Abstract
Background
Internal variation among spheno-orbital meningiomas (SOM) is surgically challenging. Optic canal invasion management is discussed.
Method
This retrospective study includes 70 patients with SOM who underwent surgery between 1995 and 2012. Preoperative ophthalmological, neurological and aesthetic clinical signs were collected. All patients benefitted from repeated tomography and magnetic resonance imaging (MRI). The surgical team consisted of a neurosurgeon and a plastic surgeon. In the majority of cases, resection was followed by bone reconstruction using an autologous iliac crest graft. The extent of resection was evaluated on the dural and osseous sides. Early clinical outcomes, long-term follow-up, recurrence and adjuvant therapies were reported.
Results
The mean age was 52 years old, and 91 % of the patients were women. Initial symptoms primarily included proptosis (65 %), decreased visual acuity (39 %) and soft tissue tumefaction (16 %). We classified 40 cases as the internal variety when considering the inner third of the greater wing of the sphenoid, optic canal, anterior clinoid process or cavernous sinus. The remaining cases were described as the external variety. The complete resection rates for the internal and external varieties were 12 % and 61 %, respectively (P < 0.001). In total, 90 % of cases were grade I meningiomas. For grade I, we reported 30 % recurrence, and 50 % of these cases recurred in the first 2 years. Grade II cases without early adjuvant radiotherapy increased at 2 years. We did not observe any difference in recurrence rate among grade I tumours with or without tumour remnants. At the end of follow-up, visual acuity was stabilised or increased in 88 % of patients. In addition, 14 % of patients experienced persistent pain at the location of the iliac harvesting site.
Conclusions
The internal SOM variety exhibited a reduced total resection rate and a shorter progression-free survival (PFS). Unroofing of the optic canal extended PFS. Among grade I cases, the persistence of a negligible tumour remnant did not alter the probability of recurrence. For superior grades, radiotherapy must be administered in addition to surgery as soon as possible. SOMs require prolonged follow-up. Autologous iliac reconstruction is related to substantial morbidity and could be replaced by prosthetic bone three-dimensional reconstruction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spheno-orbital meningiomas (SOMs) account for 9–18 % of all adult intracranial meningiomas, and their natural history differs from other meningiomas [1, 2]. These tumours are associated with a hyperostosis, which constitutes the main part of the tumour, predominantly on sphenoid bone that extends to the orbit and a widespread dural thickening, which is referred to as an “en plaque” invasion. The decrease of visual acuity, aesthetic discomfort and proptosis are prominent symptoms. The surgical management of these symptoms has remained controversial; some authors advocating for a wait and see approach [3, 4]. Nevertheless, several surgical teams adopted a new point of view, thus giving rise to functional outcomes and prescribing complete resection associated with proptosis correction and visual conservation [5, 6]. Nonetheless, this condition remains a surgical challenge with a double purpose of functional preservation and oncological resection.
Our study is to clarify SOM management based on lesion location, defining internal and external SOM varieties. Our series was designed to emphasise the crucial role of preoperative imaging in establishing a surgical strategy and to predict tumour evolution. We reported the surgical techniques and objectives, modality of follow-up and adjuvant therapies based on the initial tumour and its histological grade.
Patients and methods
Patient consent
Patients were informed that their clinical data could be used for medical research. Our institutional review board approved this study.
Patient selection
We retrospectively reviewed systematically all patients with an established diagnosis of SOM treated at our institution between 1995 and 2012. SOM was defined as a meningioma involving the sphenoid bone with predominant intraosseous tumour growth that could infiltrate the orbit and was associated with a thin “carpet-like” intradural extension.
Data collection
For every patient, clinical onset was reported, especially ophthalmological, neurological and aesthetic signs. Visual acuity was systematically noted at diagnosis. Using an ophthalmological classification [7], loss of visual acuity was classified as minimal for visual acuity ≥0.7, moderate for visual acuity between 0.3 and 0.7 and severe for visual acuity ≤0.3. Each patient was subject to multimodal imaging before surgery. Computed tomography (CT) scan provided the best images of hyperostosis of sphenoid bone and adjacent structures, whereas magnetic resonance imaging (MRI) offered the best images of tumour soft tissue infiltration, dura mater extension and the intradural compartment. Gadolinium-enhanced MRI images and fat suppression sequences were obtained to delineate the extradural, intradural and intraorbital tumour infiltration. The SOM side and type of bony invasion were reported. We precisely assessed invasion of the pterion, lesser or greater wing of the sphenoid, the orbit, the optic canal, the cavernous sinus and the anterior clinoid process. Invasion of the temporal muscle was also reported. We defined two types of SOM depending on anatomic invasion criteria as shown in Table 1 and Fig. 1. If the inner third of the sphenoid wing, optic canal, anterior clinoid process or cavernous sinus were involved, the lesion was defined as the internal variety. The lesion was classified as the external variety if none of the structures sited above were affected and if at least one of the following structures exhibited invasion: the pterion, the external third of the lesser or greater sphenoid wing, the external part of the orbital rim, and in some cases the temporal muscle. All imaging data were interpreted by a neuroradiologist and reviewed by one neurosurgeon (H.-A.L.). Our data were compared to previous significant series of SOM. The keywords used in PubMed to find these publications were: spheno-orbital meningioma, sphenoid wing tumour, skull base meningioma, orbital tumour and proptosis.
Anatomical descriptions of the internal (in red) and external (in green) SOM varieties on a three-dimensional (3D) CT scan, from a posterior and superior view. P pterion, eO external orbital wall, eSW external part of the sphenoid wing, iSW inner part of the sphenoid wing, OC optic canal, ACP anterior clinoid process, CS cavernous sinus
Surgical technique and follow-up
A multidisciplinary team, including a neurosurgeon and a plastic surgeon, performed the surgery. All interventions used an unilateral frontotemporal approach through a bi-coronal skin incision [8]. The purpose of this pterional approach was to remove the bone extension and subsequently reconstruct the craniofacial bone [9]. If the temporal muscle appeared pathological, the infiltrated portion was resected. The first and main part of the surgery consisted of drilling hyperostotic bone via two directions: (1) the spheno-optic direction was used to remove the lesser wing of the sphenoid and then potentially open the optic canal and the superior orbital fissure, (2) the sphenoid-pterygoid direction was used to remove the greater sphenoid wing, occasionally open the foramen rotundum and ovale in the most advanced SOM cases, and the lesser sphenoid wing to gain access to the orbit without removing the lateral orbital rim. The periorbita was not opened unless the tumour invaded the intraconal space. Infiltrated ocular muscles were not resected. The meningeal portion of the tumour was then removed, followed by a duraplasty using autologous epicranius. Eventually, the reconstruction of the lateral wall of the orbit and pterional area was performed by a plastic surgeon, using an autologous iliac crest graft [10]. Postoperative complications were collected with a special attention to visual acuity evolution. To analyse the extent of surgical tumour resection, operative reports were matched with postoperative data, including MRI and CT scan. Upon examination by a neuropathologist, the meningioma histological type was reported. For each patient, information regarding all adjuvant therapies, including conformational radiotherapy (denoted as “early” when delivered in the first 3 months), radiosurgery or further surgery, was collected. Tumour progression was defined as an increase of contrast enhancement tissue or an increase of bone thickening compared with initial post-operative imaging. The sequence of additional treatments was also collected through the latest date the patient was seen.
Statistical analysis
Data are presented as median (interquartile range [IQR] or range) for quantitative variables and number (percentage) for qualitative variables. Comparisons of clinical symptoms and complete resection between the two SOM varieties were made using chi-squared tests (Fisher’s exact test was used when the expected cell frequency was <5). The delay between first examination and surgery was compared between the two SOM varieties using the Mann–Whitney U test. Progression-free survival (PFS) after initial surgery was estimated and compared using the Kaplan-Meier method and log-rank test. Given the exploratory nature and small sample size of this study, multivariate analyses were not conducted. Statistical testing was performed at the two-tailed α level of 0.05. Data were analysed using the SAS software package, version 9.3 (SAS Institute, Cary, NC).
Results
During the study period, 70 consecutive patients with SOM were treated within a median delay of 14 months (IQR, 5–27) from the first clinical symptom. The median age at diagnosis was 52 years (range, 21–80 years), and 64 of the patients were women (women-to-men ratio of 9).
Clinical symptoms and radiological findings
Clinical symptoms leading to the first examination (median delay from symptom onset, 12 months [IQR, 3–24]) are detailed in Table 2. The most frequent clinical symptom was proptosis, which occurred in 80 % of cases, followed by visual acuity decrease in 39 % and soft tissue tumefaction in 16 %. Headaches were more frequently reported in the internal variety group (P = 0.04). Visual acuity decrease was associated with internal variety (P = 0.057). Among the 27 patients with a preoperative visual acuity decrease, 10 patients exhibited a severe visual acuity decrease and 8 exhibited a moderate visual acuity decrease. Eight female patients (11 %) had a previous history of thyroid dysfunction.
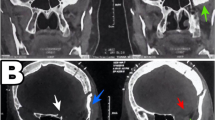
Concerning radiological findings, 42 patients (60 %) exhibited an internal variety. The optic canal was involved in 24 (57 %) of internal variety cases. Illustrative cases of the external and internal varieties on preoperative cranial CT and MRI are presented in Figs 2, 3 and 4.
Preoperative thin bone window CT sections of an external SOM variety. Left: Axial view exhibiting osseous invasion of the external wall of the orbit, greater sphenoid wing, with no invasion of the optic canal and the anterior clinoid process. Right: Coronal view illustrating hyperostosis of the superior and lateral portion of the orbital roof and lateral wall
Preoperative thin bone window CT section of an internal SOM variety. Left: Axial plane revealing osseous invasion of the sphenoid and temporal bones associated with hyperostosis affecting the inner portion of the optic canal and the anterior clinoid process. Right: Coronal view revealing important hyperostosis surrounding the orbit primarily at the inferior portion invading the temporal fossa and the emergence of the pterygoid process
Preoperative MRI axial plane view and T1 sequence with gadolinium enhancement. Left: An external SOM variety. Slight contrast enhancement of the dura, referred to as “carpet like”, is noted around the bony hyperostosis of the sphenoid wings. The cavernous sinus is not affected. Right: An internal SOM variety with more conspicuous contrast enhancement of the dura that involves the cavernous sinus associated with more important intradural soft tissue component
Surgical characteristics and short-term outcomes
The median delay between first examination and surgery was 3.7 months (IQR, 2.5–5.1) for the external variety and 2.1 months (IQR, 1.2–3.6) for the internal variety (P = 0.03). The optic canal was opened during the procedure in 26 cases. Among them, 19 (79 %) harboured documented preoperative optic canal invasion and 7 (15 %) did not. Optic canal opening was associated with the internal variety (P = 0.026). Histological analyses were available for 61 patients. Tumours were classified according to the WHO classification as grade I in 90 % of cases (n = 55), grade II in 5 % of cases (n = 3) and grade III in 5 % of cases (n = 3). Seven patients with incomplete tumour resection benefitted from early postoperative conformational radiotherapy (<3 months after surgery). These patients individually harboured three grade III, 1 grade II and three grade I meningiomas.
Complete resection was achieved in 22 cases (31 %). An increased rate of complete resection was observed in the patients with the external variety (61 %, n = 17) compared with internal variety patients (12 %, n = 5, P < 0.001). The rate of total resection was different among the external variety (61 %, n = 17), the internal variety without optic canal invasion (11 %, n = 2) and the internal variety with optic canal invasion (12.5 %, n = 3), (P < 0.0001). A major reason for incomplete resection involved cavernous sinus invasion, with tumour remnants visible to the surgeon at the end of the intervention in 23 (55 %) cases with the internal variety.
Complications
Early postoperative complications, defined as those occurring during the initial hospital stay, are summarised in Table 3. No significant difference was noted between the internal and external varieties (24 vs 19, P = 0.37). Transient homolateral ophthalmoparesis was the most frequent early complication and occurred in 23 % of cases. Major periorbital oedema and iliac sample site pain were also frequently reported individually in 14 % of cases. No cerebrospinal fluid leaks were noted. No early deaths were reported.
Long-term outcomes
Long-term outcomes were assessed at the final meeting with the patient. The median follow-up was 57 months (IQR, 21–98 months). Among the 56 patients harbouring a preoperative proptosis, 48 (86 %) exhibited significant improvement after surgery. Eight patients at the end of follow-up still harboured a slight proptosis. Regarding postoperative visual acuity evolution, 52 patients (74 %) exhibited stable visual acuity, 10 (14 %) presented visual acuity improvement and 8 (11 %) exhibited visual acuity deterioration (Table 3). No significant difference was noted between the internal and external varieties regarding postoperative visual acuity evolution (P = 0.58). However, although the difference was not significant, more visual acuity decreases were observed in the internal variety group (7 vs 1, P = 0.13) (Table 4).
Tumour recurrence occurred in 20 (29 %) patients (median delay, 22 months; IQR, 13–34), including 4 patients with the external variety, 4 patients with the internal variety without optic canal invasion and 12 patients with the internal variety with optic canal invasion. Among the 14 tumour recurrences with available histological results, operative tissue samples were classified as grade I in 10 cases, grade II in 2 cases and grade III in the remaining two cases. Nine patients benefitted from additional radiotherapy after tumour recurrences have been diagnosed (eight grade I, one grade II).
As shown in Fig. 5a, PFS was enhanced in patients with the external variety compared with patients with the internal variety, with a borderline non-significant difference (P = 0.054). When comparing patients with and without optic canal invasion (Fig. 5b), a greater difference in PFS was observed (Fig. 5b, P = 0.009). PFS at 5 years was 45 % in patients with optic canal invasion compared with 75 % in patients without optic canal invasion. However, optic canal opening was associated with improved PFS (P = 0.05). Complete resection was not significantly associated with enhanced PFS (P = 0.15). For grade I meningiomas, incomplete resection was not associated with recurrence (P = 0.14).
Discussion
Key results
Seventy SOM cases benefitted from a median long-term follow-up of 5 years. Forty-two (60 %) patients exhibited an internal variety. The optic canal was involved in more than half of the internal cases. Complete resection was achieved in 22 (31 %) cases. Internal variety patients exhibited a lower resection rate, with only five (12 %) complete resections (P < 0.001).
Forty-eight (86 %) patients reported significant improvement of their proptosis after surgery. Regarding visual acuity, 62 (89 %) patients exhibited improved or stable visual acuity at the end of follow-up.
Tumour recurrence occurred in 20 (29 %) patients, at a median delay of 2 years. Most of them occurred among patients harbouring internal variety with optic canal invasion. PFS at 5 years was 45 % in patients with optic canal invasion compared with 75 % in patients without optic canal invasion (P = 0.009). Optic canal opening was associated with enhanced PFS (P = 0.05). For grade I meningiomas, incomplete resection was not associated with recurrence (P = 0.14).
Clinical preoperative findings
Proptosis was the most frequent clinical finding, occurring in 80 % of patients as reported in other studies without differences between the external or internal varieties [11–13]. The main cause of proptosis was hyperostosis of orbital walls in the majority of cases and intraorbital meningioma invasion in a very few cases [13]. Decreased visual acuity at diagnosis was noted in 39 % of patients, as in other series [13, 14]. Preoperative visual acuity decreases were reported in a greater proportion among the internal variety group, and a nearly significant difference was noted (P = 0.056). Such a visual acuity decrease among the internal variety may be related to the following causes: optic canal invasion, optic nerve compression, and periorbital tissue infiltration or orbital apex invasion [15]. These data support the interventionist attitude of the surgical team for an internal SOM, which threatens more functional structures, such as the optic nerve or oculomotor nerves. SOM should be removed as early as possible, as Maroon et al. [2] suggested.
In our experience, the indications for surgery were: tumoural impact on visual function (visual acuity decrease, ophtalmoparesis), an aesthetic discomfort reported by the patient or a radiological progression between two exams. If not, clinical follow-up was performed, including MRI and CT scan controls at regular intervals.
Resection rate
The complete SOM resection rate was 31 % in our series. Previous studies from Ringel et al. [11] (25 %), Honig et al. [16] (33 %) and Oya et al. [17] (38 %) mostly reported values of approximately 30 %. We reported a significant difference between the external and internal varieties (61 % and 12 %, respectively; P < 0.001). The cavernous sinus and the superior orbital fissure were not removed to avoid persistent oculomotor nerve palsy and venous bleeding, as mentioned by Oya et al. [17] and Nagatani et al. [18]. In our series, according to operative reports, a macroscopic tumour remnant remained in place inside or around the cavernous sinus in 55 % of the internal variety. Anterior clinoid process invasion was also a great constraint for total tumour removal as it is in the vicinity of the internal carotid artery. Hyperostosis often tied up the internal carotid, and drilling even under operating microscopic may be very risky.
Among grade I meningiomas, which primarily consisted of meningothelial tumours, the presence of a postoperative remnant was not correlated with an increased recurrence rate. This result favours a cautious resection, preferring incomplete tumour removal instead of taking undue perioperative risks to achieve a complete resection.
Progression-free survival/recurrence
In our series, the median follow-up was approximately 5 years. The recurrence rate in our study was 29 %, consistent with previous series [13, 19]. Among recurrent tumours, the majority were histological grade I. This finding illustrates the inability of the classical histological grading system to predict tumour evolution [14]. In our series, the internal SOM variety was associated with reduced PFS, especially with optic canal invasion (P = 0.009). The 5-year PFS rate was 45 % for the internal variety with optic canal invasion compared with 75 % for non-invasion. This result is consistent with the resection rate. The majority of tumour recurrences occurred during the first 3 years following initial surgery as shown in Fig. 5. However, progression was noted more than 6 years after surgical removal. In his series, Gaillard also reported a late recurrence (7 years after initial resection) [9].
In our series, total resection was not significantly associated with a lower recurrence rate (P = 0.15). Nevertheless, previous authors, such as Schick et al. [12], reported increased recurrence rates with incomplete resection, (e.g. up to 50 % for incomplete resection vs 12 % for total resection). However, we reported that optic canal opening was statistically associated with enhanced PFS. According to Schick et al. [12], the surgeon must unroof the optic canal extradurally whenever tumour involvement is noted. The procedure should be performed at an early stage of the surgery to release the optic nerve from direct compression and prevent damage related to further intraoperative manipulations, such as prolonged compression or stretching [17, 20]. In our series, seven patients also benefitted from optic canal unroofing, although no tumour was previously described at that location. These seven patients had a “preventive” optic canal opening because of a preoperative tumoural aspect suspicious of malignancy with a threatening tumour location. Unroofing the optic canal was performed to protect these patients from an early recurrence with optic nerve compression. The patient follow-up did not allow us to draw conclusions from this small group; nevertheless, their clinical course, visual acuity follow-up and PFS appeared similar to other patients.
Functional outcome
In SOM surgery, a main challenge involves reducing proptosis, achieving an aesthetic result satisfying for the patient and preventing complications due to the permanent exposure of the cornea. In our series, proptosis was corrected in 86 % of patients. Other series reported similar results [12, 13, 17]. None of our patients required additional interventions to correct persistent proptosis. The efficiency of orbital decompression relies on the superolateral corner resection, particularly the extent of lateral wall removal [13, 21]. In some advanced cases, debulking of the infiltrated periorbita was performed to reduce proptosis. However, this procedure appeared to decrease visual performance, and an increased number of complications, such as severe ophthalmoparesis, were noted.
In our series, 89 % of patients exhibited normal or improved visual acuity at the end of the follow-up period. Among the 27 patients exhibiting a preoperative visual acuity decrease, 10 (37 %) patients were improved after surgery. The invasion of the optic canal is the main reason for visual dysfunction in patients with SOM [22]. Although these patients primarily exhibited optic canal invasion, unroofing the optic canal stabilised or even improved their visual acuity. This rate of visual acuity improvement is consistent with previous articles [12, 13, 22]. Nevertheless, visual acuity was further decreased in the internal variety group. The internal variety of SOM exhibited a greater recurrence rate and was more likely to exhibit visual pathway compression again.
Regarding preoperative temporal area bulging, no patient exhibited such a cosmetic deformity after reconstruction of the temporal convexity.
Perioperative reconstruction
The collaboration between neurosurgeons and plastic surgeons for reconstruction procedures has been effective in our institution for approximately 30 years. During this period, we changed the operative procedure from orbito-fronto-malar (OFM) “monobloc” removal to lesser sphenoid wing drilling without complete OFM removal [9, 23, 24].
The reconstruction procedure used a “tailored” iliac crest graft to rebuild the orbit walls (Fig. 6). Long-term cosmetic results were greatly improved, allowing orbital framework and temporal convexity rebuilding. The procedure allowed several complications to be avoided due to the absence of firm reconstruction of the lateral wall and roof of the orbit as pulsatile eye bulb, enophtalmos or oculomotor fibrosis [11]. The use of a “tailored” iliac crest graft allowed a majored temporal bony curve to compensate for the potential atrophy of the temporal muscle. In our series, no postoperative infection was noted, and no patient required reoperation for bony reconstruction. No CSF leak was reported. The use of an autologous bone graft reduced the risk of infection compared with prosthetic materials, such as titanium, polyetheretherketone or polymethylmethacrylate [25, 26]. Currently, we still perform iliac bone harvesting. However, in our series, 14 % of patients experienced significant postoperative pain at the location of the iliac harvesting site. Most of these patients experienced this discomfort until the final follow-up. This complication might be explained by a direct or indirect injury to the lateral femoral cutaneous nerve during the graft harvesting. To replace this technique, various authors, such as Pritz and Burgett [27], proposed the use of a pre-modelled implant to enhance the quality and symmetry of the reconstruction. He uses a three-dimensional implant generated by reversing the anticipated area of bone resection on the normal side to create a mirror-image implant. However, modelling very thin bone structures, such as the orbital roof or orbital lateral wall, remains challenging.
a, b Axial and coronal CT, thin bone window, illustrating the osseous hypertrophy of the right orbital roof and the postero-lateral wall of the orbit, typical of an external variety of SOM. c Posterior and superior view, revealing the hyperostosis of the right small sphenoid wing and the temporal bone. d–f Postoperative 3D CT, illustrating the reconstruction of the superior and lateral walls of the orbit with autologous iliac crest graft
According to several authors, firm orbital reconstruction is not mandatory in SOM surgery [2, 13, 28]. Maroon et al. [2] and De Monte et al. [28] reported no case of permanent pulsatile enophtalmos after performing orbital walls and roof resection without reconstruction. Talacchi et al. [13] stated that in cases with a preserved orbital rim, complication rates concerning enophtalmos or cosmetic defects were similar with or without bony reconstruction. Other authors suggested that corrective surgery should be delayed until a second operation [13]. Based on our experience, no reconstruction should be performed for small SOMs or in elderly patients to reduce the surgery duration.
Adjuvant radiotherapy
Early postoperative conformational radiotherapy for SOM with incomplete resection was previously reported [1, 29]. For grade II and III, additional irradiation is mandatory [30]. In our study, only two out of seven (29 %) patients exhibited tumour progression despite early irradiation. Usually for grade I meningioma, we adopt a wait-and-see approach. Among grade I with a tumoural remnant with no early irradiation, eight needed a delayed irradiation.
Conclusions
Among SOMs, separate entities can be individualised, such as the external variety with enhanced oncological and functional outcomes and the internal variety with a reduced total resection rate and PFS. The invasion of the optic canal clearly altered patient prognosis. According to our experience, unroofing the optic canal resulted in increased PFS. Immediate autologous bony reconstruction provides satisfying cosmetic results. However, the use of an autologous iliac graft is related to substantial morbidity, and 3D customised prosthetic reconstruction should be considered. Among grade I SOMs, incomplete resection did not modify the probability of recurrence, supporting the use of reasonable resection without functional risk. For superior grades, including grade II, radiotherapy should be administered in addition to surgery as soon as possible. SOMs require prolonged follow-up, including clinical and ophthalmological examination associated with multimodal brain and bone imaging.
References
Cannon PS, Rutherford SA, Richardson PL, King A, Leatherbarrow B (2009) The surgical management and outcomes for spheno-orbital meningiomas: a 7-year review of multi-disciplinary practice. Orbit 28:371–376
Maroon JC, Kennerdell JS, Vidovich DV, Abla A, Sternau L (1994) Recurrent spheno-orbital meningioma. J Neurosurg 80:202–208
Castellano F, Guidetti B, Olivecrona H (1952) Pterional meningiomas en plaque. J Neurosurg 9:188–196
Guiot G, Derome P (1966) Apropos of meningiomas “en plaque” of the pterion. Surgical treatment of hyperostotic osseous meningiomas. Ann Chir 20:1109–1127
Sekhar LN, Babu RP, Wright DC (1994) Surgical resection of cranial base meningiomas. Neurosurg Clin N Am 5:299–330
Taha AN, Erkmen K, Dunn IF, Pravdenkova S, Al-Mefty O (2011) Meningiomas involving the optic canal: pattern of involvement and implications for surgical technique. Neurosurg Focus 30:E12
Franquet N, Pellerin P, Dhellemmes P, Defoort-Dhellemmes S (2009) Ophthalmologic characteristics of spheno-orbital meningiomas: a series of 23 surgical cases. J Fr Ophtalmol 32:16–19
Yasargil MG (1996) Anterior cranial fossa meningiomas, in Yasargil MG (ed): Microneurosurgery. Volume IVB: Microsurgery of CNS tumors. Thieme-Verlag, Stuttgart, pp 141–142
Gaillard S, Lejeune J, Pellerin P, Pertuzon B, Dhellemmes P, Christiaens J (1995) Long-term results of the surgical treatment of spheno-orbital osteomeningioma. Neuro-Chirurgie 41:391–397
Gaillard S, Pellerin P, Dhellemmes P, Pertuzon B, Lejeune JP, Christiaens JL (1997) Strategy of craniofacial reconstruction after resection of spheno-orbital “en plaque” meningiomas. Plast Reconstr Surg 100:1113–1120
Ringel F, Cedzich C, Schramm J (2007) Microsurgical technique and results of a series of 63 spheno-orbital meningiomas. Neurosurgery 60:214
Schick U, Bleyen J, Bani A, Hassler W (2006) Management of meningiomas en plaque of the sphenoid wing. J Neurosurg 104:208–214
Talacchi A, De Carlo A, D’Agostino A, Nocini P (2014) Surgical management of ocular symptoms in spheno-orbital meningiomas. Is orbital reconstruction really necessary? Neurosurg Rev 37:301
Saeed P, van Furth WR, Tanck M, Kooremans F, Freling N, Streekstra GI, Regensburg NI, van der Sprenkel JW, Peerdeman SM, van Overbeeke JJ, Mourits MP (2011) Natural history of spheno-orbital meningiomas. Acta Neurochir (Wein) 153:395–402
Nochez Y, Francois P, Majzoub S, Floch E, Pisella P-J, Jan M, Velut S (2012) Predictive factors for visual outcome after resection of spheno-orbital meningiomas: a long-term review. Acta Ophthalmol 90:5
Honig S, Trantakis C, Frerich B, Sterker I, Schober R, Jr M (2010) Spheno-orbital meningiomas: outcome after microsurgical treatment: a clinical review of 30 cases. Neurol Res 32:314–325
Oya S, Sade B, Lee JH (2011) Sphenoorbital meningioma: surgical technique and outcome. J Neurosurg 114:1241–1249
Nagatani K, Takeuchi S, Otani N, Nawashiro H (2011) Surgical management of spheno-orbital meningiomas. Acta Neurochir (Wein) 153:40
Roser F, Nakamura M, Jacobs C, Vorkapic P, Samii M (2005) Sphenoid wing meningiomas with osseous involvement. Surg Neurol 64:37
Margalit NS, Lesser JB, Moche J, Sen C (2003) Meningiomas involving the optic nerve: technical aspects and outcomes for a series of 50 patients. Neurosurgery 53:523–532, discussion 532–523
Borumandi F, Hammer B, Kamer L, von Arx G (2011) How predictable is exophthalmos reduction in Graves’ orbitopathy? A review of the literature. Br J Ophthalmol 95:1625–1630
Mariniello G, Bonavolontà G, Tranfa F, Maiuri F (2013) Management of the optic canal invasion and visual outcome in spheno-orbital meningiomas. Clin Neurol Neurosurg 115:1615–1620
Lesoin F, Pellerin P, Villette L, Autricque A, Jomin M (1986) Mobilization of the median fronto-orbital band using a monobloc flap. Neuro-Chirurgie 32:161–163
Pellerin P, Lesoin F, Dhellemmes P, Donazzan M, Jomin M (1984) Usefulness of the orbitofrontomalar approach associated with bone reconstruction for frontotemporosphenoid meningiomas. Neurosurgery 15:715–718
Rosenthal G, Ng I, Moscovici S, Lee KK, Lay T, Martin C, Manley GT (2014) Polyetheretherketone implants for the repair of large cranial defects: a 3-center experience. Neurosurgery 75:523–529
Thien A, King NK, Ang BT, Wang E, Ng I (2014) Comparison of Polyetheretherketone and Titanium Cranioplasty after Decompressive Craniectomy. World Neurosurg 83:176–180
Pritz M, Burgett R (2009) Spheno-orbital Reconstruction after Meningioma Resection. Skull Base 19:163–170
DeMonte F, Tabrizi P, Culpepper SA, Suki D, Soparkar CN, Patrinely JR (2002) Ophthalmological outcome after orbital entry during anterior and anterolateral skull base surgery. J Neurosurg 97:851–856
Honig S, Trantakis C, Frerich B, Sterker I, Kortmann RDD, Meixensberger J (2010) Meningiomas involving the sphenoid wing outcome after microsurgical treatment—a clinical review of 73 cases. Central Eur Neurosurg 71:189–198
Aboukais R, Baroncini M, Zairi F, Reyns N, Lejeune J-P (2013) Early postoperative radiotherapy improves progression free survival in patients with grade 2 meningioma. Acta Neurochir (Wein) 155:1385
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
For this type of study formal consent is not required.
Funding
No funding was received for this research.
Rights and permissions
About this article
Cite this article
Leroy, HA., Leroy-Ciocanea, C.I., Baroncini, M. et al. Internal and external spheno-orbital meningioma varieties: different outcomes and prognoses. Acta Neurochir 158, 1587–1596 (2016). https://doi.org/10.1007/s00701-016-2850-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2850-0