Abstract
Hematological malignancies (HM) have been, until recently, viewed as contraindications to extracorporeal membrane oxygenation (ECMO) due to bleeding and infectious complications. However, conflicting literature regarding whether ECMO should be used for patients with HM still exists. We conducted a random effects meta-analysis to investigate the outcomes of patients with HM on ECMO. We searched Medline, Embase, Scopus, and Cochrane through 10 October 2021. Risk of bias and certainty of evidence were assessed using the JBI checklists and GRADE approach respectively. Thirteen observational studies (422 patients with HM, 9778 controls without HM) were included. The pooled in-hospital mortality for patients with HM and those with hematopoietic stem cell transplants for HM indications needing ECMO were 79.1% (95%CI: 70.2–86.9%) and 87.7% (95%CI: 80.4–93.8%), respectively. Subgroup analyses found that mortality was higher in adults than children (85.1% vs 67.9%, pinteraction = 0.003), and in Asia compared to North America and Europe (93.8% vs 69.6%, pinteraction < 0.001). Pooled ECMO duration was 10.0 days (95%CI: 7.5–12.5); pooled ICU and hospital lengths of stay were 19.8 days (95%CI: 12.4–27.3) and 43.9 days (95%CI: 29.4–58.4) respectively. Age (regression coefficient [B]: 0.008, 95%CI: 0.003–0.014), proportion of males (B: 1.799, 95%CI: 0.079–3.519), and ECMO duration (B: − 0.022, 95%CI: − 0.043 to − 0.001) were significantly associated with higher mortality. In-hospital mortality of patients with HM who needed ECMO was 79.1%, with better outcomes in children, and in North America and Europe. ECMO should not be regarded as routine support therapy in these patients but can be carefully considered on a case-by-case basis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extracorporeal membrane oxygenation (ECMO) is a form of mechanical cardiopulmonary bypass to support patients in the intensive care unit (ICU) with severe cardiac or respiratory failure. Veno-arterial (VA) ECMO provides hemodynamic support and veno-venous (VV) ECMO offers respiratory support [1]. Outcomes following ECMO vary considerably depending on the age of the patient, underlying disease, indication for ECMO, and cannulation strategy. [2, 3] Offering ECMO to patients with hematological malignancies (HM) is associated with higher risk of adverse events.
Patients with underlying HM are prone to infections due to their underlying disease process or chemotherapy [4]. In these patients, acute respiratory failure is a life-threatening complication which warrants admission to the ICU [5, 6]. Despite recent advances in treatment modalities, almost half of them end up requiring invasive ventilation and have substantial mortality rates [7, 8]. Also, the use of ECMO in these patients has been associated with increased complications, such as bleeding and nosocomial infections [4].
Despite some studies evaluating the use of ECMO in patients with HM, [9] conflicting reports have been published thus far [7, 10, 11]. A recent review concluded that while there was an increasingly favorable prognosis among HM patients requiring ECMO over time, a more systematic approach was needed to quantify their findings [7]. To address the lack of conclusive evidence, we conducted a systematic review and meta-analysis to analyze the outcomes of patients with HM on ECMO, focusing on in-hospital mortality.
Methods
Search strategy and selection criteria
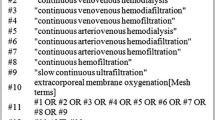
This review was registered with PROSPERO (CRD42021232647) and was conducted in adherence with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement [12]. We searched Medline, Embase, Cochrane, and Scopus databases from 1st January 1990 to 10th October 2021 using the following keywords and their variations: “extracorporeal membrane oxygenation” and “hematologic malignancies” (Supplementary Table 1). We assessed all the relevant studies, and their citation lists to identify articles for inclusion. Studies reporting on at least 5 adult or pediatric patients with HM requiring ECMO were included. We excluded any non-human studies, case reports, and articles that did not report in-hospital mortality. We also excluded reviews of Extracorporeal Life Support Organization (ELSO) registry data to minimize the risk of patient duplication. In the case of overlapping patient data across two or more studies, we included the larger study.
Data collection
Data were collected using a prespecified data extraction form, and covered study characteristics, patient demographics, pre-ECMO and ECMO characteristics, mortality outcomes, and other relevant clinical outcomes.
Risk of bias assessment
We used the appropriate Joanna Briggs Institute (JBI) critical appraisal checklists to assess the eligibility of studies. The possibility of publication bias was assessed using Egger’s test and visual inspection of the funnel plot. We performed a sensitivity analysis by excluding studies with comparatively higher risks of bias (JBI score < 8). The screening of articles, data collection, and risk of bias assessment were conducted independently by three reviewers (RRL, JJLS, SM), and any conflicts were resolved by a fourth reviewer (KR).
Statistical analysis
Statistical analyses were performed on R 4.0.2 using the meta (v4.17–0) and dmetar (v0.0.9000) packages. For continuous characteristics of studies, we generated the means and standard deviations from the information presented in each study as per Wan et al. [13] and pooled the means via meta-analysis. The primary aim of our study was to estimate the pooled in-hospital mortality among patients with HM who received ECMO. Secondary aims included the pooled risk ratio (RR) of mortality when compared to controls without HM supported on ECMO, the pooled mean of duration of ECMO support, ICU length of stay, and hospital length of stay for patients with HM. Due to the sparseness of data on the complications of ECMO, we aggregated each complication across studies and identified the most frequently reported complication and its corresponding percentage where the denominator was the total of reported complications.
We anticipated significant inter-study heterogeneity given the different intervention thresholds and subsequent management of patients with HM on ECMO. As such, random effects meta-analyses (DerSimonian and Laird) [14] were conducted. To pool the proportions across studies, the Freeman-Tukey double arcsine transformation was used [15]. For continuous outcomes, pooled means and mean differences are presented. For each pooled estimate, their respective 95% confidence intervals (CIs) are reported. For the study specific proportions, 95% CIs were computed using the Clopper-Pearson method [16].
Subgroup analyses for the primary aim of our study were conducted with continuity correction to include studies with zero events. Categorical variables included were age (adults vs children as defined by each study) and geographical region (Asia vs North America and Europe). A separate post hoc subgroup analysis looking at the mortality of those receiving hematopoietic stem cell transplants (HSCT) for HM indications, and comparing mortality between neutropenic versus non-neutropenic patients with HM was conducted as well. Univariable study-level meta-regression was conducted when the covariates were continuous and there were at least 6 studies to explore potential sources of heterogeneity or prognostically relevant study-level covariates [17].
We used the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) approach to assess the inter-study heterogeneity for our primary and secondary aims [18, 19] This helps to define the quality of the evidence in terms of the confidence that the estimated effect is similar to the true effect.
Results
Of 814 references, we assessed 56 full-text articles after initial screening. A total of 13 studies reporting on 422 patients with HM and 9778 controls without HM requiring ECMO were included in this analysis (Supplementary Fig. 1) [4, 11, 20,21,22,23,24,25,26,27,28,29,30].
Assessment of study quality
Based on the JBI critical appraisal checklist for case series, the studies included for this review were of high quality, with 8 studies scoring a minimum of 9/10 (Supplementary Table 2). A summary of the assessment of certainty using the GRADE approach is presented in Table 3.
Characteristics of patients
Table 1 reports the characteristics of the included studies. Four studies (93 patients with HM) were from Asia, 2 studies were from North America (158 patients with HM), 6 studies were from Europe (109 patients with HM), and 1 multi-continental study was conducted (62 patients with HM). The pooled mean age of patients with HM supported by ECMO was 26.7 years (95%CI: 15.0–38.5). The majority of the patients were male (61.3%, 95%CI: 53.3–68.8%), with severe acute respiratory distress syndrome (ARDS) (PaO2/FiO2 [P/F] ratio: 56.7, 95%CI: 46.8–66.6) and organ dysfunction (Sequential Organ Failure Assessment score: 12.5, 95%CI: 11.1–13.9; Simplified Acute Physiology Score II: 56.9, 95%CI: 51.2–62.6). VV ECMO was the predominant cannulation strategy utilized (79.9%, 95%CI: 58.6–91.8%), while the remaining patients were cannulated on VA ECMO. The most common HM was leukemia (65.3%, 95%CI: 45.6–80.8%), followed by lymphoma (18.8%, 95%CI: 9.8–33.2%), multiple myeloma (2.4%, 95%CI: 0.5–10.9%), and myelodysplastic syndrome (1.6%, 95%CI: 0.3–7.2%). 35.8% (95%CI: 21.5–53.2%) of patients with HM were on chemotherapy, while 46.1% (95%CI: 19.9–74.7%) received HSCT for HM indications. For patients with HM, the pooled mean platelet count was 50.9 × 103/μL (95%CI: 37.0–64.7) and pooled mean leukocyte count was 7.0 × 103/μL (95%CI: 4.3–9.7) prior to ECMO. Among the patients without HM, these were 158.1 × 103/μL (95%CI: 139.9–176.2) and 12.6 × 103/μL (95%CI: 9.4–15.7) respectively. 41.5% (95%CI: 30.6–53.2%) of patients with HM were neutropenic, defined as an absolute neutrophil count < 0.5 × 103/μL by the studies. 50.8% (95%CI: 42.33–59.2%) of patients with HM received renal replacement therapy compared to 51.8% (95%CI: 43.6–59.8%) of patients without HM.
Primary aim
Of 13 observational studies (422 patients), the pooled in-hospital mortality for patients with HM needing ECMO was 79.1% (95%CI: 70.2–86.9%, high certainty, Fig. 1), with the absence of asymmetry in the funnel plot indicating a low probability for publication bias (pegger = 0.51, Supplementary Fig. 2). Sensitivity analysis excluding 2 studies [4, 23] with a JBI score of < 8 did not significantly change the pooled estimate (79.4%, 95%CI: 69.6–87.8%).
Subgroup analysis
Based on subgroup analysis, studies reporting on adult patients had a significantly higher mortality (8 studies, 226 patients, 85.1%, 95%CI: 75.3–92.9%) compared to those reporting on pediatric patients (5 studies, 196 patients, 67.9%, 95%CI: 60.7–74.7%, pinteraction = 0.003, Fig. 2a). Similarly, studies reporting from centers in Asia (4 studies, 93 patients, 93.8%, 95%CI: 86.5–98.7%) had a higher mortality rate when compared to studies reporting from centers in North America and Europe (8 studies, 267 patients, 69.6%, 95%CI: 61.3–77.4%, pinteraction < 0.001, Fig 2b). The multi-continental study by Schmidt et al. reported a mortality rate of 75.8% (95%CI: 64.3–85.8%) [28]. The subgroup of patients who received HSCT for HM indications had a relatively higher in-hospital mortality of 87.7% (95%CI: 80.4–93.8%, Fig 2c) compared to the pooled mortality for all patients with HM. There was no significant difference in mortality between neutropenic versus non-neutropenic patients with HM (RR 1.1, 95%CI: 0.4–3.2).
Meta-regression analyses
Univariable meta-regression found that the proportion of male patients (regression coefficient [B]: 1.799, 95%CI: 0.079–3.519, p = 0.040), mean age (B: 0.008, 95%CI: 0.003–0.014, p = 0.005), and mean ECMO duration (B: − 0.022, 95%CI: − 0.043 to − 0.001, p = 0.036) had significant associations with in-hospital mortality (Fig. 3). Other factors such as mean P/F ratio and proportion of patients receiving HSCT and VV-ECMO were not significantly associated with in-hospital mortality (Table 2).
Secondary aims
Seven studies (176 patients with HM, 735 controls without HM) reported on the in-hospital mortality in patients with HM and without HM receiving ECMO support [4, 21, 24,25,26, 28, 29]. HM was not significantly associated with an increased risk of in-hospital mortality (RR: 1.28, 95%CI: 0.99–1.66, p = 0.06, very low certainty, Fig. 4).
The pooled duration of ECMO support was 10.0 days (95%CI: 7.5–12.5, 11 studies, moderate certainty); pooled ICU and hospital length of stay were 19.8 days (95%CI: 12.4–27.3, 5 studies, moderate certainty) and 43.9 days (95%CI: 29.4–58.4, 4 studies, moderate certainty), respectively (Supplementary Fig. 3). A total of 81 complications were reported among the 9 studies (171 patients) (Supplementary Table 3). Hemorrhagic (55.6%) complications were the most commonly reported among this patient cohort (Table 3).
Discussion
This review reported on the pooled in-hospital mortality in patients with HM who received ECMO. Patients were predominantly young adult males from North America and Europe with severe ARDS receiving VV-ECMO with a pooled in-hospital mortality of 79.1%. Additionally, we noted that increasing age, shorter ECMO duration, and male sex were significantly associated with higher mortality. Subgroup analysis found higher mortality in adults than children, in Asia compared to North America and Europe, and in patients who received hematopoietic stem cell transplant for HM indications (87.7%). Hemorrhagic (55.6%) complications were the most frequently reported among the studies in this review.
In a recent sub-analysis of The Large Observational Study to Understand the Global Impact of Severe Acute Respiratory Failure (LUNG SAFE) trial, immunocompromised patients with ARDS (20.8% of the patient cohort) suffered from significantly higher mortality rates (52.4%) compared to immunocompetent individuals (36.2%), irrespective of disease severity [31]. Similarly, another analysis from the same database found that active neoplasm, HM, and immunosuppression were independently associated with mortality [32] Azoulay et al. noted an in-hospital mortality of 64% in a cohort of 1004 patients with ARDS and underlying malignancies, of which 86% had HM [33]. Patients with allogeneic HSCT were also at increased risk of higher mortality if they developed hypoxemic respiratory failure [33]. Early admission to ICU was associated with improved outcomes [5]. A recent ELSO registry analysis of pediatric patients with HSCT requiring ECMO showed an overall in-hospital survival of 19%, although this had improved to 26% within the last decade (p = 0.01) [34]. Although the outcomes of patients with HM have shown considerable improvement due to advancements in therapeutic strategies in recent years, patients need to be carefully selected for resource intensive modalities like ECMO, given its high mortality and intense resource utilization [5, 35].
Patients with concomitant ARDS and HM have a relatively high mortality of 77% [36], and it has been well established that initiation of invasive ventilation accounted for poorer outcomes in this cohort [37]. Due to the complex underlying disease pathophysiology, the management of these patients using ECMO as a rescue therapy is more challenging, and they have more frequent complications such as bleeding and nosocomial infections while on ECMO [38]. Further evaluation of the safety of ECMO in spontaneously breathing patients with HM to prevent endotracheal intubation and ventilator associated pneumonia should be considered. While ELSO guidelines consider major pharmacological immunosuppression (absolute neutrophil count < 0.4 × 103/μL) as a relative contraindication to ECMO, [39] recent ECMO cohorts nonetheless enrolled immunocompromised patients [40, 41]. In the ECMO to Rescue Lung Injury in Severe ARDS (EOLIA) trial, 22% of the patients were immunocompromised with a 60-day mortality of 56% in the treatment group [42]. In contrast, we observed a pooled mortality of 79% in our cohort of patients with HM who received ECMO therapy.
The high mortality in our review could be attributed to the underlying disease process, high organ dysfunction scores, associated multi-organ failure (MOF), and nosocomial complications. Prior studies also observed poor survival patterns in patients with associated MOF in this cohort [5, 36]. We found that hemorrhagic complications were the most commonly reported complication among patients with HM, potentially attributable to the concomitant anticoagulation, thrombocytopenia and coagulation factor consumption by the ECMO circuit in addition to the underlying disease [42]. We observed that the cumulative mean platelet count in patients with HM was lower than that of patients without HM, possibly contributing to both increased bleeding episodes while on ECMO support and higher mortality. Review of existing transfusion thresholds to correct coagulopathy and thrombocytopenia in this group of high-risk patients should be considered, given the increased bleeding risk while on ECMO.
There are several limitations to our study. First, due to the resource-intensive nature of ECMO, particularly in this patient cohort, randomized controlled trials are logistically challenging. All the studies in our analysis were observational, which introduces a risk of bias and potential confounding, particularly without any risk- or propensity-score adjustment methods. This is further exacerbated by the fact that the sample sizes were small and heterogeneous — the indications for ECMO varied across studies, and patient profiles and diagnoses were diverse as well. To account for this, we used the random effects model for meta-analysis and were able to identify some sources of heterogeneity through subgroup analysis and meta-regression. Nonetheless, the meta-regression analyses are limited by the small sample size and limited number of studies. Furthermore, it is also prone to type II errors and ecological fallacy [43]. Second, patients who received HSCT for HM indications were included in the mortality analysis for patients with HM on ECMO. This may lead to confounding because up until recently, ECMO for HSCT was regarded as futile with < 10% survival, while ECMO for carefully selected patients with HM was regarded as acceptable with a 30–40% survival. Third, some data were poorly reported such as the incidence of MOF or secondary infections, which might be prognostically significant in this cohort. In our analysis, we used surrogate markers (SOFA score, leukocyte counts) to estimate the likelihood of developing these complications, but such analyses are nonetheless indirect, and do not reflect the prevalence of these complications. Some studies also did not provide data for patients with and without HM separately or did not include patients without HM, making direct comparisons or meta-regression challenging.
Conclusion
Survival of patients with HM requiring ECMO are relatively poor when compared to other indications for ECMO. Patients at risk of worse outcomes include older age, male gender, and recipients of HSCT. Given the higher mortality of this cohort while on ECMO, extracorporeal therapy should be considered judiciously on a case-by-case basis for each patient. Future studies should focus on exploring the ideal time of initiation of ECMO and attempt to establish specific initiation criteria in these patients.
References
Manaker S, Parsons PE, Finlay G (2021) Extracorporeal membrane oxygenation (ECMO) in adults. UpToDate https://www.uptodate.com/contents/extracorporeal-membrane-oxygenation-ecmo-in-adults. Accessed November 17, 2021
Cashen K, Reeder R, Dalton HJ et al (2017) Functional status of neonatal and pediatric patients after extracorporeal membrane oxygenation. Pediatr critical care med : J Soc Critical Care Med World Federation Pediatr Intensive Critical Care Soc 18(6):561–570
Kosmopoulos M, Bartos JA, Kalra R et al (2021) Patients treated with venoarterial extracorporeal membrane oxygenation have different baseline risk and outcomes dependent on indication and route of cannulation. Hellenic J Cardiol 62(1):38–45
Park TS, Oh YN, Hong S-B et al (2016) Extracorporeal membrane oxygenation support in adult patients with hematologic malignancies and severe acute respiratory failure. Korean J Crit Care Med 31(3):243–250
Azoulay E, Mokart D, Pene F et al (2013) Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium–a groupe de recherche respiratoire en reanimation onco-hematologique study. J Clin Oncol 31(22):2810–2818
Benoit DD, Vandewoude KH, Decruyenaere JM, Hoste EA, Colardyn FA (2003) Outcome and early prognostic indicators in patients with a hematologic malignancy admitted to the intensive care unit for a life-threatening complication. Crit Care Med 31(1):104–112
Tathineni P, Pandya M, Chaar B (2020) The utility of extracorporeal membrane oxygenation in patients with hematologic malignancies: a literature review. Cureus 12(7):e9118
Taccone FS, Artigas AA, Sprung CL, Moreno R, Sakr Y, Vincent JL (2009) Characteristics and outcomes of cancer patients in European ICUs. Crit Care 13(1):R15
Di Nardo M, Ahmad AH, Merli P, et al. (2021) Extracorporeal membrane oxygenation in children receiving hematopoietic cell transplantation and immune effector cell therapy: an international and multidisciplinary consensus statement. Lancet Child Adolesc Health.
Kang HS, Rhee CK, Lee HY et al (2015) Clinical outcomes of extracorporeal membrane oxygenation support in patients with hematologic malignancies. Korean J Intern Med 30(4):478–488
Wohlfarth P, Ullrich R, Staudinger T et al (2014) Extracorporeal membrane oxygenation in adult patients with hematologic malignancies and severe acute respiratory failure. Crit Care 18(1):R20
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Miller JJ (1978) The inverse of the Freeman-Tukey double arcsine transformation. Am Stat 32(4):138–138
Clopper CJ, Pearson ES (1934) The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 26(4):404–413
Geissbuhler M, Hincapie CA, Aghlmandi S, Zwahlen M, Juni P, da Costa BR (2021) Most published meta-regression analyses based on aggregate data suffer from methodological pitfalls a meta-epidemiological study. BMC Med Res Methodol 21(1):123
Guyatt GH, Oxman AD, Kunz R et al (2011) GRADE guidelines: 7 Rating the quality of evidence--inconsistency. J Clin Epidemiol. 64(12):1294–1302
Iorio A, Spencer FA, Falavigna M et al (2015) Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. BMJ : British Medical J 350:h870
Cho S, Cho WC, Lim JY, Kang PJ (2019) Extracorporeal life support in adult patients with hematologic malignancies and acute circulatory and/or respiratory failure. Korean J Thorac Cardiovasc Surg 52(1):25–31
Choi KB, Kim HW, Jo KH, Kim do Y, Choi HJ, Hong SB, (2016) Extracorporeal life support in patients with hematologic malignancies: a single center experience. Korean J Thorac Cardiovasc Surg 49(4):280–286
Coleman RD, Goldman J, Moffett B et al (2020) Extracorporeal membrane oxygenation mortality in high-risk populations: an analysis of the pediatric health information system database. ASAIO J 66(3):327–331
Cortina G, Neu N, Kropshofer G, Meister B, Klingkowski U, Crazzolara R (2018) Extracorporeal membrane oxygenation offers long-term survival in childhood leukemia and acute respiratory failure. Crit Care. 22(1):222
Maue DK, Hobson MJ, Friedman ML, Moser EA, Rowan CM (2019) Outcomes of pediatric oncology and hematopoietic cell transplant patients receiving extracorporeal membrane oxygenation. Perfusion 34(7):598–604
Na SJ, Park SH, Hong SB et al (2020) Clinical outcomes of immunocompromised patients on extracorporeal membrane oxygenation support for severe acute respiratory failure. Eur J Cardiothorac Surg 57(4):788–795
Potratz JC, Guddorf S, Ahlmann M et al (2021) Extracorporeal membrane oxygenation in children with cancer or hematopoietic cell transplantation: single-center experience in 20 consecutive patients. Front Oncol 11:664928
Ranta S, Kalzen H, Nilsson A et al (2021) Extracorporeal membrane oxygenation support in children with hematologic malignancies in Sweden. J Pediatr Hematol Oncol 43(2):e272–e275
Schmidt M, Schellongowski P, Patroniti N et al (2018) Six-month outcome of immunocompromised patients with severe acute respiratory distress syndrome rescued by extracorporeal membrane oxygenation. An international multicenter retrospective study. Am J Respir Crit Care Med 197(10):1297–1307
Stecher SS, Beyer G, Goni E et al (2018) Extracorporeal membrane oxygenation in predominantly leuco- and thrombocytopenic haematologic/oncologic patients with acute respiratory distress syndrome - a single-centre experience. Oncol Res Treat 41(9):539–543
Wohlfarth P, Beutel G, Lebiedz P et al (2017) Characteristics and outcome of patients after allogeneic hematopoietic stem cell transplantation treated with extracorporeal membrane oxygenation for acute respiratory distress syndrome. Crit Care Med 45(5):e500–e507
Cortegiani A, Madotto F, Gregoretti C et al (2018) Immunocompromised patients with acute respiratory distress syndrome: secondary analysis of the LUNG SAFE database. Crit Care 22(1):157
Laffey JG, Bellani G, Pham T et al (2016) Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: the LUNG SAFE study. Intensive Care Med 42(12):1865–1876
Azoulay E, Lemiale V, Mokart D et al (2014) Acute respiratory distress syndrome in patients with malignancies. Intensive Care Med 40(8):1106–1114
Olson TL, O’Neil ER, Kurtz KJ, MacLaren G, Anders MM (2021) Improving outcomes for children requiring extracorporeal membrane oxygenation therapy following hematopoietic stem cell transplantation. Crit Care Med 49(4):e381–e393
Tremblay LN, Hyland RH, Schouten BD, Hanly PJ (1995) Survival of acute myelogenous leukemia patients requiring intubation/ventilatory support. Clin Invest Med 18(1):19–24
Turkoglu M, Erdem GU, Suyani E et al (2013) Acute respiratory distress syndrome in patients with hematological malignancies. Hematology 18(3):123–130
Al-Dorzi HM, Al Orainni H, Al Eid F et al (2017) Characteristics and predictors of mortality of patients with hematologic malignancies requiring invasive mechanical ventilation. Ann Thorac Med 12(4):259–265
Schmidt M, Combes A, Shekar K (2019) ECMO for immunosuppressed patients with acute respiratory distress syndrome: drawing a line in the sand. Intensive Care Med 45(8):1140–1142
Extracorporeal Life Support Organization 2017 ELSO guidelines for cardiopulmonary extracorporeal life support. Version 1.4:www.elso.org.
Schmidt M, Bailey M, Sheldrake J et al (2014) Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med 189(11):1374–1382
Schmidt M, Zogheib E, Roze H et al (2013) The PRESERVE mortality risk score and analysis of long-term outcomes after extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Intensive Care Med 39(10):1704–1713
Combes A, Hajage D, Capellier G et al (2018) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med 378(21):1965–1975
Columb MO, Atkinson MS (2016) Statistical analysis: sample size and power estimations. BJA Education 16(5):159–161
Acknowledgements
The authors extend their appreciation to Suei Nee Wong from the National University of Singapore for her assistance with the search strategy.
Author information
Authors and Affiliations
Contributions
Study design: SM, KR. Search strategy and screening of articles: JJLS, RRL, SM, KR. Risk of bias assessment: JJLS, RRL. Data collection: JJLS, RRL, SM. Data analysis and interpretation: JJLS, CST, KR. Tables and figures: JJLS. Drafting of manuscript: JJLS, SM, RRL, KR. Critical revision of manuscript for intellectually important content: JJLS, SM, RRL, CST, BEF, GM, KR. All authors provided critical conceptual input, interpreted the data analysis, read, and approved the final draft.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was not applicable since the manuscript does not contain any patient data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sim, J.J.L., Mitra, S., Ling, R.R. et al. Extracorporeal membrane oxygenation in patients with hematologic malignancies: a systematic review and meta-analysis. Ann Hematol 101, 1395–1406 (2022). https://doi.org/10.1007/s00277-022-04855-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-022-04855-2