Abstract
Central nervous system vasculature (venous and arterial blood) and the cerebrospinal fluid dynamics are predominant systems which are hugely affected during spaceflight by many factors such as radiation and microgravity. Therefore, the human body should adapt by various mechanisms in such an environment. In this chapter, we will highlight the normal physiology and dynamics of cardiovascular system on Earth and how the body adapt in the long- and short-term space flights, in addition to the importance of these adaptations to the central nervous system and discuss common syndromes such as space adaptation syndrome and visual impairment intracranial pressure (VIIP) syndrome that may affect the mission quality, and effective countermeasures to mitigate these effects such as artificial gravity and lower body negative pressure (LBNP).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Central nervous system
- Space adaptation syndrome
- VIIP syndrome
- Artificial gravity (AG)
- Lower body negative pressure (LBNP)
- Cardiovascular system
- Fluid shifts
The Cardiovascular System on Earth and in Space
General Concepts of the Circulatory System on Earth and in Space
Supplying whole cells with essential nutrients such as oxygen to maintain the different cells and tissue compartments is an important role of the cardiovascular system (CVS). Oxygen diffuses from the lungs via the CVS to the brain and all tissues of the body. Hormones are also distributed in the body by blood flow. During rest, approximately 5 l/min of blood is pumped through the vascular system. Blood is pumped from the left ventricle into the arteries which feed the whole body. On average a person spends 70% of his or her day in an upright position. The pressure difference from the level of the heart to the feet is 100 mmHg during standing (Fig. 2.1). Consequently, the blood tissue fluid distributions are affected by gravity [1]. The body needs the heart’s “pump” to push enough arterial blood upward to the head to overcome gravity. It also needs other mechanisms in the veins and arteries of the lower body to prevent pooling or retrograde flow of blood in the direction of the gravitational force. Moreover, any changes in the body position will affect the hydrostatic pressure gradient induced by gravity. For instance, if one changes position from a supine to an upright posture, temporal dizziness or pre-syncope may be produced. This is because of a sudden, temporal decrease in blood pressure in the head and upper parts which is rapidly compensated by the baroreceptor reflex and myogenic mechanisms. The baroreceptor reflex is an effective way to regulate heart activity and vascular peripheral resistance, keeping the arterial blood pressure within a normal range all the time [2].
Fluid shift; preflight (left) the lower extremities are easily supplied by blood due to the work of gravity. Early in-flight the blood begins to shift from the lower extremities to the upper body causing “puffy face” [Reproduced with permission from Hargens et al., 2009] [8]
The goal of this chapter is to understand CVS mechanisms of adaptation to space and the importance of these adaptations to the central nervous system. During human spaceflight, the force of gravity is lost [2] so the blood redistributes from the lower extremes to the thorax and brain, thus producing a puffy face and swollen jugular veins, unweighting of skin and internal organs [3], and increasing intracranial and vestibular pressures generated by the headward shift of body fluids [2]. Moreover, the heart is affected during spaceflight and may be prone to arrhythmias or alterations in the normal sequence of the electrical impulses responsible for atrial and ventricular contraction [4]. Common arrhythmias involve atrial or ventricular fibrillation (disorganized regional depolarization), bradycardia (slower than normal heart rate), tachycardia (faster than normal heart rate), premature contraction, and other conduction problems [5]. Arrhythmias make the heart pump less efficiently, increasing the risk of sudden cardiac arrest, stroke, cardiovascular diseases, and dementia [6].
Seventy-five arrhythmias and 23 conduction disorders were recorded by the Russian Federation to NASA, including a 14-beat episodes of ventricular tachycardia with a maximum frequency of 215 bpm [7]. Electrolyte disruptions, abnormalities in the autonomic nervous system, and alterations in the mass of the cardiac chambers may be causative factors for these cases, but the exact mechanism remains unknown. Moreover, these risks increase during long-term spaceflight [6].
Basic Concepts of Blood–Brain Barrier
The CNS is vascularized by capillaries which are highly impermeable, called the blood–brain barrier (BBB). These capillaries are essential for providing oxygen and nutrients and for the elimination of carbon dioxide and waste products from neural tissues. The BBB allows the CNS to manage the movement of different ions, molecules, and cells between the blood and neural tissues. This barrier is essential to preserve brain homeostasis for normal neural activity in the CNS and also saves the tissue from diseases related to BBB dysfunction which may occur during space missions [9, 10].
The BBB exists in all brain regions except at circumventricular organs [10]. A physical paracellular barrier is formed by tight junctions (TJs) between brain endothelial cells (BECs) [11]. TJs consist of claudins, occludin, and zona occludens and seal the paracellular path between BECs creating a high trans-endothelial cell electrical resistance (TEER) barrier impeding the harmful substances from crossing the BBB [12, 13]. Those tight junctions are polarized into luminal (blood-facing) and abluminal (brain-facing) plasma membrane domains. The TJs are linked with adherens junctions (AJs), which sit abluminal to tight junctions and consist of VE-cadherin dimers that facilitate cell to cell membrane adhesion and bind to the actin cytoskeleton through catenins [14]. In addition, TJs induce a high TEER and reduce paracellular diffusion to a greater extent than AJs. Additionally, there are astrocytes which are highly branched cells with small bodies found in white matter (fibrous astrocytes) and gray matter (protoplasmic astrocytes), their podocytes not only encircle nerve fibers and neuronal somas (respectively) but also surround the abluminal surface of the capillaries. Then, the processes are called perivascular end-feet [10].
BECs lack fenestra and express low levels of transcytosis producing a transcellular barrier to the dissolved hydrophilic molecules [13]. These paracellular and transcellular barriers help to transfer molecules between the blood and the brain by special transporters. Commonly, these transporters fall into two groups. First, efflux transporters, such as Pgp and BCRP, are represented on the luminal membrane and use the energy (from ATP hydrolysis) to efflux small hydrophobic molecules toward their blood concentration gradients, thus providing a barrier to many small non-polar molecules that could passively diffuse via the cell membrane [15]. Second, BECs have nutrient transporter which pass substrates (such as Glut-1/glucose, Lat-1/amino acids) down their concentration gradients into the brain, supporting the neural tissue with important nutrients [9, 15]. BECs also represent low rates of leucocyte adhesion molecules (LAMs), thus reducing CNS immune surveillance by blocking the binding of immune cells to BECs and their movement to the CNS (Fig. 2.2) [16]. BECs also have unique metabolic properties such as “metabolizing molecules” that change their capacity to diffuse or be transported [17]. A high concentration of mitochondria is found in BECs relative to peripheral endothelial cells (PECs) in order to satisfy the energetic demand for BBB.
The neurovascular unit (NVU). (a) The NVU defines all the components that communicate at the interface between the blood and the CNS. ECs (blue) create the blood vessel walls and interact with pericytes (green) in the vascular abluminal surface, together are en-sheathed by astrocyte processes (orange). Neurons (light red) and microglia (purple) interact with the vasculature to form the NVU. (b) The TJs consist of transmembrane proteins such as claudins [5, 12], occludin, and junction adhesion molecules (JAMs). Adherens junctions and TJs are attached to the actin cytoskeleton by ZO-1, -2, and -3. (c) Low rates of vesicular transport limit transcellular movement of nonspecific molecules from the blood to the brain. ECs express a variety of transporters, both to efflux potential toxins (Pgp, BCRP, MRPs) and to deliver specific nutrients to the brain (glut-1/glucose; lat-1/amino acids; Mct-1/lactate) [Reproduced with permission from Elsevier] [9]
There is a similar membrane barrier that serves as an interface between blood and cerebrospinal fluid, called the blood–cerebrospinal fluid barrier. It is similar to the blood–brain barrier in the following: endothelial cells in the capillary beds, circumferential basement membrane across the abluminal domain, and astrocytes on the abluminal surface (perivascular end-feet) in the capillaries [18]. But, unlike the BBB, it has fenestrated endothelial cells(ECs) which is relatively leaky and more permeable to water, gases, and lipophilic substances from the blood to the CSF [19]. In addition, there are choroidal epithelial cells which produce cerebrospinal fluid. So if the brain is dehydrated, the CSF becomes a source of fluid to rehydrate it [20].
Adaptations to Microgravity
The differentiation between the fluid transition itself and the response to this shift provides two timeframes for physiological alteration. First, the immediate changes produced by the absence of the gravitational force are indicated as acute adaptations in the following section. Second, the consequent adaptations to these changes will be defined as long-term adaptations below [1].
Acute Adaptations and Microgravity-Induced Fluid Shift
The impact of spaceflight begins several hours before the liftoff when the astronauts are in their position in the shuttle, lying on their backs with a 90-degree hip and knee flexion (see Fig. 2.3). This supine position stopped the blood from pooling into the legs during the ascent, which may lead to syncope in serious situations, and also indicate what will happen in microgravity of moving the blood from the lower parts to the head and upper parts of the body. About two-thirds of space crew members report headache, malaise, lethargy, anorexia, nausea, vomiting, and gastric pain within the first few hours or days of spaceflight [21]. In addition, loss of hydrostatic pressures increases intraocular pressure (IOP) and induces facial edema “puffy face” and distension of temporal, forehead, and neck veins, resulting in cephalad fluid shift [8].
After entering weightlessness, astronauts suddenly feel the fluid pooling within seconds without depending on visual or physiological indicators. All the symptoms are noticed visually without physical measurements and are complete within the first 6–10 h of flight [1, 22]. The higher concentrations of fluid in the upper body are experienced through a feeling of fullness in the head and discomfort in the sinuses and eyeballs, the same as felt in nasal congestion during a cold. Smell and taste diminished as they used to during flu, and non-verbal contact between subjects may happen as facial expression is impaired [1]. The change in the thickness of superficial tissues can be assessed to determine the apparent fluid change [23]. Consequently, the thickness in the forehead increased by 7%, reflecting an increase in fluid volume of around 2 L in the upper body [11]. In the first 4 days in space, the leg circumference falls by up to 30% to the degree that remains quite low for the rest of the mission and may include “chicken-leg syndrome” 1.5 years later [10, 12].
Interestingly, heat transmission is also affected by fluid shifts. As convective and evaporative heat loss reduces in weightlessness, radiative heat loss in space becomes much more significant than on earth. In space, more than 30% of the heat exchange between the body and the atmosphere happens at the head and neck because of increasing the blood volume in this part of the body [24].
Long-Term Adaptations
Upon the sudden decrease of gravity in space [2], the cardiovascular system develops primary reactions to deal with the short-term rise in thoracic length or spinal curvature. This rapid response involves a reduction in the heart rate, as well as a dilation of the lower limb arterioles to reduce peripheral resistance, hence decreasing mean blood pressure [1].
After that, arranging a new set-point is a way for the cardiovascular system to adapt to the long-term stimuli. Due to the high blood filling of the thorax, the body become overloaded with fluid, inducing a reduction in the blood volume. This is an acceptable way to adapt to microgravity, but results in a fluid volume that is considered hypovolemic condition on Earth [25]. It is indicated by the reduction in stroke volume and plasma-atrial natriuretic peptide (ANP) levels [26]. The mechanism of volume reduction involves stretch receptors in the intrathoracic vessels and heart [27]. Higher amounts of fluid in the thorax cause greater filling of blood vessels, which activates the stretch receptors that activates baroreflexes, resulting in suppression of the renin–angiotensin–aldosterone pathway, and produces ANP [28]. Together, these processes decrease the blood plasma volume of approximately 10%–15% [29]. In addition, the reduction in plasma volume does not arise from elevated diuresis or natriuresis, but rather likely from decreased interstitial pressure in lower body and increased vascular pressure in the upper body, both which facilitate transcapillary fluid flow through the interstitial upper body [30] (Fig. 2.4). In addition, reduced plasma volume increases the concentration of circulating red blood cells (RBCs), which in turn allows the body to destroy newly released RBCs to preserve the homeostatic equilibrium [31]. Moreover, long-duration spaceflight probably decreases both systolic and mean arterial pressures, giving rise to a 10% rise in carotid diameter and cardiac output [6].
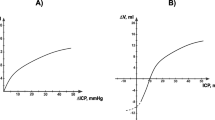
Changed capillary transmural pressure (blood to tissue) due to weightlessness. The arterial pressure (Pa), venous pressure (Pv), transmural pressure (Pt), and interstitial fluid to lymph pressure gradient (Pil) are shown, with larger arrows indicating greater pressure gradients. 1-G conditions represent relative values on Earth. In microgravity, the loss of tissue weight reduces tissue hydrostatic pressure, therefore inducing higher transmural pressure which can cause edema. Lymph flow depends mainly on tissue deformation and local hydrostatic gradients but may be reduced in space. Arterial flow depends on the input arterial pressure Pa. Capillary hydrostatic pressures are regulated by pre-capillary sphincter activity and myogenic responses [Reproduced with permission from Hargens et al., 2009] [8]
Long-term adaptations include the challenges facing the body upon return to Earth [32]. The effects of sustained exposure to microgravity and adaptation of the cardiovascular system to loss of gravitational stimulus are starting to appear [33]. The issues include dizziness, sweating, pre-syncope, decreasing blood flow to central nervous system, and, above all, orthostatic intolerance. This condition is characterized by elevated heart rate and decreased systolic pressure and may lead to faint due to hypovolemia [34]. Hypovolemia of the cardiovascular system significantly decreases exercise capacity experienced by returning astronauts and decreases VO2max (maximum amount of oxygen that can be used—the standard indicator for exercise capacity) which is a consequence of decreased intravascular blood volume and reduced stroke volume and cardiac output [35]. Of note, long-term spaceflight has led to cardiac remodeling, in other words, atrophy. Moreover, decreasing mass and size of the left ventricle have also been confirmed post-flight [36].
Circulation and the Central Nervous System
Endothelial Dysfunction
Endothelial cells are a major factor maintaining vascular integrity, angiogenesis, and many homeostatic functions in the body. Moreover, ECs improve secretive, synthetic, metabolic, and immunological activity. The endothelium of the CNS vasculature plays a vital role in the maintenance of normal CNS function. In the brain, spinal cord, and peripheral nerves, the blood vessels are distinguished by endothelial tight junctions that maintain a restrictive blood–brain barrier. This advanced adaptation ensures the adequate ion and water balance required for normal neuronal transmission inside the CNS [37]. In addition, the endothelium releases antithrombotic and fibrinolytic factors to prevent the blood from the formation of thrombi and emboli. ECs also help form new blood vessels (angiogenesis) as protagonists molecules, leading to functional capillaries. Finally, ECs efficiently regulate vasomotor reactions through the synthesis and metabolism of vasoactive molecules acting on smooth muscle cells such as endothelin-1 (ET-1), nitric oxide (NO), and angiotensin II (AngII). They also regulate the proliferation of smooth muscle cells [38,39,40].
Arterial vessels differ from venous vessels in terms of the structure and function of their ECs in micro- and macro-blood vessels. Moreover, the endothelium of the cerebral circulation, the major component of the BBB to protect the brain from harmful substances, deserves special emphasis. The BBB has uniformly tight junctions and differs from both fenestrated endothelium as cells have pores and discontinuous endothelium where cells have intracellular and transcellular discontinuities [38].
Endothelial dysfunction is sometimes caused by altered activity of the endothelium by decreased vasodilation, pro-inflammatory state, and prothrombic processes. It is associated with many causes of cardiovascular diseases, such as hypertension, coronary artery disease, chronic heart failure, peripheral vascular disease, diabetes, and chronic kidney failure. Mechanisms that engage in decreased vasodilatory responses involve reduced production of nitric oxide, oxidative overload, and reduced development of hyperpolarizing agents [41].
Endothelial dysfunction sometimes occurs from disturbances in the balance of pro-oxidant and anti-oxidant amounts due to lack of physical activity such as with spaceflight [42]. Reduced daily exercise in space is also associated with the incidence of insulin resistance, which is closely associated with endothelial dysfunction in individuals with diabetes [43]. Endothelial dysfunction is evident in animals exposed to high-energy ionizing radiation. Dysfunction of ECs is sustained for 2 weeks to 6 months after radiation exposure [44]. Whether endothelial dysfunction associates with radiation exposure in spaceflight is not well understood, but there appears some evidence that radiation and microgravity exposures may elicit more damage to ECs [45].
As mentioned above, proper brain activity relies on an intact BBB. For example, despite its small mass, the brain consumes about 20% of the oxygen intake through the body [46]. There is evidence that the brain vasculature is destroyed by high-dose low-LET radiation during space missions [47]: vascular lesions are common in areas of radiation necrosis in irradiated humans and non-human primates [48, 49]. Rodent studies also demonstrate strong consequences of low LET radiation. For example, a cranial X-ray dose of 9 Gy contributed to a decrease in hippocampal micro-vessel volumes at 2 days, which lasted to 1 month after exposure to 8-month-old male mice. Similar results were also recorded in rats 1 month after 10 Gy of cranial irradiation [50,51,52].
Previous ground-based research has shown that simulated microgravity and ionizing radiation triggered chronic endothelial dysfunction and BBB disturbance leading to maladaptive tissue remodeling [9]. Ionizing radiation is an important endogenous factor in inducing neuroinflammation, by causing a cellular damage in the brain [53]. This figure illustrates the role of inflammatory and immune reactions in the presence of radiation-induced cognitive deficits (see Fig. 2.5). In vitro models also showed that changes in BBB integrity were observed after much lower doses (4 Gy). These changes were long-lasting and followed by increased permeability for low- and high-molecular-weight proteins [53]. Morphologically, an endothelial layer rarefaction was seen, which could open the endothelial tight junctions, despite the reality that no gross changes were detected in the immuno-labeling of the tight junction protein panel (ZO-1, claudin-5, and occludin) [54]. Thus, all these processes induce endothelial dysfunction and BBB disturbances.
In the healthy brain (left part), neurons secrete CD47, CD55, CD20, and CX3CL1, which maintain adjacent microglial cells. In the irradiated brain (right part), neurons secrete pro-inflammatory cytokines, which activate microglia (a). In microglia, radiation-induced DNA damage through the NFKB pathway activates microglia (MHC, CD68 upregulation) and secretes pro-inflammatory cytokines (a). Damaged neurons secrete high-mobility group protein 1 (HMGB1) extracellular, which is a ligand for TLR4. Damaged neurons also express calreticulin, sensed by activated microglia and induces phagocytosis of damaged and healthy neurons (b). Irradiation increases the secretion of CCL2 that is a chemoattractant for CCR2-expressing peripheral macrophages, which penetrate the BBB (c). Radiation increases intercellular adhesion molecule 1 (ICAM-1) and P-selectin on brain microvascular ECs. Peripheral lymphocytes and monocytes adhere to these ECs and transmigrate through the micro-vessel wall (d). Pro-inflammatory signals and HMGB1 activate brain-residing dendritic cells, which migrate to regional lymph nodes and induce immune reactions (e) [licensed under CC BY 4.0] [54]
Despite these data, there is a relative lack of research on low-dose or high-LET radiation on brain vascular effects [49]. Interestingly, using a 3D human brain microvascular endothelial cell culture model, 1 Gy Fe and protons (both at 1000 MeV/n) affect vascular synthesis and proliferation, suggesting that regeneration of injured vessels may be impeded after radiation exposure [55].
Total peripheral vascular resistance decreased during spaceflight [26], although there is evidence of increased sympathetic nervous activity by increased catecholamine levels, which could trigger arterial stiffness [56]. As noted above, amounts of the renin–angiotensin–aldosterone hormones increase during spaceflight [43]. Angiotensin II and aldosterone are strongly involved in mechanisms that increase arterial stiffness by endothelial dysfunction, activation of collagen production, remodeling and hypertrophy of matrixes, and proliferation of smooth muscle vascular endothelial cells [57]. In addition, higher insulin resistance may increase glycation end products, including cross-bridge formation in the extracellular vascular matrix, adversely affecting arterial structure and function [58].
Importantly, endothelial gap junctions are kept locked by the combined pressure of the interstitial fluid in the brain and intracranial capillary pressure. A study has suggested that during 1-G the hydrostatic pressure is transferred from the brain to the capillaries, leading to raise the pressure required to close endothelial cell junctions. Thus the brain cannot contribute its weight to keep the balance of the pressure during spaceflight, causing capillary filtration into the interstitial fluid [59]. The brain is surrounded by a cranial vault, so its compliance is very low. As a result of the inability of these tissues to quickly extend their interstitial volume, comparatively minor increases of transcapillary fluid filtration cause large increases in interstitial fluid pressure. This, in particular, decreases the gradient of transmural vascular pressure and physically compresses capillaries, therefore limiting the perfusion of nutrient tissue due to cerebral edema [60].
CSF Hydrodynamics and Brain and Neck Venous Congestion
CSF Hydrodynamics Circulation on Earth and in Space
Cerebrospinal fluid (CSF) is secreted from choroid plexuses of ventricles (90% by lateral ventricle), a little amount is formed around cerebral vessels and from ependyma cells lining the ventricles [61]. The CSF circulates around the brain and spinal cord [62]. Its main role is to protect the brain against trauma acting as “water jacket” around it; it also keeps the volume of fluid inside skull constant and therefore maintains a constant intracranial pressure [63] (Fig. 2.6).
The traditional circulation of CSF begins from lateral ventricles and flows toward third ventricle >> fourth ventricle >> subarachnoid space. From here it flows around brain or around spinal cord. Then it drains into the arachnoid projections, especially into the superior sagitta sinus [63] [licensed under CC BY 4.0]
During long-term spaceflight, the volume of CSF spaces increase, including the subarachnoid space, causing visual impairment and eye-structural changes [64]. Van Ombergen et al. indicated in an MRI study that there is loss of brain white and gray matter volumes and changed volumes of CSF spaces. Cosmonauts’ MRI data was collected preflight, postflight, and at follow-up for 7 months after returning to Earth. The results showed a significant difference between preflight and postflight values for all supratentorial ventricular spaces, ventricular CSF volume was increased after spaceflight in supratentorial ventricular structures (i.e., lateral and the third ventricles), while the infratentorial fourth ventricle was not significantly enlarged. The superior sagittal sinus and Pachioni’s granulations (responsible for the most of CSF resorption) were compressed due to the upward fluid shifting [11], leading to a generally reduced CSF resorption [65]. Interestingly, these changes are sustained as long as 7 months after spaceflight [65].
Another study proved that changes in thoracic and abdominal cavity pressures are dominant regulators of CSF dynamics [66]. During Forced inspiration, the CSF is shifted toward head and brain ventricles against the hydrostatic pressure, while the venous outflow is shifted from the brain and cranial cavity toward the heart and therefore counterbalance the CSF upward. Both the fluid systems are in balance to keep the intracranial volume constant [67]. In contrast, during deep expiration CSF moves toward the spinal lumbar region, facilitated by hydrostatic forces [66]. Microgravity and hydrostatic pressures are affecting these downward systems, so the net result is shifting the CSF upward and widening the intracerebral CSF spaces. Forced deep expiration can be a way to mitigate the changes made by microgravity [68].
Increased ICP and ventricular volumes leads to a compression of cerebral blood vessels and enhances vascular resistance, causing a reduction of cerebral blood flow [69]. The fluid shift may cause a clinical syndrome called visual impairment intracranial pressure (VIIP) syndrome or spaceflight-associated neuro-ocular syndrome (SANS) [70]. It was indicated that VIIP or SANS is associated with choroidal folds, optic disk edema, hyperopic visual shift, and a risk of permanent visual acuity changes (discussed in section “CSF Hydrodynamics and Brain and Neck Venous Congestion”) [21].
Brain and Neck Venous Congestion
There are many factors that contribute to the elevation of intracranial pressure, including microgravity and changes in intrathoracic and abdominal cavity pressures (as mentioned in Section “Adaptations to Microgravity”). Inhibiting venous drainage from the skull is also a leading cause for ICP elevation. This may be a result of cephalad fluid shift in microgravity or increasing central venous pressure (CVP) [71], which may reduce the CSF and lymphatic drainage from the cranial cavity [72].
IJV cross-sectional area and flow are influenced by both cardiac and respiratory cycles and are affected by posture, anatomical differences, jugular valve incompetence, and changes in central venous pressure. On Earth, during standing position, venous pressure is affected by venous hydrostatic pressure and the IJVs act as a protective system that stops extreme negative ICP during collapsing (Starling resistors). Previous study showed that normal IJV blood flow changes during spaceflight. Pressure in the IJV increased during brief periods of weightlessness in parabolic flight [72]. It was observed that the IJV pressure remained elevated in the ISS during long-term spaceflight. This finding was supported by previously measured increases in ICP and central venous pressure during exposure to microgravity and cephalic fluid shifts [73].
During microgravity, astronauts are exposed to constant cerebral venous congestion with the ability to develop stagnant venous blood flow. Virchow triad identifies three main factors that lead to thrombosis: flow stasis, hypercoagulability, and endothelial injury or dysfunction. Blood flow stasis induces many thrombotic factors such as local hemostasis-activation factors and blood cell–endothelium interaction and creates local hypoxia-induced endothelial activation [74]. So the constant stagnation of blood flow in the IJV increases risk for thrombosis during weightlessness. Although during astronaut selection process, extensive medical screenings are performed to ensure they are healthy individuals. Notably, oral contraceptives are considered a risk for thrombosis during space missions. Estrogen-containing contraceptives are commonly used in human spaceflight for menstrual suppression [75]. The combination of oral contraceptives and weightlessness-induced blood flow stasis in the IJV during spaceflight leads to increased risk thrombosis formation [76].
Space Adaptation Syndrome (SMS)
Space motion sickness (SMS) occurs in 67% of the astronauts. Two hypotheses can explain SMS: the sensory conflict hypothesis and the most potential, fluid shift hypothesis [77]. The symptoms of SMS include headache, pallor, malaise, loss of appetite, nausea, vomiting, and loss of peripheral vision. The fluid shifting also causes cerebral and visible facial edema due to the filtration of fluid into tissues [71, 78] and may increase the ICP, the cerebrospinal fluid pressure, or the inner ear fluid pressures, affecting the functional properties of the vestibular receptors [77]. SMS leads to reduced astronaut performance, reduces situational awareness, and threatens the safety of the crew members [79].
Visual Impairment Intracranial Pressure Syndrome
Spaceflight affects the visual acuity negatively especially during long-term missions. It has been reported by Mader et al. [80] that the crew members after 6 months on the ISS had anatomical ophthalmic alterations such as optic disk edema, posterior globe flattening, choroidal folds, cotton wool spots, thickening of retinal nerve fiber layer (RNFL), and reduced near vision and hyperopic shifts. Unfortunately, some vision alterations persist for years after the space flights, although the relation between severity and duration mission remains unclear [21]. To date, 15 long-term male astronauts have been diagnosed with inflight and postflight visual acuity alterations and vision anatomical disorders [81].
Many hypotheses explain the VIIP pathogenesis. For instance, if subarachnoid pressure moves from the intracranial to the intraocular compartment through the peri optic subarachnoid space, it can lead to optic nerve sheath distension and disk edema [80, 81]. The chronic and mild increase in ICP leads to elevated pressure gradient across the lamina cribrosa, that may cause posterior-globe flattening, disk edema, choroid folds, and a hyperopic shift [80, 82]. In addition, elevated cabin CO2, high-salt diet, and resistive exercise are considered potential secondary contributing factors [83]. But the exact reason and pathogenesis for VIIP is still unclear. Kramer et al. [84] observed that the upward fluid shifting in microgravity which led to intracranial and intra-orbital hypertension is similar to idiopathic intracranial hypertension (IIH) (also called pseudotumor cerebri). However, some authors suggest that elevated ICP is not the only cause of VIIP, because the astronauts had not experienced many clinical symptoms of IIH such as chronic hypertension [84].
Integrated Physiologic Countermeasures
Artificial Gravity
Artificial gravity (AG) is an effective countermeasure for the effects associated with weightlessness, either by using centrifugation with a rotating spacecraft, a short-arm centrifuge within the spacecraft, or exercise via lower body negative pressure [21]. A study indicated that orthostatic intolerance caused by bed rest can be mitigated by AG [85]. However, centrifuge-induced artificial gravity of the space stations is still a theory due to the excessive amount of energy needed to keep the station spinning, and it is very expensive as well [1]. So, in order to maintain the same effective results of centrifugation, we should use an early, low power, low-cost countermeasure such as exercise within LBNP. It is an integrated, non-expensive and well-tested countermeasure for long-term spaceflights [86]. It was indicated that combining AG with aerobic exercise has been noted effective on muscle sympathetic nerve activity and fluid shifts, it also restores cardiac and muscular functions as noted with centrifugation alone [87].
Lower Body Negative Pressure With and Without Exercise
Lower body negative pressure (LBNP) is a potential countermeasure to reverse the cranial fluid shift associated with weightlessness [88]. A previous study showed that during spaceflight LBNP was associated with reducing IJV area, but the reduction did not reach seated baseline IJV values. In addition, the left IJV blood flow improved in 59% of LBNP sessions during spaceflight [89]. Furthermore, a possibility of syncope during application is a risk; thus, medical monitoring is warranted [90]. Notably, LBNP was associated with improved blood flow patterns in most LBNP sessions during spaceflight and thus may be a promising countermeasure to blood flow stasis and thrombosis associated with spaceflight [89]. Recently, Marshall-Goebel et al. established a head-down-tilt (HDT) bed rest study on nine healthy males, indicating that the LBNP-induced reactions such as improving cerebral drainage and reducing CVP, CBF, and IOP make LBNP a candidate for the study of mechanisms for the development of VIIP [91]. LBNP alone is an effective method to prevent some of the head-ward fluid shifts in microgravity [92]. During exposure to LBNP, interstitial fluid pressure decreases in parallel with LBNP chamber pressure leads to increase in leg circumference significantly by shifting plasma to interstitial fluids, thus reducing cerebral and facial edema [93]. These changes affect the area around the optic nerve, where chronic increase in intracranial, intraocular, venous, and retinal pressures may cause visual impairment. Early development of a simple LBNP chamber with mild negative pressures in about 30 mmHg moves the fluids to the lower extremes for 6–8 h/day on ISS [86]. Such a system is useful while crew members are busy at work stations so that crew operations are not interrupted [86].
Since LBNP alone offers little protection against cardiovascular deconditioning, combinations with treadmill exercise have been suggested to be more efficient. This combined technique mitigate the microgravity-induced effects on human body [8]. Many studies were developed using a treadmill exercise protocol within LBNP during prolonged (30- and 60-day) bed rest [94,95,96], they had significant effects on different muscles and bones such as the endurance of knee extensor, in the non-exercise control group, decreased significantly but was maintained in the LBNP exercise group. A bone resorption detector was increased in the control group (urinary n-telopeptide excretion), but was not changed in the countermeasure group [97, 98]. Notably, cardiac mass increased significantly in the countermeasure group, but decreased in the control one [99]. Therefore, the treadmill exercise within LBNP maintained plasma volume, orthostatic tolerance within a degree (orthostatic tolerance time decreased in women-exercise group), upright exercise capacity, muscle strength, and sprint speed [100]. Applying lower body negative pressure during HDT position provide effective results on baroreflex sensitivity and distensibility of lower limb vessels [96]. These significant mitigations of body fluid shifting (blood, lymph, and CSF) protect against brain congestion and visual impairment during spaceflight.
Coagulation and LBNP
A study was conducted on 3 astronauts using LBNP, showed that their venous blood flow changed from stagnant or reverse (grade 3 or 4) to nominal flow (grade 1 or 2), indicating that LBNP can acutely improve IJV flow and potentially reduce thrombosis risk [89]. However, from another prospective, using LBNP may activate the coagulation process and increases risk for thrombosis. The pressure gradient produced by LBNP moves intravascular fluid to the lower body’s extravascular compartments and hence increases hemoconcentration level. This increases blood viscosity and plasma protein concentrations and enhances interactions between procoagulant factors and coagulation factors, thus activating procoagulant pathway [101]. Zaar et al. observed that exposure of healthy subjects to 10 min of 30 mmHg LBNP activates thrombin-generating part of the coagulation system such as thrombin anti-thrombin (TAT) complex levels. They reported that increases in TAT level associated with LBNP is also seen in the deep venous thrombosis patients and that the fluid shifts toward the legs is similar to those associated with prolonged sitting during bus or aircraft travels [102]. It was suggested that the increased sympathetic activity seen in both LBNP and bleeding may induce coagulation by activating endothelial beta-2 adrenergic receptors [103]. Cvirn et al. noted that the presyncope state (associated with LBNP) can also activate coagulation. At presyncope, plasma volume decreases and the hemoconcentration increases leading to increased blood viscosity. Presyncope also activates thrombin generation parameters (e.g., prothrombin fragments 1 and 2 and thrombin-antithrombin complexes) and increases endothelial activation markers such as tissue plasminogen activator and tissue factor, as well as thrombin generation parameters (e.g., prothrombin 1 and 2 and thrombin-antithrombin complexes) [104]. And all these factors generated by LBNP can lead to thrombosis.
Sodium Intake
It is important to mention the role of sodium in diet in altering visual acuity in some degree. Astronauts eat a low-sodium diet in attempt to avoid long-term visual damage. The daily sodium amount in diet of astronauts is about less than 3 g/day, because high sodium levels result in an osmotic shift of body fluid from the interstitial to the intravascular spaces leading to increased venous volume, congestion, and jugular venous outflow obstruction [105].
References
Gunga H-C, Ahlefeld VW von, Coriolano H-JA, Werner A, Hoffmann U. Cardiovascular system, red blood cells, and oxygen transport in microgravity. 2016.
Kanas N, Manzey D. Space psychology and psychiatry. Space Psychol Psychiatry. 2008.
Hughson RL, Helm A, Durante M. Heart in space: effect of the extraterrestrial environment on the cardiovascular system [Internet], vol. 15. Nature Publishing Group; 2018. p. 167–80.
Leguay G, Seigneuric A. Cardiac arrhythmias in space. Role of vagotonia. Acta Astronaut. 1981;8(7):795–801.
Urban J. Systems biology and cardiac arrhythmias Andrew. Lancet. 2010;5(3):379–90.
Vernice NA, Meydan C, Afshinnekoo E, Mason CE. Long-term spaceflight and the cardiovascular system. Precis Clin Med. 2020;3:284–91.
Anzai T, Frey MA, Nogami A. Cardiac arrhythmias during long-duration spaceflights [internet]. J Arrhythmia. 2014;30:139–49.
Hargens AR, Richardson S. Cardiovascular adaptations, fluid shifts, and countermeasures related to space flight. Respir Physiol Neurobiol. 2009;169:S30–3.
Blanchette M, Daneman R. Formation and maintenance of the BBB. Mech Dev. 2015;138:8–16.
Mao XW, Nishiyama NC, Byrum SD, Stanbouly S, Jones T, Holley J, et al. Spaceflight induces oxidative damage to blood-brain barrier integrity in a mouse model. FASEB J. 2020;34(11):15516–30.
Brightman MW, Reese TS. Junctions between intimately apposed cell membranes in the vertebrate brain. J Cell Biol. 1969;40(3):648–77.
Huber JD, Egleton RD, Davis TP. Molecular physiology and pathophysiology of tight junctions in the blood -brain barrier [Internet]. Trends Neurosci. 2001;24:719–25.
Reese TS, Karnovsky MJ. Fine structural localization of a blood-brain barrier to exogenous peroxidase. J Cell Biol. 1967;34(1):207–17.
Rubin LL, Staddon JM. The cell biology of the blood-brain barrier [Internet]. Annu Rev Neurosci. 1999;22:11–28.
Abbott NJ, Patabendige AAK, Dolman DEM, Yusof SR, Begley DJ. Structure and function of the blood-brain barrier [Internet]. Neurobiol Dis. 2010;37:13–25.
Bertler A, Falck B, Owman C, Rosengrenn E. The localization of monoaminergic blood-brain barrier mechanisms. Pharmacol Rev. 1966;18(1):369–85.
Minn A, Ghersi-Egea JF, Perrin R, Leininger B, Siest G. Drug metabolizing enzymes in the brain and cerebral microvessels. Brain Res Rev. 1991;16:65–82.
Haqqani AS, Hill JJ, Mullen J, Stanimirovic DB. The blood-brain and other neural barriers. Methods Mol Biol. 2011;686(1):337–53.
Laterra J, Keep R, Betz LA, Goldstein GW. Blood-cerebrospinal fluid barrier. In: Encyclopedia of psychopharmacology. Lippincott-Raven; 2015. p. 308.
Johanson CE. Choroid plexus-CSF neuropeptide involvement in intracranial pressure regulation: implications for the putative intracranial hypertension of spaceflight. Eur J Anat. 2013.
Zhang LF, Hargens AR. Spaceflight-induced intracranial hypertension and visual impairment: pathophysiology and countermeasures. Physiol Rev. 2018;98(1):59–87.
Hargens AR, Watenpaugh DE. Cardiovascular adaptation to spaceflight. Med Sci Sports Exerc. 1996;28:977–82.
Kirsch KA, Baartz FJ, Gunga HC, Röcker L, Wicke HJ, Bünsch B. Fluid shifts into and out of superficial tissues under microgravity and terrestrial conditions. Clin Investig. 1993;71(9):687–9.
Dunn CDR, Johnson PC, Lange RD. Regulation of hematopoiesis in rats exposed to antiorthostatic hypokinetic/hypodynamia. II. Mechanisms of the “anemia.”. Aviat Sp Environ Med. 1986;57(1):36–44.
McKeon J. Principles of clinical medicine for space flight. JAMA. 2009;301(8):884.
Ertl AC, Diedrich A, Biaggioni I, Levine BD, Robertson RM, Cox JF, et al. Human muscle sympathetic nerve activity and plasma noradrenaline kinetics in space. J Physiol. 2002;538(1):321–9.
Sahm PR, Keller MH, Schiewe B. Research in space: the German spacelab missions. Köln Germany: Wissenschaftliche Projektfuhrung D-2; 1993.
Gauer OH, Henry JP. Circulatory basis of fluid volume control. Physiol Rev. 1963;43:423–81.
Christensen NJ, Drummer C, Norsk P. Renal and sympathoadrenal responses in space. Am J Kidney Dis. 2001;38(3):679–83.
Cirillo M, De Santo NG, Heer M, Norsk P, Elmann-Larsen B, Bellini L, et al. Low urinary albumin excretion in astronauts during space missions. Nephron. 2003;93(4):p102–5.
Risso A, Turello M, Antonutto G. Effects of spaceflight on erithropoiesis: a study on neocytolysis. In: European Space Agency, (Special Publication) ESA SP 2008.
Churchill S. Fundamentals of space life sciences. Choice Rev Online. 1997;35(01):35-0262.
Coupé M, Fortrat JO, Larina I, Gauquelin-Koch G, Gharib C, Custaud MA. Cardiovascular deconditioning: from autonomic nervous system to microvascular dysfunctions. Respir Physiol Neurobiol. 2009;169(SUPPL):S10–2.
Grigoriev AI, Kotovskaya AR, Fomina GA. The human cardiovascular system during space flight. Acta Astronaut. 2011;68:1495–500.
Levine BD, Lane LD, Watenpaugh DE, Gaffney FA, Buckey JC, Blomqvist CG. Maximal exercise performance after adaptation to microgravity. J Appl Physiol. 1996;81(2):686–94.
Frey MAB. Space research activities during missions of the past. Med Sci Sports Exerc. 1996;28(10 SUPPL):3–8.
Zhao Z, Nelson AR, Betsholtz C, Zlokovic BV. Establishment and dysfunction of the blood-brain barrier. Cell Cell Press. 2015;163:1064–78.
Galley HF, Webster NR. Physiology of the endothelium. Br J Anaesth. 2004;93(1):105–13.
Cines DB, Pollak ES, Buck CA, Loscalzo J, Zimmerman GA, McEver RP, et al. Endothelial cells in physiology and in the pathophysiology of vascular disorders [Internet]. Blood Am Soc Hematol. 1998;91:3527–61.
Maier JAM, Cialdai F, Monici M, Morbidelli L. The impact of microgravity and hypergravity on endothelial cells. Biomed Res Int. 2015;2015:1–13.
Endemann DH, Schiffrin EL. Endothelial dysfunction. J Am Soc Nephrol. 2004;15(8):1983–92.
Versari S, Longinotti G, Barenghi L, Maier JAM, Bradamante S. The challenging environment on board the international Space Station affects endothelial cell function by triggering oxidative stress through thioredoxin interacting protein overexpression: the ESA-SPHINX experiment. FASEB J. 2013;27(11):4466–75.
Hughson RL, Robertson AD, Arbeille P, Shoemaker JK, Rush JWE, Fraser KS, et al. Increased postflight carotid artery stiffness and inflight insulin resistance resulting from 6-mo spaceflight in male and female astronauts. Am J Physiol Heart Circ Physiol. 2016;310(5):H628–38.
Delp MD, Charvat JM, Limoli CL, Globus RK, Ghosh P. Apollo lunar astronauts show higher cardiovascular disease mortality: possible deep space radiation effects on the vascular endothelium. Sci Rep. 2016;6.
Arbeille P, Provost R, Zuj K. Carotid and femoral artery intima-media thickness during 6 months of spaceflight. Aerosp Med Hum Perform. 2016;87(5):449–53.
Raichle ME, Gusnard DA. Appraising the brain’s energy budget [Internet]. Vol. 99, Proceedings of the National Academy of Sciences of the United States of America. National Academy of Sciences; 2002. p. 10237–9.
Nelson GA, Simonsen L, Huff JL, Cucinotta FA, Kim M-HY, Saha J, et al. Risk of acute (in-flight) or late central nervous system effects from radiation exposure. Sp Radiat Progr Elem 2016;NASA SP-20.
Andrews RN, Metheny-Barlow LJ, Peiffer AM, Hanbury DB, Tooze JA, Bourland JD, et al. Cerebrovascular remodeling and neuroinflammation is a late effect of radiation-induced brain injury in non-human primates. Radiat Res. 2017;187(5):599–611.
Craver BM, Acharya MM, Allen BD, Benke SN, Hultgren NW, Baulch JE, et al. 3D surface analysis of hippocampal microvasculature in the irradiated brain. Environ Mol Mutagen. 2016;57(5):341–9.
Cucinotta FA, Alp M, Sulzman FM, Wang M. Space radiation risks to the central nervous system. Vol. 2, Life sciences in space research. Elsevier Ltd; 2014. p. 54–69.
Cekanaviciute E, Rosi S, Costes SV. Central nervous system responses to simulated galactic cosmic rays [internet]. Int J Mol Sci MDPI AG. 2018;19.
Hanbury DB, Robbins ME, Bourland JD, Wheeler KT, Peiffer AM, Mitchell EL, et al. Pathology of fractionated whole-brain irradiation in rhesus monkeys (Macaca mulatta). Radiat Res. 2015;183(3):367–74.
Fauquette W, Amourette C, Dehouck MP, Diserbo M. Radiation-induced blood-brain barrier damages: an in vitro study. Brain Res. 2012;1433:114–26.
Lumniczky K, Szatmári T, Sáfrány G. Ionizing radiation-induced immune and inflammatory reactions in the brain [Internet]. Front Immunol. 2017;8.
Grabham P, Sharma P, Bigelow A, Geard C. Two distinct types of the inhibition of vasculogenesis by different species of charged particles. Vasc Cell. 2013;5(1).
Avolio A, Butlin M, Liu YY, Viegas K, Avadhanam B, Lindesay G. Regulation of arterial stiffness: cellular, molecular and neurogenic mechanisms. Vol. 5, Artery Research No longer published by Elsevier; 2011. p. 122–7.
Zieman SJ, Melenovsky V, Kass DA. Mechanisms, pathophysiology, and therapy of arterial stiffness [Internet]. Vol. 25, Arteriosclerosis, thrombosis, and vascular biology. Lippincott Williams & Wilkins; 2005. p. 932–43.
Tuday EC, Nyhan D, Shoukas AA, Berkowitz DE. Simulated microgravity-induced aortic remodeling. J Appl Physiol. 2009 Jun;106(6):2002–8.
Michael AP. Spaceflight induced changes in the central nervous system. In: Into space–a journey of how humans adapt and live in microgravity. InTech; 2018.
Scallan J, Huxley V, Korthuis R. Pathophysiology of edema formation. Capill Fluid Exch Regul Funct Pathol. 2010:58–9.
Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4:147ra111.
Leinonen V, Vanninen R, Rauramaa T. Cerebrospinal fluid circulation and hydrocephalus. Handb Clin Neurol. 2018.
Bothwell SW, Janigro D, Patabendige A. Cerebrospinal fluid dynamics and intracranial pressure elevation in neurological diseases. Fluids Barriers CNS. 2019;16(1):1–18.
Van Ombergen A, Jillings S, Jeurissen B, Tomilovskaya E, Rühl RM, Rumshiskaya A, et al. Brain tissue–volume changes in cosmonauts. N Engl J Med. 2018.
Van Ombergen A, Jillings S, Jeurissen B, Tomilovskaya E, Rumshiskaya A, Litvinova L, et al. Brain ventricular volume changes induced by long-duration spaceflight. Proc Natl Acad Sci U S A. 2019;116(21):10531–6.
Dreha-Kulaczewski S, Konopka M, Joseph AA, Kollmeier J, Merboldt KD, Ludwig HC, et al. Respiration and the watershed of spinal CSF flow in humans. Sci Rep. 2018; 8.
Dreha-Kulaczewski S, Joseph AA, Merboldt KD, Ludwig HC, Gärtner J, Frahm J. Identification of the upward movement of human CSF in vivo and its relation to the brain venous system. J Neurosci. 2017;37:2395–402.
Ludwig HC, Frahm J, Gärtner J, Dreha-Kulaczewski S. Breathing drives CSF: Impact on spaceflight disease and hydrocephalus [Internet]. Vol. 116, Proceedings of the National Academy of Sciences of the United States of America. 2019. p. 20263–4.
Kawai Y, Doi M, Setogawa A, Shimoyama R, Ueda K, Asai Y, et al. Effects of microgravity on cerebral hemodynamics. Yonago Acta Medica. 2003.
Lee AG, Mader TH, Gibson CR, Tarver W. Space flight-associated neuro-ocular syndrome. JAMA Ophthalmol. 2017;135:992–4.
Wilson MH, Imray CHE, Hargens AR. The headache of high altitude and microgravity-similarities with clinical syndromes of cerebral venous hypertension. High Alt Med Biol. 2011;12(4):379–86.
Martin DS, Lee SMC, Matz TP, Westby CM, Scott JM, Stenger MB, et al. Internal jugular pressure increases during parabolic flight. Physiol Rep. 2016;4(24):e13068.
Taibbi G, Cromwell RL, Kapoor KG, Godley BF, Vizzeri G. The effect of microgravity on ocular structures and visual function: a review. Surv Ophthalmol. 2013;58:155–63.
Previtali E, Bucciarelli P, Passamonti SM, Martinelli I. Risk factors for venous and arterial thrombosis. Blood Transfus. 2011.
de Bastos M, Stegeman BH, Rosendaal FR, Van Hylckama Vlieg A, Helmerhorst FM, Stijnen T, et al. Combined oral contraceptives: venous thrombosis. Cochrane Database Syst Rev. 2014.
Van Hylckama VA, Helmerhorst FM, Vandenbroucke JP, Doggen CJM, Rosendaal FR. The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: results of the MEGA case-control study. BMJ. 2009;339:b2921.
Heer M, Paloski WH. Space motion sickness: incidence, etiology, and countermeasures. Auton Neurosci Basic Clin. 2006;129:77–9.
Hargens AR. Fluid shifts in vascular and extravascular spaces during and after simulated weightlessness. Med Sci Sports Exerc. 1983;15:421–7.
Thornton W, Bonato F. The human body and weightlessness: operational effects, problems and countermeasures. The human body and weightlessness: operational effects, problems and countermeasures. Springer International Publishing; 2017. 1–320 p.
Mader TH, Gibson CR, Pass AF, Kramer LA, Lee AG, Fogarty J, et al. Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmology. 2011;118(10):2058–69.
Alexander DJ, Gibson CR, Hamilton DR, Lee SMC, Mader TH, Otto C, et al. Risk of spaceflight-induced intracranial hypertension and vision alterations. HumanresearchroadmapNasaGov; 2012.
Mader TH, Gibson CR, Pass AF, Lee AG, Killer HE, Hansen HC, et al. Optic disc edema in an astronaut after repeat long-duration space flight. J Neuro-Ophthalmol. 2013;33:249–55.
Marshall-Bowman K, Barratt MR, Gibson CR. Ophthalmic changes and increased intracranial pressure associated with long duration spaceflight: an emerging understanding. Acta Astronaut. 2013;87:77–87.
Kramer LA, Sargsyan AE, Hasan KM, Polk JD, Hamilton DR. Orbital and intracranial effects of microgravity: findings at 3-T MR imaging. Radiology. 2012;263:819–27.
Nicogossian AE, Williams RS, Huntoon CL, Doarn CR, Polk JD, Schneider VS. Space physiology and medicine: from evidence to practice, fourth edition. Space physiology and medicine: from evidence to practice, 4th edn. New York: Springer; 2016. 1–509 p.
Hargens AR, Bhattacharya R, Schneider SM. Space physiology VI: exercise, artificial gravity, and countermeasure development for prolonged space flight. Eur J Appl Physiol. 2013;113:2183–92.
Iwase S, Takada H, Watanabe Y, Ishida K, Akima H, Katayama K, et al. Effect of centrifuge-induced artificial gravity and ergometric exercise on cardiovascular deconditioning, myatrophy, and osteoporosis induced by a −6 degrees head-down bedrest. J Gravit Physiol. 2004;11:P243–4.
Petersen LG, Hargens A, Bird EM, Ashari N, Saalfeld J, Petersen JCG, et al. Mobile lower body negative pressure suit as an integrative countermeasure for spacelight. Aerosp Med Hum Perform. 2019;90(12):993–9.
Auñón-Chancellor SM, Pattarini JM, Moll S, Sargsyan A. Venous thrombosis during spaceflight. N Engl J Med. 2020;382(1):89–90.
Campbell MR, Charles JB. Historical review of lower body negative pressure research in space medicine. Aerosp Med Hum Perform. 2015;86(7):633–40.
Marshall-Goebel K, Terlević R, Gerlach DA, Kuehn S, Mulder E, Rittweger J. Lower body negative pressure reduces optic nerve sheath diameter during head-down tilt. J Appl Physiol. 2017;123:1139–44.
Murthy G, Watenpaugh DE, Ballard RE, Hargens AR. Exercise against lower body negative pressure as a countermeasure for cardiovascular and musculoskeletal deconditioning. Acta Astronaut. 1994;33(C):89–96.
Aratow M, Fortney SM, Watenpaugh DE, Crenshaw AG, Hargens AR. Transcapillary fluid responses to lower body negative pressure. J Appl Physiol. 1993;74:2763–70.
Lee SMC, Schneider SM, Boda WL, Watenpaugh DE, Macias BR, Meyer RS, et al. Supine LBNP exercise maintains exercise capacity in male twins during 30-d bed rest. Med Sci Sports Exerc. 2007;39:1315–26.
Hargens AR, Whalen RT, Watenpaugh DE, Schwandt DF, Krock LP. Lower body negative pressure to provide load bearing in space. Aviat Sp Environ Med. 1991.
Guinet P, Schneider SM, Macias BR, Watenpaugh DE, Hughson RL, Le Traon AP, et al. WISE-2005: effect of aerobic and resistive exercises on orthostatic tolerance during 60 days bed rest in women. Eur J Appl Physiol. 2009;106:217–27.
Zwart SR, Hargens AR, Lee SMC, Macias BR, Watenpaugh DE, Tse K, et al. Lower body negative pressure treadmill exercise as a countermeasure for bed rest-induced bone loss in female identical twins. Bone. 2007;40:529–37.
Smith SM, Davis-Street JE, Fesperman JV, Calkins DS, Bawa M, Macias BR, et al. Evaluation of treadmill exercise in a lower body negative pressure chamber as a countermeasure for weightlessness-induced bone loss: a bed rest study with identical twins. J Bone Miner Res. 2003;18:2223–30.
Dorfman TA, Levine BD, Tillery T, Peshock RM, Hastings JL, Schneider SM, et al. Cardiac atrophy in women following bed rest. J Appl Physiol. 2007;103:8–16.
Lee SMC, Schneider SM, Boda WL, Watenpaugh DE, Macias BR, Meyer RS, et al. LBNP exercise protects aerobic capacity and sprint speed of female twins during 30 days of bed rest. J Appl Physiol. 2009;106:919–28.
Goswami N, Taucher AA, Brix B, Roessler A, Koestenberger M, Reibnegger G, et al. Coagulation changes during central hypovolemia across seasons. J Clin Med. 2020;9(11):3461.
Zaar M, Johansson PI, Nielsen LB, Crandall CG, Shibasaki M, Hilsted L, et al. Early activation of the coagulation system during lower body negative pressure. Clin Physiol Funct Imaging. 2009;29:427–30.
van Helmond N, Johnson BD, Curry TB, Cap AP, Convertino VA, Joyner MJ. Coagulation changes during lower body negative pressure and blood loss in humans. Am J Physiol Heart Circ Physiol. 2015;309:H1591–7.
Cvirn G, Schlagenhauf A, Leschnik B, Koestenberger M, Roessler A, Jantscher A, et al. Coagulation changes during presyncope and recovery. PLoS One. 2012;7:e42221.
Lane HW, Bourland C, Barrett A, Heer M, Smith SM. The role of nutritional research in the success of human space flight. Adv Nutr. 2013;4:521–3.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sayed, A.H., Hargens, A.R. (2022). Cardiovascular Physiology and Fluid Shifts in Space. In: Michael, A.P., Otto, C., Reschke, M.F., Hargens, A.R. (eds) Spaceflight and the Central Nervous System. Springer, Cham. https://doi.org/10.1007/978-3-031-18440-6_2
Download citation
DOI: https://doi.org/10.1007/978-3-031-18440-6_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-18439-0
Online ISBN: 978-3-031-18440-6
eBook Packages: MedicineMedicine (R0)