Abstract
Multiple disparities exist in human papillomavirus (HPV)-related cancers and HPV vaccination series initiation and completion in the USA. This chapter highlights community-based intervention research aimed at increasing HPV vaccination and addressing these disparities. First, the chapter provides an overview of HPV, HPV-related cancers, and HPV vaccination, including current recommendations from health and professional organizations, as well as trends in uptake in the USA. Next, the chapter describes HPV vaccination rates and unique challenges, barriers, and facilitators to vaccination among multiple US population groups that experience HPV-related disparities. Population groups featured in the chapter include individuals who live in rural areas, those who are medically underserved with limited financial resources, those who are from racial/ethnic minority groups, those who were born outside of the USA, those aged 18–26 years, and those who identify as being from sexual and gender minority groups. Findings from intervention research conducted among these specific population groups and in novel settings are also described. Finally, gaps in the literature and directions for future community-based research studies are identified.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Overview/Introduction
Human papillomavirus (HPV) is the most common sexually transmitted infection in the USA [1]. Spread through intimate skin-to-skin contact [2], more than 40 HPV types can infect human anogenital regions and mouths and throats of people through vaginal, anal, and oral sex [3]. Sexually transmitted HPV types are categorized as either low-risk or high-risk [2, 4]. Low-risk HPV types (e.g., HPV types 6, 11, 26, 40, 42, 53, 54, 55, 57, 66, 73, 82, 83, 84, 73) can cause anogenital warts and recurrent respiratory papillomatosis, whereas high-risk HPV types (e.g., HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68) can lead to multiple types of cancers in humans [4]. The majority of HPV-related cancers are attributed to high-risk HPV types 16 and 18; [5] and globally by region, the two most common HPV types are types 16 and 18 [2].
Most sexually active people will be infected with at least one HPV type at some point in their lifetime [2]. The majority of individuals are infected with HPV during or shortly after their initial sexual experience [1]. Most HPV infections are asymptomatic and resolve on their own within 2 years [2]. However, in some individuals, high-risk HPV infections persist and over the course of years can develop into oropharyngeal and anal cancers regardless of gender or biological sex at birth, penile cancer among those born male, and cervical, vaginal, and vulvar cancers among those born female [2].
In the USA, approximately 34,800 cancer cases each year are caused by HPV infections [6]. From 2012 to 2016 in the USA, 91% cases of cervical cancers and 91% of anal cancers were caused by high-risk HPV types [6]. Furthermore, most vaginal (75%), oropharyngeal (71%), vulvar (69%), and penile cancers (63%) diagnosed in the USA between 2012 and 2016 were also caused by infections from high-risk HPV types [6]. Importantly, marked disparities in HPV prevalence and/or HPV-related cancers exist based on geography, rurality, gender, race/ethnicity, and sexual and gender minority status [7,8,9]. HPV vaccination has the potential to significantly address HPV-related cancer incidence, mortality, and disparities.
Three vaccines against HPV infection have been licensed by the US Food and Drug Administration (FDA) [10]. The bivalent vaccine (2vHPV), which prevents HPV types 16 and 18, was approved in 2009 for females ages 10–25 initially [11] and subsequently extended to include 9-year-old females [11]. The quadrivalent vaccine (4vHPV) was approved for females ages 9–26 in 2006 [12] and males ages 9–26 in 2009 [13] and guards against HPV types 6, 11, 16, and 18. The nine-valent vaccine (9vHPV), which protect against HPV types 6, 11, 16, 18, 31, 33, 45, 52, and 58, was approved in 2014 for females ages 9–26 and males ages 9–15 years [14]. Approval of the 9vHPV vaccine was later extended to include males ages 16–26 years [15]. In October 2018, the FDA further extended its approval of the 9vHPV vaccine to those ages 27–45 [16]. Since 2016, only the nine-valent vaccine has been utilized in the USA [17]. Approximately 92% of HPV-related cancers in the USA each year are caused by one of the HPV types for which the 9vHPV vaccine offers protection; thus, more than 32,000 HPV-attributed cancers in the USA could be prevented each year if those ages 9–26 years received the HPV vaccine [6].
The US Advisory Committee on Immunization Practices (ACIP) has issued recommendations related to both adolescent and adult HPV vaccine administration [10]. ACIP recommendations have included routine vaccination for 11- and 12-year-old females and males since 2006 and 2011, respectively [18]. The HPV vaccine is recommended during early adolescence due to the strong immune response experienced among young adolescents as well as decreased likelihood that adolescents have prior exposure to HPV (i.e., vaccination is most effective when given prior to sexual debut) [18]. ACIP recommendations have stated that the vaccine can be administered starting at age 9 [18]. Current ACIP recommendations state that individuals who have not previously completed the HPV vaccine series are recommended to receive the vaccine through age 26 [18]. Among those aged 27–45 years, in June 2019, ACIP recommended shared clinical decision-making to consider benefits and limitations of vaccination in an age group where the majority will have had prior exposure to HPV [18]. Since 2016, ACIP recommendations have stated that individuals ages 9–14 receive two doses of the HPV vaccine, while individuals ages 15 years and older and those who are immunocompromised receive three doses [19].
Overall, US HPV vaccination rates have been trending upward among both adolescents and young adults (AYA) [10, 20]. HPV vaccine rates from the 2018 National Immunization Survey-Teen (NIS-Teen)—the most recent year for which data were available at the time of writing—were 68.1% for series initiation (at least one dose) of the HPV vaccine series and 51.1% for series completion (up-to-date on all recommended doses) among adolescents ages 13–17 years [21]. Like other adolescent vaccinations, HPV vaccination requires parental consent under the age of 18 years. However, it is notable that HPV vaccination receipt rates trail uptake rates for other adolescent vaccinations; rates of one or more doses of a meningococcal vaccine (MenACWY) was 86.6% and uptake of tetanus and reduced diphtheria toxoids and acellular pertussis vaccine (Tdap) was 88.9% in 2018 [21]. Among adults ages 18–26 years, HPV vaccine rates from the 2018 National Health Interview Survey (NHIS)—the most recent year for which data were available at the time of writing—were 39.9% for series initiation and 21.5% for series completion [20]. However, HPV vaccination initiation and completion rates vary across multiple factors, including geography (e.g., region, state, rural) and sociodemographic factors (e.g., biological sex, ethnicity, health insurance status) [21]. For instance, in 2018, Rhode Island had the highest HPV rate of teens ages 13–17 years receiving one or more HPV vaccine doses in the USA (89.3%), whereas Mississippi had the lowest rate of teens ages 13–17 years receiving one or more HPV vaccine doses (51.7%) [22]. Of note, as of 2019, Rhode Island was one of four locations in the USA with an HPV vaccine school entry requirement; the other locations are Virginia (females only), Puerto Rico, and Washington D.C. [23]. In 2020, an HPV vaccine school entry requirement rule will go into effect in Hawaii [24]. In addition, males have historically had lower initiation and completion rates compared to females, due in part to the delay in approval of the vaccine for males [20, 21]. Racial and ethnic minority adolescents are more likely to initiate the vaccine series but less likely to complete the series compared to non-Hispanic Whites [25]. Non-Hispanic White adults are more likely than Hispanic adults to have initiated the HPV vaccine series [20]. Variability in HPV vaccination series initiation and completion related to rural, medically underserved, and sexual and gender minority populations will be further described in subsequent sections of the current chapter, followed by a discussion of novel intervention settings to address the need for innovative strategies to increase HPV vaccine series initiation and completion.
HPV Vaccination Among Individuals Living in Rural Communities
Rural vs. Urban HPV Vaccination Rates
Rural geographic disparities in HPV vaccine coverage have persisted since the introduction of the vaccine, with lower vaccination in rural areas compared to urban and/or suburban areas, regardless of the definition of rurality used. Early studies examining HPV vaccine series initiation among females in 2006–2008, the first few years after approval for females, found significantly lower rates of initiation among girls living in rural areas compared to urban areas, based on data from self-reported surveys and Medicaid claims [26, 27]. In the first year after approval of the vaccine for males, 2011 NIS-Teen data indicated low rates for both female and male adolescents, with highest initiation (≥ 1 dose) for those living in mostly urban areas (56.9% among females; 10.3% among males), followed by suburban areas (53.1% among females; 7.2% among males), and then lowest in mostly rural areas (43.1% among females; 6.4% among males) [28]. Multiple studies detected the same pattern for adolescents in subsequent years [29,30,31].
According to 2018 NIS-Teen data, the HPV vaccination coverage rates for adolescents reaffirmed the pattern of lower coverage with decreasing levels of urbanicity, both for series initiation (71.9% mostly urban, 66.6% suburban, 59.5% mostly rural) and completion (56.1% mostly urban, 49.1% suburban, 40.7% mostly rural) [21]. An in-depth characterization of adolescents stratified by these three metropolitan statistical area categories found that the urban-to-rural gradient pattern was consistent across all subgroups for age, gender, immigration status, and US region [32]. The pattern was also consistent for non-Hispanic Whites and Hispanics of any race; however, for non-Hispanic Blacks, there was no difference between mostly urban and suburban residents, and the difference between mostly urban and mostly rural was not significant, potentially due to a small sample size in NIS-Teen for Blacks living in mostly rural areas.
Unique Challenges, Barriers, and Facilitators for Rural Populations
Rural populations experience a number of structural, system-level barriers to accessing healthcare, such as long distance to care, lack of public transportation, shortage of healthcare providers and facilities, and limited broadband internet access [33, 34]. After accessing care, rural patients are more likely to experience provider-level barriers, such as lack of provider recommendation for HPV vaccine [35, 36] and poor-quality provider communication [37]. In 2011 NIS-Teen, rural parents were less likely than urban or suburban parents to report having a collaborative conversation with their healthcare provider about HPV vaccination, and this communication difference significantly explained, or mediated, the rural versus urban/suburban disparity in HPV vaccination rates [37].
At the individual level, rural residents delay care more often due to higher rates of poverty and unemployment, and low levels of HPV-specific knowledge compared to urban and suburban residents, as well as health beliefs [33, 36, 38,39,40,41]. An analysis of data from the 2013 to 2017 Health Information National Trends Survey (HINTS) found that rural adults were less likely than urban adults to be aware of HPV and HPV vaccine, and they were less likely to know that HPV is a sexually transmitted infection and that it causes cervical cancer [42]. Certain parental health beliefs associated with greater HPV vaccine hesitancy in rural areas include concerns about vaccine safety, beliefs that the vaccine is not necessary or that one’s child is not at risk, and general fatalistic health beliefs [39, 43,44,45,46].
Interventions to Address Rural Disparities in HPV Vaccine Initiation and Completion
A limited number of interventions have been developed and tested that specifically target the unique barriers to HPV vaccination experienced by rural populations, as described below.
School-Based Interventions
In 2012–2013, Vanderpool and colleagues tested a school-based intervention in two high schools located in a rural county in south-central Kentucky, developed in partnership with the local public health department [47]. The school nurses utilized multiple communication channels to inform parents/students of the opportunity to receive the HPV vaccine at school after completing the required consent form as well as promotional incentives for participation. Nurses implemented grade-specific immunization clinics on site during the school day. Free vaccines were provided to all interested students with consent forms, either through the federal Vaccines for Children (VFC) program or covered by the project, since the nurses could not bill private insurance companies. The intervention resulted in improvements in the schools’ HPV vaccine initiation rate from 24% to 57% and the completion rate from 14% to 45%.
Economic Incentives for Adult Women
Cost is a substantial barrier to HPV vaccination for adults ages 18 and older since they do not qualify for free vaccines under the federal VFC program. Vanderpool and colleagues assessed rural-urban differences in the effect of removing the cost barrier for young adult women [48, 49]. In 2007–2009, the team enrolled and provided free HPV vaccine vouchers to 706 women in three clinic settings in eastern Kentucky. They observed significantly higher series initiation in the urban university clinic (50.7%) compared to a rural clinic (45.1%) and a rural community college clinic (6.8%).
Multilevel Interventions
In 2009, an academic-community partnership in North Carolina developed a theory-based, social culturally targeted marketing campaign for rural mothers of girls ages 11–12, as well as their healthcare providers and the media as important behavior influencers [50]. The team tested the multilevel, community-wide campaign in four rural counties, distributing materials via public and private health clinics and via a variety of community venues. High engagement of the healthcare providers, organizations, and mothers was documented. However, the study produced mixed results. Two of the four intervention counties experienced a modest increase in HPV vaccine initiation rates at 2% points above the trend observed in control counties, while the other two counties did not improve.
Another study in North Carolina assessed a multilevel, community-wide intervention in one rural county, compared to four control counties for 12 months during 2012–2013 [51]. The two-phase intervention included the following: (1) Phase 1 (practice-/provider-level) which is a 1-hour provider/staff education session about implementing immunization registry-driven recall with postcard reminders, optional web-based registry trainings, pre-printed postcards and posters, financial incentives for sending reminders (up to $1000), and coaching phone calls every 2 weeks and (2) Phase 2 (school-level) which is nontargeted school-generated telephone reminders sent from school to parents of adolescents. The study resulted in significant improvements in population-level HPV initiation and completion rates for adolescents, with the largest improvements among 11- and 12-year-olds (series initiation improvement of 14.2–32.1% for boys and 27.4–43.4 for girls).
In 2010–2015, an academic-community partnership designed a multilevel intervention that was culturally targeted for predominantly rural counties in the Appalachian region of Ohio [52, 53]. The intervention components included clinic-level promotion of HPV vaccine educational materials; a 1-hour provider-level training session; and parent-level education delivered via a mailed brochure, DVD video, magnet reminder, and a telephone educational session. A group-randomized trial in 24 clinics across 12 counties demonstrated that the intervention resulted in a small but significant increase in HPV vaccination series initiation by 6 months among the enrolled patients who were not vaccinated at baseline compared to the control group (13.1% versus 6.5%, respectively).
HPV Vaccination Among Medically Underserved Individuals and Those of Limited Financial Resources
HPV Vaccine Initiation and Completion Among Medically Underserved Individuals and Those of Limited Financial Resources
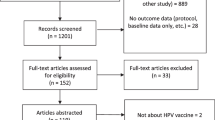
Individuals are defined as being part of a medically underserved population if there is “a shortage of providers for a specific group of people within a defined geographic area.” [54] Commonly cited medically underserved populations include those who are Medicaid-eligible, low income, migrant farm workers, homeless, and Native Americans [54]. Among medically underserved adolescents (i.e., individuals receiving care at federally qualified health centers (FQHC), safety net clinics, or funded by Medicaid), HPV vaccine initiation estimates, without intervention, vary widely across studies and show a general pattern of increasing prevalence over time (Fig. 1) [27, 55,56,57,58,59,60,61,62,63,64,65,66,67,68,69]. HPV vaccine initiation estimates range from a low of 4.5% among 10- to 26-year-old females attending a Kansas City safety net center between 2006 and 2009 to a high of 68% among 11- to 21-year-old females attending an urban academic health center or seven affiliated FQHCs in 2011 [58, 63]. One study in 2014 found that 41% of females and males receiving care in FQHC settings initiated the HPV vaccine. [62] Compared to Medicaid and safety net populations, FQHCs have the highest HPV vaccine initiation estimates with four studies showing initiation rates at 50% or higher [57,58,59]. Within safety net clinics, three studies examined HPV vaccine initiation: all three included only girls and were conducted in 2009 or earlier [63,64,65]. While most studies included adolescents as young as 9, 10, or 11 years, one study considered only adults ages 21 to 29 years in FQHCs between 2009 and 2013 and found initiation was approximately 4% [70].
Studies of HPV vaccine series completion among medically underserved adolescents show no discernable pattern over time, between types of medical services received, or by gender (Fig. 2) [55,56,57,58,59, 61, 63,64,65,66,67, 71]. It is clear that completion rates remain below 50%. The most recent study (conducted in 2017–2018) within an FQHC found that 46% of 9- to 26-year-olds completed the recommended doses [61]. Similar baseline completion rates were found among women in eight FQHC practices in 2011 (42%) and females in four safety net clinics in 2007–2009 (among those who initiated, 40% completed the vaccine series) [58, 64]. Very low completion rates were also found across time: 2% among females ages 10 to 26 years from 2006 to 2009, 2% among Medicaid enrolled females ages 11 to 18 years in June 2008, and 1% among 11- to 21-year-old boys attending an urban academic health center or seven affiliated FQHCs in 2011 [58, 63, 67].
Barriers and Facilitators to HPV Vaccination Among Medically Underserved Individuals and Those of Limited Financial Resources
Similar to the general population, physician recommendation, increased age, and receipt of other adolescent vaccines are common facilitators of HPV vaccination among medically underserved AYAs [56, 59,60,61, 65, 72, 73]. Within FQHC and Medicaid populations, the most commonly identified and strongly associated facilitator of HPV vaccination was physician discussion and recommendation of the vaccine [56, 59,60,61, 72]. For instance, in a study of Latina mothers with a daughter between the ages of 9 and 18 attending an FQHC, after adjusting for age, mother’s education, interview language, acculturation, and HPV vaccine knowledge, a physician recommendation was associated with a 493 times increased odds of HPV vaccine initiation [56]. Older age is also associated with an increased percentage of adolescents receiving the HPV vaccine [56, 59, 60, 65, 73]. However, adolescents who initiated the series at a younger rather than older age were more likely to complete the series [55, 74]. Finally, adolescents who received the other recommended vaccines for their age, especially the non-school entry required meningococcal conjugate vaccine, had higher rates of HPV vaccine receipt [58, 64].
Medically underserved adolescents are also eligible for programs providing access to affordable vaccines that can serve as facilitators of HPV vaccination. Two mechanisms provide access to vaccines for low-income adolescents: availability of the federal universal vaccine coverage program (VFC) and participation in certain health insurance plans. States can leverage the VFC program to offer vaccines recommended by the ACIP at no cost to individuals who are 18 years of age and younger universally or only those who are Medicaid-eligible, uninsured, underinsured, or American Indian or Alaskan Native [75, 76]. Underinsured individuals have to receive vaccines at FQHCs or rural health clinics to qualify for no cost vaccinations given by a VFC provider. HPV vaccination rates are higher among providers who participate in VFC and in states that expanded VFC eligibility to all children [77, 78].
Health insurance influences HPV vaccine initiation and completion within medically underserved individuals at several levels. First, compared to those who are uninsured, insured individuals, regardless of whether through Medicaid or private insurance, are more likely to initiate the HPV vaccine [55, 70]. Among insured 11- to 18-year-old males, compared to privately insured, those with Medicaid insurance were more likely to initiate the vaccine but less likely to complete the series [68, 79]. Finally, among adolescents with Medicaid insurance, participation in different plans influences rates of vaccine initiation and completion [27, 74].
Barriers to HPV vaccination among medically underserved populations are both similar and distinct from the general population. Like the general population, parents’ lack of awareness of the HPV vaccine, especially among parents of boys, can be a barrier to initiation for patients in safety net and FQHC populations [60, 65]. Practical barriers may be more important among medically underserved populations as some parents attending FQHCs worry about the cost of the vaccine and/or have competing demands of work or child care [56, 80]. Adolescent girls from households where the household income was less than 100% of the federal poverty level have been found to be less likely to complete the HPV vaccine series [55].
Interventions to Increase HPV Vaccination Among Medically Underserved Individuals and Those of Limited Financial Resources
Nine interventions have been conducted to increase HPV vaccination rates among medically underserved populations (Table 1) [57, 58, 62, 69, 73, 81,82,83,84]. Three interventions were conducted within each population of interest (i.e., FQHC, safety net, and Medicaid). Interventions have targeted parents (n = 4), providers (n = 2), parents and providers simultaneously (n = 2), and providers and clinics (n = 1). Interventions aimed to increase parents’ decision to vaccinate (n = 1), initiation (n = 3), receipt of dose two or three (n = 1), and initiation and completion (n = 4). Among the nine interventions, seven showed evidence of intervention effectiveness.
HPV Vaccination Among Individuals from Racial/Ethnic Minority Groups and/or Individuals Born Outside of the USA
HPV Vaccination Rates Among Racial/Ethnic Minority Groups and/or Individuals Born Outside of the USA
Compared to non-Hispanic Whites, racial/ethnic minority groups have demonstrated differences in HPV vaccination initiation versus completion. A systematic review indicated that Black and Hispanic adolescents were more likely to have initiated the HPV vaccine series compared to non-Hispanic White adolescents when studies were restricted to provider-verified vaccinations [25]. Despite higher vaccination initiation rates, rates of receiving subsequent doses remain significantly lower among Black and Hispanics, as compared to Whites, with disparities in vaccination completion greater among Blacks than Hispanics [25].
Unique Challenges, Barriers, and Facilitators for Racial/Ethnic Minority Groups and/or Individuals Born Outside of the USA
Several factors may influence vaccine initiation and completion rates among racial/ethnic minority groups such as differences across groups in foreign-born status, socioeconomic status, insurance coverage, healthcare access, and provider recommendation. Knowledge may also play a role in HPV vaccination among individuals from these racial/ethnic subgroups. Higher levels of knowledge about Pap testing, HPV infection, and vaccination among African American women have been associated with greater likelihood of HPV vaccination [85]. In a 2015 study, mothers of Latina, Chinese, Korean, and Black adolescent girls from low-income households, most of whom were foreign-born, had relatively low awareness of HPV and the HPV vaccine [86]. In the large, nationally representative 2013–2014 HINTS survey, non-Hispanic Black and Hispanic men and women were less likely to have heard of HPV and the HPV vaccine than non-Hispanic Whites [87]. In another study, compared to non-Hispanic White women, Black women demonstrated lower knowledge about HPV transmission and lower awareness of the HPV vaccine, but greater awareness of the link between HPV infection and cervical cancer compared to non-Hispanic White women [88]. Parents of non-Hispanic Black and Hispanic adolescents and racial/ethnic minority adolescents are significantly less likely to receive a recommendation for the HPV vaccine compared to parents of non-Hispanic White patients or non-Hispanic White patients [89, 90]. Although recommendation rates have improved among these racial/ethnic groups over time, the rate of increase in vaccine recommendation for Hispanic males ages 13–17 has remained low [91]. A systematic review conducted in 2020 identified three primary themes of barriers of vaccination among racial/ethnic minority groups when compared to non-Hispanic Whites [92]. Themes identified in articles published from July 2010 through July 2020 included differences in (1) provider recommendation and differences in patient/parent HPV/HPV vaccine knowledge and awareness, (2) mistrust in the healthcare system as well as HPV vaccine safety concerns, and (3) religious and cultural beliefs, especially among those born outside of the USA [92].
Foreign-born status may also influence disparities in HPV vaccination. In the 2011–2015 NHIS sample, 18–31-year-old foreign-born Asian and Latina women were less likely to initiate the HPV vaccine series compared to foreign-born White women, and foreign-born White, Black, Asian, and Latina women were also less likely to initiate the series than US-born White women [93]. Similarly, in 2013–2015 NHIS data of 18–35-year-old women, all foreign-born women were less likely to initiate vaccination compared with US-born women (14% vs. 30%, respectively) [94]. That same study found that foreign-born women with US citizenship status were more likely to initiate the HPV vaccine series compared to non-citizens [94]. Among young adults, vaccine initiation is often associated with having a usual source of care, OB/GYN provider, or previously receiving a Pap test, regardless of region of birth [94]. However, foreign-born women are often more likely to experience barriers related to health insurance coverage and access to care, which may account for some differences in vaccination initiation and completion among women in the AYA group [93, 94].
Trust in one’s provider and the healthcare system may also play an important role in HPV vaccination among racial/ethnic minorities. Black men and women (ages 18–73) who participated in focus groups to discuss their experiences with trustworthiness of healthcare providers reported that trust was largely based upon perceived lack of physicians’ interpersonal and technical competence [95]. Racism and experiences of discrimination were also cited as barriers to trust in physicians [95]. The authors of this qualitative study concluded that distrust is associated with decreased adherence to physician recommendations [95]. Indeed, Black men and women who report low levels of trust in healthcare providers are less willing to receive the HPV vaccine [96]. Compared to non-Hispanic White women, Black women report less trust in cancer-related information from media sources and charitable organizations but are more likely to trust cancer-related information from government health agencies, family members, religious organization and leaders, and television compared to non-Hispanic White women [88]. These findings provide insight into potential intervention strategies at the patient, provider, system, and community levels.
HPV Vaccine Interventions for Racial/Ethnic Minority Groups and/or Individuals Born Outside of the USA
There remains a need for culturally targeted interventions in preferred languages to increase vaccine acceptance, initiation, and completion among racially and ethnically diverse groups, including those who are born outside of the USA. Many prior interventions targeting these groups focus on increasing HPV knowledge among patients and/or parents. For instance, in a study conducted among Hispanic women and their daughters aged 11–17 from 2011 to 2013, individuals received either an HPV vaccine educational brochure coupled with a cervical cancer educational prevention program in their preferred language (English or Spanish) or the educational brochure in their preferred language only [97]. The educational program was delivered to both mothers and daughters by a community health educator and included components about HPV infection, vaccination, cervical cancer, screening, and reproductive health. Learning activities and tips for talking to daughters about sex were also included. In addition, participants were provided with a resource sheet containing information about referrals to local clinics, how to make an appointment to receive the vaccine, and vaccine cost and received follow-up phone calls [97]. Those in the intervention group were 2.24 times more likely to complete the vaccine series than the brochure-only group. Another intervention focused on the development of culturally and linguistically appropriate educational videos targeted to Latino and Korean-American parents of 11–17-year-olds [98]. The intervention was available in multiple languages and addressed the association between HPV infection and cervical cancer and important points about the HPV vaccine, with core elements across both parent groups, as well as elements targeted specifically for Korean and Latino parents. Individuals in the educational video intervention demonstrated significantly improved informed decision-making, increased knowledge, and decreased decisional conflict compared to those in the control condition. In addition, among Haitian mothers of adolescents, a brief motivational interviewing intervention resulted in significantly increased HPV-related knowledge but was not effective in improving initiation and completion rates [99].
Several interventions have demonstrated efficacy in increasing knowledge/awareness about HPV vaccination, specifically among females from racial/ethnic minority groups. An educational lecture series at colleges with predominantly Black students that aimed to improve knowledge about HPV vaccine, HPV infection, cervical cancer, and cancer screening significantly improved knowledge among Black female students and influenced intentions to receive the HPV vaccine [100]. During a study conducted among a group of Black and Hispanic women at high risk of cervical cancer, an educational video was presented during a visit to a colposcopy clinic with topics including HPV infection, prevalence, symptoms, HPV vaccine, cervical cancer screening, and cervical dysplasia. Knowledge was assessed pre- and post-video viewing and significantly increased, as did vaccine acceptability [101].
There are fewer multilevel interventions targeted toward racial/ethnic minority groups. However, one 2015–2016 multilevel intervention focused on improving vaccination among patients of an urban family medicine clinic which served primarily low-income and African American patients. The clinic incorporated consistent and positive HPV vaccine messaging targeted toward patients and focused on engaging community members, providers, and clinic staff [102]. Over time, this project significantly increased vaccine initiation (12.8 percentage point increase in males, 10.6 percentage point increase in females) and completion (16 percentage point increase in males, 10.9 percentage point increase in females) [102]. Significant increases in HPV vaccine completion rates were observed in young adult patients, but not adolescents [102].
HPV Vaccination Among Young Adults
HPV Vaccination Rates Among Young Adults
The period of young adulthood (aged 18–26) is often characterized by sexual exploration and autonomous decision-making [103]. The average age at which individuals in the USA report initiating sexual activity is age 18.1 among men and 17.8 among women [104]. Among sexually active adults, young women (ages 20–24) and young men (ages 25–29) [18, 19, 110,111,112] have the highest prevalence of HPV compared to other age groups [113]. Additionally, many young adults either enroll in college or begin military service, both of which impact healthcare access and related decision-making [114]. For instance, college students and military personnel are provided health insurance coverage and/or have access to designated health centers [115, 116]. In addition to increased access, the frequency of healthcare utilization often increases for young women in accordance with reproductive health guidelines [117]. For instance, the US Preventive Services Task Force recommends that women begin screening for cervical cancer starting at age 21 and continue to receive cervical cancer screenings at appropriate intervals through age 65 [118]. As individuals transition to young adulthood, they can potentially override their parents’ decisions to decline the HPV vaccine during adolescence [119]. As of 2018, 39.9% of adults aged 18–26 had initiated the HPV vaccine series, and only 21.5% had completed the recommended number of doses [20]. Overall, HPV vaccine initiation and completion rates in the USA are higher for young women ages 18–26 (53.6% and 35.3%, respectively) compared to young men ages 18–26 (27.0% and 9.0%, respectively) [20]. In addition, young adults who have previously been diagnosed with cancer are at risk for developing a second cancer (including an HPV-related cancer) and thus can greatly benefit from HPV vaccination [120]. However, prior studies have demonstrated low rates of initiation and completion among AYA cancer survivors [121]. In short, young adults are a priority population in efforts to promote the HPV vaccine due to high HPV prevalence, increased healthcare utilization (among women), low HPV vaccination rates, and self-directed healthcare decision-making.
Barriers, Facilitators, and Challenges to HPV Vaccination for Young Adults
Patient-level factors associated with HPV vaccination among young adults include HPV knowledge, attitudes, and beliefs about the HPV vaccine (e.g., perceived benefits, safety concerns, etc.), education level, health literacy, religious beliefs, relationship status, sexual activity, and perceptions of HPV risk [105, 115, 122,123,124,125]. Healthcare system-level factors influencing HPV vaccination primarily include access to healthcare (e.g., health insurance status, vaccine cost, etc.) and provider recommendation [89, 105,106,107, 115]. In fact, provider recommendation is the strongest predictor of HPV vaccination among young adults, regardless of gender, biological sex at birth, or sexual orientation [89, 106]. Unfortunately, low HPV knowledge among many healthcare providers, along with discomfort discussing sexual behavior, may prevent providers from recommending the vaccine [108]. Additionally, providers are less likely to recommend the HPV vaccine to young men compared to women [115].
Risk perception is an important patient-level factor associated with HPV vaccination among all young adults; however, reasons underlying perceptions of risk tend to vary for men and women. Young heterosexual women who are in committed relationships are less likely to be vaccinated compared to their counterparts who are single or dating, and this is largely attributed to perceptions of monogamy as protective against HPV infection [123]. Among sexually active individuals, the prevalence of any type of HPV infection is highest among men [103], yet, HPV knowledge and risk perception are low among young heterosexual men compared to women [115]. Barnard and colleagues found that many young adults did not view themselves at risk for HPV [115]. Given that contextual factors associated with HPV vaccination can vary among young adults, targeted interventions are necessary to increase HPV vaccination initiation and completion in this population.
Targeted HPV Vaccination Interventions for Young Adults
Very few interventions focused on HPV vaccine series initiation have exclusively targeted young adults or been rigorously tested in randomized controlled trials (RCTs), and only one of these studies included men [110, 111]. In a systematic review of HPV vaccine interventions conducted among college students, Barnard and colleagues found that uptake of at least one dose of the HPV vaccine ranged from 5% to 53%; but only one intervention significantly increased vaccine uptake compared to the control condition [111]. In addition to college-based interventions, a few studies have demonstrated efficacy in increasing HPV vaccine initiation and completion in clinic and community-based samples of young adults using patient reminders [110, 111].
Most interventions tested among young adults involved patient-level strategies (e.g., HPV education and/or patient reminders). In particular, individual HPV education provided through video appears to be efficacious at increasing HPV vaccine initiation and completion among young adult women [112, 126]. In an RCT, college women (aged 18–26) shown narrative HPV educational videos featuring both peers and medical experts were twice as likely to initiate the vaccine compared to those in the control group (OR = 2.07; 95% CI = 1.05, 4.10; p = 0.036), whereas the peer-only and medical expert-only videos did not improve vaccination rates [126]. In another RCT, young women (aged 18–26) recruited from community settings who had received the first dose of an HPV vaccine and who were prompted to watch a 13-minute HPV education video were more than twice as likely than control participants to complete the vaccine series (OR = 2.44; 95% CI = 1.47, 4.05; p = 0.001) [112]. Study participants were provided vaccinations at no cost, limiting external validity [112]. Importantly, both aforementioned interventions addressed patient education alone, which is not recommended by the Community Guide to Preventive Services [127]. Additionally, reminder letters sent directly to patients or their parents have demonstrated efficacy at improving HPV vaccine completion among females aged 9–26 who had already initiated the first dose (56.4% vs. 46.6%, p < 0.01), although the intervention effect was not as strong among young women aged 18–26 (43.5% vs. 37.0%, p < 0.01) compared to girls aged 9–17 (66.2 vs. 53.5%, p < 0.01) [128].
Very few HPV vaccination interventions involving young adults have been rigorously tested at the provider or systems level, and only one has shown efficacy at increasing HPV vaccine series initiation and completion [110, 111]. Ruffin and colleagues found that provider prompts generated through clinics’ electronic health record systems increased HPV vaccine series initiation and series completion among females aged 9–26 [129]. It is important to note that no provider or system-level interventions to date have focused exclusively on young adults, and only two included men (but only up to the age of 22) [110]. As system-level barriers related to access to healthcare may be mitigated by targeting young adults in college settings [115], interventions combining patient, provider, and system-level strategies in college health centers represent an emerging opportunity. Furthermore, Healthy Campus 2020 identified HPV vaccination as a health-related priority among college students [130]. Based on available research, college health centers could be enhanced to facilitate greater HPV vaccination series initiation and completion among young adults by incorporating digital patient education (e.g., videos) combined with health system-generated patient reminders and provider prompts [110,111,112, 126, 128, 129]. More research is necessary to identify intervention strategies that are most efficacious among young men, as well as to test the effectiveness of multilevel interventions specifically targeting young adult populations.
HPV Vaccination Among Sexual and Gender Minority Individuals
HPV Vaccination Rates Among Sexual and Gender Minority Individuals
As summarized from the Institute of Medicine report published in 2011 [131], researchers face three important challenges in attempting to gather valid and reliable data for describing sexual and gender minority groups in assessing their health: (1) operationally defining and measuring sexual orientation and gender identity, (2) overcoming the reluctance of some lesbian, gay, bisexual, or transgender (LGBT) individuals to identify themselves to researchers, and (3) obtaining representative samples of relatively small populations. Although there are scarce data that describe HPV vaccination rates across these vulnerable subgroups, it is well established that men who have sex with men (MSM) have a high risk for anal cancer [132], which is even greater if they are living with HIV [133]. Lesbian and bisexual women report a significant history of cervical abnormalities [135,136,137]; however, lesbian and bisexual women have also reported low perceived risk of HPV infection due to lack of male sexual partners [125]. Sexual minority women are less likely to receive regular Pap tests compared to heterosexual women [109, 138], placing them at risk for the development of cervical cancer. In some groups, such as the transgender community, empirical data assessing HPV-related cancer incidence and mortality are lacking primarily because of an absence of large-scale observational studies in this population [139].
Although HPV comorbidities and HPV-related cancers disparities are documented in a few sexual and gender minority groups, little research has addressed HPV vaccination among these populations. Available epidemiological studies indicate that HPV vaccine initiation and completion are low among sexual and gender minorities prior to and after the recommendation from the ACIP updated in late 2011 [140,141,142]. At that time, a routine recommendation was made for males at age 11 or 12, and catch-up vaccination through age 21 for all males, and through age 26 for MSM and for immunocompromised persons, including those with HIV infection [134, 142]. In 2015, recommendations for use of the nine-valent vaccine (9vHPV) were made for the same populations [143]. It is also important to note that US studies varied in their methodological approaches, some with relatively small sample sizes and variability in the year the studies were conducted (Table 2). Indeed, when interpreting the study findings, it is important to consider the temporality in which the study was conducted with regard to ACIP recommendations. Table 2 shows epidemiological studies conducted in the USA which explore HPV vaccination uptake among sexual and gender minorities. An online study of 1457 young MSM in the USA aged 18–26 reported that only 6.8% had received one or more vaccine doses [144]. During the same time period, The National HIV Behavioral Surveillance Study, a behavioral study implemented through a series of cross-sectional surveys [145], reported that for 18–26-year-old MSMs, the HPV vaccination initiation rate was 4.9% (2.7% initiation rate among MSMs 18 years and older overall) [146]. This rate increased to 17.2% among MSM aged 18–26 during the 2014 study [147]. A 2014 national sample of young adult (18–26-year-old) gay and bisexual men found that only 13% had initiated the HPV vaccine series [140]. Of those who initiated the series, more than half (56%) completed the three-dose series [140]. Conversely, a prospective study conducted from 1996 to 2014 using data from 10,663 males and females enrolled in the Growing Up Today Study reported that HPV vaccination initiation was especially low among heterosexual males, compared to bisexual or gay men [148].
In women identifying as sexual and gender minorities, similar lack of estimates for HPV vaccination initiation and completion is also observed in the literature, despite the documented burden for HPV-related comorbidities. Data from the 2006 to 2010 National Survey of Family Growth (NSFG), which used a stratified, three-stage cluster sampling strategy to establish a national probability sample, only 8.5% of lesbians and 33.2% of bisexual individuals who had heard of the HPV vaccine had initiated the HPV vaccine [149]. In 2013, data from the National Sample of Lesbian and Bisexual Women (n = 543) reported that 45% of respondents initiated the HPV vaccine series and 70% of initiators completed the series [150]. Although studies have included transgender women in their sample [151], specific information regarding vaccine uptake in this group is limited. It is also important to note that there are no HPV vaccine recommendations specifically targeting transgender individuals [152].
Barriers and Facilitators for HPV Vaccine Series Initiation and Completion Among Sexual and Gender Minority Individuals
Several studies have examined barriers to HPV vaccination among individuals from sexual minority groups using qualitative and quantitative methods [153,154,155] at the patient, provider, and system levels. Despite the lower rates of HPV initiation and completion, gay and bisexual men have indicated their willingness to receive the HPV vaccine, with estimates ranging from 36% to 74% [153, 154, 156, 157]. In a national sample of lesbian and bisexual women, 32% had completed the three dose series, and among those who had initiated, but not yet completed the series, 47% intended to complete the series [150]. At a patient level, modifiable factors such as low awareness of HPV infection, HPV-related cancers (other than cervical cancer), and HPV vaccine knowledge are consistent barriers to HPV vaccination in sexual and gender minorities [155]. Other individual-level barriers are cost, lower perceived risk of infection, and perceived benefits of the vaccine [154, 158] and, among transgender women, belief that HPV/HPV vaccination was not relevant to them [155]. At the provider and system levels, the lack of LGBT-trained providers (HPV vaccine knowledge/expertise) and identity-affirming and culturally appropriate healthcare setting deter HPV vaccination uptake among these individuals [155]. The latter barriers have also been identified in the literature across a variety of LGBT health issues, representing consistent, yet modifiable barriers to overall LGBT health [159]. Notably, studies among gender and sexual minorities have reported high rates of having a routine medical checkup in the past year (ranging from 40% to 80%) [140, 146, 160], suggesting missed opportunities for HPV vaccination among this population.
Overwhelmingly, recommendation by healthcare providers is one of the most important facilitators for HPV vaccine initiation and completion [134, 144, 150, 151, 155]. Among young adult MSM, disclosure of sexual behavior to their healthcare providers is a strong mediator of HPV uptake [161]. Although limited studies explore correlates of HPV vaccine acceptability and uptake among the LGBT community, findings from studies focused on MSM address the need for targeted educational and interventional efforts among providers and healthcare systems for culturally sensitive, affirming, and effective communication in this community [155]. Moreover, an online survey conducted in 2009 among gay/bisexual (n = 312) and heterosexual men (n = 296) found that men may be more accepting of HPV vaccine when it is framed as both preventing genital warts and an HPV-related cancer, regardless of which of the three most common HPV-related cancers in men was described (anal, oral, or penile cancers) [162]. Although only 42% of men were willing to receive the HPV vaccine when framed as preventing genital warts alone, 60% were willing to get it when it was framed as preventing cancer in addition to genital warts (p < 0.001) [162]. In the comparison performed between groups (gay/bisexual vs. heterosexual men), their findings suggest that men respond similarly to different ways of framing HPV-related disease regardless of sexual orientation (p = 0.35). However, gay and bisexual men were more willing to get the HPV vaccine than their heterosexual counterparts (p < 0.001) [162].
Interventions to Address Disparities in HPV Vaccine Initiation and Completion Among Sexual and Gender Minority Individuals
Among young adults, despite ACIP recommendations [134], many age-eligible individuals are not receiving the HPV vaccine, making efforts to increase vaccination important in this age group. The percentage of adults aged 18–26 who received the recommended number of doses of HPV vaccine increased from 13.8% in 2013 to 21.5% in 2018 [20], however these rates remain suboptimal. Most of the epidemiological and behavioral studies among sexual and gender minorities focus on HPV uptake target young adults (older than 18 years). This approach is expected as adolescents are engaged in an ongoing process of sexual development [163]; many adolescents may be unsure of their sexual orientation, while others have been clear about it since childhood [131]. Several interventions target HPV vaccine uptake among young adults at the individual, provider, and clinic levels; however, those interventions do not address clinic- or provider-level barriers for sexual and gender minorities [126, 128, 129, 164,165,166,167,168,169,170,171,172,173,174].
Of the interventions addressing HPV vaccine uptake for young adults, only one addresses sexual and gender minorities (Table 3) [135, 175, 176]. The Outsmart HPV intervention (ClinicalTrials.gov identifiers: NCT04032106 and NCT02835755) is a web-based intervention targeted to young gay and bisexual men was first pilot-tested to examine the acceptability for these individuals in influencing HPV vaccination knowledge, attitudes, and beliefs using the protection-motivation theory (PMT) as the theoretical framework [135, 175, 176]. The intervention, which includes vaccine reminders, aims at increasing HPV vaccine initiation and completion among young individuals who report having a history of same-sex partners, being sexually attracted to males, or identify as gay, bisexual, or queer (i.e., sexual minority males) [135, 175, 176]. The results of the pilot study showed that HPV vaccine initiation was higher among participants in the intervention group (45%) than those in the control group (26%; p = 0.02) [135]. HPV vaccination completion rates in the intervention group (11%) were higher than in the control group, although the difference was not statistically significant (3%; p = 0.07) [135]. Findings from the posttest survey show positive effects on several attitudes and beliefs such as greater perception that MSM are at higher risk for anal cancer relative to other men; greater HPV vaccination self-efficacy; and lower perceived harms of the HPV vaccine on posttest surveys in the intervention group compared to those in the control group (all ps < 0.05) [176].Overall, intervention participants reported high levels of acceptability and satisfaction with the Outsmart HPV intervention [176]. As of the writing of this chapter, the efficacy of the Outsmart HPV in increasing HPV vaccination rates is currently being tested in a larger trial [175].
Given the higher burden of HPV infection and disease, as well as the documented lack of evidence-based interventions, culturally appropriate interventions to promote HPV vaccine uptake among sexual and gender minorities are needed. Specifically, interventions designed to improve vaccine uptake should consider a multilevel approach, to address structural and social stigma, cultural competencies, and effective patient-provider communication to support physician recommendations [131]. Further, these findings underscore a missed prevention opportunity for these at-risk and underserved population and might also suggest, in parallel, the need for proactive strategies at a clinic, provider, or policy (e.g., school-entry requirement) level, to increase HPV vaccination uptake in young SGM, particularly prior the onset of sexual behavior.
HPV Vaccination in Novel Settings
As researchers and health professionals seek to increase HPV vaccination, interventions in novel settings for implementation of interventions will become important to reach sociocultural groups with lower rates of HPV vaccination rates. Promising novel settings to improve HPV vaccination rates in the USA include pharmacies, schools, and dental practices [178]. The use of immunization registry data is also important for increasing HPV vaccination rates.
Settings
Pharmacies
HPV vaccination provision in pharmacies has potential for considerable reach given the large number of pharmacies in the USA and their locations throughout rural and underserved areas [178]. Pharmacies are widely trusted by consumers, have longer hours, and can provide similar quality of care at comparable or lower cost than HCPs [178]. This model has been leveraged to deliver vaccines to a large segment of the population for seasonal influenza vaccination. As of 2019, in 47 states, pharmacies have the capability to vaccinate adolescents and adults against HPV within their scope of practice [179], enhancing the overall accessibility of HPV vaccinations. Restrictions exist in some states, however, including the need for a prescription (3 states) and age restrictions for adolescents (22 states) [179], which reduces the ability of age-eligible individuals to obtain the vaccine at their local pharmacy. In addition, other potential barriers exist. For instance, pharmacies may not be considered an “in-network” care provider, thereby placing the financial burden/out of pocket costs of vaccination on the patient/family [178]. Similarly, one study interviewing HPV vaccination stakeholders highlighted pharmacies as a potential strategy for improving vaccination rates, although noted that lack of insurance company reimbursement to pharmacies can be a barrier [40]. The authors of that study concluded that policy changes are needed surrounding HPV vaccination at the pharmacy level, including ensuring that all healthcare providers, including pharmacists, can administer the HPV vaccine and that pharmacies are included as providers in the VFC program [40]. In one national survey of adolescent boys and their parents on comfort with alternative settings for HPV vaccine delivery, half of parents and a third of their sons reported comfort with vaccination in pharmacy or school settings [180]. In another large, national sample, 29% of parents expressed willingness to get their child’s HPV vaccine at a pharmacy [181]. Pharmacists report positive perceptions of the HPV vaccination series but report barriers such as inadequate insurance coverage, low demand for the vaccine in pharmacies, and the subsequent expiration of vaccine before use in the pharmacy setting [182]. Studies examining effectiveness of pharmacy-based interventions for HPV vaccination are limited. In one program serving underinsured Hispanic college students, 89 (mostly female) students received the first HPV dose and 43 (48%) completed all three doses, demonstrating acceptability of pharmacy-based vaccine programs for this population [167]. Another “pharmacist-led” intervention in a clinic setting utilized an HPV vaccination strategy where the pharmacist led the education of clinic staff, stocking of HPV vaccine product, review of upcoming patients for HPV vaccine eligibility, and electronic medical record prompts for providers [183]. RCTs of pharmacy interventions compared with interventions in other traditional and novel settings are needed to demonstrate feasibility, acceptability, and efficacy.
Schools
Another promising setting for HPV vaccination is within schools with students ages 9–18. School health centers provide comprehensive medical care to students but exist in less than 10% of schools in the USA [178]. Despite this lower reach, school health centers may be more convenient for parents who have access to them, increasing the likelihood that all HPV doses will be completed. Compared with community health centers, adolescents who received HPV vaccination in school health centers were more likely to complete the series [184]. Barriers to vaccination in school health centers may include parent out-of-pocket costs, school health center costs to purchase vaccines, and obtaining parent consent. Schools hosting or promoting interventions implemented by others with dedicated staff are potential solutions, along with school distribution of HPV vaccine campaign materials and parent reminder letters about vaccine follow-up [185]. Large-scale, voluntary vaccination programs in school settings have been effective in other countries for increasing HPV vaccination (e.g., Canada, Australia) [186,187,188]. A similar program in the USA with smaller groups of schools has shown promise in rural and Appalachian Kentucky [47].
Dental Practices
Provision of HPV vaccination in dental practices may be a practical and sustainable alternative to provision in traditional settings due to the link between HPV and oral cancer. The substantial reach to adolescents who attend clinics for dental and orthodontia care may provide a large population eligible for vaccination [178]. However, feasibility of vaccination in dental practices may be lower than other novel settings given the training of dental staff [178]. Despite awareness of the link between HPV and oral cancer in the dental field, one systematic review highlighted the lack of communication about, and recommendation for, HPV vaccination by dental providers [189]. The lack of in-depth knowledge and health literacy surrounding HPV in dental providers may be a barrier to discussing the link between the virus and oral caners [190]. Dental opinion leaders reported possible facilitators of HPV vaccination in the dental setting including increasing HPV knowledge for dental providers and for parents and promoting HPV prevention as within the scope of dental care [191]. In one large, national sample of parents of adolescents, only 23% of parents indicated comfort with their teen receiving an HPV vaccination at a dentist [192]. HPV vaccination interventions in dental practices have potential for increasing vaccination rates, but both dental staff and parent comfort and knowledge must be addressed.
Using Immunization Registry and Immunization Information Systems Data
State immunization registries or immunization information systems (IIS) are computer-based systems that confidentially collect and summarize immunization data on a population level [193]. State IIS are tools that can facilitate HPV vaccination through tracking immunization doses and their timing, including series initiation, completion, up-to-date status, and missing/late doses. Registries may enable tracking HPV vaccination across multiple providers and settings (e.g., primary care providers, gynecological care, pharmacies) and enable identification of regions, health systems, or clinics with low initiation and completion rates [40]. In 2016, 49 states used IIS to track childhood immunizations [193]. IIS can potentially be integrated with electronic health records and can include decision support tools. Immunization registries are effective in increasing vaccination due to their ability to track immunizations, increase accountability for providers and practices, and support other vaccine interventions (e.g., patient and provider reminders) [194]. Currently, however, not all US providers are required to use IIS, and IIS have considerable costs in terms of necessary state-level funding, time, effort, and staff dedicated to upkeep [194, 195]. The continued use of IIS is vital for the acceleration of HPV vaccination in AYAs. The use of additional IIS capabilities has been used to improve HPV vaccination [196], including generation of patient/parent HPV vaccine reminders (via mail or phone), provider performance feedback on HPV vaccine rates, and provider reminder prompts via the electronic medical record about needed HPV doses [194].
Gaps and Future Directions
The potential for HPV vaccination to address cancer health disparities has not yet been fully realized. In general, uptake of HPV vaccination has fallen short of targets in national initiatives. Despite the potential to reduce the burden of HPV-related cancers, vaccine series initiation and completion by race/ethnicity, biological sex at birth, gender, socioeconomic status, geography, age, and sexual orientation remain suboptimal. Extensive research suggests the most effective interventions will be targeted approaches that consider multiple levels of influence, including the unique individual, interpersonal, systems, community, and policy-level factors that act as barriers and facilitators to HPV vaccine uptake. State immunization registries have the potential to identify disparities in individual states and might inform the development of targeted interventions for adolescents, parents, young adults, and providers. At the individual level, knowledge, beliefs, and attitudes can play a powerful role in understanding vaccine behaviors. As such, developing messaging and materials that are reflective of the sociocultural characteristics and language preferences of the target communities is essential. Education and messaging must consider the unique audiences involved in HPV vaccination decision-making. For instance, in the case of adolescents, parents often are the vaccine decision-makers; thus, HPV vaccination education materials must consider that parents will be a key part of the audience for this information. At the interpersonal level, communication and messaging from healthcare providers are vital. Given the well-established role of provider recommendation in HPV vaccine uptake, it is crucial that recommendation strategies are evidence-based and consider the unique context of local communities. At the systems level, leveraging well-established strategies such as reminder and recall systems can support individual and interpersonal interactions in the clinic setting. Additionally, reaching communities in settings where they are most comfortable and have established trust should also be considered in order to reduce barriers to access. Thus, at the policy level, school entry policies as well as consideration of the broader contexts or settings for vaccine delivery such as pharmacies or schools can help to remove barriers to access. Coverage for vaccination beyond age 18 through public financing mechanisms may also be an important strategy for unique populations that were not vaccinated during adolescence, such as AYA cancer survivors or LGBTQ communities.
References
Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40(3):187–93.
IARC. Human papillomaviruses. IARC. 2012;100:255–313.
Centers for Disease Control. Human Papillomavirus (HPV). 2019. https://www.cdc.gov/hpv/index.html
Cogliano V, Baan R, Grosse Y, Secretan B, Ghissassi F. Carcinogenicity of human papillomaviruses. Lancet Oncol. 2005;6(4):204.
National Cancer Institute. HPV and cancer. 2019. https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer
Senkomago V, Henley SJ, Thomas CC, Mix JM, Markowitz LE, Saraiya M. Human papillomavirus–attributable cancers—United States, 2012–2016. Morb Mortal Wkly Rep. 2019;68(33):724.
Van Dyne EA, Henley SJ, Saraiya M, Thomas CC, Markowitz LE, Benard VB. Trends in human papillomavirus–associated cancers—United States, 1999–2015. Morb Mortal Wkly Rep. 2018;67(33):918.
Zahnd WE, James AS, Jenkins WD, et al. Rural–urban differences in cancer incidence and trends in the United States. Cancer Epidemiol Biomarkers Prev. 2018;27(11):1265–74.
Sudenga SL, Nyitray AG, Torres BN, et al. Comparison of anal HPV natural history among men by country of residence: Brazil, Mexico, and the United States. J Infect. 2017;75(1):35–47.
Markowitz LE, Gee J, Chesson H, Stokley S. Ten years of human papillomavirus vaccination in the United States. Acad Pediatr. 2018;18(2):S3–S10.
U.S. Food & Drug Adminstration. Approval letter – ceravix. 2009.
U.S. Food & Drug Administration. Approval letter – human papillomavirus quadrivalent (Types 6, 11, 16, 18) vaccine, recombinant. 2006.
U.S. Food & Drug Administration. Approval letter – gardasil. 2009.
U.S. Food & Drug Administration. Approval letter – GARDASIL 9. 2014.
Services Dohah. Supplement approval for human papillomavirus 9-valent vaccine, recombinant. 2015.
U.S. Food & Drug Administration. Supplement approval, human papillomavirus 9-valent, recombinant, Ages 27–45. 2018.
Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human papillomavirus vaccination for adults: updated recommendations of the Advisory Committee on Immunization Practices. Am J Transplant. 2019;19(11):3202–6.
Meites E. Human papillomavirus vaccination for adults: updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2019;68:698–702.
Meites E. Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2016;65
Boersma P, Black LI. Human papillomavirus vaccination among adults aged 18–26, 2013–2018. NCHS Data Brief. 2020;(354):1–8.
Walker TY, Elam-Evans LD, Yankey D, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2018. Morb Mortal Wkly Rep. 2019;68(33):718.
Centers for Disease Control. TeenVaxView | 2018 adolescent HPV vaccination coverage report. Atlanta: CDC; 2019.
HPV Roundtable. School entry requirements for HPV vaccine. 2019.
Skinner EG, Alise. HPV vaccine: State Legislation and Regulation. 2020. https://www.ncsl.org/research/health/hpv-vaccine-state-legislation-and-statutes.aspx
Spencer JC, Calo WA, Brewer NT. Disparities and reverse disparities in HPV vaccination: a systematic review and meta-analysis. Prev Med. 2019;123:197–203.
Reiter PL, Cates JR, McRee A-L, et al. Statewide HPV vaccine initiation among adolescent females in North Carolina. Sex Transm Dis. 2010;37(9):549.
Staras SA, Vadaparampil ST, Haderxhanaj LT, Shenkman EA. Disparities in human papillomavirus vaccine series initiation among adolescent girls enrolled in Florida Medicaid programs, 2006–2008. J Adolesc Health. 2010;47(4):381–8.
Curtis CR, Dorell C, Yankey D, et al. National human papillomavirus vaccination coverage among adolescents aged 13–17 years—National Immunization Survey–Teen, United States, 2011. MMWR Surveill Summ. 2014;63(Suppl 2):61–70.
Henry KA, Stroup AM, Warner EL, Kepka D. Geographic factors and human papillomavirus (HPV) vaccination initiation among adolescent girls in the United States. Cancer Epidemiol Prev Biomarkers. 2016;25(2):309–17.
Vielot NA, Butler AM, Brookhart MA, Becker-Dreps S, Smith JS. Patterns of use of human papillomavirus and other adolescent vaccines in the United States. J Adolesc Health. 2017;61(3):281–7.
Henry KA, Swiecki-Sikora AL, Stroup AM, Warner EL, Kepka D. Area-based socioeconomic factors and human papillomavirus (HPV) vaccination among teen boys in the United States. BMC Public Health. 2018;18(1):19.
Williams CL, Walker TY, Elam-Evans LD, et al. Factors associated with not receiving HPV vaccine among adolescents by metropolitan statistical area status, United States, National Immunization Survey–Teen, 2016–2017. Hum Vaccin Immunother. 2020;16(3):562–72.
Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–20.
Luque J, Raychowdhury S, Weaver M. Health care provider challenges for reaching Hispanic immigrants with HPV vaccination in rural Georgia. Rural Remote Health. 2012;12(2):1975.
Allison MA, Dunne EF, Markowitz LE, et al. HPV vaccination of boys in primary care practices. Acad Pediatr. 2013;13(5):466–74.
Boyd ED, Phillips JM, Schoenberger Y-MM, Simpson T. Barriers and facilitators to HPV vaccination among rural Alabama adolescents and their caregivers. Vaccine. 2018;36(28):4126–33.
Moss JL, Gilkey MB, Rimer BK, Brewer NT. Disparities in collaborative patient-provider communication about human papillomavirus (HPV) vaccination. Hum Vaccin Immunother. 2016;12(6):1476–83.
Buchwald D, Muller C, Bell M, Schmidt-Grimminger D. Attitudes toward HPV vaccination among rural American Indian women and urban white women in the northern plains. Health Educ Behav. 2013;40(6):704–11.
Reiter PL, Brewer NT, Gottlieb SL, McRee A-L, Smith JS. Parents’ health beliefs and HPV vaccination of their adolescent daughters. Soc Sci Med. 2009;69(3):475–80.
Cartmell KB, Young-Pierce J, McGue S, et al. Barriers, facilitators, and potential strategies for increasing HPV vaccination: a statewide assessment to inform action. Papillomavirus Res. 2018;5:21–31.
Kepka DL, Ulrich AK, Coronado GD. Low knowledge of the three-dose HPV vaccine series among mothers of rural Hispanic adolescents. J Health Care Poor Underserved. 2012;23(2):626–35.
Mohammed KA, Subramaniam DS, Geneus CJ, et al. Rural-urban differences in human papillomavirus knowledge and awareness among US adults. Prev Med. 2018;109:39–43.
Tiggelaar SM, Rafalski M, Davidson MA, Hu Y, Burnett L. HPV knowledge and vaccine acceptability in Appalachian Tennessee and Kentucky, USA. J Fam Plann Reprod Health Care. 2014;40(1):75–6.
Vanderpool RC, Dressler EVM, Stradtman LR, Crosby RA. Fatalistic beliefs and completion of the HPV vaccination series among a sample of young Appalachian Kentucky women. J Rural Health. 2015;31(2):199–205.
Vanderpool RC, Huang B, Deng Y, et al. Cancer-related beliefs and perceptions in Appalachia: findings from 3 states. J Rural Health. 2019;35(2):176–88.
Thomas TL, Caldera M, Maurer J. A short report: parents HPV vaccine knowledge in rural South Florida. Hum Vaccin Immunother. 2019;15(7–8):1666–71.
Vanderpool RC, Breheny PJ, Tiller PA, et al. Implementation and evaluation of a school-based human papillomavirus vaccination program in rural Kentucky. Am J Prev Med. 2015;49(2):317–23.
Vanderpool RC, Casey BR, Crosby RA. HPV-related risk perceptions and HPV vaccine uptake among a sample of young rural women. J Community Health. 2011;36(6):903.
Crosby RA, Casey BR, Vanderpool R, Collins T, Moore GR. Uptake of free HPV vaccination among young women: a comparison of rural versus urban rates. J Rural Health. 2011;27(4):380–4.
Cates JR, Shafer A, Diehl SJ, Deal AM. Evaluating a county-sponsored social marketing campaign to increase mothers’ initiation of HPV vaccine for their preteen daughters in a primarily rural area. Soc Mark Q. 2011;17(1):4–26.
Chung RJ, Walter EB, Kemper AR, Dayton A. Keen on teen vaccines: improvement of adolescent vaccine coverage in rural North Carolina. J Adolesc Health. 2015;56(5):S14–6.
Paskett ED, Krok-Schoen JL, Pennell ML, et al. Results of a multilevel intervention trial to increase human papillomavirus (HPV) vaccine uptake among adolescent girls. Cancer Epidemiol Biomarkers Prev. 2016;25(4):593–602.
Katz ML, Paskett ED. The process of engaging members from two underserved populations in the development of interventions to promote the uptake of the HPV vaccine. Health Promot Pract. 2015;16(3):443–53.
Health Resources and Services Administration. What is shortage designation? 2021. https://bhw.hrsa.gov/workforce-shortage-areas/shortage-designation
Cowburn S, Carlson M, Lapidus J, Heintzman J, Bailey S, DeVoe J. Insurance continuity and human papillomavirus vaccine uptake in Oregon and California federally qualified health centers. Am J Public Health. 2014;104(9):e71–9.
Gerend MA, Zapata C, Reyes E. Predictors of human papillomavirus vaccination among daughters of low-income Latina mothers: the role of acculturation. J Adolesc Health. 2013;53(5):623–9.
Moss JL, Reiter PL, Dayton A, Brewer NT. Increasing adolescent immunization by webinar: a brief provider intervention at federally qualified health centers. Vaccine. 2012;30(33):4960–3.
Perkins RB, Zisblatt L, Legler A, Trucks E, Hanchate A, Gorin SS. Effectiveness of a provider-focused intervention to improve HPV vaccination rates in boys and girls. Vaccine. 2015;33(9):1223–9.
Flores YN, Salmeron J, Glenn BA, Lang CM, Chang LC, Bastani R. Clinician offering is a key factor associated with HPV vaccine uptake among Mexican mothers in the USA and Mexico: a cross-sectional study. Int J Public Health. 2019;64(3):323–32.
Colon-Lopez V, Toro-Mejias LM, Conde-Toro A, et al. Views on HPV and HPV vaccination: the experience at a Federal Qualified Clinic in Puerto Rico. J Health Care Poor Underserved. 2016;27(3):1411–26.
VanderVeen N, Wieneke A, Tran S, Kim A, Davis K, Taubel D. Perceived barriers and trends in HPV vaccination via patient survey responses at Kalamazoo, Michigan’s federally-qualified health center. J Community Health. 2020;45(1):48–54.
Fisher-Borne M, Preiss AJ, Black M, Roberts K, Saslow D. Early outcomes of a multilevel human papillomavirus vaccination pilot intervention in federally qualified health centers. Acad Pediatr. 2018;18(2S):S79–84.
Sandri KJ, Verdenius I, Bartley MJ, et al. Urban and rural safety net health care system clinics: no disparity in HPV4 vaccine completion rates. PLoS One. 2014;9(5):e96277.
Tiro JA, Pruitt SL, Bruce CM, et al. Multilevel correlates for human papillomavirus vaccination of adolescent girls attending safety net clinics. Vaccine. 2012;30(13):2368–75.
Bastani R, Glenn BA, Tsui J, et al. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiol Biomark Prev. 2011;20(7):1463–72.
Perkins RB, Brogly SB, Adams WG, Freund KM. Correlates of human papillomavirus vaccination rates in low-income, minority adolescents: a multicenter study. J Women’s Health (2002). 2012;21(8):813–20.
Cook RL, Zhang J, Mullins J, et al. Factors associated with initiation and completion of human papillomavirus vaccine series among young women enrolled in Medicaid. J Adolesc Health. 2010;47(6):596–9.
Agawu A, Buttenheim AM, Taylor L, Song L, Fiks AG, Feemster KA. Sociodemographic differences in human papillomavirus vaccine initiation by adolescent males. J Adolesc Health. 2015;57(5):506–14.
Staras SA, Vadaparampil ST, Livingston MD, Thompson LA, Sanders AH, Shenkman EA. Increasing human papillomavirus vaccine initiation among publicly insured Florida adolescents. J Adolesc Health. 2015;56(5 Suppl):S40–6.
Heintzman J, Hatch B, Coronado G, et al. Role of race/ethnicity, language, and insurance in use of cervical cancer prevention services among low-income Hispanic women, 2009–2013. Prev Chronic Dis. 2018;15:E25.
Ng J, Ye F, Roth L, et al. Human papillomavirus vaccination coverage among female adolescents in managed care plans – United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(42):1185–9.
Staras SA, Vadaparampil ST, Patel RP, Shenkman EA. Parent perceptions important for HPV vaccine initiation among low income adolescent girls. Vaccine. 2014;32(46):6163–9.
Tiro JA, Sanders JM, Pruitt SL, et al. Promoting HPV vaccination in safety-net clinics: a randomized trial. Pediatrics. 2015;136(5):850–9.
Inguva S, Barnard M, Ward LM, et al. Factors influencing human papillomavirus (HPV) vaccination series completion in Mississippi Medicaid. Vaccine. 2020;38(8):2051–7.
Centers for Disease Control and Prevention. VFC detailed questions and answers for parents. CDC. 2014 [updated Dec 17, 2014].
Centers for Disease Control and Prevention. VFC Childhood Vaccine Supply Policy 2009. CDC 2009.
Malo TL, Staras SA, Bynum SA, Giuliano AR, Shenkman EA, Vadaparampil ST. Human papillomavirus vaccine administration among Medicaid providers who consistently recommended vaccination. Sex Transm Dis. 2014;41(1):24–8.
Gowda C, Dempsey AF. Medicaid reimbursement and the uptake of adolescent vaccines. Vaccine. 2012;30(9):1682–9.
Agawu A, Hanlon AL, Buttenheim AM, Song L, Fiks AG, Feemster KA. Disparities in human papillomavirus vaccine series completion by adolescent males: a retrospective cohort study. Acad Pediatr. 2020;20(3):364–73.
Mills LA, Head KJ, Vanderpool RC. HPV vaccination among young adult women: a perspective from Appalachian Kentucky. Prev Chronic Dis. 2013;10:E17.
Baldwin AS, Denman DC, Sala M, et al. Translating self-persuasion into an adolescent HPV vaccine promotion intervention for parents attending safety-net clinics. Patient Educ Couns. 2017;100(4):736–41.
Rand CM, Brill H, Albertin C, et al. Effectiveness of centralized text message reminders on human papillomavirus immunization coverage for publicly insured adolescents. J Adolesc Health. 2015;56(5 Suppl):S17–20.
Richman AR, Torres E, Wu Q, et al. Text and email messaging for increasing human papillomavirus vaccine completion among uninsured or Medicaid-insured adolescents in rural eastern North Carolina. J Health Care Poor Underserved. 2019;30(4):1499–517.
Sanderson M, Canedo JR, Khabele D, et al. Pragmatic trial of an intervention to increase human papillomavirus vaccination in safety-net clinics. BMC Public Health. 2017;17(1):158.
Bynum SA, Brandt HM, Sharpe PA, Williams MS, Kerr JC. Working to close the gap: identifying predictors of HPV vaccine uptake among young African American women. J Health Care Poor Underserved. 2011;22(2):549–61.
Glenn BA, Tsui J, Singhal R, et al. Factors associated with HPV awareness among mothers of low-income ethnic minority adolescent girls in Los Angeles. Vaccine. 2015;33(2):289–93.
Adjei Boakye E, Tobo BB, Rojek RP, Mohammed KA, Geneus CJ, Osazuwa-Peters N. Approaching a decade since HPV vaccine licensure: racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Hum Vaccin Immunother. 2017;13(11):2713–22.
Ojeaga A, Alema-Mensah E, Rivers D, Azonobi I, Rivers B. Racial disparities in HPV-related knowledge, attitudes, and beliefs among African American and white women in the USA. J Cancer Educ. 2019;34(1):66–72.
Gilkey MB, McRee A-L. Provider communication about HPV vaccination: a systematic review. Hum Vaccin Immunother. 2016;12(6):1454–68.
Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US National Immunization Survey. Am J Public Health. 2013;103(1):164–9.
Burdette AM, Webb NS, Hill TD, Jokinen-Gordon H. Race-specific trends in HPV vaccinations and provider recommendations: persistent disparities or social progress? Public Health. 2017;142:167–76.
Amboree TL, Darkoh C. Barriers to human papillomavirus vaccine uptake among racial/ethnic minorities: a systematic review. J Racial Ethn Health Disparities. 2020;8:1–16.
Agénor M, Abboud S, Delgadillo JG, Pérez AE, Peitzmeier SM, Borrero S. Intersectional nativity and racial/ethnic disparities in human papillomavirus vaccination initiation among US women: a national population-based study. Cancer Causes Control. 2018;29(10):927–36.
Cofie LE, Hirth JM, Guo F, Berenson AB, Markides K, Wong R. HPV vaccination among foreign-born women: examining the National Health Interview Survey 2013–2015. Am J Prev Med. 2018;54(1):20–7.
Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, Warnecke RB. Understanding African Americans’ views of the trustworthiness of physicians. J Gen Intern Med. 2006;21(6):642.
Otanez S, Torr BM. Ethnic and racial disparities in HPV vaccination attitudes. J Immigr Minor Health. 2018;20(6):1476–82.
Parra-Medina D, Morales-Campos DY, Mojica C, Ramirez AG. Promotora outreach, education and navigation support for HPV vaccination to Hispanic women with unvaccinated daughters. J Cancer Educ. 2015;30(2):353–9.
Valdez A, Stewart SL, Tanjasari SP, Levy V, Garza A. Design and efficacy of a multilingual, multicultural HPV vaccine education intervention. J Commun Healthc. 2015;8(2):106–18.
Joseph NP, Bernstein J, Pelton S, et al. Brief client-centered motivational and behavioral intervention to promote HPV vaccination in a hard-to-reach population: a pilot randomized controlled trial. Clin Pediatr. 2016;55(9):851–9.
Staples JN, Wong MS, Rimel B. An educational intervention to improve human papilloma virus (HPV) and cervical cancer knowledge among African American college students. Gynecol Oncol. 2018;149(1):101–5.
Mora AS, Madrigal JM, Jordan L, Patel A. Effectiveness of an educational intervention to increase human papillomavirus knowledge in high-risk minority women. J Low Genit Tract Dis. 2018;22(4):288–94.
McGaffey A, Lombardo NP, Lamberton N, et al. A “sense”-ational HPV vaccination quality improvement project in a family medicine residency practice. J Natl Med Assoc. 2019;111(6):588–99.
Mulye TP, Park MJ, Nelson CD, Adams SH, Irwin CE Jr, Brindis CD. Trends in adolescent and young adult health in the United States. J Adolesc Health. 2009;45(1):8–24.
Finer LB, Philbin JM. Trends in ages at key reproductive transitions in the United States, 1951–2010. Womens Health Issues. 2014;24(3):e271–9.
Newman PA, Logie CH, Doukas N, Asakura K. HPV vaccine acceptability among men: a systematic review and meta-analysis. Sex Transm Infect. 2013;89(7):568–74.
Rosenthal S, Weiss TW, Zimet GD, Ma L, Good M, Vichnin M. Predictors of HPV vaccine uptake among women aged 19–26: importance of a physician’s recommendation. Vaccine. 2011;29(5):890–5.
Laz TH, Rahman M, Berenson AB. Human papillomavirus vaccine uptake among 18-to 26-year-old women in the United States: National Health Interview Survey, 2010. Cancer. 2013;119(7):1386–92.
Leung SOA, Akinwunmi B, Elias KM, Feldman S. Educating healthcare providers to increase human papillomavirus (HPV) vaccination rates: a qualitative systematic review. Vaccine: X. 2019;3:100037.
Agénor M, Krieger N, Austin SB, Haneuse S, Gottlieb BR. Sexual orientation disparities in Papanicolaou test use among US women: the role of sexual and reproductive health services. Am J Public Health. 2014;104(2):e68–73.
Smulian EA, Mitchell KR, Stokley S. Interventions to increase HPV vaccination coverage: a systematic review. Hum Vaccin Immunother. 2016;12(6):1566–88.
Barnard M, Cole AC, Ward L, Gravlee E, Cole ML, Compretta C. Interventions to increase uptake of the human papillomavirus vaccine in unvaccinated college students: a systematic literature review. Prev Med Rep. 2019;14:100884.
Vanderpool RC, Cohen EL, Crosby RA, et al. “1-2-3 Pap” intervention improves HPV vaccine series completion among Appalachian women. J Commun. 2013;63(1):95–115.
Lewis RM, Markowitz LE, Gargano JW, Steinau M, Unger ER. Prevalence of genital human papillomavirus among sexually experienced males and females aged 14–59 years, United States, 2013–2014. J Infect Dis. 2018;217(6):869–77.
Park MJ, Mulye TP, Adams SH, Brindis CD, Irwin CE Jr. The health status of young adults in the United States. J Adolesc Health. 2006;39(3):305–17.
Barnard M, George P, Perryman ML, Wolff LA. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: implications from the Precaution Adoption Process Model. PLoS One. 2017;12(8):e0182266.
Hoerster KD, Lehavot K, Simpson T, McFall M, Reiber G, Nelson KM. Health and health behavior differences: US military, veteran, and civilian men. Am J Prev Med. 2012;43(5):483–9.
Martinez G. Use of family planning and related medical services among women aged 15–44 in the United States: National Survey of Family Growth, 2006–2010. Washington, DC: US Department of Health and Human Services, Centers for Disease Control and …; 2013.
Curry SJ, Krist AH, Owens DK, et al. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018;320(7):674–86.
Hopfer S, Clippard JR. College women’s HPV vaccine decision narratives. Qual Health Res. 2011;21(2):262–77.
Klosky JL, Hudson MM, Chen Y, et al. Human papillomavirus vaccination rates in young cancer survivors. J Clin Oncol. 2017;35(31):3582.
Castellino SM, Allen KE, Pleasant K, Keyes G, Poehling KA, Tooze JA. Suboptimal uptake of human papillomavirus (HPV) vaccine in survivors of childhood and adolescent and young adult (AYA) cancer. J Cancer Surviv. 2019;13(5):730–8.
Preston SM, Darrow WW. Are men being left behind (or catching up)? Differences in HPV awareness, knowledge, and attitudes between diverse college men and women. Am J Mens Health. 2019;13(6):1557988319883776.
Thompson EL, Vamos CA, Piepenbrink R, et al. Human papillomavirus risk perceptions and relationship status: a barrier to HPV vaccination? J Behav Med. 2019;42(5):991–7.
Best AL, Thompson EL, Adamu AM, et al. Examining the influence of religious and spiritual beliefs on HPV vaccine uptake among college women. J Relig Health. 2019;58(6):2196–207.
Agénor M, Jahn JL, Kay E, et al. Human papillomavirus risk perceptions among young adult sexual minority cisgender women and nonbinary individuals assigned female at birth. Perspect Sex Reprod Health. 2019;51(1):27–34.
Hopfer S. Effects of a narrative HPV vaccination intervention aimed at reaching college women: a randomized controlled trial. Prev Sci. 2012;13(2):173–82.
The Community Guide. Vaccination programs: community-based interventions implemented in combination. 2015.
Chao C, Preciado M, Slezak J, Xu L. A randomized intervention of reminder letter for human papillomavirus vaccine series completion. J Adolesc Health. 2015;56(1):85–90.
Ruffin MT, Plegue MA, Rockwell PG, Young AP, Patel DA, Yeazel MW. Impact of an electronic health record (EHR) reminder on human papillomavirus (HPV) vaccine initiation and timely completion. J Am Board Fam Med. 2015;28(3):324–33.
American College Health Association. Healthy Campus. Student objectives. 2020. https://www.acha.org/HealthyCampus/HealthyCampus/Student_Objectives.aspx
IOM (Institute of Medicine). 2011. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: The National Academies Press.
Palefsky J. Human papillomavirus and anal neoplasia. Curr HIV/AIDS Rep. 2008;5(2):78.
Colón-López V, Shiels MS, Machin M, et al. Anal cancer risk among people with HIV infection in the United States. J Clin Oncol. 2018;36(1):68.
Gerend MA, Madkins K, Gregory Phillips I, Mustanski B. Predictors of human papillomavirus vaccination among young men who have sex with men. Sex Transm Dis. 2016;43(3):185.
Reiter PL, Katz ML, Bauermeister JA, Shoben AB, Paskett ED, McRee A-L. Increasing human papillomavirus vaccination among young gay and bisexual men: a randomized pilot trial of the outsmart HPV intervention. LGBT Health. 2018;5(5):325–9.
Eaton L, Kalichman S, Cain D, et al. Perceived prevalence and risks for human papillomavirus (HPV) infection among women who have sex with women. J Women’s Health. 2008;17(1):75–84.
Chido-Amajuoyi OG, Shete S, Talluri R. Prevalence of abnormal cervical cancer screening outcomes among women in the United States: results from the National Health Interview Survey, 2018. Am J Obstet Gynecol. 2020;223(6):938–41.
Grasso C, Goldhammer H, Brown RJ, Furness B. Using sexual orientation and gender identity data in electronic health records to assess for disparities in preventive health screening services. Int J Med Inform. 2020;142:104245.
Braun H, Nash R, Tangpricha V, Brockman J, Ward K, Goodman M. Cancer in transgender people: evidence and methodological considerations. Epidemiol Rev. 2017;39(1):93–107.
Reiter PL, McRee A-L, Katz ML, Paskett ED. Human papillomavirus vaccination among young adult gay and bisexual men in the United States. Am J Public Health. 2015;105(1):96–102.
Polek C, Hardie T. Changing HPV vaccination rates in bisexual and lesbian women. J Am Assoc Nurse Pract. 2017;29(6):333–9.
Control CfD, Prevention. Recommendations on the use of quadrivalent human papillomavirus vaccine in males – advisory committee on immunization practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60(50):1705–8.
Petrosky E, Bocchini JA Jr, Hariri S, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2015;64(11):300.
Cummings T, Kasting ML, Rosenberger JG, Rosenthal SL, Zimet GD, Stupiansky NW. Catching up or missing out? Human papillomavirus vaccine acceptability among 18-to 26-year-old men who have sex with men in a US national sample. Sex Transm Dis. 2015;42(11):601–6.
Centers for Disease Control. National HIV Behavioral Surveillance (NHBS) | Surveillance Systems | Statistics Center | HIV/AIDS | CDC. 2020.
Meites E, Markowitz LE, Paz-Bailey G, Oster AM, Group NS. HPV vaccine coverage among men who have sex with men – National HIV Behavioral Surveillance System, United States, 2011. Vaccine. 2014;32(48):6356–9.
Oliver SE, Hoots BE, Paz-Bailey G, Markowitz LE, Meites E, Group NS. Increasing human papillomavirus vaccine coverage among men who have sex with men—National HIV Behavioral Surveillance, United States, 2014. J Acquir Immune Defic Syndr (1999). 2017;75(Suppl 3):S370.
Charlton BM, Reisner SL, Agénor M, Gordon AR, Sarda V, Austin SB. Sexual orientation disparities in human papillomavirus vaccination in a longitudinal cohort of US males and females. LGBT Health. 2017;4(3):202–9.
Agénor M, Peitzmeier S, Gordon AR, Haneuse S, Potter JE, Austin SB. Sexual orientation identity disparities in awareness and initiation of the human papillomavirus vaccine among US women and girls: a national survey. Ann Intern Med. 2015;163(2):99–106.
McRee A-L, Katz ML, Paskett ED, Reiter PL. HPV vaccination among lesbian and bisexual women: findings from a national survey of young adults. Vaccine. 2014;32(37):4736–42.
Gorbach PM, Cook R, Gratzer B, et al. Human papillomavirus vaccination among young men who have sex with men and transgender women in 2 US cities, 2012–2014. Sex Transm Dis. 2017;44(7):436.
Brown B, Poteat T, Marg L, Galea JT. Human papillomavirus-related cancer surveillance, prevention, and screening among transgender men and women: neglected populations at high risk. LGBT Health. 2017;4(5):315–9.
Gutierrez B Jr, Leung A, Jones KT, et al. Acceptability of the human papillomavirus vaccine among urban adolescent males. Am J Mens Health. 2013;7(1):27–36.
Wheldon CW, Daley EM, Buhi ER, Nyitray AG, Giuliano AR. Health beliefs and attitudes associated with HPV vaccine intention among young gay and bisexual men in the southeastern United States. Vaccine. 2011;29(45):8060–5.
Apaydin KZ, Fontenot HB, Shtasel D, et al. Facilitators of and barriers to HPV vaccination among sexual and gender minority patients at a Boston community health center. Vaccine. 2018;36(26):3868–75.
Reiter PL, Brewer NT, McRee A-L, Gilbert P, Smith JS. Acceptability of HPV vaccine among a national sample of gay and bisexual men. Sex Transm Dis. 2010;37(3):197.
Gilbert P, Brewer NT, Reiter PL, Ng TW, Smith JS. HPV vaccine acceptability in heterosexual, gay, and bisexual men. Am J Mens Health. 2011;5(4):297–305.
Daley EM, Vamos CA, Zimet GD, Rosberger Z, Thompson EL, Merrell L. The feminization of HPV: reversing gender biases in US human papillomavirus vaccine policy. Am J Public Health. 2016;106(6):983.
Smalley KB, Warren JC, Barefoot KN. LGBT health: meeting the needs of gender and sexual minorities. Cham: Springer; 2017.
Meites E, Krishna NK, Markowitz LE, Oster AM. Health care use and opportunities for human papillomavirus vaccination among young men who have sex with men. Sex Transm Dis. 2013;40(2):154.
Stupiansky NW, Liau A, Rosenberger J, et al. Young men’s disclosure of same sex behaviors to healthcare providers and the impact on health: results from a US national sample of young men who have sex with men. AIDS Patient Care STDs. 2017;31(8):342–7.
McRee A-L, Reiter PL, Chantala K, Brewer NT. Does framing human papillomavirus vaccine as preventing cancer in men increase vaccine acceptability? Cancer Epidemiol Prev Biomarkers. 2010;19(8):1937–44.
Rosario M, Schrimshaw EW, Hunter J. Predicting different patterns of sexual identity development over time among lesbian, gay, and bisexual youths: a cluster analytic approach. Am J Community Psychol. 2008;42(3–4):266–82.
Preston SM, Darrow WW. Improving human papillomavirus-related knowledge and attitudes among ethnically diverse young adults. Health Equity. 2019;3(1):254–63.
Juraskova I, Bari RA, O’Brien MT, McCaffery KJ. HPV vaccine promotion: does referring to both cervical cancer and genital warts affect intended and actual vaccination behavior? Womens Health Issues. 2011;21(1):71–9.
Moore GR, Crosby RA, Young A, Charnigo R. Low rates of free human papillomavirus vaccine uptake among young women. Sex Health. 2010;7(3):287–90.
Navarrete JP, Padilla ME, Castro LP, Rivera JO. Development of a community pharmacy human papillomavirus vaccine program for underinsured university students along the United States/Mexico border. J Am Pharm Assoc. 2014;54(6):642–7.
Pahud B, Clark S, Herigon JC, et al. A pilot program to improve vaccination status for hospitalized children. Hosp Pediatr. 2015;5(1):35–41.
Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012;44(2):171–80.
Szilagyi PG, Humiston SG, Gallivan S, Albertin C, Sandler M, Blumkin A. Effectiveness of a citywide patient immunization navigator program on improving adolescent immunizations and preventive care visit rates. Arch Pediatr Adolesc Med. 2011;165(6):547–53.
Kharbanda EO, Stockwell MS, Fox HW, Andres R, Lara M, Rickert VI. Text message reminders to promote human papillomavirus vaccination. Vaccine. 2011;29(14):2537–41.
Matheson EC, Derouin A, Gagliano M, Thompson JA, Blood-Siegfried J. Increasing HPV vaccination series completion rates via text message reminders. J Pediatr Health Care. 2014;28(4):e35–9.
Patel A, Stern L, Unger Z, et al. Staying on track: a cluster randomized controlled trial of automated reminders aimed at increasing human papillomavirus vaccine completion. Vaccine. 2014;32(21):2428–33.
Perkins R, Zisblatt L, Legler A, Trucks E, Hanchate A, Gorin S. Effectiveness of a provider-focused intervention to improve HPV vaccination rates in boys and girls. Vaccine. 2015;33(9):7.
Reiter PL, Gower AL, Kiss DE, et al. A web-based human papillomavirus vaccination intervention for young gay, bisexual, and other men who have sex with men: protocol for a randomized controlled trial. JMIR Res Protoc. 2020;9(2):e16294.
McRee A-L, Shoben A, Bauermeister JA, Katz ML, Paskett ED, Reiter PL. Outsmart HPV: acceptability and short-term effects of a web-based HPV vaccination intervention for young adult gay and bisexual men. Vaccine. 2018;36(52):8158–64.
Halkitis PN, Valera P, LoSchiavo CE, et al. Human papillomavirus vaccination and infection in young sexual minority men: the P18 cohort study. AIDS Patient Care STDs. 2019;33(4):149–56.
Shah PD, Gilkey MB, Pepper JK, Gottlieb SL, Brewer NT. Promising alternative settings for HPV vaccination of US adolescents. Expert Rev Vaccines. 2014;13(2):235–46.
Brewer NT, Chung JK, Baker HM, Rothholz MC, Smith JS. Pharmacist authority to provide HPV vaccine: novel partners in cervical cancer prevention. Gynecol Oncol. 2014;132:S3–8.
McRee A-L, Reiter PL, Pepper JK, Brewer NT. Correlates of comfort with alternative settings for HPV vaccine delivery. Hum Vaccin Immunother. 2013;9(2):306–13.
Calo WA, Gilkey MB, Shah P, Marciniak MW, Brewer NT. Parents’ willingness to get human papillomavirus vaccination for their adolescent children at a pharmacy. Prev Med. 2017;99:251–6.
Hastings TJ, Hohmann LA, McFarland SJ, Teeter BS, Westrick SC. Pharmacists’ attitudes and perceived barriers to human papillomavirus (HPV) vaccination services. Pharmacy. 2017;5(3):45.
Cebollero J, Walton SM, Cavendish L, Quairoli K, Cwiak C, Kottke MJ. Evaluation of human papillomavirus vaccination after pharmacist-led intervention: a pilot project in an ambulatory clinic at a large academic urban medical center. Public Health Rep. 2020;135(3):313–21.
Federico SG, Abrams L, Everhart RM, Melinkovich P, Hambidge SJ. Addressing adolescent immunization disparities: a retrospective analysis of school-based health center immunization delivery. Am J Public Health. 2010;100(9):1630–4.
Moss JL, Feld AL, O’Malley B, et al. Opportunities for increasing human papillomavirus vaccine provision in school health centers. J Sch Health. 2014;84(6):370–8.
Cheffins T, De La Rue S, Reeve C, Culpan M. School-based vaccinations delivered by general practice in rural North Queensland: an evaluation of a new human papillomavirus vaccination program. Commun Dis Intell Q Rep. 2008;32(1):94.
Ogilvie G, Anderson M, Marra F, et al. A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med. 2010;7(5):e1000270.
Watson M, Shaw D, Molchanoff L, McInnes C. Challenges, lessons learned and results following the implementation of a human papilloma virus school vaccination program in South Australia. Aust N Z J Public Health. 2009;33(4):365–70.
Walker KK, Jackson RD, Sommariva S, Neelamegam M, Desch J. USA dental health providers’ role in HPV vaccine communication and HPV-OPC protection: a systematic review. Hum Vaccin Immunother. 2019;15(7–8):1863–9.
Vázquez-Otero C, Vamos CA, Thompson EL, et al. Assessing dentists’ human papillomavirus-related health literacy for oropharyngeal cancer prevention. J Am Dent Assoc. 2018;149(1):9–17.
Griner SB, Thompson EL, Vamos CA, et al. Dental opinion leaders’ perspectives on barriers and facilitators to HPV-related prevention. Hum Vaccin Immunother. 2019;15(7–8):1856–62.
Lazalde GE, Gilkey MB, Kornides ML, McRee A-L. Parent perceptions of dentists’ role in HPV vaccination. Vaccine. 2018;36(4):461–6.
Murthy N, Rodgers L, Pabst L, Fiebelkorn AP, Ng T. Progress in childhood vaccination data in immunization information systems—United States, 2013–2016. MMWR Morb Mortal Wkly Rep. 2017;66(43):1178.
Groom H, Hopkins DP, Pabst LJ, et al. Immunization information systems to increase vaccination rates: a community guide systematic review. J Public Health Manag Pract. 2015;21(3):227–48.
Centers for Disease Control and Prevention. 2013–2018 immunization information functional standards 2019. https://www.cdc.gov/vaccines/programs/iis/functional-standards/func-stds-2013-2018.html
Szilagyi P, Albertin C, Gurfinkel D, et al. Effect of state immunization information system centralized reminder and recall on HPV vaccination rates. Pediatrics. 2020;145(5):e20192689.
Acknowledgments
The authors of the chapter wish to thank Mary Katherine Haver, MLIS, AHIP, Medical Librarian, at the Moffitt Cancer Center Biomedical Library for conducting an initial search for articles for this chapter.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Christy, S.M. et al. (2023). Community-Based Interventions for HPV Vaccination. In: Hughes Halbert, PhD, C. (eds) Cancer Health Disparities. Springer, Cham. https://doi.org/10.1007/978-3-031-37638-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-031-37638-2_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-37637-5
Online ISBN: 978-3-031-37638-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)