Abstract
Background: The increase in the elderly population and life expectancy brings new challenges to RNs. The promotion and empowerment of these people for self-care is an added value in the search for well-being and quality of life, where the RN can intervene effectively.
-
Objective: Identify which RN interventions for empowering the elderly person with mobility impairment and self-care deficit.
-
Methodology: SLR by searching RCTs using the EBSCO Host - Research Databases platform, including the following databases: Academic Search CompIete; Business Source CompIete; CINAHL Plus with Full Text; Cochrane; ERIC; Library, Information Science & Technology Abstracts; MedicLatina; MEDLINE with Full Text; Nursing & Allied Health Collection: Comprehensive; PsychoIogy and Behavioral Sciences CoIIection; RegionaI Business News; SPORTDiscus with Full Text; Teacher Reference Center in the period between 2016 and 2022.
-
Results: A total of 12 studies were found that demonstrate functional gains in the elderly with mobility impairment as a result of rehabilitation interventions or caregiver involvement in the rehabilitation process.
-
Conclusion: The implementation of a functional re-education plan can be effective in promoting functionality and empowering the elderly for self-care. RN interventions comprise conventional therapeutic exercise training, the application of functional electrical stimulation and neuromuscular bands, and the implementation of new technologies in rehabilitation. The caregiver can incorporate the re-education plan without endangering the person.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Aging is characterized as a continuous, dynamic and progressive process of biopsychosocial changes that affect the health status, the level of dependence and autonomy of human beings [1]. The World Health Organization (WHO) defines elderly as any individual aged 60 years or more, however, in more developed countries, an individual aged 65 years or more is considered elderly [2,3,4], including the situation of the population in Portugal [5].
Data from the 2021 Census of the National Institute of Statistics in Portugal reveal that the age group of people aged 65 or older registered a population increase [6], representing 22.1% of the Portuguese population in 2020 [7]. In the 2019–2021 triennium life expectancy at age 65 was estimated for the total Portuguese population to be 19.35 years [8].
However, as people get older, there is an increase in morbidity and disability caused by diseases and injuries, most of which are chronic, with impact on self-care and, consequently, on quality of life [9,10,11].
Data from 2019 reveal that 52.5% of the Portuguese population has difficulties satisfying the Activities of Daily Living (ADLs) and Instrumental Life Activities, compared to 49.7% in the European Union [12].
According to the Regulation of the Specific Competences of the Specialist Nurse in Rehabilitation Nursing [13] in force in Portugal, the Rehabilitation Nurse (RN) develops a functional re-education plan aimed at improving residual functions, maintaining or regaining independence in ADLs, and minimizing the impact of installed disabilities, with a focus on empowering the person and maximizing their functionality.
Given the characteristics of the Portuguese population and the RN’s skills, there was a need to identify RN interventions for empowering the elderly with mobility impairment and a self-care deficit via this systematic literature review (SLR) of randomized controlled trials (RCT).
2 Methodology
This SLR followed the Joanna Briggs Institute (JBI) guidelines [14] and employed the PICO[D] method in formulating the research question, as follows: P - Persons aged 65 or older with mobility impairment; I - Empowerment; C - Self-care deficit; O - RN interventions; D - Randomized controlled trials. The research question “What are the RN interventions for the empowerment of older people with mobility impairment and self-care deficit?” emerged.
During the period of July 2022 a search was conducted on the EBSCO Host - Research Databases platform, selecting the following databases: Academic Search CompIete; Business Source CompIete; CINAHL Plus with Full Text; Cochrane Central Register of Controlled Trials; Cochrane Clinical Answers; Cochrane Database of Systematic Reviews; Cochrane Methodology Register; eBook Collection (EBSCOhost); eBook University Press Collection (EBSCOhost); ERIC; Library, Information Science & Technology Abstracts; MedicLatina; MEDLINE with Full Text; Nursing & Allied Health Collection: Comprehensive; PsychoIogy and Behavioral Sciences CoIIection; RegionaI Business News; SPORTDiscus with Full Text; Teacher Reference Center.
We used the MeSH (Medical Subject Heading) and CINAHL validated descriptors “elderly”, “empowerment”, “mobility”, “randomized control trial”, “rehabilitation nurse” and “self-care deficit”, using the Boolean “AND” and “OR”, resulting in the Boolean phrase [(elderly) AND (mobility) AND (self-care deficit)] AND [(rehabilitation nurs*) OR (nurs*) AND (intervention or program) OR (rehabilitation) OR (empowerment)] AND [(randomi?ed control* trial*) OR (randomi?ed clinical trial*)].
The inclusion criteria were randomized controlled studies with full text available, in English, published between 2016 and 2022, and that answered the research question. The studies should show functional gains in the elderly person resulting from rehabilitation interventions in inpatient or outpatient settings, or from the involvement of caregivers in the rehabilitation process.
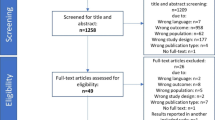
Figure 1 systematizes the methodological path of the research developed through the Prisma Flow Diagram [15].
Prisma Flow Diagram research methodology [15].
The search resulted in a total of 136 articles, which after the elimination of duplicate results resulted in 97 articles for title and abstract analysis. After this analysis 71 articles were eliminated whose theme or methodology did not fit the intended outcome or whose results did not show positive outcomes in this area of intervention, resulting in 26 articles for full text analysis. From this analysis we obtained a total of 12 articles to be included in this review, whose methodological quality assessment [16] and levels of evidence of JBI Critical Appraisal Tools [17] meet more than 50% of the proposed quality criteria. All articles were reviewed by two authors.
This SLR is registered in PROSPERO with ID CRD42022365894.
4 Discussion
The loss of functionality that older people may suffer during or after periods of hospitalization may not only result in loss of independence in ADLs and decreased quality of life, but may also affect the rehabilitation process itself [18,19,20,21].
The introduction of a rehabilitation program, as early as possible, through a multidisciplinary team where the RN is included, is extremely important for older people with mobility impairment and self-care deficit, and has been proven by several authors [20,21,22], namely in two SLRs [20, 21], coexisting gains for individuals, family members and the community.
4.1 Conventional Exercises and Electrical Stimulation
The study by Lee et al. [23] asserts that in people with hemiplegia due to stroke, trunk stability training with selective activation of the abdominal muscles has beneficial effects on abdominal muscles, balance, and mobility. The results of this study are corroborated by other authors [24,25,26,27].
The use of electrical stimulation has also been tested. In the rehabilitation of people with foot drop due to stroke, Sharif et al. [28] proved that gait training with functional electrical stimulation produces greater gains in mobility, balance, gait performance and reduction of spasticity, when compared to muscular electrical stimulation. There are more studies solidifying the gains from the use of electrical stimulation, such as the study by Tan et al. [29] that demonstrates the efficacy of gait training and the study by Stein et al. [30] that validates the use of neuromuscular electrical stimulation in improving specificity and range of motion in people with stroke. On the other hand, Fossat et al. [31] point out that electrical stimulation of the quadriceps muscles, associated with early exercise practice with a cycloergometer and standardized rehabilitation, does not show benefits when compared to standardized rehabilitation practice alone.
The RSL conducted by Martínez-Velilla et al. [20] advocates that people should initiate short periods of walking while still in hospital, using auxiliary devices, which is corroborated by the study of Gazineo et al. [32], concluding that, in hospitalized people, an individualized assisted walking program improves the ability to walk at discharge.
In a study by Dong et al. [33], a strategy to increase activity levels in the older population with mobility impairment, namely after stroke, leading to a promotion of their functional independence, is the use of accelerometers during gait, recording the activity performed. The feedback from this instrument can serve as a stimulus (maintain activity, promote motivation and increase self-efficacy). Peel et al. [34] validated that providing participants and professionals with daily accelerometer walking times leads to an increase in average daily walking time. In contrast, in the study by Atkins et al. [35], when testing the pedometer as a motivational tool, they concluded that it does not improve functional mobility if no goals are set, although an increase in daily time in the orthostatic position was observed.
Raymond et al. [36] state that high intensity functional exercise in conjunction with individual physiotherapy sessions produces a similar effect to individual physiotherapy alone, with the benefit that group physiotherapy sessions result in greater practitioner efficiency, as they save 31 to 205 min per week. This is consistent with research by Sunde et al. [37], who found that a group exercise program led by a rehabilitation professional significantly improves functional capacity and quality of life compared with a home exercise program in older adults with, or at risk for, mobility impairment.
4.2 Application of Neuromuscular Taping
In the field of rehabilitation of the person with musculoskeletal changes, Donec and Kubilius [38] evaluated the effectiveness of neuromuscular bands (Kinesio Taping®). The intervention did not produce better results in mobility and functional improvement, compared to nonspecific knee banding. However, it did have better results on a subjective, participant-reported assessment for symptom alleviation and increased mobility experienced. The intervention had already been tested by other authors who achieved a similar result [39,40,41].
Also, Donec and Kriščiūnas [42] stated that the use of neuromuscular bands may be beneficial in reducing postoperative pain and edema, improving knee joint extension, in the early postoperative rehabilitation period of total knee arthroplasty.
In an RSL with a meta-analysis of ERC performed by Wang et al. [43], the use of the Kinesio Taping® method demonstrated benefits in lower limb rehabilitation of people with stroke, significantly improving spasticity, motor function, balance, gait ability and quality, and ADLs. However, the authors suggest further studies to identify the benefits of neuromuscular taping, due to the limited number of articles selected and the quality of the research performed.
4.3 New Technologies
The study by van den Berg et al. [44] proved that the addition of interactive video/computer-based exercises to geriatric and neurological rehabilitation of hospitalized persons induces task-specific improvements in balance, but not in mobility in general. However, Cannell et al. [45] demonstrated no significant differences in stroke patients’ rehabilitation with the use of virtual reality with gesture controlled interactive video and Li et al. [46] corroborated these results by demonstrating that the use of an app supported exercise program (mHealth) can facilitate supplemental exercise, but does not directly affect functionality outcomes compared to traditional rehabilitation programs.
Recently, Hassett et al. [47] implemented a study and contrary to previous studies, there was an improvement in mobility in the intervention group, but the time spent in the orthostatic position did not change.
Piau et al. [48] demonstrated the feasibility and acceptability of the use of a robotic walking aid (SafeWalker®), from the perspective of participants and professionals, in the context of older people with a severe fear of falling.
Homonymous hemianopia after stroke is equally impactful for independence and insertion in the community for the elderly population, some authors [49, 50] argue that these people have reduced independence and a lower quality of life when compared to people with other visual deficits [49].
Crotty et al. [49] proved that a standardized intervention using scanning techniques, using NVT scanning equipment, which allows training a set of visual enhancement techniques and mobility training, improves quality of life, when compared to usual individualized rehabilitation care.
4.4 Caregiver Involvement
Taking into account the limitations that rehabilitation units have to meet all the needs of the population, the importance of informal caregivers in the process of rehabilitation at home of older people, reaching out similar results in terms of effectiveness, freeing the elderly and their caregivers from traveling to rehabilitation units [51, 52].
Zhou et al. [53], found no benefit in caregiver empowerment as they tested a complex intervention in the rehabilitation of people with stroke that combined caregiver empowerment through a cell phone application with teachings/training during the hospital stay focusing on mobility and self-care. In parallel, Chu et al. [54], conducted another intervention study in stroke survivors focusing on mobility, self-care, and toilet use. This study concluded that the new rehabilitation model implemented by nurses and practiced by family members improved physical recovery, as evidenced by Barthel Index values, without increasing caregiver burden, compared to usual care.
Jarbandhan and his collaborators [55] certify this statement, proving that the rehabilitation care provided at home and through tele-rehabilitation, promotes better results in functional independence, when compared to general care. They also present a better cost-benefit ratio compared to rehabilitation care in hospital rehabilitation units.
5 Conclusion
The scientific evidence on the RN intervention for the empowerment of the elderly person with mobility impairment and self-care deficit is still limited. The need to develop evidence-based practice is urgent, and the consequent publication of these studies is an added value in the promotion and visibility of RN interventions within this theme.
From the analysis performed, all studies showed gains resulting from rehabilitation interventions in older people with mobility impairments, highlighting conventional exercises and electrical stimulation, neuromuscular banding, new technologies, and caregiver involvement in rehabilitation care.
To contribute to increasing the mobility and functionality of the elderly is to contribute to their empowerment for self-care, improvement of quality of life, relationships with family members, the community, and society in general.
References
Organização Mundial da Saúde: Relatório Mundial sobre Envelhecimento e Saúde - Resumo (2015)
Marques-Vieira, C., Amaral, T., Pontífice-Sousa, P.: Contributos para um En-velhecimento Ativo. Em: Marques-Vieira, C. e Sousa, L. (eds.) Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida, pp. 525–534. Lusodi-dacta, Loures (2017)
Organização Mundial da Saúde: Decade of Healthy Ageing Baseline Report Summary (2021)
Organização Mundial de Saúde: Active Ageing: A Policy Framework. Organização Mundial da Saúde (2002)
Instituto Nacional de Estatística: Estatísticas Demográficas - 2019. Lisboa (2020)
Instituto Nacional de Estatística: População residente (N.o) por Local de residên-cia (à data dos Censos 2021), Sexo e Grupo etário. https://tabulador.ine.pt/in-dicador/?id=0011609
Comissão Europeia: Estado da Saúde na UE. Portugal. Perfil de saúde do país 2021. (2021)
Instituto Nacional de Estatística: Esperança de vida de 80,72 anos à nascença e de 19,35 anos aos 65 anos - 2019–2021. https://www.ine.pt/xpor-tal/xmain?xpid=INE&xpgid=ine_destaques&DESTAQUESdest_boui=540806507&DESTAQUESmodo=2
Fonseca, C.: Modelo de Autocuidado Para Pessoas com 65 e Mais Anos de Idade, Necessidades de Cuidados de Enfermagem. Tese de Doutoramento (2014)
DGS. Direção de Serviços de Informação e Análise: A Saúde dos Portugueses 2016. Direção Geral da Saúde (2017)
Tomey, A.M., Alligood, M.R.: Teóricas de Enfermagem e a sua Obra (Modelos e Teorias de Enfermagem). Lusociência, Loures (2004)
Eurostat: Dificuldades em atividades de cuidados pessoais ou atividades do-mésticas por sexo, idade e nível de escolaridade. https://ec.europa.eu/euro-stat/data-browser/view/HLTH_EHIS_TAE/default/table?lang=en&category=hlth.hlth_state.hlth_fal
Regulamento n.o 392/2019: Regulamento das Competências Específicas do Enfermeiro Especialista em Enfermagem de Reabilitação (2019)
Aromataris, E., Munn, Z.: JBI Manual for Evidence Synthesis. JBI (2020)
Page, M.J., et al.: The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. n71 (2021). https://doi.org/10.1136/bmj.n71
Tufanaru, C., Munn, Z., Aromataris, E., Campbell, J., Hopp, L.: Chapter 3: systematic reviews of effectiveness. In: Em: Aromataris, E. e Munn, Z. (eds.) JBI Manual for Evidence Synthesis, pp. 71–133. JBI (2020)
Joanna Briggs Institute: Ovid Database Guide. https://ospguides.ovid.com/OSPguides/jbidb.htm
Said, C.M., et al.: Factors associated with improved walking in older people during hospital rehabilitation: secondary analysis of a randomized controlled trial. BMC Geriatr. 21, 90 (2021). https://doi.org/10.1186/s12877-021-02016-0
Turunen, K., et al.: A tailored counseling and home-based rehabilitation program to increase physical activity and improve mobility among community-dwelling older people after hospitalization: protocol of a randomized controlled trial. BMC Musculoskelet. Disord. 18, 477 (2017). https://doi.org/10.1186/s12891-017-1825-5
Martínez-Velilla, N., Cadore, E.L., Casas-Herrero, Á., Idoate-Saralegui, F., Izquierdo, M.: Physical activity and early rehabilitation in hospitalized elderly medical patients: systematic review of randomized clinical trials. J. Nutr. Health Aging 20(7), 738–751 (2016). https://doi.org/10.1007/s12603-016-0683-4
Lopes, M.J., Silva, C., Nunes, I., Pimenta, E., Seromenho, V.: Sensitive Indicators for Rehabilitation Nursing Care in Older Persons with Mobility Impairment Through a Rehabilitation Program: A Systematic Literature Review. Em: García-Alonso, J., e Fonseca, C., (eds.) Gerontechnology IV, pp. 158–170. Springer (2022)
Garlet, A.B., Plentz, R.D.M., Blauth, A.H.E.G., Righi, T.T., Righi, N.C., Schar-dong, J.: Reabilitação Robótica em Pacientes com AVC: Protocolo de Ensaio Clínico Randomizado. Fisioter. e Pesqui. 28, 483–490 (2021). https://doi.org/10.1590/1809-2950/21020028042021
Lee, J., Jeon, J., Lee, D., Hong, J., Yu, J., Kim, J.: Effect of trunk stabilization exercise on abdominal muscle thickness, balance and gait abilities of patients with hemiplegic stroke: a randomized controlled trial. NeuroRehabilitation 47, 435–442 (2020). https://doi.org/10.3233/NRE-203133
Karthikbabu, S., et al.: Comparison of physio ball and plinth trunk exercises regimens on trunk control and functional balance in patients with acute stroke: a pilot randomized controlled trial. Clin. Rehabil. 25, 709–719 (2011). https://doi.org/10.1177/0269215510397393
Mew, R.: Comparison of changes in abdominal muscle thickness between standing and crook lying during active abdominal hollowing using ultra-sound imaging. Man. Ther. 14, 690–695 (2009). https://doi.org/10.1016/j.math.2009.05.003
Suehiro, T., Mizutani, M., Watanabe, S., Ishida, H., Kobara, K., Osaka, H.: Comparison of spine motion and trunk muscle activity between abdominal hollowing and abdominal bracing maneuvers during prone hip extension. J. Bodyw. Mov. Ther. 18, 482–488 (2014). https://doi.org/10.1016/j.jbmt.2014.04.012
Teyhen, D.S., et al.: The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J. Orthop. Sport. Phys. Ther. 35, 346–355 (2005). https://doi.org/10.2519/jospt.2005.35.6.346
Sharif, F., Ghulam, S., Malik, A.N., Saeed, Q.: Effectiveness of functional electrical stimulation (FES) versus conventional electrical stimulation in gait re-habilitation of patients with stroke. J. Coll. Phys. Surg. Pak. 27, 703–706 (2017)
Tan, Z.M., Jiang, W.W., Yan, T.B., Wu, W., Song, R.: Effects of functional electrical stimulation based on normal gait pattern on walking function in subjects with recovery of stroke. Zhonghua Yi Xue Za Zhi 96, 2342–2346 (2016). https://doi.org/10.3760/cma.j.issn.0376-2491.2016.29.012
Stein, C., Fritsch, C.G., Robinson, C., Sbruzzi, G., Plentz, R.D.M.: Effects of electrical stimulation in spastic muscles after stroke. Stroke 46, 2197–2205 (2015). https://doi.org/10.1161/STROKEAHA.115.009633
Fossat, G., et al.: Effect of in-bed leg cycling and electrical stimulation of the quadriceps on global muscle strength in critically III adults. JAMA 320, 368 (2018). https://doi.org/10.1001/jama.2018.9592
Gazineo, D., et al.: Assisted walking program on walking ability in in-hospital geriatric patients: a randomized trial. J. Am. Geriatr. Soc. 69, 637–643 (2021). https://doi.org/10.1111/jgs.16922
Dong, Y., et al.: Does feedback on daily activity level from a smart watch during inpatient stroke rehabilitation increase physical activity levels? study protocol for a randomized controlled trial. Trials 19, 177 (2018). https://doi.org/10.1186/s13063-018-2476-z
Peel, N.M., Paul, S.K., Cameron, I.D., Crotty, M., Kurrle, S.E., Gray, L.C.: Promoting activity in geriatric rehabilitation: a randomized controlled trial of accelerometry. PLoS ONE 11, e0160906 (2016). https://doi.org/10.1371/jour-nal.pone.0160906
Atkins, A., Cannell, J., Barr, C.: Pedometers alone do not increase mobility in inpatient rehabilitation: a randomized controlled trial. Clin. Rehabil. 33, 1382–1390 (2019). https://doi.org/10.1177/0269215519838312
Raymond, M.J.M., Jeffs, K.J., Winter, A., Soh, S.-E., Hunter, P., Holland, A.E.: The effects of a high-intensity functional exercise group on clinical outcomes in hospitalised older adults: an assessor-blinded. Randomised-Controlled Trial. Age Ageing. 46, 208–213 (2017). https://doi.org/10.1093/ageing/afw215
Sunde, S., et al.: Effects of a multicomponent high intensity exercise program on physical function and health-related quality of life in older adults with or at risk of mobility disability after discharge from hospital: a randomised controlled trial. BMC Geriatr. 20, 464 (2020). https://doi.org/10.1186/s12877-020-01829-9
Donec, V., Kubilius, R.: The effectiveness of kinesio taping ® for mobility and functioning improvement in knee osteoarthritis: a randomized, double-blind. Controlled Trial. Clin. Rehabil. 34, 877–889 (2020). https://doi.org/10.1177/0269215520916859
Wageck, B., Nunes, G.S., Bohlen, N.B., Santos, G.M., de Noronha, M.: Kinesio taping does not improve the symptoms or function of older people with knee osteoarthritis: a randomised trial. J. Physiother. 62, 153–158 (2016). https://doi.org/10.1016/j.jphys.2016.05.012
Kaya Mutlu, E., Mustafaoglu, R., Birinci, T., Razak Ozdincler, A.: Does Kinesio taping of the knee improve pain and functionality in patients with knee oste-oarthritis? Am. J. Phys. Med. Rehabil. 96, 25–33 (2017). https://doi.org/10.1097/PHM.0000000000000520
Kocyigit, F., et al.: Kinesio taping or sham taping in knee osteoarthritis? a randomized, double-blind. Sham-controlled Trial. Complement. Ther. Clin. Pract. 21, 262–267 (2015). https://doi.org/10.1016/j.ctcp.2015.10.001
Donec, V., Kriščiūnas, A.: The effectiveness of Kinesio taping after total knee replacement in early postoperative rehabilitation period. a randomized controlled trial. Eur. J. Phys. Rehabil. Med. 50, 363–371 (2014)
Wang, M., Pei, Z., Xiong, B., Meng, X., Chen, X., Liao, W.: Use of Kinesio taping in lower-extremity rehabilitation of post-stroke patients: a systematic review and meta-analysis. Complement. Ther. Clin. Pract. 35, 22–32 (2019). https://doi.org/10.1016/j.ctcp.2019.01.008
van den Berg, M., et al.: Video and computer-based interactive exercises are safe and improve task-specific balance in geriatric and neurological rehabilitation: a randomised trial. J. Physiother. 62, 20–28 (2016). https://doi.org/10.1016/j.jphys.2015.11.005
Cannell, J., et al.: The efficacy of interactive, motion capture-based rehabilitation on functional outcomes in an inpatient stroke population: a randomized controlled trial. Clin. Rehabil. 32, 191–200 (2018)
Li, I., Bui, T., Phan, H.T., Llado, A., King, C., Scrivener, K.: App-based supplemental exercise in rehabilitation, adherence, and effect on outcomes: a randomized controlled trial. Clin. Rehabil. 34, 1083–1093 (2020). https://doi.org/10.1177/0269215520928119
Hassett, L., et al.: Digitally enabled aged care and neurological rehabilitation to enhance outcomes with activity and mobility using technology (AMOUNT) in Australia: a randomised controlled trial. PLOS Med. 17, e1003029 (2020). https://doi.org/10.1371/jour-nal.pmed.1003029
Piau, A., Krams, T., Voisin, T., Lepage, B., Nourhashemi, F.: Use of a robotic walking aid in rehabilitation to reduce fear of falling is feasible and acceptable from the end user’s perspective: a randomised comparative study. Maturitas 120, 40–46 (2019). https://doi.org/10.1016/j.maturitas.2018.11.008
Crotty, M., van den Berg, M., Hayes, A., Chen, C., Lange, K., George, S.: Hemianopia after stroke: a randomized controlled trial of the effectiveness of a standardised versus an individualized rehabilitation program, on scanning ability whilst walking. NeuroRehabilitation 43, 201–209 (2018). https://doi.org/10.3233/NRE-172377
Sand, K.M., Midelfart, A., Thomassen, L., Melms, A., Wilhelm, H., Hoff, J.M.: Visual impairment in stroke patients - a review. Acta Neurol. Scand. 127, 52–56 (2013). https://doi.org/10.1111/ane.12050
Nordin, N.A.M., Aziz, N.A., Sulong, S., Aljunid, S.M.: Effectiveness of home-based carer-assisted in comparison to hospital-based therapist-delivered therapy for people with stroke: a randomised controlled trial. NeuroRehabilitation 45, 87–97 (2019). https://doi.org/10.3233/NRE-192758
Fonseca, C., de Pinho, L.G., Lopes, M.J., Marques, M.D.C., Garcia-Alonso, J.: The elderly nursing core set and the cognition of Portuguese older adults: a cross-sectional study. BMC Nurs. 20(1), 1–8 (2021). https://doi.org/10.1186/s12912-021-00623-1
Zhou, B., et al.: Caregiver-delivered stroke rehabilitation in rural China. Stroke 50, 1825–1830 (2019). https://doi.org/10.1161/STROKEAHA.118.021558
Chu, K., et al.: Feasibility of a nurse-trained, family member-delivered rehabilitation model for disabled stroke patients in rural chongqing. China. J. Stroke Cerebrovasc. Dis. 29, 105382 (2020). https://doi.org/10.1016/j.jstrokecerebro-vasdis.2020.105382
Jarbandhan, A., Toelsie, J., Veeger, D., Bipat, R., Vanhees, L., Buys, R.: Feasibility of a home-based physiotherapy intervention to promote post-stroke mobility: a randomized controlled pilot study. PLoS ONE 17, e0256455 (2022). https://doi.org/10.1371/journal.pone.0256455
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Costa, T., Lopes, M., Bia, F. (2023). The Rehabilitation Nurse and the Empowerment of Older Adults with Mobility Impairment and Self-care Deficits: A Systematic Literature Review. In: Moguel, E., de Pinho, L.G., Fonseca, C. (eds) Gerontechnology V. IWoG 2022. Lecture Notes in Bioengineering. Springer, Cham. https://doi.org/10.1007/978-3-031-29067-1_32
Download citation
DOI: https://doi.org/10.1007/978-3-031-29067-1_32
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-29066-4
Online ISBN: 978-3-031-29067-1
eBook Packages: MedicineMedicine (R0)