Abstract
Spheno-orbital meningioma is a unique skull base neoplasm characterized by intracranial and intraorbital tumor involvement and variable and often extensive bone invasion. It accounts for 2–9% of all intracranial meningiomas. In most cases, it is a slow-growth and benign tumor. The classic triad of proptosis, visual deficit, and diplopi represents the most frequent clinical symptoms and signs.
Currently, there are not defined guidelines concerning the best treatment strategy, which should be tailored for each patient and its goal established during the decision-making process. Surgery represents the first option when functional impairment occurs; its main goal is to preserve the visual function. The improvement of the clinical symptoms is achieved in almost all cases. Nevertheless, because of the anatomical relationship of this tumor with highly functional neurovascular structures, the gross total resection is hard to achieve; it results in high rate of recurrence ranging from 0 to 56%.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Since the first definition of spheno-orbital meningiomas (SOM) as en-plaque meningiomas provided by Cushing and Eisenhardt in 1938 [1], several terminologies have been adopted over the years to define these tumors, such as “sphenoid wing meningioma,” “en-plaque meningioma,” “hyperostosing meningioma of the sphenoid ridge,” and “pterional meningioma.” They are tumors arising at the sphenoid wing with secondary involvement of the periorbit [2], usually through the lateral wall and roof of the orbit, the superior orbital fissure (SOF), and/or the optic canal (OC) and characterized by an hyperostotic component of various degree and thin, carpet-like soft tissue growth at the dura. This pattern of growth accounts for the classic triad of presenting symptoms and signs of SOMs, consisting of proptosis, visual impairment, and ocular paresis.
There is no unanimous consensus in literature concerning the best treatment strategy, which should be tailored according to the tumor size and extension and the patient’s clinical features.
This chapter reports the current knowledge concerning the spheno-orbital meningiomas, mainly focusing on their surgical management.
2 Natural History
Spheno-orbital meningiomas account for 2–9% of all intracranial meningiomas [3]. They mainly affect females (82%), who usually are younger than males at diagnosis, with a mean age of 51 ± 6 years old and who more often express the progesterone receptor at histological examination [4, 5]. Furthermore, the spheno-orbital region represents the most frequent location for intracranial meningiomas in sex female [5].
In most cases, these tumors are slow-growing (0.3 cm3 per year) [6] and benign (WHO grade I).
The site of origin and the pattern of growth account for the main presenting signs and symptoms due to the mass effect: proptosis (84%), visual acuity (46%), and visual field (31%) deficits for the involvement of the optic nerve, and ophthalmoplegia (22%) with consequent diplopia due to the involvement of the oculomotor cranial nerves (III 11%, IV 6%, VI 4%). Other less frequent clinical manifestations include neurological impairment, such as mental change, memory deficit, and seizures [4].
3 Clinical and Neuroradiological Evaluation
A careful clinical and radiological evaluation for the tumor definition and planning of the therapeutic strategy is required and includes.
The clinical evaluation includes: the neurologic examination by a neurologist to evaluate symptoms of intracranial tumor extension; the assessment of proptosis with an ophthalmometer, the ocular motility, the visual acuity, and visual field by an ophthalmologist; the optic coherence tomography (OCT) may be sometimes useful.
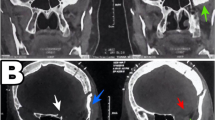
The diagnostic imaging by a radiologist must include high-resolution 3D CT scans and MRI. CT scan of the skull must assess the hyperostosis degree of the sphenoid wing and the surrounding structures, mainly the optic canal, superior orbital fissure, and anterior clinoidal process. The contrast-enhanced MRI must define the intracranial and intraorbital components of the tumor, the extent of dura mater involvement, the relationship of the tumor with the surrounding soft tissues and neurovascular structures (Fig. 13.1). Finally, the neurosurgeon and radiotherapist complete the multidisciplinary team for the decision-making process about the treatment strategy.
Preoperative axial images of left spheno-orbital meningioma: (a–c) MRI T2-weighted sequences showing the lesion arising from the dura of greater sphenoid wing, with caudal involvement of the inferior orbital fissure and the insertion of the temporalis muscle; MRI T1-weigthed pre- (d) and post- (e) contrast sequences; (f) bone-window CT scan showing the bone remodeling of the greater sphenoid wing resulting from the lesion
4 Treatment Strategies
At the state of the art, there are no defined guidelines in literature concerning the best treatment strategy, which presents several controversies, such as the “wait and see” option, the role of surgery and its timing, the surgical approach, the extension of the tumor resection or decompression of the hyperostosis, the management of the periorbita, the dural and bone reconstruction, the role of radiation therapy and the management of the residual tumor and recurrences, the validity of the Simpson grading system.
4.1 The Role of Surgery
The role of surgery was matter of debate in the past for several reasons [7]. The spheno-orbital meningiomas are slow-growing tumors with often long and stable clinical phase; there is involvement of vulnerable and highly functional nervous structures, such as optic and/or oculomotor cranial nerves; the possibility of a total resection is limited and increases the risk of postoperative morbidity.
Some authors are in favor of a “wait and scans” strategy [6], others are oriented toward a gross-total resection with proptosis correction [8, 9], others aim at a symptom-oriented surgery [10].
Nowadays, the surgery represents the first choice when functional impairment occurs, with the aim of an onco-functional balance between the need to achieve a maximal safe resection and the need to preserve/restore a good neurological and ophthalmological function [4, 11, 12]. In this scenario, the subtotal resection followed by radiation therapy for selected locations of residual meningioma, that is, -the cavernous sinus [2], or without adjuvant treatment but with second surgery at regrowth [13] are some of the management strategies.
Surgery of spheno-orbital meningiomas is extremely challenging, due to their anatomical relationship with vulnerable and highly functional neurovascular structures, such as optic and oculomotor nerves, cavernous sinus, trigeminal nerve branches. Therefore, the choice of an aggressive surgical approach might lead to unnecessary peri- and postoperative morbidity; on the other hand, a less invasive and more conservative approach might not provide an adequate exposure of the surgical target area, not guarantee the control of the neurovascular structures, a satisfying bony decompression and tumor removal. It results in no clinical improvement and high rate of recurrence.
Although the extent of resection affects the progression-free survival, the gross-total resection of spheno-orbital meningiomas is achieved in 25%–69% [3] and is burdened by high risk of severe morbidity.
Several surgical approaches have been described for the treatment of spheno-orbital meningiomas, either microsurgical, such as the pterional and its “extended” variant, the lateral orbitotomy [14], the supraorbital-pterional, the frontotemporo-orbitozygomatic (FTOZ), and more recently, endoscopic, via endonasal, transorbital, supraorbital and trans-maxillary, the latter being performed in isolated or combined multiportal manner, based on the tumor size and extension, each of them with related advantages and limits [4, 14,15,16,17,18,19,20].
Concerning the transcranial microsurgical routes, our group in the past has proposed an algorithm in the choice of the approach according to the intraorbital tumor extent in relationship with the axis of the optic nerve [19]: in the detail, we suggested the lateral orbitotomy [14] in cases of lateral and superolateral involvement of the orbit, the supraorbital-pterional approach for medial, inferomedial and orbital apex meningiomas, and the fronto-temporo-orbito-zygomatic approach for diffuse meningiomas with invasion of the cavernous sinus and infratemporal fossa.
The endoscopic approaches aim to minimize perioperative and postoperative morbidity and reducing aesthetic disfigurement. The surgical indications of superior eyelid transorbital endoscopic approach for neurosurgical intracranial pathologies are constantly and rapidly increasing, mainly for spheno-orbital meningiomas. This endoscopic technique has concrete advantages, such as the minimally invasive nature, short distance and direct access to the target, reduced bone destruction, minimal brain retraction and manipulation, early tumor deafferentation, satisfactory aesthetic result, short hospital-stay and rapid patient recovery.
From a recent meta-analysis and systematic review on surgical techniques and outcome for SOM [4], which included 38 articles out of 621 identified, the extended pterional resulted the workhorse approach, being the most performed in 37 among 38 surgical series, whereas the endoscopic technique, vie endonasal route, was reported in only three articles. Furthermore, the optic canal was the most frequently decompressed structure (31/38, 82%), followed by the superior orbital fissure (25/38, 66%), while no trend in the extent of decompression or resection of the hyperostotic bone was registered. The data concerning the reconstruction technique was almost heterogeneous: some authors (7/38, 18%) repaired the dural defect with free draft of fascia, others (6/38, 16%) with pericranium, whereas for the bony defect, some authors used the titanium mesh (14/38, 37%), others (11/38, 29%) the inner calvaria graft or polymethylmethacrylate (10/38, 26%). Among the clinical symptoms and signs, proptosis, diplopia, and ophthalmoplegia improved in 96% of cases, visual acuity deficit in 91% and visual field deficit in 87%. Finally, the most common reported complication was trigeminal hypoesthesia (19%), followed by ptosis (17%), cranial nerve deficit (17%), diplopia (17%), ophthalmoplegia (16%), visual acuity deficit (9%), and visual field deficit (4%).
Some authors recommend reconstruction of the orbital walls in order to prevent enophthalmos and/or diplopia; in our experience, we found that partial or complete resection of the orbital roof did not require reconstruction.
The transcranial approach allows wider exposure of the lateral wall and roof of the orbit and the middle cranial fossa but at risk of temporal muscle atrophy and complications related to the brain manipulation [2, 10, 21, 22].
The continue research of the minimal invasiveness to reduce the perioperative and postoperative morbidity and the peculiar advantages demonstrated over the years since its introduction at the beginning of the last century by endoscopic approaches, via endonasal and, more recently transorbital routes, in the management of skull base pathologies, led to progressive expansion of their surgical indication. Nowadays, transorbital endoscopic approaches are used for the management of wide variety of skull base lesions with or without orbit involvement, mainly meningiomas [18].
There is strong evidence of postoperative improvement of the clinical symptoms, mainly proptosis and ocular motility deficits, but also visual acuity and visual field deficits [4]; therefore, the visual outcomes endorse surgery of patients with spheno-orbital meningiomas even with minimal visual impairment or hyperostosis [23], although there are no defined knowledge on the effect of the timing of surgery on visual and neurological outcomes.
At the light of these findings and in agreement with the concept of symptoms-oriented surgery for spheno-orbital meningiomas, we consider that the surgery is primarily directed to the optic nerve decompression in cases of decreased visual acuity; on the other hand, when the proptosis is the main clinical sign without tumor involvement of the optic canal, a lateral orbitotomy may result effective to obtain adequate reduction of the proptosis.
In this scenario, the decompression of the optic canal and nerve, and/or the superior orbital fissure, associated to the maximal safe tumor resection, represent the most appropriated surgical maneuvers.
4.2 Adjuvant Treatments
Currently, there is no clear evidence about the indications and the efficacy of the radiation therapy on the treatment of spheno-orbital meningiomas as few studies are focused on this aspect. Some authors suggest performing radiotherapy in WHO grade II tumors and with rapid pattern of growth [10, 21, 24]; or in cases of involvement of the superior orbital fissure and cavernous sinus [2, 9]; or after subtotal resection or WHO grade II and III meningiomas [3, 25].
We recommend the radiation therapy in patients undergone subtotal resection, with ocular muscles infiltration and only a close clinical and radiological follow-up when a gross total resection (Simpson’s grades I and II) is achieved, regardless the WHO grade of the tumor.
Concerning the role of the radiosurgery, its application is different among the institutions; its main limit remains the proximity of the optic pathway to the tumor [9].
5 Recurrences
5.1 Prognostic Risk Factors
Several factors affect the recurrence rate of spheno-orbital meningiomas, including the extent of resection, the tumor location, the WHO grade, and the length of follow-up.
Because of their deep-seated location on the skull base, their pattern of growth, extension, and invasiveness, anatomical relationships with functional neurovascular structures, the gross total resection of spheno-orbital meningiomas is hard to achieve, and this aspect affects the recurrence rate, which ranges from 0 to 56% [13]. In terms of Simpson’s grading system [26], the recurrence rate is greater after Simpson’s grade III and IV than after grade I [27].
The invasion of the cavernous sinus and intraconal compartment [3], as well as of the orbital apex [13], optic canal [13, 24] and superior orbital fissure [13] are considered unfavorable prognostic factors of progression free survival; in these conditions, the risk of postoperative morbidity resulting from an aggressive treatment limits the extent of resection in favor of a more conservative approach.
The recurrence rate is also related to the WHO grade, with atypical grade II meningiomas recurring more frequently than the benign grade I (63% vs 18%, respectively) [13].
Finally, the risk of recurrence is affected by the length of follow-up, with a higher recurrence rate after a long follow-up [2, 13].
5.2 Management
The management of recurrent spheno-orbital meningiomas is still matter of debated.
We consider the reoperation as the first treatment option in cases of symptomatic tumors at the regrowth and/or recurrence and the “wait and see” strategy for asymptomatic patients with limited regrowth. The aim of the re-surgery, as for the surgery at the first diagnosis, is the relief, restoration/improvement of clinical signs, and symptoms or the arrest of their deterioration. For these purposes, even several reoperations are justified. The role of the radiation treatments on the recurrences is the same for patients at the first diagnosis.
6 Conclusion
Spheno-orbital meningioma is a unique skull base tumor representing a challenge of treatment. Although in most cases it is a benign and slow-growth tumor, if underestimated it may lead to highly functional and irreversible neurological deficits. A multidisciplinary team is required for the decision-making concerning the diagnostic and therapeutic processes. The surgery represents the first choice when functional impairment occurs; although the gross total resection is difficult to achieve without severe morbidity, the improvement of the main clinical symptoms is achieved in almost all cases.
References
Cushing H, Meningiomas LE. Their classification, regional behaviour, life history, and surgical end results. Springfield, IL: Charles C. Thomas; 1938.
Terrier LM, Bernard F, Fournier HD, Morandi X, Velut S, Hénaux PL, et al. Spheno-orbital Meningiomas surgery: multicenter management study for complex extensive tumors. World Neurosurg. 2018;112:e145–e56. https://doi.org/10.1016/j.wneu.2017.12.182.
Masalha W, Heiland DH, Steiert C, Krüger MT, Schnell D, Scheiwe C, et al. Progression-free survival, prognostic factors, and surgical outcome of spheno-orbital meningiomas. Front Oncol. 2021;11:672228. https://doi.org/10.3389/fonc.2021.672228.
Fisher FL, Zamanipoor Najafabadi AH, Schoones JW, Genders SW, van Furth WR. Surgery as a safe and effective treatment option for spheno-orbital meningioma: a systematic review and meta-analysis of surgical techniques and outcomes. Acta Ophthalmol. 2021;99(1):26–36. https://doi.org/10.1111/aos.14517.
Apra C, Roblot P, Alkhayri A, Le Guérinel C, Polivka M, Chauvet D. Female gender and exogenous progesterone exposition as risk factors for spheno-orbital meningiomas. J Neuro-Oncol. 2020;149(1):95–101. https://doi.org/10.1007/s11060-020-03576-8.
Saeed P, van Furth WR, Tanck M, Kooremans F, Freling N, Streekstra GI, et al. Natural history of spheno-orbital meningiomas. Acta Neurochir. 2011;153(2):395–402. https://doi.org/10.1007/s00701-010-0878-0.
Cophignon J, Lucena J, Clay C, Marchac D. Limits to radical treatment of spheno-orbital meningiomas. Acta Neurochir Suppl (Wien). 1979;28(2):375–80.
Bikmaz K, Mrak R, Al-Mefty O. Management of bone-invasive, hyperostotic sphenoid wing meningiomas. J Neurosurg. 2007;107(5):905–12. https://doi.org/10.3171/JNS-07/11/0905.
Boari N, Gagliardi F, Spina A, Bailo M, Franzin A, Mortini P. Management of spheno-orbital en plaque meningiomas: clinical outcome in a consecutive series of 40 patients. Br J Neurosurg. 2013;27(1):84–90. https://doi.org/10.3109/02688697.2012.709557.
Freeman JL, Davern MS, Oushy S, Sillau S, Ormond DR, Youssef AS, et al. Spheno-orbital meningiomas: a 16-year surgical experience. World Neurosurg. 2017;99:369–80. https://doi.org/10.1016/j.wneu.2016.12.063.
Zamanipoor Najafabadi AH, Peeters MCM, Dirven L, Lobatto DJ, Groen JL, Broekman MLD, et al. Impaired health-related quality of life in meningioma patients-a systematic review. Neuro-Oncology. 2017;19(7):897–907. https://doi.org/10.1093/neuonc/now250.
Gonen L, Nov E, Shimony N, Shofty B, Margalit N. Sphenoorbital meningioma: surgical series and design of an intraoperative management algorithm. Neurosurg Rev. 2018;41(1):291–301. https://doi.org/10.1007/s10143-017-0855-7.
Mariniello G, de Divitiis O, Corvino S, Strianese D, Iuliano A, Bonavolontà G, et al. Recurrences of spheno-orbital meningiomas: risk factors and management. World Neurosurg. 2022;161:e514. https://doi.org/10.1016/j.wneu.2022.02.048.
Mariniello G, Maiuri F, de Divitiis E, Bonavolontà G, Tranfa F, Iuliano A, et al. Lateral orbitotomy for removal of sphenoid wing meningiomas invading the orbit. Neurosurgery. 2010;66(6 Suppl Operative):287–92; discussion 92. https://doi.org/10.1227/01.NEU.0000369924.87437.0B.
Abou-Al-Shaar H, Krisht KM, Cohen MA, Abunimer AM, Neil JA, Karsy M, et al. Cranio-orbital and Orbitocranial approaches to orbital and intracranial disease: eye-opening approaches for neurosurgeons. Front Surg. 2020;7:1. https://doi.org/10.3389/fsurg.2020.00001.
Dallan I, Cristofani-Mencacci L, Fiacchini G, Caniglia M, Sellari-Franceschini S, Berrettini S. When multidisciplinary surgical trans-orbital approaches should be considered to reach the skull base. Acta Otorhinolaryngol Ital. 2021;41(Suppl. 1):S59–66. https://doi.org/10.14639/0392-100X-suppl.1-41-2021-06.
Locatelli D, Restelli F, Alfiero T, Campione A, Pozzi F, Balbi S, et al. The role of the Transorbital superior eyelid approach in the Management of Selected Spheno-orbital meningiomas: in-depth analysis of indications, technique, and outcomes from the study of a cohort of 35 patients. J Neurol Surg B Skull Base. 2022;83(2):145–58. https://doi.org/10.1055/s-0040-1718914.
Kong DS, Kim YH, Hong CK. Optimal indications and limitations of endoscopic transorbital superior eyelid surgery for spheno-orbital meningiomas. J Neurosurg. 2020;134(5):1472–9. https://doi.org/10.3171/2020.3.JNS20297.
Mariniello G, Maiuri F, Strianese D, Donzelli R, Iuliano A, Tranfa F, et al. Spheno-orbital meningiomas: surgical approaches and outcome according to the intraorbital tumor extent. Zentralbl Neurochir. 2008;69(4):175–81. https://doi.org/10.1055/s-2008-1077077.
Lew H, Rootman DB, Nassiri N, Goh A, Goldberg RA. Transorbital approach without craniotomy to orbital tumors with extradural intracranial extension. Orbit. 2014;33(5):343–51. https://doi.org/10.3109/01676830.2014.904374.
Cannon PS, Rutherford SA, Richardson PL, King A, Leatherbarrow B. The surgical management and outcomes for spheno-orbital meningiomas: a 7-year review of multi-disciplinary practice. Orbit. 2009;28(6):371–6. https://doi.org/10.3109/01676830903104645.
Shrivastava RK, Sen C, Costantino PD, Della RR. Sphenoorbital meningiomas: surgical limitations and lessons learned in their long-term management. J Neurosurg. 2005;103(3):491–7. https://doi.org/10.3171/jns.2005.103.3.0491.
Zamanipoor Najafabadi AH, Genders SW, van Furth WR. Visual outcomes endorse surgery of patients with spheno-orbital meningioma with minimal visual impairment or hyperostosis. Acta Neurochir. 2021;163(1):73–82. https://doi.org/10.1007/s00701-020-04554-9.
Leroy HA, Leroy-Ciocanea CI, Baroncini M, Bourgeois P, Pellerin P, Labreuche J, et al. Internal and external spheno-orbital meningioma varieties: different outcomes and prognoses. Acta Neurochir. 2016;158(8):1587–96. https://doi.org/10.1007/s00701-016-2850-0.
Terpolilli NA, Ueberschaer M, Niyazi M, Hintschich C, Egensperger R, Muacevic A, et al. Long-term outcome in orbital meningiomas: progression-free survival after targeted resection combined with early or postponed postoperative radiotherapy. J Neurosurg. 2019;133:1–11. https://doi.org/10.3171/2019.3.JNS181760.
Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957;20(1):22–39.
Mariniello G, Bonavolontà G, Tranfa F, Maiuri F. Management of the optic canal invasion and visual outcome in spheno-orbital meningiomas. Clin Neurol Neurosurg. 2013;115(9):1615–20. https://doi.org/10.1016/j.clineuro.2013.02.012.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mariniello, G., Corvino, S., Iuliano, A., Maiuri, F. (2023). Spheno-orbital Meningiomas. In: Bonavolontà, G., Maiuri, F., Mariniello, G. (eds) Cranio-Orbital Mass Lesions. Springer, Cham. https://doi.org/10.1007/978-3-031-35771-8_13
Download citation
DOI: https://doi.org/10.1007/978-3-031-35771-8_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-35770-1
Online ISBN: 978-3-031-35771-8
eBook Packages: MedicineMedicine (R0)