Abstract
The prevalence of tobacco use disorder, with cigarette smoking recognized as the most dangerous, has far-reaching and harmful health effects. These deleterious health effects and premature death are directly correlated with the duration and intensity of tobacco smoke exposure. There is strong evidence demonstrating the benefits of quitting smoking before, at the time of, and following a lung cancer diagnosis and survival from other smoking-related disorders. There is much to be gained with successful cessation efforts. People at high risk for developing lifelong tobacco use disorder commonly experience social and economic inequities contributing to their tobacco dependence. Targeting the factors that lead to chronic tobacco use and health inequities is vital in addressing related health disparities, effective tobacco cessation services, and achieving cessation success. No one-size-fits-all model exists in the effective integration and implementation of tobacco treatment. Tobacco treatment should be threaded throughout all ambulatory encounters and integrated with every touchpoint patients have across the continuum of clinical care, where healthcare providers and staff are universally trained and prepared to provide comprehensive combination tobacco dependence treatment that includes counseling and pharmacotherapy. Integration and implementation of tobacco dependence treatment is enhanced by patient- and family-centered care and communication, the power of the electronic health record, and the proactive engagement of healthcare providers and health system leadership.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Tobacco use disorder (TUD), with cigarette smoking as the most prevalent form of tobacco use, is a chronic illness that commonly leads to premature morbidity, disability, and death. If not adequately addressed, people who smoke long-term die 10 years before their never-smoking peers [1].
While cigarette smoking rates have consistently dropped and are now at an all-time low (14% in 2019) in the United States (U.S.), 34 million people continue to smoke combustible cigarettes in the U.S [2] and are continuously exposed to the deleterious effects of cigarette smoke. Diseases related to cigarette smoking account for 5 of the 6 top causes of death, with coronary artery disease (CAD) being the most predominant, followed by stroke, chronic obstructive pulmonary disease (COPD), and cancers of the head and neck and lung [3, 4].
Most, if not all, of the leading preventable cancers and deaths in the U.S. are at least in part or entirely attributable to tobacco use [2, 5], with lung cancer being the leading cause of cancer deaths [6]. Cigarette smoking is directly implicated in 87% of all lung cancers [7, 8]. People who smoke cigarettes are 25 times more likely to develop lung cancer than people who never smoked [9]. Healthcare providers, both at the individual and large health system level, have an immense opportunity to harness formative moments in people’s lives to proactively address cigarette smoking, provide a potentially life-altering opportunity in successfully quitting, and enhance the chances of never suffering or prematurely dying from a tobacco-related disease.
Cessation Related Risk Reduction in Lung Cancer Screening, Cancer Care, and Beyond
Teachable moments and opportunities to integrate smoking cessation into clinical care are accentuated at the time of lung cancer screening [10,11,12], major procedures and surgery [13], and at an acute health event necessitating an emergency room admission [14], among other sentinel moments in a person’s health journey. Regardless of the length of time having smoked, a person’s age, or their current health state, people who smoke cigarettes have an immense amount to gain from successfully quitting smoking. It is imperative to identify where and when to help people within the continuum of care in all healthcare settings. Prioritizing screening for tobacco use and integration of comprehensive cessation services in all clinical care settings is paramount. An end goal of helping people successfully quit smoking is an essential duty of all healthcare providers in all ambulatory care settings.
Lung Cancer Screening
Approximately 50% of individuals enrolled in lung cancer screening (LCS) currently smoke cigarettes [15]. At least that many or more are smoking up to a year before they are diagnosed with lung cancer and continue to smoke after a lung cancer diagnosis. Those who are at high risk for developing lung cancer and are also eligible for LCS can benefit from a three to fivefold mortality reduction when they quit smoking and stay quit [16]. Validated microsimulation lung cancer natural history modeling, using the 2021 United States Preventive Services Task Force (USPSTF) LCS recommendation, has been used to determine the value of joint LCS and cessation interventions measured in averted lung cancers and life-years gained. This modeling shows that even with a modest 30% uptake of LCS and a 15% quit rate following a cessation intervention at the time of the initial screen, an estimated 2422 additional lung cancer related deaths can be averted (representing a 73% increase compared to not quitting) and 322,785 life-years gained (318% increase), presumably in mortality reductions from lung cancer and other smoking-related diseases [17]. Predictably, there would be an exponential benefit if all (100%) screen eligible individuals engaged in LCS had a 15% quit rate following first-time screening; this would yield 31, 998 lung cancer deaths averted and 1,086,840 life-years gained [17]. Building on this modeling research, a study examining survival from smoking cessation in the National Lung Screening Trial demonstrated a similar mortality reduction at 7 years following successful smoking cessation as compared to the survival benefit of early detection of lung cancer by LCS [18].
Lung Cancer
The mortality risk for people who continue smoking after a lung cancer diagnosis is twice that of someone who quits smoking [19]. The benefits of quitting smoking once a lung cancer diagnosis is established are well documented. A systematic review with meta-analysis examining the effects of smoking cessation after diagnosis of a primary lung tumor shows that quitting smoking following a diagnosis of an early-stage lung cancer results in at least a 30% increased 5-year survival for people who quit smoking compared to those who do not quit [19]. Finally, there is also evidence that for people who have a history of lung cancer, smoking cessation yields an 83% risk reduction for the development of second primary lung cancers [20], thus enhancing the survival benefit of cessation.
Cancer Treatment
The primary goals of cancer treatment are to avoid disease progression and achieve recurrence-free survival from cancer. Cessation of tobacco use is an effect modifier for people with cancer who use tobacco products. Quitting smoking enhances the therapeutic response to cancer treatment, reduces treatment related toxicities, and reduces the incidence of disease progression, development of second primary cancers, and cancer recurrence [20,21,22]. The benefits of quitting tobacco products, including cigarette smoking, are not only measurable in people with lung cancer but have also been shown to control other cancers and improve cancer and non-cancer related outcomes, with a 43%–52% mortality risk reduction across the cancer continuum when people quit smoking compared to those who continue to smoke [21, 23].
Non-Cancer Related Conditions
While lung cancer is the leading cause of cancer deaths in the U.S., the annual mortality related to cardiovascular disease (the leading cause of non-cancer related deaths) is nearly five times higher (690,882) [4] than lung cancer deaths (131, 880) [9]. Cigarette smoking is an independent risk factor for cardiovascular disease (CVD), and added CVD risk factors such as uncontrolled diabetes or hyperlipidemia in addition to cigarette smoking result in exponential risk for CVD and related morbidity and mortality [24]. Thirty to fifty percent of people who clinically present with their first cardiovascular event are actively smoking cigarettes [25]. Successful cessation after an initial cardiovascular event significantly reduces the risk of recurrent cardiovascular events and adds an average of 5 years of life [25].
Marginalized Populations and Tobacco Use Disorder
While the overall cigarette smoking rates are at an all-time low, specific vulnerable populations and minority groups suffer disproportionately high rates of tobacco use disorder, nicotine dependence, and morbidity and mortality related to smoking cigarettes, including lung cancer and other tobacco-related diseases (Chap. 1). The highest attainment of health begins with addressing health disparities and resulting health inequities. Most people who have fallen victim to a lifetime of smoking cigarettes have been historically or are currently marginalized. Healthcare systems and providers must take heed of the social determinants of health and risk factors for tobacco use disorder to best understand the patients who are being served and build care systems and delivery models to accommodate their needs effectively.
The risk factors for tobacco use disorder, including smoking cigarettes, are not always evident. People who are especially at risk, impacted by tobacco use, and regularly use some form of tobacco are more commonly [26]:
-
black, indigenous people of color (BIPOC),
-
people who have a high school education or less,
-
those with an annual household income at the federal poverty level or below,
-
belong to the LGBTQ+ community,
-
uninsured, underinsured, or on state Medicaid coverage,
-
having any level of generalized anxiety disorder or other serious mental health disorder,
-
of male gender.
These factors are significant predictors of cigarette smoking. In addition, people who are uninsured or on state Medicaid health coverage are twice as likely (24.9%) to smoke cigarettes than those with private insurance coverage (10.7%) [27], well above the 14% national average for cigarette smoking [27]. People who experience poverty below the U.S. threshold have double the chances of smoking cigarettes (22.6%) than those 2× above the poverty threshold (11.2%) [26]. People whose highest educational attainment is a general education diploma certificate are nearly 5× as likely (35.0%) to smoke cigarettes than those with at least a four-year college education (6.9%), and American Indian and Native Alaskan people experience the highest smoking prevalence (20.9%) compared to the lowest prevalence in the Hispanic race (8.8%) [27]. Finally, people who experience psychiatric-mental health disorders are three times more likely to smoke cigarettes than those not afflicted by such diseases [28]. These patterns are steady and ultimately preventable, and because of this, the fight against tobacco starts upstream in our communities and across the care continuum in our health systems [27].
Systemic and Structural Racism and Cessation Services
People at risk for and who suffer from tobacco dependence are predominantly at the lower end of the social and economic structure and power differential, exacerbating marginalization and subsequent inequities in providing smoking cessation services and health disparities. Notably, this is reflected in the fact that less than 5% of people who smoke receive the evidence-based standard of care of combination behavioral health counseling and medication therapy [26] and further demonstrated in the lower rates (44.1%) of advice to quit smoking for people who are uninsured compared to 56.8% quit advice provided to people who have commercial or employer-based insurance. The more disparate use of evidence-based cessation interventions is also illustrated by only 21.4% uninsured people (58.9% who are BIPOC and 78.7% being at 100–400% below the Federal poverty level) receiving treatment, compared to 32.1% of the privately insured, who are 41.1% white [26, 29]. Such inequities reflect structural and systemic racism and economic inequality that lead to persistent and chronic tobacco use and the subsequent health effects from TUD and cigarette smoking.
This evidence underscores the need for social and healthcare systems that humanize care, establish, build, maintain trust, and prepare to serve the specific needs of people affected by TUD and cigarette smoking. This includes identifying and addressing the systemic factors, including policies that contribute to these vast disparities, and building care systems that are just in resource allocation of comprehensive cessation services. This will be reflected in the prioritization of universal access to equitable care delivery and quality health outcomes for everyone they serve.
Quality and Personalized Patient Engagement
Quality Healthcare Underpinnings
With the continued shift from fee-for-service toward bundled care and value-based reimbursement models, an emphasis on prioritizing the provision of high-impact health care that produces high-quality outcomes is pronounced in the U.S. Successful integration of tobacco cessation services into clinical care calls for the convergence of the Institute of Medicine’s six measurable domains of health care quality that includes [30]:
-
Safe care that avoids harm to patients from the care intended to help them.
-
Care that is Effective and provides services based on scientific knowledge to all who could benefit and refraining from providing services that are not known to be beneficial.
-
It provides Patient-Centered Care that is respectful of and responsive to individual patient preferences, needs, and values (“nothing about me without me”). Patient-centered care ensures that this information and the patient’s voice are central to the clinical decision framework and guide all clinical decisions.
-
Quality care is timely and reduces long waits and sometimes harmful delays for those who receive and those who give care.
-
It is Efficient care that avoids waste.
And finally, quality health care is represented in the provision of Equitable care where the care does not vary in quality because of personal characteristics such as gender, ethnicity, sexual or gender identity, geographic location, and socioeconomic status [30]. These health care quality domains should be threaded throughout the care continuum and intentionally embedded in cessation services to achieve high-impact and personalized care.
Healthcare Provider Positionality, Implicit Bias, and Stigma
The life experiences and resources that accelerate opportunities and advantages for some people, including many who become healthcare providers, shape how they understand the world, their privileges in society, and the power they may possess over others, including patients [31]. It is critical to understand how social privilege, which leverages access to resources and power, shapes healthcare providers’ identities and the lens through which they interpret the world, called positionality [31, 32]. Having insight into one’s positionality can be particularly impactful when working with people who are marginalized and experience societal inequities that can lead to tobacco use disorder (cigarette smoking) and additional health inequities.
Healthcare providers’ racial and ethnic unconscious bias (implicit bias) leads to discrimination in care delivery, compromised clinical outcomes [32], and resulting health disparities for people of color compared to white people [33]. The stigmatizing effects of belief that people are responsible for their substance dependence may result in healthcare providers withholding healthcare services and reinforcing continuance of substance use [34], all leading to internalized stigma (self-blame) [35, 36]. These all serve as barriers to medical help-seeking behavior [37] and contribute to worse quality of life and higher psychological distress for patients with lung cancer [38]. It is imperative for healthcare providers to have full awareness of their own biases—those which are “baked in” to the health system and institutional policies, and the stigma surrounding smoking. Proactive and intentional work must occur in these areas to dismantle these biases and the stigma of smoking. By doing so, we enhance the opportunity to genuinely reach patients who smoke cigarettes and are at risk for lung cancer and other tobacco-related disorders; this includes the demonstration of nonjudgmental and compassionate attitudes and the use of empathic communication [39]. The mindful and strategic construction of healthcare delivery models that support vulnerable individuals who smoke cigarettes with healthcare providers entering every patient relationship with an awareness of their positionality, implicit biases, and contributions to stigma is critical to the success of patient-centered care, reducing health disparities, and improving clinical outcomes.
Patient- and Family-Centered Care and Communication
Addressing TUD is a prime opportunity to utilize patient- and family-centered care and communication. The Institute for Patient- and Family-Centered Care, in collaboration with the Institute of Healthcare Improvement, identifies key concepts that are essential in patient- and family-centered care. These include promoting patient dignity and respect while honoring them and their families’ cultural backgrounds and beliefs. It also provides an opportunity for patients and family members to participate in care and decision-making and encourages information sharing with the patient and families [40]. Finally, collaboration is a core concept that represents a collaboration by healthcare providers and organizations with patients and families in the planning, development, implementation, and delivery of health care [40].
Lung Cancer Screening: An Opportunity for Patient-Centered Tobacco Treatment Care
Lung Cancer Screening
The past two decades have witnessed monumental advances in early detection of lung cancer predominantly through seminal research performed by the Early Lung Cancer Action Program [41], the National Lung Screening Trial [15], and most recently, the Nederlands–Leuvens Longkanker Screenings Onderzoek (NELSON) Trial [42]. These clinical trials and research demonstrate that the effective use of low dose computed tomography (LDCT) screening for early detection of lung cancer reduces mortality from this dreadful disease.
Using the 2021 United States Preventive Services Task Force (USPSTF) lung cancer screening criteria, an estimated 13.5 million people are at risk of developing lung cancer and are eligible for LCS [43]. Roughly half of these people are currently smoking cigarettes [44]. This yields a staggering 6.75 million people who could benefit from effective integration of cessation services in their care continuum and the opportunity to quit smoking, the most effective risk reduction method for developing lung cancer [45].
Shared Decision-Making Visits in Lung Cancer Screening
The 2015 Centers for Medicare and Medicaid Services (CMS) National Coverage Determination (NCD) for LCS mandated that a shared decision-making (SDM) visit is provided to all patients before LDCT screening occurs [46]. This was upheld in the most recent NCD, updated in 2022 [47], and represents the first example in the history of CMS, where service coverage is contingent on an SDM encounter. This mandate has been met with some opposition and concern that mandated SDM represents a barrier to LCS. Whether or not SDM continues to be a mandated precursor to LCS, it is essential to reframe the opportunity and value of SDM in the setting of LCS and beyond. The spirit of decision-making in a clinical encounter captures an opportunity for patient- and family-centered care. This facilitates an opportunity for providers to share important information with the patient, including the potential benefit and harms of an intervention. It also intentionally creates a space where the patient’s beliefs and values can be embraced. This vital patient information can then be incorporated into decision-making, in partnership with the patient, about their health, including that for LCS, smoking cessation (SC), other clinically relevant conditions, and for trust-building to occur. We must never forget that the patient is always an expert in their cultural beliefs and health values and the ultimate decision maker.
Tobacco Cessation in Lung Cancer Screening
The 2015 and 2022 NCDs for LCS also mandate counseling for people who formerly smoked on the importance of sustained abstinence. Counseling on SC is provided for people who currently smoke, and information about SC interventions is provided as appropriate [46]. The SDM visits open an excellent opportunity to capture this mandated tobacco moment with patients, initiate a conversation about their tobacco use, and offer cessation services.
Tobacco Use Disorder as a Chronic and Relapsing Condition Requires Comprehensive Cessation Services
The characteristics of tobacco use disorder and the chronic relapsing nature of this disease call for early intervention and ongoing management and monitoring, similar to other chronic diseases. With increased interest and emphasis on quality and health disparity outcomes measures, tobacco use disorder should be thoughtfully and meaningfully included with every patient touchpoint, in all clinical encounters, and universally and consistently addressed no matter where people are on the care continuum. This care should consist of routine screening for the use of any tobacco product, universal preparedness in providing continuing treatment and counseling or referring for such services, and relapse prevention, with all touchpoints across the healthcare and social service continuum with access to SC services and individualized risk and harm reduction assessment. It is essential that coordinated care planning and comprehensive services that meet patients’ tobacco use disorder, mental health, social, and primary care needs are provided, when necessary, with one-on-one support and follow-up. Furthermore, patient panel’s quality tracking and outcome measures are essential to short- and long-term success for individual and population health management.
Tobacco Treatment Recommendations
Identification of people who are actively smoking is essential to meaningfully reduce the risk of lung cancer and other tobacco-related diseases that contribute to disease, suffering, and premature death. Tobacco dependence can be effectively combated through many modalities, including providing combination behavioral and pharmacotherapy (see Chaps. 4 and 5). Behavioral strategies have been shown to improve outcomes and may be administered through various modalities (see Table 9.1 Behavioral Heath Tobacco Treatment Modalities) [48].
Behavioral counseling and pharmacotherapy provided in combination yield a 70–100% increased smoking cessation rate compared to either intervention alone [49] and 83% increased cessation compared to minimal intervention or usual care [50]. Equally important, a recent systematic review demonstrates the safety of the US Food and Drug Administration (FDA) approved pharmacotherapies for tobacco cessation with no associations with serious adverse events [50] in people with an established psychiatric disorder [51] or serious cardiovascular events [52]. Such evidence is the premise for the Grade A, Tobacco Smoking Cessation in Adults recommendation by the USPSTF that all adults are asked about tobacco use, advised to quit using tobacco and provided behavioral interventions and US FDA-approved pharmacotherapy for cessation [53].
More Quit Attempts But Dismal Dissemination and Uptake of Cessation Services
Nearly 80% of people at risk for lung cancer report they have tried to quit. This is much higher than the 50% in the general population who make a quit attempt every year [54]. However, 60% of these people report low levels of confidence that they can quit [55]; this low level of confidence is a barrier to successful cessation and just one of the many signals to healthcare providers that tobacco use disorder is complex and people who smoke need a broad array of resources to quit.
Finally, despite the current research that shows the benefits of evidence-based interventions for cessation success, the national USPSTF recommendation, and expanded coverage for cessation in the Affordable Care Act, people still are not getting what they need. More than half (57.2%) of people who smoke are advised to quit [26]. Yet, only 40% are provided some treatment (29% medication treatment, 6.8% cessation counseling, 4.7% using both) with nearly 60% not using evidence-based cessation treatment [26], leading to ineffectual and failed opportunities for successful cessation. These dismal statistics are a call to action and demonstrate an opportunity for healthcare institutions to proactively build out and invest in cessation opportunities and offerings.
Key Components of Integrated Tobacco Treatment in Clinical Care
National Call for Integration of Tobacco Treatment in Clinical Care
Increasingly, national organizations such as the National Comprehensive Cancer Network, The American Thoracic Society, The American College of Chest Physicians, and The American College of Cardiology are calling for integrating cessation into clinical care pathways. Federal research dollars are also being directed specifically to study such efforts and determine the most effective approach to implementing integrated tobacco cessation services into clinical care.
Collaborative and Comprehensive Patient-Centered Care
Broad variation in health care access, coverage, services, and coordination of care are barriers and current contributors to the detriment of effective clinical care and quality healthcare aims, particularly in the setting of tobacco use disorder. There is a great need for social and healthcare networks that serve the specific needs of people who struggle with tobacco dependence and cigarette smoking. Every encounter with a patient who is smoking is an opportunity for the healthcare team to positively impact cessation efforts and related short- and long-term health outcomes.
As a complex condition, tobacco use disorder treatment is time-consuming for all healthcare providers. Referral to a dedicated tobacco treatment program for comprehensive services and follow-up where a specific tobacco treatment team assumes full responsibility for all aspects of care is a largely idyllic and unattainable solution for most due to the resource-intensive needs for such services. Furthermore, making a referral for follow-up, specifically with a dedicated tobacco treatment provider, does not necessarily yield a high volume of long-term cessation success [56], introduces a significant chance of being lost to the referral process [57], and risks fragmenting care rather than capturing the opportunity in the teachable moment. Identifying available resources, including healthcare staff who can be developed and prepared to address tobacco use and the complexities of this disorder, is crucial when executing a plan for integration of cessation services across the care continuum.
Healthcare Workforce Bridging Health Equity and Gaps in Cessation Services
With growing attention to cessation priorities, health professionals and those in related fields are increasingly seeking cessation knowledge, skills, and preparation as certified tobacco treatment specialists. While such focused education for professionals who are independently motivated to help people quit smoking exist and continue to emerge, a commitment to embedding cessation services across the care continuum calls for a much more broad and systematic approach in developing healthcare staff to ensure that patients have access to such services. This includes not only healthcare staff and providers who are equipped and licensed to prescribe FDA-approved evidence-based pharmacotherapies but extends to those with expertise in behavioral and mental health and trusted members of the community like public and community health workers and social workers who are prepared to screen for tobacco use and collaborate in providing comprehensive smoking cessation support services.
The healthcare workforce can be positioned to close health equity gaps by bridging the chasms in healthcare where disadvantaged patients fall. Cessation knowledge and skills can be adopted and adapted by health professionals with diverse training and licensure. The identification and development of the healthcare workforce to identify tobacco use and provide cessation services can be especially effective in meeting the patient at any and all touchpoints in their healthcare journey. Universally training all workers in healthcare ensures opportunities to equitably provide people with timely, effective, efficient, and patient-centered cessation services. Training healthcare professionals in tobacco treatment improves the provision of smoking cessation services [58]. For example, targeting the training of nurses in tobacco treatment and equipping them with other tobacco treatment resources to support tobacco treatment interventions has shown to improve their ability to provide tobacco treatment with a 79% report of satisfaction with the training and a decline in reported barriers to delivering such treatment [59].
Table 9.2 titled Healthcare Workforce Positioned to Deliver Tobacco Treatment shows a comprehensive list of health care professionals who hold the potential to be skilled and positioned to serve as integral members of the frontline tobacco cessation workforce across the clinical and social care continuum.
Considerations for Pragmatic Integration of Tobacco Treatment in Clinical Care
The value and importance of integration of tobacco treatment services into clinical care delivery, including and not limited to smoking cessation counseling, is not a new concept. Professional organizations are calling for this integration and many, like the American Lung Association, have developed cessation guidance toolkits [60] or process improvement roadmaps like that created by the Centers for Disease Control and Prevention [61] to facilitate this integration. However, while the need for integration is well accepted, how to actually design and implement cessation services into established, functioning clinical workflows is challenged and not well described.
Emerging Implementation Research for Tobacco Cessation Services in Cancer and Lung Cancer Screening
The necessity for a full complement of smoking cessation services in clinical care has become more evident in the past decade. This became particularly apparent when CMS delivered the initial NCD for LCS in 2015 that mandates the provision of smoking cessation services in the LCS process. This positions LCS to model implementation of tobacco cessation services, not only where these services are best offered but what interventions most effectively yield successful cessation. However, a recent systematic review revealed insufficient data to identifying the optimal approach to integrating cessation services in LCS [62].
The National Institutes of Health and National Cancer Institute (NCI) have responded to the need for research in this area that will inform best practices. The NCI’s commitment to developing knowledge is notable in the Cancer Center Cessation Initiative (3CI): NCI Cancer Moonshot Project that has funded over 30 U.S cancer centers to examine how best to integrate cessation services into routine cancer care. The NCI has also dedicated research funding to the Smoking Cessation at Lung Examination: The SCALE Collaboration. This collaboration has funded eight research projects to examine the design and implementation of smoking cessation treatment in the LCS setting. The 3CI and SCALE Collaboration research results are expected soon and anticipated to transform current knowledge and clinical care.
Proposed Models for Integration of Cessation Services in Lung Cancer Screening
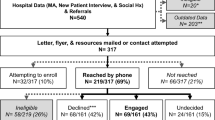
The NCD does not specify where and by whom the cessation services must be provided. Similar to all clinical settings, the operational design and local resources vary across LCS programs. Generally, there are three recognized LCS program models (decentralized, centralized, and hybrid). The decentralized LCS program model (Fig. 9.1) positions the PCP to have sole responsibility for providing the initial and subsequent smoking cessation services. The centralized LCS program (Fig. 9.2) traditionally owns the responsibility for providing smoking cessation services and in the hybrid LCS program (Fig. 9.3), cessation services may be owned by either the PCP or LCS team.
Who is on point to deliver cessation services in any of these LCS program models depends on many conditions. A multidisciplinary approach that calls for the onsite healthcare provider(s) (pulmonologist, oncologist, nurse, advanced practice provider, or other staff) within the screening pathway to deliver collaborative comprehensive smoking cessation services is also an option and may indeed optimize opportunities for successful cessation. In the event that any of the LCS programs do not have access to or embedded smoking cessation services, patients may be referred out for such services. It is important to note that in all LCS program models, integration of cessation services is a continuous loop threaded longitudinally throughout the initial screen and short- and long-term follow-up, whichever comes first.
Critical Components of Tobacco Cessation Services on the Front Lines
The recalcitrant nature of TUD that afflicts so many, including the most under-resourced and vulnerable, calls for an all-hands-on-deck approach to be effective at leading people away from nicotine dependence. The responsibility for addressing and managing TUD cannot fall on any single entity or individual and this must reside with all healthcare providers and staff. The complexity of this disorder demands effective coordination of care that ensures people get the right care at the right time and the appropriate follow-up, to quit tobacco successfully, stay quit, and benefit from sustained cessation.
Clinical care delivery models must be designed with the intention and commitment to tailor tobacco cessation services to each person and their specific needs. Effective tobacco treatment plans will provide a combination of evidence-based, FDA-approved pharmacotherapies and one or more behavioral health modalities proven to yield greater chances of successful cessation. Given the prevalence of TUD in people who experience complex social, educational, and economic inequities or who have mental or behavioral health disorders, active engagement of social, mental, and behavioral health services is a critical component of TUD management.
Finally, there are many examples in healthcare systems where leadership and provider commitment with a well-resourced strategic approach yields high functioning care delivery models and quality outcomes [63, 64]. Well-orchestrated and intentional partnerships between healthcare leaders and providers are critical to the health systems change in TUD and cessation services and are desperately needed to move the needle on the health care costs in human suffering and lives lost.
Leveraging the Electronic Health Record to Support Integration of End-to-End Cessation Services
The ever-evolving and expanding domain of health technology positions the electronic health record (EHR) with immense opportunity to establish, build, integrate, and advance cessation services in health care. The EHR may be leveraged to promote quality health systems change, facilitate the integration of efficient and timely cessation services in healthcare delivery models, and foster patient-centered care and effective clinical outcomes. Tobacco use and cessation data may be elicited from the electronic health records for utilization and quality improvement, review of the provision of cessation services, treatment uptake, program evaluation, clinical outcomes [65], and determination of who is not being reached. The EHR plays a key role in continuity of care through the availability of health record information and healthcare team communication. Finally, the EHR may also be proactively utilized for population health management. The patient portal is instrumental in proactive outreach and communication, patient education, and clinical management of tobacco use and cessation efforts (see Fig. 9.4 for Electronic Health Record Functions).
Leveraging Telehealth to Facilitate Integration of Equitable Access to Care
The global COVID-19 pandemic and resulting public health emergency forced the advancement and utilization of technology to reach patients by telehealth. Extension of clinical services by telehealth through access expansion, cost reduction, and improved quality of care is now more realistic than ever before. Telehealth is positioned to continue to address barriers for marginalized people and connect them to vital and lifesaving services. Continued advocacy for expansion, reimbursement, and aggressive adoption of telehealth services will ensure sustainability of remote healthcare delivery services. Access to clinical care by telehealth is critical for implementing tobacco cessation services for those suffering from tobacco use disorder and healthcare providers who are dedicated to this work.
Making the Economic Business Case for Integrating Tobacco Treatment into Clinical Care
Annual healthcare spending on cigarette smoking-related direct healthcare costs alone is estimated at $227 billion per year in the U.S., with greater than 60% of that spending covered by federally funded public health insurance programs [66]. This spending includes an estimated $8.2 billion on tobacco-related cancer hospitalizations, accounting for 45% of cancer hospitalizations [67]. It is estimated that an additional $156 billion annual expenditure occurs from lost productivity due to illness and death [8].
This smoking-related economic burden representing 7.6–8.7% of all annual US healthcare expenditures [8] demonstrates the pressing need to integrate practical smoking cessation efforts into clinical care delivery models. The median cost for successful cessation is $2688, with a broad range of $330–$9628 [68]. Variation in a patient’s readiness to quit and the modalities and options for care delivery of cessation services exist. This variation in services, modalities of care delivery, and their efficacy make direct comparisons of services and determination of their cost-effectiveness to one another challenging. However, the evidence does show that any intervention is more effective in cessation rates and healthcare cost reduction than no intervention [69, 70]. A Canadian study using simulation modeling (Oncosim) demonstrates a modest but favorable change in healthcare costs by adding just one-time SC interventions in an LCS program [71]. Perhaps more important, healthcare costs drop significantly for people who quit smoking. For people without chronic conditions, healthcare costs are comparable, within 5 years, to those who never smoked, and for people with chronic diseases, healthcare costs are comparable within 10 years of having quit [72]. Cessation services are currently poorly reimbursed, treatment is costly, and healthcare providers are not well rewarded for the investment of time and successfully helping their patients quit. Finally, tobacco-related diseases, human suffering, disability, and loss of life continue to be expensive, unnecessary, and preventable.
Conclusion
Tobacco cessation is never easy, and the journey is never over for people who currently or previously used tobacco products, including cigarette smoking. Anywhere along the care continuum is a perfect place to integrate tobacco cessation services through partnership with patients in patient- and family-centered care on the cessation journey. This work must be adopted and adapted by a broad range of frontline health care providers and staff to understand their positionality and implicit biases that further marginalize people who experience TUD. Commitment to engagement in key partnerships and addressing internal policy and procedures that promote the integration of evidence-based tobacco cessation counseling and treatment and, when appropriate, social, mental, and behavioral health services, is paramount for prioritizing tobacco work with recovery as the end goal. Each patient must be met where they are, on the care continuum, for success and to address tobacco use with every touchpoint.
References
Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341–50. https://doi.org/10.1056/NEJMsa1211128.
American Cancer Society. Cancer prevention & early detection facts & figures 2021–2022. Atlanta, GA: American Cancer Society; 2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-prevention-and-early-detection-facts-and-figures/2021-cancer-prevention-and-early-detection.pdf.
World Health Organization. The top 10 causes of death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed 30 Aug 2021.
Ahmad FB, Anderson RN. The leading causes of death in the US for 2020. JAMA. 2021;325(18):1829–30. https://doi.org/10.1001/jama.2021.5469.
Islami F, Goding Sauer A, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68(1):31–54. https://doi.org/10.3322/caac.21440.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33. https://doi.org/10.3322/caac.21654.
Hecht SS, Szabo E. Fifty years of tobacco carcinogenesis research: from mechanisms to early detection and prevention of lung cancer. Cancer Prev Res (Phila). 2014;7(1):1–8. https://doi.org/10.1158/1940-6207.CAPR-13-0371.
U.S. Department of Health & Human Services. The health consequences of smoking—50 years of progress: a report of the surgeon general 2014. Executive summary. 2014. https://www.hhs.gov/surgeongeneral/reports-and-publications/tobacco/index.html.
American Cancer Society. Cancer facts & figures 2021. Atlanta: American Cancer Society; 2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf.
Pineiro B, Simmons VN, Palmer AM, Correa JB, Brandon TH. Smoking cessation interventions within the context of low-dose computed tomography lung cancer screening: a systematic review. Lung Cancer. 2016;98:91–8. https://doi.org/10.1016/j.lungcan.2016.05.028.
Taylor KL, Cox LS, Zincke N, Mehta L, McGuire C, Gelmann E. Lung cancer screening as a teachable moment for smoking cessation. Lung Cancer. 2007;56(1):125–34. https://doi.org/10.1016/j.lungcan.2006.11.015.
Ostroff JS, Buckshee N, Mancuso CA, Yankelevitz DF, Henschke CI. Smoking cessation following CT screening for early detection of lung cancer. Prev Med. 2001;33(6):613–21. https://doi.org/10.1006/pmed.2001.0935.
Shi Y, Warner DO. Surgery as a teachable moment for smoking cessation. Anesthesiology. 2010;112(1):102–7. https://doi.org/10.1097/ALN.0b013e3181c61cf9.
Bernstein SL, Boudreaux ED, Cabral L, Cydulka RK, Schwegman D, Larkin GL, et al. Nicotine dependence, motivation to quit, and diagnosis among adult emergency department patients who smoke: a national survey. Nicotine Tob Res. 2008;10(8):1277–82. https://doi.org/10.1080/14622200802239272.
Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409. https://doi.org/10.1056/NEJMoa1102873.
Pastorino U, Boffi R, Marchiano A, Sestini S, Munarini E, Calareso G, et al. Stopping smoking reduces mortality in low-dose computed tomography screening participants. J Thorac Oncol. 2016;11(5):693–9. https://doi.org/10.1016/j.jtho.2016.02.011.
Meza R, Cao P, Jeon J, Taylor KL, Mandelblatt JS, Feuer EJ, et al. Impact of joint lung cancer screening and cessation interventions under the new recommendations of the U.S. preventive services task force. J Thorac Oncol. 2022;17(1):160–6. https://doi.org/10.1016/j.jtho.2021.09.011.
Tanner NT, Kanodra NM, Gebregziabher M, Payne E, Halbert CH, Warren GW, et al. The association between smoking abstinence and mortality in the National lung screening trial. Am J Respir Crit Care Med. 2016;193(5):534–41. https://doi.org/10.1164/rccm.201507-1420OC.
Parsons A, Daley A, Begh R, Aveyard P. Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: systematic review of observational studies with meta-analysis. BMJ. 2010;340:b5569. https://doi.org/10.1136/bmj.b5569.
Aredo JV, Luo SJ, Gardner RM, Sanyal N, Choi E, Hickey TP, et al. Tobacco smoking and risk of second primary lung cancer. J Thorac Oncol. 2021;16(6):968–79. https://doi.org/10.1016/j.jtho.2021.02.024.
Warren GW, Alberg AJ, Cummings KM, Dresler C. Smoking cessation after a cancer diagnosis is associated with improved survival. J Thorac Oncol. 2020;15(5):705–8. https://doi.org/10.1016/j.jtho.2020.02.002.
Toll BA, Brandon TH, Gritz ER, Warren GW, Herbst RS, Tobacco ASo, et al. Assessing tobacco use by cancer patients and facilitating cessation: an American Association for Cancer Research policy statement. Clin Cancer Res. 2013;19(8):1941–8. https://doi.org/10.1158/1078-0432.CCR-13-0666.
Department of Health and Human Services. Smoking cessation: a report of the surgeon general. Washington, DC: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2020.
U.S. Department of Health & Human Services. Cardiovascular diseases. How tobacco smoke causes disease: the biology and Behavioral basis for smoking-attributable disease, a report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services; 2010. p. 355–409.
van den Berg MJ, van der Graaf Y, Deckers JW, de Kanter W, Algra A, Kappelle LJ, et al. Smoking cessation and risk of recurrent cardiovascular events and mortality after a first manifestation of arterial disease. Am Heart J. 2019;213:112–22. https://doi.org/10.1016/j.ahj.2019.03.019.
Babb S, Malarcher A, Schauer G, Asman K, Jamal A. Quitting smoking among adults—United States, 2000–2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457–64.
Cornelius M, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco product use among adults—United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(46):1736–42.
Smith PH, Mazure CM, McKee SA. Smoking and mental illness in the U.S. population. Tob Control. 2014;23(e2):e147–53. https://doi.org/10.1136/tobaccocontrol-2013-051466.
Kaiser Family Foundation. Key facts about the unisnured population. 2020. https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population/. Accessed 1 Dec 2021.
Institute of Medicine (U.S.), Committee on Quality of Health Care in America, National Academies Press (U.S.). Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press; 2001.
Ellis C, Jacobs M, Kendall D. The impact of racism, power, privilege, and positionality on communication sciences and disorders research: time to reconceptualize and seek a pathway to equity. Am J Speech Lang Pathol. 2021;30(5):2032–9. https://doi.org/10.1044/2021_AJSLP-20-00346.
FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19. https://doi.org/10.1186/s12910-017-0179-8.
Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):e60–76. https://doi.org/10.2105/AJPH.2015.302903.
Volkow ND. Stigma and the toll of addiction. N Engl J Med. 2020;382(14):1289–90. https://doi.org/10.1056/NEJMp1917360.
Hamann HA, Ostroff JS, Marks EG, Gerber DE, Schiller JH, Lee SJ. Stigma among patients with lung cancer: a patient-reported measurement model. Psychooncology. 2014;23(1):81–92. https://doi.org/10.1002/pon.3371.
Rigney M, Rapsomaniki E, Carter-Harris L, King JC. A 10-year cross-sectional analysis of public, oncologist, and patient attitudes about lung cancer and associated stigma. J Thorac Oncol. 2021;16(1):151–5. https://doi.org/10.1016/j.jtho.2020.09.011.
Carter-Harris L. Lung cancer stigma as a barrier to medical help-seeking behavior: practice implications. J Am Assoc Nurse Pract. 2015;27(5):240–5. https://doi.org/10.1002/2327-6924.12227.
Chambers SK, Dunn J, Occhipinti S, Hughes S, Baade P, Sinclair S, et al. A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BMC Cancer. 2012;12:184. https://doi.org/10.1186/1471-2407-12-184.
Banerjee SC, Haque N, Schofield EA, Williamson TJ, Martin CM, Bylund CL, et al. Oncology care provider training in empathic communication skills to reduce lung cancer stigma. Chest. 2021;159(5):2040–9. https://doi.org/10.1016/j.chest.2020.11.024.
Johnson B, Abraham M, Conway J, Simmons L, Edgman-Levitan S, Sodomka P, Schlucter J, Ford D. Partnering with patients and families to design a patient-and family-centered health care system. Bethesda, MD: Institue for Patient-and Family-Centered Care and Institute for Healthcare Improvement; 2008. https://www.ipfcc.org/resources/PartneringwithPatientsandFamilies.pdf.
Henschke CI, McCauley DI, Yankelevitz DF, Naidich DP, McGuinness G, Miettinen OS, et al. Early lung cancer action project: overall design and findings from baseline screening. Lancet. 1999;354(9173):99–105. https://doi.org/10.1016/S0140-6736(99)06093-6.
de Koning HJ, van der Aalst CM, de Jong PA, Scholten ET, Nackaerts K, Heuvelmans MA, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med. 2020;382(6):503–13. https://doi.org/10.1056/NEJMoa1911793.
Force USPST, Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, et al. Screening for lung cancer: US preventive services task force recommendation statement. JAMA. 2021;325(10):962–70. https://doi.org/10.1001/jama.2021.1117.
Landy R, Young CD, Skarzynski M, Cheung LC, Berg CD, Rivera MP, et al. Using prediction-models to reduce persistent racial/ethnic disparities in draft 2020 USPSTF lung-cancer screening guidelines. J Natl Cancer Inst. 2021;113(11):1590–4. https://doi.org/10.1093/jnci/djaa211.
Villanti AC, Jiang Y, Abrams DB, Pyenson BS. A cost-utility analysis of lung cancer screening and the additional benefits of incorporating smoking cessation interventions. PLoS One. 2013;8(8):e71379. https://doi.org/10.1371/journal.pone.0071379.
Centers for Medicare and Medicaid Services. Decision memo for screening for lung cancer with low dose computed tomography (LDCT) (CAG-00439N). 2015. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=274. Accessed 1 May 2021.
Centers for Medicare & Medicaid Services. Screening for lung cancer with low dose computed tomography. 2022. https://www.cms.gov/medicare-coverage-database/view/ncacal-decision-memo.aspx?proposed=Y&ncaid=304&#:~:text=In%202021%2C%20the%20most%20recent,within%20the%20past%2015%20years. Accessed 6 Feb 2022.
Park E, Aronson MD, Kathuria H, Kunins L. Behavioral approaches to smoking cessation. Waltham: UpToDate; 2020.
Stead L, Koilipillai P, Fanshawe T, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database Syst Rev. 2016;3:CD008286.
Patnode CD, Henderson JT, Coppola EL, Melnikow J, Durbin S, Thomas RG. Interventions for tobacco cessation in adults, including pregnant persons: updated evidence report and systematic review for the US preventive services task force. JAMA. 2021;325(3):280–98. https://doi.org/10.1001/jama.2020.23541.
Anthenelli RM, Benowitz NL, West R, St Aubin L, McRae T, Lawrence D, et al. Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. Lancet. 2016;387(10037):2507–20. https://doi.org/10.1016/S0140-6736(16)30272-0.
Benowitz NL, Pipe A, West R, Hays JT, Tonstad S, McRae T, et al. Cardiovascular safety of varenicline, bupropion, and nicotine patch in smokers: a randomized clinical trial. JAMA Intern Med. 2018;178(5):622–31. https://doi.org/10.1001/jamainternmed.2018.0397.
United States Preventive Services Task Force. Tobacco smoking cessation in adults, including pregnant persons: interventions. 2021. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions. Accessed 1 Nov 2021.
Creamer MR, Wang TW, Babb S, Cullen KA, Day H, Willis G, et al. Tobacco product use and cessation indicators among adults—United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(45):1013–9. https://doi.org/10.15585/mmwr.mm6845a2.
Quaife SL, Ruparel M, Dickson JL, Beeken RJ, McEwen A, Baldwin DR, et al. Lung screen uptake trial (LSUT): randomized controlled clinical trial testing targeted invitation materials. Am J Respir Crit Care Med. 2020;201(8):965–75. https://doi.org/10.1164/rccm.201905-0946OC.
Borsari L, Storani S, Malagoli C, Filippini T, Tamelli M, Malavolti M, et al. Impact of referral sources and waiting times on the failure to quit smoking: one-year follow-up of an Italian cohort admitted to a smoking cessation service. Int J Environ Res Public Health. 2018;15(6):1234. https://doi.org/10.3390/ijerph15061234.
Cabrita BMO, Galego MA, Fernandes AL, Dias S, Correia S, Simao P, et al. Follow-up loss in smoking cessation consultation: can we predict and prevent it? J Thorac Dis. 2021;13(4):2331–8. https://doi.org/10.21037/jtd-20-1832.
Carson K, Verbiest ME, Crone MR, Brin MP, Esterman AJ, Assendelft WJ, Smith BJ. Training health professionals in smoking cessation. Cochrane Database Syst Rev. 2012;16(5):CD000214. Accessed 1 Dec 2021.
Duffy SA, Ronis DL, Ewing LA, Waltje AH, Hall SV, Thomas PL, et al. Implementation of the tobacco tactics intervention versus usual care in trinity health community hospitals. Implement Sci. 2016;11(1):147. https://doi.org/10.1186/s13012-016-0511-6.
American Lung Association. Affordable care act tobacco cessation guidance toolkit. 2022. https://www.lung.org/policy-advocacy/healthcare-lung-disease/healthcare-policy/affordable-care-act-tobacco. Accessed 2 Dec 2021.
Centers for Disease Control and Prevention. Tobacco cessation change package. 2020. https://millionhearts.hhs.gov/tools-protocols/action-guides/tobacco-change-package/index.html.
Laccarino JM, Duran C, Slatore CG, Wiener RS, Kathuria H. Combining smoking cessation interventions with LDCT lung cancer screening: a systematic review. Prev Med. 2019;121:24–32. https://doi.org/10.1016/j.ypmed.2019.02.016.
Curry SJ, Keller PA, Orleans CT, Fiore MC. The role of health care systems in increased tobacco cessation. Annu Rev Public Health. 2008;29:411–28. https://doi.org/10.1146/annurev.publhealth.29.020907.090934.
Sarna L, Fiore MC, Schroeder SA. Tobacco dependence treatment is critical to excellence in health care. JAMA Intern Med. 2020;180(11):1413–4. https://doi.org/10.1001/jamainternmed.2020.3972.
Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Best practices for comprehensive tobacco control programs. Atlanta: U.S. Department of Health and Human Services; 2014.
Xu X, Shrestha SS, Trivers KF, Neff L, Armour BS, King BA. U.S. healthcare spending attributable to cigarette smoking in 2014. Prev Med. 2021;150:106529. https://doi.org/10.1016/j.ypmed.2021.106529.
Tai EW, Guy GP Jr, Steele CB, Henley SJ, Gallaway MS, Richardson LC. Cost of tobacco-related cancer hospitalizations in the U.S., 2014. Am J Prev Med. 2018;54(4):591–5. https://doi.org/10.1016/j.amepre.2017.12.004.
Salloum RG, D'Angelo H, Theis RP, Rolland B, Hohl S, Pauk D, et al. Mixed-methods economic evaluation of the implementation of tobacco treatment programs in National Cancer Institute-designated cancer centers. Implement Sci Commun. 2021;2(1):41. https://doi.org/10.1186/s43058-021-00144-7.
Ekpu VU, Brown AK. The economic impact of smoking and of reducing smoking prevalence: review of evidence. Tob Use Insights. 2015;8:1–35. https://doi.org/10.4137/TUI.S15628.
Kahende JW, Loomis BR, Adhikari B, Marshall L. A review of economic evaluations of tobacco control programs. Int J Environ Res Public Health. 2009;6(1):51–68. https://doi.org/10.3390/ijerph6010051.
Goffin JR, Flanagan WM, Miller AB, Fitzgerald NR, Memon S, Wolfson MC, et al. Biennial lung cancer screening in Canada with smoking cessation-outcomes and cost-effectiveness. Lung Cancer. 2016;101:98–103. https://doi.org/10.1016/j.lungcan.2016.09.013.
Musich S, Faruzzi SD, Lu C, McDonald T, Hirschland D, Edington DW. Pattern of medical charges after quitting smoking among those with and without arthritis, allergies, or back pain. Am J Health Promot. 2003;18(2):133–42. https://doi.org/10.4278/0890-1171-18.2.133.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fathi, J.T. (2023). Integration of Tobacco Dependence Treatment in Lung Cancer Screening and Other Ambulatory Care Settings. In: Eakin, M.N., Kathuria, H. (eds) Tobacco Dependence. Respiratory Medicine. Humana, Cham. https://doi.org/10.1007/978-3-031-24914-3_9
Download citation
DOI: https://doi.org/10.1007/978-3-031-24914-3_9
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-031-24913-6
Online ISBN: 978-3-031-24914-3
eBook Packages: MedicineMedicine (R0)