Abstract
The global burden of parasitic diseases combined is unknown, but hundreds of millions of the people are infected each year, with the greatest charge borne by developing countries in tropical and subtropical regions of the world. Despite the enormous toll on human health, development of new therapeutic drugs for parasitic diseases has largely been neglected. Between 1975 and 1999, only 13 of 1300 (0.01%) new pharmaceutical drugs were introduced for parasitic infections. However, this has improved since 2000 as 20 new agents were developed or in development for parasitic diseases. Since 2015, two old and three new anti-parasitic agents were approved in the United States, and this chapter reviews their chemistry, pharmacology, indication, efficacy, and safety. These drugs include tafenoquine for malaria, benznidazole (old agent) for Chagas disease, fexinidazole for African trypanosomiasis, moxidectin for onchocerciasis, and triclabendazole (old drug) for fascioliasis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Plasmodium vivax
- P. ovale
- Moxidectin
- Tafenoquine
- Benznidazole
- Fexinidazole
- Chagas disease
- Fascioliasis
- Onchocerciasis
- African trypanosomiasis
- Triclabendazole
1 Introduction
Parasitic diseases afflict hundreds of millions of people globally each year but the actual burden on global health has been difficult to estimate. The greatest charge from parasitic diseases is borne by populations in developing countries located in tropical and subtropical regions of the world. Despite their enormous toll on human health, development of new therapeutic drugs for these diseases has long been neglected. Between 1975 and 1999, only 13 of 1300 (0.01%) new therapeutic drugs introduced were slated for parasitic diseases [1]. However, since 2000 there has been 20 new anti-parasitic drugs introduced or in development, which is a great stride forward. This chapter reviews two old and three new anti-parasitic drugs approved by the Federal Food and Drug Administration (FDA) in the United States (US) since 2015: (i) benznidazole (old drug) for Chagas disease; (ii) fexinidazole for African trypanosomiasis; (iii) moxidectin for onchocerciasis; (iv) tafenoquine for malaria; and (v) triclabendazole (old drug) for fascioliasis.
2 Benznidazole
2.1 Chagas Disease
Chagas disease, also known as American trypanosomiasis, caused by the protozoa, Trypanosoma cruzi, is a vector-borne zoonosis transmitted by the Triatominae insect (“kissing bug”), but occasionally transmitted by blood transfusion, orally (food-borne), vertically (mother-to-child), and organ transplantation. Worldwide, mostly in Latin America, it is estimated that six to seven million people are infected with the parasite [2]. Chagas disease used to be limited to the rural areas of Latin America, but with increased migration in the last decade most infected people live in urban settings and the disease is now present in North America and Europe. In 2016 it was estimated that there were 238,000 cases of Chagas disease in the US [3], and studies in Europe showed an overall 4.2% prevalence, with the highest infection rates in people from Bolivia (18.1%) [4].
Infection with T. cruzi from the vector typically occurs in early childhood and the acute phase is usually asymptomatic but fever and malaise occur in about 5%, followed by a prolonged asymptomatic indeterminate phase (>50% remain in this phase for life with no sequelae); after a decade or more 35% to 50% enter a chronic phase with chronic heart disease (up to 30%) and intestinal disease (10% with megacolon and megaesophagus) [2, 5]. Congenital infection and reactivation in immunosuppressed patients, including those with AIDS, can occasionally lead to myocarditis and meningoencephalitis or focal brain lesions, and AIDS patients can also present with subcutaneous nodules [6]. The infection is estimated to cause 10,000 deaths every year [5].
2.2 Treatment of Chagas Disease
No new therapy has been introduced for Chagas disease since the 1970s, but benznidazole which has been used in Latin America for decades was only approved by the FDA in 2017. This is due to the increasing number of migrants from Central and South America now recognized to have Chagas disease in the US. The two available drugs for Chagas disease belong to the nitroimidazole class: nifurtimox was released in 1967, followed by benznidazole in 1972 [7]. Both drugs were very effective in the acute phase of Chagas disease and were generally not used in the chronic phase, as the persistence of the protozoa was not believed responsible for chronic disease but considered related to the immune response of the host. Benznidazole (BZN) is better tolerated than nifurtimox and is considered the first drug of choice by many experts [7].
BZN is a prodrug that is enzymatically activated by the trypanosomal type I nitroreductases to produce reactive metabolites which are toxic to cells and DNA, causing rapid trypanosomal effect of intracellular and extracellular parasite [8]. It is active against both the trypomastigote and amastigote forms [6]. The tablet is well absorbed (92% bioavailability) and not affected by food but the peak serum concentration occurs at 2 h in the fasting state and 3.2 h after meals, with maximum serum concentration (Cmax) of 2.4 μg/ml and half-life of 12 h (Exeltis drug manual). The volume of distribution was higher in men than women (125.9 versus 88.6 liters), which may account for lower Cmax (1.6 vs 2.9 μg/ml) [9]. BZN is excreted primarily by the kidneys and 22% by the fecal route [6]. The dose is 5–8 mg/kg/day in two divided doses for 60 days, and it is available as 12.5 mg and 100 mg tablets. It should not be given to pregnant women (in animals causes fetal toxicity) and should not be used in renal or hepatic failure [2].
2.3 Efficacy of Benznidazole
BZN is most effective in acute or early congenital infection to shorten clinical course and clear parasitemia, with parasitological cure of 60–85% in the acute phase and 90% of congenital infection in the first year [6]. For children <30 kg body weight, the 12.5 mg tablet can be made into a slurry with water.
The use of BZN in the chronic phase of Chagas disease has been controversial, but currently there is consensus that the persistence of the parasite is responsible for inducing persistent inflammation that leads to chronic disease progression. Hence, eradication of the trypanosome may be necessary to prevent progression from the intermediate phase to Chagas heart disease (cardiomyopathy). This is supported by the presence of the trypanosome antigen and the severity of myocardial inflammation in Chagas disease [9]. Previous randomized trials in children aged 6–12 years with asymptomatic chronic T. cruzi infection demonstrated that treatment resulted in seroconversion from positive to negative serology in 60% [6]. Thus, early diagnosis and BZN treatment was recommended for all children.
But does treatment of chronic Chagas disease produce any clinical benefit? In a multicenter, randomized study, 2854 patients with Chagas cardiomyopathy received BZN (n = 1431) or placebo (n = 1432) for 80 days [10]. Of 1896 patients with blood tested for T. cruzi by PCR, 60.5% were positive and rates of conversion to negative PCR were greater in the treated group at the end of treatment, 2 and 5 years post-treatment (p < 0.001), but the gap narrowed at 5 years to 46.7% versus 33.1% for BZN and placebo, respectively. However, there was no difference in the rate of clinical deterioration between the two groups.
What is the benefit of treatment in the indeterminate phase of Chagas disease without cardiac disease? There is no randomized study to prove the benefit of BZN in the indeterminate stage of Chagas disease, but several observation studies suggest that treatment may slow the progression to Chagas heart disease. In a retrospective observational cohort of 228 patients, 114 patients treated with BZN for 30–60 days were compared to matched non-treated patients with a median follow-up of 15.1 years [11]. The rate of progression was less with treatment, 21.1% of untreated patients progressed to cardiac form of Chagas compared to 7.9% of treated patients, p = 0.04.
The indications for treatment with BZN include all acute and congenital infections, reactivated infections (immunosuppressed), for children 18 years or younger with chronic infection, and women of child-bearing age (before or after pregnancy) to prevent congenital infection [2, 6]. Adults under 60 years of age in the chronic stage without advanced cardiac disease should also be offered treatment.
2.4 Adverse Effects of Benznidazole
BZN is genotoxic and can cause risk to a fetus and is contraindicated in pregnancy and during lactation. The most common side effects are gastrointestinal (GI) in nature, abdominal pain (up to 25%), nausea and vomiting (5%), decreased appetite, rashes (11–16%), occasionally dizziness, peripheral neuropathy, tremors, leucopenia, or neutropenia (see drug manual). However, most patients treated with nifurtimox experience side effects, 68.7% GI adverse events and 60.5% neurologic events (MMWR, March 11, 2022).
3 Fexinidazole
3.1 African Trypanosomiasis
There are two forms of human African trypanosomiasis, depending on the subspecies of the parasite: (i) Trypanosoma brucei gambiense which causes 95% of cases of sleeping sickness and is found in 24 countries of west and central Africa. Infected patients can remain subclinical for months to years, and central nervous system (CNS) signs represent advanced disease. (ii) Trypanosoma brucei rhodesiense accounts for 5% of reported cases and is found in 13 countries in eastern and southern Africa [12]. Acute infection results in signs and symptoms in weeks to a few months with rapid involvement of the CNS.
With sustained control measures for many years, the number of cases fell below 10,000 for the first time in 2009, and only 992 new cases were recorded in 2019 [12]. Thus, eradication of the disease is in sight. Infection is transmitted by the bite of the tsetse fly with trypanosome from infected humans or animals. Infection that can be transmitted rarely by other means, vertically from mother to fetus, from contact with contaminated needles, and transmission by sexual contact has been reported [12].
Clinically the disease is divided into two stages: the first stage or hemolymphatic stage, the parasite multiply in the subcutaneous tissues, blood, and lymph, and patients present with fever, headaches, lymphadenopathy, joint pains, and pruritus; the second stage the trypanosome enters the CNS to cause the meningo-encephalic stage. The second stage is characterized by disturbance of sleep cycle, confusion, changes in behavior, sensory disturbance, and poor coordination.
3.2 Treatment of African Trypanosomiasis
There are six drugs used in the treatment of African trypanosomiasis, and this depends on the stage of disease. Drugs used in the first stage: (i) pentamidine in the first stage of T. b. gambiense infection; (ii) and suramin used for the first stage of T. b. rhodesiense infection.
Drugs used in the second stage are the following: (iii) melarsoprol (arsenic compound) used as first-line treatment of rhodesiense form and rarely used in the gambiense form; (iv) eflornithine is only effective against T. b. gambiense; (v) nifurtimox is used in combination with eflornithine for the gambiense form. Then drugs used in both stages—(vi) fexinidazole.
Fexinidazole (FNZ) is indicated as first-line treatment of the first stage of gambiense form and non-severe second stage [12], and it was approved by the US FDA in 2021. FNZ is a 2-substituted 5-nitroimidazole discovered in the late 1970s but rediscovered >30 years later by the Drugs for Neglected Diseases initiative. FNZ and its two active metabolites (a sulfoxide and a sulfone) are active against the 2 human African trypanosoma species in vitro with the inhibitory concentration of 50% (IC50) of clinical isolates ranging between 0.16 and 0.93 μg/ml [13]. The mechanism of action is unclear but it is believed that reduction of FNZ and its two active metabolites by trypanosome nitroreductase produce reactive intermediates that damage the protozoa DNA and proteins [14].
3.3 Pharmacology of Fexinidazole
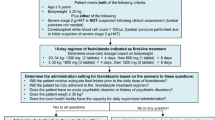
FNZ is rapidly absorbed after oral dosing and rapidly metabolized by the cytochrome P450 enzymes to its active metabolites with maximum concentration at 2–5 h, and food increases the bioavailability greatly (Winthrop drug manual). The half-life of FNZ is about 11–14 h and the active metabolites 15 to 23 h, the protein binding is 95.4%, and the cerebrospinal fluid (CSF) concentration of the active metabolites in adults is about 31% to 52% of plasma concentration. Only <3.15% of the dose is excreted in the urine and most is excreted by the biliary route. The usual adult dose is 1800 mg (3 tablets) once daily with food for 4 days, then 1200 mg daily for 6 days; in children ≥20 and < 35 kg, the dose is 1200 mg daily for 4 days and then 600 mg daily for 6 days. No dose adjustment is needed for renal impairment, and no data is available for hepatic impairment, but it is contraindicated in patients with signs of cirrhosis or jaundice.
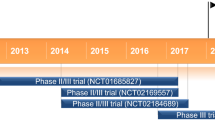
3.4 Clinical Efficacy of Fexinidazole
FNZ is the first exclusively oral treatment for human African trypanosomiasis (HAT). In a randomized, phase 2/3, noninferiority, open-label trial, 394 patients with late-stage HAT were randomized to oral FNZ (n = 264) or nifurtimox/eflornithine (NECT) combination (n = 130) [15]. FNZ was given once daily, 1800 mg for 4 days, and then 1200 mg for 6 days. Oral nifurtimox (10 mg/kg/day) was given three times a day for 10 days with eflornithine (400 mg/kg/day) infusions twice daily for 7 days. Success was assessed at 18 months, patient being alive, having no evidence of trypanosomes in any fluid, not requiring rescue medication, and CSF leukocyte count ≤20 cells per μl. The success rate of FNZ was lower than the combination (91% vs 98%), but the difference was within the predetermined acceptability margin of 13% [16]. In the subgroup of patients with severe CNS disease, >100 leucocytes in the CSF, FNZ showed less favorable outcome compared to NECT (86.9% vs 98.7%), but in the less severe cases (CSF leucocytes <100) treatment success was 98.7% for FNZ and 95.9% for NECT. The rates of death and treatment-related serious adverse event were similar, but some adverse events such as headaches, insomnia, and anxiety were more frequent with FNZ. This is the first oral monotherapy shown to be effective for the second stage HAT. This allowed home-based treatment and is more cost-effective to the healthcare system. It is the first oral treatment for all stages of T. b. gambiense HAT.
In an open-label, prospective, multicenter, cohort study, 227 patients with stage 1 gambiense HAT and 41 with early stage 2 (absence in CSF) were treated with FNZ [17]. Treatment was effective at 12 months in 227 of 230 patients (99%). No new safety issues were recognized in this study, and the commonest adverse events were headache and vomiting, and serious emergent adverse events were reported in 22 (9%).
3.5 Side Effects of Fexinidazole
Although FNZ appeared to be mutagenic in the AMES test, no genotoxic potential was found from a series of in vitro, in vivo, or ex vivo tests in mammalian cells (Drug manual). There is no data on use in pregnant or lactating women and effects on embryo-fetal development in animals were secondary to maternal toxicity.
The most frequently reported adverse events from pooled data were vomiting (38%), nausea (33%), asthenia (20%), decreased appetite (17%), headache (16%), insomnia (15%), tremor (14%), and dizziness (14%) (see Drug manual). Psychiatric-related events (>1%) include hallucination and psychotic disorder. QTc prolongation of >450 ms have been seen in 7.2% of patients, but tachycardia is very uncommon.
4 Moxidectin
4.1 Onchocerciasis
Onchocerciasis, also known as river blindness, is the second commonest cause of blindness due to an infection after trachoma. It is due to the filarial nematode, Onchocerca volvulus, transmitted by the bite of the female black fly (genus Simulium damnosum) that breeds along fast flowing rivers of parts of Africa and South America. River blindness is endemic in 31 countries of sub-Saharan Africa, the Arabian Peninsula, and the Amazonian focus straddling Venezuela and Brazil [18]. The WHO estimates that there are 25 million people with the disease and 90% are in sub-Saharan Africa.
Black flies inoculate patients with the infective microfilariae larvae during a blood meal and the microfilariae would develop into adult worms in 6–12 months that reside subcutaneously in fibrous nodules, commonly located around the head, torso, and the iliac crest. The fertilized adult worms produce 1000 to 1500 microfilariae daily and live for 10–15 years [18]. Dermatological manifestations are the commonest presentation, preceding ocular disease by years. These include severe pruritus, papular dermatitis, licheniform dermatitis, and areas of depigmentation, commonly around the shins—called “leopard skin.” Ocular involvement is a result of inflammatory response to dead or dying microfilariae seeded to the eye. Vision loss can result from sclerosing keratitis, uveitis, optic nerve and chorioretinal atrophies, secondary cataract, and rarely glaucoma.
4.2 Treatment of Onchocerciasis
Diagnosis of onchocerciasis is usually made by examination of skin snips and slit-lamp examination of the eye and serological tests, enzyme-linked immunosorbent (ELISA), and Western blot. Diethylcarbamazine was first used for the disease, which was effective but caused serious ocular and systemic complications and is no longer recommended. Ivermectin was considered the treatment of choice up to recently; it kills the microfilariae but had no effect on the adult worm. The usual dose is 150 μg/kg orally once or twice a year for 10–15 years for the lifespan of the adult worm. Mass drug administration of ivermectin to endemic villages has been found to be effective to control the disease. The lack of safe and effective drugs to kill the adult worms has been a major restriction in the therapy of onchocerciasis.
The adult worm depends on an endosymbiotic bacteria, Wolbachia, for its survival and embryogenesis. Thus, therapy aimed at the bacteria can be used to kill the adult worm using doxycycline 200 mg daily for 6 weeks and ivermectin started 1 week before [19]. Doxycycline can kill 60% of adult female worms and sterilize up to 90%. However, this has not been instituted as standard therapy due to lack of robust data showing clinical ocular benefit. The efficacy of doxycycline with ivermectin in onchocerciasis was previously reviewed in the Cochrane Database [20]. Three randomized controlled trials included 466 patients treated with doxycycline and ivermectin versus ivermectin alone. However, the studies were considered low quality with missing data and selective outcome reporting.
Moxidectin was approved for treatment for human onchocerciasis by the US FDA in 2018, but it was used for years in veterinary medicine to treat farm animals with helminth infections. It is a semisynthetic macrocyclic lactone of the milbemycin class, a derivative of nemadectin which is a fermentation product of Streptomyces species [21].
4.3 Pharmacology of Moxidectin
Moxidectin is rapidly absorbed with peak plasma concentration in 3–4 h, and the total AUC0–24 increases linearly with the dose [21]. It can be taken with or without food and a liquid formulation only increases the bioavailability modestly. Administration with a high fat meal increases the Cmax and AUC by 34–39% but is considered not clinically meaningful. It is lipophilic and may be retained in adipose tissue, widely distributed with a large volume of distribution (1.2 L/kg) and half-life of 20–43 days. The plasma protein binding is unknown in humans. Moxidectin is minimally metabolized in the body, it is not a substrate or inhibitor of CYP enzymes, renal elimination of the intact drug is negligible, and only 2% of the dose is excreted unchanged in the feces within 72 h. Mild to moderate renal impairment is not expected to affect the drug exposure, and it has not been studied in severe renal impairment. There is no known drug-drug interactions. A single dose of 8 mg is recommended for onchocerciasis.
4.4 Mechanism of Action of Moxidectin
The mechanisms of action of moxidectin have not been studied in O. volvulus but in other nematodes. It binds to glutamate-gated chloride ion channels vital to the function of invertebrate nerves and muscle cells, leading to influx of chloride ions, hyperpolarization, and muscle paralysis leading to death [21]. The drug is active against the microfilariae of O. volvulus and not effective in killing the adult worms, but it inhibits the intra-uterine embryogenesis and release of microfilariae from the adult worms (Moxidectin accessdata.fda.gov.).
Resistance of O. volvulus to moxidectin has not been found as yet but likely will occur with widespread use as it is common in nematodes of livestock. Continued use can result in therapeutic failure and cross-resistance between moxidectin and ivermectin [21].
4.5 Clinical Efficacy of Moxidectin
Phase II trial compared 2, 4, and 8 mg dose of moxidectin to the standard dose of ivermectin (150 μg/kg) and all three moxidectin doses resulted in faster and more complete clearance of microfilariae from skin than ivermectin [21]. Microfilaridermia reappeared after 2 months with ivermectin and progressively longer with increasing dose of moxidectin—up to 12 months after 8 mg, which was chosen for the dose in the phase III trial.
The phase III trial enrolled patients from 4 sites in sub-Saharan Africa to receive single oral dose of 8 mg moxidectin (n = 978) or oral ivermectin at 150 μg/kg (n = 494) and assessed clinical response at 1 year for skin microfilarial density [22]. The microfilarial density was significantly lower in the moxidectin group, treatment difference 86% (p < 0.0001). Mazzotti reactions (host response to dying microfilariae) occurred in 99% of moxidectin-treated patients and 97% of the ivermectin group, but no serious adverse reactions were related to treatment. Severe transient postural hypotension (causing dizziness and weakness) was the only efficacy-related grade 4 reaction that was more common in the moxidectin than the ivermectin group (5% vs 1%). Drug adverse events were rare with moxidectin, other than the Mazzotti reactions. Ocular Mazzotti reactions were similar in the two groups, 12% for moxidectin and 10% for ivermectin, including pruritus, conjunctivitis, eye pain, eyelid swelling, blurred vision, or tearing.
4.6 Adverse Effects of Moxidectin
The adverse reactions to moxidectin, similar to ivermectin, were nearly all related to the Mazzotti reaction of the host to the dying microfilariae, and these include flu-like illness, pruritus, rash, musculoskeletal pain, headaches, ocular reactions, dizziness, weakness, enteritis, edema, worsening onchodermatitis, severe eosinophilia, leukocytosis, leucopenia, and increased liver enzymes (Moxidectin accessdata.fda.gov.). Similar to ivermectin, encephalopathy can occur with co-infection with Loa loa, which should be excluded before its use.
5 Tafenoquine
5.1 Plasmodium vivax Malaria
Plasmodium vivax malaria is the commonest form of malaria globally [23] and since 1980, relapse after treatment with chloroquine was thought to be due to activation of hypnozoites that reside in the liver. However, reactivation of malaria hypnozoites have only been shown recently [24]. Hence, standard treatment usually consists of 3-days chloroquine to clear the circulating trophozoites followed by 14 days primaquine to eradicate hypnozoites from the liver. For many decades, primaquine was the only drug available for radical cure of P. vivax and P. ovale malaria. Moreover, 14 days of primaquine often leads to poor compliance and incomplete treatment, and it can cause hemolytic anemia in subjects with glucose-6-phosphate dehydrogenase (G6PD) deficiency. However, the burden of P. vivax malaria decreased by 41.6% from 24.5 million cases in 2000 to 14.3 million cases in 2017 [23].
5.2 Pharmacology of Tafenoquine
Tafenoquine (TQ) was approved by the FDA for the radical cure of P. vivax malaria in 2018, the first new treatment in about 60 years. It is an 8-aminoquinoline derivative of primaquine which varies only by the presence of a 5-phenoxy group [25].
Oral TQ is slowly absorbed with peak plasma concentration in 8–12 h, and fatty meal increases the absorption by 30–40% [26]. The terminal plasma half-life is 12–16 days, and it is highly protein bound, 99.5%, but widely distributed with volume of distribution >200 liters. After degradation by several different pathways, TQ is slowly excreted primarily in the feces and renal elimination of the unchanged form is very low. The active metabolite 5,6 ortho-quinone-tafenoquine is produced in the liver by the activity of CYUP 2D6 microsomal enzyme (DrugBank Online). The dose of TQ for radical cure of vivax malaria is a single oral dose of 300 mg.
5.3 Antimalarial Activity of Tafenoquine
The mechanism of action of TQ is not fully known, but it appears that the active metabolite is internalized by the parasite and the oxidized metabolite produced hydrogen peroxide and hydroxyl radicals that lead to death of the parasite (Tafenoquine, DrugBank Online). It is active against the developing and dormant liver stages of the hypnozoites, the erythrocytes asexual stages (schizonticidal), gametocytes transmitted to mosquitoes, and sporozoites injected into humans by the mosquitoes.
5.4 Clinical Efficacy of Tafenoquine
Three randomized clinical trials in 9 malaria-endemic countries were conducted in 747 adult patients with P. vivax malaria [27]. All patients received chloroquine to clear the blood parasites and some groups received placebo, or primaquine 15 mg daily for 14 days, or single 300 mg dose of TQ. Patients receiving TQ had fewer relapse than those receiving placebo within 6 months and appeared to be similarly effective as primaquine. However, relapse of vivax malaria can occur up to a year which would not be captured by these studies. Overall the adverse events of TQ were similar to primaquine. TQ was found to have low efficacy to prevent vivax malaria in Indonesia when combined with dihydroartemisinin-piperaquine for unknown reasons [28].
TQ has also been studied for malaria prophylaxis in residents of malaria-endemic countries of Africa in placebo controlled studies and with mefloquine [29]. The drug was given as 3 daily loading doses plus weekly maintenance of 200 mg weekly for 10 weeks or more. Its pooled prophylactic efficacy was 93% and was similar to that of mefloquine 250 mg weekly.
5.5 Safety of Tafenoquine
TQ safety profile is similar to primaquine and patients before treatment should be tested for glucose-6-phosphate dehydrogenase (G6PD). Similar to primaquine, it can cause anemia, methemoglobinemia, leucopenia, and hemolytic anemia in subjects with G6PD deficiency (fda.gov/media/114755/download). In most studies, adverse events have been mild, most commonly nausea and abdominal cramps (≥5%) and CNS side effects (headaches, dizziness, abnormal dreams, insomnia, anxiety, and depression) [28]. TQ is not indicated in pregnancy, and it should be used with caution in psychotic disorders. Although primaquine can cause cardiac arrhythmia and prolongation of QT interval, no similar effects have been reported with TQ even in patients receiving the drug for 26 weeks [30].
6 Triclabendazole
6.1 Human Fascioliasis
Fascioliasis is a foodborne nematode infection, considered a neglected zoonosis by the WHO that has been reported in 81 countries with estimate of 2.6 million people infected globally [31]. The burden of disease of liver flukes is believed to be underestimated, and the disease appears to be emerging with climate change and 91 million people are at risk for infection globally.
Two trematode parasites are responsible for disease, Fasciola hepatica, reported throughout the world in patchy distribution, and Fasciola gigantica, present mainly in tropical regions of Africa, South and East Asia, and the Middle East. Sheep and cattle are the natural hosts of the parasites, but a wide range of wild and domestic mammals (46 species) can be infected, including humans [32]. Eggs shed in the stool of definitive mammal host embryonate in fresh water, releasing miracidia which infect 30 snail species (intermediate host), which release cercariae in the water that encyst to metacercariae on leafy water vegetables [32]. Humans become infected by eating contaminated watercress or other water plants. After ingestion, the metacercariae excyst in the intestines, allowing the immature parasites to penetrate the wall of the intestine, migrate in the abdominal cavity, and penetrate the liver to reach the bile ducts [32].
The acute migratory phase may last >12 weeks and associated with upper abdominal pain, fever, high eosinophilia, and hypodense track-like lesions on liver imaging. Mature parasites in the bile ducts produce inflammation, biliary obstruction, intermittent pain, and jaundice, which may result in subcapsular hematoma, liver abscess, liver fibrosis, and cirrhosis [32]. Otherwise asymptomatic patients may present with weight loss and anemia.
Livestock industry is markedly affected with estimates of 10–80% of dairy and meat cattle infected in developing and developed countries, and human populations in developing countries are mostly affected [32]. People living in poverty in small communities in the Andes Mountains of Bolivia, Ecuador, and Peru account for large portion of the global burden of fascioliasis. Other endemic countries include the Middle East (Egypt, Turkey, Iran), African countries, Asia (China and Vietnam), and some European countries (Portugal, Spain, and France).
Diagnosis of fascioliasis can be challenging and include abdominal imaging, ultrasound or computerized tomography (CT), serology and detection of the Fasciola spp. eggs, or antigen in duodenal aspirate or stools. Treatment includes anthelmintics to kill the flukes and symptomatic therapy.
6.2 Triclabendazole for Fascioliasis
Triclabendazole (TCZ) is a benzamidine derivative with a chlorinated benzene ring but no carbamate group, unlike other benzimidazole family of anthelmintics, that was developed and marketed by Ciba Pharmaceuticals (Fasinex) to treat fascioliasis in livestock in 1983, subsequently marketed for human use in the 1990s, and only approved by the FDA in 2019 for human fascioliasis [33].
TCZ, distributed by Novartis as Egaten for human fascioliasis, is a narrow-spectrum anthelmintic with activity only against Fasciola (F. hepatica and F. gigantica) and Paragonimus spp. [33]. The mechanism of action is not completely clear, but it may involve multiple targets, such as tegument disruption by preventing the polymerization of microtubules or adenylate cyclase activity [34]. The sulfoxide metabolite appears to have greater effect on the parasite motility than TCZ, through marked disruption of the integument and inhibition of protein synthesis [35].
6.3 Pharmacology of Triclabendazole
Oral TCZ is rapidly absorbed to produce mean Cmax in 3–4 h and food enhance the absorption to increase Cmx and AUC of TCZ and sulfoxide metabolite two to three fold [33]. The drug is metabolized primarily by CYP1A2 and CYP2C9 into the active sulfoxide and sulfone metabolites, and the elimination half-life of TCZ and the metabolites is about 8 and 11–14 h [36]. The protein binding of TCZ was 96.7% and the metabolites 98.4–98.8% and the volume of distribution for the sulfoxide metabolite 1 L/kg. There is no excretion data in humans, but in animals the drug and the metabolites are largely excreted by the biliary tract and the feces (90%) with less than 10% in the urine [33]; its metabolites have the potential to inhibit many cytochrome P enzymes, the greatest inhibition on CYP2C19.
The recommended dose for acute or chronic fascioliasis is two doses of 10 mg/kg per dose with food separated by 12–24 h.
6.4 Clinical Efficacy of Triclabendazole
Clinical trials conducted over the past 25 years, and multiple case reports, found TCZ to have high efficacy (>70–100%, with dose dependent response) and was well tolerated [33]. Two randomized, controlled trials have been conducted. In Vietnam, 100 patients with fascioliasis were randomized to TCZ (2 doses of 10 mg/kg, 12 h apart) or artesunate 4 mg/kg once daily for 10 days [37]. The clinical response rate at 3 months (resolution of symptoms) was higher with TCZ (92%) versus 76% for artesunate (p = 0.05), but the improvement on imaging with ultrasound were similar (76% vs 70%). However, stools were not examined for microbiological response.
Uncontrolled studies that used fecal egg counts to assess efficacy of TCZ were summarized in a review article [33]. Different doses were used in various studies (10 mg/kg, 15 mg/kg and 20 mg/kg total dose) in 364 patients in 6 studies. The rate of clearance from the stools varied from 69% to 100% with the highest response usually occurring with 20 mg/kg given as two separate doses.
6.5 Treatment Failure and Resistance to Triclabendazole
Resistance of F. hepatica to TCZ has become widespread in livestock and has been reported in 17 endemic countries around the world, but the mechanisms of resistance are unknown [38]. Treatment failure and resistance of human cases of fascioliasis are sporadic and include a farmer in the Netherlands, four cases from Chile, one case from Turkey, and seven cases from Peru [39]. This is an emerging problem in the Andes of Peru, where 7 of 19 selected cases failed to clear Fasciola eggs after multiple courses of 2 doses of TCZ at 10 mg/kg per dose [40].
The underlying biochemical mechanisms of TCZ resistance remains unclear, but there is evidence of metabolic differences between susceptible and resistant isolates, indicating that altered uptake, efflux, and metabolism of TCZ are more important in the resistance than the tubulin-based process [39]. A single amino acid substitution in glutathione S-transfer in a resistant F. hepatica isolate had been detected, but this has not been confirmed in other resistant isolates [39].
6.6 Safety of Triclabendazole
TCZ is generally well tolerated and adverse reactions such as abdominal pain (56–93%), nausea (8–18%), and liver enzyme elevations (3.6–8%) may be due to expulsion of the liver fluke than from toxicity of the drug [36]. Other side effects greater than 2% include vomiting (6–7%), urticaria (7–11%), headache (6–14%), and musculoskeletal pain (4%).
7 Conclusion
Of the five drugs recently approved by the US FDA for treating invasive parasites, only three are actually new agents. For summary of the drugs profile, see Table 11.1. FNZ and moxidectin for African trypanosomiasis and onchocerciasis, respectively, represent real advance in the management of two serious neglected tropical diseases. TQ, a new drug for radical cure of P. vivax and P. ovale, represent a modest advance in the management of these malaria species, allowing single dose therapy which should improve compliance in completing treatment compared to 14 days of primaquine. BZN and TCZ are older drugs that were available in endemic countries of Chagas disease and fascioliasis, respectively, now allowing physicians in the US to access these drugs for infected migrants that moved to North America.
More effective and safer drugs are needed for serious and expanding parasitic infections such as multidrug-resistant falciparum malaria and the less frequent visceral leishmaniasis. Falciparum malaria resistant to artemisinin/artemether combinations are now spreading throughout Asia and eventually will be a global problem. Yet we have no new agents approved to meet this challenge. The time to act is now before it’s too late.
References
Pink R, Hudson A, Mouries M-A, Bendig M. Opportunities and challenges in antiparasitic drug discovery. Nat Rev. 2005;4:727–40.
WHO. Chagas disease [also known as American trypanosomiasis] World Health Organization, 1 April, 2021. https://www.who.int/news-room/fact-sheets/detail/chagas-disease-[american-trypanosomiasis
Manne-Goehle J, Umeh CA, Montgomery SP, Wirtz VJ. Estimating the burden of Chagas disease in the United States. PLoS Negl Trop Dis. 2016;10:e0005033.
Antinori S, Galimberti L, Bianco R, Grande R, Galli M, Coprbillino M. Chagas disease in Europe: a review for the internist in the globalized world. Eur J Intern Med. 2017;43:6–15.
Stanaway JD, Roth G. The burden of Chagas disease. Glob Heart. 2015;10:139–44.
Bern C, Montgomery SP, Herwaldt BL, et al. Evaluation of treatment of Chagas disease in the United States. JAMA. 2007;298:2171–81.
Perez-molina JA, Perez-Ayala A, Moreno S, Fernandez-Gonzalez C, Zamora J, Lopez-Valez R. Use of benznidazole to treat chronic Chagas’ disease: a systematic review with a meta-analysis. J Antimicrob Chemother. 2009;64:1139–47.
Wilkinson SR, Kell JM. Trypanosomal drugs: mechanisms, resistance and new targets. Expert Rev Mol Med. 2009;11:e31.
de Higuchi ML, De Brito T, Martins Reis M, et al. Correlation between Trypanosoma cruzi parasitism and myocardial inflammatory infiltrate in human chronic chagasic myocarditis: light microscopy and immunohistochemical findings. Cardiovasc Pathol. 1993;2:101–6.
Morillo CA, Marin-Neto JA, Avezum A, et al. Randomized trial of benznidazole for chronic Chagas cardiomyopathy. NEJM. 2015;373:1295–306.
Hasslocher-Moreno AM, Saraiva RM, Sangenis LHC, et al. Benznidazole decreases the risk of Chagas disease progression and cardiovascular events: a long-term follow-up study. EClinicalMedicine. 2021;31:100694.
WHO. Trypanosomiasis, human African [sleeping sickness]. World Health Organization; 18 May 2021. https://www.who.int/news-room/fact-sheets/detail/trypanosomiasis-human-african-[sleepingsickness].
Torrele E, Trunz BB, Tweats D, Kaiser M, Brun R, Mazue G, Bray MA, Pecoul B. Fexinidazole—a new nitroimidazole drug candidate entering clinical development for the treatment of sleeping sickness. PLoS Negl Trop Dis. 2010;4:e923.
Kaiser M, Bray S, Cal M, Bopurdin Trunz B, Torreale E, Brun R. Antitrypanosomal activity of fexinidazole, a new nitroimidazole entering clinical development for the treatment of sleeping sickness. Antimicrob Agents Chemother. 2011;55:5602–8.
Betu Ku Mesu VK, Kalonji MK, Bardonneau C, et al. Oral fexinidazole for late-stage African Trypanosoma brucei gambiense trypanosomiasis: a pivotal multicenter, randomized, non-inferiority trial. Lancet. 2018;391:144–54.
Chappuis F. Oral fexinidazole for human African trypanosomiasis. Lancet. 2018;391:100–2.
Betu Ku Mesu VK, Kalonji WM, Bardonneau C, et al. Oral fexinidazole for stage 1 or early stage 2 African trypanosome brucei gambiense trypanosomiasis: a prospective, multicenter, open-label, cohort study. Lancet Glob Health. 2021;9:e999–1008.
Gyasi M, Okonkwo ON, Tripathy K. Onchocerciasis. NCBI Bookshelf. Updated Sept. 2021. https://www.ncbi.nim.nih.gov/books/NBK559027/
Hoerauf A, Mand S, Volkmann L, Buttner M, Marfo-Debrekyei Y, Taylor M, Adjei O, Buttner DW. Doxycycline in the treatment of human onchocerciasis: kinetics of Wolbachia endobacteria reduction and inhibition of embryogenesis in female Onchocerca worms. Microbes Infect. 2003;5:261–73.
Abegunde AT, Ahuja RM, Okafor NJ. Doxycycline plus ivermectin versus ivermectin alone for treatment of patients with onchocerciasis. Cochrane Database Syst Rev. 2016;(1):Art. No.: CD011146. https://doi.org/10.1002/1451858.CD011145.pub2.
Milton P, Hamley JID, Walker M, Basanez M-G. Moxidectin: an oral treatment for human onchocerciasis. Expert Rev Anti-infect Ther. 2020;18:1067. https://doi.org/10.1080/14787210.2020.1792772.
Opoku NO, Bakajika DK, Kanza EM, et al. Single dose moxidectin versus ivermectin for Onchocerca volvulus infection in Ghana, Liberia, and The Democratic Republic of the Congo: a randomized, controlled, double-blind phase 3 trial. Lancet. 2018;392:1207.
Battle KE, Lucas TCD, Nguyen M, et al. Mapping the global endemicity and clinical burden of Plasmodium vivax, 2000–17: a spatial and temporal modelling study. Lancet. 2019;394:332–43.
Markus MB. Transition from plasmodial hypnozoite to schizont demonstrated. Trends Parasitol. 2020;36:407–8.
Luk K-Y, Derbyshire ER. Tafenoquine: a step towards malaria elimination. Biochemistry. 2020;59:911–20.
Edstein MD, Kocisko DA, Brewer TG, et al. Population pharmacokinetics of the new antimalarial agent tafenoquine in Thai soldiers. Br J Clin Pharmacol. 2001;52:663–70.
Rodrigo C, Rajapakse S, Fernando D. Tafenoquine for preventing relapse in people with Plasmodium vivax malaria. Cochrane Database Syst Rev. 2020; https://doi.org/10.1002/14651858.CD01458.pub3.
Markus MB. Safety and efficacy of tafenoquine for Plasmodium vivax malaria prophylaxis and radical cure: overview and perspectives. Ther Clin Risk Manag. 2021;17:989–99.
Dow GS, Liu J, Hetzell B, et al. Summary of anti-malarial prophylactic efficacy of tafenoquine from three placebo-controlled studies of residents of malaria-endemic countries. Malar J. 2015;14. https://malariajournal.biomedicentral.com/articles/10.1186/s12936-015-0991-x
Chu CS, Hwang J. Tafenoquine: a toxicity overview. Expert Opin Drug Safety. 2021;20:349–62.
Furst T, Keiser J, Utzinger J. Global burden of human foodborne trematodiasis: a systematic review and meta-analysis. Lancet Infect Dis. 2021;12:210–21.
Carvedo MJ, Cabada MM. Human fasciolosis: current epidemiological status and strategies for diagnosis, treatment, and control. Res Reports Trop Med. 2020;11:149–58.
Gandhi P, Schmitt EK, Chen C-W, Samantray S, Venishetty VK, Hughes D. Triclabendazole in the treatment of human fascioliasis: a review. Trans R Soc Trop Med Hyg. 2019;112:797–804.
Kelley JM, Elliott TP, Beddoe T, et al. Current threat of triclabendazole resistance in Fasciola hepatica. Trends Parasitol. 2016;32:458–69.
Keiser J, Engels D, Buscher G, Utzinger J. Triclabendazole for the treatment of fascioliasis and paragonimiasis. Expert Opin Investig Drugs. 2005;14:1513–26.
EGATEN™ (triclabendazole) tablets. Product Mono[1]graph. 2019. Novartis Pharmaceuticals Corporation, East Hanover, New Jersey. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/208711s000lbl.pdf. Accessed 24 Mar 2022.
Hien TT, Ttruong NT, Minh NH, et al. A randomized controlled pilot study of artesunate versus triclabendazole for human fascioliasis in Central Vietnam. Am Trop Med Hyg. 2008;78:388–92.
Fairweather I, Brennan GP, Hanna REB, Robinson MW, Skuce PJ. Drug resistance in liver flukes. Int J Paarsitol Drugs Drug Resist. 2020;12:12–39.
Kelley JM, Ellioott TP, Beddoe T, Anderson G, Skuce P, Spithill TW. Current threat of triclabendazole resistance in Fasciola hepatica. Trends Parasitol. 2016;32:458–69.
Cabada MM, Lopez M, Cruz M, Delgado J, Hill V, White C Jr. Treatment failure after multiple courses of triclabendazole among patients with fascioliasis in Cusco, Peru: a case series. PLoS Negl Trop Dis. 2016;10:e0004361.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fong, I.W. (2023). Newly Approved Anti-parasitic Drugs for Malaria, Fascioliasis, Onchocerciasis, Chagas Disease, and African Trypanosomiasis. In: New Antimicrobials: For the Present and the Future. Emerging Infectious Diseases of the 21st Century. Springer, Cham. https://doi.org/10.1007/978-3-031-26078-0_11
Download citation
DOI: https://doi.org/10.1007/978-3-031-26078-0_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-26077-3
Online ISBN: 978-3-031-26078-0
eBook Packages: MedicineMedicine (R0)