Abstract
Most recent non-invasive blood pressure measurements only show systolic and diastolic pressure; some devices can alert the abnormal heart rhythm. This report aimed to show how the cuff pressure waveforms of a non-invasive blood pressure measurement device combined with an IoT system detects the abnormal heart function related to some common cardiovascular disease. We developed a blood pressure machine based on an IoT system for collecting patient data. Heart rhythm and function abnormality can be detected via the cuff pressure waveforms. The cardiac output can also be calculated following the result of treatment via heart function changes. Cuff pressure waveforms of blood pressure machines based on medical knowledge, platform IoT and data science can be used to detect abnormality of heart function and follow up the treatment result. The device was given a personal notification based on the users’ medical data. The information was also collected, saved on server, and then sent to the user’s family and their family doctor via the web interface. We recently designed, produced and implemented 30 prototypes in Vietnam from June 2022 to test their stability, accuracy, and usefulness.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
The physiological signs of the human body or human bio-signals can be measured and recorded by the machine based on sensor technology to transfer from electrical signs to biochemical ones; in the technology field of sensors, there are some main aspects such as long-term stability, resiliency and biocompatibility; this information is possible to be used for understanding the health condition and reaction to external factors when they were extracted for analyzing [1].
There are many methods to diagnose cardiovascular disease, such as an electrocardiogram (ECG) - the irregularities in the heart’s rhythm and structure can be detected by these electrical signals; echocardiography – the images of the heart’s structure and function can be shown detailed by this non-invasive exam, cardiac catheterization - the dye can be injected, and the heart chambers pressures can be measured, with these images the doctor can evaluate the blood flow through blood vessels, heart, and valves to check for abnormalities, computerized cardiac tomography (CT) scan, Magnetic Resonance Imaging - MRI, Digital Subtraction Angiography - DSA etc.
Blood pressure is the most common sign of heart disease [2], such as cardiac hypertrophy, aortic aneurysm etc., which is why there are many non-invasive blood pressure measurement device’s researches for improvement in the health care system. Blood pressure is commonly described as including the pressure in the systolic and diastolic heart circle; it is divided into hypertension, normal or hypotension. The value of blood pressure directly shows the heart function and sometimes indirectly reveals cardiovascular disease [3].
The abnormal heart function relates to the brain, kidney, and heart damage via the stiffness arteries. The stiffness limits the transmission of pulsatility pressure to important organs such as the brain and kidney (Fig. 1A). The stiff small arteries lose their elasticity for the pulsatility ejection, which leads to damage to the target organs (Fig. 1B).
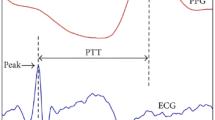
The abnormal heart function (heart damage) affects arterial stiffness, which can be detected from aorta pulse wave velocity (PWV) [4].
To measure the pulse wave velocity (PWV) for assess the stiffness, the methods include the invasive estimate direct from pressure catheters or non-invasive such as magnetic resonance imaging (MRI), tonometer ultrasound, or indirect from a single cuff recording (Fig. 2).
The aorta pulse wave velocity can be indirect measuring from single cuff pressure [5].
With the development of technologies in the Internet of Things (IoT), sensors and science for big data, many blood pressure machines recently can collect the patient’s blood pressure and then directly send it to iCloud. The data will be summarized for individuals followed on a smartphone by patients and family doctors for designing the optimised treatment, and a machine learning system will analyze this information for early detection of abnormal signs of the heart [6,7,8].
Nevertheless, the most recent non-invasive blood pressure measurement devices only show systolic and diastolic pressure. Some devices can alert the abnormal heart rhythm, while the oscillation and variability of blood pressure are more important for early cardiovascular function disorder prediction [9].
Oscillometry is recently the methodology for automatic cuff blood pressure devices and is being researched to extend to wearable devices such as smartwatches (Fig. 3).
The oscillation of blood pressure was the principal measurement of most automatic cuff devices, (a) Intravascular blood pressure and cuff pressure. (b) Normalized arterial area change [10].
The oscillometric algorithms for estimating blood pressure have previously been examined via mathematical modeling; specifically, sensitivity analyses were applied to computational oscillometric models to determine the factors that affect the accuracy of the maximum amplitude algorithm [11, 12].
The oscillation of blood pressure was the principal measurement of most automatic cuff devices, so the important purpose of this study was to show how the cuff pressure waveforms could detect the abnormality of heart function (which could not be captured from commercial devices) via developed a non-invasive blood pressure measurement device combine with IoT system.
2 Method
First, we designed a blood pressure machine (which can pick up the pressure waveform or the oscillometry from the cuff) based on a sensor and IoT system to collect health data which were recorded on our server via a sim card.
We improved the deflated valve system to clearly capture the waveform in the stable pressure while measuring (data not shown). Then, we self-made this device, including the mechanical system for pressure measurement, mainboard, data logger, wifi module, Radio Frequency Identification (RFID) module and other details were printed by a 3D machine (Figs. 4, 5, 6). The 2SMPP-O2 MEMS Gauge Pressure Sensor from OMRON Corporation - Electronic and Mechanical Components Company were used for pressure detection with a pressure range of 0 to 37 kPa (around 270 mmHg).
The firmware was coded (data not shown), and then the device was tested by the Vietnamese standard guideline (ĐLVN 343: 2020) and directly real-time compared with the mercury sphygmomanometer when measuring.
Next, we built a server with a web interface for real-time receiving and recording of the user’s medical information, which was transferred via a sim card so that the users could set-following their conditions or share it with their family or family doctor from anywhere at any time.
Using the collected data, the system can calculate the heart function via the Windkessel formula COest = (SBP-DBP)xHRx0.002 [13, 14], then analyse and classify detected patterns that cause risks of cardiovascular diseases, especially risks of stroke and heart attack.
From the predicted results, our project also provides utility services on the mobile application for users, such as suggesting treatment and alerting the users’ doctors and relatives in case of emergency.
3 Results
We successfully designed, produced and implemented 30 prototypes in Vietnam from June 2022, recently for testing their stability, accuracy, and usefulness.
The oscillometry was recorded and sent directly to the server via a 3G sim card (you do not need to connect with a smartphone as other devices).
This information on blood pressure, pulse rate, and cardiac output also was plotted as a comparison chart for tracking between measurements; this information was used for calculating the systolic and diastolic pressure, the inter-pulse interval and cardiac output (CO) on our device (Fig. 7). Then, this system notices the results to users with some personal recommends after compared with their medical records.
The user’s information was shown via the web interface and notification about the user’s family conditions or the patient for medical doctor user (Fig. 8).
4 Discussion and Conclusion
Stroke and heart attack are popular and dangerous cardiovascular diseases. Abnormal blood pressure is considered a sign of heart function disorder; hypotension (low blood pressure) is related to heart failure, and hypertension (high blood pressure) is related to stroke and heart attack. Thus, early detection of abnormal blood pressure is the most important solution to prevent target organ disorders due to abnormal heart function.
In addition, the variability of blood pressure and pulse could early predict the abnormality of heart function with big data of the user. The doctor can get information on how your blood pressure changes throughout the variability graph and then design a suitable treatment plan.
Together with the development of sensor technology and data science, our research aims to propose an IoT platform for cardiovascular diseases, including hardware devices and solutions for collecting data, reliably transferring data via a sim card, building mobile applications and predicting heart disease of users by mining big data. Finally, security and privacy issues are also a concern in this solution.
Cuff pressure waveforms of blood pressure machines based on medical knowledge, platform IoT and data science can be used to detect early heart disease abnormality. Furthermore, this IoT system also can be used to follow up on the result of treatment; this protocol can affect the medical treatment with an efficient clinical study.
When there are emergency signs and risks, the system monitors and sends alerts to the users assigned. In addition, data accessed by other users are controlled by privacy-preserving access policies. Medical specialists can also use the research data and results to research symptoms of early detection of cardiovascular diseases.
This system is useful for personal users and can be customised to apply for hospitals, clinics or other homecare systems.
References
Dias, D., Cunha, J.P.S.: Wearable health devices—vital sign monitoring, systems and technologies. Sensors 18(8), 2414 (2018)
Kaplan, N.M., Opie, L.H.: Controversies in hypertension. Lancet 367(9505), 168–176 (2006). https://doi.org/10.1016/s0140-6736(06)67965-8
Ma, Y., et al.: Relation between blood pressure and pulse wave velocity for human arteries. Proc. Nat. Acad. Sci. 115(44), 11144–11149 (2018)
Laurent, S., Boutouyrie, P.: Arterial stiffness and hypertension in the elderly. Front. Cardiovas. Med. 7, 544302 (2020)
Segers, P., Rietzschel, E.R., Chirinos, J.A.: How to measure arterial stiffness in humans. Arterioscler. Thromb. Vasc. Biol. 40(5), 1034–1043 (2020)
Islam, S.R., Kwak, D., Kabir, M.H., Hossain, M., Kwak, K.S.: The internet of things for health care: a comprehensive survey. IEEE Access 3, 678–708 (2015)
Zheng, Y.L., Yan, B.P., Zhang, Y.T., Poon, C.C.: An armband wearable device for overnight and cuff-less blood pressure measurement. IEEE Trans. Biomed. Eng. 61(7), 2179–2186 (2014)
Weinberg, I., Gona, P., O’Donnell, C.J., Jaff, M.R., Murabito, J.M.: The systolic blood pressure difference between arms and cardiovascular disease in the Framingham heart study. Am. J. Med. 127(3), 209–215 (2014)
Alpert, B.S., Quinn, D., Gallick, D.: Oscillometric blood pressure: a review for clinicians. J. Am. Soc. Hypert. 8, 930–938 (2014). https://doi.org/10.1016/j.jash.2014.08.014
Ma, Y., Chen, Y., Ma, Y., Feng, X.: The effect of arterial stiffness on cuff-based blood pressure measurement. Extreme Mech. Lett. 48, 101298 (2021)
Berger, A.: Oscillatory blood pressure monitoring devices. BMJ. 20, 323(7318), 919 (2001). PMCID: PMC1121444
Chandrasekhar, A., et al.: Formulas to explain popular oscillometric blood pressure estimation algorithms. Front. Physiol. 21(10), 1415 (2019). https://doi.org/10.3389/fphys.2019.01415.PMID:31824333;PMCID:PMC6881246
Sun, J.X., Reisner, A.T., Saeed, M., Mark, R.G.: Estimating cardiac output from arterial blood pressurewaveforms: a critical evaluation using the MIMIC II database. In: Computers in Cardiology, pp. 295–298. IEEE (2005)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
Conflicts of Interest
The authors have no conflict of interest to declare
Rights and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Thang, B.Q., Duy, P.D.T., Thien, V.T. (2024). Early Detecting the Abnormality of Heart Function via drtabc.com System (Made by Viet Nam). In: Vo, V.T., Nguyen, TH., Vong, B.L., Le, N.B., Nguyen, T.Q. (eds) 9th International Conference on the Development of Biomedical Engineering in Vietnam. BME 2022. IFMBE Proceedings, vol 95. Springer, Cham. https://doi.org/10.1007/978-3-031-44630-6_85
Download citation
DOI: https://doi.org/10.1007/978-3-031-44630-6_85
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-44629-0
Online ISBN: 978-3-031-44630-6
eBook Packages: EngineeringEngineering (R0)