+-binding EF-hand domains (cEF), non-Ca2+-binding hidden EF-hand domains (hEF) and a sterile α-motif (SAM). The cytoplasmic domains contain two coiled-coil domains (CC1 and CC2), a proline/serine-rich domain (P/S) and a C-terminal lysine-rich domain (K), involved in phospholipid interactions. The STIM-Orai-activating region (SOAR) within STIM1 is also indicated
The role of STIM1 and Orai in Ca2+ store refilling in ASM. The four images (a–d) illustrate the sequential process of intracellular Ca2+ release, store-operated Ca2+ entry and Ca2+ store refilling in response to activation of the B2 bradykinin receptor in ASM cells. In each case, the graph in the bottom left-hand corner demonstrates the relative Ca2+ concentration in the cytoplasm occurring under the conditions depicted in the corresponding figure. (a) Under basal conditions the vast majority of STIM1 molecules are found spanning the membrane of intracellular stores with the SOAR-containing C-terminus located in the cytoplasm and the SAM- and EF-domain-containing N-terminus located inside the intracellular store. At resting levels of Ca2+ within the ER store (~400 μM), STIM1 is believed to exist as a dimer. Ca2+ ions bound to the EF-hand regions of STIM1 maintain the localization and conformation observed under basal conditions. SERCA pumps maintain basal Ca2+ levels within the ER stores by actively pumping Ca2+ ions into the store. (b) Exposure of the ASM cell to an agonist such as bradykinin promotes activation of the bradykinin B2 GPCR and of its downstream signaling pathway [via Gαq and PLC-induced inositol 1,4,5-trisphosphate (IP3) generation], resulting in activation of the IP3 receptor (IP3R). (c) Activation of IP3R drives the release of Ca2+ ions from the ER stores into the cytoplasm, resulting in a net drop in ER store Ca2+ concentration. When the concentration reaches ~300 μM, the lost contact between Ca2+ ions and the EF-hand domains of the STIM1 molecules prompts STIM1 to undergo conformational changes, exposing the SOAR domain. STIM1 also rapidly oligomerizes and translocates along the ER membrane to regions in close proximity to the plasma membrane. (d) The exposure of the SOAR domain allows Orai molecules on the plasma membrane to be harnessed, resulting in punctae containing STIM1 and Orai. They are believed to exist in a 1:1 ratio of STIM1 dimers to Orai subunits, i.e. eight STIM1 molecules interacting with one tetrameric Orai molecule. As a result of these interactions, extracellular Ca2+ enters the cell via the Orai channel, increasing intracellular Ca2+ and allowing the refilling of ER stores via SERCA activity. As intracellular Ca2+ returns to resting levels, the localization and conformation of STIM1 and Orai also return to the basal conditions depicted in Fig. 2a
Under basal conditions, STIMs likely exist as dimers with Ca2+ ions bound to the cEF-hand domain in the N-terminus. The combined sterile-α motif (SAM) and EF-hand domains function as highly sensitive Ca2+ sensors, and when ER Ca2+ stores are depleted, these Ca2+ ions are released from STIMs, resulting in a conformational change. When the exodus of Ca2+ from ER stores leads to an ER luminal concentration of less than approx. 300 μM, the “empty-handed” STIMs undergo a conformational change exposing the STIM-Orai activating region (SOAR) domain. These “empty handed” STIMs are driven to oligomerize and then translocate along the ER membrane to regions where the ER membrane is in close proximity (one study suggests 10–25 nm [65]) to the plasma membrane (shown schematically in Fig. 2 and in human ASM cells in Fig. 3). In addition to conformational changes in STIMs, the mechanism by which STIMs translocate along the ER membrane following store depletion also involves remodeling of the ER, and the details of this process were revealed by elegant experimentation and systematically reviewed in 2011 by Shen et al. [54].
To observe the cellular localization of STIM and Orai, researchers commonly use recombinant versions fused to fluorescent proteins which can be transiently expressed in cells. In this series of images from our laboratory, the same human ASM cell is shown overexpressing STIM1 fused to a yellow fluorescent protein (YFP) and Orai fused to a cyan fluorescent protein (CFP) (STIM1-YFP and Orai-CFP respectively). The top row of images (a, c, e, and g) shows STIM1-YFP, whereas the bottom row (b, d, f, and h) shows Orai-CFP. Each vertical set of panels represents a different time point, with a and b imaged at time 0, c and d at 1 min, e and f at 6 min and g and h at 8 min. Thus, in human ASM cells under basal conditions and in the presence of low (0.1 mM) extracellular Ca2+, STIM1-YFP exhibits a cytoplasmic distribution (panel a), whereas Orai-CFP localizes more to the plasma membrane (panel b) [7]. Following store depletion induced by combined exposure to 1 μM bradykinin (acting via the mechanisms depicted in Fig. 2) and the SERCA pump inhibitor 1 μM thapsigargin, both STIM1-YFP and Orai-CFP alter their cellular locations and co-localize in punctae (panels c–f). Removal of bradykinin and thapsigargin from the extracellular environment, combined with perfusion of buffer containing 2 mM extracellular Ca2+ into the system, causes the punctae to disperse, and both STIM1-YFP and Orai-CFP begin to return to their initial cellular locations (g and h)
As the name suggests, the SOAR domain of STIMs is that responsible for the interaction between STIMs and Orai (Orai is described below in Sect. 4). As observed and described in Figs. 2 and 3, aggregates of STIM and Orai molecules form junctional assemblies, resulting in an influx of extracellular Ca2+ into the cytoplasm. Although not yet confirmed in ASM cells, in other cell systems a number of binding and regulatory proteins have been identified which can also modulate this process. These include junctate, calmodulin, CRAC regulatory protein 2A, Golli and SOCE-associated regulatory factor; their putative roles have recently been reviewed [56, 58]. Roles for these proteins have been demonstrated in both the formation and dissociation of junctional assemblies. Whilst Orai channels appear to be turned off by a calcium-dependent inactivation (CDI) process involving the STIM1 cytoplasmic inhibitory domain region, STIM1 itself returns to its resting conformation and location following the increase in Ca2+ concentration within the ER stores [56].
Peel et al. confirmed the expression of STIM1 and STIM2 in human cultured ASM cells in 2006 [45]. Using siRNA specifically targeted against STIM1 or STIM2, a functional role was found for STIM1 (but not STIM2), with STIM1 knockdown leading to decreased store-operated Ca2+ influx following store depletion by CPA. Interestingly, the functional importance of STIM1 varied according to the mechanism by which intracellular stores were depleted, with Ca2+ re-entry following histamine-mediated store depletion being much more susceptible to STIM1 knockdown than that following exposure to bradykinin [45].
4 Orai
Following on from the identification of the STIM proteins as key mediators in the SOCE process, a further significant advance was made with the discovery of the Orai family of proteins [20]. Named after the sisters guarding the gates of heaven in Greek mythology, three Orai genes have been identified (Orai1–3) from genome-wide RNAi screens, each encoding a protein containing four transmembrane domains, with both N- and C-termini located intracellularly (Fig. 4) [20, 63, 69]. This topology did not immediately suggest that the Orai proteins were ion channels, yet Orai1 (also known as CRACM) appears to constitute the pore-forming subunits of ICRAC channels. A modified linkage analysis identified a single point mutation in Orai1 (R91W), which leads to severe combined immunodeficiency (SCID) syndrome through the disruption of Ca2+ entry in T-cells [20]. The executive role of Orai1 in SOCE is further supported by the findings that ICRAC activity is rescued in SCID patients’ T-cells by expression of wild-type Orai1 [20] and that the R91W mutation in Orai1 ablates ICRAC in cells [20, 63, 69]. Finally, when recombinant Orai1 is co-expressed with STIM1, large ICRAC currents can be detected with properties very similar to those of native ICRAC [36, 47, 57, 69].
Schematic illustration of Orai1. Orai1 consists of four transmembrane domains (TM1–TM4), with intracellular N- and C-termini. The second extracellular domain (between TM3 and TM4) is heavily glycosylated, and the C-terminus contains a coiled-coil (CC) domain. The C-terminus of Orai1 (in particular the coiled-coil domain) plays a critical role in STIM1 binding, but the role of the N-terminus in association with STIM1 is less clear (see [19] for review)
The functional roles of Orai2 and Orai3 remain somewhat unclear, but both can couple with STIM1 to generate ICRAC-like channels, with properties slightly different from those of the Orai1-containing channels [17, 33]. In addition, functional Orai channels appear to exist as tetramers [29, 37], with hetero-oligomerization between Orai isoforms likely to generate further diversity [33]. How these multiple potential channels relate to the variety of SOC channels observed in vivo remains to be established.
Using an approach identical to that adopted for investigations into the role of STIMs in human cultured ASM cells, Peel et al. uncovered the contribution of the Orai proteins to store refilling [46]. Expression studies confirmed that all three Orai isoforms were present at the level of mRNA in ASM. However, due to a lack of availability of antibodies against Orai2 or Orai3 at that time, only the presence of Orai1 could be confirmed at the protein level. Subsequent siRNA-based experiments revealed a role for Orai1 but not Orai2 in both CPA- and thapsigargin-mediated Ca2+ influx. The role of Orai1 in ASM cell SOCE (in response to CPA) was recently confirmed by Sathish et al. [53] using siRNA targeting Orai1. Interestingly, Peel et al. [46] also found that Orai3 knockdown resulted in a decrease in both CPA-mediated store release and subsequent Ca2+ influx, suggesting that this isoform could regulate basal Ca2+ levels or Ca2+ release from stores.
Electrophysiologically, cultured human ASM cells exhibited a two-component, store-operated current following exposure to the SERCA inhibitor CPA [46]. The first component was a small, transient inward current with characteristics typical of ICRAC (very positive reversal potential with limited outward rectification), while a subsequent component was more similar to the ISOC currents previously reported in human bronchial smooth muscle cells [61]. The initial ICRAC-like current was inhibited by Orai1 depletion, whilst the ISOC-like current was relatively unaffected [46]. These findings suggest a key role for Orai1 in the ICRAC-like current, consistent with findings in other systems [20, 63, 69], but the molecular nature of the larger ISOC-like current remains unclear. It is likely that one or more of the five TRPC homologues identified in human ASM cells (TRPC1, 3, 4, 5 and 6) [14, 40, 64] might contribute to this current (see Sect. 5 for further discussion).
In addition to STIM1, numerous other Orai1 binding partners have been identified [see [58] for a review]. For instance, the N-terminus of Orai1 has been demonstrated to interact with caveolin-1 to regulate dynamin-dependent internalization of the channel in oocytes [67]. An interaction between caveolin-1 and Orai1 may be important in regulating SOCE in ASM cells, as it was recently reported that caveolin-1 over-expression enhanced Orai1 levels and elevated SOCE, whilst siRNA-mediated knockdown of caveolin-1 blunted SOCE and reduced Orai1 expression [53]. The mechanism of this regulation by caveolin-1 has not been investigated, but given the findings in oocytes [67], it would be interesting to examine whether manipulations in caveolin-1 expression altered the internalization of the channel in ASM cells.
5 TRPC
The TRPC family consists of seven genes (TRPC1–7), which have been proposed as key molecular components of the non-selective cation currents (NSCCs) found in a variety of excitable and non-excitable cells [38]. In human ASM cells, five members of the TRPC family (TRPC1, 3, 4, 5 and 6) have been identified at the mRNA level, with TRPC1, 4, 5 and 6 confirmed at the protein level [14, 40, 64]. However, the functions of these TRPC channels in ASM are less well defined.
In human ASM cells, Corteling et al. [14] observed a histamine-induced Ca2+ entry pathway with characteristics similar to those of TRPC-dependent entry, while the large ISOC currents identified in ASM cells [46, 61] were also consistent with TRPC channel activity. Indeed, Sweeney et al. found that TRPC1 mRNA was elevated under conditions in which ISOC was enhanced (in proliferating cells), suggesting a role for TRPC1 in mediating at least part of the observed ISOC current. However, a causal link between TRPC1 mRNA levels and ISOC was not firmly established, so this remains speculative. In contrast, TNFα treatment selectively increased TRPC3 expression in human ASM cells, which was demonstrated to be responsible for an elevated basal intracellular Ca2+ and enhanced SOCE, suggesting a pathophysiological role for TRPC3 in inflammatory airway disease [64].
But which TRPC isoforms are involved in gating Ca2+ in healthy ASM cells? The role of TRPC6 was investigated in guinea pig ASM cells, using siRNA to knock down the channel [23]. The researchers found that TRPC6 depletion had no effect on oleyl acetyl glycerol (OAG)-mediated Ca2+ entry, suggesting that TRPC6 is not a primary Ca2+-conducting channel in ASM cells. However, the authors suggested that the channel could still be contributing to NSCCs without directly gating Ca2+ if Na+ ions were the main conductance through TRPC6, as has been demonstrated in human embryonic kidney (HEK) cells [18].
In contrast, TRPC3 was reported to be crucial in generating NSCCs (whose constitutive activity at rest contributes to the relatively depolarized resting membrane potential) in normal mouse ASM cells, with an emerging role for TRPC1 in an asthmatic mouse model [66]. This differs somewhat from the findings of White et al. [64], who only found a significant expression/function of TRPC3 following TNFα treatment, but this may reflect the different species used in the two studies. The role of TRPC isoforms in mediating Ca2+ entry in ASM cells therefore remains unresolved. Indeed, it has been argued that the major cellular role of TRPC channels is not in SOCE but in receptor-operated Ca2+ entry, as a result of their sensitivity to diacylglycerol, generated predominantly by PLC activity (see [50] and references therein).
The potential for TRPC channels to interact with STIM and Orai proteins adds a further layer of complexity to the study of their role in Ca2+ homeostasis and may partly explain the difficulties in clearly identifying their functions. It is possible that STIM1 provides a common mechanism for sensing store depletion and stimulating the activity of an array of store-operated currents, since it has been shown to interact with TRPC1-6, in addition to the Orai family (see [11] and [68] for a review). For instance, TRPC1 and TRPC4 have recently been demonstrated to interact with STIM1 and form functional store-operated channels in murine and human lung endothelial cells [60]. Furthermore, Orai1 has been reported to regulate or contribute to TRPC currents in a variety of systems [30, 31, 41]. So what is the nature of the relationship between STIM1, Orai1 and TRPC channels and how does it relate to the range of store-operated currents and Ca2+ signals observed in cells?
It has been established in a number of cell backgrounds that while the interaction between STIM1 and Orai1 generates an ICRAC current, the ISOC current requires the expression of STIM1, Orai1 and TRPC1 [12, 13, 30]. As a result, in Jurkat cells, where ICRAC is the predominant store-operated current, only Orai1 (and STIM1) is required to mediate SOCE [30]. However, in other cells (such as HEK-293 cells), SOCE also requires TRPC1 expression as a result of a dependence on ISOC for Ca2+ entry [12, 30]. Kim et al. [30] found that Orai1 and TRPC1 were mutually dependent upon each other for their interaction with STIM1 and concluded that they were present within the same complex in HEK-293 cells. However, Cheng et al. [13] presented an alternative model in human salivary gland cells, in which STIM1 complexes with TRPC1 and Orai1 separately (to generate ICRAC and NSCC currents respectively). They propose that Ca2+ entry through ICRAC is necessary for the insertion of TRPC1 into the plasma membrane, generating a subsequent NSCC through TRPC1/STIM1 complexes. Intriguingly, they reported that ICRAC and the NSCC performed distinct functions within the cell, with ICRAC leading to nuclear factor of activated T-cell (NFAT) stimulation and the NSCC being responsible for NFκB stimulation and sustained KCa channel activity [13]. The potential for generating multiple intracellular signals via distinct SOCE pathways would be worthy of investigation in ASM cells, where two components of store-operated current have been isolated [46].
6 Plasma Membrane Sodium/Calcium Exchanger
The plasma membrane sodium/calcium exchanger (NCX) is an ion transporter protein which imports three sodium ions into a cell in exchange for one calcium ion via an electrochemical gradient. However, an excess of sodium within the cell can force the NCX into reverse mode and hence play a role in Ca2+ influx into the cell. While this system has been extensively researched in other cells, most notably cardiomyocytes, only a few studies have researched the role of NCX transporters in ASM. Studies using KB-R7943, a relatively selective antagonist of the reverse mode of NCX, reveal a role for this transporter in store refilling as exposure to KB-R7943 decreased ASM contraction induced by acetylcholine, histamine, 5-hydroxytryptamine or caffeine [15, 26, 27, 34]. However, it should be noted that KB-R7943 has recently been shown to block L-type VDCCs in addition to NCX [21]. In the light of the potential role of L-type VDCCs in ASM Ca2+ homeostasis, e.g. [15], results obtained using KB-R7943 should perhaps be interpreted with caution.
The NCX transporter is encoded for by three genes (NCX1, 2 and 3), with NCX1 occurring as diverse splice variants. In human ASM cells only NCX1 has been identified and, unlike cardiomyocytes in which NCX1.1 is the predominant functional variant, it is variant NCX1.3 which is present in human ASM [34, 48]. Liu et al. observed that NCX1.3 was functional in human ASM cells in both forward and reverse mode, and these currents could be inhibited by both KB-R7943 and siRNA-mediated knockdown [34]. The similar effects of KB-R7943 and NCX1.3 siRNA suggest that, at least in these experiments, KB-R7943 was acting through NCX inhibition. Interestingly, siRNA-mediated knockdown of STIM1 also inhibited the observed outwardly rectifying current, providing the first potential link between SOC and NCX1.
7 Functional Significance of SOCE in ASM Cells
As discussed earlier, ASM intracellular Ca2+ levels impact such physiologically critical functions as contraction, migration, proliferation, cytokine secretion and cell adhesion. While the roles of STIM, Orai and SOCE have yet to be dissected for many of these aspects of cell biology, significant evidence has accrued on their role in ASM proliferation. Zou et al. utilized a short hairpin RNA (shRNA) approach to specifically knock down STIM1 and Orai1 and found this to attenuate SOCE, as expected, but also to inhibit serum- and PDGF-BB-induced ASM cell proliferation [70]. Further evidence for the involvement of SOCE in ASM proliferation was provided by Gao et al. [22], who found that IL-13 increased thapsigargin-stimulated SOCE in rat bronchial smooth muscle cells. This effect on SOCE partially contributed to the pro-proliferative effects of IL-13 on ASM cells, suggesting that enhanced SOCE could be implicated in inflammatory remodeling of the airways, such as occur in asthma [22].
Interestingly, SOCE was observed to be higher in proliferating ASM cells when compared with quiescent cells, as was expression of Orai1 [70]. Sweeney et al. [61] also reported that SOCE was enhanced in proliferating porcine ASM cells, while similar results have been obtained in vascular smooth muscle cells [5]. This seems to contrast with the well-established notion that SOCE is substantially attenuated during mitosis [49, 62]. It is possible that this discrepancy indicates a difference in Ca2+ handling during cell division in smooth muscle. However, it is worth noting that studies in ASM cells to date have relied upon the relatively crude approach of comparing SOCE in serum-starved versus serum-replete cells, whereas a more detailed dissection of SOCE/ICRAC during different phases of the cell cycle (e.g. [62]) has led to the consensus in other cell types that SOCE is lost in cells undergoing mitosis.
Direct evidence for the role of SOCE in ASM contraction is surprisingly limited, but Sweeney et al. [61] investigated the contribution of SOCE to acetylcholine (ACh)-induced constriction in rat bronchial rings. They found that in the absence of extracellular Ca2+, only a weak, transient constriction was observed in response to ACh. When extracellular Ca2+ was restored, however, a 2.8-fold greater (and more sustained) contraction was obtained, highlighting the significant contribution of SOCE to cholinergic bronchoconstriction [61]. In addition, Ohga et al. reported that the novel SOCE blocker YM-58483/BTP-2 attenuated ovalbumin-mediated bronchoconstriction in guinea pigs, illustrating that SOCE may also be important for in vivo bronchoconstriction [39].
8 Ca2+ Oscillations in ASM
Physiological levels of bronchoconstrictors often trigger sustained oscillations in intracellular Ca2+ levels, rather than large, global elevations [6]. While it is generally accepted that these oscillations predominantly result from Ca2+ store release, they require Ca2+ influx to support them, and it is believed that this influx is via SOCE [9, 50]. Indeed, Putney has recently proposed that SOCE may do more than simply replenish the pool of Ca2+ available for oscillatory release and that in some cases Ca2+ entry through Orai channels may directly generate Ca2+ oscillations and drive downstream signaling events [50].
In human ASM cells, asynchronous Ca2+ waves can occur through repetitive cycles of SR Ca2+ release and reuptake by SERCA [15]. These Ca2+ waves are important in generating contraction in intact human bronchial smooth muscle bundles and were shown to rely upon ROC/SOC entry (as well as Na+/Ca2+ exchanger and, to a lesser extent, L-type VDCCs), as they could be abolished by the ROC/SOC channel blocker SKF96365 [15]. A similar profile was observed in porcine tracheal smooth muscle bundles [16]. In addition, inhibition of SOCE ablated LTD4-induced Ca2+ oscillations in human ASM cells [35]. However, these experiments were performed on cells pretreated with IL-13, an inflammatory mediator known to enhance SOCE [22]. It may, therefore, be that the role of SOCE in Ca2+ oscillations was exaggerated in this instance, but since the IL-13 pretreatment could (to some extent) mimic the inflammatory environment found in asthmatic airways, this study might provide an indication of the contribution of SOCE to asthmatic ASM hyper-contractility [35]. Whether SOCE-derived Ca2+ acts in an executive (as proposed by Putney) or facilitatory (as commonly believed) manner in ASM cells remains to be established. The pharmacological tools utilized in the aforementioned studies are relatively poorly selective, so the use of more selective molecular techniques (e.g. siRNA targeting STIM and Orai family members) might provide stronger evidence for the role of SOCE in Ca2+ signaling/contraction, as well as greater mechanistic insight into the link between Ca2+ entry and downstream cellular function.
9 Summary
In this chapter we have discussed the mechanisms underlying Ca2+ store refilling in ASM. SOCE-mediated Ca2+ homeostasis appears to be the most functionally important Ca2+-handling process in ASM, controlling key physiological endpoints including contraction, proliferation and cytokine release. Although some key participants in SOCE have been identified and their role assessed in ASM (e.g. STIM, Orai1), there remains a significant amount of mechanistic information which has only been demonstrated in other cell systems. Whether the process of SOCE, so elegantly dissected in cell lines, occurs in the same manner in ASM cells is as yet largely unknown. Unanswered questions include the following: (1) In what combination do STIM1, Orai1 and the variety of TRPC channels expressed in ASM cells assemble to generate the observed SOCE signals? (2) Do distinct Ca2+ entry pathways generate discrete intracellular signals, each coupled to the regulation of a different subset of downstream effectors? (3) What role do Orai2 and Orai3 play in ASM cells? (4) What is the contribution of SOCE to pathophysiological changes (e.g. in contractile hyperresponsiveness) in ASM cells? These (and many other) questions provide the challenge for future research in the field of ASM Ca2+ signaling.
References
Albert AP, Saleh SN, Large WA (2008). Inhibition of native TRPC6 channel activity by phosphatidylinositol 4,5-bisphosphate in mesenteric artery myocytes. J Physiol 586(13): 3087–3095.
Barnes PJ (1998). Pharmacology of airway smooth muscle. Am J Respir Crit Care Med 158(5 Pt 3): S123-132.
Bazan-Perkins B, Flores-Soto E, Barajas-Lopez C, Montano LM (2003). Role of sarcoplasmic reticulum Ca2+ content in Ca2+ entry of bovine airway smooth muscle cells. Naunyn Schmiedebergs Arch Pharmacol 368(4): 277–283.
Bazan-Perkins B, Sanchez-Guerrero E, Carbajal V, Barajas-Lopez C, Montano LM (2000). Sarcoplasmic reticulum Ca2+ depletion by caffeine and changes of [Ca2+](i) during refilling in bovine airway smooth muscle cells. Archives of medical research 31(6): 558–563.
Berra-Romani R, Mazzocco-Spezzia A, Pulina MV, Golovina VA (2008). Ca2+ handling is altered when arterial myocytes progress from a contractile to a proliferative phenotype in culture. Am J Physiol Cell Physiol 295(3): C779–790.
Berridge MJ (2008). Smooth muscle cell calcium activation mechanisms. J Physiol 586(Pt 21): 5047–5061.
Billington CK, Peel SE, Swan C, Liu X, Liu B, Hall IP (2010). Real Time Confocal Imaging and FRET-based Studies of Dynamic Stim1 and Orai Interactions in Human Airway Smooth Muscle cells during Store-Operated Calcium Influx. Am J Respir Crit Care Med 181: A5306.
Billington CK, Penn RB (2003). Signaling and regulation of G protein-coupled receptors in airway smooth muscle. Respir Res 4: 2.
Bird GS, Putney JW, Jr. (2005). Capacitative calcium entry supports calcium oscillations in human embryonic kidney cells. J Physiol 562(Pt 3): 697–706.
Bourreau JP, Abela AP, Kwan CY, Daniel EE (1991). Acetylcholine Ca2+ stores refilling directly involves a dihydropyridine-sensitive channel in dog trachea. Am J Physiol 261(3 Pt 1): C497-505.
Cahalan MD (2009). STIMulating store-operated Ca(2+) entry. Nat Cell Biol 11(6): 669–677.
Cheng KT, Liu X, Ong HL, Ambudkar IS (2008). Functional requirement for Orai1 in store-operated TRPC1-STIM1 channels. J Biol Chem 283(19): 12935–12940.
Cheng KT, Liu X, Ong HL, Swaim W, Ambudkar IS (2011). Local Ca(2)+ entry via Orai1 regulates plasma membrane recruitment of TRPC1 and controls cytosolic Ca(2)+ signals required for specific cell functions. PLoS biology 9(3): e1001025.
Corteling RL, Li S, Giddings J, Westwick J, Poll C, Hall IP (2004). Expression of transient receptor potential C6 and related transient receptor potential family members in human airway smooth muscle and lung tissue. Am J Respir Cell Mol Biol 30(2): 145–154.
Dai JM, Kuo KH, Leo JM, Pare PD, van Breemen C, Lee CH (2007). Acetylcholine-induced asynchronous calcium waves in intact human bronchial muscle bundle. Am J Respir Cell Mol Biol 36(5): 600–608.
Dai JM, Kuo KH, Leo JM, van Breemen C, Lee CH (2006). Mechanism of ACh-induced asynchronous calcium waves and tonic contraction in porcine tracheal muscle bundle. Am J Physiol Lung Cell Mol Physiol 290(3): L459-469.
DeHaven WI, Smyth JT, Boyles RR, Putney JW, Jr. (2007). Calcium inhibition and calcium potentiation of Orai1, Orai2, and Orai3 calcium release-activated calcium channels. J Biol Chem 282(24): 17548–17556.
Estacion M, Sinkins WG, Jones SW, Applegate MA, Schilling WP (2006). Human TRPC6 expressed in HEK 293 cells forms non-selective cation channels with limited Ca2+ permeability. J Physiol 572(Pt 2): 359–377.
Fahrner M, Muik M, Derler I, Schindl R, Fritsch R, Frischauf I, et al. (2009). Mechanistic view on domains mediating STIM1-Orai coupling. Immunological reviews 231(1): 99–112.
Feske S, Gwack Y, Prakriya M, Srikanth S, Puppel SH, Tanasa B, et al. (2006). A mutation in Orai1 causes immune deficiency by abrogating CRAC channel function. Nature 441(7090): 179–185.
Flores-Soto E, Reyes-Garcia J, Sommer B, Chavez J, Barajas-Lopez C, Montano LM (2012). PPADS, a P2X receptor antagonist, as a novel inhibitor of the reverse mode of the Na(+)/Ca(2)(+) exchanger in guinea pig airway smooth muscle. Eur J Pharmacol 674(2–3): 439–444.
Gao YD, Zou JJ, Zheng JW, Shang M, Chen X, Geng S, et al. (2010). Promoting effects of IL-13 on Ca2+ release and store-operated Ca2+ entry in airway smooth muscle cells. Pulm Pharmacol Ther 23(3): 182–189.
Godin N, Rousseau E (2007). TRPC6 silencing in primary airway smooth muscle cells inhibits protein expression without affecting OAG-induced calcium entry. Molecular and cellular biochemistry 296(1–2): 193–201.
Gosens R, Roscioni SS, Dekkers BG, Pera T, Schmidt M, Schaafsma D, et al. (2008). Pharmacology of airway smooth muscle proliferation. Eur J Pharmacol 585(2–3): 385–397.
Helli PB, Janssen LJ (2008). Properties of a store-operated nonselective cation channel in airway smooth muscle. Eur Respir J 32(6): 1529–1539.
Hirota S, Janssen LJ (2007a). Store-refilling involves both L-type calcium channels and reverse-mode sodium-calcium exchange in airway smooth muscle. Eur Respir J 30(2): 269–278.
Hirota S, Pertens E, Janssen LJ (2007b). The reverse mode of the Na(+)/Ca(2+) exchanger provides a source of Ca(2+) for store refilling following agonist-induced Ca(2+) mobilization. Am J Physiol Lung Cell Mol Physiol 292(2): L438-447.
Hoth M, Penner R (1992). Depletion of intracellular calcium stores activates a calcium current in mast cells. Nature 355(6358): 353–356.
Ji W, Xu P, Li Z, Lu J, Liu L, Zhan Y, et al. (2008). Functional stoichiometry of the unitary calcium-release-activated calcium channel. Proc Natl Acad Sci U S A 105(36): 13668–13673.
Kim MS, Zeng W, Yuan JP, Shin DM, Worley PF, Muallem S (2009). Native Store-operated Ca2+ Influx Requires the Channel Function of Orai1 and TRPC1. J Biol Chem 284(15): 9733–9741.
Liao Y, Erxleben C, Yildirim E, Abramowitz J, Armstrong DL, Birnbaumer L (2007). Orai proteins interact with TRPC channels and confer responsiveness to store depletion. Proc Natl Acad Sci U S A 104(11): 4682–4687.
Liou J, Kim ML, Heo WD, Jones JT, Myers JW, Ferrell JE, Jr., et al. (2005). STIM is a Ca2+ sensor essential for Ca2+−store-depletion-triggered Ca2+ influx. Curr Biol 15(13): 1235–1241.
Lis A, Peinelt C, Beck A, Parvez S, Monteilh-Zoller M, Fleig A, et al. (2007). CRACM1, CRACM2, and CRACM3 are store-operated Ca2+ channels with distinct functional properties. Curr Biol 17(9): 794–800.
Liu B, Peel SE, Fox J, Hall IP (2010). Reverse mode Na+/Ca2+ exchange mediated by STIM1 contributes to Ca2+ influx in airway smooth muscle following agonist stimulation. Respir Res 11: 168.
Matsumoto H, Hirata Y, Otsuka K, Iwata T, Inazumi A, Niimi A, et al. (2012). Interleukin-13 enhanced Ca2+ oscillations in airway smooth muscle cells. Cytokine 57(1): 19–24.
Mercer JC, Dehaven WI, Smyth JT, Wedel B, Boyles RR, Bird GS, et al. (2006). Large store-operated calcium selective currents due to co-expression of Orai1 or Orai2 with the intracellular calcium sensor, Stim1. J Biol Chem 281(34): 24979–24990.
Mignen O, Thompson JL, Shuttleworth TJ (2008). Orai1 subunit stoichiometry of the mammalian CRAC channel pore. J Physiol 586(2): 419–425.
Montell C, Birnbaumer L, Flockerzi V (2002). The TRP channels, a remarkably functional family. Cell 108(5): 595–598.
Ohga K, Takezawa R, Yoshino T, Yamada T, Shimizu Y, Ishikawa J (2008). The suppressive effects of YM-58483/BTP-2, a store-operated Ca2+ entry blocker, on inflammatory mediator release in vitro and airway responses in vivo. Pulm Pharmacol Ther 21(2): 360–369.
Ong HL, Chen J, Chataway T, Brereton H, Zhang L, Downs T, et al. (2002). Specific detection of the endogenous transient receptor potential (TRP)-1 protein in liver and airway smooth muscle cells using immunoprecipitation and Western-blot analysis. Biochem J 364(Pt 3): 641–648.
Ong HL, Cheng KT, Liu X, Bandyopadhyay BC, Paria BC, Soboloff J, et al. (2007). Dynamic assembly of TRPC1-STIM1-Orai1 ternary complex is involved in store-operated calcium influx. Evidence for similarities in store-operated and calcium release-activated calcium channel components. J Biol Chem 282(12): 9105–9116.
Oritani K, Kincade PW (1996). Identification of stromal cell products that interact with pre-B cells. J Cell Biol 134(3): 771–782.
Orrenius S, Zhivotovsky B, Nicotera P (2003). Regulation of cell death: the calcium-apoptosis link. Nat Rev Mol Cell Biol 4(7): 552–565.
Parekh AB, Putney JW, Jr. (2005). Store-operated calcium channels. Physiol Rev 85(2): 757–810.
Peel SE, Liu B, Hall IP (2006). A key role for STIM1 in store operated calcium channel activation in airway smooth muscle. Respir Res 7: 119.
Peel SE, Liu B, Hall IP (2008). ORAI and store-operated calcium influx in human airway smooth muscle cells. Am J Respir Cell Mol Biol 38(6): 744–749.
Peinelt C, Vig M, Koomoa DL, Beck A, Nadler MJ, Koblan-Huberson M, et al. (2006). Amplification of CRAC current by STIM1 and CRACM1 (Orai1). Nat Cell Biol 8(7): 771–773.
Pitt A, Knox AJ (1996). Molecular characterization of the human airway smooth muscle Na+/Ca2+ exchanger. Am J Respir Cell Mol Biol 15(6): 726–730.
Preston SF, Sha’afi RI, Berlin RD (1991). Regulation of Ca2+ influx during mitosis: Ca2+ influx and depletion of intracellular Ca2+ stores are coupled in interphase but not mitosis. Cell regulation 2(11): 915–925.
Putney JW (2011). The physiological function of store-operated calcium entry. Neurochem Res 36(7): 1157–1165.
Putney JW, Jr. (1986). A model for receptor-regulated calcium entry. Cell Calcium 7(1): 1–12.
Roos J, DiGregorio PJ, Yeromin AV, Ohlsen K, Lioudyno M, Zhang S, et al. (2005). STIM1, an essential and conserved component of store-operated Ca2+ channel function. J Cell Biol 169(3): 435–445.
Sathish V, Abcejo AJ, Thompson MA, Sieck GC, Prakash YS, Pabelick CM (2012). Caveolin-1 regulation of store-operated Ca2+ influx in human airway smooth muscle. Eur Respir J 40(2): 470–478.
Shen WW, Frieden M, Demaurex N (2011). Remodelling of the endoplasmic reticulum during store-operated calcium entry. Biology of the cell / under the auspices of the European Cell Biology Organization 103(8): 365–380.
Smyth JT, Hwang SY, Tomita T, DeHaven WI, Mercer JC, Putney JW (2010). Activation and regulation of store-operated calcium entry. J Cell Mol Med 14(10): 2337–2349.
Soboloff J, Rothberg BS, Madesh M, Gill DL (2012). STIM proteins: dynamic calcium signal transducers. Nat Rev Mol Cell Biol 13(9): 549–565.
Soboloff J, Spassova MA, Tang XD, Hewavitharana T, Xu W, Gill DL (2006). Orai1 and STIM reconstitute store-operated calcium channel function. J Biol Chem 281(30): 20661–20665.
Srikanth S, Gwack Y (2012). Orai1, STIM1, and their associating partners. J Physiol 590(Pt 17): 4169–4177.
Stathopulos PB, Ikura M (2010). Partial unfolding and oligomerization of stromal interaction molecules as an initiation mechanism of store operated calcium entry. Biochemistry and cell biology = Biochimie et biologie cellulaire 88(2): 175–183.
Sundivakkam PC, Freichel M, Singh V, Yuan JP, Vogel SM, Flockerzi V, et al. (2012). The Ca(2+) sensor stromal interaction molecule 1 (STIM1) is necessary and sufficient for the store-operated Ca(2+) entry function of transient receptor potential canonical (TRPC) 1 and 4 channels in endothelial cells. Mol Pharmacol 81(4): 510–526.
Sweeney M, McDaniel SS, Platoshyn O, Zhang S, Yu Y, Lapp BR, et al. (2002). Role of capacitative Ca2+ entry in bronchial contraction and remodeling. J Appl Physiol 92(4): 1594–1602.
Tani D, Monteilh-Zoller MK, Fleig A, Penner R (2007). Cell cycle-dependent regulation of store-operated I(CRAC) and Mg2+−nucleotide-regulated MagNuM (TRPM7) currents. Cell Calcium 41(3): 249–260.
Vig M, Peinelt C, Beck A, Koomoa DL, Rabah D, Koblan-Huberson M, et al. (2006). CRACM1 is a plasma membrane protein essential for store-operated Ca2+ entry. Science 312(5777): 1220–1223.
White TA, Xue A, Chini EN, Thompson M, Sieck GC, Wylam ME (2006). Role of transient receptor potential C3 in TNF-alpha-enhanced calcium influx in human airway myocytes. Am J Respir Cell Mol Biol 35(2): 243–251.
Wu MM, Buchanan J, Luik RM, Lewis RS (2006). Ca2+ store depletion causes STIM1 to accumulate in ER regions closely associated with the plasma membrane. J Cell Biol 174(6): 803–813.
Xiao JH, Zheng YM, Liao B, Wang YX (2010). Functional role of canonical transient receptor potential 1 and canonical transient receptor potential 3 in normal and asthmatic airway smooth muscle cells. Am J Respir Cell Mol Biol 43(1): 17–25.
Yu F, Sun L, Machaca K (2010). Constitutive recycling of the store-operated Ca2+ channel Orai1 and its internalization during meiosis. J Cell Biol 191(3): 523–535.
Yuan JP, Kim MS, Zeng W, Shin DM, Huang G, Worley PF, et al. (2009). TRPC channels as STIM1-regulated SOCs. Channels (Austin) 3(4): 221–225.
Zhang SL, Yeromin AV, Zhang XH, Yu Y, Safrina O, Penna A, et al. (2006). Genome-wide RNAi screen of Ca(2+) influx identifies genes that regulate Ca(2+) release-activated Ca(2+) channel activity. Proc Natl Acad Sci U S A 103(24): 9357–9362.
Zou JJ, Gao YD, Geng S, Yang J (2011). Role of STIM1/Orai1-mediated store-operated Ca(2)(+) entry in airway smooth muscle cell proliferation. J Appl Physiol 110(5): 1256–1263.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Billington, C.K., Hall, I.P., Nelson, C.P. (2014). Mechanisms Underlying Ca2+ Store Refilling in Airway Smooth Muscle. In: Wang, YX. (eds) Calcium Signaling In Airway Smooth Muscle Cells. Springer, Cham. https://doi.org/10.1007/978-3-319-01312-1_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-01312-1_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-01311-4
Online ISBN: 978-3-319-01312-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)