Abstract
During ageing molecular damage leads to the accumulation of several hallmarks of ageing including mitochondrial dysfunction, cellular senescence, genetic instability and chronic inflammation, which contribute to the development and progression of ageing-associated diseases including cardiovascular disease. Consequently, understanding how these hallmarks of biological ageing interact with the cardiovascular system and each other is fundamental to the pursuit of improving cardiovascular health globally. This review provides an overview of our current understanding of how candidate hallmarks contribute to cardiovascular diseases such as atherosclerosis, coronary artery disease and subsequent myocardial infarction, and age-related heart failure. Further, we consider the evidence that, even in the absence of chronological age, acute cellular stress leading to accelerated biological ageing expedites cardiovascular dysfunction and impacts on cardiovascular health. Finally, we consider the opportunities that modulating hallmarks of ageing offer for the development of novel cardiovascular therapeutics.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction: Cardiovascular Ageing
More than 75% of Americans between the ages of 60 and 79, and nearly 90% of those over 80, suffer from cardiovascular disease (CVD) (Virani et al. 2021). It is therefore unsurprising that CVD is the leading cause of death for people over the age of 65 (North and Sinclair 2012). In the decades to come, increased prevalence of age-related CVDs such as atherosclerosis, coronary artery disease, myocardial infarction (MI), thoracic aortic aneurysm, valvular heart disease, and heart failure (HF) will contribute to even greater health and economic burden as the world’s population continues to age (Childs et al. 2017; Olivieri et al. 2013). In this review, the mechanisms of cardiovascular ageing concerning several age-related CVDs will be described, with a focus on mitochondrial dysfunction and the non-canonical roles of telomerase.
Cardiovascular Ageing and Atherosclerosis
Atherosclerosis is classed as a disease of ageing and is the leading cause of vascular disease worldwide (Wang and Bennett 2012). Atherosclerosis is initiated by endothelial injury or accumulation of low-density lipoproteins (LDLs) within the arterial wall which leads to the development of lipid and protein-filled “plaques”, triggering both the innate and adaptive immune responses (Moriya 2019). Inflammation stimulates necrotic core enlargement, extracellular matrix degeneration and cap thinning, erosion, calcification, and intra-plaque angiogenesis (Stojanović et al. 2020). Ultimately the atherosclerotic plaque can become unstable until rupture triggers thrombus formation, leading to blockage of the artery and thus cessation of blood flow distal to the occlusion leading to severe ischaemic injuries including MI and stroke (Montecucco et al. 2016; Thygesen et al. 2012; Moriya 2019).
Ageing and Heart Failure
An estimated 6.2 million adults in the USA are currently living with clinical HF with approximately 90% of these individuals being over 60 years old (Benjamin et al. 2019). HF is associated with ageing as a result of several pathophysiologies that contribute to impaired myocardial function and the inability of the heart to provide the circulatory efficiency required to meet organ demand.
At a cellular level, myocardial ageing is associated with structural, biochemical, and biomechanical changes including increased arterial stiffness, cardiomyocyte hypertrophy, chronic sterile inflammation, amyloid deposition, and increased interstitial fibrosis (Horn and Trafford 2016). Interestingly, fibrosis can occur in the absence of hypertension (Lin et al. 2008), suggesting that age-related fibrosis is driven by an independent mechanism. Together these cellular changes affect the heart at the tissue level, leading to myocardial remodelling which is characterised by increased left ventricular (LV) mass, due to the thickening and stiffening of the LV walls and interventricular septum, and a decrease in diastolic functions such as myocardial relaxation and peak contractility (Triposkiadis et al. 2019). The apparent lack of systolic dysfunction with age has led to age-associated HF often being considered as HF with preserved ejection fraction (HFpEF) (Borlaug and Paulus 2011). However, it is becoming evident that with age, the systolic functional reserve is also diminished, and the heart is unable to respond to periods of increased cardiac demand (Norman et al. 2011). Over 50% of hospitalised HF patients exhibit HFpEF and the prevalence is expected to increase at a rate of over 10% per decade with population ageing (Benjamin et al. 2019; Borlaug and Paulus 2011).
As discussed above, atherosclerosis is ageing-associated and therefore there is also an increased prevalence of coronary heart disease (CHD) in the older population. The critical outcome of CHD is plaque rupture, causing artery blockage and myocardial infarction. If the blockage is not rapidly removed and sustained ischemia occurs, extensive cardiomyocyte death and cellular necrosis may take place, impacting cardiac function which can result in death. Following MI, the hearts of surviving patients undergo a rapid maladaptive myocardial remodelling characterised by dilatation, hypertrophy, and the formation of a discrete collagen scar. Additionally, progressive ventricular remodelling can continue for weeks or months following MI (Sutton and Sharpe 2000). Most patients receiving intervention for MI are in the older age range (mean age of 65 years old), and age remains the most important predictor of outcomes following MI, with the older population having increased mortality and poorer functional outcomes than younger individuals. Patients older than 70 account for up to half of those admitted to hospital with MI and 80% of deaths due to MI occur in those aged over 65 years (McMechan and Adgey 1998). Age is associated with an increased risk of developing heart failure: in a study of 896 patients, Torabi et al. observed that in the six years after MI, 50% of patients aged younger than 65 years, 73% of patients aged between 65–75 years, and 87% of patients over 75 years had developed heart failure (Torabi et al. 2014).
Ageing and Cardiothoracic Surgery
Ageing impacts, and is the most important prognostic indicator of cardiothoracic surgical outcome (Duncan et al. 2020). Subsequent to surgery, including that required to treat CVD, older individuals have increased mortality and are at higher risk of developing organ injury (Benedetto et al. 2021; Baquero and Rich 2015) which can lead to the progression of multiple chronic conditions (DiMaria-Ghalili et al. 2014; Matsuura et al. 2020), disability (Hong et al. 2021), and lower quality of life (Koch et al. 2007). The cost of treating organ injury as a result of cardiac surgery alone is >£100M per year in the UK (Sergin et al. 2016).
Senescence as a Driver of Cardiovascular Disease
Cellular senescence is considered a hallmark of ageing (López-Otín et al. 2013) defined as a loss of the division potential of mitotic cells and the production of the senescence-associated secretory phenotype (SASP), a cocktail of proinflammatory cytokines, chemokines, and growth factors. Therefore, senescence contributes to age-related tissue dysfunction through impaired homeostasis and elevated inflammation (Wiley and Campisi 2021). Senescent cells accumulate in most organ tissues with age, as well as in several age-related diseases and can be driven by several interconnected mechanisms including mitochondrial dysfunction, increased reactive oxygen species (ROS), DNA damage and telomere attrition (Kuilman et al. 2010). The identification of senescent cells is difficult as there are currently no known specific markers that unambiguously identify all senescent cells (Sharpless and Sherr 2015). As such, multiple markers including senescence-associated β-galactosidase (SA-β-Gal) activity, expression of cyclin-dependent kinase inhibitors (p21Cip, p16Ink4a, and p53), presence of DNA damage or critically short telomere length, and lack of proliferation, are often used in combination with each other to facilitate the characterisation of senescent cells (González-Gualda et al. 2021; de Magalhaes and Passos 2018). Transgenic mice which allow pharmacogenetic induction of apoptosis in p16-expressing senescent cells have been developed to investigate the contribution of senescence to ageing and age-associated disease (Baker et al. 2011; Demaria et al. 2014). The p16-INKATTAC and p16-3MR transgenic mice share a similar approach, as they both contain an apoptosis-inducing protein transgene, driven by the p16Ink4a promoter, which is only functional after the administration of pharmacological agents (Baker et al. 2011; Demaria et al. 2014). More recently, senescent cells have been shown to upregulate pro-survival pathways, thus protecting themselves from a hostile microenvironment (Zhu et al. 2015; Wang 1995). This not only aids senescent cell identification but can be exploited scientifically, as inhibiting these pathways causes apoptosis in senescent cells (Zhu et al. 2015). Several compounds that inhibit these pathways, including Bcl-2 family members, p53/p21Cip, ephrins, phosphatidylinositol-4,5-bisphosphate 3-kinase, plasminogen-activated inhibitor-1 and 2 and hypoxia-inducible factor-1α, have now been identified as promoting apoptosis in senescent cells, and have therefore been termed senolytics (Zhu et al. 2015). Together, these tools for senescent cell elimination have been used to demonstrate that in preclinical models, senescence is causal to the pathophysiology of multiple age-related diseases, including several CVDs (Anderson et al. 2019; Dookun et al. 2020; Martin-Ruiz et al. 2020; Walaszczyk et al. 2019; Baker et al. 2016; Demaria et al. 2017; Childs et al. 2016; Roos et al. 2016).
Clinically, there is extensive evidence of the association between vessel wall senescence accumulation and atherosclerosis (Stojanović et al. 2020). Histological analysis of post-mortem tissues has identified that atherosclerotic vessels contain more senescent endothelial and vascular smooth muscle cells than aged-matched healthy arteries (Stojanović et al. 2020). Moreover, expression of p16 in diseased human coronary arteries positively correlates with plaque instability (Holdt et al. 2011), and the capability of cellular senescence to drive atherosclerosis is indicated by the increased risk of MI in relatively chronologically young patients with human progeria syndromes (Prakash et al. 2018).
Preclinically, LDL receptor-deficient and apolipoprotein E–deficient mouse models of atherosclerosis demonstrate that senescence accumulates in several cell populations in and around the atherogenic plaque during atherogenesis (Childs et al. 2016; Roos et al. 2016). These populations contribute to a proinflammatory environment and plaque development, indicated by the fact that senescent cell elimination reduces the expression of typical proinflammatory SASP proteins including matrix metalloproteinases (MMP) MMP-3, MMP-13, and the inflammatory cytokines IL-1α and tumour necrosis factor-α, and furthermore decreases plaque burden (Childs et al., 2016).
Senescence of immune cells, including the T cell population, is associated with atherogenesis and is a biomarker of CVD risk (Martin-Ruiz et al. 2020). Senescent, terminally differentiated CD8+ T-cells (TEMRA) are found inside unstable plaques and are an independent predictor of all-cause mortality in the elderly (Martin-Ruiz et al. 2020; Nakajima et al. 2002). While the studies of Childs et al. (2016) did not investigate if the elimination of senescent T-cells contributed to a reduced plaque burden, senolytics have been demonstrated to reduce T-cell immunosenescence in aged mice (Martin-Ruiz et al. 2020).
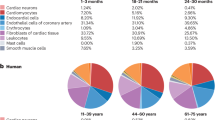
Senescence accumulates in cardiomyocytes, endothelial cells, cardiac fibroblasts and cardiac progenitor cells within the myocardium during ageing and is increased in the myocardium with age-associated CVD (Shimizu and Minamino 2019). Clinically, aged patients presenting with ventricular dysfunction have increased cardiomyocyte expression of p53 and p16, with increased expression being associated with hypertrophy at either an organ or cellular level (Song et al. 1999; Birks et al. 2008; Predmore et al. 2010). Cardiomyocyte senescence has also been linked to an increased risk of ventricular arrhythmias (Chadda et al. 2018). Endothelial cell senescence is observed with HF, particularly in patients suffering from HFpEF (Gevaert et al. 2017) and myocardial fibrosis and myofibroblast differentiation, which are increased with age and associated with HFpEF, are induced by senescent stimuli (Mellone et al. 2016; Zhu et al. 2013).
In vitro, paracrine SASP signalling from senescent myocardial cells, such as cardiomyocytes, endothelial cells, and fibroblasts, causes phenotypic alterations associated with cardiac remodelling. Several independent studies have also demonstrated that senescence promotes cardiac remodelling in preclinical studies: using senomorphic, senolytic, or pharmacogenetic approaches to reduce senescence, it has been demonstrated that attenuation of cardiac senescence decreases inflammation, cardiomyocyte hypertrophy and fibrosis in several different models of cardiovascular ageing (Anderson et al. 2019; Walaszczyk et al. 2019; Lewis-McDougall et al. 2019; Zhu et al. 2015; Baker et al. 2016; Iske et al. 2020; Demaria et al. 2017; Correia-Melo et al. 2019). In particular, elimination of senescent cells from aged mice also reduced LV mass and improved LV function (Walaszczyk et al. 2019; Zhu et al. 2015).
It is well-recognised that biological processes and phenomena associated with increased senescence are also associated with poorer surgical outcomes. Frailty, one of the best indicators of accumulated senescence, is prognostic of surgical outcome and increased age is associated with an increased peri-surgical likelihood of myocardial injury, accelerated progression of chronic conditions, disability, lower quality of life, and death (Koch et al. 2007; DiMaria-Ghalili et al. 2014; Matsuura et al. 2020; Nashef et al. 2012; Sun et al. 2021; Hong et al. 2021; Duncan et al. 2020). Preclinical studies have demonstrated a direct link between increased myocardial senescence, increased mortality and poorer outcomes following surgery (Walaszczyk et al. 2019; Iske et al. 2020). Interestingly, an accumulation of myocardial senescence is also associated with reduced resilience to isoproterenol-induced myocardial stress (Baker et al. 2016). Taken together, it is possible that increased myocardial senescence reduces a patient’s resilience to cardiac surgery and contributes to poorer outcomes. If this is the case, blood sampling and SASP quantification prior to surgery may allow for better risk stratification of patients and would also suggest that targeting senescence is a potential therapeutic intervention to improve surgical outcomes.
Mitochondrial Dysfunction and Oxidative Stress
Progressive or chronic alterations in mitochondrial function and bioenergetics such as increased production of ROS, mitochondrial DNA (mtDNA) damage and respiratory chain dysfunction, occur in both the heart and vascular system (Judge et al. 2005; Ungvari et al. 2007; Navarro and Boveris 2007) and are associated with several age-related CVDs (Poznyak et al. 2020). Reduced mitochondrial bioenergetics is suggested to be a key contributor to the progression of heart failure. For example, polymorphisms in the gene peroxisome proliferator-activated receptor-gamma coactivator (PGC-1α), responsible for controlling and maintaining mitochondrial content, are linked to an increased risk of hypertrophic cardiomyopathy (Oka et al. 2020). Furthermore, a significant positive relationship exists between myocardial ROS levels and LV contractile dysfunction in failing hearts (Ide et al. 2000). Experimentally, mice deficient in mitochondrial superoxide dismutase, a ROS scavenger, exhibit characteristics of dilated cardiomyopathy (Lebovitz et al. 1996).
Age-related mitochondrial dysfunction has also been proposed as a key driver of the atherogenic processes (Nowak et al. 2017). Oxidative modification of LDL, and its transport into the subendothelial space of the arterial wall, is considered an initiating event for atherosclerosis (Nowak et al. 2017). Increased ROS and oxidative stress also promote endothelial dysfunction and apoptosis, as well as influencing T-cell and vascular smooth muscle cell proliferation and apoptosis (Richardson et al. 2018; Nowak et al. 2017). Together, this increases inflammation and the development of the atherosclerotic plaque, ultimately contributing to plaque rupture (Madamanchi and Runge 2007; Anderson et al. 2018). PGC-1α dysfunction leading to increased ROS production can drive telomere shortening alongside both telomeric and non-telomeric DNA damage, accelerating vascular ageing and promoting atherosclerosis (Xiong et al. 2015). T cell mitochondrial function also declines with increased age (Ron-Harel et al. 2018) and T cells with dysfunctional mitochondria accelerate senescence in mice, leading to a premature ageing phenotype triggered by the induction of proinflammatory cytokines: so-called “inflammageing” (Desdín-Micó et al. 2020).
Similar to senescence, mitochondrial dysfunction is considered a key hallmark of ageing (López-Otín et al. 2013). However, only recently has the intricate and complex relationship between these two processes been identified. It is now clear that mitochondrial dysfunction is both a driver and consequence of cellular senescence (Chapman et al. 2019). Mitochondrial dysfunction, increased ROS production and associated oxidative stress activate the DNA damage response (DDR) and drive senescence (Chapman et al. 2019). ROS can cause DNA damage in the form of either single or double-stranded breaks (DSBs) throughout the genome, and telomeres appear to be particularly sensitive to ROS-induced damage due to their guanine-rich regions which have increased susceptibility to oxidation (Grollman and Moriya 1993). Single-strand DNA damage within telomeric regions can also accelerate telomere shortening due to the low efficiency of single-strand telomeric DNA damage repair (von Zglinicki et al. 2000). Telomeres containing single-strand DNA damage do not fully replicate during cellular division and shorten more in the following cellular division as the sequence beyond the damage is lost (von Zglinicki et al. 2000).
While many senescent cells have an increase in mitochondrial mass, their mitochondria are dysfunctional and demonstrate a decreased mitochondrial membrane potential, an increased proton leak and elevated ROS (Passos et al. 2007). Mitochondrial-derived ROS are a component of the SASP (Nelson et al. 2018), and mitochondria themselves are essential for the expression of SASP proteins (Correia-Melo et al. 2016). Senescent cells with depleted mitochondria lose their proinflammatory and pro-oxidant phenotype as well as the expression of the cyclin-dependent kinase inhibitors p21 and p16, however they remain in cell cycle arrest (Correia-Melo et al. 2016). Mitochondrial-mediated SASP production is at least in part controlled by a ROS–JNK signalling pathway which drives the release of cytoplasmic chromatin fragments, triggering the innate immunity cytosolic DNA-sensing cGAS-STING pathway (Vizioli et al. 2020). This in turn activates NFκB signalling, switching on the transcription of proinflammatory genes and the SASP (Vizioli et al. 2020). It has also been suggested that in senescent cells, increased mitochondrial outer membrane permeability (MOMP) allows the release of mtDNA which also activates cGAS-STING signalling, thus increasing proinflammatory gene expression. Further, the expression of pro-survival pathways may allow for sublethal apoptosis, termed minority MOMP, in which cytochrome c release and caspase activation induce DNA damage in the absence of apoptosis, contributing to genetic instability and perhaps deeper senescence (Birch and Passos 2017).
The mitochondrial genome is relatively sensitive to oxidative stress (Richter et al. 1988), further exacerbating the effects of mitochondrial dysfunction on disease pathophysiology: mitochondrial dysfunction ultimately leads to DNA damage in the mitochondrial genome and further mitochondrial dysfunction (Hollensworth et al. 2000). While the precise mechanisms for this remain unclear, the proximity of the mitochondrial genome to sites of ROS production and the lack of histones to provide protection have all been discussed (Miller et al. 2021). Together, these observations highlight the cyclical interactions between mitochondrial dysfunction, oxidative stress and senescence, and illustrate how the initiation of any of these processes could lead to a downward spiral in tissue function (Fig. 4.1).
Mitochondrial senescence and the SASP. (1) Mitochondrial dysfunction contributes to increased ROS production. (2) ROS can directly induce DNA damage in the form of double and single-stranded breaks in the genomic and telomeric DNA. DNA damage can also accelerate telomere shortening. Together these induce senescence. (3) Mitochondrial-derived ROS drives autocrine and paracrine mtDNA damage, further contributing to mitochondrial dysfunction. (4) Senescent cells have increased MOMP, allowing the release of caspase-activating cytochrome c. However, due to increased pro-survival protein expression in senescent cells, this release is insufficient to induce apoptosis (minority MOMP) and instead leads to increased mitochondrial and genomic DNA damage. (5) ROS activation of JNK inhibits tumour suppressor P53-binding protein 1 (53BP1) and thereby DSB end restriction, contributing to the release of cytoplasmic chromatin fragments which are detected by the cGAS-STING pathway (6), an innate immune system double-stranded DNA sensor which responds to CCF and (7) mtDNA release, due to increased mitochondrial membrane permeability, with NFκβ activation and expression of proinflammatory SASP genes which increases inflammation (8). These proinflammatory proteins, together with ROS, maintain autocrine cellular senescence but also induce senescence in surrounding tissues (bystander effect), propagating mitochondrial dysfunction and leading to a cascade in mitochondrial dysfunction and senescence
In the heart, the cardiomyocytes of aged mice display a decline in expression of most mitochondrial genes, including those involved in the electron transport chain (Anderson et al. 2019). Moreover, and demonstrating that oxidative stress can drive cardiomyocyte senescence, transgenic mice overexpressing the pro-oxidant enzyme monoamine oxidase A (MAO-A), specifically in the cardiomyocytes, show increased myocardial senescence and exhibit myocardial dysfunction (Anderson et al. 2019).
Mitochondria also have mechanistic roles in acute CVD. This is notably seen in the context of ischaemia-reperfusion injury (IRI) which, though not an age-related disease per se, does primarily affect the older population since it is a significant consequence of reperfusion therapies used to return the blood supply to the myocardium following a heart attack (Aversano et al. 2002). IRI is a highly complex and multifactorial process (Neri et al. 2017; Halladin 2015; Hausenloy and Yellon 2013), but mitochondrial ROS generation is key to the pathophysiology driving cardiomyocyte death, endothelial dysfunction and microvascular occlusion, and promotes inflammation in this injury setting (Kalogeris et al. 2012; Neri et al. 2017; Hausenloy and Yellon 2013). As ROS can act as a contributor to mitochondrial Ca2+ overload, it can further increase ROS levels, creating a feedback loop whereby a state of Ca2+ overload is maintained and ROS generation is increased (Penna et al. 2009; Murphy and Steenbergen 2007; Kaneko et al. 1990). Unfortunately, while it is clear mitochondria and oxidative stress contribute to the pathophysiology of IRI, and several preclinical studies have reported antioxidants to protect against cardiac IRI (Dhalla et al. 2000), these results have failed to transfer clinically (Hausenloy and Yellon 2013; Desmet et al. 2011; Siddiqi et al. 2014; Atar et al. 2015). However, it may be that targeting the downstream effects of oxidative stress such as senescence, rather than oxidative stress itself, is a preferable strategy which may provide a longer treatment window to attenuate maladaptive remodelling post-cardiac IRI. In preclinical models of cardiac IRI, increased senescence has been observed in multiple cell types within the area of myocardium that experienced increased oxidative stress (Dookun et al. 2020). Interestingly, elimination of senescence following cardiac IRI using a senolytic approach improved cellular respiration, attenuated inflammation and remodelling, and enhanced revascularisation, all of which were associated with an improved myocardial function (Dookun et al. 2020). Numerous clinical conditions besides MI including stroke, organ transplantation, and peripheral vascular disease (Widgerow 2014; Kalogeris et al. 2012) are linked to the occurrence of IRI, however, it has yet to be identified if senescence contributes to pathophysiology in these disease settings.
Telomeres and Telomerase in Cardiovascular Disease, Replicative Senescence and Beyond
The association between telomere length and CVD is well-established and reviewed (Hoffmann et al. 2021). Telomerase reporter mice and knockout models, such as those lacking expression of either the telomerase RNA component (TERC) or telomerase reverse transcriptase (TERT), have aided our understanding of how experimentally-induced myocardial senescence can contribute to CVD (Blasco et al. 1997; Leri et al. 2003; Richardson et al. 2012, 2018). However, it is now apparent that telomeres and telomerase interact with CVD beyond their roles in regulating replicative senescence.
It had long been debated as to how predominantly post-mitotic cardiomyocytes, which rarely proliferate and therefore are protected from replicative stress, can acquire a senescent phenotype. Data from recent studies, including our own, have now determined that senescence can also be induced by DNA-damaging agents including oxidative stress, which cause DNA damage foci that are preferentially located within telomeres, termed telomere-associated foci (TAF) (Hewitt et al. 2012; Anderson et al. 2019). During physiological ageing, cardiomyocytes in humans and mice accumulate TAF (Anderson et al. 2019). TAF are persistent (they are not as efficiently repaired as non-telomeric damaged DNA), induce senescence via activation of the p16 and p21 pathways, and occur independently of telomere shortening and proliferation (Anderson et al. 2019) (Fig. 4.2). Pharmacogenetic elimination of senescent cells from aged mice reduces the number of TAF-positive cardiomyocytes but does not affect telomere length (Anderson et al. 2019), suggesting that TAF accumulation is the primary trigger of cardiomyocyte senescence during ageing.
Cardiomyocyte senescence is induced independently of telomere shortening. Mitochondrial dysfunction and increased ROS generation induce telomeric DNA damage in cardiomyocytes. While DNA damage occurs in both genomic and telomeric regions, genomic DNA damage is repaired, resulting in a transient DDR that may not be sufficient for senescence establishment. Alternatively, irreparable and therefore persistent DNA damage at telomeres causes a persistent DDR and cardiomyocyte senescence, which is associated with SASP-mediated inflammation
Telomerase activity is protective against senescence: cells stably transfected with human telomerase can divide indefinitely (Bodnar et al. 1998). Conversely, inhibition of either TERT or TERC promotes senescence, reduces lifespan and accelerates ageing in cells and small animal models (Shay and Wright 2004). Clinically, patients suffering from mutations in genes that encode TERT demonstrate an accelerated ageing phenotype that includes an increased prevalence of CVD (Armanios et al. 2005; Vulliamy et al. 2001; Ballew and Savage 2013; Khincha et al. 2017; Lina et al. 2008). While telomere maintenance contributes to these anti-senescence effects, TERT has activity independent of telomere preservation that may also protect against senescence. In particular, mitochondrial-localised TERT expression improves mitochondrial function, reduces mitochondrial ROS production, and protects against DNA damage and instability in both genomic and mitochondrial DNA (Haendeler et al. 2009; Ahmed et al. 2008; Fleisig et al. 2016). Mice which constitutively express TERT but are cancer-resistant (due to enhanced expression of the tumour suppressors p53, p16, and p19ARF) demonstrate decreased ageing-associated pathologies and an increase in median lifespan (Tomás-Loba et al. 2008). Interestingly, this anti-aged phenotype was associated not only with telomere maintenance but also a reduction in both genomic and telomere-associated DNA damage (Tomás-Loba et al. 2008), supporting a senoprotective role of telomerase that is independent of telomere maintenance.
The senescent phenotype is associated with a reduction in both canonical and non-canonical telomerase function, as p53 attenuates TERT expression via the inhibition of PGC-1α, which upregulates TERT expression in proliferative cells. As such, a crisis point must be reached in conditions of oxidative stress whereby sufficient DDR signalling activates p53, and presumably the senescence pathway, which then inhibits both mitochondrial biogenesis and the defensive functions of TERT. This facilitates escalating ROS generation, DNA damage (both mitochondrial and genomic) and ROS-mediated telomere shortening (Fig. 4.3). Indicating this may contribute to CVD are the observations that, in both cardiomyocytes and T-cells, p53 downregulates PGC-1α, resulting in increased mitochondrial oxidative damage (Villeneuve et al. 2013; Schank et al. 2020).
TERT mediated protection from senescence. (1) In conditions of increased oxidative stress, PGC-1α promotes mitochondrial biogenesis and upregulates TERT expression. (2) Through canonical roles and telomerase function, TERT maintains telomeres, and oxidative stress promotes the export of TERT from the nucleus. (3) Through unknown mechanisms TERT translocates into the mitochondria. (4) Increases in mitochondrial-located TERT are associated with improved electron transport chain function and a decrease in ROS, processes which will attenuate DNA damage and telomere shortening. (5) TERT interacts with mtDNA and protects mtDNA from damage, maintaining mitochondrial biogenesis and thereby function. (A) If telomeres reach a crisis point or DNA damage is persistent, activation of the classical senescence pathways that converge in p53 activation (B). (C) p53 inhibits PGC-1α and therefore both mitochondrial biogenesis and TERT expression, preventing the defensive functions of TERT enabling increased oxidative stress, telomere attrition, and further DNA damage
TERT is increased in multiple cell populations including cardiomyocytes in response to cardiac injury (Richardson et al. 2012). While the functionality of this expression is not yet known, given the post-mitotic nature of cardiomyocytes, it is arguably unlikely that TERT is upregulated to maintain telomeres during extensive proliferation. Instead, TERT upregulation could provide a mechanism for the cardiomyocyte, and potentially other cell types, to protect against mitochondrial dysfunction and oxidative stress, which in turn may protect against DNA damage and senescence/apoptosis. In support of this notion, recent studies have demonstrated that mice which overexpress mitochondrial TERT, but lacked nuclear TERT, had improved mitochondrial respiration, attenuated myocardial remodelling and increased revascularization after they were subjected to cardiac IRI; these factors contributed to improved cardiac function (Ale-Agha et al. 2021). These benefits overlap with the outcome of the studies described earlier, in which senescence was eliminated following cardiac IRI (Dookun et al. 2020).
While the relationship between telomere length, atherosclerosis and the development of CHD has been studied extensively (Harst et al. 2007; Samani et al. 2001; Brouilette et al. 2007), little is known regarding the interactions between non-canonical telomerase activities and these diseases. T-cells express telomerase to maintain telomere length and protect against senescence (Weng et al. 1996). It has been demonstrated that oxidative stress can suppress telomerase activity within T-cells (Callender et al. 2018) which could accelerate T-cell senescence through two mechanisms: (i) as a result of replication in the absence of telomerase and (ii) through increased mitochondrial dysfunction and ROS generation due to suppression of mitochondrial TERT activity. Given that T-cell senescence is associated with a proinflammatory phenotype, chronic oxidative stress within an atherosclerotic plaque could contribute to disease pathophysiology. Furthermore, subpopulations of T-cells, such as TReg cells, are anti-atherogenic, and therefore senescence in these populations could also promote atherosclerosis.
Taken together this data suggests that if the pro-tumourigenic activities of TERT can be overcome, enhancing telomerase expression may have therapeutic value for a wide range of CVDs through senescence protection (telomere-dependent and -independent mechanisms), improved mitochondrial function, reduced oxidative stress and reduced inflammation. Interestingly statins, one of the most potent drug families which can slow the progression of atherosclerosis (by delaying age-related inflammatory changes in the arterial vessel wall), have been shown to stimulate telomerase activity (Bennaceur et al. 2014). Although, it remains unknown if stimulation of TERT’s non-canonical activities contributes to the benefits associated with statin use.
Mitochondrial Dysfunction of T Lymphocytes as a Potential Mechanism of Enhanced Inflammation Post-myocardial Infarction
In vertebrates, premature ageing of the immune system (termed “immunosenescence”) is mainly linked to thymic involution and changes in cellular immunity as a response to pathogens, such as recurrent viral infections, throughout life (Müller et al. 2013). These include a reduction in circulating lymphocytes and naïve T lymphocytes, the loss of stimulatory T lymphocyte co-receptors, the increase of oligoclonal memory cells, and finally, increased levels of proinflammatory cytokines. Immune ageing has been proven to correlate with higher mortality across different age groups (Strindhall et al. 2007; Alpert et al. 2019). Relative lymphopenia in over 50,000 otherwise healthy middle-aged Americans has recently been identified as a strong predictor of overall mortality as well as cardiovascular mortality (Zidar et al. 2019). In the Newcastle 85+ study, we have previously shown that women exhibited higher lymphocyte counts and a higher frequency of naïve T-cells, paralleled by lower cardiovascular mortality, without differences in non-cardiovascular mortality (Martin-Ruiz et al. 2020; Spyridopoulos et al. 2016). We also found in a different study that MI leads to accelerated immunosenescence and shorter leukocyte telomere length (Hoffmann et al. 2015; Spyridopoulos et al. 2009). Finally, fewer lymphocytes following MI also predicted higher mortality in our patients (Boag et al. 2015; Spray et al. 2021). Lymphocyte proliferation can be enhanced in vitro by activating telomerase (Richardson et al. 2018). We have shown that T lymphocyte proliferation can be induced in a TERT-dependent manner in vitro by the telomerase activator (Richardson et al. 2018), TA-65MD® (T.A. Sciences, New York, USA). Further, TA-65 treatment has been shown to improve the outcome of mice after experimental MI, a function that required the presence of mitochondrial TERT (Ale-Agha et al. 2021; Jabbour et al. 2019). Importantly, mice that express mitochondrial-localised but lack nuclear-localised TERT are phenotypically normal and show no obvious signs of hyperproliferative diseases (Ale-Agha et al. 2021), suggesting that the TA-65-enhanced mitochondrial-TERT expression is not pro-tumourigenic. Our TACTIC (Telomerase Activator to Reverse Immunosenescence in Acute Coronary Syndrome: A Double-Blind, Phase II, Randomised Controlled Trial) study 5 is the first randomised clinical trial using a telomerase activator in patients following myocardial infarction, and will investigate whether treatment reduces inflammation while simultaneously enhancing immunity following MI.
Inflammation Is an Important Residual Risk Post-myocardial Infarction
Following myocardial infarction, secondary prevention for patients nowadays consists of targeting their residual risk, which is thought to be largely attributed to either hypercholesterolemia (which can be targeted with statins and proprotein convertase subtilisin/kexin type 9 inhibitors) or platelet aggregation (which can be treated with dual antiplatelet therapy). Recently inflammation, as quantified by high-sensitivity C-reactive protein (hsCRP), has been added to this. The CANTOS trial has successfully proven that reducing inflammation in CAD patients with elevated hsCRP (>2 mg/L) improves outcomes (Ridker et al. 2017). In a more detailed subanalysis of the CANTOS trial, the authors found that the relative improvement of outcome correlated directly to the magnitude of hsCRP reduction (Ridker et al. 2018). Secondly, adverse remodelling is also propagated by excessive inflammation; early studies with the IL-1 antagonist Anakinra following MI suggest treatment can reduce the progression to heart failure (Abbate et al. 2020). However, a major limitation of the CANTOS trial was the effect of IL-1β blockade on immunity, as patients in the treatment group had a higher risk for infections as well as a higher risk of dying from sepsis. Clearly, there is a need for anti-inflammatory targets post-MI without compromising immunity; targeting immune ageing directly could present a viable option.
Mitophagy and Age-Related Cardiovascular Disease
In the heart, the mitochondria can metabolically adapt to changes in cardiac stress, ensuring they meet the high energy demand of the heart. However, as previously mentioned, ageing is associated with altered cardiac mitochondrial metabolism and mitochondrial dysfunction (Lesnefsky et al. 2016; Lesnefsky and Hoppel 2006). In order to prevent cardiomyocytes containing damaged mitochondria from undergoing cell death, the adaptive process mitophagy facilitates the efficient removal of dysfunctional and damaged mitochondria within a cell. Thus, the physiological consequences of mitophagy prevent ROS-mediated damage to proteins and DNA, and prevents inflammation. Hence, mitophagy maintains cardiac homeostasis by controlling a dynamic balance between the elimination of mitochondria and mitochondrial biogenesis, maintaining a healthy mitochondrial network. Mitophagy is defined as mitochondrial autophagy and is a selective form of autophagy specifically eliminating dysfunctional mitochondria in cells (Narendra et al. 2008). Autophagy is a key catabolic pathway in cellular quality control. During autophagy, damaged organelles are engulfed by autophagosomes and are subsequently degraded by fusion with lysosomes. There are two known mechanisms for mitophagy: adaptor-mediated and receptor-mediated. The former pathway functions via Phosphatase and Tensin Homolog (PTEN)-induced putative kinase 1 (PINK) and Parkin-mediated mitophagy, and this is the most well-characterised pathway. When a mitochondrion is dysfunctional or damaged, PINK1 accumulates on the outer surface of the mitochondrion (Lazarou et al. 2015). Here, PINK1 phosphorylates ubiquitin and the E3 ubiquitin ligase, Parkin, which ubiquitinates key mitochondrion-associated proteins (Jin et al. 2010; Matsuda et al. 2010; Narendra et al. 2008). These signals are bound by autophagic adaptor proteins such as p62/SQSTM1 that subsequently bind with microtubule-associated protein 1A/1B-light chain 3 (LC3), which is tethered on the phagophore membranes (Gustafsson and Dorn 2019), hence sequestering the ubiquitinated mitochondrion within the autophagosome. This fuses with a lysosome leading to the degradation of the damaged mitochondria (Pankiv et al. 2007; Lazarou et al. 2015). As such, impaired mitophagy leads to an accumulation of “old”, defective mitochondria. While it remains unclear if impaired mitophagy contributes to senescence induction, is a result of senescence, or both, there are clear interactions between senescence-inducing pathways, the senescent phenotype and attenuated mitophagy. The senescence regulator p53 can interact with Parkin by blocking the translocation of Parkin, p53 can suppress mitophagy (Ahmad et al. 2015).
Impaired mitophagy has been implicated in the pathology of various age-related CVDs (Dominic et al. 2014). In healthy young hearts, there is an underlying level of baseline mitophagy essential for maintaining the cellular homeostasis in an energy-efficient heart, and for responding and adapting to stress. Thus, the mitophagy pathways are tightly regulated. However, there is evidence that a decrease in mitophagy is associated with ageing (Zhou et al. 2017) and also with the pathogenesis of the CVD (Taneike et al. 2010), due to the accumulation of dysfunctional mitochondrial which reduces the ability of the heart to adapt to stress. In patients with the late stages of heart disease, a low number of autophagosomes is associated with a poor prognosis (Saito et al. 2016). This accounts for the pathological changes which are observed in the cardiac mitochondria of CVD patients, including the presence of giant megamitochondria, the loss, reorientation, or change in the shape of the cristae, formation of intramitochondrial rods and crystalloids (Hoppel et al. 2009).
In atherosclerosis, destabilisation of the atherosclerotic plaques has been associated with deficient mitophagy which in turn is linked to cell death, cell stress, and ROS accumulation in the plaques (Madamanchi and Runge 2007; Grootaert et al. 2018). Various studies have shown that within atherosclerotic plaques from human samples and mouse models, autophagy is either decreased or dysfunctional, shown by reduced expression of autophagic markers p62 and LC3-II (Razani et al. 2012; Sergin et al. 2016; Swaminathan et al. 2014). Activation of mitophagy has been suggested as a possible mechanism to slow disease progression. Antioxidant therapeutic strategies, such as melatonin treatment (which has anti-inflammatory properties) (Ma et al. 2018), activate mitophagy and as a consequence stabilise atherosclerotic plaques.
One important role of mitophagy is to suppress inflammation, which can lead to myocardial damage and is described as a key feature of CVD. ROS excretion and release of mtDNA from dysfunctional mitochondria activate the NLRP3 inflammasome (Nakahira et al. 2011; Heid et al. 2013) leading to inflammation in the heart. However, mitophagy can remove these damaged mitochondria and thus has an important role in suppressing inflammation. This was highlighted when transgenic mice with cardiac-specific overexpression of Beclin1 (a key regulator of autophagy) were exposed to lipopolysaccharide-induced sepsis, and an activation of the PINK1/Parkin mitophagy pathway was observed—this was noted alongside reduced inflammation, fibrosis and improved cardiac function in the mice (Sun et al. 2018).
Mouse models which are Parkin-deficient or overexpress Parkin have illustrated that loss of mitophagy accelerates ageing in the heart (Kubli et al. 2013; Hoshino et al. 2013) or that enhancement of mitophagy delays cardiac ageing (Hoshino et al. 2013; Gao et al. 2021), respectively, highlighting the benefits of promoting Parkin-mediated mitophagy. Furthermore, following MI, cardiac-specific Parkin-deficient mice show that mitophagy is essential to reduce cardiac injury. After MI, the Parkin-deficient mice had reduced survival and developed larger infarcts: when compared to the control mice, these infarcts had reduced mitophagy and increased dysfunctional mitochondria in the border zone, accounting for the observed heart failure (Kubli et al. 2013). Hence it has been demonstrated that loss of mitophagy exacerbates cardiac injury, leading to reduced survival.
Myocardial IRI leads to mitochondrial damage accompanied by an initial adaptive autophagic response to cardiac injury (Gustafsson and Gottlieb 2009), which is shown by an increase in mitophagy in both cardiomyocytes and platelets (Zhang et al. 2018). However, this response may be short-lived: Billia and colleagues showed that acute cardiac IRI ultimately leads to a reduction of autophagy flux, as seen in heart tissue from patients with end-stage heart failure (Billia et al. 2011). In the tissue, PINK1 protein levels were reduced compared to control samples, thus leading to the accumulation of damaged mitochondria, severe oxidative stress and apoptosis of cardiomyocytes (Campos et al. 2016). Studies from transgenic mouse models illustrate the initial cardioprotective role of mitophagy. In one example, cardiac-specific deletion of Drp1 (a mitochondrial fission mediator) leads to an accumulation of elongated and damaged mitochondria, and suppresses mitophagy, thus promoting cardiac dysfunction and increasing susceptibility to IRI (Ikeda et al. 2015). An alternative mitophagy pathway is via the autophagy receptor Fun14 domain-containing protein 1 (FUNDC1), which interacts directly with LC3. In response to IRI-induced hypoxia, the Fund1 knockout mouse model is unable to protect the heart from IRI due to a lack of mitophagy specifically (Zhang et al. 2017). It was later shown that general autophagy remained unchanged (Xu et al. 2022). Similarly, Pink1-deficient mice are more susceptible to IRI (Siddall et al. 2013), a phenotype which is rescued when Pink1 is overexpressed, as this reduces cell death and decreases infarct size (Wang et al. 2015). Thus, it is the induction of mitophagy that contributes to the cardioprotective effect of attenuating cardiac injury. This has been proposed as a strategy to protect the cardiac environment in CVD, although this needs to be carefully appraised as excessive mitochondrial removal in response to IRI can increase cardiomyocyte death (Lesnefsky et al. 2017).
The association between mitophagy and senescence in CVD is evidenced by two independent studies which demonstrated that restoration of mitophagy prevents age-related CVDs by delaying cellular senescence. D-galactose-induced accelerated ageing mice display a phenotype which, when untreated, leads to increased cardiac cellular senescence and impaired cardiac function: mice were administered acacetin (Cui et al. 2018) or Kanglexin (KLX) (Li et al. 2022) and both treatments improved the cardiac function of these mice. In the former study, the authors found that the underlying mechanism for this improvement was protection from cellular senescence which was attributed to an upregulation of mitophagy (Hong et al. 2021). After treatment with KLX, a similar increase in mitophagy is noted, specifically in senescent cardiomyocytes, which was shown to be due to the enhanced stability of Parkin (Li et al. 2022). Moreover, treatment of a mouse model of accelerated ageing (caused by activation of the major proinflammatory NF-κB pathway) with rapamycin (a known autophagy and mitophagy activator) reduced cellular senescence, prevented age-related frailty and reduced histopathological evidence of age-related disease in several organs including the heart (Correia-Melo et al. 2019). Thus, enhancing mitophagy could represent a useful strategy for targeting age/senescence-related CVD. Manipulation of mitophagy is an attractive model to delay cardiac ageing and disease, however there are challenges as the level of mitophagy must be tightly regulated and is dose-dependent. Increasing autophagy excessively can lead to unnecessary degradation of cellular organelles and proteins leading to counterproductive energy deficiency.
Accelerated Ageing and Cardiovascular Disease: Chemotherapy-Induced Cardiotoxicity
Though cancer survival is improving globally, many anticancer interventions leave survivors with lasting off-target effects. Though radiation therapy has been reported to increase frailty, especially in the context of neurocognitive defects from cranial radiotherapy (Armstrong et al. 2013), pharmacological approaches can also promote an ageing phenotype in various organ systems. Given the increasing population of cancer survivors, understanding the long-term impacts of these off-target effects is a priority for clinicians, and chemotherapy-induced cardiotoxicity (CIC) is a major player in the field, which plagues even newer-generation chemotherapies such as tyrosine kinase inhibitors (Chaar et al. 2018). The anthracycline drug class, which remains a cornerstone of anticancer treatment for countless patients globally, is one of the most well-studied examples of CIC-inducing drugs. Most commonly used for breast cancer and sarcoma treatments, these drugs have long been associated with cardiovascular toxicity, most notoriously in a delayed symptomatic form, whereby cardiovascular phenomena arise many years after therapy conclusion. Typically, patients may present with arrhythmias, reduced LV function or fulminant heart failure, and interventions at this late stage in the disease are often inefficient. In the past, anthracycline-induced cardiotoxicity was categorised as either acute, early-onset, or late-onset. More recently, however, studies by Cardinale et al. have pointed towards anthracycline-induced cardiotoxicity (AIC) being one continuous phenomenon, with the temporal difference in presentation being perhaps due to patient risk factors and cumulative anthracycline dosage (Cardinale et al. 2015). This paradigm shift has facilitated a re-appraisal of how AIC may play out over time mechanistically, and this has allowed for more intuitive parallels to be drawn between progressive AIC and an accelerated ageing phenotype in the cardiac environment (Mitry et al. 2020; Maejima et al. 2008; Rebbaa et al. 2003). There is increasing interest in the concept that anthracycline-induced senescence may contribute to the long-term cardiotoxicity associated with these drugs (Saleh et al. 2020). Senescence induction is a recognised response to chemotherapy (Perkins et al. 2020; Ewald et al. 2010; Wang et al. 2020; Saleh et al. 2020; Wyld et al. 2020) and cancer survivors demonstrate an accelerated ageing phenotype overall, including increased comorbidity manifesting as conditions usually associated with ageing, including increased cardiac events, peripheral neuropathy, a decline in bone health and cognitive decline, all consistent with an increase in systemic senescence (Cupit-Link et al. 2017). With regards to the heart, the commonly used anthracycline doxorubicin (DOX), for which DNA damage is a primary therapeutic mechanism, can induce fibroblasts and cardiomyocytes to senescence in vitro (Zhang et al. 2009; Maejima et al. 2008; Fourie et al. 2019). Murine studies have also implicated the accumulation of senescent cells within the heart as causal to AIC (Demaria et al. 2017). Using a transgenic model that allows the identification and elimination of p16-expressing senescent cells, Demaria et al. demonstrated that following exposure to DOX, senescence is increased, and cardiac function is reduced (Demaria et al. 2017). However, the elimination of senescent cells prevented the functional decline (Demaria et al. 2017). Similarly, elimination of senescence with the senolytic navitoclax reduced markers of cardiotoxicity and restored cardiac function in DOX-treated mice (Lérida-Viso et al. 2022). These data suggest that senescence is an active participant in the progression to myocardial dysfunction and not just a passive bystander. Interestingly, first-generation TERT-knockout mice (which retain long telomeres but lack the non-canonical activities of TERT) are more sensitive to DOX-induced cardiotoxicity than littermates (Werner et al. 2008), further supporting the notion that mitochondrial TERT is senoprotective. Moreover, cardiomyocyte-specific overexpression of TERT also protects from DOX-induced cardiac dysfunction (Chatterjee et al. 2021). Upon DOX exposure, TERT overexpression enhances TERT mitochondrial translocation, which protects against mitochondrial dysfunction and ROS generation (Chatterjee et al. 2021). While this study did not quantify senescence, the obvious DNA-damaging properties of DOX coupled with mitochondrial dysfunction/ROS being drivers of cardiomyocyte senescence prompt the idea that mitochondrial TERT may prevent or delay cardiomyocyte senescence, preventing senescence-induced myocardial remodelling and cardiac dysfunction. To date, most studies regarding CIC have focused on the anthracycline class of drugs. However, due to aforementioned improvements in cancer survivorship, it is now becoming evident that delayed and chronic cardiotoxicity may also be a factor with other classes of chemotherapeutic agents (Florescu et al. 2013; Michel et al. 2019) Interestingly, chemotherapeutics including paclitaxel, temozolomide, and cisplatin can induce senescence in murine skin (Demaria et al. 2017). Despite these studies, it remains unknown if senescence induction underlies the cardiotoxicity of these chemotherapies. Furthermore, as with ageing, interactions between the senescent myocardium and the adaptive immune system may contribute to CIC.
Figure 4.4 summarises how intrinsic and extrinsic stresses may drive mitochondrial dysfunction and oxidative stress leading senescence and CVD.
Intrinsic and extrinsic stresses drive mitochondrial dysfunction and oxidative stress. This stress leads to increased TERT expression, which is senoprotective. If stress outweighs these protective functions, DNA damage leads to p53 activation, which downregulates TERT expression, and expression of p53 targets leads to senescence. Senescence drives local and systemic inflammation via the SASP, leading to age-related disease and a cascade of oxidative stress through a positive feedback loop. Activation of mitochondrial TERT with TA65 or pharmacological elimination of senescent cells reduces oxidative stress at a cellular- and organ-level, attenuating the cascade of oxidative stress. DNA-damaging agents such as anthracyclines may directly induce cellular senescence, contributing to increased systemic inflammation and oxidative stress through the same mechanisms
Viral Infection, Inflammation, Senescence, and Cardiovascular Disease
The presence of senescent immune cells can lead to a reduction in effective immunity, enhanced inflammation (by driving the secretion of inflammatory cytokines via the SASP), and as a result of endothelial and myocardial cell targeting through cytotoxic, pro-apoptotic mediators (granzyme, perforin) as previously reviewed (Liu et al. 2020). Ageing is related to chronic low-grade sterile inflammation, increased immunosenescence and a high risk for cardiovascular-related mortality. We have observed that viral infection may accelerate immunosenescence as cytomegalovirus (CMV)-seropositive patients demonstrate signs of accelerated immune ageing following myocardial infarction, that seem to link with impaired myocardial healing (Spyridopoulos et al. 2009; Hoffmann et al. 2015). Importantly, in patients with previous CMV infection, where there is a known abundance of virus-specific cytotoxic T lymphocytes, we have found an (i) increased Th1 proinflammatory response, (ii) enhanced infiltration of the heart with T lymphocytes, and finally (iii) adverse cardiac remodelling (Martin-Ruiz et al. 2020; Hoffmann et al. 2015; Spyridopoulos et al. 2016; Spray et al. 2021). Accumulation of T-cell senescence is associated with higher mortality, age-related myocardial decline and a predisposition towards CVDs (Martin-Ruiz et al. 2020; Hoffmann et al. 2015; Spyridopoulos et al. 2016). Together, this suggests that CMV infection mediates immunosenescence, and the associated immune cell dysregulation contributes to excessive inflammation and thereby adverse remodelling following a myocardial infarction.
Acute cardiovascular complications are also associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and it is established that age is the greatest risk for mortality and morbidity post-infection (Xie et al. 2022). It is possible that these associations are a result of viral induction of senescence: it has been demonstrated that similar to CMV, albeit in a more acute setting, SARS-CoV-2 infection increases immune cell senescence, compromises cytotoxic T-cell activity, and that the SASP has been implicated in contributing to cytokine storm in coronavirus disease 2019 (COVID-19) patients (Lee et al. 2022). While the interaction between SARS-CoV-2 and senescence is not yet fully understood, the best indication that senescence contributes to COVID-19 are studies which have shown that the elimination of senescent cells improves the survival of aged mice against ß-coronavirus infection (Camell et al. 2021), and those that show that senescence elimination post SARS-CoV-2 infection reduced inflammation and mitigated a COVID-19-reminiscent lung disease in both hamsters and mice (Lee et al. 2021). Studies are underway to explore whether the senolytic Fisetin can reduce the requirement for hospitalisation in a cohort of older COVID-19 patients (Camell et al. 2021). Given the association between senescence and chronic diseases, including those of the cardiovascular system, it is possible that SARS-CoV-2-induced senescence may underlie several post-infection conditions, perhaps including so-called “long-COVID”.
References
Abbate A, Trankle CR, Buckley LF, Lipinski MJ, Appleton D, Kadariya D, Canada JM, Carbone S, Roberts CS, Abouzaki N, Melchior R, Christopher S, Turlington J, Mueller G, Garnett J, Thomas C, Markley R, Wohlford GF, Puckett L, Chazal HM, Chiabrando JG, Bressi E, Buono MGD, Schatz A, Vo C, Dixon DL, Biondi-Zoccai GG, Kontos MC, Tassell BWV (2020) Interleukin-1 blockade inhibits the acute inflammatory response in patients with ST-Segment–elevation myocardial infarction. J Am Heart Assoc 9(5):e014941. https://doi.org/10.1161/JAHA.119.014941
Ahmad T, Sundar IK, Lerner CA, Gerloff J, Tormos AM, Yao H, Rahman I (2015) Impaired mitophagy leads to cigarette smoke stress-induced cellular senescence: implications for chronic obstructive pulmonary disease. FASEB J 29(7):2912–2929. https://doi.org/10.1096/fj.14-268276
Ahmed S, JoF P, Birket MJ, Beckmann T, Brings S, Peters H, Birch-Machin MA, von Zglinicki T, Saretzki G (2008) Telomerase does not counteract telomere shortening but protects mitochondrial function under oxidative stress. J Cell Sci 121(7):1046–1053. https://doi.org/10.1242/jcs.019372
Ale-Agha N, Jakobs P, Goy C, Zurek M, Rosen J, Dyballa-Rukes N, Metzger S, Greulich J, von Ameln F, Eckermann O, Unfried K, Brack F, Grandoch M, Thielmann M, Kamler M, Gedik N, Kleinbongard P, Heinen A, Heusch G, Gödecke A, Altschmied J, Haendeler J (2021) Mitochondrial telomerase reverse transcriptase protects from myocardial ischemia/reperfusion injury by improving complex I composition and function. Circulation 144(23):1876–1890. https://doi.org/10.1161/circulationaha.120.051923
Alpert A, Pickman Y, Leipold M, Rosenberg-Hasson Y, Ji X, Gaujoux R, Rabani H, Starosvetsky E, Kveler K, Schaffert S, Furman D, Caspi O, Rosenschein U, Khatri P, Dekker CL, Maecker HT, Davis MM, Shen-Orr SS (2019) A clinically meaningful metric of immune age derived from high-dimensional longitudinal monitoring. Nat Med 25(3):487–495. https://doi.org/10.1038/s41591-019-0381-y
Anderson R, Richardson GD, Passos JF (2018) Mechanisms driving the ageing heart. Exp Gerontol 109:5–15. https://doi.org/10.1016/j.exger.2017.10.015
Anderson R, Lagnado A, Maggiorani D, Walaszczyk A, Dookun E, Chapman J, Birch J, Salmonowicz H, Ogrodnik M, Jurk D, Proctor C, Correia-Melo C, Victorelli S, Fielder E, Berlinguer-Palmini R, Owens A, Greaves LC, Kolsky KL, Parini A, Douin-Echinard V, LeBrasseur NK, Arthur HM, Tual-Chalot S, Schafer MJ, Roos CM, Miller JD, Robertson N, Mann J, Adams PD, Tchkonia T, Kirkland JL, Mialet-Perez J, Richardson GD, Passos JF (2019) Length-independent telomere damage drives post-mitotic cardiomyocyte senescence. EMBO J. https://doi.org/10.15252/embj.2018100492
Armanios M, Chen J-L, Chang Y-PC, Brodsky RA, Hawkins A, Griffin CA, Eshleman JR, Cohen AR, Chakravarti A, Hamosh A, Greider CW (2005) Haploinsufficiency of telomerase reverse transcriptase leads to anticipation in autosomal dominant dyskeratosis congenita. Proc Natl Acad Sci U S A 102(44):15960–15964. https://doi.org/10.1073/pnas.0508124102
Armstrong GT, Reddick WE, Petersen RC, Santucci A, Zhang N, Srivastava D, Ogg RJ, Hillenbrand CM, Sabin N, Krasin MJ, Kun L, Pui CH, Hudson MM, Robison LL, Krull KR (2013) Evaluation of memory impairment in aging adult survivors of childhood acute lymphoblastic leukemia treated with cranial radiotherapy. J Natl Cancer Inst 105(12):899–907. https://doi.org/10.1093/jnci/djt089
Atar D, Arheden H, Berdeaux A, Bonnet JL, Carlsson M, Clemmensen P, Cuvier V, Danchin N, Dubois-Rande JL, Engblom H, Erlinge D, Firat H, Halvorsen S, Hansen HS, Hauke W, Heiberg E, Koul S, Larsen AI, Le Corvoisier P, Nordrehaug JE, Paganelli F, Pruss RM, Rousseau H, Schaller S, Sonou G, Tuseth V, Veys J, Vicaut E, Jensen SE (2015) Effect of intravenous TRO40303 as an adjunct to primary percutaneous coronary intervention for acute ST-elevation myocardial infarction: MITOCARE study results. Eur Heart J 36(2):112–119. https://doi.org/10.1093/eurheartj/ehu331
Aversano T, Aversano LT, Passamani E, Knatterud GL, Terrin ML, Williams DO, Forman SA (2002) Thrombolytic therapy vs primary percutaneous coronary intervention for myocardial infarction in patients presenting to hospitals without on-site cardiac surgery: a randomized controlled trial. JAMA 287(15):1943–1951. https://doi.org/10.1001/jama.287.15.1943
Baker DJ, Wijshake T, Tchkonia T, LeBrasseur NK, Childs BG, van de Sluis B, Kirkland JL, van Deursen JM (2011) Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature 479(7372):232–236. https://doi.org/10.1038/nature10600
Baker DJ, Childs BG, Durik M, Wijers ME, Sieben CJ, Zhong J, Saltness RA, Jeganathan KB, Verzosa GC, Pezeshki A, Khazaie K, Miller JD, van Deursen JM (2016) Naturally occurring p16Ink4a-positive cells shorten healthy lifespan. Nature 530(7589):184–189. https://doi.org/10.1038/nature16932
Ballew BJ, Savage SA (2013) Updates on the biology and management of dyskeratosis congenita and related telomere biology disorders. Expert Rev Hematol 6(3):327–337. https://doi.org/10.1586/ehm.13.23
Baquero GA, Rich MW (2015) Perioperative care in older adults. J Geriatr Cardiol 12(5):465–469. https://doi.org/10.11909/j.issn.1671-5411.2015.05.018
Benedetto U, Sinha S, Dimagli A, Cooper G, Mariscalco G, Uppal R, Moorjani N, Krasopoulos G, Kaura A, Field M, Trivedi U, Kendall S, Angelini GD, Akowuah EF, Tsang G (2021) Decade-long trends in surgery for acute Type A aortic dissection in England: a retrospective cohort study. Lancet Reg Health - Europe 7:100131. https://doi.org/10.1016/j.lanepe.2021.100131
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR et al (2019) Heart Disease and Stroke Statistics-2019 Update: a report from the American Heart Association. Circulation 139(10):e56–e528. https://doi.org/10.1161/CIR.0000000000000659
Bennaceur K, Atwill M, Al Zhrany N, Hoffmann J, Keavney B, Breault D, Richardson G, von Zglinicki T, Saretzki G, Spyridopoulos I (2014) Atorvastatin induces T cell proliferation by a telomerase reverse transcriptase (TERT) mediated mechanism. Atherosclerosis 236(2):312–320. https://doi.org/10.1016/j.atherosclerosis.2014.07.020
Billia F, Hauck L, Konecny F, Rao V, Shen J, Mak TW (2011) PTEN-inducible kinase 1 (PINK1)/Park6 is indispensable for normal heart function. Proc Natl Acad Sci U S A 108(23):9572–9577. https://doi.org/10.1073/pnas.1106291108
Birch J, Passos JF (2017) Targeting the SASP to combat ageing: mitochondria as possible intracellular allies? BioEssays 39(5):1600235. https://doi.org/10.1002/bies.201600235
Birks EJ, Latif N, Enesa K, Folkvang T, Luong LA, Sarathchandra P, Khan M, Ovaa H, Terracciano CM, Barton PJR, Yacoub MH, Evans PC (2008) Elevated p53 expression is associated with dysregulation of the ubiquitin-proteasome system in dilated cardiomyopathy. Cardiovasc Res 79(3):472–480. https://doi.org/10.1093/cvr/cvn083
Blasco MA, Lee HW, Hande MP, Samper E, Lansdorp PM, DePinho RA, Greider CW (1997) Telomere shortening and tumour formation by mouse cells lacking telomerase RNA. Cell 91(1):25–34. https://doi.org/10.1016/s0092-8674(01)80006-4
Boag SE, Das R, Shmeleva EV, Bagnall A, Egred M, Howard N, Bennaceur K, Zaman A, Keavney B, Spyridopoulos I (2015) T lymphocytes and fractalkine contribute to myocardial ischemia/reperfusion injury in patients. J Clin Invest 125(8):3063–3076. https://doi.org/10.1172/jci80055
Bodnar AG, Ouellette M, Frolkis M, Holt SE, Chiu CP, Morin GB, Harley CB, Shay JW, Lichtsteiner S, Wright WE (1998) Extension of life-span by introduction of telomerase into normal human cells. Science 279(5349):349–352. https://doi.org/10.1126/science.279.5349.349
Borlaug BA, Paulus WJ (2011) Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J 32(6):670. https://doi.org/10.1093/eurheartj/ehq426
Brouilette SW, Moore JS, McMahon AD, Thompson JR, Ford I, Shepherd J, Packard CJ, Samani NJ (2007) Telomere length, risk of coronary heart disease, and statin treatment in the West of Scotland Primary Prevention Study: a nested case-control study. Lancet 369(9556):107–114. https://doi.org/10.1016/s0140-6736(07)60071-3
Callender LA, Carroll EC, Beal RWJ, Chambers ES, Nourshargh S, Akbar AN, Henson SM (2018) Human CD8+ EMRA T cells display a senescence-associated secretory phenotype regulated by p38 MAPK. Aging Cell 17(1):e12675. https://doi.org/10.1111/acel.12675
Camell CD, Yousefzadeh MJ, Zhu Y, Prata LGPL, Huggins MA, Pierson M, Zhang L, O’Kelly RD, Pirtskhalava T, Xun P, Ejima K, Xue A, Tripathi U, Espindola-Netto JM, Giorgadze N, Atkinson EJ, Inman CL, Johnson KO, Cholensky SH, Carlson TW, LeBrasseur NK, Khosla S, O’Sullivan MG, Allison DB, Jameson SC, Meves A, Li M, Prakash YS, Chiarella SE, Hamilton SE, Tchkonia T, Niedernhofer LJ, Kirkland JL, Robbins PD (2021) Senolytics reduce coronavirus-related mortality in old mice. Science 373(6552):eabe4832. https://doi.org/10.1126/science.abe4832
Campos JC, Bozi LH, Bechara LR, Lima VM, Ferreira JC (2016) Mitochondrial quality control in cardiac diseases. Front Physiol 7:479. https://doi.org/10.3389/fphys.2016.00479
Cardinale D, Colombo A, Bacchiani G, Tedeschi I, Meroni CA, Veglia F, Civelli M, Lamantia G, Colombo N, Curigliano G, Fiorentini C, Cipolla CM (2015) Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation 131(22):1981–1988. https://doi.org/10.1161/CIRCULATIONAHA.114.013777
Chaar M, Kamta J, Ait-Oudhia S (2018) Mechanisms, monitoring, and management of tyrosine kinase inhibitors-associated cardiovascular toxicities. Onco Targets Ther 11:6227–6237. https://doi.org/10.2147/OTT.S170138
Chadda KR, Ajijola OA, Vaseghi M, Shivkumar K, Huang CL, Jeevaratnam K (2018) Ageing, the autonomic nervous system and arrhythmia: from brain to heart. Ageing Res Rev 48:40–50. https://doi.org/10.1016/j.arr.2018.09.005
Chapman J, Fielder E, Passos JF (2019) Mitochondrial dysfunction and cell senescence: deciphering a complex relationship. FEBS Lett 593(13):1566–1579. https://doi.org/10.1002/1873-3468.13498
Chatterjee S, Hofer T, Costa A, Lu D, Batkai S, Gupta SK, Bolesani E, Zweigerdt R, Megias D, Streckfuss-Bömeke K, Brandenberger C, Thum T, Bär C (2021) Telomerase therapy attenuates cardiotoxic effects of doxorubicin. Mol Ther 29(4):1395–1410. https://doi.org/10.1016/j.ymthe.2020.12.035
Childs BG, Baker DJ, Wijshake T, Conover CA, Campisi J, van Deursen JM (2016) Senescent intimal foam cells are deleterious at all stages of atherosclerosis. Science 354(6311):472–477. https://doi.org/10.1126/science.aaf6659
Childs BG, Gluscevic M, Baker DJ, Laberge RM, Marquess D, Dananberg J, van Deursen JM (2017) Senescent cells: an emerging target for diseases of ageing. Nat Rev Drug Discov 16(10):718–735. https://doi.org/10.1038/nrd.2017.116
Correia-Melo C, Marques FD, Anderson R, Hewitt G, Hewitt R, Cole J, Carroll BM, Miwa S, Birch J, Merz A, Rushton MD, Charles M, Jurk D, Tait SW, Czapiewski R, Greaves L, Nelson G, Bohlooly YM, Rodriguez-Cuenca S, Vidal-Puig A, Mann D, Saretzki G, Quarato G, Green DR, Adams PD, von Zglinicki T, Korolchuk VI, Passos JF (2016) Mitochondria are required for pro-ageing features of the senescent phenotype. EMBO J 35(7):724–742. https://doi.org/10.15252/embj.201592862
Correia-Melo C, Birch J, Fielder E, Rahmatika D, Taylor J, Chapman J, Lagnado A, Carroll BM, Miwa S, Richardson G, Jurk D, Oakley F, Mann J, Mann DA, Korolchuk VI, Passos JF (2019) Rapamycin improves healthspan but not inflammaging in nfκb1−/− mice. Aging Cell 18(1):e12882. https://doi.org/10.1111/acel.12882
Cui S, Xue L, Yang F, Dai S, Han Z, Liu K, Liu B, Yuan Q, Cui Z, Zhang Y, Xu F, Chen Y (2018) Postinfarction hearts are protected by premature senescent cardiomyocytes via GATA4-dependent CCN1 secretion. J Am Heart Assoc 7(18):e009111. https://doi.org/10.1161/JAHA.118.009111
Cupit-Link MC, Kirkland JL, Ness KK, Armstrong GT, Tchkonia T, LeBrasseur NK, Armenian SH, Ruddy KJ, Hashmi SK (2017) Biology of premature ageing in survivors of cancer. ESMO Open 2(5):e000250. https://doi.org/10.1136/esmoopen-2017-000250
de Magalhaes JP, Passos JF (2018) Stress, cell senescence and organismal ageing. Mech Ageing Dev 170:2–9. https://doi.org/10.1016/j.mad.2017.07.001
Demaria M, Ohtani N, Youssef Sameh A, Rodier F, Toussaint W, Mitchell James R, Laberge R-M, Vijg J, Van Steeg H, Dollé Martijn ET, Hoeijmakers Jan HJ, de Bruin A, Hara E, Campisi J (2014) An essential role for senescent cells in optimal wound healing through secretion of PDGF-AA. Dev Cell 31(6):722–733. https://doi.org/10.1016/j.devcel.2014.11.012
Demaria M, O’Leary MN, Chang J, Shao L, Liu S, Alimirah F, Koenig K, Le C, Mitin N, Deal AM, Alston S, Academia EC, Kilmarx S, Valdovinos A, Wang B, de Bruin A, Kennedy BK, Melov S, Zhou D, Sharpless NE, Muss H, Campisi J (2017) Cellular senescence promotes adverse effects of chemotherapy and cancer relapse. Cancer Discov 7(2):165–176. https://doi.org/10.1158/2159-8290.Cd-16-0241
Desdín-Micó G, Soto-Heredero G, Aranda JF, Oller J, Carrasco E, Gabandé-Rodríguez E, Blanco EM, Alfranca A, Cussó L, Desco M, Ibañez B, Gortazar AR, Fernández-Marcos P, Navarro MN, Hernaez B, Alcamí A, Baixauli F, Mittelbrunn M (2020) T cells with dysfunctional mitochondria induce multimorbidity and premature senescence. Science 368(6497):1371–1376. https://doi.org/10.1126/science.aax0860
Desmet W, Bogaert J, Dubois C, Sinnaeve P, Adriaenssens T, Pappas C, Ganame J, Dymarkowski S, Janssens S, Belmans A, Van de Werf F (2011) High-dose intracoronary adenosine for myocardial salvage in patients with acute ST-segment elevation myocardial infarction. Eur Heart J 32(7):867–877. https://doi.org/10.1093/eurheartj/ehq492
Dhalla NS, Elmoselhi AB, Hata T, Makino N (2000) Status of myocardial antioxidants in ischemia–reperfusion injury. Cardiovasc Res 47(3):446–456. https://doi.org/10.1016/s0008-6363(00)00078-x
DiMaria-Ghalili RA, Sullivan-Marx EM, Compher C (2014) Inflammation, functional status, and weight loss during recovery from cardiac surgery in older adults: a pilot study. Biol Res Nurs 16(3):344–352. https://doi.org/10.1177/1099800413503489
Dominic EA, Ramezani A, Anker SD, Verma M, Mehta N, Rao M (2014) Mitochondrial cytopathies and cardiovascular disease. Heart 100(8):611–618. https://doi.org/10.1136/heartjnl-2013-304657
Dookun E, Walaszczyk A, Redgrave R, Palmowski P, Tual-Chalot S, Suwana A, Chapman J, Jirkovsky E, Donastorg Sosa L, Gill E, Yausep OE, Santin Y, Mialet-Perez J, Andrew Owens W, Grieve D, Spyridopoulos I, Taggart M, Arthur HM, Passos JF, Richardson GD (2020) Clearance of senescent cells during cardiac ischemia-reperfusion injury improves recovery. Aging Cell 19(10):e13249. https://doi.org/10.1111/acel.13249
Duncan AE, Kartashov A, Robinson SB, Randall D, Zhang K, Luber J, James RA, Halvorson S, Bokesch P (2020) Risk factors, resource use, and cost of postoperative low cardiac output syndrome. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2020.06.125
Ewald JA, Desotelle JA, Wilding G, Jarrard DF (2010) Therapy-induced senescence in cancer. J Natl Cancer Inst 102(20):1536–1546. https://doi.org/10.1093/jnci/djq364
Fleisig HB, Hukezalie KR, Thompson CA, Au-Yeung TT, Ludlow AT, Zhao CR, Wong JM (2016) Telomerase reverse transcriptase expression protects transformed human cells against DNA-damaging agents, and increases tolerance to chromosomal instability. Oncogene 35(2):218–227. https://doi.org/10.1038/onc.2015.75
Florescu M, Cinteza M, Vinereanu D (2013) Chemotherapy-induced cardiotoxicity. Maedica (Bucur) 8(1):59–67
Fourie C, Davis T, Kriel J, Engelbrecht AM (2019) The paracrine effects of fibroblasts on Doxorubicin-treated breast cancer cells. Exp Cell Res 381(2):280–287. https://doi.org/10.1016/j.yexcr.2019.05.020
Gao B, Yu W, Lv P, Liang X, Sun S, Zhang Y (2021) Parkin overexpression alleviates cardiac aging through facilitating K63-polyubiquitination of TBK1 to facilitate mitophagy. Biochim Biophys Acta Mol Basis Dis 1867(1):165997. https://doi.org/10.1016/j.bbadis.2020.165997
Gevaert AB, Shakeri H, Leloup AJ, Van Hove CE, De Meyer GRY, Vrints CJ, Lemmens K, Van Craenenbroeck EM (2017) Endothelial senescence contributes to heart failure with preserved ejection fraction in an aging mouse model. Circ Heart Fail 10(6). https://doi.org/10.1161/circheartfailure.116.003806
González-Gualda E, Baker AG, Fruk L, Muñoz-Espín D (2021) A guide to assessing cellular senescence in vitro and in vivo. FEBS J 288(1):56–80. https://doi.org/10.1111/febs.15570
Grollman AP, Moriya M (1993) Mutagenesis by 8-oxoguanine: an enemy within. Trends Genet 9(7):246–249. https://doi.org/10.1016/0168-9525(93)90089-Z
Grootaert MOJ, Roth L, Schrijvers DM, De Meyer GRY, Martinet W (2018) Defective autophagy in atherosclerosis: to die or to senesce? Oxid Med Cell Longev 2018:7687083. https://doi.org/10.1155/2018/7687083
Gustafsson AB, Dorn GW 2nd (2019) Evolving and expanding the roles of mitophagy as a homeostatic and pathogenic process. Physiol Rev 99(1):853–892. https://doi.org/10.1152/physrev.00005.2018
Gustafsson AB, Gottlieb RA (2009) Autophagy in ischemic heart disease. Circ Res 104(2):150–158. https://doi.org/10.1161/CIRCRESAHA.108.187427
Haendeler J, Dröse S, Büchner N, Jakob S, Altschmied J, Goy C, Spyridopoulos I, Zeiher AM, Brandt U, Dimmeler S (2009) Mitochondrial telomerase reverse transcriptase binds to and protects mitochondrial DNA and function from damage. Arterioscler Thromb Vasc Biol 29(6):929–935. https://doi.org/10.1161/ATVBAHA.109.185546
Halladin N (2015) Oxidative and inflammatory biomarkers of ischemia and reperfusion injuries. Danish Med J 62(4):B5054
Harst P, Steege G, Boer RA, Voors AA, Hall AS, Mulder MJ, Gilst WH, Veldhuisen DJ (2007) Telomere length of circulating leukocytes is decreased in patients with chronic heart failure. J Am Coll Cardiol 49(13):1459–1464. https://doi.org/10.1016/j.jacc.2007.01.027
Hausenloy DJ, Yellon DM (2013) Myocardial ischemia-reperfusion injury: a neglected therapeutic target. J Clin Invest 123(1):92–100. https://doi.org/10.1172/JCI62874
Heid ME, Keyel PA, Kamga C, Shiva S, Watkins SC, Salter RD (2013) Mitochondrial reactive oxygen species induces NLRP3-dependent lysosomal damage and inflammasome activation. J Immunol 191(10):5230–5238. https://doi.org/10.4049/jimmunol.1301490
Hewitt G, Jurk D, Marques FDM, Correia-Melo C, Hardy T, Gackowska A, Anderson R, Taschuk M, Mann J, Passos JF (2012) Telomeres are favoured targets of a persistent DNA damage response in ageing and stress-induced senescence. Nat Commun 3:708
Hoffmann J, Shmeleva EV, Boag SE, Fiser K, Bagnall A, Murali S, Dimmick I, Pircher H, Martin-Ruiz C, Egred M, Keavney B, von Zglinicki T, Das R, Todryk S, Spyridopoulos I (2015) Myocardial ischemia and reperfusion leads to transient CD8 immune deficiency and accelerated immunosenescence in CMV-seropositive patients. Circ Res 116(1):87–98. https://doi.org/10.1161/circresaha.116.304393
Hoffmann J, Richardson G, Haendeler J, Altschmied J, Andrés V, Spyridopoulos I (2021) Telomerase as a therapeutic target in cardiovascular disease. Arterioscler Thromb Vasc Biol 41(3):1047–1061. https://doi.org/10.1161/ATVBAHA.120.315695
Holdt LM, Sass K, Gäbel G, Bergert H, Thiery J, Teupser D (2011) Expression of Chr9p21 genes CDKN2B (p15(INK4b)), CDKN2A (p16(INK4a), p14(ARF)) and MTAP in human atherosclerotic plaque. Atherosclerosis 214(2):264–270. https://doi.org/10.1016/j.atherosclerosis.2010.06.029
Hollensworth SB, Shen C, Sim JE, Spitz DR, Wilson GL, LeDoux SP (2000) Glial cell type-specific responses to menadione-induced oxidative stress. Free Radic Biol Med 28(8):1161–1174. https://doi.org/10.1016/s0891-5849(00)00214-8
Hong YX, Wu WY, Song F, Wu C, Li GR, Wang Y (2021) Cardiac senescence is alleviated by the natural flavone acacetin via enhancing mitophagy. Aging (Albany NY) 13(12):16381–16403. https://doi.org/10.18632/aging.203163
Hoppel CL, Tandler B, Fujioka H, Riva A (2009) Dynamic organization of mitochondria in human heart and in myocardial disease. Int J Biochem Cell Biol 41(10):1949–1956. https://doi.org/10.1016/j.biocel.2009.05.004
Horn MA, Trafford AW (2016) Aging and the cardiac collagen matrix: novel mediators of fibrotic remodelling. J Mol Cell Cardiol 93:175–185. https://doi.org/10.1016/j.yjmcc.2015.11.005
Hoshino A, Mita Y, Okawa Y, Ariyoshi M, Iwai-Kanai E, Ueyama T, Ikeda K, Ogata T, Matoba S (2013) Cytosolic p53 inhibits Parkin-mediated mitophagy and promotes mitochondrial dysfunction in the mouse heart. Nat Commun 4:2308. https://doi.org/10.1038/ncomms3308
Ide T, Tsutsui H, Kinugawa S, Suematsu N, Hayashidani S, Ichikawa K, Utsumi H, Machida Y, Egashira K, Takeshita A (2000) Direct evidence for increased hydroxyl radicals originating from superoxide in the failing myocardium. Circ Res 86(2):152–157. https://doi.org/10.1161/01.RES.86.2.152
Ikeda Y, Shirakabe A, Maejima Y, Zhai P, Sciarretta S, Toli J, Nomura M, Mihara K, Egashira K, Ohishi M, Abdellatif M, Sadoshima J (2015) Endogenous Drp1 mediates mitochondrial autophagy and protects the heart against energy stress. Circ Res 116(2):264–278. https://doi.org/10.1161/CIRCRESAHA.116.303356
Iske J, Seyda M, Heinbokel T, Maenosono R, Minami K, Nian Y, Quante M, Falk CS, Azuma H, Martin F, Passos JF, Niemann CU, Tchkonia T, Kirkland JL, Elkhal A, Tullius SG (2020) Senolytics prevent mt-DNA-induced inflammation and promote the survival of aged organs following transplantation. Nat Commun 11(1):4289. https://doi.org/10.1038/s41467-020-18039-x
Jabbour E, Mullighan CG, Pullarkat VA, Lacayo NJ, Bajel A, Rubnitz J, Leonard J, Khaw SL, Vear SI, Alexander T, Norris R, Salem A, Schmidt M, Tong B, Zhou Y, Ross JA, Bensman L, Jacobson A, Stock W (2019) Combination BCL-2 inhibitor therapy with venetoclax and navitoclax in patients with relapsed/refractory acute lymphoblastic leukemia and lymphoblastic lymphoma. Clin Lymphoma Myeloma Leuk 19:S184–S185. https://doi.org/10.1016/j.clml.2019.07.022
Jin SM, Lazarou M, Wang C, Kane LA, Narendra DP, Youle RJ (2010) Mitochondrial membrane potential regulates PINK1 import and proteolytic destabilization by PARL. J Cell Biol 191(5):933–942. https://doi.org/10.1083/jcb.201008084
Judge S, Jang YM, Smith A, Hagen T, Leeuwenburgh C (2005) Age-associated increases in oxidative stress and antioxidant enzyme activities in cardiac interfibrillar mitochondria: implications for the mitochondrial theory of aging. FASEB J 19(3):1–21. https://doi.org/10.1096/fj.04-2622fje
Kalogeris T, Baines CP, Krenz M, Korthuis RJ (2012) Cell biology of ischemia/reperfusion injury. Int Rev Cell Mol Biol 298:229–317. https://doi.org/10.1016/B978-0-12-394309-5.00006-7
Kaneko M, Singal PK, Dhalla NS (1990) Alterations in heart sarcolemmal Ca2+-ATPase and Ca2+-binding activities due to oxygen free radicals. Basic Res Cardiol 85(1):45–54. https://doi.org/10.1007/bf01907013
Khincha PP, Bertuch AA, Agarwal S, Townsley DM, Young NS, Keel S, Shimamura A, Boulad F, Simoneau T, Justino H, Kuo C, Artandi S, McCaslin C, Cox DW, Chaffee S, Collins BF, Giri N, Alter BP, Raghu G, Savage SA (2017) Pulmonary arteriovenous malformations: an uncharacterised phenotype of dyskeratosis congenita and related telomere biology disorders. Eur Respir J 49(1):1601640. https://doi.org/10.1183/13993003.01640-2016
Koch CG, Li L, Lauer M, Sabik J, Starr NJ, Blackstone EH (2007) Effect of functional health-related quality of life on long-term survival after cardiac surgery. Circulation 115(6):692–699. https://doi.org/10.1161/CIRCULATIONAHA.106.640573
Kubli DA, Quinsay MN, Gustafsson AB (2013) Parkin deficiency results in accumulation of abnormal mitochondria in aging myocytes. Commun Integr Biol 6(4):e24511. https://doi.org/10.4161/cib.24511
Kuilman T, Michaloglou C, Mooi WJ, Peeper DS (2010) The essence of senescence. Genes Dev 24(22):2463–2479. https://doi.org/10.1101/gad.1971610
Lazarou M, Sliter DA, Kane LA, Sarraf SA, Wang C, Burman JL, Sideris DP, Fogel AI, Youle RJ (2015) The ubiquitin kinase PINK1 recruits autophagy receptors to induce mitophagy. Nature 524(7565):309–314. https://doi.org/10.1038/nature14893
Lebovitz RM, Zhang H, Vogel H, Cartwright J, Dionne L, Lu N, Huang S, Matzuk MM (1996) Neurodegeneration, myocardial injury, and perinatal death in mitochondrial superoxide dismutase-deficient mice. Proc Natl Acad Sci 93(18):9782–9787. https://doi.org/10.1073/pnas.93.18.9782
Lee S, Yu Y, Trimpert J, Benthani F, Mairhofer M, Richter-Pechanska P, Wyler E, Belenki D, Kaltenbrunner S, Pammer M et al (2021) Virus-induced senescence is a driver and therapeutic target in COVID-19. Nature 599(7884):283–289. https://doi.org/10.1038/s41586-021-03995-1
Lee KA, Flores RR, Jang IH, Saathoff A, Robbins PD (2022) Immune senescence, immunosenescence and aging. Front Aging 3:900028. https://doi.org/10.3389/fragi.2022.900028
Leri A, Franco S, Zacheo A, Barlucchi L, Chimenti S, Limana F, Nadal-Ginard B, Kajstura J, Anversa P, Blasco MA (2003) Ablation of telomerase and telomere loss leads to cardiac dilatation and heart failure associated with p53 upregulation. EMBO J 22(1):131–139. https://doi.org/10.1093/emboj/cdg013
Lérida-Viso A, Estepa-Fernández A, Morellá-Aucejo Á, Lozano-Torres B, Alfonso M, Blandez JF, Bisbal V, Sepúlveda P, García-Fernández A, Orzáez M, Martínez-Máñez R (2022) Pharmacological senolysis reduces doxorubicin-induced cardiotoxicity and improves cardiac function in mice. Pharmacol Res:106356. https://doi.org/10.1016/j.phrs.2022.106356
Lesnefsky EJ, Hoppel CL (2006) Oxidative phosphorylation and aging. Ageing Res Rev 5(4):402–433. https://doi.org/10.1016/j.arr.2006.04.001
Lesnefsky EJ, Chen Q, Hoppel CL (2016) Mitochondrial metabolism in aging heart. Circ Res 118(10):1593–1611. https://doi.org/10.1161/CIRCRESAHA.116.307505
Lesnefsky EJ, Chen Q, Tandler B, Hoppel CL (2017) Mitochondrial dysfunction and myocardial ischemia-reperfusion: implications for novel therapies. Annu Rev Pharmacol Toxicol 57:535–565. https://doi.org/10.1146/annurev-pharmtox-010715-103335
Lewis-McDougall FC, Ruchaya PJ, Domenjo-Vila E, Shin Teoh T, Prata L, Cottle BJ, Clark JE, Punjabi PP, Awad W, Torella D, Tchkonia T, Kirkland JL, Ellison-Hughes GM (2019) Aged-senescent cells contribute to impaired heart regeneration. Aging Cell 18(3):e12931. https://doi.org/10.1111/acel.12931
Li HM, Liu X, Meng ZY, Wang L, Zhao LM, Chen H, Wang ZX, Cui H, Tang XQ, Li XH, Han WN, Bai X, Lin Y, Liu H, Zhang Y, Yang BF (2022) Kanglexin delays heart aging by promoting mitophagy. Acta Pharmacol Sin 43(3):613–623. https://doi.org/10.1038/s41401-021-00686-5
Lin J, Lopez EF, Jin Y, Van Remmen H, Bauch T, Han H-C, Lindsey ML (2008) Age-related cardiac muscle sarcopenia: combining experimental and mathematical modeling to identify mechanisms. Exp Gerontol 43(4):296–306. https://doi.org/10.1016/j.exger.2007.12.005
Lina B-V, Inderjeet D, Hannah T, Abraham A, Ben Zion G, Alexander V, Tom V (2008) Expanding the clinical phenotype of autosomal dominant dyskeratosis congenita caused by TERT mutations. Haematologica 93(6):943–944. https://doi.org/10.3324/haematol.12317
Liu D, Richardson G, Benli FM, Park C, de Souza JV, Bronowska AK, Spyridopoulos I (2020) Inflammageing in the cardiovascular system: mechanisms, emerging targets, and novel therapeutic strategies. Clin Sci (Lond) 134(17):2243–2262. https://doi.org/10.1042/cs20191213
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G (2013) The hallmarks of aging. Cell 153(6):1194–1217. https://doi.org/10.1016/j.cell.2013.05.039
Ma S, Chen J, Feng J, Zhang R, Fan M, Han D, Li X, Li C, Ren J, Wang Y, Cao F (2018) Melatonin ameliorates the progression of atherosclerosis via mitophagy activation and NLRP3 inflammasome inhibition. Oxid Med Cell Longev 2018:9286458. https://doi.org/10.1155/2018/9286458
Madamanchi NR, Runge MS (2007) Mitochondrial dysfunction in atherosclerosis. Circ Res 100(4):460–473. https://doi.org/10.1161/01.RES.0000258450.44413.96
Maejima Y, Adachi S, Ito H, Hirao K, Isobe M (2008) Induction of premature senescence in cardiomyocytes by doxorubicin as a novel mechanism of myocardial damage. Aging Cell 7(2):125–136. https://doi.org/10.1111/j.1474-9726.2007.00358.x
Martin-Ruiz C, Hoffmann J, Shmeleva E, Zglinicki TV, Richardson G, Draganova L, Redgrave R, Collerton J, Arthur H, Keavney B, Spyridopoulos I (2020) CMV-independent increase in CD27-CD28+ CD8+ EMRA T cells is inversely related to mortality in octogenarians. NPJ Aging Mech Dis 6:3. https://doi.org/10.1038/s41514-019-0041-y
Matsuda N, Sato S, Shiba K, Okatsu K, Saisho K, Gautier CA, Sou YS, Saiki S, Kawajiri S, Sato F, Kimura M, Komatsu M, Hattori N, Tanaka K (2010) PINK1 stabilized by mitochondrial depolarization recruits Parkin to damaged mitochondria and activates latent Parkin for mitophagy. J Cell Biol 189(2):211–221. https://doi.org/10.1083/jcb.200910140
Matsuura R, Iwagami M, Moriya H, Ohtake T, Hamasaki Y, Nangaku M, Doi K, Kobayashi S, Noiri E (2020) The clinical course of acute kidney disease after cardiac surgery: a retrospective observational study. Sci Rep 10(1):6490. https://doi.org/10.1038/s41598-020-62981-1
McMechan SR, Adgey AA (1998) Age related outcome in acute myocardial infarction. Elderly people benefit from thrombolysis and should be included in trials. BMJ 317(7169):1334–1335. https://doi.org/10.1136/bmj.317.7169.1334
Mellone M, Hanley CJ, Thirdborough S, Mellows T, Garcia E, Woo J, Tod J, Frampton S, Jenei V, Moutasim KA, Kabir TD, Brennan PA, Venturi G, Ford K, Herranz N, Lim KP, Clarke J, Lambert DW, Prime SS, Underwood TJ, Vijayanand P, Eliceiri KW, Woelk C, King EV, Gil J, Ottensmeier CH, Thomas GJ (2016) Induction of fibroblast senescence generates a non-fibrogenic myofibroblast phenotype that differentially impacts on cancer prognosis. Aging (Albany NY) 9(1):114–132. https://doi.org/10.18632/aging.101127
Michel L, Rassaf T, Totzeck M (2019) Cardiotoxicity from immune checkpoint inhibitors. Int J Cardiol Heart Vasc 25:100420. https://doi.org/10.1016/j.ijcha.2019.100420
Miller KN, Dasgupta N, Liu T, Adams PD, Vizioli MG (2021) Cytoplasmic chromatin fragments-from mechanisms to therapeutic potential. Elife 10. https://doi.org/10.7554/eLife.63728
Mitry MA, Laurent D, Keith BL, Sira E, Eisenberg CA, Eisenberg LM, Joshi S, Gupte S, Edwards JG (2020) Accelerated cardiomyocyte senescence contributes to late-onset doxorubicin-induced cardiotoxicity. Am J Physiol Cell Physiol 318(2):C380–C391. https://doi.org/10.1152/ajpcell.00073.2019
Montecucco F, Carbone F, Schindler TH (2016) Pathophysiology of ST-segment elevation myocardial infarction: novel mechanisms and treatments. Eur Heart J 37(16):1268–1283. https://doi.org/10.1093/eurheartj/ehv592
Moriya J (2019) Critical roles of inflammation in atherosclerosis. J Cardiol 73(1):22–27. https://doi.org/10.1016/j.jjcc.2018.05.010
Müller L, Fülöp T, Pawelec G (2013) Immunosenescence in vertebrates and invertebrates. Immun Ageing 10(1):12. https://doi.org/10.1186/1742-4933-10-12
Murphy E, Steenbergen C (2007) Preconditioning: the mitochondrial connection. Annu Rev Physiol 69(1):51–67. https://doi.org/10.1146/annurev.physiol.69.031905.163645
Nakahira K, Haspel JA, Rathinam VA, Lee SJ, Dolinay T, Lam HC, Englert JA, Rabinovitch M, Cernadas M, Kim HP, Fitzgerald KA, Ryter SW, Choi AM (2011) Autophagy proteins regulate innate immune responses by inhibiting the release of mitochondrial DNA mediated by the NALP3 inflammasome. Nat Immunol 12(3):222–230. https://doi.org/10.1038/ni.1980
Nakajima T, Schulte S, Warrington KJ, Kopecky SL, Frye RL, Goronzy JJ, Weyand CM (2002) T-cell-mediated lysis of endothelial cells in acute coronary syndromes. Circulation 105(5):570–575. https://doi.org/10.1161/hc0502.103348
Narendra D, Tanaka A, Suen DF, Youle RJ (2008) Parkin is recruited selectively to impaired mitochondria and promotes their autophagy. J Cell Biol 183(5):795–803. https://doi.org/10.1083/jcb.200809125
Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, Lockowandt U (2012) EuroSCORE II. Eur J Cardiothorac Surg 41(4):734–744; discussion 744-735. https://doi.org/10.1093/ejcts/ezs043
Navarro A, Boveris A (2007) The mitochondrial energy transduction system and the aging process. Am J Physiol-Cell Physiol 292(2):C670–C686. https://doi.org/10.1152/ajpcell.00213.2006
Nelson G, Kucheryavenko O, Wordsworth J, von Zglinicki T (2018) The senescent bystander effect is caused by ROS-activated NF-κB signalling. Mech Ageing Dev 170:30–36. https://doi.org/10.1016/j.mad.2017.08.005
Neri M, Riezzo I, Pascale N, Pomara C, Turillazzi E (2017) Ischemia/reperfusion injury following acute myocardial infarction: a critical issue for clinicians and forensic pathologists. Mediators Inflamm 2017:7018393. https://doi.org/10.1155/2017/7018393
Norman HS, Oujiri J, Larue SJ, Chapman CB, Margulies KB, Sweitzer NK (2011) Decreased cardiac functional reserve in heart failure with preserved systolic function. J Card Fail 17(4):301–308. https://doi.org/10.1016/j.cardfail.2010.11.004
North BJ, Sinclair DA (2012) The intersection between aging and cardiovascular disease. Circ Res 110(8):1097–1108. https://doi.org/10.1161/circresaha.111.246876
Nowak WN, Deng J, Ruan XZ, Xu Q (2017) Reactive oxygen species generation and atherosclerosis. Arterioscler Thromb Vasc Biol 37(5):e41–e52. https://doi.org/10.1161/ATVBAHA.117.309228
Oka SI, Sabry AD, Cawley KM, Warren JS (2020) Multiple levels of PGC-1α dysregulation in heart failure. Front Cardiovasc Med 7:2. https://doi.org/10.3389/fcvm.2020.00002
Olivieri F, Recchioni R, Marcheselli F, Abbatecola AM, Santini G, Borghetti G, Antonicelli R, Procopio AD (2013) Cellular senescence in cardiovascular diseases: potential age-related mechanisms and implications for treatment. Curr Pharm Des 19(9):1710–1719
Pankiv S, Clausen TH, Lamark T, Brech A, Bruun JA, Outzen H, Overvatn A, Bjorkoy G, Johansen T (2007) p62/SQSTM1 binds directly to Atg8/LC3 to facilitate degradation of ubiquitinated protein aggregates by autophagy. J Biol Chem 282(33):24131–24145. https://doi.org/10.1074/jbc.M702824200
Passos J, Saretzki G, Ahmed S, Nelson G, Richter T, Peters H, Wappler I, Birket M, Harold G, Schaeuble K, Birch-Machin M, Kirkwood T, von Zglinicki T (2007) Mitochondrial dysfunction accounts for the stochastic heterogeneity in telomere-dependent senescence. PLoS Biol 5(5). https://doi.org/10.1371/journal.pbio.0050110
Penna C, Mancardi D, Rastaldo R, Pagliaro P (2009) Cardioprotection: a radical view: free radicals in pre and postconditioning. Biochim Biophys Acta (BBA) - Bioenergetics 1787(7):781–793. https://doi.org/10.1016/j.bbabio.2009.02.008
Perkins DW, Haider S, Robertson D, Buus R, O’Leary L, Isacke CM (2020) Therapy-induced senescence in normal tissue promotes breast cancer metastasis. bioRxiv:2020.2010.2017.343590. https://doi.org/10.1101/2020.10.17.343590
Poznyak AV, Ivanova EA, Sobenin IA, Yet SF, Orekhov AN (2020) The role of mitochondria in cardiovascular diseases. Biology (Basel) 9(6). https://doi.org/10.3390/biology9060137
Prakash A, Gordon LB, Kleinman ME, Gurary EB, Massaro J, D’Agostino R Sr, Kieran MW, Gerhard-Herman M, Smoot L (2018) Cardiac abnormalities in patients with Hutchinson-Gilford Progeria Syndrome. JAMA Cardiol 3(4):326–334. https://doi.org/10.1001/jamacardio.2017.5235
Predmore JM, Wang P, Davis F, Bartolone S, Westfall MV, Dyke DB, Pagani F, Powell SR, Day SM (2010) Ubiquitin proteasome dysfunction in human hypertrophic and dilated cardiomyopathies. Circulation 121(8):997–1004. https://doi.org/10.1161/CIRCULATIONAHA.109.904557
Razani B, Feng C, Coleman T, Emanuel R, Wen H, Hwang S, Ting JP, Virgin HW, Kastan MB, Semenkovich CF (2012) Autophagy links inflammasomes to atherosclerotic progression. Cell Metab 15(4):534–544. https://doi.org/10.1016/j.cmet.2012.02.011
Rebbaa A, Zheng X, Chou PM, Mirkin BL (2003) Caspase inhibition switches doxorubicin-induced apoptosis to senescence. Oncogene 22(18):2805–2811. https://doi.org/10.1038/sj.onc.1206366
Richardson GD, Breault D, Horrocks G, Cormack S, Hole N, Owens WA (2012) Telomerase expression in the mammalian heart. FASEB J 26(12):4832–4840. https://doi.org/10.1096/fj.12-208843
Richardson GD, Sage A, Bennaceur K, Al Zhrany N, Coelho-Lima J, Dookun E, Draganova L, Saretzki G, Breault DT, Mallat Z, Spyridopoulos I (2018) Telomerase mediates lymphocyte proliferation but not the atherosclerosis-suppressive potential of regulatory T-cells. Arterioscler Thromb Vasc Biol 38(6):1283–1296. https://doi.org/10.1161/ATVBAHA.117.309940
Richter C, Park JW, Ames BN (1988) Normal oxidative damage to mitochondrial and nuclear DNA is extensive. Proc Natl Acad Sci 85(17):6465–6467. https://doi.org/10.1073/pnas.85.17.6465
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ (2017) Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 377(12):1119–1131. https://doi.org/10.1056/NEJMoa1707914
Ridker PM, MacFadyen JG, Everett BM, Libby P, Thuren T, Glynn RJ, Ridker PM, MacFadyen JG, Everett BM, Libby P et al (2018) Relationship of C-reactive protein reduction to cardiovascular event reduction following treatment with canakinumab: a secondary analysis from the CANTOS randomised controlled trial. Lancet 391(10118):319–328. https://doi.org/10.1016/S0140-6736(17)32814-3
Ron-Harel N, Notarangelo G, Ghergurovich JM, Paulo JA, Sage PT, Santos D, Satterstrom FK, Gygi SP, Rabinowitz JD, Sharpe AH, Haigis MC (2018) Defective respiration and one-carbon metabolism contribute to impaired naïve T cell activation in aged mice. Proc Natl Acad Sci U S A 115(52):13347–13352. https://doi.org/10.1073/pnas.1804149115
Roos CM, Zhang B, Palmer AK, Ogrodnik MB, Pirtskhalava T, Thalji NM, Hagler M, Jurk D, Smith LA, Casaclang-Verzosa G, Zhu Y, Schafer MJ, Tchkonia T, Kirkland JL, Miller JD (2016) Chronic senolytic treatment alleviates established vasomotor dysfunction in aged or atherosclerotic mice. Aging Cell 15(5):973–977. https://doi.org/10.1111/acel.12458
Saito T, Asai K, Sato S, Hayashi M, Adachi A, Sasaki Y, Takano H, Mizuno K, Shimizu W (2016) Autophagic vacuoles in cardiomyocytes of dilated cardiomyopathy with initially decompensated heart failure predict improved prognosis. Autophagy 12(3):579–587. https://doi.org/10.1080/15548627.2016.1145326
Saleh T, Bloukh S, Carpenter VJ, Alwohoush E, Bakeer J, Darwish S, Azab B, Gewirtz DA (2020) Therapy-induced senescence: an “old” friend becomes the enemy. Cancers (Basel) 12(4). https://doi.org/10.3390/cancers12040822
Samani NJ, Boultby R, Butler R, Thompson JR, Goodall AH (2001) Telomere shortening in atherosclerosis. Lancet 358(9280):472–473. https://doi.org/10.1016/s0140-6736(01)05633-1
Schank M, Zhao J, Wang L, Li Z, Cao D, Nguyen LN, Dang X, Khanal S, Nguyen LNT, Thakuri BKC, Ogbu SC, Lu Z, Zhang J, Wu XY, Morrison ZD, El Gazzar M, Ning S, Moorman JP, Yao ZQ (2020) Telomeric injury by KML001 in human T cells induces mitochondrial dysfunction through the p53-PGC-1α pathway. Cell Death Dis 11(12):1030. https://doi.org/10.1038/s41419-020-03238-7
Sergin I, Bhattacharya S, Emanuel R, Esen E, Stokes CJ, Evans TD, Arif B, Curci JA, Razani B (2016) Inclusion bodies enriched for p62 and polyubiquitinated proteins in macrophages protect against atherosclerosis. Sci Signal 9(409):ra2. https://doi.org/10.1126/scisignal.aad5614
Sharpless NE, Sherr CJ (2015) Forging a signature of in vivo senescence. Nat Rev Cancer 15(7):397–408. https://doi.org/10.1038/nrc3960
Shay JW, Wright WE (2004) Senescence and immortalization: role of telomeres and telomerase. Carcinogenesis 26(5):867–874. https://doi.org/10.1093/carcin/bgh296
Shimizu I, Minamino T (2019) Cellular senescence in cardiac diseases. J Cardiol 74(4):313–319. https://doi.org/10.1016/j.jjcc.2019.05.002
Siddall HK, Yellon DM, Ong SB, Mukherjee UA, Burke N, Hall AR, Angelova PR, Ludtmann MH, Deas E, Davidson SM, Mocanu MM, Hausenloy DJ (2013) Loss of PINK1 increases the heart’s vulnerability to ischemia-reperfusion injury. PLoS One 8(4):e62400. https://doi.org/10.1371/journal.pone.0062400
Siddiqi N, Neil C, Bruce M, MacLennan G, Cotton S, Papadopoulou S, Feelisch M, Bunce N, Lim PO, Hildick-Smith D, Horowitz J, Madhani M, Boon N, Dawson D, Kaski JC, Frenneaux M, investigators N (2014) Intravenous sodium nitrite in acute ST-elevation myocardial infarction: a randomized controlled trial (NIAMI). Eur Heart J 35(19):1255–1262. https://doi.org/10.1093/eurheartj/ehu096
Song H, Conte JV, Foster AH, McLaughlin JS, Wei C (1999) Increased p53 protein expression in human failing myocardium. J Heart Lung Transplant 18(8):744–749. https://doi.org/10.1016/S1053-2498(98)00039-4
Spray L, Park C, Cormack S, Mohammed A, Panahi P, Boag S, Bennaceur K, Sopova K, Richardson G, Stangl VM, Rech L, Rainer PP, Ramos GC, Hofmann U, Stellos K, Spyridopoulos I (2021) The Fractalkine Receptor CX(3)CR1 links lymphocyte kinetics in CMV-seropositive patients and acute myocardial infarction with adverse left ventricular remodeling. Front Immunol 12:605857–605857. https://doi.org/10.3389/fimmu.2021.605857
Spyridopoulos I, Hoffmann J, Aicher A, Brümmendorf TH, Doerr HW, Zeiher AM, Dimmeler S (2009) Accelerated telomere shortening in leukocyte subpopulations of patients with coronary heart disease: role of cytomegalovirus seropositivity. Circulation 120(14):1364–1372. https://doi.org/10.1161/circulationaha.109.854299
Spyridopoulos I, Martin-Ruiz C, Hilkens C, Yadegarfar ME, Isaacs J, Jagger C, Kirkwood T, von Zglinicki T (2016) CMV seropositivity and T-cell senescence predict increased cardiovascular mortality in octogenarians: results from the Newcastle 85+ study. Aging Cell 15(2):389–392. https://doi.org/10.1111/acel.12430
Stojanović SD, Fiedler J, Bauersachs J, Thum T, Sedding DG (2020) Senescence-induced inflammation: an important player and key therapeutic target in atherosclerosis. Eur Heart J 41(31):2983–2996. https://doi.org/10.1093/eurheartj/ehz919
Strindhall J, Nilsson BO, Löfgren S, Ernerudh J, Pawelec G, Johansson B, Wikby A (2007) No Immune Risk Profile among individuals who reach 100 years of age: findings from the Swedish NONA immune longitudinal study. Exp Gerontol 42(8):753–761. https://doi.org/10.1016/j.exger.2007.05.001
Sun Y, Yao X, Zhang QJ, Zhu M, Liu ZP, Ci B, Xie Y, Carlson D, Rothermel BA, Sun Y, Levine B, Hill JA, Wolf SE, Minei JP, Zang QS (2018) Beclin-1-dependent autophagy protects the heart during sepsis. Circulation 138(20):2247–2262. https://doi.org/10.1161/CIRCULATIONAHA.117.032821
Sun LY, Eddeen AB, Mesana TG (2021) Disability-free survival after major cardiac surgery: a population-based retrospective cohort study. CMAJ Open 9(2):E384–E393. https://doi.org/10.9778/cmajo.20200096
Sutton MGSJ, Sharpe N (2000) Left ventricular remodeling after myocardial infarction. Circulation 101(25):2981–2988. https://doi.org/10.1161/01.CIR.101.25.2981
Swaminathan B, Goikuria H, Vega R, Rodriguez-Antiguedad A, Lopez Medina A, Freijo Mdel M, Vandenbroeck K, Alloza I (2014) Autophagic marker MAP1LC3B expression levels are associated with carotid atherosclerosis symptomatology. PLoS One 9(12):e115176. https://doi.org/10.1371/journal.pone.0115176
Taneike M, Yamaguchi O, Nakai A, Hikoso S, Takeda T, Mizote I, Oka T, Tamai T, Oyabu J, Murakawa T, Nishida K, Shimizu T, Hori M, Komuro I, Takuji Shirasawa TS, Mizushima N, Otsu K (2010) Inhibition of autophagy in the heart induces age-related cardiomyopathy. Autophagy 6(5):600–606. https://doi.org/10.4161/auto.6.5.11947
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD (2012) Third universal definition of myocardial infarction. J Am Coll Cardiol 60(16):1581–1598. https://doi.org/10.1016/j.jacc.2012.08.001
Tomás-Loba A, Flores I, Fernández-Marcos PJ, Cayuela ML, Maraver A, Tejera A, Borrás C, Matheu A, Klatt P, Flores JM, Viña J, Serrano M, Blasco MA (2008) Telomerase reverse transcriptase delays aging in cancer-resistant mice. Cell 135(4):609–622. https://doi.org/10.1016/j.cell.2008.09.034
Torabi A, Cleland JG, Rigby AS, Sherwi N (2014) Development and course of heart failure after a myocardial infarction in younger and older people. J Geriatr Cardiol 11(1):1–12. https://doi.org/10.3969/j.issn.1671-5411.2014.01.002
Triposkiadis F, Xanthopoulos A, Butler J (2019) Cardiovascular aging and heart failure: JACC review topic of the week. J Am Coll Cardiol 74(6):804–813. https://doi.org/10.1016/j.jacc.2019.06.053
Ungvari Z, Orosz Z, Labinskyy N, Rivera A, Xiangmin Z, Smith K, Csiszar A (2007) Increased mitochondrial H2O2 production promotes endothelial NF-κB activation in aged rat arteries. Am J Physiol-Heart C 293(1):H37–H47. https://doi.org/10.1152/ajpheart.01346.2006
Villeneuve C, Guilbeau-Frugier C, Sicard P, Lairez O, Ordener C, Duparc T, De Paulis D, Couderc B, Spreux-Varoquaux O, Tortosa F, Garnier A, Knauf C, Valet P, Borchi E, Nediani C, Gharib A, Ovize M, Delisle MB, Parini A, Mialet-Perez J (2013) p53-PGC-1α pathway mediates oxidative mitochondrial damage and cardiomyocyte necrosis induced by monoamine oxidase-A upregulation: role in chronic left ventricular dysfunction in mice. Antioxid Redox Signal 18(1):5–18. https://doi.org/10.1089/ars.2011.4373
Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN et al (2021) Heart Disease and Stroke Statistics-2021 Update. Circulation 143(8):e254–e743. https://doi.org/10.1161/CIR.0000000000000950
Vizioli MG, Liu T, Miller KN, Robertson NA, Gilroy K, Lagnado AB, Perez-Garcia A, Kiourtis C, Dasgupta N, Lei X, Kruger PJ, Nixon C, Clark W, Jurk D, Bird TG, Passos JF, Berger SL, Dou Z, Adams PD (2020) Mitochondria-to-nucleus retrograde signaling drives formation of cytoplasmic chromatin and inflammation in senescence. Genes Dev 34(5-6):428–445. https://doi.org/10.1101/gad.331272.119
von Zglinicki T, Pilger R, Sitte N (2000) Accumulation of single-strand breaks is the major cause of telomere shortening in human fibroblasts. Free Radic Biol Med 28(1):64–74. https://doi.org/10.1016/s0891-5849(99)00207-5
Vulliamy T, Marrone A, Goldman F, Dearlove A, Bessler M, Mason PJ, Dokal I (2001) The RNA component of telomerase is mutated in autosomal dominant dyskeratosis congenita. Nature 413(6854):432–435. https://doi.org/10.1038/35096585
Walaszczyk A, Dookun E, Redgrave R, Tual-Chalot S, Victorelli S, Spyridopoulos I, Owens A, Arthur HM, Passos JF, Richardson GD (2019) Pharmacological clearance of senescent cells improves survival and recovery in aged mice following acute myocardial infarction. Aging Cell:e12945. https://doi.org/10.1111/acel.12945
Wang E (1995) Senescent human fibroblasts resist programmed cell death, and failure to suppress bcl2 is involved. Cancer Res 55(11):2284–2292
Wang JC, Bennett M (2012) Aging and atherosclerosis. Circ Res 111(2):245–259. https://doi.org/10.1161/CIRCRESAHA.111.261388
Wang K, Zhou LY, Wang JX, Wang Y, Sun T, Zhao B, Yang YJ, An T, Long B, Li N, Liu CY, Gong Y, Gao JN, Dong YH, Zhang J, Li PF (2015) E2F1-dependent miR-421 regulates mitochondrial fragmentation and myocardial infarction by targeting Pink1. Nat Commun 6:7619. https://doi.org/10.1038/ncomms8619
Wang B, Kohli J, Demaria M (2020) Senescent cells in cancer therapy: friends or foes? Trends Cancer 6(10):838–857. https://doi.org/10.1016/j.trecan.2020.05.004
Weng NP, Levine BL, June CH, Hodes RJ (1996) Regulated expression of telomerase activity in human T lymphocyte development and activation. J Exp Med 183(6):2471–2479. https://doi.org/10.1084/jem.183.6.2471
Werner C, Hanhoun M, Widmann T, Kazakov A, Semenov A, Pöss J, Bauersachs J, Thum T, Pfreundschuh M, Müller P, Haendeler J, Böhm M, Laufs U (2008) Effects of physical exercise on myocardial telomere-regulating proteins, survival pathways, and apoptosis. J Am Coll Cardiol 52(6):470–482. https://doi.org/10.1016/j.jacc.2008.04.034
Widgerow AD (2014) Ischemia-reperfusion injury: influencing the microcirculatory and cellular environment. Ann Plast Surg 72(2):253–260. https://doi.org/10.1097/SAP.0b013e31825c089c
Wiley CD, Campisi J (2021) The metabolic roots of senescence: mechanisms and opportunities for intervention. Nat Metab 3(10):1290–1301. https://doi.org/10.1038/s42255-021-00483-8
Wyld L, Bellantuono I, Tchkonia T, Morgan J, Turner O, Foss F, George J, Danson S, Kirkland JL (2020) Senescence and cancer: a review of clinical implications of senescence and senotherapies. Cancers (Basel) 12(8). https://doi.org/10.3390/cancers12082134
Xie Y, Xu E, Bowe B, Al-Aly Z (2022) Long-term cardiovascular outcomes of COVID-19. Nat Med 28(3):583–590. https://doi.org/10.1038/s41591-022-01689-3
Xiong S, Patrushev N, Forouzandeh F, Hilenski L, Alexander RW (2015) PGC-1α modulates telomere function and DNA damage in protecting against aging-related chronic diseases. Cell Rep 12(9):1391–1399. https://doi.org/10.1016/j.celrep.2015.07.047
Xu C, Cao Y, Liu R, Liu L, Zhang W, Fang X, Jia S, Ye J, Liu Y, Weng L, Qiao X, Li B, Zheng M (2022) Mitophagy-regulated mitochondrial health strongly protects the heart against cardiac dysfunction after acute myocardial infarction. J Cell Mol Med 26(4):1315–1326. https://doi.org/10.1111/jcmm.17190
Zhang Y-W, Shi J, Li Y-J, Wei L (2009) Cardiomyocyte death in doxorubicin-induced cardiotoxicity. Archivum Immunologiae et Therapiae Experimentalis 57(6):435–445. https://doi.org/10.1007/s00005-009-0051-8
Zhang W, Siraj S, Zhang R, Chen Q (2017) Mitophagy receptor FUNDC1 regulates mitochondrial homeostasis and protects the heart from I/R injury. Autophagy 13(6):1080–1081. https://doi.org/10.1080/15548627.2017.1300224
Zhang W, Chen C, Wang J, Liu L, He Y, Chen Q (2018) Mitophagy in cardiomyocytes and in platelets: a major mechanism of cardioprotection against ischemia/reperfusion injury. Physiology (Bethesda) 33(2):86–98. https://doi.org/10.1152/physiol.00030.2017
Zhou J, Chong SY, Lim A, Singh BK, Sinha RA, Salmon AB, Yen PM (2017) Changes in macroautophagy, chaperone-mediated autophagy, and mitochondrial metabolism in murine skeletal and cardiac muscle during aging. Aging (Albany NY) 9(2):583–599. https://doi.org/10.18632/aging.101181
Zhu F, Li Y, Zhang J, Piao C, Liu T, Li HH, Du J (2013) Senescent cardiac fibroblast is critical for cardiac fibrosis after myocardial infarction. PLoS One 8(9):e74535. https://doi.org/10.1371/journal.pone.0074535
Zhu Y, Tchkonia T, Pirtskhalava T, Gower AC, Ding H, Giorgadze N, Palmer AK, Ikeno Y, Hubbard GB, Lenburg M, O’Hara SP, LaRusso NF, Miller JD, Roos CM, Verzosa GC, LeBrasseur NK, Wren JD, Farr JN, Khosla S, Stout MB, McGowan SJ, Fuhrmann-Stroissnigg H, Gurkar AU, Zhao J, Colangelo D, Dorronsoro A, Ling YY, Barghouthy AS, Navarro DC, Sano T, Robbins PD, Niedernhofer LJ, Kirkland JL (2015) The Achilles’ heel of senescent cells: from transcriptome to senolytic drugs. Aging Cell 14(4):644–658. https://doi.org/10.1111/acel.12344
Zidar DA, Al-Kindi SG, Liu Y, Krieger NI, Perzynski AT, Osnard M, Nmai C, Anthony DD, Lederman MM, Freeman ML, Bonomo RA, Simon DI, Dalton JE (2019) Association of lymphopenia with risk of mortality among adults in the US general population. JAMA Network Open 2(12):e1916526–e1916526. https://doi.org/10.1001/jamanetworkopen.2019.16526
Acknowledgements
The authors acknowledge the contribution of past and present members of the laboratory of G.R who have contributed to the data discussed in this review. We acknowledge the funding support of the British Heart Foundation PG/22/10788 and PG/21/10761. Figures were created with BioRender.com.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Booth, L.K., Redgrave, R.E., Tual-Chalot, S., Spyridopoulos, I., Phillips, H.M., Richardson, G.D. (2023). Heart Disease and Ageing: The Roles of Senescence, Mitochondria, and Telomerase in Cardiovascular Disease. In: Harris, J.R., Korolchuk, V.I. (eds) Biochemistry and Cell Biology of Ageing: Part IV, Clinical Science. Subcellular Biochemistry, vol 103. Springer, Cham. https://doi.org/10.1007/978-3-031-26576-1_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-26576-1_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-26575-4
Online ISBN: 978-3-031-26576-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)