Abstract
Transtibial amputation involves the loss of the ankle joint, distal tibia, and fibula, while preserving the knee joint. For this type of amputation, a prosthesis is required to replace the missing limb for the patient to continue their daily activities. However, some patients experience poor prosthetic adaptation, leading to gait abnormalities. A case study was conducted on a patient with left transtibial amputation to evaluate the kinetics and kinematics using baropodometry, accelerometry, and electromyography, aiming to identify potential anomalies experienced by the patient during short walking periods. Static baropodometry analysis indicated that the patient had a greater distribution of body weight on the forefoot, resulting in a forward body displacement and instability. The overall symmetry index was below normal values, indicating differences in gait between the left and right foot. Additionally, the muscle coactivation index was above normal values, indicating excessive muscle contraction and consequently poor muscle coordination.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Transtibial amputation constitutes a significant impairment to the neural, muscular, and skeletal systems, involving the loss of the ankle, distal tibia, and fibula articulation while retaining the knee joint. Individuals with this type of amputation experience challenges in walking and increased energy consumption [1]. Patients with transtibial amputation require a prosthesis that enhances efficiency and gait pattern during both static and dynamic phases. This involves cushioning impacts from body weight and achieving proper prosthetic suspension in the swinging phase as well as stable support during the stance phase [2]. Achieving this involves assessing biomechanical variables such as baropodometry, accelerometry, and electromyography to understand how prosthetic adaptation occurs in amputee patients. Consequently, there has been a growing focus on prosthetic alignment studies, particularly regarding the impact of socket alignment with the foot and the assessment of associated energy costs [2].
Among baropodometric variables, weight distribution assesses how weight is borne by the prosthetic device and the contralateral limb in an orthostatic position [3]. Additionally, the center of pressure trajectory is associated with postural stability and balance evaluation. On the other hand, ground reaction force (GRF) identifies the effects of misalignment in prosthetic gait, indicating that misalignments increase the load on the contralateral limb and likewise extend the support phase time, as well as causing differences in vertical GRF peaks [4, 5].
Acelerometry evaluation identifies propulsion indices, describing a subject’s ability to push the center of mass forward during the single support phase [6]. The symmetry index represents the difference in percentage terms between support and swing phases of the healthy and amputated limbs [7]. The quality index characterizes a single limb, assessing the subject’s ability to correctly time and balance their gait cycle between the healthy and amputated limbs [8]. Lastly, pelvic kinematics are assessed in different planes, providing information about inclination, obliquity, and rotation during the gait cycle. Ultimately, muscle coactivation informs about the overall compensatory strategy adopted by amputees in the intact limb, where high values indicate the need for amputees to increase simultaneous activation of multiple muscles for an extended duration. This may lead to compensatory increases in stiffness, force production, and support time [9].
Biomechanical assessments are crucial for prosthesis users as they provide quantitative information about prosthetic adaptation, aiming to improve patient function and prosthetic component effectiveness in terms of user safety and stability [2]. Therefore, the main objective of this study is to evaluate kinetic and kinematic signals of lower limbs using baropodometry, accelerometry, and electromyography during the walking motion in a patient with transtibial amputation.
2 Materials and Methods
A 66-year-old patient with left transtibial amputation was evaluated. The patient reported fatigue when attempting short walks with the prosthetic provided by their healthcare institution. The study took place at the Biomechanics and Rehabilitation Laboratory of the Metropolitan Technological Institute in Medellín, Colombia. The patient participated voluntarily after signing the appropriate informed consent, which was approved by the Ethics Committee of the Metropolitan Technological Institute and adhered to the principles outlined in the Helsinki Declaration (DoH), as recommended by the World Medical Association [10].
2.1 Baropodometry Analysis
The EcoWalk plantar pressure platform (Ecosanit, Arezzo, Italy) was utilized for the study. Data processing was conducted using the EcoFoot 4.0 software developed by the same company, which includes predefined protocols for defining specific characteristics in both static and dynamic positions. This encompasses weight distribution, calculation of the center of gravity trajectory, and the ground reaction force vector.
For static position data acquisition, the patient stood on the platform, facing a fixed point, with relaxed arms and feet shoulder-width apart for 60 s (see Fig. 1). Subsequently, the patient was instructed to perform a short walk, alternating steps, to ensure recording of at least 4 steps for each foot during the dynamic assessment.
2.2 Accelerometry and Surface Electromyography (EMG) Analysis
The G-walk inertial sensor (BTS Bioengineering, Milan, Italy) was used for Accelerometry Analysis. This sensor includes an accelerometer (frequency: 4–1.000 Hz), a gyroscope (frequency: 4–8.000 Hz), and a magnetometer. For signal processing, the G-Studio software version 3.2.25.0 developed by the same company was implemented.
This device facilitates the spatial and temporal evaluation of gait parameters, including quality index, propulsion, temporal parameters, and pelvic kinematics.
The inertial sensor was placed at the S1 and S2 vertebrae level, specifically below the line connecting the two dimples of Venus, to align it accurately with the patient’s spine. Once the sensor was securely positioned, the patient received instructions to walk along a 6-m path, maintaining a natural pace. You were also asked to perform a wide turn and return to the starting point of the test. This sequence was repeated multiple times, with each repetition lasting no more than 1 min.
To analyze muscle activity using surface electromyography, the wireless electromyograph FREEEMG 1000 (BTS Bioengineering, Milan, Italy) was utilized. This device is equipped with 8 sensors and operates at a sampling frequency of 1000 Hz. For signal processing, the EMG-Analyzer software version 2.10.44.0, developed by the same company, was employed. The calculation of the coactivation index followed the methodologies outlined in previous studies [11, 12]. Electrodes were placed on the right tibialis anterior, right medial gastrocnemius, right rectus femoris, right semitendinosus, left rectus femoris and left semitendinosus as shown in Fig. 2. After the sensor was stabilized, the patient then walked a 6-m path at a natural pace until reporting fatigue, marking the end of the test.
3 Results and Discussion
3.1 Baropodometry Analysis
In the static baropodometry results, it’s observed that the right foot bears 50.1% of the load, while the left foot carries 49.9%. Furthermore, the left foot has 38.1% of the load on the forefoot, whereas the right foot records 31.3%, totaling 69.4% on the forefoot. These values suggest that the metatarsals bear the majority of the patient’s weight, leading to a forward displacement of the center of pressure, causing instability, fatigue, and wear in this area [13].
In the posterior zone, a total load of 30.5% is presented, with an uneven distribution between the feet.
The left foot bears 11.8% of the load, whereas the right foot reaches 18.8%. This discrepancy indicates that the patient doesn’t fully support the heel of the prosthetic foot, and there is a force compensation in the right foot’s heel (see Fig. 3). It’s crucial that the body weight is evenly distributed, with 50% of the load on both lower limbs, as well as anteroposteriorly, to avoid potential discomfort or long-term injuries [6].
In the dynamic analysis, for the left foot, the ground reaction force (GRF) exerted is low (68.9 kPa), representing less than 20% of the total weight. In the rearfoot, there’s a percentage of 5.49%, midfoot 2.94%, and forefoot 6.47%. These percentages add up to a total of 14.9% of the total weight, indicating that the patient exerts very little force with their left foot, possibly due to the lack of confidence they feel with the prosthesis.
On the other hand, the right foot records a higher force percentage (253.6 kPa). Specifically, there’s 15.29% in the rearfoot, 9.80% in the midfoot, and 24.31% in the forefoot, adding up to a total of 48.88% of the total weight. Although all these percentages are below normal values, the right foot shows a higher force percentage compared to the left foot and a longer time in the support phase, which is consistent with findings reported in other studies [5] (see Fig. 4).
3.2 Analysis of Accelerometry and Surface Electromyography
The global symmetry index is 1.7%, indicating that the gait cycle in both feet is not symmetric, as the value is below the normal range [8]. Furthermore, the gait cycle quality index is 88.5% in the right limb and 85.5% in the left limb, indicating that the subject lacks symmetry in accelerating the center of mass similarly during the walking cycle in the right and left feet. The closer the index is to 100, the more symmetrical the gait pattern is [7] (see Table 1).
The propulsion index presents a normal value when it’s > 5.5. In the case of this study, the values are slightly higher than the normal range, indicating that the patient has good propulsion, but might not possess all the necessary strength to execute it in the most correct and comfortable manner (see Fig. 5).
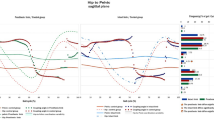
Figure 6 illustrates pelvic kinematics in all three anatomical planes. The graphs feature two continuous lines representing the right side (green) and the left side (red). The gray lines correspond to the normal range. On the right side of the figure, the symmetry index is generated for each evaluated angle, along with maximum and minimum values for each foot, and the range between these values [14].
The inclination displays a symmetry index of 73.7%, indicating alignment issues with the pelvis and a tendency towards positive values, signifying anterior pelvic movement. This relates to maximum metatarsal support and confirms the patient’s forward-leaning body posture. In pelvis obliquity, there’s a symmetry of 33.5%, with an opposing angular pattern in each limb. The right pelvis remains higher than the left, potentially indicating poor prosthetic adaptation due to gait pattern asymmetry. Finally, in pelvic rotation, a symmetry index of 62.3% is observed, indicating neutral movement (see Fig. 6). Changes in pelvic kinematics might arise from relative compensations due to different prosthetic components. Inclination can be influenced by stability in re-establishing the center of gravity, and obliquity might be influenced by prosthetic adjustments like prosthesis length and suspension system [15].
The results of muscular activity can be observed in Fig. 7. The gray band indicates the phase during which each muscle should be activated, and the absence of a band signifies the resting phase of muscular contraction. For the right foot, muscles display activation throughout most of the gait cycle, without clear relaxation during the appropriate phase. This finding is consistent with studies indicating that the intact limb increases simultaneous activation for a longer duration to compensate for stiffness, force production, and support time in the healthy limb [16]. The rectus femoris and semitendinosus muscles show peaks of electrical activity closer to normal values; however, the voltage values obtained are low, suggesting that these muscles might not be generating sufficient force to adequately contribute to the gait cycle. On the other hand, in the left lower limb, the semitendinosus muscle’s activation is not consistent but shows relatively low voltage values, indicating insufficient force generation for a proper gait cycle with the amputated limb. However, the rectus femoris displays better activation and less silence, indicating that this muscle tends to experience faster fatigue, given that it bears the weight of the prosthesis. Consequently, the foot support might be lighter.
The coactivation index reflects the postural stability of the patient [17]. According to the data reported in Table 2, the coactivation values are higher than normal, indicating that the patient has balance issues during gait.
4 Conclusions
The results of this study revealed altered biomechanical behaviors in both joint and muscular aspects in a patient with transtibial amputation, underscoring the importance of such assessments for proper prosthetic adaptation. The absence of these considerations can lead to muscular fatigue, instability, and gait difficulties, significantly impacting the patient’s quality of life. It’s important to note that this study was conducted with a single patient, thus further evaluation with a larger amputee population is crucial to obtain comparative results. Moreover, the devices used for measurements necessitate trained personnel to ensure their proper utilization. Despite limitations, this study provides vital insights in biomedicine and rehabilitation, highlighting overlooked healthcare research that ensures proper patient prosthetic adaptation and quality of life. These findings advance understanding and stress the need for broader future approaches.
References
Sarroca, N., Valero, J., Deus, J., Casanova, J., Luesma, M.J., Lahoz, M.: Quality of life, body image and self-esteem in patients with unilateral transtibial amputations. Sci. Rep. 11(1), 12559 (2021). https://doi.org/10.1038/s41598-021-91954-1
Chui, K.K., Milagros, J., Sheng-Che, Y., Lusardi, M.M.: Orthotics and Prosthetics in Rehabilitation. 4th ed. (2020)
da Fontes, C.H.S., et al.: Bodyweight distribution between limbs, muscle strength, and proprioception in traumatic transtibial amputees: a cross-sectional study. Clinics 76, e2486 (2021). https://doi.org/10.6061/clinics/2021/e2486
Kobayashi, T., et al.: Ground reaction forces during double limb stances while walking in individuals with unilateral transfemoral amputation. Front. Bioeng. Biotechnol. 10 (2023) https://doi.org/10.3389/fbioe.2022.1041060
Cárdenas, A.M., Uribe, J., Font-Llagunes, J.M., Hernández, A.M., Plata, J.A.: The effect of prosthetic alignment on the stump temperature and ground reaction forces during gait in transfemoral amputees. Gait Posture 95, 76–83 (2022). https://doi.org/10.1016/j.gaitpost.2022.04.003
Bernardini, M., Quarto, G., Del Sole, D., Bernardini, E.: Influences of postural alterations on the hemodynamic of the gait in patients with saphenous incompetence a preliminary study. . Ann. Ital. Chir. 90, 545–550 (2019)
Winiarski, S., Rutkowska-Kucharska, A., Kowal, M.: Symmetry function – an effective tool for evaluating the gait symmetry of trans-femoral amputees. Gait Posture 90, 9–15 (2021). https://doi.org/10.1016/j.gaitpost.2021.07.021
BTS Bioengineering. WALK Evaluación de La Coordinación Muscular Durante La Marcha (2020)
Tatarelli, A., et al.: Global muscle coactivation of the sound limb in gait of people with transfemoral and transtibial amputation. Sensors 20(9), 2543 (2020). https://doi.org/10.3390/s20092543
The World Medical Association. Declaración de Helsinki. Investigación médica en seres humanos Mar 21 (2017)
Boudarham, J., Hameau, S., Zory, R., Hardy, A., Bensmail, D., Roche, N.: Coactivation of lower limb muscles during gait in patients with multiple sclerosis. PLoS ONE 11(6), e0158267 (2016). https://doi.org/10.1371/journal.pone.0158267
Chow, J.W., Yablon, S.A., Stokic, D.S.: Coactivation of ankle muscles during stance phase of gait in patients with lower limb hypertonia after acquired brain injury. Clin. Neurophysiol. 123(8), 1599–1605 (2012). https://doi.org/10.1016/j.clinph.2012.01.006
Contreras, L.A.L., Ramírez, M.Á.G., G.S.P.: Distribución de presión plantar en pacientes con amputación transtibial unilateral (2018)
Izzo, R., Bertoni, M., Cejudo, A., Giovannelli, M., VardeI, C.H.: The global symmetry index, symmetry index, quality index and kinematics of the gait cycle with the synchronized contribution of the latest generation magneticinertial and electromyographic technology. Practical surveys and planning hypotheses for the revision of gesture. J. Phys. Educ. Sport 22(5), 1258–1270 (2022)
Valle, M.S., et al.: Use of a single wearable sensor to evaluate the effects of gait and pelvis asymmetries on the components of the timed up and go test, in persons with unilateral lower limb amputation. Sensors 22(1), 95 (2021). https://doi.org/10.3390/s22010095
Varrecchia, T., et al.: Common and specific gait patterns in people with varying anatomical levels of lower limb amputation and different prosthetic components. Hum. Mov. Sci. 66, 9–21 (2019). https://doi.org/10.1016/j.humov.2019.03.008
Olaya Mira, N., Soto Cardona, I.C., Martínez Osorno, L.V., Mercado Díaz, D.R., Henao Ceballos, L.M.: Evaluating the effect of a water exercise routine on the postural stability of the elderly. Colomb Med. 52(3), e2014537 (2021). https://doi.org/10.25100/cm.v52i3.4537
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Martínez, K., Soto, I.C., Pareja, E. (2024). Kinetic and Kinematic Analysis of Gait in a Patient with Transtibial Amputation: A Case Study. In: Flores Cuautle, J.d.J.A., et al. XLVI Mexican Conference on Biomedical Engineering. CNIB 2023. IFMBE Proceedings, vol 97. Springer, Cham. https://doi.org/10.1007/978-3-031-46936-7_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-46936-7_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-46935-0
Online ISBN: 978-3-031-46936-7
eBook Packages: EngineeringEngineering (R0)