Abstract
High blood pressure (BP) or hypertension is the single most crucial adjustable risk factor for cardiovascular diseases (CVDs) and monitoring the arterial blood pressure (ABP) is an efficient way to detect and control the prevalence of the cardiovascular health of patients. Therefore, monitoring the regulation of BP during patients’ daily life plays a critical role in the ambulatory setting and the latest mobile health technology. In recent years, many studies have been conducted to explore the feasibility and performance of such techniques in the health care system. The ultimate aim of these studies is to find and develop an alternative to conventional BP monitoring by using cuff-less, easy-to-use, fast, and cost-effective devices for controlling and lowering the physical harm of CVDs to the human body. However, most of the current studies are at the prototype phase and face a range of issues and challenges to meet clinical standards. This review focuses on the description and analysis of the latest continuous and cuff-less methods along with their key challenges and barriers. Particularly, most advanced and standard technologies including pulse transit time (PTT), ultrasound, pulse arrival time (PAT), and machine learning are investigated. The accuracy, portability, and comfort of use of these technologies, and the ability to integrate to the wearable healthcare system are discussed. Finally, the future directions for further study are suggested.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Blood pressure (BP) is the pressure of the blood within the arteries as it circulates through the body. BP is generally expressed in terms of systolic pressure and diastolic pressure. Prehypertension ranging starts from 120 to 139 mmHg systolic blood pressure (SBP) and 80 to 89 mmHg diastolic blood pressure (DBP) [1, 2]. Hypertension is the single most important modifiable risk factor for cardiovascular diseases (CVD), and monitoring arterial blood pressure (ABP) is an efficient way to detect CVD [3]. CVD is associated with the world’s highest mortality and disability rate, also called a “silent killer” because it rarely shows early symptoms before significant damage is made to the heart, arteries, brain, eyes, and kidneys [4]. The world health organization (WHO) global status report has shown that 7.5 million deaths annually are caused by diseases related to high BP and this number is likely to increase in coming years as the population ages [5, 6]. In spite of these facts, it has been shown that only 33% of hypertensive patients are aware of their disease and had their BP under control by receiving related treatments [7].
Considering the fact that hypertension is preventable and its effective management is a key component of any healthcare strategy in the ambulatory setting, a reliable continuous BP monitoring system would increase the rate of awareness, treatment, and control of hypertension. By collecting activities of daily life (ADL) and BP variations in individuals at risk of CVD, there is a possibility to improve the assessment of the patient’s hypertension state. As a result, risk factors can be minimised and clinicians can encourage patients to adopt lifestyle modifications and early medical intervention [8]. The recent studies have been conducted that the non-invasive and continuous BP monitoring could give this opportunity to the clinicians to measure patients’ BP variation during their daily activity and predict BP related risks [9, 10]. Therefore, continuous BP monitoring is vital to improve diagnosis in health care and better prediction in the related treatments plan [11,12,13]. Furthermore, early detection and treatment of hypertension can reduce the associated economic and social costs [14].
For the first time in history, William Harvey described arterial pulse and circulation physiology in the sixteenth century [15]. He also introduced hemodynamic parameters such as cardiac output, stroke volume, and ejection fraction [15,16,17]. In 1733, Reverend Stephen Hales noted that the presence of BP and pulse pressure could be used to observe the pulsatile rise and fall of an animal’s BP [18]. In the same century, John Floyer measured pulse rate. The Kymograph (“wave writer” in Greek) was developed by Carl Ludwig in 1847 to graphically record arterial pressure; this involved inserting a brass pipe cannula into the artery and the use of a mercury manometer. Vierordt in 1855 used the sphygmograph to develop a non-invasive BP technique. In 1985, Scipione Riva-Rocci developed the inflatable cuff armband [19]. The common traditional auscultatory method was first introduced by a Russian surgeon named Korotkoff in 1905; this method involves an inflatable BP cuff and stethoscope and it has become the clinical standard over the last centuries [19].
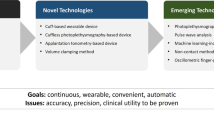
Traditional BP measurement methods, based on auscultatory and oscillometric techniques, considered the standard method for over 100 years. The significant drawback of this technique is the inclusion of cuff-based technology for measurement. The repeated inflation and deflation of the cuff cause discomfort for the patients, especially during night time monitoring, which means that these methods are not practical for long-term and continuous BP monitoring [20]. To overcome the shortcomings of auscultatory and oscillometric techniques, significant research has been conducted using a cuff-less BP device that is incorporated into daily objects (weighing scales, chairs, rings, watches, cameras, shirts, and mobiles) [21,22,23,24,25,26,27]. Recent research focuses on continuous and cuff-less BP monitoring techniques based on pulse transit time (PTT), pulse arrival time (PAT), and ultrasound. Among these advanced techniques, the PTT-based approach shows better results and higher accuracy rates.
BP is influenced by many factors such as various abnormalities in cardiac output, blood vessel wall elasticity, circulation blood volume, peripheral resistance, respiration, and emotional behaviour [28]. Importantly, the complex and dynamic nature of the cardiovascular system necessitates that any BP monitoring system should benefit an intelligent technology that can select and analyse compelling BP features. Therefore, this idea has motivated researchers to investigate the use of latest machine learning technology to extract the best features required for BP monitoring and modelling the cardiovascular system accordingly to meet the advancement of medical instrumentation (AAMI) [29] or the British Hypertension Society (BHS) standard [30].
This paper aims to provide a comprehensive review of the most common BP measurement techniques as well as challenges and opportunities for future study. An extensive search was conducted on the most reliable scientific databases including Google Scholar, PubMed, IEEE Xplore, Scopus, and ScienceDirect. The keywords used in the search were “blood pressure monitoring”, “continuous non-invasive measurements”, “pulse transit time (PPT)”, “photoplethysmogram (PPG)”, “pulse arrival time (PAT)”, “cuff-less monitoring”, and “ubiquitous measurement”. The inclusion criteria for this search were:
-
1.
Peer-reviewed articles published as a journal article or in conference proceedings
-
2.
Publication or reporting year 2015 (inclusive) to 2019
-
3.
Continuous BP monitoring was the primary subject of this study
-
4.
Targeted article focusing on cuff-less BP monitoring with advanced techniques
-
5.
Written and published in English
In the following sections, first, classical non-invasive, non-continuous BP measurement methods are briefly presented as background information. This is followed by a discussion of the current continuous BP monitoring techniques along with their strengths and limitations, and finally, the conclusion and direction for future research are presented.
Background on existing classical non-invasive and non-continuous BP measurement techniques
The auscultatory method involves standard clinical cuff-based BP monitoring. It measures SBP and DBP using a sphygmomanometer. This non-invasive method employs an inflatable cuff. A stethoscope is placed at the brachial artery and is used to listen to the Korotkoff’s sounds during cuff deflation. Then, SBP is estimated as the first sound detected and DBP is determined at the moment the Korotkoff sound disappears [31]. However, it cannot be used for continuous measurement of BP since there must be a time gap of three minutes between any two measurements [32, 33].
The oscillometric method is very similar to auscultation and is a popular automatic technique for measuring SBP, DBP and mean BP. This technique also involves an inflatable cuff with a built-in pressure sensor [34]. The pulsatile BP in the artery is measured during cuff inflation and deflation. This method even indicates tiny oscillations in cuff pressure [20] and is normally employed when Korotkoff sounds are difficult to hear [19]. However, the main disadvantage of this method is the sensitivity to motion artifacts [34]. Moreover, Fibrillation, obesity, respiration, and atherosclerosis can also affect the accuracy of this type of BP measurement method [35, 36].
Volume clamping as another non-invasive and automatic method was first introduced by Penaz in 1973 [21]. This method employs a small finger cuff containing a PPG to absorb infrared light and estimate blood volume [19]. Using this methodology, the Finapres medical device was developed in 1986 [37]. However, this technique is cuff-based, bulky and the finger cuff can be uncomfortable for the patient.
Tonometry is another non-invasive beat-to-beat BP measurement technique in which a monometer-tipped probe is placed over a superficial artery against the skin to indicate the maximum pulse pressure constantly. This technique needs a cuff-based calibration to achieve the desired accuracy [38]. One of the significant drawbacks of this technique is the difficulty in manually or atomically positioning the probe on the artery.
In sum, none of the classic BP measuring methods is suitable for ambulatory, continuous, and cuff-less BP monitoring due to lack of accuracy during constant and long-term monitoring. Besides, these techniques are inconvenient for children and the elderly, and cannot be used in remote healthcare systems. A comparison of the existing BP measurement techniques in terms of advantages and limitations is summarized in Table 1.
Advanced continuous and non-invasive techniques for BP measurement
Given the increasing prevalence of non-communicable diseases (like heart attacks and stroke) and increasing the median age in the population [39], a growing interest exists for providing a continuous and ubiquitous BP monitoring method with cuff-free calibration that minimizes any discomfort for patients. Currently, the most clinically adopted continuous BP monitoring method is the intra-arterial catheter that can be used only in the intensive care unit (ICU). Even though this method is considered the gold standard for BP measurement, it is invasive [40]. It is typically performed using a high-pressure plastic tube that connects to the peripheral artery of the patient with a catheter. The most common site for cannulation is the radial artery as this is associated with a low rate of complications. Although this technique has high accuracy and high precision, this intra-arterial method is associated with bleeding, infection risk, and nerve damage [41, 42].
PTT-based modelling approaches
The PTT is defined as the required time for the pulse pressure wave (PWV) to propagate between two arterial points within the cardiovascular system. The mathematical relation between PWV and the elasticity of the arterial vessel is described by the Moens-Korteweg (M–K) Eq. (1) below:
where E is the elasticity of the artery, h is wall thickness of arterial, ρ is the blood density, and D is the artery diameter [43]. The PTT is usually measured as the time difference between the R wave of an electrocardiogram (ECG) and the specific points of the PPG (Fig. 1) [44]. PPG is a non-invasive, continuous, low-cost, and well-developed technique for measuring the distal signal. However, a PTT measurement only from the ECG and PPG signals may not be an accurate method for BP estimation since BP is related to a complex set of parameters such as tissue compliance, muscle tone, peripheral resistance, and ventricular contraction [44].
A new indicator, the photoplethysmogram intensity ratio (PIR) has been presented by Xiao et al. [45, 46]. The PIR was defined as the ratio of PPG peak intensity to valley intensity which contributes to the change in arterial diameter and is capable of tracing low frequency (LF) variations in BP. The ratio of the PPG peak intensity to the PPG valley intensity of one cardiac cycle was determined by the PIR [46] The author combined both PIR and PTT methods to develop a new BP measurement algorithm. PTT is advanced to track the BP in the high frequency (HF) range and PIR in the LF range. To validate the results, a total of 27 subjects were selected for this experiment. The results of BP measurement using the proposed technique compared with Finapres measurements as a reference method to confirm the influence of vasomotor tone on LF components and accurate results [47]. However, the results needed to be validated with a gold standard that involved adequately powered studies with a sufficient number of patients with CVD and who are monitored over the long term.
Following the PIR study [46], a new feature related to BP named the intensity ratio of the first derivative wave of the PPG (1th dPIR) has been proposed by Wan-Hua et al. [48]. Where 1th dPIR was calculated by differentiating the original PPG wave and likely to remove the low frequency and bassline noise to improve the accuracy. Twenty-two healthy volunteers participated in mental arithmetic stress and Valsalva’s manoeuver tests. The Finapres device was used as a reference, and the result showed standard deviation errors of 3.22 ± 8.02 mmHg and 3.13 ± 4.82 mmHg for SBP and DBP estimation respectively. The proposed method is linear and makes the character points of the waveform more visible so it could improve the accuracy of BP estimation. Regarding the sample size of the subjects, this study didn’t meet the requirement of standards.
Jing Liu et al. [49, 50] used a four-channel PPG signal system to collect the PPG waveform of the different blood vessels to estimate PTT. A simple infrared (IR) at only one body location was used to measure the time interval between the PPG signals at different skin depths as a PTT. Six signals including ECG, continuous BP measured by Finapres, Blue PPG, green PPG, yellow PPG, and IR PPG signals were collected and analysed through an algorithm. Eventually, the peak amplitude of continuous BP was identified as a SBP measurement. This technique eases the integration of the system and the architecture which makes it also suitable for wearable cuff-less BP monitoring. Although MW-PPG produced better results compared to previous methods, the size of PPG sensor need to be miniaturized, and the effect of motion artifacts should be considered for BP estimation.
A combination of contactless image-based PTT (iPTT) and image-based PPG (iPPG) using a high-speed camera has been introduced by Cheol et al. [51, 52]. The interval time between the arrivals of the pulse wave at two body locations is measured with iPPG using an analysis of sequential images. The images were obtained using a high-speed video camera with the subject in the seated position. The potential feasibility result of this research was validated in a small preliminary ‘in vivo’ assessment with seven healthy volunteers. The iPPT data was calculated as the time interval between the derivative of the face blood volume pulse wave (FdBV) and a derivate of the right-hand palm blood volume pulse wave (HdBV). The iPTT and SBP had a high correlation in each subject compared to the high-precision clinical automated oscillometric method results. However, individualized calibration is needed for this method as iPPT versus the SBP slope will be different in each subject depending on the light reflection, skin penetration, and the pulse wave propagation.
In [53] the author employed a linear regression algorithm to estimate the PTT. The correlation between the ECG and the PPG in five different positions (recumbent, seated, standing, walking, and cycling) in 14 healthy subjects have been estimated. The main concern of this research was considering the effect of patient’s activities on PTT-based estimation. For this purpose, a wearable biomedical device was used to capture and record three channels of ECG and one channel of PPG by the local pod. A customized Matlab algorithm was designed to compute the PTT automatically from the PPG and the ECG signals. The results were compared to the reference standard and the root-mean-squared-error was within 1% of the standard measurement. However, this technique has shown accurate result the seated or standing positions, but not during other positions. Moreover, this approach needs a cuff-based method for calibration.
An affordable, simple, and portable BP estimation method has been proposed by Aishwarya et al. [54] to monitor the SBP and DBP. This technique required a smartphone camera to capture only the PPG signal by placing a finger over the camera lens of an iPhone 4. A total of 17 features, including the time domain features of the PPG signals and the height, weight, and age of each subject were used to train the system. To detect and remove the noise of the PPG signal, a finite state machine (FSM) was applied as a pre-processing system. Two different training model was used for estimation and the result of both models has been compared. The results showed that the support vector machine (SVM) model had a better performance in comparison with the linear regression model. In addition, to evaluate the proposed method, the University Queensland Vital Sign dataset and outcomes from 17 healthy subjects have been used in the experiments. Although the results approved the ability to use this technique in BP estimation, this study involved only an iOS, and so an Android device capability should be considered in future work. Moreover, the feature selection method needs to be improved in order to capture more parameters related to BP.
A PTT-based technique using wearable BP device controlled by a smartphone has used to estimate the BP continously [55]. Both ECG and PPG signals were captured via the PPG and ECG sensors. A peak detection algorithm from previous studies was employed to extract the BP features from the PPG signal. Eventually, Matlab software was used for testing, calibrating and estimating the BP. An Android application was developed to allow users to monitor their ECG, PPG, SBP, DBP and heart rate indexes.
Moreover, a new PPG sensor with four LEDs which can detect different blood vessels and different blood volume has been introduced. The result showed that the new sensor provided a 30% current saving compared to a one LED case. The adaptive threshold algorithm was used to test ten recordings from the MIT-BIH database. The results showed a reduction in both power consumption and motion artifacts (MA) disturbance.
Aliar et al. [56] also used a smartphone camera and microphone to measure PTT and then estimate the BP. PTT was calculated as the time difference between blood leaves the heart and the time it reaches to the finger. For measuring these two values the heart sound recorded using a smartphone’s microphone and its camera as a PPG sensor to measure the pulse wave respectively. To achieve a reliable heart rate, a combination of autocorrelation and a Fast Fourier Transform (FFT)-based algorithm was used to detect the exact moment the pressure pulse reached the distal point. The proposed method involved processing the PPG and PCG signals to estimate the PTT using inexpensive sensors. Although the results were within the acceptable range and could detect the beat-t-beat variations of PTT, the sample size was relatively small, and the results need to be validated with the gold standard and during motion. Moreover, positioning the smartphone correctly is very difficult for users.
A dual-modality arterial pulse monitoring system was proposed to overcome the limitation of the PTT-based technique.[57]. In this method, a pressure–volume cure was created by recording the pressure wave and PPG signals related to the radial artery. Then the elasticity index (EI), and viscosity index (VI) was extracted to calculate the PTT. The pressure wave and PPG signals were collected from seven healthy subjects, and at the same time, ECG and BP signals were monitored by Finapres device as a reference. The average correlation of EI, VI, and PTT was compared, and the results showed that both EI and VI have a high correlation with SBP and DBP compared to PTT. Even the combination of EI and VI had a significantly higher correlation coefficient than PTT. However, this method could not track the BP in low-frequency due to the vasomotor tone.
A novel method to estimate the PTT using a seismocardiogram (SCG) was proposed by Chenxi Yang and Negar Tavassolian [58]. A three-axis MEMS accelerometer was strapped to the chest wall of a subject to record the SCG signal. A customized microphone sensor and pre-amplifying circuit were placed inside the ear to record the distal arterial location data [58]. At the same time, a cuff-based BP monitor recorded DBP and SBP every 30–40 s as a reference. All high-frequency SCG signals were removed by an infinite impulse response (IIR) filter. Likewise, all the PPG signals underwent a finite impulse response (FIR) filtering. All the synchronized data were then fed to the Matlab so that PTT could be calculated. Although a high correlation coefficient was obtained in this study, the age and a small number of subjects (ten only), limited the generalisability of these results to daily life.
As PTT mostly calculated from ECG and PPG signal and very related to pulse wave (PW) shape, an algorithm was proposed to remove the effect of artifacts and movement of subject on PW signal [59]. A “Seven Step PW-Filter” algorithm was proposed to remove the inappropriate PW characteristics which not related to PTT calculation to improve the accuracy of the measurement. Compared to previous studies on manual/visual filtering, the proposed algorithm achieved 99.3% accuracy in detecting any unwanted PW. Moreover, elimination using the seven-step PW-Filter was much faster compared with manual elimination. Further experiments need to be considered including CVD subjects in a different position.
Bassem et al. [60] used a combination of synchronized ECG, PPG, and bio-potential based impedance (Bio-Z) to estimate the PTT. All the signals were filtered by a low pass filter in order to remove high frequency and noise. After filtering, the ECG, Bio-Z and PPG signals are analyzed to determine the points of R peaks in ECG, the points of maximum negative slope of the Bio-Z and maximum positive slope of the PPG in order to calculate the corresponding PTT values. To evaluate the results of this method, the outcomes were compared with PPT measured from only ECG and PPG signals. The result of experiments done in vivo gave a correlation coefficient of 0.92 which correlates closely with previous measurements. These outcomes suggest that this method could be used as an alternative to establishing a PTT measurement technique for ambulatory and cuff-less monitoring. However, a reliable calibration for long-time monitoring needs to be investigated.
A watch-based system (SeismoWatch) to estimate the PTT using SCG and PPG signals were presented by Andrew et al. [61]. A prototype watch included an accelerometer to measure the SCG, and photodiodes and LEDs were designed to measure PTT and estimate the BP without the need for a cuff. The watch is pressed against the sternum to measure the micro-vibrations of the chest wall associated with the heartbeat. The time that a pulse wave travels from the heart to wrist calculated with an accelerometer and optical sensor mounted on watch as PTT. This is the first time that this technique was used in an at-home setting rather than a clinic environment and supine position. To validate this study, three different sections were considered for 13 healthy subjects who participated in the experiment; one minute of rest, one minute of exercise, and five minutes of recovery. The results were indicated that the accuracy of this watch-based method improved significantly compared to a conventional BP monitoring method. However, this technique needs cuff-based calibration, and only young and healthy subjects were selected for validation. Moreover, PTT was calculated through the brachial arteries rather than the larger arteries.
Less computation makes any technique more suitable for use as a wearable BP monitoring device. Hence, a single PPG signal feature has been proposed by Yang et al. [62] The mean slope transit time (MSTT) as a new and only feature with more stability compared to the slope transit time (STT) was introduced in this study. Ten subjects with no CVD history participated to validate the method. All subjects were in the supine position, and all signals were recorded for five minutes. The results showed the mean error of − 0.90 ± 3.84 mmHg and − 0.31 ± 3.36 mmHg for the SBP and DBP estimation respectively, which determined a better performance compared to the conventional PTT method. An obvious limitation of this study is that only healthy and young people participated in the experiment.
In order to estimate PTT and PATat the central of arteries, an electrical bio-impedance (BImp) ECG across the shoulder, and continuous wave radar antennas on the sternum were used by Buxi et al. [63]. The Pan-Tompkins algorithm was employed to detect the ECG R-peak and a tangent hyperbole function was used to calculate the arrival of the BImp pulse wave, and finally, the radar signal was used to estimate the PTT. The result was validated with six healthy male subjects during exercise. The proposed architecture can be utilized while completely hidden under patients’ clothes, making it suitable for ambulatory BP, sleeping time and during exercise. However, this method only has the potential to estimate SBP a method for positioning the antenna in terms of the electrical axis, size, and female anatomy need to be studied.
According to the clinical demand for cuff-less ambulatory BP monitoring, Josep Sola et al. [64] introduced a method to estimate mean arterial pressure (MAP) using the chest-BP sensor. The proposed method required two measurements. First, impedance cardiography (ICG) technology was used to estimate the opening time of the aortic valve, and then a multichannel PPG was employed to measure the arrival time at the sternum. Finally, PTT determined the time difference between the PAT and a pre-ejection period (PEP). The results were validated with 15 healthy subjects, and overall baseline MAP values were 80 ± 6 mmHg, and maximum MAP values of 107 ± 9 mmHg during handgrip maneuvers. Also, the method was tested with six different calibration strategies for each subject. It has been proven that this method can provide continuous BP monitoring in a clinical environment. However, the subjects involved were all healthy, and only the single stress maneuver was considered. Also, the results were compared with a single brachial oscillometric device and not with the gold standard.
In [65] a system to integrate both electrocardiography and BP measurement by adopting transit pulse time was proposed. The PTT was defined as the systematic time lay off between oscillometric pulses and R-peaks of ECG waveform. The major advantage of the system is to exhibit non-zero crossing and gives a more accurate result. They evaluated their method only for thirty seconds and didn’t mention the number of subjects involved in the experiments. Although the proposed method increased the accuracy of BP measurement, further evaluation needs to be done in a long period.
In conclusion, this section on PTT-based techniques indicates that most techniques employed the ECG for proximal timing reference and PPG to measure the distal waveform. Additionally, some studies use the ICG, BCG, and SCG to determine the PTT through cardiac mechanical vibration information. Interestingly, the PTT/PWV based technique revealed the high potential for cuff-less BP measurement and PTT consider as one of the most related features to BP variation. Nevertheless, we have found that the low accuracy rate of long-term monitoring and lack of acceptable validation are the main bottlenecks of most PTT-based techniques. It is difficult to compare the results of all previously discussed methods as they are using different evaluation techniques. However, a comparative analysis of PPT-based techniques in terms of the number of extracted features, experimental tools, sample size, and type of calibration is presented in Table 2.
Ultrasound-based methods
The ultrasound can track the diameter waveforms and vessel wall thickness accurately [66]. Any artery which is visible for ultrasound can be monitored with this technique. Most ultrasound-based techniques do not require cuffs for measurements. Furthermore, this user-friendly method can indirectly measure pulse wave velocity (PWV) and estimate BP for long-time monitoring. Some of the ultrasound-based studies are discussed below.
A new non-invasive continuous BP monitoring has been presented by Weber et al. [67] using ultrasound to detect the blood velocity in the wrist vessel. A polyurethane balloon was placed over the wrist radial artery to measure the blood velocity. The BP was controlled by an ultrasound sensor and voice coil actuator placed on the lower arm. A microcontroller Arduino DUE R3 board including an iterative learning controller (ILC) and a proportional-integral-derivative controller was implemented to control the balloon pressure and adjust the collected ultrasound signals. This method can provide BP monitoring for over 24 h and does not require a cuff. However, the balloon attached to the wrist is compulsory and the patient's position change will affect the measurements. Moreover, further analysis of the controller is required and reducing the size of the voice coil actuator power amplifier should be considered.
Joohyun et al. [68] estimated ABP by employing a two-channel ultrasound system. PWV was calculated based on a combination of arterial vessel cross-sectional area and elasticity of the vessel. A flow phantom including a diaphragm pump, a soft latex rubber, and a reservoir was designed for the experimented setup. The pre-processing of signals was done by a bandpass filter to remove all the RF signal noise on both channels. The feasibility of ABP waveform calculation was shown in this research and the effect of PWV reflection on ABP was discussed. The measured PWV, using 16 cardiac cycles of data was 8.47 ± 0.63 m/s with an associated scaling error of − 1.56 ± 14.0% in a direct pressure waveform comparison, showing minimum error on average. To meet the standard accuracy, the feasibility of this technique in vivo needs to be further validated.
A calibration-free technique using a dual magnetic plethysmograph (MPG) transducer and a single-element ultrasound transducer has been presented by Jayaraj et al. [69]. The measurement of arterial dimensions along with local PWV was needed for calibration-free evaluation. Therefore, an arterial compliance probe from the carotid artery was designed and validated for pulse pressure measurement on superficial arteries. The results of this study validated with ten volunteers highlights the value in tracking local PWV changes and carotid pulse pressure. Although, the measured local PWV obtained a large correlation with brachial BP, the absolute value of local PWV and calculated carotid pulse pressure correlated at lower than the previously reported value.
Aaron et al. [70] placed an ultrasound probe with force measuring capability, on the carotid artery and then the contact force between the probe and the patient skin was slowly increased. Meanwhile, the ultrasound images and contact forced data video were recorded. An optimization Matlab algorithm was used to calculate the BP from the video segmentation done by a Star-Kalman filter. Each time the pressure was reported, an algorithm calculated the patient-specific artery stiffness making it suitable for the patients with atherosclerosis. Moreover, the pressure measurement can apply to any artery and does not require medical supervision. Nevertheless, obtaining BP through this method takes a long time, and the result did not validate with any clinically approved technique.
In sum, the ultrasound approach does not need the inflatable cuff, so it does not affect patient comfort. Nevertheless, the ultrasound device is large and needs calibration to estimate absolute BP value. In addition, this method depends on reliable detection of the foot of the diameter waveforms and an appropriately high sampling frequency.
PAT-based methods
The PAT is defined as the sum of PTT and the time taken for the opening of the aortic valve which is known as the PEP. In this method, an ECG represents the proximal arterial waveform and a PPG at the finger a surrogate of the distal waveform, in which case PTT is known as PAT. A great number of studies focus on PAT-based techniques and some of them achieved accurate results compared with actual BP. This section reviews some of the highlighted studies carried out using the PAT-based method.
Braiam et al. [72] calculated the PAT as difference time between R-peak of ECG and two points of PPG waveform, first is the maximum amplitude of PPG and second is the sharpest slope of the rising edge of PPG. After initial filtering, eight subjects from the MIMIC database were selected for the experiment. A linear regression model was used to show the relationship between the PAT and the systolic, diastolic and mean BP. While the results showed a strong correlation between BP and PAT, but the sample size was not large enough to meet the clinical standards.
A chair-based method using PAT-based technique has been presented by Zunyi et al. [73]. This system consists of an ECG with four electrodes, a PPG sensor with green lighting LED and a photodetector. Additionally, a control circuit with a Bluetooth module and a high capacity battery was mounted on a common armchair. The ECG and PPG signals were collected from users while they are in sitting position. All the collected data transfer to a PC to calculate the beat-to-beat PAT. A cuff-based method was considered as a reference and the results were validated on 12 subjects with no CVD histories. In spite of the acceptable results of this method, elderly subjects and hypertensive people need to be involved in further validation and a cuff-less calibration method needs to be considered.
The motion artifacts and daily activities reduce the accuracy of the PAT-based technique. Qiang et al. [74] used a Kalman filter to improve signal quality and overcome this issue. The MIMIC II database was used to evaluate the method and the twenty signals including the ECG, ABP, and PPG were selected. An FIR band-pass filter was employed to filter all signals during the process and the Pan-Tompkins algorithm was considered to select the R-peak of ECG. The PAT was then calculated as the time difference between the R wave and the synchronized PPG signal. The least-square algorithm was used to calibrate the PAT to BP every 30 min. A joint signal quality index (JSQI) was used to adjust the Kalman filter and reduce the effect of noise and artifacts on the PPG and ECG signals. The simple computation of the proposed algorithm makes it very suitable for wearable devices. Nevertheless, the MIMIC II database has small BP variation, and different database needs to be used for validation of such a technique.
A study has been conducted by Yali et al. [75] to validate the accuracy of the PAT method on 24 subjects including 15 hypertensive patients. A PAT-based cuff-less armband wearable device including one PPG sensor and two pieces of e-textile ECG patch was used every 15–30 min to monitor the BP during daily activities. At the same time, an experienced nurse measured the BP with an oscillometric BP device attached to the upper arm of the subjects. The Bland–Altman plots were employed to estimate mean SBP and DBP during the day and night-time activities. The results showed that the PAT-based method could replace the traditional BP monitoring for night-time ABP monitoring via cuff-less and convenient monitoring methods. However, the accuracy of this method on day-time is not accurate as nigh-time.
Satu et al. [76] used an arm ECG and finger PPG to measure the PAT in four different methods. The PAT was estimated as the time interval between the ECG R peak and four different points in the PPG. Ten subjects in a seated position were involved for measurements and the signal processing was completed by using the Matlab program. The results of different measurement techniques were compared, and the first PPG signal derivative was considered as the most promising method. To enhance the accuracy and increase the reliability of the measurement, the signal quality in noisy environments needs to be further investigated and improved.
In summary, the PAT has a correlation with BP and it can be used as an indicator of big trends changes such as hypertensive or hypotensive episodes. However, the ability of PAT for continuous and non-invasive BP estimation is not confirmed due to the limited experimental setup.
Machine learning-based techniques
Considering the fact that BP is the result of multiple parameters and highly influenced by various factors, multiple features extraction BP monitoring methods could significantly improve the accuracy of BP monitoring. Moreover, there is a growing demand for automated BP monitoring to perform efficient daily regular home BP monitoring, aiming to improve remote healthcare. Automated BP monitoring produces a significant amount of digital data, which increases the rate of diagnosis and ideal treatments. However, the predictive analytics model of such big data is very challenging. Many recent studies have adopted machine learning as an effective method in managing big data and predict the risk factor of hypertension. By taking advantage of machine learning computational power and ability to develop the big data, the accuracy of machine learning-based BP monitoring has been improved. The main idea is to extract multiple features related to BP from time and frequency domains of physiological signals, then use machine learning to eliminate unwanted features and calculate the BP from extracted data. In this section, a variety of different machine learning techniques are reviewed.
Back-propagation neural network and radial basis function (RBF) network algorithms have been used by Tony et al. [77] to predict BP. The aim of this study was to monitor the SBP in young and middle-aged people and provide them with early warning of a heart disease problem. SBP, age, BMI, exercise level, smoking status, alcohol use level, stress level, and salt intake level were collected from 498 subjects as a variable in this study [77]. The results were more accurate for the RBF network, however, further study needs to carry out with a bigger database. Although the result obtained the average estimate error, the accuracy of this system was not compared to the gold standard.
Similarly, the features including age, height, weight, BMI, PTT, and BP were extracted via the ECG and PPG signals in 75 healthy subjects in the supine position. The regression forest technique was employed by Mototaka et al. [78] to train the regression forests network and predict continuous BP. A non-contact system consisting of a microwave sensor for heartbeat detection and collecting ECG signal, and a camera for facial PPG detection was used. Both devices recorded the signals at the same sampling frequency and synchronized. At the same time, the ECG and PPG of the subject were recorded by a cuff-based sensor as a reference. The results showed a high correlation coefficient of 0.7. The proposed method is very suitable for remote health monitoring if the future investigation has been done with a bigger database.
The random forest (RF) method has been used to measure the ambulatory blood pressure by Rui et al. [79]. The MIMIC-II database was used as training data. Total of 285 records with available ABP, ECG, and PPG signals was selected. A derivative algorithm was used to detect 18 features from the PPG signal. The extracted features were used to train the random forest model and obtain BP. Although this method is more accurate compared to the PTT-based technique, the low speed of RF technique cannot be neglected which might make some difficulty for real-time monitoring. Also, the experiment was carried for one and a half hours and the CVD subjects were excluded from the database.
Yue et al. [80] used the SVM model to predict BP. To demonstrate the pulse and pressure variation, training data was extracted from the University of Queensland Vital Signs Dataset. In order to train the network, nine features were extracted from the PPG signal. The SVM method showed better accuracy compared to the linear regression method and arterial neural network (ANN) method. The accuracy of this method needs to be improved to the clinical level. Also, the bigger sample data should be collected to get the optimal parameters and exclude the outliers.
Xiaoman et al. [81] were employed an FFT-based algorithm to extract the amplitude and phase features from PPG signals collected from a fingertip sensor. The back-propagation ANNwas used to estimate complex and continuous function. The extracted features were trained by ANN and a Levenberg–Marquardt algorithm. The data related to 69 patients from the MIMIC II database and 23 volunteers were used to validate the proposed method. The results were compared with both gold standard and a commercial cuff sphygmomanometer. Producing a more robust and clear PPG waveform has remained a challenge for this study.
Zhihong Xu et al. [82] also used multi-parameter fusion to improve the accuracy of BP measurement. Fifteen features related to BP were extracted from the ECG and synchronize PPG. Then a pre-processing algorithm was designed to de-noise the signals. A simple algorithm was also employed to extract the R-peak and other PPG features. The trained data was fed to a back-propagation neural network to estimate the beat-to-beat systolic and diastolic BP. then, an optional calibration technique was considered to increase the accuracy of the measurement. The results were validated with seven healthy volunteers for 15 min in the supine position. The Finometer device was used as a reference and the mean ± SD errors of the systolic and diastolic BP are – 0.41 ± 2.02 mmHg and 0.46 ± 2.21 mmHg respectively, which indicates high accuracy of the system [82]. However, a bigger sample size including older people and those with hypertension history was needed for further validation.
Fen Miao et al. [83] extracted 14 features related to BP from the ECG and PPG signals to improve the accuracy of BP measurement. The Genetic algorithm was used to select the most critical features for each subject. The multivariate linear regression (MLR) and the support vector regression (SVR) were used to construct the BP model. Pearson’s correlation coefficient (CC), the mean difference (MD), and the difference in the standard derivation (SD) were calculated for each subject in three static and dynamic and long-term performances. Finapres BP measurement was used as a reference to evaluate the accuracy of the proposed method in 73 subjects. A large correlation was gained between the estimated BP and the reference results for static and dynamic estimation. The long-term estimation showed 20% less correlation compared to the previous study. From one day to three days and then to six months, the estimation error was fairly stable for both SBP and DBP.
Kengo et al. [84] used only a PPG signal using a wrist watch-type PPG to estimate BP via the data-oriented method. Twenty features were extracted from PPG, an acceleration plethysmogram (APG) and a preliminary questionnaire to calculate the BP. The machine learning algorithm was used to train huge collected data. A unique cloud system was proposed to deal with BP and life-log data through HTTP which would solve the data capacity problem. To collect the daily data of patients, a smartphone application was created. The correlation coefficient between the experiment results with 25 subjects and the estimated result was 0.80. This method showed high accuracy, but it did not meet the clinical standard acceptance.
David et al. [86] measured aortic pulse wave velocity by combining ballistocardiography (BCG), a bathroom scale as impedance plethysmography (IPG), and height of the subject in the supine position. The training data set including the IPG and BCG signals were collected from 106 subjects to train the random forest algorithm. This group included 12 people with CVD history and 28 smokers. The accuracy and feasibility of the results were verified by comparing with previous techniques, but it still needs to be compared to the gold standard technique. BP monitoring over a long period of time, different populations and different conditions also need to be investigated.
Jun et al. [85] extracted 26 features including amplitude features, time domain features, age, and sex of subjects. All these features were fed to a backpropagation neural network algorithm after pre-processing to estimate SBP and DBP. In order to show the efficiency of the approach method, data relating to 10 subjects from the MIMIC II database were used to validate the result. The results showed a mean error of 5 mmHg and a standard deviation of ± 8 mmHg compared to the gold standard. However, sample size and measurement period time are not enough to meet the clinical standards.
Linear regression models were trained for assessing the linear range of the problem. The main idea of the multiple regression analysis is to find which instructively variables contribute to the variation of the response variable. The outcome of analysis will indicate if the final models are not applicable when the target and features parameters have a non-linear relationship. Moreover, the linear regression models are more efficient for implementation due to their simplicity, being easy to train, requiring less training samples, and being less prone to overfitting. To train the algorithm, the static and dynamic PPT features were used by Hsieh et al. [87]. The data related to five patients from the MIMIC database were used to evaluate the experiment, and the result shows better accuracy than the conventional one. To reduce the deficiencies effect of internal and external factors, the re-calibration process was proposed by authors for the future direction of this study.
Deep learning is a type of machine learning which capable of supervised and unsupervised learning from data that are unlabelled or unstructured. Deep learning has shown promising results in biomedical technologies such as risk assessment for hypertension [88, 89], and echocardiography images analysis [90, 91]. Also, there are a few studies that have used deep learning techniques to monitor BP continuously.
The Deep belief network (DBN)-deep neural network (DNN) was proposed by Lee et al. [92, 93] to learn the complicated nonlinear relationship between artificial feature vectors and the reference BP. The bootstrap technique was used to generate eight artificial features from original oscillometric waveforms. Consequently, a significant number of training samples from artificial features were used to estimate the SBP and DBP. A total of 85 healthy subjects in a seated position participated to validate this experiment. The proposed method with artificial features has shown very accurate results.
Su et al. [94] proposed a new deep recurrent neural network (RNN) consisting of multi-layered long short-term memory (LSTM) networks to address the accuracy issue over long-term BP monitoring. The authors have selected seven features from ECG and PPG signals to train the proposed system. The experimental results show that the deep RNN model achieves acceptable accuracy using static and multi-day continuous BP datasets.
Zhao et al. [95] also used LSTM networks to design a BP prediction model. The pulse wave signals related to 6 healthy goats were collected in different time series. All the raw data was filtered using FIR filter and divided by cardiac cycles for future extracting step. Based on the previous studies, ten of the most characters that related to BP was extracted to train the LSTM network. The network implanted in the tensorflow deep learning framework and the networks were run in Matlab. The results showed a low mean square error which is confirmed the feasibility of the proposed technique to estimate BP. However, more reliable evaluation technique needs to be used to meet the clinical standard.
In summary, BP is a complex parameter and it is highly influenced by physiological and neurological factors. Hence, concatenating multiple feature extraction methods could obtain more accurate and clinically accepted BP measurement methods. With the latest trends in increasing the BP indicators and requirements for analyzing the complex big data, recent studies have adopted machine learning as an effective method for BP monitoring. The main idea is to extract multiple features from the time or frequency domains of physiological signals, such as ECG and PPG, then use machine learning to eliminate unwanted features and calculate the BP from the trained data. These methods have attracted attention due to their computational power for a reconstructing the BP as an output. Overall, the machine learning-based obtained considerable prediction accuracy for the BP model [79]. Among the variety of machine learning algorithms, linear regression, neural network, support vector machine, random forest, and deep learning are the most common models that have been used to develop BP models. However, most of the methods are still at the prototype stage and a further improvement in data size and quality could improve the clinical validity of these methods. Table 3, presents the state-of-the-art machine learning methods for cuff-less and continuous BP measurements.
Discussion
Accurate measurement of BP is essential to evaluate BP-related risks, diagnose hypertension, monitor the treatment response, and guide the management of diseases. Therefore, the development of cuff-less and continuous BP methods could provide a novel way to overcome various medical problems. The assessment criteria for evaluating the accuracy of BP measurement is thus should be well established before it is recommended for clinical use.
Among all existing studies, PTT-based techniques are the most common models being used for cuff-less BP monitoring. However, this study has indicated that there are still issues and challenges need to be addressed for the pervasive and ubiquitous BP monitoring. First, the arterial BP is determined by many other factors in addition to the PTT. Hence, taking only PTT into the estimation cannot fully represent BP. Second, most studies employed PTT to estimate the SBP rather than DBP or MBP. Third, most of the studies have attempted to use cuff-based and regular calibration to remain the acceptable accuracy, a simple and cuff-less calibration approach needs to be investigated taking into account the convenience of the patients. Forth, the PTT/PWV methods could be affected by the arteries diseases and most of the reviewed studies exclude CVD patients from their validation data. It is essential to consider large databases include both patients and healthy people to investigate the estimation precision and robustness. Finally, as most of the studies compared their results with a cuff-based technology and used a cuff-based device for calibration, the accuracy of the reference device needs to be mentioned in any comparative study.
Importantly, it is crucial that the BP measurement technique meets the standard for evaluating BP measurement accuracy. The difference between test value and the reference value is considered as the accuracy of the device. This accuracy could be calculated in terms of standard deviation, mean absolute difference or absolute difference. Generally, there are four standards with different criteria for evaluation of the accuracy of BP monitoring device. These standards are included the British Hypertension Society (BHS) standard [30], the Association for the AAMI standards [29], the IEEE standard for Wearable, Cuffless Blood Pressure Measuring Devices [96], and the European Society of Hypertension (ESH) evaluation standard [97].
Several machine learning-based studies have challenged the limitation of PTT-based methods. It is found that the performance and accuracy of BP measurements have been improved by considering more comprehensive features related to BP and employing multi fusion parameter extraction techniques. Machine learning as one of the most intelligent, efficient, and popular technique has been used to select optimal features related to BP and estimate BP continuously and non-invasively by combining physiological and mathematical modeling. A wide variety of supervised and unsupervised machine learning techniques such as SVM and random forest were used to overcome the limitation in complex mathematical concepts. However, to compete with traditional BP monitoring devices, more studies need to be conducted to evaluate the existing methods with the ideal sample size. Moreover, it is possible to overcome the main issues of analysing complex cardiovascular systems by employing fast and straightforward algorithms to select the features that can best define BP. Besides, it is critical to allocate ample memory storage for implanting a continuous BP monitoring device with big collected data in a clinical setting.
Overall, this study indicated that there is a potential of machine learning-based method for BP monitoring but none of the existing techniques possesses sufficient accuracy to allow them to replace traditional BP measurement techniques. With the advanced architecture of deep learning design, there is a chance to detect the best patterns for BP estimation and overcome the non-linear complex biological relationship. Optimized design of machine learning methods could transform classic clinical methods to well-designed clinical trial model and play a significant role in the early stages of hypertension treatments. In the next studies, further research and validation are needed to evaluate the accuracy and validity of machine learning techniques in the clinical setting.
Conclusion and Future direction
This review has focused on various non-invasive continuous BP measurement techniques with great potential for widely clinically use. It was found that methods such as PTT-based and machine learning-based can enhance the required accuracy of BP monitoring devices. Advanced features of deep learning are inspiring researchers towards the adoption of Artificial Intelligence (AI) in clinical settings. However, current machine learning methods are still in their preliminary stage, and at this point, there is no valid design to replace the traditional BP measurements.
This review paper investigated the current state of the art of the continuous and cuff-less BP monitoring and discussed their challenges. It was found that while obstacles in developing clinically cuff-less and continuous BP monitoring remain, the desire to finding an ambulatory technology with connectivity online network is strong. Moreover, the need for home-based technology is more evident in the case of CVD and sleep apnea patients. The early diagnosis and treatment of BP-related events could save lives. We aim to consider the combination of more variables such as dietary, environmental and physiological factors into the conventional BP factors for further development of a continuous BP measurement system.
The brain-spired mathematical models, known as AI, have been used as primary tools in machine learning. They are one of the most promising techniques to recognize patterns of too complex functions and emulate the nonlinear relationship between inputs and outputs of nonlinear systems. Particularly, the deep learning class of machine learning algorithms have shown promising results in biomedical technologies such as risk assessment for hypertension [88], and echocardiography images analysis [90].
Considering the fact that convolutional neural network (CNN) is the most popular technique used in deep learning [98], we have found that a CNN-based architecture could be investigated as continuous and cuff-less BP monitoring technique using the ECG and PPG as input signals. One of the significant benefits of such method is the ability of CNNs to perform perception tasks, which allows them to learn the BP relevant features from ECG and PPG signals and skip the complicated feature extraction step. Therefore, the first step would be choosing a suitable architecture for the network and then train it with ECG and PPG signals as a training set. The last layer of the network would be a regression layer to estimate BP as the output of the proposed system.
In the future, the wearable and ambulatory technology will emerge as reliable, accurate, clinically adaptable, and user-friendly technologies. These technologies will give the chance of real-time risk factor modification based on data from system biology, lifestyle, and electronic health records.
References
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT (2003) Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42(6):1206–1252
Williams JS, Brown SM, Conlin PR (2009) Blood-pressure measurement. N Engl J Med 360(5):e6
Modesti PA, Agostoni P, Agyemang C, Basu S, Benetos A, Cappuccio FP, Ceriello A, Del Prato S, Kalyesubula R, O’Brien E (2014) Cardiovascular risk assessment in low-resource settings: a consensus document of the European Society of Hypertension Working Group on Hypertension and Cardiovascular Risk in Low Resource Settings. J Hypertens 32(5):951
Mensah GA, Croft JB, Giles WH (2002) The heart, kidney, and brain as target organs in hypertension. Cardiol Clin 20(2):225–247
World Health Organization (WHO) Global Health Observatory (GHO) data https://www.who.int/mediacentre/factsheets/fs317/en/. Accessed 10 Aug 2018
Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, Burnett R, Casey D, Coates MM, Cohen A (2015) Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet 386(10010):2287–2323
Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, Bahonar A, Chifamba J, Dagenais G, Diaz R (2013) Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high, middle, and low-income countries. JAMA 310(9):959–968
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, AlMazroa MA, Amann M, Anderson HR, Andrews KG (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet 380(9859):2224–2260
Pickering TG, Shimbo D, Haas D (2006) Ambulatory blood-pressure monitoring. N Engl J Med 354(22):2368–2374
Hermida RC, Smolensky MH, Ayala DE, Portaluppi F, Crespo JJ, Fabbian F, Haus E, Manfredini R, Mojon A, Moya A (2013) 2013 Ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goals: joint recommendations from the International Society for Chronobiology (ISC), American Association of Medical Chronobiology and Chronotherapeutics (AAMCC), Spanish Society of Applied Chronobiology, Chronotherapy, and Vascular Risk (SECAC). Chronobiol Int 30(3):355–410
Group SR (2015) A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015(373):2103–2116
Zheng Y-L, Ding X-R, Poon CCY, Lo BPL, Zhang H, Zhou X-L, Yang G-Z, Zhao N, Zhang Y-T (2014) Unobtrusive sensing and wearable devices for health informatics. IEEE Trans Biomed Eng 61(5):1538–1554
Steinhubl SR, Muse ED, Barrett PM, Topol EJ (2016) Off the cuff: rebooting blood pressure treatment. Lancet 388(10046):749
Moran AE, Odden MC, Thanataveerat A, Tzong KY, Rasmussen PW, Guzman D, Williams L, Bibbins-Domingo K, Coxson PG, Goldman L (2015) Cost-effectiveness of hypertension therapy according to 2014 guidelines. N Engl J Med 372(5):447–455
Ghasemzadeh N, Zafari AM (2011) A brief journey into the history of the arterial pulse. Cardiol Res Pract. https://doi.org/10.4061/2011/164832
Fye WB (1993) Disorders of the heartbeat: a historical overview from antiquity to the mid-20th century. Am J Cardiol 72(14):1055–1070
O’Rourke MF, O’Brien C, Edelman ER (2016) Arterial stiffening in perspective: advances in physical and physiological science over centuries. Am J Hypertens 29(7):785–791
Ward M, Langton JA (2007) Blood pressure measurement. Continuing education in anaesthesia, Crit Care Pain 7(4):122–126
Chung E, Chen G, Alexander B, Cannesson M (2013) Non-invasive continuous blood pressure monitoring: a review of current applications. Front Med 7(1):91–101
Mukkamala R, Hahn J-O, Inan OT, Mestha LK, Kim C-S, Töreyin H, Kyal S (2015) Toward ubiquitous blood pressure monitoring via pulse transit time: theory and practice. IEEE Trans Biomed Eng 62(8):1879–1901
Shin JH, Lee KM, Park KS (2009) Non-constrained monitoring of systolic blood pressure on a weighing scale. Physiol Meas 30(7):679
Wu K-f, Chan C-h, Zhang Y-t (2016) Contactless and cuffless monitoring of blood pressure on a chair using e-textile materials. 3rd IEEE/EMBS International Summer School on Medical Devices and Biosensors, pp 98–100
Poon CC, Wong YM, Zhang Y-t (2006) M-health: the development of cuff-less and wearable blood pressure meters for use in body sensor networks. Life Science Systems and Applications Workshop, IEEE/NLM. IEEE, pp 1–2
Shaltis PA, Reisner AT, Asada HH (2008) Cuffless blood pressure monitoring using hydrostatic pressure changes. IEEE Trans Biomed Eng 55(6):1775–1777
Zhang Y-t, Poon CC, Chan C-h, Tsang MW, Wu K-f (2006) A health-shirt using e-textile materials for the continuous and cuffless monitoring of arterial blood pressure. 3rd IEEE/EMBS International Summer School on Medical Devices and Biosensors, pp 86–89
Poon CC, Zhang Y-T, Bao S-D (2006) A novel biometrics method to secure wireless body area sensor networks for telemedicine and m-health. IEEE Commun Mag 44(4):73–81
Jeong IC, Finkelstein J (2016) Introducing contactless blood pressure assessment using a high speed video camera. J Med Syst 40(4):77
Ding X-R, Zhao N, Yang G-Z, Pettigrew RI, Lo B, Miao F, Li Y, Liu J, Zhang Y-T (2016) Continuous blood pressure measurement from invasive to unobtrusive: celebration of 200th birth anniversary of carl ludwig. IEEE J Biomed Health Inform 20(6):1455–1465
ANSI A (2002) & ANSI/AAMI SP10: 2002/A1: 2003. American National Standard Manual, electronic, or automated sphygmomanometers
O’Brien E, Petrie J, Littler W, de Swiet M, Padfield PL, Altman D, Bland M, Coats A, Atkins N (1993) The British Hypertension Society protocol for the evaluation of blood pressure measuring devices. J Hypertens 11(Suppl 2):S43–S62
Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, Morgenstern BZ (1993) Human blood pressure determination by sphygmomanometry. Circulation 88(5):2460–2470
Taha Z, Shirley L, Razman MAM (2017) A review on non-invasive hypertension monitoring system by using photoplethysmography method. Mov Health Exerc 6(1):47–57
Peter L, Noury N, Cerny M (2014) A review of methods for non-invasive and continuous blood pressure monitoring: Pulse transit time method is promising? IRBM 35(5):271–282
Alpert BS, Quinn D, Gallick D (2014) Oscillometric blood pressure: a review for clinicians. J Am Soc Hypertens 8(12):930–938
Forouzanfar M, Ahmad S, Batkin I, Dajani HR, Groza VZ, Bolic M (2013) Coefficient-free blood pressure estimation based on pulse transit time–cuff pressure dependence. IEEE Trans Biomed Eng 60(7):1814–1824
Zheng D, Di Marco LY, Murray A (2014) Effect of respiration on Korotkoff sounds and oscillometric cuff pressure pulses during blood pressure measurement. Med Biol Eng Comput 52(5):467–473
Kim S-H, Lilot M, Sidhu KS, Rinehart J, Yu Z, Canales C, Cannesson M (2014) Accuracy and precision of continuous noninvasive arterial pressure monitoring compared with invasive arterial pressure: a systematic review and meta-analysis. Anesthesiology 120(5):1080–1097
Hansen S, Staber M (2006) Oscillometric blood pressure measurement used for calibration of the arterial tonometry method contributes significantly to error. Eur J Anaesthesiol 23(9):781–787
Kontis V, Mathers CD, Rehm J, Stevens GA, Shield KD, Bonita R, Riley LM, Poznyak V, Beaglehole R, Ezzati M (2014) Contribution of six risk factors to achieving the 25 × 25 non-communicable disease mortality reduction target: a modelling study. Lancet 384(9941):427–437
McGhee BH, Bridges EJ (2002) Monitoring arterial blood pressure: what you may not know. Crit Care Nurse 22:60–79
Brzezinski M, Luisetti T, London MJ (2009) Radial artery cannulation: a comprehensive review of recent anatomic and physiologic investigations. Int Anesth Res Soc 109(6):1763–1781
Li-wei HL, Saeed M, Talmor D, Mark R, Malhotra A (2013) Methods of blood pressure measurement in the ICU. Crit Care Med 41(1):34
Hennig A, Patzak A (2013) Continuous blood pressure measurement using pulse transit time. Somnologie-Schlafforschung und Schlafmedizin 17(2):104–110
Ding X, Dai W, Luo N, Liu J, Zhao N, Zhang Y (2015) A flexible tonoarteriography-based body sensor network for cuffless measurement of arterial blood pressure. IEEE 12th International Conference on Wearable and Implantable Body Sensor Networks (BSN), pp 1–4
Ding X-R, Zhang Y-T, Liu J, Dai W-X, Tsang HK (2016) Continuous cuffless blood pressure estimation using pulse transit time and photoplethysmogram intensity ratio. IEEE Trans Biomed Eng 63(5):964–972
Ding X-R, Zhang Y-T (2015) Photoplethysmogram intensity ratio: A potential indicator for improving the accuracy of PTT-based cuffless blood pressure estimation. 2015 IEEE 37th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), pp 398–401
Ding X-R, Zhang Y-T, Tsang HK (2016) A new modeling methodology for continuous cuffless blood pressure measurement. 2016 IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI). IEEE, pp 264–267
Lin W-H, Wang H, Samuel OW, Li G (2017) Using a new PPG indicator to increase the accuracy of PTT-based continuous cuffless blood pressure estimation. 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), pp 738–741
Liu J, Zhang Y-T, Ding X-R, Dai W-X, Zhao N (2016) A preliminary study on multi-wavelength PPG based pulse transit time detection for cuffless blood pressure measurement. IEEE 38th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), pp 615–618
Liu J, Li Y, Ding X-R, Dai W-X, Zhang Y-T (2015) Effects of cuff inflation and deflation on pulse transit time measured from ECG and multi-wavelength PPG. IEEE 37th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), pp 5973–5976
Jeong IC, Finkelstein J (2016) Introducing contactless blood pressure assessment using a high speed video camera. J Med Syst 40(4):1–10
Sun Y, Thakor N (2016) Photoplethysmography revisited: from contact to noncontact, from point to imaging. IEEE Trans Biomed Eng 63(3):463–477
Ghosh S, Banerjee A, Ray N, Wood PW, Boulanger P, Padwal R (2016) Continuous blood pressure prediction from pulse transit time using ECG and PPG signals. IEEE Healthcare Innovation Point-Of-Care Technologies Conference (HI-POCT), pp 188–191
Visvanathan A, Sinha A, Pal A (2013) Estimation of blood pressure levels from reflective photoplethysmograph using smart phones. IEEE 13th International Conference on Bioinformatics and Bioengineering (BIBE), pp 1–5
Atef M, Xiyan L, Wang G, Lian Y (2016) PTT based continuous time non-invasive blood pressure system. IEEE 59th International Midwest Symposium on Circuits and Systems (MWSCAS), pp 1–4
Junior AD, Murali S, Rincon F, Atienza D (2016) Methods for reliable estimation of pulse transit time and blood pressure variations using smartphone sensors. Microprocess Microsyst 46:84–95
Dai W-X, Zhang Y-T, Liu J, Ding X-R, Zhao N (2016) Dual-modality arterial pulse monitoring system for continuous blood pressure measurement. IEEE 38th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), pp 5773–5776
Yang C, Tavassolian N (2017) Pulse transit time measurement using seismocardiogram, photoplethysmogram, and acoustic recordings: evaluation and comparison. IEEE J Biomed Health Inform 22(3):733–740
Van Velzen MH, Loeve AJ, Niehof SP, Mik EG (2017) Increasing accuracy of pulse transit time measurements by automated elimination of distorted photoplethysmography waves. Med Biol Eng Comput 55(11):1989–2000
Ibrahim B, Nathan V, Jafari R (2017) Exploration and validation of alternate sensing methods for wearable continuous pulse transit time measurement using optical and bioimpedance modalities. In: 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), pp 2051–2055
Carek AM, Conant J, Joshi A, Kang H, Inan OT (2017) SeismoWatch: wearable cuffless blood pressure monitoring using pulse transit time. Proc ACM Interact Mob Wearable Ubiquitous Technol 1(3):40
Chen Y, Cheng S, Wang T, Ma T (2017) Novel blood pressure estimation method using single photoplethysmography feature. 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), pp 1712–1715
Buxi D, Redouté J-M, Yuce MR (2017) Blood pressure estimation using pulse transit time from bioimpedance and continuous wave radar. IEEE Trans Biomed Eng 64(4):917–927
Sola J, Proença M, Ferrario D, Porchet J-A, Falhi A, Grossenbacher O, Allemann Y, Rimoldi SF, Sartori C (2013) Noninvasive and nonocclusive blood pressure estimation via a chest sensor. IEEE Trans Biomed Eng 60(12):3505–3513
Prabhu V, Kuppusamy P, Karthikeyan A, Sucharitha M (2018) A novel approach for non-invasive measurement of mean arterial pressure using pulse transit time. Multimed Tools Appl. https://doi.org/10.1007/s11042-018-6971-8
Meinders JM, Hoeks AP (2004) Simultaneous assessment of diameter and pressure waveforms in the carotid artery. Ultrasound Med Biol 30(2):147–154
Weber S, Scharfschwerdt P, Schauer T, Seel T, Kertzscher U, Affeld K (2013) Continuous wrist blood pressure measurement with ultrasound. Biomed Eng. https://doi.org/10.1515/bmt-2013-4124
Seo J, Pietrangelo SJ, Lee H-S, Sodini CG (2015) Noninvasive arterial blood pressure waveform monitoring using two-element ultrasound system. IEEE Trans Ultrason Ferroelectr Freq Control 62(4):776–784
Joseph J, Nabeel P, Shah MI, Sivaprakasam M (2016) Arterial compliance probe for calibration free pulse pressure measurement. IEEE International Symposium on Medical Measurements and Applications (MeMeA), pp 1–6
Zakrzewski AM, Anthony BW (2017) Arterial blood pressure estimation using ultrasound: clinical results on healthy volunteers and a medicated hypertensive volunteer. 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), pp 2154–2157
Ding X-R, Zhang Y-T, Tsang HK (2016) A New Modeling Methodology for Continuous Cuffless Blood Pressure Measurement. IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI), pp 264–267
Escobar B, Torres R (2014) Feasibility of non-invasive blood pressure estimation based on pulse arrival time: a MIMIC Database Study. Computing in Cardiology Conference (CinC), pp 1113–1116
Tang Z, Tamura T, Sekine M, Huang A, Chen W, Yoshida M, Sakatani K, Kobayashi H, Kanaya S (2016) A chair-based unobtrusive cuffless blood pressure monitoring system based on pulse arrival time. IEEE J Biomed Health Informat 21(5):1194–1205
Zhang Q, Chen X, Fang Z, Xue Y, Zhan Q, Yang T, Xia S (2017) Cuff-less blood pressure measurement using pulse arrival time and a Kalman filter. J Micromech Microeng 27(2):024002
Zheng Y, Poon CC, Yan BP, Lau JY (2016) Pulse arrival time based cuff-less and 24-H wearable blood pressure monitoring and its diagnostic value in hypertension. J Med Syst 40(9):195
Rajala S, Ahmaniemi T, Lindholm H, Taipalus T (2017) Pulse arrival time (PAT) measurement based on arm ECG and finger PPG signals-comparison of PPG feature detection methods for PAT calculation. 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), pp 250–253
Wu TH, Pang GK-H, Kwong EW-Y (2014) Predicting systolic blood pressure using machine learning. 7th International Conference on Information and Automation for Sustainability (ICIAfS), pp 1–6
Yoshioka M, Bounyong S (2017) Regression-forests-based estimation of blood pressure using the pulse transit time obtained by facial photoplethysmogram. 2017 International Joint Conference on Neural Networks (IJCNN), pp 3248–3253
He R, Huang Z-P, Ji L-Y, Wu J-K, Li H, Zhang Z-Q (2016) Beat-to-beat ambulatory blood pressure estimation based on random forest. IEEE 13th International Conference on Wearable and Implantable Body Sensor Networks (BSN), pp 194–198
Zhang Y, Feng Z (2017) A SVM method for continuous blood pressure estimation from a PPG signal. Proceedings of the 9th International Conference on Machine Learning and Computing. ACM, pp 128–132
Xing X, Sun M (2016) Optical blood pressure estimation with photoplethysmography and FFT-based neural networks. Biomed Opt Express 7(8):3007–3020
Xu Z, Liu J, Chen X, Wang Y, Zhao Z (2017) Continuous blood pressure estimation based on multiple parameters from eletrocardiogram and photoplethysmogram by back-propagation neural network. Comput Ind 89:50–59
Miao F, Fu N, Zhang Y-T, Ding X-R, Hong X, He Q, Li Y (2017) A novel continuous blood pressure estimation approach based on data mining techniques. IEEE J Biomed Health Informat 21(6):1730–1740
Atomi K, Kawanaka H, Bhuiyan MS, Oguri K (2017) Cuffless blood pressure estimation based on data-oriented continuous health monitoring System. Comput Math Methods Med. https://doi.org/10.1155/2017/1803485
Xu J, Jiang J, Zhou H, Yan Z (2017) A novel blood pressure estimation method combing pulse wave transit time model and neural network model. 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), pp 2130–2133
Campo D, Khettab H, Yu R, Genain N, Edouard P, Buard N, Boutouyrie P (2017) Measurement of aortic pulse wave velocity with a connected bathroom scale. Am J Hypertens 30(9):876–883
Hsieh Y-Y, Wu C-D, Lu S-S, Tsao Y (2016) A linear regression model with dynamic pulse transit time features for noninvasive blood pressure prediction. IEEE of Biomedical Circuits and Systems Conference (BioCAS), pp 604–607
Rodrigues JC, Amadu AM, Ghosh Dastidar A, McIntyre B, Szantho GV, Lyen S, Godsave C, Ratcliffe LE, Burchell AE, Hart EC (2016) ECG strain pattern in hypertension is associated with myocardial cellular expansion and diffuse interstitial fibrosis: a multi-parametric cardiac magnetic resonance study. Eur Heart J 18(4):441–450
Saeki M, Sato N, Kawasaki M, Tanaka R, Nagaya M, Watanabe T, Ono K, Noda T, Zile MR, Minatoguchi S (2015) Left ventricular layer function in hypertension assessed by myocardial strain rate using novel one-beat real-time three-dimensional speckle tracking echocardiography with high volume rates. Hypertens Res 38(8):551
Madani A, Arnaout R, Mofrad M, Arnaout R (2018) Fast and accurate view classification of echocardiograms using deep learning. npj Dig Med 1 (1):6
van Everdingen WM, Maass AH, Vernooy K, Meine M, Allaart CP, De Lange FJ, Teske AJ, Geelhoed B, Rienstra M, Van Gelder IC (2017) Comparison of strain parameters in dyssynchronous heart failure between speckle tracking echocardiography vendor systems. Cardiovasc Ultrasound 15(1):25
Lee S, Chang J-H (2017) Oscillometric blood pressure estimation based on deep learning. IEEE Trans Industr Inf 13(2):461–472
Lee S, Chang J-H (2017) Deep learning ensemble with asymptotic techniques for oscillometric blood pressure estimation. Comput Methods Programs Biomed 151:1–13
Peng Su, Xiao-Rong Ding, Yuan-Ting Zhang, Jing Liu, Fen Miao, Zhao N (2018) Long-term blood pressure prediction with deep recurrent neural networks. 2018 IEEE Conference on Biomedical and Health Informatics (BHI)
Zhao Q, Hu X, Lin J, Deng X, Li H (2019) A novel short-term blood pressure prediction model based on LSTM. AIP Conference Proceedings. vol 1. AIP Publishing, p 020003
Association IS (2014) IEEE standard for wearable cuffless blood pressure measuring devices. IEEE Std 1708–2014
O'Brien E, Atkins N, Stergiou G, Karpettas N, Parati G, Asmar R, Imai Y, Wang J, Mengden T, Shennan A (2010) European Society of Hypertension International Protocol revision 2010 for the validation of blood pressure measuring devices in adults. Blood Press Monit 15(1):23–38
Tsinalis O, Matthews PM, Guo Y, Zafeiriou S (2016) Automatic sleep stage scoring with single-channel EEG using convolutional neural networks. Cornell University, Ithaca
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rastegar, S., GholamHosseini, H. & Lowe, A. Non-invasive continuous blood pressure monitoring systems: current and proposed technology issues and challenges. Phys Eng Sci Med 43, 11–28 (2020). https://doi.org/10.1007/s13246-019-00813-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-019-00813-x