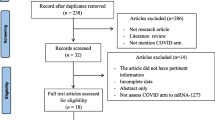
Abstract
Information regarding cutaneous adverse reactions (CARs) from non-mRNA COVID-19 vaccine remains scarce. In this narrative review, we aimed to characterize CARs following non-mRNA COVID-19 vaccination. The common CARs due to the non-mRNA vaccines were acute local injection site reactions, rash/dermatitis, or unspecified skin eruption, urticaria or angioedema, maculopapular rash, herpes zoster, delayed large local reactions, petechiae/purpura/ecchymosis, pityriasis rosea/pityriasis rosea-like eruption, vasculitis/vasculitis-like lesion, vesiculobullous lesion, and chilblains/chilblains-like lesion. Less common conditions included exacerbation of preexisting dermatosis, erythema multiforme, and severe cutaneous adverse reactions to drugs (SCARs). The types of CARs remain similar across the vaccine platforms. However, certain findings such as delayed large local reactions are found far more frequent with the mRNA vaccines. Considering widely COVID-19 vaccines administered, CARs are not common. The severity of the reactions is mostly mild. Skin reactions should not deter individuals from receiving vaccinations according to the advised schedule.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Prompt vaccination against SARS-CoV-2 plays a major role in controlling the COVID-19 pandemic. The urgent need for mass COVID-19 vaccination has sped up the research and development of COVID-19 vaccines. To date, there are various platforms of COVID-19 vaccines being used and under development; inactivated whole-virus vaccines such as Sinovac Life Sciences (CoronaVac) and Sinopharm (WIV04 and HB02): protein subunit vaccine: Novavax (NVX-CoV2373): viral vector vaccines: Oxford-AstraZeneca (ChAdOx1 nCoV-19) and Johnson and Johnson (Ad26.CoV2.S): messenger ribonucleic acid (mRNA)-based vaccines: Pfizer-BioNTech (BNT162b2) and Moderna (mRNA-1273): Deoxyribonucleic Acid (DNA) vaccines: Zydus Cadila (ZyCoV-D) (Rabaan et al. 2022). At the time of this writing, 176 vaccines are in clinical development while 199 are in preclinical phase (https://www.who.int/publications/m/item/draft-landscape-of-COVID-19-candidate-vaccines; (Rabaan et al. 2022; Lamb 2021; Robinson et al. 2021; Rerknimitr et al. 2022)).
Incidence, Prevalence, and Type of Cutaneous Adverse Reactions Following Non-mRNA COVID-19 Vaccination
COVID-19 vaccination started in December 2020, after the approval of emergency use authorization mRNA vaccines (Lamb 2021). Until now, approximately 12,248,795,623 doses have been administered worldwide (Rabaan et al. 2022). A number of cases with cutaneous adverse reactions (CARs) from the vaccine have gradually emerged, and that number continues to grow. However, considering their widely use, CARs are not common. The incidence of cutaneous reactions following mRNA vaccines was 1.9% after the first dose and 2.3% after the second dose (Robinson et al. 2021), whereas those from inactivated virus vaccine, CoronaVac, was 0.94% and 0.70% from the first and second doses, and those of viral vector, ChAdOx1 nCoV-19 were 1% and 0.52%, respectively (Rerknimitr et al. 2022). A recent systematic review and meta-analysis indicated that the pooled incidence of overall CARs was 5%. The studies involving the mRNA vaccines alone showed the incidence of 3%, whereas when other platforms were combined, the incidence was 5% (Bellinato et al. 2022).
In addition, we have conducted a systematic review and meta-analysis of CARs following COVID-19 vaccination. Of the 946,366 vaccine doses administered, we found that the pooled prevalence of overall cutaneous adverse reactions was 3.8%. Interestingly, comparing the various platforms, the mRNA vaccines exhibited the highest prevalence, followed by the viral vector-based vaccines and the inactivated SARS-CoV-2 vaccine (at 6.9%, 3.5%, and 0.9%, respectively) (Washrawirul et al. 2022). The fact that CARs occur most frequently from the mRNA vaccine administration was also confirmed by others systematic reviews and/or meta-analysis (Kroumpouzos et al. 2022; Bostan et al. 2022; Avallone et al. 2022; Seirafianpour et al. 2022). However, it is important to note that mRNA vaccine is the first platform being used. This allows a greater number of administered doses and more reported cases. Intriguingly, a meta-analysis in which CARs from mRNA were compared with those of viral vector platform, indicated that overall relative risk ratio for development of local side effects was greater with the mRNA vaccine while for non-local side effects, rash, urticaria, and angioedema, the risk was higher with the viral vector vaccine group (Shafie’ei et al. 2022).
The common CARs following the non-mRNA vaccines were acute local injection site reactions, rash/dermatitis, or unspecified skin eruption, urticaria or angioedema, maculopapular rash, herpes zoster, delayed large-local reactions, petechiae/purpura/ecchymosis, pityriasis rosea/pityriasis rosea-like eruption, vasculitis/vasculitis-like lesion, vesiculobullous lesion, and chilblains/chilblains-like lesion. Less common conditions included exacerbation of preexisting dermatosis, erythema multiforme, and severe cutaneous adverse drug reactions (SCARs) (Bellinato et al. 2022; Washrawirul et al. 2022; Avallone et al. 2022). The types of CARs remain similar across the vaccine platforms. However, certain findings such as delayed large local reactions are found far more frequent with the mRNA vaccines (Washrawirul et al. 2022; Kroumpouzos et al. 2022). Interestingly, the rate of CARs was not different between the first and second doses of vaccination (Bellinato et al. 2022; Washrawirul et al. 2022) and usually more reported in female (Kroumpouzos et al. 2022).
Cutaneous Adverse Reactions from Non-mRNA COVID-19 Vaccine
CARs following non-mRNA vaccines are like those of mRNA platforms, but a lower number of cases are reported, as discussed earlier. CARs can be categorized by the underlying immunopathogenesis as follows; type 1 hypersensitivity, type IV hypersensitivity, autoimmune-mediated, and other reactions (Shafie’ei et al. 2022).
Type 1 Hypersensitivity Reactions
Type 1, also known as immediate-type hypersensitivity reaction, includes urticaria, angioedema, and anaphylaxis.
Urticaria and angioedema are common CARs. Almost half of the reported cases were from the mRNA vaccine, leaving inactivate viral and viral vector vaccines the second and the third culprit agents (Washrawirul et al. 2022). From our study where CoronaVac and ChAdOx1 nCoV-19 were administered in healthcare personnel, urticaria was the most skin reactions observed, reported in 92 of 29,907 CoronaVac and 12 of 5322 ChAdOx1 nCoV-19 injections. The overall incidence of urticaria was n = 104/35,229 (0.3%) (Rerknimitr et al. 2022). The median onset (IQR) of urticaria was 6 (1.5, 24) h, and the duration was 2 (0.2, 8) h. Of 104 reports of urticaria, 3 (0.99%) were observed with angioedema and 2 (0.66%) were with anaphylaxis. Among urticaria following CoronaVac injections, a number of reactions with onset less than 4 h was 40 (40/92). Among these 40, there were only two reactions that the wheals presented in more than one site of the body. Recurrent eruption was found in one of these two cases with a decrease in severity, when the second dose of CoronaVac was administered. No case of anaphylaxis occurred in those with urticaria from the first dose vaccination. Therefore, we speculate that urticaria alone post CoronaVac injection is quite benign (Rerknimitr et al. 2022). From a recent perspective observational study on CARs following Sinopharm vaccination, it was shown that urticaria and angioedema occurred in 4.6 and 2.3% of the vaccine recipients, respectively (Shawky et al. 2023). Figure 4.1 shows urticaria following CoronaVac.
Regarding the treatments, 26% of the patients with urticaria and angioedema were treated with oral antihistamine followed by intravenous antihistamine and systemic steroid (at 20% and 17%, respectively). Spontaneous improvement was observed in 40% of the patients. The mean duration of the condition was for 24.28 ± 34.38 h (Washrawirul et al. 2022).
Anaphylaxis is a life-threatening reaction that occurs rarely from COVID-19 vaccination (Washrawirul et al. 2022; Banerji et al. 2021). The clinical symptoms include generalized urticaria, angioedema, diarrhea, respiratory distress, and possibility of anaphylactic shock in some patients. This type of hypersensitivity develops within 4 h after the vaccines are administered. Further dosage of the vaccine is contraindicated in patients with a history of anaphylaxis to the vaccine (Banerji et al. 2021; Alpalhão et al. 2021). The incidence of anaphylaxis following the vaccine was 7.91 cases per million (n = 41,000,000 vaccinations; 95% confidence interval [95% CI] 4.02–15.59; 26, with no report of fatalities. Compared to mRNA, the adenoviral vector (OR 0.47; 95% CI 0.33–0.68) and inactivated virus vaccines (OR 0.31; 95% CI 0.18–0.53) showed lower anaphylaxis rates (Greenhawt et al. 2021). In participants receiving CoronaVac, the reported incidence rate of anaphylaxis was 0.007–0.09% (Rerknimitr et al. 2022; Öztürk et al. 2022). The onset of the reaction was 12 ± 6 min (range, 3–15 min) after vaccination. Associated systemic symptoms are shortness of breath (75%) and alteration of consciousness (75%) (Öztürk et al. 2022). A case series from Thailand reported 12 cases of anaphylaxis following CoronaVac vaccination (Laisuan et al. 2021). The mean interval from the vaccination to the onset of symptoms was 30 min (range, 6–180 min). One-third of the patients had onset within 15 min, and two-thirds within 30 min. Fifty percent of the patients had associated urticaria and/or angioedema. Ten out of 12 patients underwent skin testing. Interestingly, only two exhibited positive skin tests. Moreover, serum tryptase was not elevated in these patients. These findings suggested that anaphylaxis following CoronaVac might be mediated through various mechanisms; possibly through IgE/FcƐR1-dependent mast cell activation or not (Laisuan et al. 2021). The excipients of the vaccines, not the viral antigen, is thought to be responsible for the immediate-type hypersensitivity reactions. For CoronaVac, aluminum is the most likely allergen, while polysorbate 80, also known as Tween 80, was responsible for the viral vector, ChAdOx1 nCoV-19, and Johnson & Johnson COVID-19 vaccines (Laisuan et al. 2021; Kounis et al. 2021). For those who experience anaphylaxis from CoronaVac, it is recommended to consider the alternative vaccine platforms, if the patients wish to have further COVID-19 vaccination (Laisuan et al. 2021).
Type IV Hypersensitivity
Examples of type IV or delayed-type hypersensitivity reactions are delayed large local (COVID arm), delayed inflammatory reactions (DIR) to hyaluronic acid dermal filler, maculopapular eruption, and erythema multiforme (Nakashima et al. 2023).
The most common CAR from vaccines is local reaction including erythema, edema, and tenderness at the injection site (Alpalhão et al. 2021). From phase 1/2 clinical trial of CoronaVac in healthy adults aged 18–59 years (Zhang et al. 2021) and 60 years and older (Wu et al. 2021), injection site reactions were found in 11–18.8%, and mucocutaneous eruption was found in 4% of the volunteers (Zhang et al. 2021; Wu et al. 2021). Similarly, the most common CAR of ChAdOx1 nCoV-19 is local reaction. Itch, redness, and swelling were observed in 2–12%, 0–2%, and 0–2% respectively from phase1/2 and 2/3 clinical trials (Folegatti et al. 2020; Ramasamy et al. 2021).
Nonetheless, delayed large local reaction (COVID arm) is different from the acute local injection site reaction in that the former takes place approximately 1 week after vaccination. This usually manifests as tender, indurated erythematous subcutaneous nodule at the injection site with possible extension to upper arm. Figure 4.2 denotes delayed large local reaction from ChAdOx1 nCoV-19. The onset was 7 days after the first vaccination and 2 days after the second dose (McMahon et al. 2021). The most common associated platform was the mRNA vaccine, followed by the viral vectors. The symptoms are usually mild. The main treatment was topical corticosteroids and oral antihistamines (Washrawirul et al. 2022; Kroumpouzos et al. 2022). Interestingly, DIR to hyaluronic acid dermal filler was reported mainly in the mRNA vaccine recipients (Washrawirul et al. 2022). Only three reported cases were associated with non-mRNA vaccines: two with ChAdOx1 nCoV-19 and one case with Sinopharm (Ortigosa et al. 2022). The reported clinical presentation was edematous inflammatory erythematous papules and nodules over the injected areas (Munavalli et al. 2022; Safir et al. 2022).
Maculopapular eruptions and erythema multiforme can be observed after the mRNA, viral vector, and inactivated virus vaccines administration (the number of reported cases in descending order) (Washrawirul et al. 2022). The distribution of maculopapular rashes can be generalized, acral, and extremities predominant (Nakashima et al. 2023).
Autoimmune-Mediated Reaction
The spike protein of COVID-19 vaccines may induce immune reactions in human via molecular mimicry. For that reason, new onset and exacerbation of autoimmune diseases have been reported after the vaccination (Nakashima et al. 2023). Examples of autoimmune diseases that were reported to be aggravated by the vaccination are cutaneous lupus erythematosus, vasculitis, bullous pemphigoid, pemphigus vulgaris, vitiligo, lichen planus, and adult-onset Still’s a disease (Washrawirul et al. 2022).
Though the exact causes of vasculitis in almost half of patients cannot be identified, it is known that drugs, vaccines, and infectious agents are major triggering factors (Antiga et al. 2015). Almost all available COVID-19 vaccines are associated with vasculitis. The highest number of reported cases were induced by mRNA vaccines, followed by viral vector, and inactivated vaccines (Washrawirul et al. 2022; Azzazi et al. 2022; Corrà et al. 2022; Bencharattanaphakhi and Rerknimitr 2021). In a review article that focused on cutaneous vasculitis, predominantly leukocytoclastic vasculitis (LCV), 39 cases were identified. The temporal relationship between vaccination and development of lesions ranged from 36 h to 20 days. Most manifested as multiple palpable purpuric papules on the legs. Figure 4.3 shows LCV associated with CoronaVac. Direct immunofluorescence (DIF) was available in 18 (46.2%) cases; 13/18 cases showed positive results. In those with positivity, heterogeneous findings were found, 12.8% with IgA and 7.7% with C3 deposition around blood vessels (Corrà et al. 2022). Our systematic review also identified newly developed and flaring of existing vasculitis cases. If presented, concomitant systemic findings were arthralgia, fever, myalgia, fatigue, diarrhea, abdominal pain, and hematuria. Most were treated with systemic corticosteroids, and the mean duration of the illness was 15.21 (13.70) days (Washrawirul et al. 2022).
In addition to LCV, a global pharmacovigilance study described 330 cases of de novo IgA vasculitis. Eighty-five percent (280/330) of patients were associated with mRNA vaccines. Moreover, there was no significant difference between mRNA and viral vector vaccines (Ramdani et al. 2023). Interestingly, skin biopsy specimens from the IgA vasculitis lesions were examined for the presence of neutrophil extracellular traps (NETs) in the dermis in a study to investigate the differences among COVID-19, COVID-19-vaccine-induced, and non-COVID-19-related IgA vasculitis. NETs deposition is thought to underlie the pathogenesis of COVID-19. From this study, there were no differences in NETs deposition among the three groups. The author concluded that it was not the directly coronavirus-induced NETs that were responsible for the development of the lesions. On the other hand, various environmental triggers including infectious agents, drugs, and vaccines might similarly trigger the development of IgA vasculitis leading to NETs deposition (Kawakami et al. 2023).
Autoimmune bullous diseases (AIBDs) have also been reported following COVID-19 vaccination either as de novo or flaring of the diseases. The reported AIBDs were mostly non-identified AIBDs, followed by bullous pemphigoid, pemphigus vulgaris, linear IgA bullous dermatosis, and pemphigus foliaceus. The mRNA vaccines were responsible in 81.1%, viral vectors in 15.5%, and inactivated vaccine in 1.8%. The onset ranged from 1 day to 6 weeks following the vaccination. The symptoms can be controlled with traditional immunosuppressive therapy (Kasperkiewicz and Woodley 2022).
Others
Pityriasis rosea (PR) was reported after all vaccine platforms. The mean onset was 9.64 (6.11) days after the vaccination and last for 49 (24.09) days. The patients may manifest with a typical herald patch followed by minute erythematous patches with collarette scale or atypical lesions. The lesion appeared on the trunk (79.17%), extremities (70.83%), and generalized (8.33%) with pruritus. This condition can be self-limited, but several patients were treated with topical corticosteroids, systemic corticosteroids, and antihistamines (Washrawirul et al. 2022). Multiple viral reactivations including human herpesvirus-6 (HHV-6), HHV-7, and Epstein-Barr virus have been demonstrated in COVID-19 infection (Drago et al. 2021). The reactivation might also play an important role in the development of PR post vaccination.
Herpes zoster reactivation is triggered by COVID-19 vaccination and is reported in all administered vaccine platforms. The mean onset was 7.76 (6.38) days after the vaccination and lasted for 12.46 ± 6.81 days. The reactivation may present after the first, second, and both doses of injections (58.73, 38.10, and 3.17, orderly). The lesions were located along the dermatome, mostly thoracic (50.88%), cranial (31.58%), lumbar (15.79%), and sacral (5.26%). Two cases were diagnosed with herpes zoster ophthalmicus (Bernardini et al. 2021). Most of the cases were treated with antiviral agents: acyclovir or valacyclovir (89.06%). Gabapentin was given in case of neuropathic pain (18.75%) simultaneously with analgesics drug (14.06%) (Washrawirul et al. 2022).
Vaccine-induced immune thrombotic thrombocytopenia (VITT) is an emerging syndrome from adenoviral-based platform vaccines, especially with ChAdOx1 nCoV-19. It is characterized by thrombocytopenia and thrombosis of the unusual sites, namely cerebral and/or splanchnic veins (Arepally and Ortel 2021). In addition to systemic symptoms, skin findings such as multiple small ecchymosis, purpura, and petechiae may be found (Bogdanov et al. 2021). In our study in which ChAdOx1 nCoV-19 was administered in healthcare personnel, we found no case of VITT. However, a case of secondary immune thrombotic thrombocytopenia (ITP) post ChAdOx1 nCoV-19 with multiple ecchymosis was observed (Rerknimitr et al. 2022). This is in keeping with the ongoing reports in the literature of newly developed ITP post COVID-19 vaccination (Welsh et al. 2021). Dermatologists should be aware of the importance of these skin findings, and prompt investigations should be undertaken in suspected cases.
Severe cutaneous adverse reactions to drug (SCARs) encompass Stevens–Johnson syndrome/toxic epidermal necrolysis (SJS/TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), acute generalized exanthematous pustulosis (AGEP), and generalized bullous fixed drug eruptions (GBFDE). These conditions are life-threatening resulting in mortality and morbidity. Few cases of SCARs due to COVID-19 vaccination have been reported. These included AGEP (n = 4), SJS-TEN (n = 4), DRESS (n = 1), GBFDE (n = 1), bullous drug eruption with features of SJS (n = 1), and inconclusive diagnosis (differential diagnosis to AGEP, DRESS, or AGEP/DRESS overlap) (n = 1). All vaccine platforms were capable of inducing these severe reactions (ChAdOx1-S 42%, BNT162b2 17%, mRNA-1273 17%, Ad26.COV2.S 8%, BBiBP 8%, and unidentified vaccines 8%). Six cases occurred in the first dose only, three cases in the second dose, and one case in both doses of vaccination. The mean onset was 9.34 (15.38) days following the vaccination, and the duration was 20.83 (9.56) days (Drago et al. 2021; Aimo et al. 2022). Other minor drug eruptions, such as fixed drug eruption, systemic drug-related intertriginous, and flexural exanthema (SDRIFE), were also stated in publications (Washrawirul et al. 2022).
Table 4.1 summarized the various cutaneous reactions to non mRNA-COVID-19 vaccines. The number of the cases from the table came from our recent meta-analysis and systematic review that included case reports, case series, case–control studies, retrospective/prospective cohort studies, and randomized controlled trials published between January 1, 2019 and December 31, 2021 (Washrawirul et al. 2022).
Conclusions
The most common CARs from non-mNRA vaccines are injection site reaction, followed by urticaria and/or angioedema, maculopapular rash, and COVID arm. Flare-up of autoimmune and preexisting dermatosis was also observed, presumably due to immune dysregulation induced by the vaccination. Delayed large local reactions and DIRs to hyaluronic dermal fillers were much more common in the mRNA platform. Skin reactions should not prevent individuals from the scheduled vaccinations.
References
Aimo C, Mariotti EB, Corrà A, Cipollini E, Le Rose O, Serravalle C, et al. Stevens-Johnson syndrome induced by Vaxvetria (AZD1222) COVID-19 vaccine. J Eur Acad Dermatol Venereol. 2022;36(6):e417–e9. https://doi.org/10.1111/jdv.17988.
Alpalhão M, Maia-Silva J, Filipe P. Severe acute respiratory syndrome coronavirus 2 vaccines and cutaneous adverse reactions: a review. Dermatitis. 2021;32(3):133–9. https://doi.org/10.1097/der.0000000000000755.
Antiga E, Verdelli A, Bonciani D, Bonciolini V, Quintarelli L, Volpi W, et al. Drug-induced cutaneous vasculitides. G Ital Dermatol Venereol. 2015;150(2):203–10.
Arepally GM, Ortel TL. Vaccine-induced immune thrombotic thrombocytopenia (VITT): what we know and Don’t know. Blood. 2021;138:293. https://doi.org/10.1182/blood.2021012152.
Avallone G, Quaglino P, Cavallo F, Roccuzzo G, Ribero S, Zalaudek I, et al. SARS-CoV-2 vaccine-related cutaneous manifestations: a systematic review. Int J Dermatol. 2022;61(10):1187–204. https://doi.org/10.1111/ijd.16063.
Azzazi Y, Abdelkader HA, Khedr H, El-Komy MHM. Extensive cutaneous leukocytoclastic vasculitis after Sinopharm vaccine: case report and review of the literature. J Cutan Pathol. 2022;49(8):736–42. https://doi.org/10.1111/cup.14235.
Banerji A, Wickner PG, Saff R, Stone CA Jr, Robinson LB, Long AA, et al. mRNA vaccines to prevent COVID-19 disease and reported allergic reactions: current evidence and suggested approach. J Allergy Clin Immunol Pract. 2021;9(4):1423–37. https://doi.org/10.1016/j.jaip.2020.12.047.
Bellinato F, Fratton Z, Girolomoni G, Gisondi P. Cutaneous adverse reactions to SARS-CoV-2 vaccines: a systematic review and meta-analysis. Vaccines (Basel). 2022;10(9):1475. https://doi.org/10.3390/vaccines10091475.
Bencharattanaphakhi R, Rerknimitr P. Sinovac COVID-19 vaccine-induced cutaneous leukocytoclastic vasculitis. JAAD Case Rep. 2021;18:1–3. https://doi.org/10.1016/j.jdcr.2021.10.002.
Bernardini N, Skroza N, Mambrin A, Proietti I, Marchesiello A, Marraffa F, et al. Herpes zoster ophthalmicus in two women after Pfizer-BioNTech (BNT162b2) vaccine. J Med Virol. 2021;94:817. https://doi.org/10.1002/jmv.27366.
Bogdanov G, Bogdanov I, Kazandjieva J, Tsankov N. Cutaneous adverse effects of the available COVID-19 vaccines. Clin Dermatol. 2021;39:523. https://doi.org/10.1016/j.clindermatol.2021.04.001.
Bostan E, Yel B, Karaduman A. Cutaneous adverse events following 771 doses of the inactivated and mRNA COVID-19 vaccines: a survey study among health care providers. J Cosmet Dermatol. 2022;21(9):3682–8. https://doi.org/10.1111/jocd.15203.
Corrà A, Verdelli A, Mariotti EB, Ruffo di Calabria V, Quintarelli L, Aimo C, et al. Cutaneous vasculitis: lessons from COVID-19 and COVID-19 vaccination. Front Med. 2022;9:1013846. https://doi.org/10.3389/fmed.2022.1013846.
Drago F, Ciccarese G, Rebora A, Parodi A. Human herpesvirus-6, -7, and Epstein-Barr virus reactivation in pityriasis rosea during COVID-19. J Med Virol. 2021;93(4):1850–1. https://doi.org/10.1002/jmv.26549.
Folegatti PM, Ewer KJ, Aley PK, Angus B, Becker S, Belij-Rammerstorfer S, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020;396(10249):467–78. https://doi.org/10.1016/s0140-6736(20)31604-4.
Greenhawt M, Abrams EM, Shaker M, Chu DK, Khan D, Akin C, et al. The risk of allergic reaction to SARS-CoV-2 vaccines and recommended evaluation and management: a systematic review, meta-analysis, GRADE assessment, and international consensus approach. J Allergy Clin Immunol Pract. 2021;9(10):3546–67. https://doi.org/10.1016/j.jaip.2021.06.006.
Kasperkiewicz M, Woodley DT. Association between vaccination and immunobullous disorders: a brief, updated systematic review with focus on COVID-19. J Eur Acad Dermatol Venereol. 2022;36(7):e498–500. https://doi.org/10.1111/jdv.18030.
Kawakami T, Yokoyama K, Ikeda T, Nishibata Y, Masuda S, Tomaru U, et al. Similar deposition of neutrophil extracellular traps in the dermis among COVID-19-associated IgA vasculitis, post-COVID-19 vaccination IgA vasculitis, and COVID-19-unrelated IgA vasculitis. J Dermatol. 2023;50:e151. https://doi.org/10.1111/1346-8138.16673.
Kounis NG, Koniari I, de Gregorio C, Velissaris D, Petalas K, Brinia A, et al. Allergic reactions to current available COVID-19 vaccinations: pathophysiology, causality, and therapeutic considerations. Vaccines (Basel). 2021;9(3):221. https://doi.org/10.3390/vaccines9030221.
Kroumpouzos G, Paroikaki ME, Yumeen S, Bhargava S, Mylonakis E. Cutaneous complications of mRNA and AZD1222 COVID-19 vaccines: a worldwide review. Microorganisms. 2022;10(3):624. https://doi.org/10.3390/microorganisms10030624.
Laisuan W, Wongsa C, Chiewchalermsri C, Thongngarm T, Rerkpattanapipat T, Iamrahong P, et al. CoronaVac COVID-19 vaccine-induced anaphylaxis: clinical characteristics and revaccination outcomes. J Asthma Allergy. 2021;14:1209–15. https://doi.org/10.2147/jaa.s333098.
Lamb YN. BNT162b2 mRNA COVID-19 vaccine: first approval. Drugs. 2021;81(4):495–501. https://doi.org/10.1007/s40265-021-01480-7.
McMahon DE, Amerson E, Rosenbach M, Lipoff JB, Moustafa D, Tyagi A, et al. Cutaneous reactions reported after Moderna and Pfizer COVID-19 vaccination: a registry-based study of 414 cases. J Am Acad Dermatol. 2021;85(1):46–55. https://doi.org/10.1016/j.jaad.2021.03.092.
Munavalli GG, Guthridge R, Knutsen-Larson S, Brodsky A, Matthew E, Landau M. COVID-19/SARS-CoV-2 virus spike protein-related delayed inflammatory reaction to hyaluronic acid dermal fillers: a challenging clinical conundrum in diagnosis and treatment. Arch Dermatol Res. 2022;314(1):1–15. https://doi.org/10.1007/s00403-021-02190-6.
Nakashima C, Kato M, Otsuka A. Cutaneous manifestations of COVID-19 and COVID-19 vaccination. J Dermatol. 2023;50:280. https://doi.org/10.1111/1346-8138.16651.
Ortigosa LCM, Lenzoni FC, Suárez MV, Duarte AA, Prestes-Carneiro LE. Hypersensitivity reaction to hyaluronic acid dermal filler after COVID-19 vaccination: a series of cases in São Paulo, Brazil. Int J Infect Dis. 2022;116:268–70. https://doi.org/10.1016/j.ijid.2022.01.024.
Öztürk B, Akdemir İ, Azap A, Çelik G, Bavbek S, Mungan D. Anaphylaxis is rare due to CoronaVac in a population of healthcare workers. Asia Pac Allergy. 2022;12(4):e35. https://doi.org/10.5415/apallergy.2022.12.e35.
Rabaan AA, Mutair AA, Hajissa K, Alfaraj AH, Al-Jishi JM, Alhajri M, et al. A comprehensive review on the current vaccines and their efficacies to combat SARS-CoV-2 variants. Vaccines (Basel). 2022;10(10):1655. https://doi.org/10.3390/vaccines10101655.
Ramasamy MN, Minassian AM, Ewer KJ, Flaxman AL, Folegatti PM, Owens DR, et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet. 2021;396(10267):1979–93. https://doi.org/10.1016/s0140-6736(20)32466-1.
Ramdani Y, Largeau B, Jonville-Bera A-P, Maillot F, Audemard-Verger A, Ramdani Y, et al. COVID-19 vaccination as a trigger of IgA vasculitis: a global pharmacovigilance study. J Rheumatol. 2023;50:564. https://doi.org/10.3899/jrheum.220629.
Rerknimitr P, Puaratanaarunkon T, Wongtada C, Wittayabusarakam N, Krithin S, Paitoonpong L, et al. Cutaneous adverse reactions from 35,229 doses of Sinovac and AstraZeneca COVID-19 vaccination: a prospective cohort study in healthcare workers. J Eur Acad Dermatol Venereol. 2022;36(3):e158–e61. https://doi.org/10.1111/jdv.17761.
Robinson LB, Fu X, Hashimoto D, Wickner P, Shenoy ES, Landman AB, et al. Incidence of cutaneous reactions after messenger RNA COVID-19 vaccines. JAMA Dermatol. 2021;157(8):1000–2. https://doi.org/10.1001/jamadermatol.2021.2114.
Safir A, Samuelov L, Sprecher E, Daniely D, Artzi O. Association between BNT162b2 vaccination and the development of delayed inflammatory reactions to hyaluronic acid-based dermal fillers—a nationwide survey. J Cosmet Dermatol. 2022;21(10):4107–13. https://doi.org/10.1111/jocd.15260.
Seirafianpour F, Pourriyahi H, Gholizadeh Mesgarha M, Pour Mohammad A, Shaka Z, Goodarzi A. A systematic review on mucocutaneous presentations after COVID-19 vaccination and expert recommendations about vaccination of important immune-mediated dermatologic disorders. Dermatol Ther. 2022;35(6):e15461. https://doi.org/10.1111/dth.15461.
Shafie’ei M, Jamali M, Akbari Z, Sarvipour N, Ahmadzade M, Ahramiyanpour N. Cutaneous adverse reactions following COVID-19 vaccinations: a systematic review and meta-analysis. J Cosmet Dermatol. 2022;21(9):3636–50. https://doi.org/10.1111/jocd.15261.
Shawky A, Elrewiny EM, Gharib K, Sallam M, Mansour M, Rageh MA. A prospective multicenter study on cutaneous reactions reported after Sinopharm COVID-19 vaccination. Int J Dermatol. 2023;62(2):221–4. https://doi.org/10.1111/ijd.16391.
Washrawirul C, Triwatcharikorn J, Phannajit J, Ullman M, Susantitaphong P, Rerknimitr P. Global prevalence and clinical manifestations of cutaneous adverse reactions following COVID-19 vaccination: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2022;36(11):1947–68. https://doi.org/10.1111/jdv.18294.
Welsh KJ, Baumblatt J, Chege W, Goud R, Nair N. Thrombocytopenia including immune thrombocytopenia after receipt of mRNA COVID-19 vaccines reported to the Vaccine Adverse Event Reporting System (VAERS). Vaccine. 2021;39(25):3329–32. https://doi.org/10.1016/j.vaccine.2021.04.054.
Wu Z, Hu Y, Xu M, Chen Z, Yang W, Jiang Z, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy adults aged 60 years and older: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect Dis. 2021;21(6):803–12. https://doi.org/10.1016/s1473-3099(20)30987-7.
Zhang Y, Zeng G, Pan H, Li C, Hu Y, Chu K, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18-59 years: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect Dis. 2021;21(2):181–92. https://doi.org/10.1016/s1473-3099(20)30843-4.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
None.
Conflicts of Interest
None.
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rerknimitr, P., Washrawirul, C., Triwatcharikorn, J. (2023). Cutaneous Reactions to Non-mRNA COVID-19 Vaccines. In: Oon, H.H., Goh, C.L. (eds) COVID-19 in Dermatology. Updates in Clinical Dermatology. Springer, Cham. https://doi.org/10.1007/978-3-031-45586-5_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-45586-5_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-45585-8
Online ISBN: 978-3-031-45586-5
eBook Packages: MedicineMedicine (R0)