Abstract
Acute respiratory failure (ARF) is a common complication following hematopoietic stem cell transplant (HSCT). Despite improvements in mortality over time, intensive care unit (ICU) and in-hospital mortality remains higher than the oncology and non-oncology cohorts. The approach to supportive care management surrounding respiratory support often is extrapolated from the non-oncology cohort. However, the unique pathophysiology behind the cause of ARF warrants dedicated research to be focused on this cohort independently of the general population. In this chapter, we review the evidence surrounding noninvasive respiratory support and invasive mechanical ventilation for critically ill hematopoietic stem cell transplant recipients with ARF.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute respiratory failure
- Invasive mechanical ventilation
- Noninvasive mechanical ventilation
- High-flow nasal cannula
Introduction
Owing to advancements in oncology and critical care, the outcomes of acute respiratory failure (ARF) among cancer patients have improved significantly over the last three decades [1,2,3,4]. However, patients with cancer have a higher mortality rate than non-cancer cohorts (50–60% vs. 30–40%) in the setting of mechanical ventilation [2, 3, 5]. In more recent years, intensive care unit (ICU) mortality has continued to decrease steadily for most subtypes of cancer; however, in recent years, mortality across patients receiving hematopoietic stem cell transplant (HSCT) (specifically allogeneic) has plateaued [4].
Compared to other hematological malignant (HM) conditions and most other cancers, the HSCT population experiences a higher frequency of ARF necessitating ICU admission [6,7,8]. Approximately 25% of HSCT patients require an ICU admission within 1 year of procedure [1, 9]. The predominant cause of critical illness remains ARF. ICU mortality in this population in the setting of ARF ranges from 50% to 70%. Higher mortality rates are often related to the presence of invasive fungal infections or indeterminant ARF [10,11,12,13,14,15,16]. This high mortality rate is in contrast to 32% ARF mortality in the general population requiring ventilation [17] and 56% in an immunocompromised population requiring ventilation [18]. It remains unclear whether the higher mortality is predominantly due to (1) patient factors (e.g., greater propensity for frailty), (2) disease factors (e.g., higher severity of illness/more challenging organisms), (3) physician factors (e.g., preconceived perception of poor prognosis driving end-of-life conversations), (4) difference in mechanical ventilation practices (e.g., use of noninvasive devices), or (5) pathophysiologic differences in ARF.
This chapter will focus on respiratory support for the HSCT population in the setting of ARF. It is important to highlight that determining the cause of ARF through a safe and precise approach is possibly one of the most important principles in managing these patients as delays in diagnosis or indeterminant ARF carries a high mortality rate for this population [19,20,21].
Features of Pulmonary Complications Following HSCT
There are distinct immunologic states that occur post-HSCT that render patients susceptible to specific etiologies of ARF following transplant (see Chap. 3). The differential for causes of ARF is vast with infectious and noninfectious causes occasionally occurring simultaneously. Knowing the timeline following transplant, prophylactic therapy received, type of immunosuppression, and duration of immunosuppression is imperative to inform investigative workup and approach to empiric therapy in the setting of severe illness. An early (0–100 days post-HSCT) and late (roughly beyond 100 days) timeline can be used to approach the etiology. Early can be categorized as pre-engraftment (first 30 days), peri-engraftment (within 7 days of engraftment), and early post-engraftment (30–100 days) [15, 22]. In a recent cohort study that assessed post-HSCT ARF in the first year, 65% were identified as severe, and 69% occurred in the first 100 days following the transplant. Occasionally, ARF can progress to the more severe form known as acute respiratory distress syndrome (ARDS). ARDS, as a syndrome, is intended to identify a process that results in diffuse alveolar damage. Neutrophil activation is a core process in ARDS; however, despite neutropenia, ARDS is known to occur in the HSCT population. More research is needed to inform whether the process of ARDS is similar in the general population compared to the HSCT cohort. This is imperative to informing support ventilatory care and best ICU practices for this population.
Noninvasive and Invasive Respiratory Support
The goal of respiratory support is to improve patient’s oxygenation, decrease respiratory work of breathing, and reverse any ventilation impairment. Respiratory support measures could be roughly divided into two categories: noninvasive respiratory support and invasive mechanical ventilation. Noninvasive devices may include high-flow nasal cannula (HFNC), continuous positive airway pressure (CPAP), and noninvasive mechanical ventilation (NIV).
The decision between noninvasive ventilation and upfront invasive mechanical ventilation (IMV) involves balancing the risks associated with coupling a patient to a ventilator and ventilator-associated lung injury against the risk of prolonged exposure to potentially injurious spontaneous breathing under a noninvasive strategy. Deciding between noninvasive and invasive may also be governed by the need for more invasive procedures that can be more safely executed under invasive mechanical ventilatory settings.
Noninvasive Respiratory Support
HFNC uses a heated and humidified gas, providing a wide range of FiO2 (0.21–1) and maximum flow up to 60–80 L/min. The high flows help minimize dilution of ambient air to ensure that the intended oxygen is delivered to the alveoli. An additional benefit is the creation of a low positive end expiratory pressure (PEEP), mucociliary clearance given the humidification, CO2 washout from the upper airways, ease of use, and patient comfort [23]. CPAP and NIV use positive pressure ventilation through a tight-fitting face mask (oronasal or total face) or a helmet (plastic hood that is secured on the neck). Modes that are mainly used are continuous positive airway pressure (CPAP only), or pressure support (PS) ventilation in addition to CPAP, often termed bilevel positive airway pressure (BiPAP).
Historically, invasive mechanical ventilation in immunocompromised patients was associated with high mortality and was considered an unfavorable approach that should be avoided [24,25,26,27]. Given that historic trials demonstrated reduced need for intubation and mortality with an upfront approach of noninvasive ventilation, guideline recommendations suggested the use of noninvasive devices for this population. In a secondary analysis of a large epidemiologic study of ARDS, upfront NIV was used at a higher frequency in immunocompromised patients compared to non-immunocompromised patients [18]. However, subsequent evidence reflecting contemporary IMV and critical care practices have not shown the same benefit of NIV in this population.
Non-immunocompromised Patient Population
Outside of the immunocompromised population, there has been a surge of evidence evaluating the comparative effectiveness of different noninvasive respiratory devices. A series of systematic reviews and meta-analyses have demonstrated that HFNC and NIV decrease the risks of intubation compared to standard oxygen therapies. In a comparative evaluation of HFNC, face mask NIV, and standard oxygen therapies, HFNC decreased the need for intubation in more severely hypoxemic patients and decreased 90-day mortality compared to face mask NIV and standard oxygen therapy [23]. Patients under NIV with a high tidal volume 1 h after initiation of NIV or more severely hypoxemic patients (PaO2/FiO2 < 200 mmHg) were more likely to be intubated. Patients with high tidal volumes on NIV had a higher mortality rate compared to the other modes. These findings, in general, raised enthusiasm for the use of HFNC and concern surrounding the use of NIV.
Immunocompromised Patient Population
The EFRAIM study assessed 1611 immunocompromised patients with ARF and the initial approach of respiratory support [19]. The study evaluated the association between initial oxygen modality and need for IMV and in-hospital all-cause mortality. Among these patients, 54.9% were HM, 6.7% were post-auto-HSCT, and 9.7% were post-allo-HSCT. Factors that were associated with IMV included age, day-1 severity of illness, day-1 PaO2/FiO2, and ARF etiology (Pneumocystis jirovecii pneumonia, invasive pulmonary aspergillosis, and undetermined etiology). Factors that were associated with increased in-hospital mortality were age, indirect admission to the ICU, day-1 severity of illness, PaO2/FiO2 < 100, and indeterminate ARF etiology. Initial oxygen strategy was not associated with mortality [19].
Utility of face mask NIV and HFNC has been specifically evaluated across the general immunocompromised patient population. In a multicenter randomized controlled study (INVICTUS trial), the outcome of early face mask NIV vs. standard oxygen therapy in 374 critically ill immunocompromised patients with ARF did not reduce 28-day mortality, nor did it show any significant benefit for other secondary outcomes (need for intubation, severity of illness at day 3 of ICU admission, ICU-acquired infections, duration of mechanical ventilation, and ICU length of stay) [28].
Contemporary studies have further demonstrated that the frequency of face mask NIV failure is not uncommon, particularly across higher severities of illness as well as in patients with hematologic malignancies [28]. Furthermore, face mask NIV failure is associated with poor outcomes [19, 29]. In the large epidemiologic study of ARDS (LUNG SAFE study), upfront NIV was used in 15% of cases. NIV use was not restricted to primarily mild ARDS and was seen across all severities of ARDS: 22.2% of mild, 42.3% of moderate, and 47.1% of patients with severe ARDS. Increasing ARDS severity was associated with an increased incidence of NIV failure. Hospital mortality in patients with NIV success and failure was 16.1% and 45.4%, respectively. In a propensity score-matched analysis, ICU mortality was higher in patients who received upfront NIV compared to invasively ventilated patients with a PaO2/FiO2 lower than 150 mmHg [30]. A secondary analysis of this study focused on immunocompromised patients demonstrated that NIV was used more frequently as first-line respiratory support compared to the immunocompetent population [18]. While there may be a role for NIV in less-severe ARF, its routine role as first-line therapy for immunocompromised (and non-immunocompromised) patients has been called into question.
HFNC as compared to standard oxygen therapy was evaluated in a trial across 778 immunocompromised patients with ARF (the HIGH trial) [31]. Forty-five percent (348/778) of patients had an underlying hematologic malignancy with 48 auto-HSCT and 61 allo-HSCT. In this population, HFNC was not found to significantly decrease intubation or 28-day mortality [31]. Finally, a more recent trial by Coudroy et al. comparing face mask NIV to HFNC across 300 immunocompromised patients with ARF did not show any differences in 28-day mortality between HFNC and NIV alternating with HFNC.
Placing Research into Context for the HSCT Patient Population
The current state of the literature does not definitively recommend one noninvasive oxygen strategy over another across immunocompromised patients. It is likely that there is not a one-size-fits-all approach to noninvasive respiratory support across patients (HSCT, immunocompromised nor immunocompetent). Different respiratory phenotypes likely exist and need to be tailored to individual patients. Currently, these phenotypes have not been defined, but future research should be dedicated to evaluating these. It may also be discovered that the clusters of phenotypes transverse the historic “immunocompromised vs. non-immunocompromised” categorization and even “hematologic oncology vs. solid tumor.” Evidence to date has demonstrated certain risk factors more likely to be associated with noninvasive respiratory failure (particularly centered around face mask NIV but not specific to the HSCT or immunocompromised population).
Higher severity of ARF (i.e., PaO2/FiO2 < 150–200 mmHg), number of organs failed, and large tidal volumes 1 h after initiation have been found to be associated with face mask NIV failure and higher risk of death. The HACOR score is a composite score that considers heart rate, pH, level of consciousness, severity of hypoxemia, and respiratory rate, and when measured 1 h after NIV treatment, it may predict the need for intubation [32].
For HFNC, the ROX index (SaO2/FiO2/respiratory rate (RR)) was a tool validated to predict HFNC failure leading to IMV across patients with pneumonia [33]. As delayed intubation by using HFNC may be associated with higher mortality [34], it is of interest to develop a decision-making supporting tool to predict high risk of HFNC failure. The ROX index (SpO2/FiO2/RR) found that a score over 4.88 within 2–12 h of starting HFNC is associated with a lower risk of intubation (area under the curve [AUC] of the receiver operating characteristic [ROC] curve in the validation cohort was 0.703 [0.616–0.790] at 6 h and 0.752 [0.664–0.840] at 12 h) [33, 35]. The ROX index performance was also evaluated in immunocompromised patients and found a score of 4.88 still highly associated with HFNC failure and need for intubation but with poorer accuracy and predictability (AUC = 0.623) [36].
Spontaneous breathing may have beneficial physiological effects; however, an emerging area of interest surrounds the potential harm associated with spontaneous breathing. Large swings in intrathoracic pressure with vigorous breathing may also be injurious to the lungs. This concept has been labeled patient self-inflicted lung injury and is becoming increasingly recognized as a potential contributor to noninvasive respiratory support failure and/or mortality [37]. Ultimately, patients with an ARF trajectory that is about to peak/plateau and recover are likely the ones who would most benefit from noninvasive respiratory support compared to those who are still on their trajectory of worsening. Accurately identifying this cohort has not yet been accomplished; however, patients with more protracted ARF may be less likely to benefit from an upfront noninvasive device. Additional considerations specific to the HSCT population surround the need for invasive investigations to identify the cause of ARF for treatment to be tailored. In cases of diagnostic uncertainty, noninvasive techniques may lead to delays in diagnostic measures [19]. If bronchoscopy or computed tomography (CT) scans are necessary for the diagnostic workup and cannot safely be performed under noninvasive respiratory support due to hypoxemia risk, transitioning to IMV may be necessary to both support the patient and facilitate these investigations.
Future Role of Noninvasive Respiratory Support
In addition to accurately identifying sub-phenotypes, matching noninvasive devices to these phenotypes, predicting trajectory of ARF, and better describing how to measure patient self-inflicted lung injury, new noninvasive devices are currently under evaluation with promising preliminary data. One of the greatest challenges with face mask NIV is patient tolerance. Helmet is a unique interface that can couple a patient noninvasively to NIV or CPAP using a transparent plastic hood. An exploratory trial evaluating helmet NIV compared to face mask NIV demonstrated improved mortality with the helmet interface [38]. The authors theorized that the mortality benefit might have been attributable to more effective PEEP application and tolerability with helmet compared to face mask. A network meta-analysis evaluated 25 trials comparing four different oxygen modalities (HFNC, face mask NIV/CPAP, helmet NIV/CPAP, or standard oxygen therapy). Helmet NIV (and face mask NIV) reduced intubation and mortality compared to the other modalities; however, this mortality benefit was no longer true with face mask NIV across patients with more severe ARF (studies with PaO2/FiO2 < 200 mmHg) [39]. The HENIVOT study was a multicenter randomized clinical trial that randomized 109 patients with COVID-19 and moderate to severe ARF to helmet ventilation for at least 48 h eventually followed by high-flow nasal oxygen (n = 54) or high-flow oxygen alone (n = 55). The median days free of respiratory support within 28 days were not significantly different between groups (primary outcome). The helmet group had significantly lower rate of endotracheal intubations and higher rate of days free of invasive mechanical ventilation within 28 days [40]. The option of helmet ventilation may offer some advantages in immunocompromised patients, but evidence is still lacking. Currently, there are a series of ongoing trials evaluating helmet compared to other modalities, and its role in immunocompromised, cancer, and HSCT patients has yet to be reported.
Palliative Use of Noninvasive Respiratory Support
Noninvasive devices also serve the purpose of buying time for decision-making about escalating to IMV. Furthermore, an important aspect of HFNC specifically is its potential role in palliative care as it provides comfort and ease of use [41, 42].
Invasive Mechanical Ventilation
Despite being a unique population, with distinct causes and mechanisms of severe respiratory failure pathophysiology, general ARDS categorization, prognostication, and management are currently generalized to the HSCT population [43]. However, as we better understand respiratory phenotypes, mechanisms of ARF across neutropenic/non-neutropenic patients, and their impact on respiratory physiology, our management may become more precisely tailored to the unique features of the specific patient. This is particularly important for patients with HSCT given the very heterogeneous causes of ARF that can develop post-transplant.
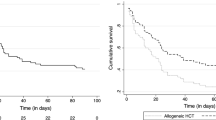
In a secondary analysis of the EFRAIM study evaluating the cohort that fulfilled criteria for ARDS, 52% were HM patients, 7% and 10% allo-HSCT and auto-HSCT [44]. ARDS of undetermined etiology, need for vasopressors, and need for renal replacement therapy were independently associated with hospital mortality. Higher plateau pressures (Pplat), higher driving pressures (∆Prs), and lower compliance (Crs) were associated with higher mortality. Interestingly, ARDS severity according to the Berlin definition, neutropenia on admission, and the type of underlying disease were not associated with mortality. These findings highlight the importance of striving for a sound diagnosis and the importance of implementing lung protective ventilation strategy in all critical care patients including in immunocompromised patients [44]. Interestingly, the lack of association between ARDS severities and outcome highlights the need for tailored evaluation of ARDS categorization in this cohort. More specifically, an observational study of HSCT patients with ARF reported contemporary outcomes in the setting of IMV [12]. Seventy patients from two centers, who needed IMV within 90 days of HSCT, were evaluated. ICU mortality was 63%, and 90-day mortality was 73%. Mortality was higher in patients who required a longer duration of MV with 76% mortality for those requiring MV over 14 days and 91% mortality for those requiring MV for more than 21 days. Most of the patients were intubated within 30 days of the HSCT, emphasizing the vulnerability of these patients in the pre- and peri-engraftment phases. Allo-HSCT (OR = 11.3), higher illness severity, and longer interval between HSCT and MV were found to be independently associated with higher all-cause mortality at 90 days. This study reflects persistent poor outcomes seen in the setting of IMV despite contemporary ICU practices across HSCT recipients and in particular across allo-HSCT patients.
Above all, a question that remains surrounds whether higher mortality in patients treated with IMV has a causal relation or is merely a consequence of a higher burden of disease and multiorgan involvement [16]. Once decision has been made to intubate and to proceed with IMV, the principles of “lung protective ventilation” should be followed to minimize the risk of ventilator-induced lung injury (VILI) [45,46,47,48,49] along with the emphasis on meticulous care and efforts to prevent additional complications that would act as a “second hit” such as preventing fluid overload and restriction of blood products, decreasing the risk of aspirations, adequate empiric antimicrobial treatment with de-escalation when appropriate, daily assessment of ventilation weaning, and early mobilization [49].
Given the conflicting body of evidence described above, when approaching an HSCT with ARF, considerations should include: patient severity, comfort and safety, the need for prompt diagnostic measures and associated safety, the different options of noninvasive support and their efficiency as well as the local experience, optimal timing for intubation, and implications on other aspects of care such as chemotherapy, nutrition, etc.
Severe ARDS Adjunctive Measures and Extracorporeal Life Support (ECLS)
Currently, the approach to severe ARDS management in patients with HSCT is extrapolated from management used in the general population, with some exceptions. In the LUNG SAFE study of patients with ARDS, the frequency of the use of adjunctive measures such as neuromuscular blockade, recruitment maneuvers, prone positioning, inhaled vasodilators, high-frequency oscillatory ventilation, and extracorporeal life support was described. The secondary analysis focused on immunocompromised patients demonstrated that the adjuncts were used at the same frequency in the non-immunocompromised cohort with the exception of increased use of neuromuscular blockade. All adjuvants lack specific high-quality trial data evaluating their use across immunocompromised and specifically HSCT patients.
The one adjuvant measure that has been evaluated in this cohort is the use of extracorporeal life support (ECLS). ECLS is associated with significant health-care resource implications. Given this, most ECLS programs aim to restrict it to patients who would derive the greatest benefit. Historically, ECLS was discouraged in some programs across immunocompromised patients given their higher ARF mortality; however, with advancements in ARF outcomes and ECLS programs, its use has been expanded to select immunocompromised cohorts.
Several cohorts reported that 19–31% of ARDS patients treated with ECLS were immunocompromised [50,51,52,53]. A retrospective study that evaluated outcomes of 203 adult immunocompromised patients that were supported with ECLS for moderate to severe ARDS showed that 42% of the patients were weaned from ECLS. The overall survival rate was 30%. However, across all subtypes of immunocompromised patients, those with HM had the worse outcomes; 6-month survival varied between different immunocompromised groups with a 24% 6-month survival in the HM population. ECLS-related bleeding and nosocomial infections were frequent. A recent diagnosis of immunocompromised state, higher platelet counts, lower CO2, and driving pressure were associated with better prognosis [54]. These findings have decreased enthusiasm for the application of ECLS across HM patients in general and specifically in the HSCT cohort. The more prolonged immunocompromised state, low platelet counts, and high frequency of indeterminate ARDS make this cohort less favorable candidates for ECLS. A recent cohort study of 297 patients with cancer who underwent veno-venous extracorporeal membrane oxygenation (ECMO) for ARF demonstrated a 27% 60-day overall survival. In a propensity score-matched analysis to patients who did not receive ECMO, there was no significant survival advance for treatment with ECMO [55].
For the HSCT population, Wohlfarth et al. studied ECLS use after allogeneic HSCT in 37 patients and found only 19% survival rate. However, ECLS survival was higher across patients who were cannulated more than 240 days post-transplant [56]. In a recent meta-analysis of ECMO use in patients with HSCT, survival rates were similarly low (13% in hospital mortality) [57]. Overall, data are still limited, and the approach to consideration should be taken on a case-by-case basis by an ECMO expert. Tools of prognostications, such as the RESP score (for hospital survival) and the PRESERVE score (for 6-month survival), have been created by analyzing an international ECLS registry or using a program-based cohort, respectively [52, 58]. Both recognized immunocompromised as a bad prognostic factor. However, the RESP score was validated in 2012 in which only 5% of the patients were diagnosed as immunocompromised and HSCT patients are not reported, and the PRESERVE score was validated in 2013, reporting 31% of patients who were immunocompromised and 9% with HM [51]. The low survival rates, the high rate of complications, and the high burden of ECLS raise numerous ethical questions about their use in this cohort, and more research is needed to inform optimal patient selection for severe ARF. Considerations for management are outlined in Fig. 25.1.
Conclusion
Despite significant advances both in oncology and critical practice, post-HSCT patients are at high risk of developing ARF. While outcomes have improved, severe ARF is still associated with high mortality rates. Meticulous understanding of the pathophysiology, the risk factors, and cause is essential to tailoring effective therapy—ideally before the need for IMV. Further research of this unique population in critical care is needed to further our understanding of the mechanisms and causes of ARF. This is essential to develop studies targeted at evaluating optimal approaches to respiratory support (invasive and noninvasive) in this population.
References
Ferreyro BL, Law AD, Munshi L. Acute respiratory distress syndrome following hematopoietic stem cell transplantation: one more piece in the puzzle. Ann Am Thorac Soc. 2021;18(6):950–2. https://doi.org/10.1513/AnnalsATS.202103-273ED.
Darmon M, Bourmaud A, Georges Q, et al. Changes in critically ill cancer patients’ short-term outcome over the last decades: results of systematic review with meta-analysis on individual data. Intensive Care Med. 2019;45(7):977–87. https://doi.org/10.1007/s00134-019-05653-7.
Azoulay E, Pène F, Darmon M, et al. Managing critically ill hematology patients: time to think differently. Blood Rev. 2015;29(6):359–67. https://doi.org/10.1016/j.blre.2015.04.002.
Mokart D, Pastores SM, Darmon M. Has survival increased in cancer patients admitted to the ICU? Yes. Intensive Care Med. 2014;40(10):1570–2. https://doi.org/10.1007/s00134-014-3433-2.
Niederwieser D, Baldomero H, Szer J, et al. Hematopoietic stem cell transplantation activity worldwide in 2012 and a SWOT analysis of the worldwide network for blood and marrow transplantation group including the global survey. Bone Marrow Transplant. 2016;51(6):778–85. https://doi.org/10.1038/bmt.2016.18.
Afessa B, Abdulai RM, Kremers WK, Hogan WJ, Litzow MR, Peters SG. Risk factors and outcome of pulmonary complications after autologous hematopoietic stem cell transplant. Chest. 2012;141(2):442–50. https://doi.org/10.1378/chest.10-2889.
Bergeron A, Chevret S, de Latour RP, et al. Noninfectious lung complications after allogeneic haematopoietic stem cell transplantation. Eur Respir J. 2018;51(5):1702617. https://doi.org/10.1183/13993003.02617-2017.
Ho VT, Weller E, Lee SJ, Alyea EP, Antin JH, Soiffer RJ. Prognostic factors for early severe pulmonary complications after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2001;7(4):223–30. https://doi.org/10.1053/bbmt.2001.v7.pm11349809.
Herasevich S, Frank RD, Bo H, et al. Pretransplant risk factors can predict development of acute respiratory distress syndrome after hematopoietic stem cell transplantation. Ann Am Thorac Soc. 2021;18(6):1004–12. https://doi.org/10.1513/AnnalsATS.202004-336OC.
Saillard C, Darmon M, Bisbal M, et al. Critically ill allogenic HSCT patients in the intensive care unit: a systematic review and meta-analysis of prognostic factors of mortality. Bone Marrow Transplant. 2018;53(10):1233–41. https://doi.org/10.1038/s41409-018-0181-x.
Mokart D, van Craenenbroeck T, Lambert J, et al. Prognosis of acute respiratory distress syndrome in neutropenic cancer patients. Eur Respir J. 2012;40(1):169–76. https://doi.org/10.1183/09031936.00150611.
Hamidi M, Gossack-Keenan KL, Ferreyro BL, Angriman F, Rochwerg B, Mehta S. Outcomes of hematopoietic cell transplant recipients requiring invasive mechanical ventilation: a two-centre retrospective cohort study. Can J Anesth. 2019;66(12):1450–7. https://doi.org/10.1007/s12630-019-01439-z.
Chi AK, Soubani AO, White AC, Miller KB. An update on pulmonary complications of hematopoietic stem cell transplantation. Chest. 2013;144(6):1913–22. https://doi.org/10.1378/chest.12-1708.
Yadav H, Nolan ME, Bohman JK, et al. Epidemiology of acute respiratory distress syndrome following hematopoietic stem cell transplantation*. Crit Care Med. 2016;44(6):1082–90. https://journals.lww.com/ccmjournal/Fulltext/2016/06000/Epidemiology_of_Acute_Respiratory_Distress.9.aspx.
Wieruszewski PM, Herasevich S, Gajic O, Yadav H. Respiratory failure in the hematopoietic stem cell transplant recipient. World J Crit Care Med. 2018;7(5):62–72. https://doi.org/10.5492/wjccm.v7.i5.62.
Azoulay E, Mokart D, Kouatchet A, Demoule A, Lemiale V. Acute respiratory failure in immunocompromised adults. Lancet Respir Med. 2019;7(2):173–86. https://doi.org/10.1016/S2213-2600(18)30345-X.
Laffey JG, Bellani G, Pham T, et al. Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: the LUNG SAFE study. Intensive Care Med. 2016;42(12):1865–76. https://doi.org/10.1007/s00134-016-4571-5.
Cortegiani A, Madotto F, Gregoretti C, Bellani G, Laffey JG, Pham T. Immunocompromised patients with acute respiratory distress syndrome: secondary analysis of the LUNG SAFE database. Crit Care. 2018;22:157.
Azoulay E, Pickkers P, Soares M, et al. Acute hypoxemic respiratory failure in immunocompromised patients: the Efraim multinational prospective cohort study. Intensive Care Med. 2017;43(12):1808–19. https://doi.org/10.1007/s00134-017-4947-1.
Azoulay E, Mokart D, Rabbat A, et al. Diagnostic bronchoscopy in hematology and oncology patients with acute respiratory failure: prospective multicenter data*. Crit Care Med. 2008;36(1):100–7. https://journals.lww.com/ccmjournal/Fulltext/2008/01000/Diagnostic_bronchoscopy_in_hematology_and_oncology.14.aspx.
Azoulay É, Thiéry G, Chevret S, et al. The prognosis of acute respiratory failure in critically ill cancer patients. Medicine. 2004;83(6):360–70. https://doi.org/10.1097/01.md.0000145370.63676.fb.
Astashchanka A, Ryan J, Lin E, et al. Pulmonary complications in hematopoietic stem cell transplant recipients—a clinician primer. J Clin Med. 2021;10(15):3227. https://doi.org/10.3390/jcm10153227.
Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185–96. https://doi.org/10.1056/nejmoa1503326.
Guideline. Guidelines for intensive care unit admission, discharge, and triage. Crit Care Med. 1999;27(3):633. https://journals.lww.com/ccmjournal/Fulltext/1999/03000/Guidelines_for_intensive_care_unit_admission.48.aspx.
Gruson D, Vargas F, Hilbert G, et al. Predictive factors of intensive care unit admission in patients with haematological malignancies and pneumonia. Intensive Care Med. 2004;30(5):965–71. https://doi.org/10.1007/s00134-004-2237-1.
Hilbert G, Gruson D, Vargas F, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med. 2001;344(7):481–7. https://doi.org/10.1056/NEJM200102153440703.
Paz HL, Crilley P, Weinar M, Brodsky I. Outcome of patients requiring medical ICU admission following bone marrow transplantation. Chest. 1993;104(2):527–31. https://doi.org/10.1378/chest.104.2.527.
Lemiale V, Mokart D, Resche-Rigon M, et al. Effect of noninvasive ventilation vs oxygen therapy on mortality among immunocompromised patients with acute respiratory failure: a randomized clinical trial. JAMA. 2015;314(16):1711–9. https://doi.org/10.1001/jama.2015.12402.
Adda M, Coquet I, Darmon M, Thiery G, Schlemmer B, Azoulay É. Predictors of noninvasive ventilation failure in patients with hematologic malignancy and acute respiratory failure*. Crit Care Med. 2008;36(10):2766. https://journals.lww.com/ccmjournal/Fulltext/2008/10000/Predictors_of_noninvasive_ventilation_failure_in.9.aspx.
Bellani G, Laffey JG, Pham T, et al. Noninvasive ventilation of patients with acute respiratory distress syndrome: insights from the LUNG SAFE study. Am J Respir Crit Care Med. 2017;195(1):67–77. https://doi.org/10.1164/rccm.201606-1306OC.
Azoulay E, Lemiale V, Mokart D, et al. Effect of high-flow nasal oxygen vs standard oxygen on 28-day mortality in immunocompromised patients with acute respiratory failure: the HIGH randomized clinical trial. JAMA. 2018;320(20):2099–107. https://doi.org/10.1001/jama.2018.14282.
Magdy DM, Metwally A. The utility of HACOR score in predicting failure of high-flow nasal oxygen in acute hypoxemic respiratory failure. Adv Respir Med. 2021;89(1):23–9. https://doi.org/10.5603/ARM.a2021.0031.
Roca O, Messika J, Caralt B, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: the utility of the ROX index. J Crit Care. 2016;35:200–5. https://doi.org/10.1016/j.jcrc.2016.05.022.
Kang BJ, Koh Y, Lim CM, et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med. 2015;41(4):623–32. https://doi.org/10.1007/s00134-015-3693-5.
Roca O, Caralt B, Messika J, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy. Am J Respir Crit Care Med. 2019;199(11):1368–76. https://doi.org/10.1164/rccm.201803-0589OC.
Lemiale V, Dumas G, Demoule A, et al. Performance of the ROX index to predict intubation in immunocompromised patients receiving high-flow nasal cannula for acute respiratory failure. Ann Intensive Care. 2021;11(1):17. https://doi.org/10.1186/s13613-021-00801-z.
Carteaux G, Parfait M, Combet M, Haudebourg AF, Tuffet S, Dessap AM. Patient self-inflicted lung injury: a practical review. J Clin Med. 2021;10(12):1–13. https://doi.org/10.3390/jcm10122738.
Patel BK, Wolfe KS, Pohlman AS, Hall JB, Kress JP. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome a randomized clinical trial. JAMA. 2016;315(22):2435–41. https://doi.org/10.1001/jama.2016.6338.
Ferreyro BL, Angriman F, Munshi L, et al. Association of noninvasive oxygenation strategies with all-cause mortality in adults with acute hypoxemic respiratory failure: a systematic review and meta-analysis. JAMA. 2020;324(1):57–67. https://doi.org/10.1001/jama.2020.9524.
Grieco DL, Menga LS, Cesarano M, et al. Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: the HENIVOT randomized clinical trial. JAMA. 2021;325(17):1731–43. https://doi.org/10.1001/jama.2021.4682.
Hui D, Morgado M, Chisholm G, et al. High-flow oxygen and bilevel positive airway pressure for persistent dyspnea in patients with advanced cancer: a phase II randomized trial. J Pain Symptom Manag. 2013;46(4):463–73. https://doi.org/10.1016/j.jpainsymman.2012.10.284.
Epstein AS, Hartridge-Lambert SK, Ramaker JS, Voigt LP, Portlock CS. Humidified high-flow nasal oxygen utilization in patients with cancer at Memorial Sloan-Kettering Cancer Center. J Palliat Med. 2011;14(7):835–9. https://doi.org/10.1089/jpm.2011.0005.
Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–33. https://doi.org/10.1001/jama.2012.5669.
Demoule A, Antonelli M, Schellongowski P, et al. Respiratory mechanics and outcomes in immunocompromised patients with ARDS: a secondary analysis of the EFRAIM study. Chest. 2020;158(5):1947–57. https://doi.org/10.1016/j.chest.2020.05.602.
Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–8. https://doi.org/10.1056/NEJM200005043421801.
Amato MBP, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747–55. https://doi.org/10.1056/nejmsa1410639.
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354(24):2564–75. https://doi.org/10.1056/NEJMoa062200.
Fan E, del Sorbo L, Goligher EC, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(9):1253–63. https://doi.org/10.1164/rccm.201703-0548ST.
Yadav H, Thompson BT, Gajic O. Is acute respiratory distress syndrome a preventable disease? Am J Respir Crit Care Med. 2017;195(6):725–36. https://doi.org/10.1164/rccm.201609-1767CI.
ANZICS Investigators. Extracorporeal membrane oxygenation for 2009 influenza a(H1N1) acute respiratory distress syndrome. JAMA. 2009;302(17):1888–95. https://doi.org/10.1001/jama.2009.1535.
Schmidt M, Zogheib E, Rozé H, et al. The PRESERVE mortality risk score and analysis of long-term outcomes after extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Intensive Care Med. 2013;39(10):1704–13. https://doi.org/10.1007/s00134-013-3037-2.
Schmidt M, Bailey M, Sheldrake J, et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure: the respiratory extracorporeal membrane oxygenation survival prediction (RESP) score. Am J Respir Crit Care Med. 2014;189(11):1374–82. https://doi.org/10.1164/rccm.201311-2023OC.
Combes A, Hajage D, Capellier G, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378(21):1965–75. https://doi.org/10.1056/NEJMoa1800385.
Schmidt M, Schellongowski P, Patroniti N, et al. Six-month outcome of immunocompromised patients with severe acute respiratory distress syndrome rescued by extracorporeal membrane oxygenation an international multicenter retrospective study. Am J Respir Crit Care Med. 2018;197(10):1297–307. https://doi.org/10.1164/rccm.201708-1761OC.
Kochanek M, Kochanek J, Boll B, et al. Veno-venous extracorporeal membrane oxygenation (vv-ECMO) for severe respiratory failure in adult cancer patients: a retrospective multicenter analysis. Intensive Care Med. 2020;48:332–42.
Wohlfarth P, Beutel G, Lebiedz P, et al. Characteristics and outcome of patients after allogeneic hematopoietic stem cell transplantation treated with extracorporeal membrane oxygenation for acute respiratory distress syndrome*. Crit Care Med. 2017;45(5):e500.
Sim JJL, Mitra S, Ling RR, et al. Extracorporeal membrane oxygenation in patients with hematologic malignancies: a systematic review and meta-analysis. Ann Hematol. 2022;101:1395–406.
Schmidt M, Combes A, Shekar K. ECMO for immunosuppressed patients with acute respiratory distress syndrome: drawing a line in the sand. Intensive Care Med. 2019;45(8):1140–2. https://doi.org/10.1007/s00134-019-05632-y.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Munshi, L., Stavi, D. (2023). Respiratory Support of the Critically Ill Hematopoietic Stem Cell Transplant Patient. In: Soubani, A.O. (eds) Pulmonary and Critical Care Considerations of Hematopoietic Stem Cell Transplantation. Springer, Cham. https://doi.org/10.1007/978-3-031-28797-8_25
Download citation
DOI: https://doi.org/10.1007/978-3-031-28797-8_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-28796-1
Online ISBN: 978-3-031-28797-8
eBook Packages: MedicineMedicine (R0)